
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
80 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
CASE STUDY
“Tom” is a 23-year-old, single, white male who
present- ed for treatment approximately 1 year
after a traumatic event that occurred during his
military service in Iraq. Tom received CPT while
on active duty in the Army.
Background
Tom was born the third of four children to his
parents. He described his father as an alcoholic
who was frequently absent from the home due to
work travel prior to his parents’ divorce. Tom
indicated that his father was always emotionally
distant from the family, especially after the
divorce. Tom had close relationships with his
mother and siblings. He denied having any
significant mental health or physical health
problems in his childhood. However, he described
two significant traumatic events in his
adolescence. Specifically, he described witnessing
his best friend commit suicide by gunshot to the
head. Tom indicated that this event severely
affected him, as well as his entire community. He
went on to report that he still felt responsible for
not preventing his friend’s suicide. The second
traumatic event was the death of Tom’s brother in
an automobile accident when Tom was 17 years
old. Tom did not receive any mental health
treatment during his childhood or after these
events, though he indicated that he began using
alcohol and illicit substances after these traumatic
events in his youth. He admitted to using
cannabis nearly daily during high school, as well
as daily use of alcohol, drinking as much as a 24-
pack of beer per day until he passed out. Tom
reported that he decreased his alcohol
consumption and ceased using cannabis after his
enlistment.
Tom served in the Infantry. He went to Basic
Training, then attended an advanced training
school prior to being deployed directly to Iraq.
While in Iraq, Tom witnessed and experienced a
number of traumatic incidents. He spoke about
fellow soldiers who were killed and injured in
service, as well as convoys that he witnessed
being hit by improvised explosive devices (IEDs).
However, the traumatic event that he identified
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
81
as most distressing and anxiety-provoking was shoot-
ing a pregnant woman and child.
Tom described this event as follows: Suicide bomb-
ers had detonated several bombs in the area where Tom
served, and a control point had been set up to contain
the area. During the last few days of his deployment,
Tom was on patrol at this control point. It was dark out-
side. A car began approaching the checkpoint, and of-
ficers on the ground signaled for the car to stop. The car
did not stop in spite of these warnings. It continued to
approach the control point, entering the area where the
next level of Infantrymen were guarding the entrance.
Per protocol, Tom fired a warning shot to stop the ap-
proaching car, but the car continued toward the control
point. About 25 yards from the control point gate, Tom
and at least one other soldier fired upon the car several
times.
After a brief period of disorientation, a crying man
with clothes soaked with blood emerged from the car
with his hands in the air. The man quickly fell to his
knees, with his hands and head resting on the road.
Tom could hear the man sobbing. According to Tom,
the sobs were guttural and full of despair. Tom looked
over to find in the pedestrian seat a dead woman who
was apparently pregnant. A small child in the backseat
was also dead. Tom never confirmed this, but he and
his fellow soldiers believed that the man crying on the
road was the husband of the woman and the father of
the child and fetus.
Tom was immediately distressed by the event, and a
Combat Stress Control unit in the field eventually had
him sent back to a Forward Operating Base because
of his increasing reexperiencing and hypervigilance
symptoms. Tom was eventually brought to a major
Army hospital and received individual CPT within this
setting.
Tom was administered the CAPS at pretreatment;
his score was in the severe range, and he met diagnostic
criteria for PTSD. He also completed the Beck Depres-
sion Inventory–II (BDI-II) and the State–Trait Anxiety
Inventory (STAI). His depression and anxiety symp-
toms at pretreatment were in the severe range. Tom was
provided feedback about his assessment results in a
session focused on an overview of his psychological as-
sessment results and on obtaining his informed consent
for a course of CPT. After providing feedback about
his assessment, the therapist gave Tom an overview of
CPT, with an emphasis on its trauma-focused nature,
expectation of out-of-session practice adherence, and
the client’s active role in getting well. Tom signed a
“CPT Treatment Contract” detailing this information
and was provided a copy of the contract for his records.
The CPT protocol began in the next session.
Session 1
Tom arrived 15 minutes prior to his first scheduled ap-
pointment of CPT. He sat down in the chair the therapist
gestured that he sit in, but he was immediately restless
and repositioned frequently. Tom quickly asked to move
to a different chair in the room, so that his back was
not facing the exterior door and his gaze could monitor
both the door and the window. He asked the therapist
how long his session would take and whether he would
have to “feel anything.” The therapist responded that
this session would last 50–60 minutes, and that, com-
pared with other future sessions, she would be doing
most of the talking. She added that, as discussed during
the treatment contracting session, the focus would be
on Tom’s feelings in reaction to the traumatic event but
that the current session would focus less on this. The
therapist also explained that she would have the treat-
ment manual in her lap, and would refer to it throughout
to make sure that she delivered the psychotherapy as it
was prescribed. She encouraged Tom to ask any ques-
tions he might have as the session unfolded.
The therapist explained that at the beginning of each
session they would develop an agenda for the session.
The purposes of the first therapy session were to (1)
describe the symptoms of PTSD; (2) give Tom a frame-
work for understanding why these symptoms had not
remitted; (3) present an overview of treatment to help
Tom understand why practice outside of session and
therapy attendance were important to elicit cooperation
and to explain the progressive nature of the therapy; (4)
build rapport between Tom and the therapist; and (5)
give the client an opportunity to talk briefly about his
most distressing traumatic event or other issues.
The therapist then proceeded to give didactic infor-
mation about the symptoms of PTSD. She asked Tom
to provide examples of the various clusters of PTSD
symptoms that he was experiencing, emphasizing how
reexperiencing symptoms are related to hyperarousal
symptoms, and how hyperarousal symptoms elicit a
desire to avoid or become numb. The paradoxical ef-
fect of avoidance and numbing in maintaining, or even
increasing, PTSD symptoms was also discussed. Tom
indicated that this was the first time someone had ex-
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
82 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
plained the symptoms of PTSD in this way, putting
them “in motion” by describing how they interact with
one another.
The therapist transitioned to a description of trauma
aftereffects within an information-processing frame-
work. She described in lay terms how traumas may be
schema-discrepant events; traumatic events often do
not fit with prior beliefs about oneself, others, or the
world. To incorporate this event into one’s memory,
the person may alter his/her perception of the event
(assimilate the event into an existing belief system).
Examples of assimilation include looking back on the
event and believing that some other course of action
should have been taken (“undoing” the event) or blam-
ing oneself because it occurred. The therapist went
on to explain that Tom could have also attempted to
change his prior belief system radically to overaccom-
modate the event to his prior beliefs. “Overaccommo-
dation” was described as changing beliefs too much as
a result of the traumatic event (e.g., “I can’t trust myself
about anything”). She explained that several areas of
beliefs are often affected by trauma, including safety,
trust, power/control, esteem, and intimacy. She further
explained that these beliefs could be about the self and/
or others. The therapist also pointed out that if Tom had
negative beliefs prior to the traumatic event relative to
any of these topics, the event could serve to strengthen
these preexisting negative beliefs.
At this point, Tom described his childhood and ado-
lescent experiences, and how they had contributed to
his premilitary trauma beliefs. The therapist noted that
Tom tended to blame himself and to internalize the bad
things that had happened in his family and the suicide
of his friend. She also noted his comment, “I wonder if
my father drank to cope with me and my siblings.” In
Tom’s case, it seemed likely that the traumatic experi-
ence served more to confirm his preexisting beliefs that
he had caused or contributed to bad things happening
around and to him.
Tom then spent some time describing how drasti-
cally things had changed after his military traumas.
Prior to his military experiences and, specifically, the
shooting of the woman and child, Tom described him-
self as “proud of being a soldier” and “pulling his life
together.” He indicated that the military structure had
been very good for him in developing self-discipline
and improving his self-esteem. He indicated that he
felt good about “the mission to end terrorism” and was
proud to serve his country. He felt camaraderie with his
fellow soldiers and considered a career in the military.
He denied any authority problems and in fact believed
that his commanding officers had been role models
of the type of leader he wished to be. Prior to his de-
ployment to Iraq, Tom met and married his wife, and
they appeared to have a stable, intimate relationship.
After his return from Iraq, Tom indicated that he did
not trust anyone, especially anyone associated with the
U.S. government. Tom expressed his disillusionment
with the war effort and distrust of the individuals who
commanded his unit. He also articulated distrust of
himself: “I always make bad decisions when the chips
are down.” He stated that he felt completely unsafe in
his environment. In his immediate postdeployment pe-
riod, Tom had occasionally believed snipers on the base
grounds had placed him in their crosshairs to kill him.
He indicated that he minimally tolerated being close
to his wife, including sexual contact between the two
of them.
The therapist introduced the notion of “stuck points,”
or ways of making sense of the trauma or of thinking
about himself, others, and the world, as getting in the
way of Tom’s recovery from the traumatic events. The
therapist noted that a large number of individuals are
exposed to trauma. In fact, military personnel are
among the most trauma-exposed individuals. However,
most people recover from their trauma exposure. Thus,
a primary goal of the therapy was to figure out what had
prevented Tom from recovering (i.e., how his thinking
had got him “stuck,” leading to the maintenance of his
PTSD symptoms).
The therapist then asked Tom to provide a 5-minute
account of his index traumatic event. Tom immediately
responded, “There were so many bad things over there.
How could I pick one?” The therapist asked, “Which of
those events do you have the most thoughts or images
about? Which of those events do you dislike thinking
about the most?” The therapist indicated that Tom did
not need to provide a fine-grained description of the
event, but rather a brief overview of what happened.
Tom provided a quick account of the shooting of the
woman and child. The therapist praised Tom for shar-
ing about the event with her and asked about his feel-
ings as a result of sharing the information. Tom said
that he felt anxious and wanted the session to be over.
The therapist used this as an opportunity to describe
the differences between “natural” and “manufactured”
emotions.
The therapist first described “natural” emotions as
those feelings that are commensurate reactions to expe-
riences that have occurred. For example, if we perceive
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
83
that someone has wronged us, it is natural to feel anger.
If we encounter a threatening situation, it is natural to
feel fear. Natural emotions have a self-limited and di-
minishing course. If we allow ourselves to feel these
natural emotions, they will naturally dissipate. The
therapist used the analogy of the energy contained in
a bottle of carbonated soda to illustrate this concept.
If the top of the bottle is removed, the pressure ini-
tially comes out with some force, but that force sub-
sides and eventually has no energy forthcoming. On
the other hand, there are “manufactured” emotions,
or emotions that a person has a role in making. Our
thoughts contribute to the nature and course of these
emotions. The more that we “fuel” these emotions with
our self-statements, the more we can increase the “pres-
sure” of these emotions. For example, if a person tells
himself over and over that he is a stupid person and
reminds himself of more and more situations in which
he perceived that he made mistakes, then he is likely to
have more and more anger toward himself. The thera-
pist reiterated that the goals of the therapy were (1) to
allow Tom to feel the natural emotions he has “stuffed,”
which keep him from recovering from his trauma; and
(2) to figure out how Tom was manufacturing emotions
that were unhelpful to him.
The therapist summarized for Tom the three major
goals of the therapy: (1) to remember and to accept
what happened to him by not avoiding those memories
and associated emotions; (2) to allow himself to feel his
natural emotions and let them run their course, so the
memory could be put away without such strong feelings
still attached; and (3) to balance beliefs that had been
disrupted or reinforced, so that Tom did not manufac-
ture unhelpful emotions.
The therapist made a strong pitch for the importance
of out-of-session practice adherence before assigning
Tom the first practice assignment. The therapist told
Tom that there appeared to be no better predictor of
response to the treatment than how much effort a pa-
tient puts into it. She pointed out that of the 168 hours
in a week, Tom would be spending 1–2 hours of that
week in psychotherapy sessions (Note. We have found
it helpful to do twice-weekly sessions, at least in the
initial portion of the therapy, to facilitate rapport build-
ing, to overcome avoidance, and to capitalize on early
gains in the therapy.) If Tom only spent the time dur-
ing psychotherapy sessions focused on these issues, he
would be spending less than 1% of his week focused
on his recovery. To get better, he would be using daily
worksheets and other writing assignments to promote
needed skills in his daily life and to decrease his avoid-
ance. The therapist also pointed out that at the begin-
ning of each session they would review the practice as-
signments that Tom had completed. The therapist asked
Tom if this made sense, and he responded, “Sure. It
makes sense that you get out of it what you put into it.”
Tom’s first assignment was to write an Impact State-
ment about the meaning of the event to determine how
he had made sense of the traumatic event, and to help
him begin to determine what assimilation, accommo-
dation, and overaccommodation had occurred since
the event. Stuck points that get in the way of recovery
are identified with this first assignment. Tom was in-
structed to start writing the assignment later that day
to address directly any avoidance about completing the
assignment. He was specifically reminded that this was
not a trauma account (that would come later) and that
this assignment was specifically designed to get at the
meaning of the event in his life, and how it had im-
pacted his belief systems.
The specific assignment was as follows:
Please write at least one page on what it means to
you that you that this traumatic experience happened.
Please consider the effects that the event has had on
your beliefs about yourself, your beliefs about others,
and your beliefs about the world. Also consider the fol-
lowing topics while writing your answer: safety, trust,
power/competence, esteem, and intimacy. Bring this
with you to the next session.
Session 2
The purposes of the second session are (1) to discuss
the meaning of the event and (2) to help Tom begin to
recognize thoughts, label emotions, and see the con-
nection between what he says to himself and how he
feels. Tom arrived with obvious anger and appeared
defensive throughout most of the session. He stated
that he had been feeling quite angry all week, and that
he was “disgusted” with society and particularly poli-
ticians, who were “all self-interested or pandering to
those with money.” He expressed a great deal of anger
over the reports of alleged torture at Abu Ghraib pris-
on, which was a major news item during his therapy.
The therapist was interested in the thinking behind
Tom’s anger about the events at Abu Ghraib. However,
she first reviewed Tom’s practice assignment, writing
the first Impact Statement, to reinforce the completion
of this work and to maintain the session structure she
had outlined in the first session.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
84 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
The therapist asked Tom to read his Impact State-
ment aloud. Clients in individual CPT are always asked
to read their practice assignments aloud. Should the
therapist read them, the client could dissociate or oth-
erwise avoid his/her own reactions to their material.
Tom had written:
The reason that this traumatic event happened is be-
cause I was friggin’ stupid and made a bad decision.
I killed an innocent family, without thinking. I mur-
dered a man’s wife and child. I can’t believe that I did
it. I took that man’s wife and child, and oh, yeah, his
unborn child, too. I feel like I don’t deserve to live, let
alone have a wife and child on the way. Why should I be
happy when that man was riddled with despair, and that
innocent woman, child, and unborn child died? Now, I
feel like I’m totally unsafe. I don’t feel safe even here
on the hospital grounds, let alone in the city or back
home with my family. I feel like someone is watching
me and is going to snipe at me and my family because
the terrorists had information about the situation and
passed it on. I also don’t feel that people are safe around
me. I might go off and hurt someone, and God forbid
it be my own family. With my wife pregnant, I am re-
ally concerned that I might hurt her. I don’t trust any-
one around me, and especially the government. I don’t
even trust the military treating me. I also don’t trust
myself. If I made a bad decision at that time, who is
to say that I won’t make a bad decision again? About
power and control, I feel completely out of control of
myself, and like the military and my commanding of-
ficer have complete control over me. My self-esteem is
in the toilet. Why wouldn’t it be given the crappy things
that I have done? I don’t think there are many positive
things that I’ve done with my life, and when the chips
are down, I always fail and let others down. I’m not sure
what other-esteem is, but I do like my wife. In fact, I
don’t think she deserves to have to deal with me, and I
think they would be better without me around. I don’t
want to be close to my wife, or anyone else for that mat-
ter. It makes me want to crawl out of my skin when my
wife touches me. I feel like I’ll never get over this. It
wasn’t supposed to be like this.
The therapist asked Tom what it was like to write and
then read the Impact Statement aloud. Tom responded
that it had been very difficult, and that he had avoided
the assignment until the evening before his psycho-
therapy session. The therapist immediately reinforced
Tom for his hard work in completing the assignment.
She also used the opportunity to gently address the
role of avoidance in maintaining PTSD symptoms. She
asked specific Socratic questions aimed at elucidating
the distress associated with anticipatory anxiety, and
wondered aloud with Tom about what it would have
been like to have completed the assignment earlier in
the week. She also asked Socratic questions aimed at
highlighting the fact that Tom felt better, not worse,
after completing the assignment.
Tom’s first Impact Statement and the information he
shared in the first session made evident the stuck points
that would have to be challenged. In CPT, areas of as-
similation are prioritized as the first targets of treat-
ment. Assimilation is targeted first because changes
in the interpretation of the event itself are integrally
related to the other, more generalized beliefs involved
in overaccommodation. In Tom’s case, he was assimi-
lating the event by blaming himself. He used the term
“murderer” to describe his role in the event, disregard-
ing important contextual factors that surrounded the
event. These beliefs would be the first priority for chal-
lenging. Tom’s overaccommodation is evident in his
general distrust of society and authority figures, and his
belief that he will make bad decisions in difficult situ-
ations. His overaccommodation is also evident in his
sense of threat in his environment (e.g., snipers), dif-
ficulty being emotionally and physically intimate with
his wife, and low esteem for others and himself.
The therapist returned to Tom’s anger about Abu
Ghraib to get a better sense of possible stuck points, and
also to experiment with Tom’s level of cognitive rigid-
ity or openness to cognitive challenging. The following
exchange ensued between Tom and the therapist:
T
HERAPIST: Earlier you mentioned that you were feel-
ing angry about the reports from Abu Ghraib. Can
you tell me what makes you angry?
T
OM: I can’t believe that they would do that to those
prisoners.
T
HERAPIST: What specifically upsets you about Abu
Ghraib?
T
OM: Haven’t you heard the reports? I can’t believe that
they would humiliate and hurt them like that. Once
again, the U.S. military’s use of force is unaccept-
able.
T
HERAPIST: Do you think your use of force as a mem-
ber of the U.S. military was unacceptable?
T
OM: Yes. I murdered innocent civilians. I am no dif-
ferent than those military people at Abu Ghraib. In
fact, I’m worse because I murdered them.
T
HERAPIST: “Murder.” That’s a strong word.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
85
TOM: Yeah?
T
HERAPIST: From what you’ve told me, it seems like
you killed some people who may or may not have
been “innocent.” Your shooting occurred in a very
specific place and time, and under certain circum-
stances.
T
OM: Yes, they died at my hands.
T
HERAPIST: Yes, they died, and it seems, at least in
part, because of your shooting. Does that make you
a murderer?
T
OM: Innocent people died and I pulled the trigger. I
murdered them. That’s worse than what happened at
Abu Ghraib.
T
HERAPIST: (quietly) Really, you think it is worse?
T
OM: Yes. In one case, people died, and in another they
didn’t. Both are bad, and both were caused by sol-
diers, but I killed people and they didn’t.
T
HERAPIST: The outcomes are different—that is true.
I’m curious if you think how it happened matters?
T
OM: Huh?
T
HERAPIST: Does it matter what the soldiers’ intentions
were in those situations, regardless of the outcome?
T
OM: No. The bottom line is killing versus no killing.
T
HERAPIST: (realizing that there was minimal flexibil-
ity at this point) I agree that there is no changing the
fact that the woman and child died, and that your
shooting had something to do with that. However,
I think we might slightly disagree on the use of the
term “murder.” It is clear that their deaths have been
a very difficult thing for you to accept, and that you
are trying to make sense of that. The sense that you
appear to have made of their deaths is that you are a
“murderer.” I think this is a good example of one of
those stuck points that seem to have prevented you
from recovering from this traumatic event. We’ll
definitely be spending more time together on under-
standing your role in their deaths.
In addition to testing Tom’s cognitive flexibility,
the therapist also wanted to plant the seeds of a dif-
ferent interpretation of the event. She was careful not
to push too far and retreated when it was clear that
Tom was not amenable to an alternative interpretation
at this point in the therapy. He was already defensive
and somewhat angry, and she did not want to exacer-
bate his defensiveness or possibly contribute to dropout
from the therapy.
From there, the therapist described how important it
was to be able to label emotions and to begin to iden-
tify what Tom was saying to himself. The therapist and
Tom discussed how different interpretations of events
can lead to very different emotional reactions. They
generated several examples of how changes in thoughts
result in different feelings. The therapist also reminded
Tom that some interpretations and reactions follow
naturally from situations and do not need to be altered.
For example, Tom indicated that he was saddened by
the death of the family; the therapist did not challenge
that statement. She encouraged Tom to feel his sadness
and to let it run its course. He recognized that he had
lost something, and it was perfectly natural to feel sad
as a result. At this point Tom responded, “I don’t like to
feel sad. In fact, I don’t like to feel at all. I’m afraid I’ll
go crazy.” The therapist gently challenged this belief.
“Have you ever allowed yourself to feel sad?” Tom re-
sponded that he worked very hard to avoid any and all
feelings. The therapist encouraged Tom, “Well, given
that you don’t have much experience with feeling your
feelings, we don’t know that you’re going to go crazy
if you feel your feelings, right?” She also asked him
whether he had noticed anyone in his life who had felt
sad and had not gone crazy. He laughed. The therapist
added, “Not feeling your feelings hasn’t been working
for you so far. This is your opportunity to experiment
with feeling these very natural feelings about the trau-
matic event to see whether it can help you recover now
from what has happened.”
Tom was given a number of A-B-C Sheets as prac-
tice assignments to begin to identify what he was telling
himself and his resulting emotions. In the first column,
under A, “Something happens,” Tom was instructed
to write down an event. Under the middle column, B,
“I tell myself something,” he was asked to record his
thoughts about the event. Under column C, “I feel and/
or do something,” Tom was asked to write down his
behavioral and emotional responses to the event. The
therapist pointed out that if Tom says something to
himself a lot, it becomes automatic. After a while, he
does not need to think the thought consciously, he can
go straight to the feeling. It is important to stop and rec-
ognize automatic thoughts to decide whether they ei-
ther make sense or should be challenged and changed.
Session 3
Tom handed the therapist his practice assignments as
soon as he arrived. The therapist went over the individ-

From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
86 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
ual A-B-C Sheets Tom had completed and emphasized
that he had done a good job in identifying his feelings
and recognizing his thoughts. Some of this work is
shown in Figure 2.1.
The purpose of reviewing this work at this point in
the therapy is to identify thoughts and feelings, not to
heavily challenge the content of those thoughts. The
therapist did a minor correction of Tom’s identification
of the thought “I feel like I’m a bad person” (bolded
in Figure 2.1) as a feeling. She commented that feel-
ings are almost always one word and what you feel in
your “gut,” and that adding the stem “I feel . . . ” does
not necessarily make it a feeling. The therapist noticed
the pattern of thoughts that Tom tended to record (i.e.,
internalizing and self-blaming), as well as the charac-
teristic emotions he reported.
The therapist noted the themes of assimilation that
again emerged (i.e., self-blame) and chose to focus on
mildly challenging these related thoughts. She specifi-
cally chose to focus on Tom’s thoughts and feelings re-
lated to his wife’s pregnancy, which ultimately seemed
to be related to his assimilation of the traumatic event.
T
HERAPIST: You don’t think you deserve to have a fam-
ily? Can you say more about that?
T
OM: Why should I get to have a family when I took
someone else’s away?
T
HERAPIST: OK, so it sounds like this relates to the first
thought that you wrote down on the A-B-C Sheet
about being a murderer. When you say to yourself, “I
took someone else’s family away,” how do you feel?
T
OM: I feel bad.
T
HERAPIST: Let’s see if we can be a bit more precise.
What brand of bad do you feel? Remember how we
talked about the primary colors of emotion? Which
of those might you feel?
T
OM: I feel so angry at myself for doing what I did.
T
HERAPIST: OK. Let’s write that down—anger at self.
So, I’m curious, Tom, do the other people you’ve told
about this situation, or who were there at the time,
think what you did was wrong?
T
OM: No, but they weren’t the ones who did it, and they
don’t care about the Iraqi people like I do.
ACTIVATING EVENT
A
“Something happens”
BELIEF
B
“I tell myself something”
CONSEQUENCE
C
“I feel something”
I killed an innocent family. “I am a murderer.” I feel like I’m a bad person.
Avoid talking about it.
My wife is pregnant. “I don’t deserve to have a family.” Guilty
Abu Ghraib “The government sucks.” Angry
Going to therapy
“I’m weak. I shouldn’t have PTSD.
PTSD is only for the weak.”
Angry
Are my thoughts in B realistic?
Yes.
What can you tell yourself on such occasions in the future?
?
FIGURE 2.1.
A-B-C Sheet.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
87
THERAPIST: Hmm . . . that makes me think about some-
thing, Tom. In the combat zone in which you were
involved in Iraq, how easy was it to determine who
you were fighting?
T
OM: Not always particularly easy. There were lots of
insurgents who looked like everyday people.
T
HERAPIST: Like civilians? Innocent civilians? (pause)
T
OM: I see where you are going. I feel like it is still
wrong because they died.
T
HERAPIST: I believe you when you say that it feels that
way. However, feeling a certain way doesn’t neces-
sarily mean that it is based on the facts or the truth.
We’re going to work together on seeing whether that
feeling of guilt or wrongdoing makes sense when we
look at the situation very carefully in our work to-
gether.
Because the goal is for Tom to challenge and dis-
mantle his own beliefs, the therapist probed and plant-
ed seeds for alternative interpretations of the traumatic
event but did not pursue the matter too far. Although
Tom did move some from his extreme stance within the
session, the therapist was not expecting any dramatic
changes. She focused mostly on helping Tom get the
connections among thoughts, feelings, and behaviors,
and developing a collaborative relationship in which
cognitive interventions could be successfully delivered.
The therapist praised Tom for his ability to recog-
nize and label thoughts and feelings, and said that she
wanted Tom to attend to both during the next assign-
ment, which was writing about the index traumatic
event. Tom was asked to write as his practice assign-
ment a detailed account of the event, and to include
as many sensory details as possible. He was asked to
include his thoughts and feelings during the event. He
was instructed to start as soon as possible on the assign-
ment, preferably that day, and to pick a time and place
where he would have privacy and could allow himself
to experience his natural emotions. Wherever he had to
stop writing his account of the event, he was asked to
draw a line. (The place where the client stops is often
the location of a stuck point in the event, where the cli-
ent gave up fighting, where something particularly hei-
nous occurred, etc.) Tom was also instructed to read
the account to himself every day until his next session.
The therapist predicted that Tom would want to avoid
writing the account and procrastinate until as late as
possible. She asked Tom why it would be important for
him to do the assignment and do it as soon as possible.
This was a technique to determine how much Tom
was able to recount the rationale for the therapy, and
to strengthen his resolve to overcome avoidance. Tom
responded that he needed to stop avoiding, or he would
remain scared of his memory. The therapist added that
the assignment was to help Tom get his full memory
back, to feel his emotions about it, and for therapist and
client to begin to look for stuck points. She also reas-
sured Tom that although doing so could be difficult for
a relatively brief period of time, it would not continue
to be so intense, and he would soon be over the hardest
part of the therapy.
Session 4
During the settling-in portion of the session, Tom in-
dicated that he had written the account of the event
the evening before, although he had thought about and
dreaded it every day prior to that. He admitted that he
had been avoidant due to his anxiety. The therapist
asked Tom to read his account aloud to her. Before
starting, Tom asked why it was important to read it in
the session. The therapist reminded Tom of what they
had talked about the previous session, and added that
the act of reading aloud would help him to access the
whole memory and his feelings about it. Tom read what
he wrote quickly, like a police report, and without much
feeling:
There were several of us who were assigned to guard a
checkpoint south of Baghdad. We were there because
insurgents were beginning to take over the particu-
lar area, and we were there to contain the area. I was
placed on top of the checkpoint. It was dusk. It had been
a fairly routine day, with people coming through the
checkpoint like they were going through a toll booth.
Off in the distance I noticed a small, dark car that was
going faster than most cars. I could tell it was going
faster because there was more sand smoke kicking up
behind it. Men out in front of the checkpoint were mo-
tioning for the car to slow down, but it didn’t seem to be
slowing down. Someone shot into the air to warn them,
but they kept on coming. I could see two heads in the
car coming toward us. We had been told to shoot at any
vehicle that came within 25 yards of the gate to protect
those around the gate, and the area beyond the gate.
The car kept coming. I shot a bunch of rounds at the car.
At least one other person shot, too. There was so
much chaos after that. I remember feeling my gun in
my hand as I stood there. After a few moments, I also
remember my legs carrying me down to the car. I don’t
really remember how I got there, but I did. Several men
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
88 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
had surrounded the car, and a man got out of it. The
man was crying. No, sobbing. He was speaking fast
while he cried. He turned toward the car, resisting the
men who attempted to remove him from the scene. I
turned to see what the man was looking at and saw
them for the first time. I saw the woman first.
There was blood everywhere, and her face had been
shot. Then I saw the little girl in the backseat slumped
over, holding a doll. There was blood all over her, too.
I saw the gunshots through the car. I looked back at the
woman, but avoided looking at her face. I saw a bump
under her dress. She was pregnant.
I don’t remember much else after that. I know I went
back to camp and basically fell apart. They took me
off duty for a couple of days, but eventually they sent
me back to the Forward Operating Base because I was
such a mess.
After reading the account, Tom quickly placed it in
his binder of materials and closed the binder as if to
indicate that he was ready to move onto something else.
The therapist asked Tom what he was feeling, and he
indicated that he was feeling “nothing.” The therapist
followed up, saying, “Nothing at all?” Tom reluctantly
admitted that he was feeling anxious. The therapist
then asked him to read the account again, but this time
to slow down his reading rate, and allow himself to
experience the emotions he had felt at the time of the
event.
After reading the account for the second time, the
therapist sought to flush out details of the event that
Tom had “glossed over” and to focus on what appeared
to be the most difficult aspects of the situation.
THERAPIST: What part of what you just read to me is
the most difficult?
T
OM: It is all difficult. The whole thing is horrible.
T
HERAPIST: What is the worst of it, though?
TOM: I guess the worst of it is seeing that small girl in
the backseat of the car.
T
HERAPIST: What did she look like when you saw her?
(Tom describes his memory of the girl when he arrived
at the car.)
T
HERAPIST: What are you feeling right now?
T
OM: I feel sick to my stomach. I feel like I did at the
time—that I want to throw up. I am also disgusted
and sad. I killed an innocent child. There are so
many things I could have done differently not to have
taken her life.
(The therapist is aware of the assimilation process in
Tom’s use of hindsight bias. She stores that information
away for future reference because she wants to make
sure that Tom is feeling strongly as many of his natural
emotions as possible about the traumatic event.)
T
HERAPIST: Continue to feel those feelings. Don’t run
away from them. Anything else that you’re feeling?
T
OM: I feel mad at myself and guilty.
T
HERAPIST: Were you feeling mad at yourself and
guilty at the time?
T
OM: No. I was horrified.
T
HERAPIST: OK, let’s stay with that feeling.
T
OM: (Pauses.) I don’t want to feel this anymore.
T
HERAPIST: I know you don’t want to feel this anymore.
You’re doing a great job of not avoiding your feelings
here. In order to not feel like this for a long time,
you need to feel these absolutely natural feelings. Let
them run their course. They’ll decrease if you stay
with them.
After a period in which Tom experienced his feel-
ings related to the situation and allowed them to dis-
sipate, a discussion ensued regarding how hurtful it
was to Tom to hear other people’s reaction to the war.
He expressed specific frustration with the presidential
administration and its policy on the war. The therapist
gently redirected Tom’s more philosophical discussion
of international policy to the effects of the trauma on
him. Tom then told a story of how he had shared his
traumatic experience with a high school friend. He felt
that this person had a negative reaction to him as a result
of sharing the story. Tom felt judged and unsupported
by this friend. Since this experience with his friend,
Tom had refrained from telling others about his combat
experience. Using Socratic questioning, the therapist
asked Tom if there might be any reason, outside of his
actions, that someone might have a negative reaction
to hearing about the shooting. Through this exchange,
Tom was able to recognize that when others hear about
traumatic events, they also are trying to make sense of
these experiences in light of their existing belief sys-
tems. In other words, others around him might fall prey
to the “just world” belief that bad things only happen
to bad people. They also might not take into account
the entire context in which Tom shot the passengers in
the car. This recognition resulted in Tom feeling less
angry at his friend for this perceived judgment. He was
also somewhat willing to admit that his interpretation
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
89
of his friend’s reaction might have been skewed by his
own judgment of himself. In fact, later in the therapy,
when Tom was able to ask his friend directly about the
perceived reaction, the friend indicated that it had been
hard for him to hear, but that he had not been judging
Tom at all. In actuality, he was thinking about the ter-
rible predicament Tom had endured at the time.
The therapist asked Tom what stuck points he had
identified in writing and reading his account. The fol-
lowing dialogue then occurred:
T
OM: I’m not sure what the stuck points are, but from
what you’ve been asking me, I guess you question
whether or not I murdered this family.
T
HERAPIST: That’s true. I think it is worthwhile for
us to discuss the differences between blame and
responsibility. Let’s start with responsibility. From
your account, it sounds like you were responsible for
shooting the family. It sounds like other people may
have been responsible, too, given that you were not
the only person who shot at them.
(The therapist stores this fact in her mind to challenge
Tom later about the appropriateness of his actions.
This also provides a good opportunity to reinforce Tom
for performing well in a stressful situation.)
The bottom line is that responsibility is about your
behavior causing a certain outcome. Blame has to do
with your intentionality to cause harm. It has to do
with your motivations at the time. In this case, did
you go into the situation with the motivation and in-
tention to kill a family?
T
OM: No, but the outcome was that they were murdered.
T
HERAPIST: Some died. From what you’ve shared, if
we put ourselves back into the situation at the time,
it was not at all your intention for them to die. They
were coming down the road too fast, not responding
to the very clear efforts to warn them to stop. Your
own and others’ intentions were to get them to stop
at the checkpoint. Your intention at the time did not
seem to be to kill them. In fact, wasn’t your intention
quite the opposite?
T
OM: Yes. (Begins to cry.)
T
HERAPIST: (Pauses until Tom’s crying subsides some-
what.) It doesn’t seem that your intention was to kill
them at all. Thus, the word “blame” is not appro-
priate. Murder or considering yourself a murderer
does not seem accurate in this situation. The reason
I’ve questioned the term “murder” or “murderer” all
along was because it doesn’t seem like your intention
was to have to shoot them.
T
OM: But why do I feel like I am to blame?
T
HERAPIST: That’s a good question. What’s your best
guess about why that is?
T
OM: (Still crying) If someone dies, someone should
take responsibility.
T
HERAPIST: Do you think it is possible to take respon-
sibility without being to blame? What would be a
better word for a situation that is your responsibility,
but that you didn’t intend to happen? If a person shot
someone but didn’t intend to do that, what would we
call that?
T
OM: An accident, I guess.
T
HERAPIST: That’s right. In fact, what would you call
shooting a person when you are trying to protect
something or someone?
T
OM: Self-defense.
T
HERAPIST: Yes, very good. Weren’t you responsible
for guarding the checkpoint?
T
OM: Yeah.
T
HERAPIST: So, if you were responsible for guard-
ing that checkpoint, and they continued through,
wouldn’t that have put the area at risk?
T
OM: Yes, but it was a family—not insurgents.
T
HERAPIST: How did you know that at the time?
T
OM: There was woman and child in the car.
THERAPIST: But, did you know that at the time?
T
OM: No.
T
HERAPIST: So only in hindsight do you know that it
was a family that might have had no bad intention.
We actually don’t know the family’s intention, do
we? They didn’t heed the several warnings, right?
T
OM: Yes. (Pauses.) I hadn’t thought that they would
be looking to do something bad with a woman and
child in the car.
T
HERAPIST: We don’t know, and won’t ever know, bot-
tom line. However, what we do know is what you
knew at the time. What you knew at the time is that
they did not heed the warnings, that you were re-
sponsible for securing the checkpoint, and that you
took action when you needed to take action to pro-
tect the post. Thinking about those facts of what hap-
pened and what you knew at the time, how do you
feel?
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
90 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
TOM: Hmm . . . I guess I’d feel less guilty.
T
HERAPIST: You’d feel less guilty, or you feel less
guilty?
T
OM: When I think through it, I do feel less guilty.
T
HERAPIST: There may be points when you start feel-
ing guiltier again. It will be important for you to hold
onto the facts of what happened versus going to your
automatic interpretation that you’ve had for awhile
now. Is there any part of it that makes you proud?
T
OM: Proud?
T
HERAPIST: Yes. It seems like you did exactly what you
were supposed to do in a stressful situation. Didn’t
you show courage under fire?
T
OM: It’s hard for me to consider my killing them as
courageous.
T
HERAPIST: Sure. You haven’t been thinking about it
in this way for a long time, but it is something to
consider.
The therapist’s Socratic dialogue was designed to
help Tom consider the entire context in which he was
operating. She also began to plant the seed that Tom
not only did nothing wrong but he also did what he was
supposed to do to protect the checkpoint. Whenever
possible, pointing out acts of heroism or courage can be
powerful interventions with trauma survivors.
Prior to ending the session, the therapist checked
Tom’s emotional state to make sure he was calmer than
he had been during the session. She also inquired about
his reaction to the therapy session. He commented that
it had been very difficult, but that he felt better than he
expected in going into the “nitty-gritty” of what hap-
pened. He also noted that there were things he had not
considered about the event that were “food for thought.”
The therapist praised Tom for doing a great job on the
writing assignment and reinforced the importance of
not quitting now. She commented that he had complet-
ed one of the hardest steps of the therapy, which would
help him recover.
The therapist took the first account of the trauma and
gave Tom his next practice assignment: to write the en-
tire account again. The therapist asked Tom to add any
details he might have left out of the first account and
to provide even more sensory details. She also asked
him to record any thoughts and feelings he was hav-
ing in the here-and-now in parentheses, along with his
thoughts and feelings at the time of the event.
Session 5
Tom arrived at Session 5 looking brighter and making
more eye contact with the therapist. He indicated that
he had written the account again, right after the previ-
ous session. He commented that the writing was hard,
but not as hard as the first time. The therapist used this
as an opportunity to reinforce how natural emotions
resolve naturally as they are allowed expression. Tom
noted that he had talked with his wife more this week,
avoiding her less. Their increased communication al-
lowed Tom’s wife to express her concerns about Tom’s
well-being. She shared that he seemed disinterested
in her and in their unborn child. Tom had previously
told his wife about the incident, but he had not shared
the specific detail that the woman in the vehicle was
pregnant. Tom perceived his wife as having a very good
reaction to his disclosure about the pregnant woman.
He noted that she asked him questions, and that her
comments indicated that she did not blame him for his
actions. For example, she asked, “How could you have
known at the time that it was a family?” She also re-
portedly said, “It’s hard to know with terrorism if they
were actually just a family traveling.” Tom laughed
when he reported that their conversation sounded like
his last psychotherapy session.
The therapist asked Tom to read his second account
out loud, with as many emotions as possible. Tom had
written more about the event, and the therapist noted
that he had included more information about what he
and the other guards had done to warn the passengers
in the car to slow down for the checkpoint. Tom read
the second account more slowly and was not as tense as
he had been the first time he read aloud. Tom’s second
account included much more detail and focused more
on the vehicle and its occupants after he had fired upon
them.
THERAPIST: I notice that you wrote more about the car
and the family. What are you feeling about that right
now?
T
OM: I feel sad.
T
HERAPIST: Do you feel as sad as you felt the first time
you wrote about it?
T
OM: I think I may feel sadder about it now.
T
HERAPIST: Hmm . . . Why do you think that might be?
T
OM: I think it’s like what I wrote in the parenthesis
about what I’m thinking now. Now, instead of feeling
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
91
so much guilt that I shot them, I think it’s sad that
they didn’t heed the warnings.
T
HERAPIST: You mentioned that you’re feeling less
guilt now. Why is that?
T
OM: I’m beginning to realize that I was not the only
one there that was trying to stop them. Several of us
were trying to get them to stop. There is still some
guilt that I was the one who shot them.
T
HERAPIST: If one of the other guards had shot them,
would you blame him or her for the shooting? Would
you expect him or her to feel guilty for their behav-
ior?
T
OM: (Laughs.) I started thinking about that this week.
It made me wonder if it was really me who even shot
them. As I was writing and thinking about it more,
I realized that there is a possibility that another of
the guards may have been shooting at the same time.
T
HERAPIST: What would it mean if he or she was shoot-
ing at the same time?
T
OM: If he was shooting at the same time, it means that
he thought that shooting at them might be the right
thing to do in that situation.
T
HERAPIST: Might have been the right thing to do?
TOM: (smiling) Yeah, I still have questions that we
might have been able to do something else.
T
HERAPIST: It seems like you’re still trying to “undo”
what happened. I’m curious, what else could you
have done?
T
OM: Not have shot at them.
THERAPIST: Then what would have happened?
T
OM: They might have stopped. (Pauses.) Or I guess
they could have gone through the checkpoint and
hurt other people past the checkpoint. I guess they
could have also been equipped with a car bomb that
could have hurt many other people. That seems hard
to believe, though, because of the woman and child
in the car.
T
HERAPIST: It is impossible for us to know their inten-
tions, as we discussed before. The bottom line is that
you’ve tended to assume that doing something dif-
ferent, or doing nothing, would have led to a better
outcome.
T
OM: That is true. I still feel sad.
T
HERAPIST: Sure you do—that’s natural. I take it as a
good sign that you feel sad. Sadness seems like a very
natural and appropriate reaction to what happened—
much more consistent with what happened than the
guilt and self-blame that you’ve been experiencing.
Tom and the therapist discussed how the goal of the
therapy was not to forget what had happened, but to
have the memory without all of the anxiety, guilt, and
other negative emotions attached to it. Tom indicated
that he was becoming less afraid and more able to tol-
erate his feelings, even when they were intense. Tom
acknowledged that reading his account, talking about
his trauma, and coming to psychotherapy sessions were
becoming easier and that his negative feelings were be-
ginning to diminish.
After discussing Tom’s reactions to his memories,
with a focus on how he had attempted to assimilate the
memory into his existing beliefs, the therapist began
to discuss areas of overaccommodation. One area of
overaccommodation was Tom’s beliefs about the U.S.
military. He had entered the service with a very posi-
tive view of the military. Tom had a family history of
military service and believed in service to country and
the “rightfulness” of the military.
Subsequent to his traumatic event and military ser-
vice in Iraq, he developed a negative view of the mili-
tary that had extended to the Federal government in
general. The therapist used this content to introduce the
first series of tools to help challenge Tom’s stuck points.
She also emphasized how he would gradually be taking
over as his own therapist, capable of challenging his
own patterns of thinking that kept him “stuck.”
T
HERAPIST: It seems that you have some very strong
beliefs about the military and the U.S. government
since your service. I’d like to use those beliefs to
introduce some new material that will be helpful
to you in starting to challenge stuck points on your
own. You’ve done an outstanding job of considering
the way that you think and feel about things. You’ve
been very open to considering alternative interpreta-
tions of things. Starting in this session, I’m going to
help you to become your own therapist and to attack
your own stuck points directly.
T
OM: OK.
T
HERAPIST: Today we will cover the first set of skills.
We’re going to be building your skills over the next
few sessions. The first tool is a sheet called the Chal-
lenging Questions Sheet. Our first step is to identify
a single belief you have that may be a stuck point.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
92 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
As I mentioned before, I’d like us to use your beliefs
about the Federal government now. So, if you were
to boil down what you believe about the Federal gov-
ernment or the military, what is it?
T
OM: I don’t know. I’m not sure. I guess I’d say that the
U.S.
military is extremely corrupt.
T
HERAPIST: Good. That is very clear and to the point.
So let’s go over these questions and answer them as
they relate to this belief. The first question you ask
yourself is, “What’s the evidence for and against this
idea?”
T
OM: The evidence for this is Abu Ghraib. Can you be-
lieve that they would do that? I would have also put
my own shooting under the “for” list, but I’m begin-
ning to question that.
T
HERAPIST: What other evidence is there of corrup-
tion?
T
OM: Oh, and these defense contractors . . . what a
scam! That leads me to the current administration
and its vested interests in going to war to make
money on defense contracting. And, oh, of course,
to make money on the oil coming out of these coun-
tries!
T
HERAPIST: OK. Sounds like you have some “for” evi-
dence. What about the “against” evidence?
T
OM: Well, some of my fellow soldiers were very good.
They were very committed in their service and to
the mission. I also had mostly good leaders, although
some of them were real pigs. Some were really
power-hungry a—holes, frankly.
T
HERAPIST: So, it sounds like you have some pros and
cons that support your belief that the U.S. military is
completely corrupt. In the process of changing, it is
not uncommon to have thoughts on both sides. That
is great news! It means that you are considering dif-
ferent alternatives, and are not “stuck” on one way of
seeing things. Let’s take the next one. . . .
The therapist spent the balance of the session going
over the list of questions to make sure that Tom un-
derstood them. Although most of the questions focused
on the issue of corruption in the military, other issues
were also brought in to illustrate the meaning of the
questions. For example, the therapist introduced the
probability questions with the example from Tom’s life
in which he believed that he was going to be shot by
an insurgent sniper while back home. These questions
are best illustrated with regard to issues of safety. The
therapist pointed out that perhaps not all of the ques-
tions applied to the belief on which Tom was working.
The question “Are you thinking in all-or-none terms?”
seemed to resonate with Tom the most because it ap-
plied to his belief about the military. He commented
that he was applying a few examples of what seemed to
be corruption to the entire military. Tom also indicated
that his description of the military as “extremely” cor-
rupt was consistent with the question “Are you using
words or phrases that are extreme or exaggerated?” In-
dicative of his grasp of the worksheet, Tom also noticed
that the question “Are you taking selected examples out
of context?” applied to his prior view of his behavior as
a murder in the traumatic event.
For his practice assignment prior to Session 6, Tom
agreed to complete one Challenging Questions Sheet
each day. He and the therapist brainstormed about po-
tential stuck points prior to the end of the session to
facilitate practice assignment completion. These stuck
points included “I don’t deserve to have a family,” “I
murdered an innocent family,” and “I am weak because
I have PTSD.”
Session 6
Tom completed Challenging Questions Sheets about all
of the stuck points he and the therapist had generated.
The therapist reviewed these worksheets to determine
whether Tom had used the questions as designed. She
asked Tom which of the worksheets he had found least
helpful. He responded that he had had the most diffi-
culty completing the sheet about deserving to have a
family. The therapist then reviewed this sheet in detail
with Tom (see Figure 2.2).
THERAPIST: So, I notice that in your answer about the
evidence for and against this idea about deserving a
family, you included as evidence that you took some
other man’s family. I’m glad to see that you didn’t in-
clude the word “murder”—that’s progress. But, how
is that evidence for you not deserving a family?
T
OM: It is evidence because I feel like I took someone
else’s; therefore, I don’t deserve one for myself. It
seems fair.
T
HERAPIST: Remind me to make sure and look what
you put for item 9 about confusing feelings and facts.
For now, though, help me understand the math of
why you don’t deserve your family, and your happi-
ness about your family, because of what happened?

From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
93
Challenging Questions Sheet
Below is a list of questions to be used in helping you challenge your maladaptive or problematic beliefs.
Not all questions will be appropriate for the belief you choose to challenge. Answer as many questions
as you can for the belief you have chosen to challenge below.
Belief: I don’t deserve to have a family.
1. What is the evidence for and against this idea?
FOR: I took some other man’s family.
AGAINST: I didn’t want to have to shoot anyone. An “eye for an eye” does not apply here.
2. Is your belief a habit or based on facts?
It is a habit for me to think this way. The facts are that I didn’t do something wrong to deserve to be
punished in this way.
3. Are your interpretations of the situation too far removed from reality to be accurate?
My interpretation of the original situation has been fairly unrealistic, which is where I get this belief.
4. Are you thinking in all-or-none terms?
N/A
5. Are you using words or phrases that are extreme or exaggerated? (i.e., always, forever, never, need,
should, must, can’t, and every time)
I guess maybe “deserve” could be an extreme word.
6. Are you taking the situation out of context and only focusing on one aspect of the event?
Yes, like #3, I tend to forget what all was going on at the time of my shooting.
7. Is the source of information reliable?
No, I’m not very reliable these days.
8. Are you confusing a low probability with a high probability?
N/A
9. Are your judgments based on feelings rather than facts?
I’m feeling guilty like I did something wrong when the truth is that I did what I was supposed to do.
10. Are you focused on irrelevant factors?
Maybe my deserving a family has nothing to do with someone else losing theirs?
FIGURE 2.2. Challenging Questions Sheet.
TOM: I don’t know—it just seems fair.
T
HERAPIST: Fair? That implies that you did something
bad that requires you to be punished.
T
OM: As I’ve been thinking about it more, I don’t think
I did something wrong when I really look at it, but
it still feels like I did something wrong and that I
shouldn’t have something good like a wife and child
in my life.
T
HERAPIST: Maybe we should look at your response
to item 9 now. What did you put in response to the
question “Are your judgments based on feelings
rather than facts?”
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
94 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
TOM: I wrote, “I’m feeling guilty, like I did something
wrong when the truth is that I did what I was sup-
posed to do.” I try to remember what we talked
about, and what my wife also has said to me about
them not responding to the warnings and my shoot-
ing them, which may have prevented something else
that was bad. I still feel bad—not as bad as I did—
but I still feel like I did something wrong.
(The therapist uses this as an opportunity to talk about
the need for practicing new alternative thoughts in
order to elicit emotional change.)
T
HERAPIST: You are well on your way, Tom, to getting
unstuck and recovering. Your head is starting to get
it, and your feelings need to catch up. You’ve been
thinking about what happened and what you did
in a certain way for awhile now. You blamed your-
self over and over and over again, telling yourself
that you did something wrong. You gave yourself a
steady diet of that type of thinking, which resulted
in you feeling guilty about what happened. It is like
a well-worn rut of thinking in your brain that auto-
matically leads you down the path of feeling guilty.
What you need to do now is start a new road of more
realistic and truthful thinking about the situation
that will eventually be a well-worn path. What is the
more realistic view of your role in this event?
T
OM: (tearfully) I had to shoot at the car, and people
died.
T
HERAPIST: That’s right. And, let’s pretend for a second
that you really do believe that thought. If so, what
would you feel?
T
OM: I’d feel so much lighter. I wouldn’t feel guilty. I’d
continue to feel sad about this horrible situation, but
I wouldn’t blame myself.
T
HERAPIST: Let’s take it the next step. If you didn’t
blame yourself and feel guilty, then would you be-
lieve that you deserve to be happy with your wife and
the baby that will soon be here?
T
OM: Sure.
THERAPIST: So, Tom, your work is to practice, practice,
practice this new and more accurate way of looking
at what happened and your role in it. With practice,
your feelings will start matching the truth about
what happened and the fact that you are not to blame.
T
OM: It is kind of like training to use a weapon. They
made us do certain things with our guns over and
over and over again, until it was automatic. It was
very automatic after a while.
T
HERAPIST: That’s right. There are other questions on
this sheet that might be helpful in convincing you of
the truth about this in your practice. What did you
put for the question “Is your belief a habit or based
on a fact?”
This dialogue illustrates a common occurrence at
this stage in the therapy. Tom was starting to experi-
ence cognitive change, but his emotional change was
lagging. The therapist reinforced the need to practice
the new ways of thinking to feel different. It is also
important to highlight clients’ gains in changing their
thinking, even if their feelings have not changed or are
ambivalent. A change in thinking is framed as more
than halfway to a change in feeling. In effect, changed
thinking involves competing thoughts or learning, and
with more repetitions of the new thought, the associ-
ated feelings follow and eventually win out.
In the latter portion of this session the therapist in-
troduced the Patterns of Problematic Thinking Sheet
and provided an explanation of how this list was dif-
ferent from the Challenging Questions Sheet (see Fig-
ure 2.3). More specifically, she indicated that the Pat-
terns of Problematic Thinking Sheet pertains to more
general patterns of thinking versus challenging indi-
vidual thoughts that Tom might have. The Patterns of
Problematic Thinking Sheet lists seven types of faulty
thinking patterns (e.g., oversimplifying, overgeneraliz-
ing, emotional reasoning).
Tom and the therapist went through the list and gen-
erated examples for each of the patterns. For example,
for “Disregarding important aspects of a situation,” the
therapist pointed out something that Tom had brought
up several times during therapy. Initially Tom had not
included the important information that he and the
other guards had attempted to stop the car before shoot-
ing at it. She also pointed out that emotional reasoning
was similar to confusing a feeling with a fact, which
had been a primary focus of the session.
When they got to the item “Overgeneralizing from
a single incident,” Tom said that he had noticed he was
beginning to change his thoughts about the government
and its leaders. He commented that it had been very
powerful for him to consider that, in a number of in-
stances, his fellow soldiers had operated with integrity
and were committed to the mission, and to the safety
and protection of others. Tom said spontaneously, “I
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
95
guess that is also kind of like drawing conclusions when
evidence is lacking or even contradictory.” He said that
he had started stereotyping after the traumatic event—
applying negative attributes and opinions to everyone
in the military and the government too broadly. Tom
and the therapist discussed how the goal of the thera-
py was to have a balanced and realistic view of things
versus the overly ideal version he had pretrauma or the
overly pessimistic version he had posttrauma. In other
words, the goal was to find shades of gray and balance
in his thinking about the government, the military, and
their leadership. Tom added an example of this think-
ing: “There are at least some people in government who
want to do good for others.”
Tom was given the practice assignment to read over
the list in the Patterns of Problematic Thinking Sheet
and to note examples of times he used each of the prob-
lematic thinking patterns.
Session 7
Tom began the session by stating that he was feeling
better, and that his wife had also noted a difference in
him and was feeling less concerned about the therapy
making him worse rather than better. The therapist had
given Tom the PCL and the BDI-II to complete while
he was waiting for his appointment. She quickly scored
these assessment measures and gave Tom feedback
Patterns of Problematic Thinking
Listed below are several types of patterns of problematic thinking that people use in different life
situations. These patterns often become automatic, habitual thoughts that cause us to engage in self-
defeating behavior. Considering your own stuck points, find examples for each of these patterns. Write in
the stuck point under the appropriate pattern and describe how it fits that pattern. Think about how that
pattern affects you.
1. Jumping to conclusions when the evidence is lacking or even contradictory.
I tend to jump to the conclusion that I have done something wrong when bad things happen. I
assume things are my fault.
2. Exaggerating or minimizing a situation (blowing things way out of proportion or shrinking their
importance inappropriately).
I minimize the things that I have done well in the military.
3. Disregarding important aspects of a situation.
In the past I have tended to neglect the important aspect that several of us tried to stop the car from
going through the checkpoint.
4. Oversimplifying things as good–bad or right–wrong.
I can sometimes think of all Iraqis as all bad.
5. Overgeneralizing from a single incident (a negative event is seen as a never-ending pattern).
I have assumed that because of my traumatic event, I could not be safe with my baby to be born.
6. Mind reading (you assume people are thinking negatively of you when there is no definite evidence
for this).
I assume that everyone thinks I am a terrible person, a murderer, because of what I did.
7. Emotional reasoning (you have a feeling and assume there must be a reason).
This one is easy—I feel guilty, and therefore I must be.
FIGURE 2.3. Patterns of Problematic Thinking Sheet.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
96 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
about his scores at the beginning of this session. His
PCL score had decreased from 68 to 39, which was a
clear and clinically meaningful change in his PTSD
symptomatology. She noticed that his avoidance and
reexperiencing symptoms had decreased the most; his
hyperarousal symptoms had also decreased, but less so.
His score on the BDI-II had decreased from 28 to 14,
clearly indicating a reduction in his depressive symp-
toms.
The therapist asked whether Tom had completed
his practice assignment, the Patterns of Problematic
Thinking Sheet. He indicated that he had not, but that
he had thought about it over the week. He also laughed
and said that he had noticed the thinking patterns in his
wife and others. The therapist asked Tom to complete
some of the sheet in session. At this point in therapy,
the therapist was sitting back more as Tom took on the
role of challenging his own cognitions. The therapist
provided both minimal clarification and additional ex-
amples that she had noticed in working with Tom.
In this session, the therapist introduced the Chal-
lenging Beliefs Worksheet. She was careful to point out
that the worksheet integrated all of the previous work
Tom had done and added a few new elements. The
following dialogue illustrates the introduction of this
sheet (see Figure 2.4).
T
HERAPIST: I want to show you the final worksheet that
we’re going to be using for the rest of the therapy.
T
OM: OK. Wow—that looks complicated!
T
HERAPIST: Actually, you’ve done pretty much ev-
erything on this worksheet already. This worksheet
brings together into one place everything that we’ve
been working on.
T
OM: I’ll take your word for it, Doc.
T
HERAPIST: Remember the A-B-C Sheets from way
back when?
T
OM: Yes.
T
HERAPIST: (pointing to first three columns on the
Challenging Beliefs Worksheet) This is A, B, and
C. You have in column A the situation, or “Activat-
ing Event” that you had on the A-B-C Sheet. In col-
umn B you have “Automatic Thoughts,” which is the
“Belief” portion of the A-B-C Sheet. Last, column
C, “Emotions,” is the “Consequence” portion of the
A-B-C Sheet.
T
OM: OK. So far, so good.
T
HERAPIST: Column D is where you identify the “Chal-
lenging Questions” from that sheet that apply to the
thought or stuck point that you’re working on. In col-
umn E, you identify the type of “Patterns of Prob-
lematic Thinking” that apply to the thought or stuck
point that you’re working on. Make sense?
T
OM: Yes.
T
HERAPIST: So, only column F, “Alternative Thought,”
is new. Here you identify alternative thoughts that
you could have about the situation. In other words,
we’re looking for alternative statements that you can
tell yourself or different interpretations of the event.
In columns G and H, you get to see how your belief
in your original thoughts may change and how the
new thoughts affect your feelings.
T
OM: OK.
T
HERAPIST: So, let’s pick a stuck point and start using
this Challenging Beliefs Worksheet. We’re going to
be talking about safety as one of the first topics of the
next few sessions. Can you think of a stuck point that
relates to your ability to keep yourself safe or to how
safe others are around you?
TOM: Well, I still wonder if there are people out in the
world who want to hurt me, even if I now realize that
no sniper is going to take me out.
T
HERAPIST: So, let’s pick a specific event—the more
specific, the better.
T
OM: I was in the grocery store, and I had my uniform
on. There was this guy who seemed to have a chip
on his shoulder about it—like he hated me or some-
thing.
T
HERAPIST: So, write down the event in Column A.
(Pauses.) What was your thought? You’ve already
mentioned one of them.
T
OM: This guy has a chip on his shoulder about me be-
cause I’m in the military.
T
HERAPIST: Good. How strongly do you believe that
thought?
T
OM: 100%.
T
HERAPIST: OK, let’s write that next to the thought.
We are now rating how much you believe in your
thoughts because you’re going to see at the end how
much your thought has changed. What feeling or
feelings are associated with that thought?
T
OM: Definitely anger.

A. Situation B. Thoughts D. Challenging Thoughts E. Problematic Patterns F. Alternative Thought
Describe the event,
thought, or belief
leading to the
unpleasant
emotion(s).
Write thought(s) related to
Column A.
Rate belief in each thought
below from 0–100%.
(How much do you believe
this thought?)
Use Challenging Questions to
examine your automatic thoughts from
Column B.
Is the thought balanced and factual or
extreme?
Use the Problematic Thinking
Patterns sheet to decide if this is one
of your problematic patterns of
thinking.
What else can I say
instead of Column B?
How else can I interpret
the event instead of
Column B?
Rate belief in alternative
thought(s) from 0–100%.
Evidence? Jumping to conclusions
“I don’t know if he has
chip on his shoulder.”
(60%)
“If he does have a chip
on his shoulder, I don’t
know what it is about –
maybe it isn’t even about
me, let alone having
served in Iraq.” (80%)
At store in uniform
“This guy has a chip on
his shoulder because I
am in the military.”
(100%)
Habit or Fact?
Habit to think everyone dislikes me
because I was in Iraq.
Interpretations not accurate?
Exaggerating or minimizing
Disregarding important aspects
All or none?
Oversimplifying
Extreme or exaggerated?
Out of context? Overgeneralizing
G. Rerate Old Thoughts
C. Emotion(s)
Source unreliable? Me
Low versus high probability?
Based on feelings or facts?
Mind reading
I am assuming that he is thinking
the worst of me
.
Emotional reasoning
Rerate how much you now
believe the thought in
Column B from 0–100%.
35%
Specify sad, angry, etc.,
and rate how strongly you
feel each emotion from 0–
100%.
H. Emotion(s)
Anger (80%)
Fear (30%)
Irrelevant factors?
Now what do you feel? 0–
100%
Anger (20%)
Fear (15%)
FIGURE 2.4. Challenging Beliefs Worksheet completed in session.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under Inte
9
rn
7
ational Copyright Convention.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
98 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
THERAPIST: Makes sense, given your thought. How
much anger from 0 to 100%, with 100% being as
much anger as you could possibly imagine having?
T
OM: Hmm . . . I’d say 80%.
T
HERAPIST: Any other feelings? You can have more
than one.
T
OM: I guess when I stop and think about it, there is
some fear there, too.
T
HERAPIST: That makes sense, too. How much fear
from 0 to 100%?
T
OM: Oh, maybe 30%. It’s not the strongest feeling, but
it’s there, because I’m wondering if he is going to say
something or do something.
T
HERAPIST: Nice job. Let’s move onto the next col-
umn that relates to the Challenging Questions Sheet
you’ve already done. Take a look at this list. What
questions might apply here?
T
OM: I guess I might be confusing a habit with a fact.
It seems like it is a habit for me to assume that ev-
eryone dislikes me because I was in Iraq. I really
don’t know if that is why he seemed to have a chip
on his shoulder. I guess I also don’t know for sure if
he had a chip on his shoulder. He didn’t say anything
to me. (Pauses.) I guess that is also an example of
the source of information being unreliable, and that
source is me! (Laughs.)
T
HERAPIST: While you were talking, I was thinking
that the same things applied. So you’d write those in
this column. You can also pick out other challenging
questions that might apply, but usually two or three
will do the trick. In the next column, we’re going to
refer to the Patterns of Problematic Thinking Sheet.
What might fit here?
T
OM: I guess one jumps out—mind reading.
T
HERAPIST: How so?
T
OM: I’m assuming that he is thinking the worst about
me and about my having served my country in this
war. I’m good at that.
T
HERAPIST: Write that down. You can add others later
if something seems to apply. The next column is very
important. This is where you start coaching yourself
to come up with alternative thoughts or perceptions
about the situation. Based on having asked yourself
these questions and noticing the problematic think-
ing patterns, what other ways might you think about
this situation?
T
OM: I guess one thing I could say to myself is, “I don’t
know if he has chip on his shoulder.” I could also say,
“If he does have a chip on his shoulder, I don’t know
what it is about—maybe it isn’t even about me, let
alone about my having served in Iraq.”
T
HERAPIST: Wow! You’re doing great at this. Let’s get
those written down. Let’s also add how much you
believe those two new thoughts. Below those alter-
native thoughts is the column that asks you to recon-
sider how much you believe your original thoughts
over here in column B. How much do you believe
them after walking through this process? Before you
said 100%.
T
OM: Oh, I’d say now it is only about 35%.
T
HERAPIST: That is a big change. You went from 100%
certainty to 35% certainty that he had a chip on his
shoulder because you fought in the war.
TOM: I’m a little surprised by that myself.
T
HERAPIST: Let’s take it the final step. How about your
feelings now? Let’s rerate those here.
T
OM: My anger is way down—I’d say only about 20%.
The anxiety is still there because I really wouldn’t
want to have to protect myself, and he might have
had a chip on his shoulder at me. It is down a little,
though, because I realize I’m not 100% certain he
was out to get me. I’d say maybe 15% on fear.
T
HERAPIST: Do you have questions about what we just
did here?
T
OM: Not at the moment. I’ll get back to you.
T
HERAPIST: I’m going to ask that you do one of these
sheets on a stuck point per day until I see you again.
I’m also going to give you some example sheets other
patients have done that might be helpful to you.
T
OM: OK. Should be interesting. . . .
The therapist reminded Tom that he might find he
is not using problematic thinking, and in that case, no
change in feelings would be expected. She also cau-
tioned Tom that he should not expect his beliefs and
feelings always to change completely in the process of
doing the sheet. The old thought would need to be com-
pletely dismantled and the new thought would need to
become more habitual for him to see a more perma-
nent change. The therapist suggested that Tom read the
sheets he completed over to himself a number of times
to facilitate the process.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
99
The Safety module was then introduced. Safety is
the first of five modules (two- to three-page handouts)
that also include Trust, Power/Control, Esteem, and In-
timacy. The therapist oriented Tom to the format of the
module, which included discussion about how beliefs
about the self and others in this area can be disrupted
or seemingly confirmed after a traumatic event, de-
pending on one’s history prior to the traumatic event.
The modules describe how these problematic beliefs
are manifested emotionally and behaviorally (e.g., not
leaving one’s home because of the belief that the world
is unsafe). It also provides alternative self-statements
that are more balanced and realistic in each area.
Tom had felt safe with others before the traumatic
event occurred, and this sense of safety about others
had been disrupted, as evidenced by his sense that oth-
ers around him were out to get him. Pretrauma, Tom
had also felt as though he was not a danger to others.
Posttrauma, he believed that he could not be safe with
others, which specifically manifested in his concerns
about being around his pregnant wife. The therapist
suggested that Tom complete at least one worksheet on
his stuck points about others being safe, as well as his
being a possible danger to others. The therapist also re-
minded Tom that he needed to finish the Patterns of
Problematic Thinking Sheet assignment from last ses-
sion.
Session 8
Tom arrived at the session having completed the Pat-
terns of Problematic Thinking Sheet, as well as two
Challenging Beliefs Worksheets. The therapist spent
a little time looking at his answers to the Patterns of
Problematic Thinking Sheet because she did not want
to send the message inadvertently that completing the
assignments was unimportant. She asked Tom to read
the patterns that he had completed at home, as opposed
to those in their previous session.
Tom completed two Challenging Beliefs Worksheets
related to the topic of safety, as the therapist had in-
structed. He did one each on self and other safety be-
liefs. He did not seem to understand that he could use
the Challenging Beliefs Worksheets on everyday events
that were distressing or even positive for him. Thus, the
therapist emphasized how Tom might use this process
more generally in his day-to-day life, and highlighted
how more practice would lead to more results. She
noted that using the process on less emotionally dis-
tressing topics could actually be very helpful in getting
the process down. It is always easier to learn something
when one is not dealing with the most challenging cir-
cumstances. She used a military analogy with Tom
about learning to load and shoot a gun—best learned in
a nonconflict situation, so that it is a more rote behavior
when under fire.
The therapist skimmed the two sheets Tom had com-
pleted and noticed that he had struggled most coming
up with alternative statements about his own sense of
dangerousness related to his wife’s impending delivery
of their child. The following dialogue ensued (see Fig-
ure 2.5):
T
HERAPIST: I notice that you might have had the most
trouble coming up with alternative thoughts about
how safe you can be with your wife and your child
who is about to be born.
T
OM: Yeah, I don’t really like to talk about it. It freaks
my wife out. I’m uncomfortable being around my
wife, which makes her feel bad, but I’m just afraid
I’m going to hurt her or the child.
T
HERAPIST: Let’s take your first thought because it is
kind of general. How is it that you think you’re going
to hurt them? Are we talking physically or mentally?
TOM: Oh, physically is what I mean. I don’t know how
exactly, but somehow, some way, I guess.
T
HERAPIST: That makes it a bit more concrete. How
do you physically think you’re going to hurt them?
Do you think you’ll shoot them, given your trauma
history?
T
OM: No. Absolutely not. There are no firearms in my
house, and I don’t go hunting or have friends or fam-
ily who hunt—nothing that would make guns a part
of our life.
T
HERAPIST: So, what have you considered in your
mind?
T
OM: I guess I’m worried that, out of nowhere, I’ll get
physically violent.
T
HERAPIST: OK, now we’re cooking. Let’s write that
down. “Out of nowhere I’ll get physically violent.”
I noticed that in column C you didn’t mention any-
thing about probabilities. Safety issues are almost
always about gauging probabilities. The world is not
a completely safe place, and every day we all make
calculated risks about our safety based on the prob-
ability of bad things happening to us or to someone

A. Situation
B. Thoughts
D. Challenging Thoughts
E. Problematic Patterns
F. Alternative Thought
Describe the event,
thought, or belief
leading to the
unpleasant
emotion(s).
Write thought(s) related to
Column A.
Rate belief in each thought
below from 0–100%.
(How much do you believe
this thought?)
Use Challenging Questions to
examine your automatic thoughts from
Column B.
Is the thought balanced and factual or
extreme?
Use the Problematic Thinking
Patterns sheet to decide if this is one
of your problematic patterns of
thinking.
What else can I say
instead of Column B?
How else can I interpret
the event instead of
Column B?
Rate belief in alternative
thought(s) from 0–100%.
Evidence? Jumping to conclusions
“It is unlikely that I’ll hurt
my family, and even
more unlikely that it will
be sudden and
unexpected.”
(95%)
Being around my
wife and child
“Out of nowhere, I’ll get
physically violent.”
(80%)
Habit or fact?
Interpretations not accurate?
All or none?
Extreme or exaggerated?
Exaggerating or minimizing
I’m exaggerating the likelihood that
I’d be violent.
Disregarding important aspects
Oversimplifying
G. Rerate Old Thoughts
C. Emotion(s)
Out of context?
Source unreliable?
Low versus high probability?
Given my history, it is actually a
low probability not high.
Based on feelings or facts?
Overgeneralizing
I’m assuming because I shot once
in a certain situation, I’ll be violent
in general.
Mind reading
Emotional reasoning
Rerate how much you now
believe the thought in
Column B from 0–100%.
10%
Specify sad, angry, etc.,
and rate how strongly you
feel each emotion from 0–
100%.
Fear (85%)
H. Emotion(s)
Now what do you feel? 0–
100%
Irrelevant factors?
Fear (< 10%)
FIGURE 2.5. Challenging Beliefs Worksheet regarding safety.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved unde
1
r
0
In
0
ternational Copyright Convention.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
101
else. How do you think the probability questions
might apply?
T
OM: Are you getting at the idea that I’m confusing a
low probability with a high probability?
T
HERAPIST: Precisely. How do you think that applies
here?
T
OM: I’m convinced that “somehow, some way” I’m
going to hurt my family, so I believe that it is a high
probability that it will happen and not a low prob-
ability. I think you think that the probability I will do
that is low. But, I’m still concerned about it.
T
HERAPIST: Let’s talk about the actual probability.
How often have you hurt your family physically?
T
OM: Never. Are you kidding?
T
HERAPIST: I thought as much, but you made it sound
like it was very likely to happen. I guess that’s part
of the problem, right?
T
OM: You’re right.
THERAPIST: How often have you been physically vio-
lent against anyone?
T
OM: I haven’t, besides the shooting. And it surely
hasn’t been unexpected. Now that we’re talking
through it, it feels a little silly.
T
HERAPIST: So, it sounds like figuring out the actual
probability of this is right where we needed to go.
Given what we’ve talked about, what is an alterna-
tive statement you can tell yourself and how much
do you believe it?
T
OM: It is unlikely that I’ll hurt my family, and even
more unlikely that it will be sudden and unexpected
given that it has never happened.
T
HERAPIST: Let’s keep going to see how that might
change how you feel. You wrote that you had 85%
fear. What is that rating now?
T
OM: Less than 10%. There is some fear now that I
know I am capable of hurting a family, but like we’ve
talked about before—and what I have to remember—
is that it occurred in a certain situation and not in my
everyday life now as a civilian in my family.
This exchange between Tom and the therapist illus-
trates the hallmark role of probability in assessments
and beliefs about safety. It is important to realize that
there are some objectively unsafe situations or behav-
iors, and these should not be minimized or challenged.
If there are unreasonable safety precautions or beliefs,
the actual probability of harm should be carefully eval-
uated, keeping in mind that 100% safety is rarely, if
ever, guaranteed.
The therapist transitioned the session to introduce the
Trust module. Tom noted that he had pretty good trust
of himself and others prior to his best friend commit-
ting suicide when they were in high school. Tom said
that after the experience, he sometimes did not trust his
judgments about other people, and that he felt respon-
sible for not anticipating his friend’s suicide. The mili-
tary traumatic event served to confirm his belief that he
could not trust his judgments about others’ intentions.
Tom’s concerns about his ability to be safe with his
wife and unborn child also dovetailed with the issue of
trust. The therapist and Tom went over the information
in the Trust module handout, and Tom seemed to reso-
nate with all of the potential effects. He reported that
he had really been trying to open up with his wife and
not avoid her. He noted that they were communicating
more, which made both of them more relaxed and com-
fortable in the final days of her pregnancy.
The therapist closed the session by assigning daily
Challenging Beliefs Worksheets, asking Tom to do at
least one on the topic of trust. She reminded him that,
like other areas, the goal is to develop balanced alterna-
tive thoughts. In the case of trust, she noted that stuck
points about trust often revolve around making all-or-
none judgments, either trusting or not. The goal is to
consider trust as multidimensional, with different types
of issues resulting in different levels of trust in different
situations.
Session 9
Tom arrived at this session having completed a num-
ber of Challenging Beliefs Worksheets. Several of
them were about trust, including his level of trust of
the government and trust of himself in being a father.
He had also used the worksheets on non-trust-related
topics related to his daily life. He commented that the
worksheets had been helpful in working out his think-
ing before he behaved impulsively or felt miserable.
The therapist praised Tom for completing the work-
sheets so well, and asked him whether he felt he could
use assistance with any of the worksheets. Tom quickly
responded that he wanted to focus on the sheet about fa-
therhood because he was experiencing so much anxiety
about his child’s impending birth. In turning their at-
tention to this worksheet, the therapist immediately no-
ticed that Tom had probably struggled with this work-
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
102 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
sheet because he had listed so many different types of
thoughts that were fueling his anxiety about becoming
a father. She used this as an opportunity to fine-tune
Tom’s use of the worksheets. The therapist’s choice in
thoughts to challenge first also illustrates the prioritiza-
tion of treatment targets in the therapy. She chose to
go after the more directly trauma-related thoughts that
contained remnants of assimilation. Tom’s thoughts
about deserving to be happy about starting a family,
given the death of the woman, fetus, and child, sug-
gested that he had not fully accepted the traumatic
event and the circumstances surrounding it. Thus, she
addressed this thought first (see Figure 2.6).
T
HERAPIST: Wow, you’ve got lots of thoughts going on
in your head about becoming a father, don’t you? I’m
going to suggest that we use a different worksheet for
each of the clusters of thoughts you’re having on this
topic. I think that will make your use of the Chal-
lenging Beliefs Worksheet better. It seems that some
thoughts are directly related to your traumatic expe-
rience, others are specifically related to your wife’s
labor and delivery, and still others are related more
generally to being a parent. Let’s focus on those that
are directly related to your trauma. You wrote that
one of your feelings was guilt (85%), and I’m assum-
ing that it is related to your thought that it isn’t right
that you’re happy with a soon-to-be-born baby given
what happened.
T
OM: That’s right. If I’m really honest, I still feel guilty
that the Iraqi woman was pregnant and getting ready
to have a child, and the shooting deprived her of the
ability to have that child and be happy, and I’m get-
ting ready to have that happiness.
T
HERAPIST: We’ve talked about this before, but we’ve
been more focused on the man involved in the situ-
ation.
T
OM: Yeah, I think the closer my wife gets to delivery,
the more I think about the Iraqi woman. I’ve been
imagining that she wasn’t part of a potential plot for
terrorist activity and was more an innocent partici-
pant. Then, I go back and forth, thinking that she
might have actually been involved and didn’t care
that she was pregnant. Or maybe it was just an ac-
cident, and they truly didn’t understand that they
needed to stop. Uggghhhh, it is exhausting.
T
HERAPIST: And we’ll never know. If your friend were
saying all of this to you, what would be your re-
sponse to him?
T
OM: I’d be telling him to quit beating himself up and
feeling guilty.
T
HERAPIST: Easier said than done. Anything else?
Maybe it would help to look at the Challenging Ques-
tions and Patterns of Problematic Thinking Sheets.
I’m wondering if you are focusing on irrelevant
factors—item 10 on the Challenging Questions Sheet.
T
OM: Hmm . . . what is irrelevant in this case?
T
HERAPIST: How relevant are her intentions to deserv-
ing to be happy yourself about having a child?
T
OM: (Pauses.) I’m going to have to think about that
for a second.
T
HERAPIST: Aren’t your intentions in that situation
what is relevant? Were your intentions at that time
to deprive her of the right to bear her child and live
happily ever after?
T
OM: No, not at all.
T
HERAPIST: So, why the guilt? What did you do wrong
that you should be punished about?
T
OM: Oh, wow. I hadn’t thought of that. Her intentions
are irrelevant. It only makes me crazy to try to get in
her head. I guess that would be mind-reading, now
wouldn’t it?
THERAPIST: Very good—a different spin on mind read-
ing. So what is the alternative, more balanced and
realistic thought?
T
OM: My intentions are what matter. I didn’t intend for
her to lose her own or her baby’s life.
T
HERAPIST: Go on . . . do you have a right to experience
happiness?
T
OM: I guess I do. It just feels weird.
T
HERAPIST: Sure—it feels different. It is different than
what you’ve been thinking about it for awhile. I’m
curious—what would you feel if you said to yourself,
“I did not intentionally do anything to deprive some-
one else of family happiness. I deserve to be happy
in becoming a father.”
T
OM: I’d feel less guilty for sure, and even happy.
T
HERAPIST: Let’s get this all written down. Now you
have the job of holding on to these new insights and
practicing them. Read over this worksheet every day
until you see me again. I’d also like you to take these
other thoughts on your original Challenging Beliefs
Worksheet about this topic and put them on separate
worksheets and work through them. Can you commit
to doing that?
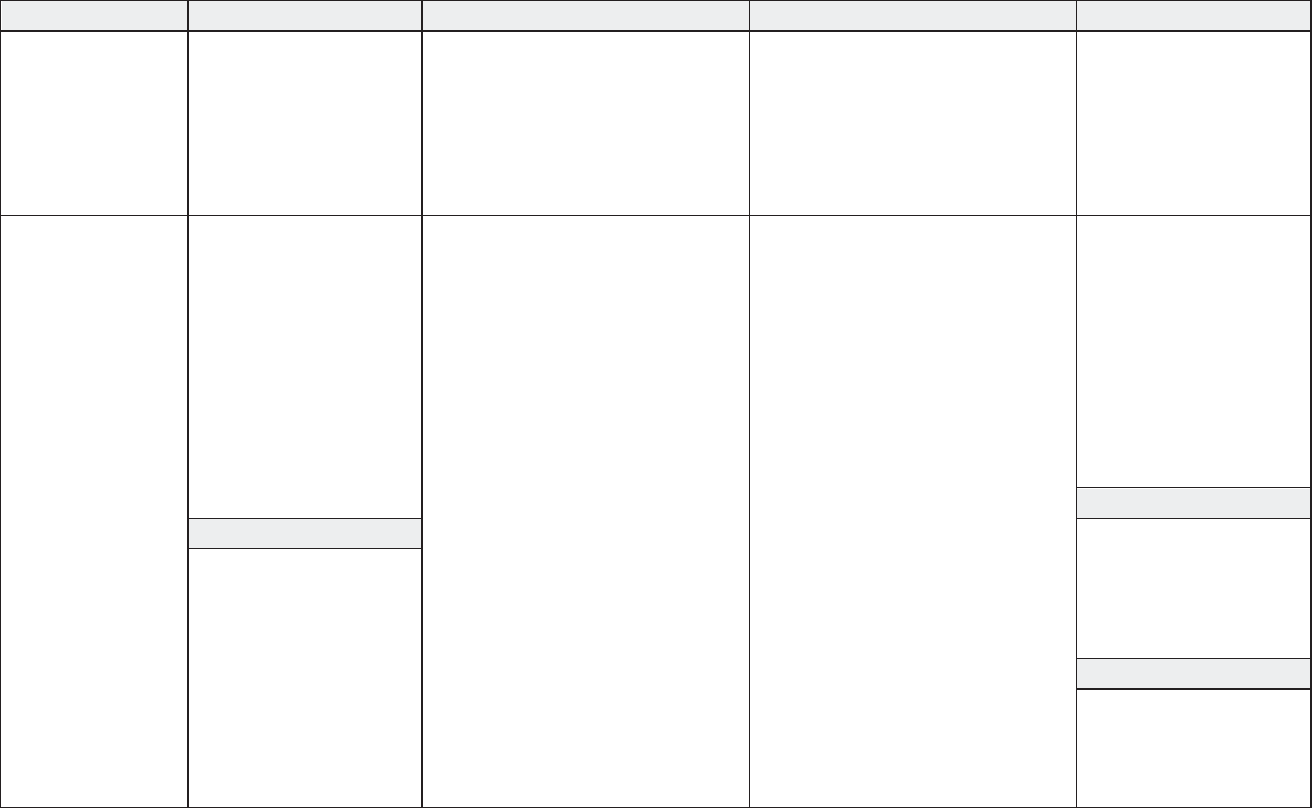
A. Situation
B. Thoughts
D. Challenging Thoughts
E. Problematic Patterns
F. Alternative Thought
Describe the event,
thought, or belief
leading to the
unpleasant
emotion(s).
Write thought(s) related to
Column A.
Rate belief in each thought
below from 0–100%.
(How much do you believe
this thought?)
Use Challenging Questions to
examine your automatic thoughts from
Column B.
Is the thought balanced and factual or
extreme?
Use the Problematic Thinking
Patterns sheet to decide if this is one
of your problematic patterns of
thinking.
What else can I say
instead of Column B?
How else can I interpret
the event instead of
Column B?
Rate belief in alternative
thought(s) from 0–100%.
Evidence? Jumping to conclusions
Killing a pregnant
Iraqi woman and
her son.
“It isn’t right that I’m
happy with a baby on the
way, given what
happened.”
(80%)
Habit or fact?
Interpretations not accurate?
All or none?
Exaggerating or minimizing
Disregarding important aspects
Oversimplifying
“My intentions are what
matter. I didn’t intend to
do anything to deprive
someone else of family
happiness.”
(85%)
“She might not have
been part of a terrorist
plot, but just a
passenger.”
(50%)
Extreme or exaggerated?
Out of context?
Source unreliable?
Overgeneralizing
Mind reading
I’m trying to figure out what was in
her head.
G. Rerate Old Thoughts
C. Emotion(s)
Low versus high probability?
Based on feelings or facts?
Irrelevant factors?
Her intentions are not relevant. Mine
are.
Emotional reasoning
Rerate how much you now
believe the thought in
Column B from 0–100%.
15%
(2
nd
doesn’t matter)
Specify sad, angry, etc.,
and rate how strongly you
feel each emotion from 0–
100%.
Guilt (85%)
H. Emotion(s)
Now what do you feel? 0–
100%
Guilt (5%)
Happy (10%)
FIGURE 2.6. Challenging Beliefs Worksheet regarding trauma.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under Inte
1
r
0
na
3
tional Copyright Convention.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
104 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
TOM: Yes, I already feel lighter.
T
HERAPIST: This is an exciting time—you’ve got to
continue to work on this, so that you can have the
enjoyment you deserve!
At this point, the therapist introduced the Power/
Control module. Tom admitted that prior to the trau-
matic event, he was someone who liked to be in control.
He did not like unpredictability, and he noticed that this
tendency had gotten especially bad after his friend’s
suicide. The military lifestyle seemed to be congruent
with this tendency. Tom indicated that he had not had
authority issues prior to the traumatic event, but he had
noticed himself questioning authority much more since
his military trauma. As with previous sessions, Tom
was given the practice assignment to complete Chal-
lenging Beliefs Worksheets every day prior to the next
session, and at least one was assigned on power/control.
Session 10
Tom began the session by saying that his wife had gone
to her obstetrician the previous day, and that her labor
would be induced in 1 week if she did not naturally
go into labor before then. Tom indicated that the last
session had been very good in helping him to become
happier about his child’s impending birth, and that he
had read the Challenging Questions Worksheet about
deserving to be happy several times since the last ses-
sion. He believed it more and more. He stated that he
was still having some anxiety about becoming a father,
and about everything going OK with his wife’s labor
and delivery. The therapist normalized some of Tom’s
anxiety, stressing how it was very natural for a first-
time father, and Tom was able to recognize the typical-
ity of this anxiety in others he had witnessed becoming
parents.
Tom stated that since reading the Power/Control
module after the last session, he had started to realize
that not everyone in authority over him had wielded his/
her authority malevolently. This was very important in
light of Tom’s preexisting history of desiring to exert
control; he had directly confronted his illusion of con-
trol. The therapist and Tom went over this worksheet.
Tom went on to describe how his belief that he could
and should have control over everything had resulted
in low self-esteem. In general, when things did not go
as he desired, Tom felt as though he was a failure for
not controlling the outcome. This belief structure led
him to think that he should have been able to control
his friend and stop him from committing suicide. It
also led him to believe that he should have been able
to create a positive outcome in the military traumatic
event. This discussion served as a natural segue to the
next topic—esteem. Tom admitted that he had become
someone who thrived too much on accomplishment.
This had affected his self-esteem and was especially
relevant to his belief that he had not accomplished his
goal in the military because he had to be taken from the
field after the traumatic event at the checkpoint.
After reviewing the Esteem module, the therapist
asked Tom to complete Challenging Beliefs Work-
sheets on his remaining stuck points, as well as any
stuck points relating to esteem. He was also given two
other assignments: to practice giving and receiving
compliments every day, and to do one nice thing for
himself every day that was not contingent on “achiev-
ing” something. These assignments were to help him
with his self- and other-esteem.
Session 11
Tom completed a worksheet on self-esteem related to
his belief that he had not achieved his goal within the
military. The therapist and Tom went over this work-
sheet, and both noted that he had made significant
progress by using the worksheet to change the way he
thought and felt about himself. He asserted that he was
beginning to see that people are much more than their
professional accomplishments. They also have other
activities and relationships with their families, friends,
and themselves.
The therapist inquired about the assignment of giv-
ing and receiving compliments. Tom replied that it had
gone well, even though it felt a bit awkward and forced.
He was even able to notice that when he gave compli-
ments and was more positive toward other people, he
seemed to get more positive responses back from them.
The therapist noticed that several of the compliments
were to his wife, and she pointed out that Tom seemed
more connected to his wife. He said that he was ac-
tually beginning to feel glimmers of excitement about
the birth of their child. He reported that he was still
feeling some anxiety about becoming a father, and
about how the labor and delivery would go, but that
the anxiety was less and more manageable. When the
therapist asked about Tom receiving compliments, he
reported more difficulties. She asked what Tom typi-
cally did when he received compliments, and it became
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
105
clear that he often deflected or minimized them. Cor-
respondingly, Tom also said that he had only done one
nice thing for himself since the last session, and that it
had felt uncomfortable. This pattern seemed to fit with
Tom’s overall schema of being unworthy and undeserv-
ing. The following dialogue ensued between the thera-
pist and Tom:
THERAPIST: It seems like you have a hard time letting
someone be nice to you and being nice to yourself.
T
OM: Yes.
T
HERAPIST: Why do you think that is?
T
OM: I don’t know. (Pauses.) I don’t like it. It feels like
they shouldn’t be nice to me, and I shouldn’t be nice
to me.
T
HERAPIST: Hmm . . . I wonder if there is anything
“off” about that thinking? What do you think?
T
OM: As I hear myself say it, it sounds a little weird.
It sounds like I don’t deserve to have nice things for
me. Kind of like not deserving to have a family . . .
T
HERAPIST: This seems like a larger tendency in your
life—one of those problematic thinking patterns.
What pattern do you hear in your thinking? Look at
the worksheet if you want to.
T
OM: Maybe emotional reasoning. I feel like I don’t de-
serve it; therefore, I must not deserve it. That seems
like the best one. Maybe I’m also drawing a conclu-
sion when the evidence is lacking.
T
HERAPIST: I agree. Given how much you seem to fol-
low this pattern of thinking, I’m betting it has been
around for awhile—maybe even before the shooting
occurred in Iraq.
T
OM: It has. I think it had to do with my dad, his alco-
holism, and not being close to me. As a kid, I always
thought I had done something wrong, or that I was so
bad that he didn’t want to be around me.
T
HERAPIST: Now, with adult eyes, what do you think
about your dad not being close to you?
T
OM: I figure that he drank for a reason, and that it
might have been me and my other brothers and sis-
ters.
T
HERAPIST: Why do you assume that he drank because
of you kids?
T
OM: I don’t know. I figure it was stressful having four
kids.
T
HERAPIST: It probably was at times, but as you hear
yourself talk about this, what is amiss in how you’ve
made sense of his drinking and being close to you?
T
OM: I’ve known other people who had four kids and
didn’t have drinking problems. There were a lot of
big families where I grew up. Plus, I know that he
and my mom had money problems when we were
young, and that they fought a lot.
T
HERAPIST: So, again, why then do you assume it was
you who caused his drinking and alienation?
T
OM: When we talk about it, I guess I see that it might
not have been me alone.
T
HERAPIST: Or not even you at all. Everybody has a
choice about how they handle their stress, and it
seems that he was distant from everyone, not just
you.
T
OM: True. It still feels that way.
T
HERAPIST: There seems to be a well-worn path in your
brain that when something goes wrong, you blame
yourself. The next step is that you deserve to be pun-
ished, or at least you don’t deserve anything good.
I don’t think this tendency is going to change over-
night. You’re going to need to work hard at talking
to yourself more rationally to change how you feel.
For that new path to get worn, you’re going to have
to walk down it a number of times. Pretty soon, the
path will be more worn and automatic. It will take
some effort, but you can change the way you auto-
matically feel. I’d like you to do a Challenging Be-
liefs Worksheet about what we’ve just talked about.
Once we get a good one about it, you can read and
refer to it as part of forging that new path. Can you
do that?
TOM: Yes. I think it would be good.
This exchange regarding Tom’s dad dovetailed nice-
ly with the final module, Intimacy. The therapist noted
that people tend to think of intimacy as it relates to ro-
mantic relationships, and especially in terms of sexual
intimacy. She stressed that there are all kinds of intima-
cy with different people. In essence, intimacy relates to
how close and open we feel with other people. She went
on to discuss the notion of self-intimacy, or how well
we take care of, support, and soothe ourselves. In other
words, it reflects how good a relationship we have with
ourselves. Tom admitted that he struggled with being
close to other people, which had most obviously mani-
fested in the work he had done relative to his wife and
unborn child. As noted earlier, Tom also struggled with
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
106 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
doing nice things and taking good care of himself. Both
of these areas seemed to be affected by Tom’s underly-
ing schema that he was undeserving and unworthy.
The therapist assigned daily Challenging Beliefs
Worksheets and requested that he do worksheets on
being nice to himself and being close to his wife. In ad-
dition, she asked Tom to write a final Impact Statement,
specifically about his understanding of the trauma now,
after all the work he had done. The therapist asked him
to write about his current thoughts/beliefs in the areas
of safety, trust, power/control, esteem, and intimacy.
Session 12
The day after Session 11, Tom left a message indicating
that his wife had delivered a healthy baby girl. He indi-
cated in his voice mail message that he felt happy and
relieved. He went on about how beautiful the baby was,
how well his wife had done in labor and delivery, and
how he had enjoyed holding his daughter in his arms
the first time. The 12th session was delayed an extra
week because of the baby’s arrival.
Tom’s wife and new daughter accompanied him to
the final session. The therapist spent some time admir-
ing Tom’s new baby and congratulating his wife before
starting the final session. Tom seemed genuinely proud
and happy about his daughter, and noted that becoming
a father had been more natural than he had anticipated.
He commented that he had been worried that he would
not want to hold the infant for fear of hurting her or be-
cause he would do something wrong. Instead, he found
it almost “instinctual” to hold her, and that soothing
her had come more naturally than he expected. Tom
seemed surprised about how natural his role as a father
had come.
The therapist inquired about how the assignments
had gone. Tom said that he had not done as much as
he had hoped given the baby’s arrival, but that he had
done worksheets about his father and about being close
to his wife. The therapist looked over these worksheets,
which Tom had done very well. She asked Tom about
how helpful they had been, and he reported that they
had been very helpful. He added that he was still strug-
gling about his father, but that he was beginning to
think that it was not all about him, which had made him
feel better about himself and less guilty in general. He
mentioned that he was considering writing a letter to
his father about his daughter’s arrival, and that he was
thinking about asking his father about why he drank
and distanced himself from his family. The therapist
reinforced Tom for considering this and for not blind-
ly making assumptions about his role in his father’s
drinking. However, she also attempted to inoculate
Tom to the possibility that his father could blame him
or his siblings for his alcoholism (given that she did
not know his father or his history), and that this did not
necessarily mean that it was true. She reminded him
that he needed to consider the source of information,
and that any good detective would get multiple reports.
Tom seemed to like the idea of getting more informa-
tion from others, mentioning that he and his siblings
had never really talked about his belief that they were
to blame for their father’s alcoholism.
Tom also shared that he better understood the idea
of having intimacy, without sex, in his relationship with
his wife. He said that since the birth of their child, he
felt closer to his wife and had generally been more open
and present to her. The therapist asked him about doing
nice things for himself, and Tom laughed and said that
he was more open to that but was finding less time to
do it with a new baby.
The therapist then asked Tom to read the final Im-
pact Statement about the meaning of the event for him
after the work that he had done. He wrote:
There is no doubt that this traumatic event has deeply
impacted me. My thoughts about myself, others, and
the world were changed. When I started therapy, I
believed that I was a murderer. I blamed myself com-
pletely. Now, I believe that I shot a family, but I did not
murder them. I realize that I and others around me had
to do what we did at the time, and that we chose to shoot
because we had to. I will never know what that man,
or maybe even the family, was trying to do by going
through that checkpoint, but I know now that I had no
choice but to shoot to stop them. Regarding safety, I
used to think that there were people out to get me, but
now I realize that the probability of that is slim. I still
feel a little anxious about me, my wife, and now my
daughter, getting hurt, but not by a sniper. That seems
unlikely. Now I worry about the stuff that everyone
worries about—like crazy drivers, illness, or some ac-
cident. About safety, I used to worry that I was going
to go “off” and hurt my family. I don’t believe that I
will do that because I’ve never done that before and
basically this trauma messed with my head about how
likely I would be to hurt someone unless I had to. I’m
trusting myself more in terms of the decisions I make,
and I have some more faith and trust in my government
now that I realize I really needed to shoot in that situa-
tion. I think I may always struggle with wanting to have
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
107
power and control over things, but I’m working on not
having control over everything. The fact is, I don’t have
control, even though I like to think that I do. My self-
esteem is improving. I have to remember that not every
bad thing that happens is my fault, and that I deserve
to be happy even if I don’t fully believe it yet. One of
the biggest things that seems to be changing is that I’m
enjoying being close to my wife and my new daughter.
I used to avoid my wife because I thought I didn’t de-
serve to be happy and that I might hurt her. Slowly I’m
realizing that it is not very likely that I’ll hurt my wife
or my new daughter, or at least hurt them intentionally.
My wife seems much happier now. I want to hold on
to this time in my life and provide a good life for my
daughter and wife. I’m happy to know that my daughter
is not going to know someone who thought that snipers
were out to get him, and who was anxious, avoiding
everything and everyone. It sounds silly, but I’m kind of
glad that I went through this because I think I’m going
to be better dad and person because of it.
Tom was a bit teary as he finished reading. The
therapist asked Tom whether he remembered what he
wrote the first time. Tom said no, so the therapist read
to him his first Impact Statement. She pointed out that
Tom had come a long way, and he agreed. The thera-
pist and Tom reviewed the whole therapy process, what
they had covered, and the “stuck points” that Tom had
challenged. Tom said that he was going to continue
using the worksheets because they had been so helpful
in making him slow down to think about things instead
of just reacting. They did some lapse planning, and the
therapist asked Tom what he could do if he sensed that
he was struggling with PTSD or depressive symptoms,
or second-guessing his new ways of thinking. He men-
tioned that he was going to share the materials with
his wife because she was very good at helping him to
“get his head on straight.” He also included on his list
a review of the materials he had completed during the
course of therapy. The therapy session ended with a dis-
cussion of Tom’s goal to write his father a letter and to
increase his contact with his siblings. He was planning
to use these contacts to discover more about the reasons
his father was alcoholic and had seemed to abandon the
family. Tom also shared his goals about the type of fa-
ther and husband he hoped to be, and what his profes-
sional future held as he left the military. The therapist
congratulated Tom on his willingness to do the hard
work to recover from what happened to him and wished
him the best with his family and future. Tom expressed
his appreciation for the therapy.
REFERENCES
American Psychiatric Association. (1994). Diagnostic and
statistical manual of mental disorders (4th ed.). Washing-
ton, DC: Author.
American Psychiatric Association. (2013). Diagnostic and
statistical manual of mental disorders (5th ed.). Arling-
ton, VA: Author.
Astin, M. C., Layne, C. M., Camilleri, A. J., & Foy, D. W.
(1994). Posttraumatic stress disorder in victimization-
related traumata. In I. J. Briere (Ed.), Assessing and treat-
ing victims of violence: New directions for mental health
services (pp. 39–51). San Francisco: Jossey-Bass.
Becker, J. V., Skinner, L. J., Abel, G. G., Axelrod, R., &
Cichon, J. (1984). Sexual problems of sexual assault survi-
vors. Women and Health, 9, 5–20.
Beckham, J. C., Feldman, M. E., & Kirby, A. C. (1998).
Atrocities exposure in Vietnam combat veterans with
chronic posttraumatic stress disorder: Relationship to
combat exposure, symptom severity, guilt, and interper-
sonal violence. Journal of Traumatic Stress, 11, 777–785.
Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G.,
Gusman, F. D., Charney, D. S., et al. (1995). The develop-
ment of a Clinician-Administered PTSD Scale. Journal of
Traumatic Stress, 8, 75–90.
Blanchard, E. B., Hickling, E. J., Buckley, T. C., & Taylor, A.
E. (1996). Psychophysiology of posttraumatic stress dis-
order related to motor vehicle accidents: Replication and
extension. Journal of Consulting and Clinical Psychology,
64, 742–751.
Blanchard, E. B., Hickling, E. J., Devinei, T., Veazey, C. H.,
Galovski, T. E., & Mundy, E. (2003). A controlled evalu-
ation of cognitive behavioral therapy for posttraumatic
stress in motor vehicle accident survivors. Behaviour Re-
search and Therapy, 41, 79–96.
Bowen, G. R., & Lambert, J. A. (1986). Systematic desensiti-
zation therapy with post-traumatic stress disorder cases. In
C. R. Figley (Ed.), Trauma and its wake: Vol. II. Traumat-
ic stress theory, research, and intervention (pp. 280–291).
New York: Brunner/Mazel.
Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D.
(2005). A multidimensional meta-analysis of psycho-
therapy for PTSD. American Journal of Psychiatry, 162,
214–227.
Breslau, N., Davis, G. C., & Andreski, P. (1995). Risk factors
for PTSD-related traumatic events: A prospective analy-
sis. American Journal of Psychiatry, 152, 529–535.
Brewin, C. R., Dalgleish, T., & Joseph, S. (1996). A dual rep-
resentation theory of posttraumatic stress disorder. Psy-
chological Review, 103, 670–686.
Briere, J. (1995). The Trauma Symptom Inventory (TSI): Pro-
fessional manual. Odessa, FL: Psychological Assessment
Resources.
Brom, D., Kleber, R. J., & Defares, P. B. (1989). Brief psy-
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
108 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
chotherapy for PTSD. Journal of Consulting and Clinical
Psychology, 57, 607–612.
Bryant, R. A., Moulds, M. L., Guthrie, R. M., Dang, S. T., &
Nixon, R. D. V. (2003). Imaginal exposure alone and ima-
ginal exposure with cognitive restructuring in treatment of
posttraumatic stress disorder. Journal of Consulting and
Clinical Psychology, 71, 706–712.
Buckley, T. C., Blanchard, E. B., & Hickling, E. J. (1998).
A confirmatory factor analysis of posttraumatic stress
symptoms. Behaviour Research and Therapy, 36, 1091–
1099.
Burt, M. R. (1980). Cultural myths and supports for rape.
Journal of Personality and Social Psychology, 38, 217–
230.
Chard, K. M. (2005). An evaluation of cognitive processing
therapy for the treatment of posttraumatic stress disorder
related to childhood sexual abuse. Journal of Consulting
and Clinical Psychology, 73, 965–971.
Chemtob, C., Roitblat, H. L., Hamada, R. S., Carlson, J. G.,
& Twentyman, C. T. (1988). A cognitive action theory of
post-traumatic stress disorder. Journal of Anxiety Disor-
ders, 2, 253–275.
Cloitre, M. (1998). Sexual revictimization: Risk factors
and prevention. In V. M. Follette, J. I. Ruzek, & F. R.
Abueg (Eds.), Cognitive-behavioral therapies for trauma
(pp. 278–304). New York: Guilford Press.
Cloitre, M., Koenen, K. C., Cohen, L. R., & Han, H. (2002).
Skills training in affective and interpersonal regulation
followed by exposure: A phase-based treatment for PTSD
related to childhood abuse. Journal of Consulting and
Clinical Psychology, 70, 1067–1074.
Cloitre, M., Petkova, E., Wang, J., & Lu Lassell, F. (2012). An
examination of the influence of a sequential treatment on
the course and impact of dissociation among women with
PTSD related to childhood abuse. Depression and Anxi-
ety, 29, 707–717.
Cloitre, M., Stovall-McClough, K. C., Miranda, R., & Chem-
tob, C. M. (2004). Therapeutic alliance, negative mood
regulation, and treatment outcome in child abuse-related
posttraumatic stress disorder. Journal of Consulting and
Clinical Psychology, 72, 411–416.
Cox, B. J., Clara, I. P., & Enns, M. W. (2002). Posttraumatic
stress disorder and the structure of common mental disor-
ders. Depression and Anxiety, 15, 168–171.
Creamer, M., Burgess, P., & Pattison, P. (1992). Reactions to
trauma: A cognitive processing model. Journal of Abnor-
mal Psychology, 101, 452–459.
Creamer, M., Morris, P., Biddle, D., & Elliott, P. (1999).
Treatment outcome in Australian veterans with combat-
related posttraumatic stress disorder: A cause for cautious
optimism? Journal of Traumatic Stress, 12, 545–558.
Dalgleish, T. (2004). Cognitive approaches to posttraumatic
stress disorder: The evolution of multirepresentational
theorizing. Psychological Bulletin, 130, 228–260.
Denny, N., Robinowitz, R., & Penk, W. (1987). Conduct-
ing applied research on Vietnam combat-related post-
traumatic stress disorder. Journal of Clinical Psychology,
43, 56–66.
Derogatis, L. R. (1983). SCL-90-R: Administration, scoring
and procedures manual–II. Towson, MD: Clinical Psy-
chometric Research.
Devilly, G. J., & Spence, S. H. (1999). The relative efficacy
and treatment distress of EMDR and a cognitive-behavior
trauma treatment protocol in the amelioration of posttrau-
matic stress disorder. Journal of Anxiety Disorders, 13,
131–157.
Dohrenwend, B. P., Turner, J. B., Turse, N. A., Adams, B. G.,
Koenen, K. C., & Marshall, R. (2006). The psychological
risks of Vietnam for U.S. veterans: A revisit with new data
and methods. Science, 313, 979–982.
Ehlers, A., & Clark, D. M. (2000). A cognitive model of post-
traumatic stress disorder. Behaviour Research and Thera-
py, 38, 319–345.
Ehlers, A., Clark, D. M., Hackmann, A., McManus, F., Fen-
nell, M., Herbert, C., et al. (2003). A randomized con-
trolled trial of cognitive therapy, a self-help booklet, and
repeated assessments as early interventions for posttrau-
matic stress disorder. Archives of General Psychiatry, 60,
1024-1032.
Ehlers, A., Hackmann, A., Steil, R., Clohessy, S., Wenninger,
K., & Winter, H. (2002). The nature of intrusive memories
after trauma: The warning signal hypothesis. Behaviour
Research and Therapy, 40, 995–1002.
Falsetti, S. A., Resnick, H. S., Resick, P. A., & Kilpatrick, D.
G. (1993). The Modified PTSD Symptom Scale: A brief
self-report measure of posttraumatic stress disorder. Be-
havior Therapist, 16, 161–162.
First, M. B., Spitzer, R. L., Williams, J. B. W., & Gibbon,
M. (1995). Structured Clinical Interview for DSM-IV—
Patient Edition (SCID-P). Washington, DC: American
Psychiatric Press.
Foa, E. B. (1995). Posttraumatic Stress Diagnostic Scale
(manual). Minneapolis, MN: National Computer Systems.
Foa, E. B., Dancu, C. V., Hembree, E. A., Jaycox, L. H.,
Meadows, E. A., & Street, G. P. (1999). A comparison
of exposure therapy, stress inoculation training, and their
combination for reducing posttraumatic stress disorder in
female assault victims. Journal of Consulting and Clinical
Psychology, 67, 194–200.
Foa, E. B., Hembree, E. A., Cahill, S. E., Rauch, S. A. M.,
Riggs, D. S., Feeny, N. C., et al. (2005). Randomized trial
of prolonged exposure for posttraumatic stress disorder
with and without cognitive restructuring: Outcome at aca-
demic and community clinics. Journal of Consulting and
Clinical Psychology, 73, 953–964.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A.
(Eds.). (2008). Effective treatments for PTSD: Practice
guidelines from the International Society for Traumatic
Stress Studies (2nd ed.). New York: Guilford Press.
Foa, E. B., Riggs, D. S., Dancu, C. V., & Rothbaum, B. O.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
109
(1993). Reliability and validity of a brief instrument for
assessing post-traumatic stress disorder. Journal of Trau-
matic Stress, 6, 459–473.
Foa, E. B., & Rothbaum, B. O. (1998). Treating the trauma of
rape: Cognitive-behavioral therapy for PTSD. New York:
Guilford Press.
Foa, E. B., Rothbaum, B., Riggs, D., & Murdock, T. (1991).
Treatment of posttraumatic stress disorder in rape victims:
A comparison between cognitive-behavioral procedures
and counseling. Journal of Consulting and Clinical Psy-
chology, 59, 715–723.
Foa, E. B., Steketee, G., & Rothbaum, B. O. (1989). Behav-
ioral/cognitive conceptualizations of post-traumatic stress
disorder. Behavior Therapy, 20, 155–176.
Frank, E., Anderson, B., Stewart, B. D., Dancu, C., Hughes,
C., & West, D. (1988). Efficacy of cognitive behavior ther-
apy and systematic desensitization in the treatment of rape
trauma. Behavior Therapy, 19, 403–420.
Frank, E., & Stewart, B. D. (1983). Treating depression in
victims of rape. Clinical Psychologist, 36, 95–98.
Frank, E., & Stewart, B. D. (1984). Depressive symptoms in
rape victims: A revisit. Journal of Affective Disorders, 1,
269–277.
Green, B. L. (1996). Trauma History Questionnaire. In B. H.
Stamm (Ed.), Measurement of stress, trauma, and adap-
tation (pp. 366–369). Lutherville, MD: Sidran.
Griffin, M. G., Resick, P. A., & Mechanic, M. B. (1997). Ob-
jective assessment of peritraumatic dissociation: Psycho-
physiological indicators. American Journal of Psychiatry,
154, 1081–1088.
Griffin, M. G., Uhlmansiek, M. H., Resick, P. A., & Me-
chanic, M. B. (2004). Comparison of the Posttraumatic
Stress Disorder Scale versus the Clinician-Administered
Posttraumatic Stress Disorder Scale in domestic violence
survivors. Journal of Traumatic Stress, 17, 497–504.
Gutner, C., Rizvi, S. L., Monson, C. M., & Resick, P. A.
(2006). Changes in coping strategies, relationship to the
perpetrator, and posttraumatic stress disorder in female
crime victims. Journal of Traumatic Stress, 19, 813–823.
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006).
Mental health problems, use of mental health services,
and attrition from military service after returning from de-
ployment to Iraq or Afghanistan. Journal of the American
Medical Association, 295, 1023–1032.
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cot-
ting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq
and Afghanistan, mental health problems, and barriers to
care. New England Journal of Medicine, 351, 13–22.
Holmes, M. R., & St. Lawrence, J. S. (1983). Treatment of
rape-induced trauma: Proposed behavioral conceptualiza-
tion and review of the literature. Clinical Psychology Re-
view, 3, 417–433.
Horowitz, M. J. (1986). Stress response syndromes (2nd ed.).
New York: Aronson.
Ironson, G., Freund, B., Strauss, J. L., & Williams, J. (2002).
Comparison of two treatments for traumatic stress: A
community-based study of EMDR and prolonged expo-
sure. Journal of Clinical Psychology, 58, 113–128.
Janoff-Bulman, R. (1985). The aftermath of victimization:
Rebuilding shattered assumptions. In C. R. Figley (Ed.),
Trauma and its wake: Vol. I. The study and treatment
of posttraumatic stress disorder (pp. 15–35). New York:
Brunner/Mazel.
Janoff-Bulman, R. (1992). Shattered assumptions: Towards a
new psychology of trauma. New York: Free Press.
Jordan, B. K., Marmar, C. R., Fairbank, J. A., Schlenger, W.
E., Kulka, R. A., Hough, R. L., et al. (1992). Problems
in families of male Vietnam veterans with posttraumatic
stress disorder. Journal of Consulting and Clinical Psy-
chology, 60, 916–926.
Keane, T. M., Brief, D. J., Pratt, E. M., & Miller, M. W.
(2007). Assessment and its comorbidities in adults. In M.
J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Hand-
book of PTSD: Science and practice (pp. 279–305). New
York: Guilford Press.
Keane, T. M., Caddell, J. M., & Taylor, K. L. (1988). Missis-
sippi Scale for Combat-Related Posttraumatic Stress Dis-
order: Three studies in reliability and validity. Journal of
Consulting and Clinical Psychology, 56, 85–90.
Keane, T. M., Fairbank, J. A., Caddell, J. M., & Zimering, R.
T. (1989). Implosive (flooding) therapy reduces symptoms
of PTSD in Vietnam combat veterans. Behavior Therapy,
20, 245–260.
Keane, T. M., Kolb, L. C., Kaloupek, D. G., Orr, S. P.,
Blanchard, E. B., Thomas, R. G., et al. (1998). Utility of
psychophysiology measurement in the diagnosis of post-
traumatic stress disorder: Results from a Department of
Veteran’s Affairs cooperative study. Journal of Consulting
and Clinical Psychology, 66, 914–923.
Keane, T. M., Malloy, P. F., & Fairbank, J. A. (1984). Empiri-
cal development of an MMPI subscale for the assessment
of combat-related posttraumatic stress disorder. Journal of
Consulting and Clinical Psychology, 52, 888–891.
Keane, T. M., Zimering, R. T., & Caddell, J. M. (1985). A
behavioral formulation of posttraumatic stress disorder.
Behavior Therapist, 8, 9–12.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas,
K. R., & Walters, E. E. (2005). Lifetime prevalence and
age-of-onset distributions of DSM-IV disorders in the Na-
tional Comorbidity Survey Replication. Archives of Gen-
eral Psychiatry, 62, 593–602.
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., &
Walters, E. E. (2005). Prevalence, severity, and comorbid-
ity of 12-month DSM-IV disorders in the National Comor-
bidity Survey Replication. Archives of General Psychia-
try, 62, 617–627.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nel-
son, C. B. (1995). Posttraumatic stress disorder in the Na-
tional Comorbidity Survey. Archives of General Psychia-
try, 52, 1048–1060.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
110 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
Kilpatrick, D. G. (1983). Rape victims: Detection, assessment
and treatment. Clinical Psychologist, 36, 92–95.
Kilpatrick, D. G., & Amick, A. E. (1985). Rape trauma. In
M. Hersen & C. Last (Eds.), Behavior therapy casebook
(pp. 86–103). New York: Springer.
Kilpatrick, D. G., Edmunds, C. N., & Seymour, A. K. (1992).
Rape in America: A report to the nation. Arlington, VA:
National Victim Center.
Kilpatrick, D. G., Resnick, H. S., & Freedy, J. R. (1991). The
Potential Stressful Events Interview. Unpublished instru-
ment, National Crime Victims Research and Treatment
Center, Medical University of South Carolina, Charleston.
Kilpatrick, D. G., Saunders, B. E., Veronen, L. J., Best, C.
L., & Von, J. M. (1987). Criminal victimization: Lifetime
prevalence, reporting to police, and psychological impact.
Crime and Delinquency, 33, 479–489.
Kilpatrick, D. G., & Veronen, L. J. (1983). Treatment for
rape-related problems: Crisis intervention is not enough.
In L. H. Cohen, W. L. Claiborn, & G. A. Specter (Eds.),
Crisis intervention (pp. 165–185). New York: Human Sci-
ences Press.
Kilpatrick, D. G., Veronen, L. J., & Best, C. L. (1985). Factors
predicting psychological distress among rape victims. In
C. R. Figley (Ed.), Trauma and its wake: Vol. I. The study
and treatment of posttraumatic stress disorder (pp. 114–
141). New York: Brunner/Mazel.
Kilpatrick, D. G., Veronen, L. J., & Resick, P. A. (1982).
Psychological sequelae to rape: Assessment and treat-
ment strategies. In D. M. Doleys, R. L. Meredith, & A.
R. Ciminero (Eds.), Behavioral medicine: Assessment
and treatment strategies (pp. 473–497). New York: Ple-
num Press.
Koss, M. P., & Harvey, M. R. (1991). The rape victim: Clini-
cal and community interventions (2nd ed.). Thousand
Oaks, CA: Sage.
Kubany, E. S., Haynes, S. N., Leisen, M. B., Owens, J. A., Ka-
plan, A. S., Watson, S. B., et al. (2000). Development and
preliminary validation of a brief broad-spectrum measure
of trauma exposure: The Traumatic Life Events Question-
naire. Psychological Assessment, 12, 210–224.
Kubany, E. S., Hill, E. E., Owens, J. A., Iannce-Spencer, C.,
McCaig, M. A., & Tremayne, K. J. (2004). Cognitive trau-
ma therapy for battered women with PTSD (CTT-BW).
Journal of Consulting and Clinical Psychology, 72, 3–18.
Kubany, E. S., Leisen, M. B., Kaplan, A. S., & Kelly, M. P.
(2000). Validation of a brief measure of posttraumatic
stress disorder: The Distressing Event Questionnaire
(DEQ). Psychological Assessment, 12, 197–209.
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R.
L., Jordan, B. K., Marmar, C. R., et al. (1990). Trauma
and the Vietnam war generation: Report of findings from
the National Vietnam Veterans Readjustment Study. New
York: Brunner/Mazel.
Lang, P. J. (1968). Fear reduction and fear behavior: Problems
in treating a construct. In J. M. Schlien (Ed.), Research in
psychotherapy (pp. 90–102). Washington, DC: American
Psychological Association.
Lang, P. J. (1977). Imagery in therapy: An information pro-
cessing analysis of fear. Behavior Therapy, 8, 862–886.
Lanius, R. A., Vermetten, E., Loewenstein, R. J., Brand, B.,
Schmahl, C., Bremner, J. D., et al. (2010). Emotion modu-
lation in PTSD: Clinical and neurobiological evidence for
a dissociative subtype. American Journal of Psychiatry,
167(6), 640–647.
Lauterbach, D., & Vrana, S. R. (1996). Three studies on the
reliability and validity of a self-report measure of posttrau-
matic stress disorder. Assessment, 3, 17–25.
Lauterbach, D., Vrana, S., King, D. W., & King, L. A. (1997).
Psychometric properties of the civilian version of the Mis-
sissippi PTSD scale. Journal of Traumatic Stress, 10,
499–513.
Lee, C., Gavriel, H., Drummond, P., Richards, J., & Green-
wald, R. (2002). Treatment of PTSD: Stress inoculation
training with prolonged exposure compared to EMDR.
Journal of Clinical Psychology, 58, 1071–1089.
Lester, K. M., Resick, P. A., Young-Xu, Y., & Artz, C. E.
(2010). Impact of ethnicity on early treatment termination
and outcomes in PTSD treatment. Journal of Consulting
and Clinical Psychology, 4, 480-489.
Mahoney, M. J., & Lyddon, W. J. (1988). Recent develop-
ments in cognitive approaches to counseling and psycho-
therapy. Counseling Psychologist, 16, 190–234.
Marks, I., Lovell, K., Noshirvani, H., Livanou, M., & Thrash-
er, S. (1998). Treatment of posttraumatic stress disorder
by exposure and/or cognitive restructuring: A controlled
study. Archives of General Psychiatry, 55, 317–325.
McCann, I. L., & Pearlman, L. A. (1990). Vicarious trauma-
tization: A framework for understanding the psychologi-
cal effects of working with victims. Journal of Traumatic
Stress, 3, 131–149.
McFall, M., Fontana, A., Raskind, M., & Rosenheck, R.
(1999). Analysis of violent behavior in Vietnam combat
veteran psychiatric inpatients with posttraumatic stress
disorder. Journal of Traumatic Stress, 12, 501–517.
McNair, L. D., & Neville, H. A. (1996). African American
women survivors of sexual assault: The intersection of
race and class. In M. Hill & E. D. Rothblum (Eds.), Clas-
sism and feminist therapy: Counting costs (pp. 107–118).
New York: Haworth.
Meichenbaum, D. H. (1985). Stress inoculation training.
Elmsford, NY: Pergamon.
Miller, M. W., Greif, J. L., & Smith, A. A. (2003). Multidi-
mensional Personality Questionnaire profiles of veterans
with traumatic combat exposure: Externalizing and inter-
nalizing subtypes. Psychological Assessment, 15, 205–215.
Miller, M. W., Kaloupek, D. G., Dillon, A. L., & Keane, T.
M. (2004). Externalizing and internalizing subtypes of
combat-related PTSD: A replication and extension using
the PSY-5 scales. Journal of Abnormal Psychology, 113,
636–645.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
111
Miller, M. W., & Resick, P. A. (2007). Internalizing and ex-
ternalizing subtypes in female sexual assault survivors:
Implications for the understanding of complex PTSD. Be-
havior Therapy, 38, 58–71.
Monson, C. M., Gradus, J. L., Young-Xu, Y., Schnurr, P. P.,
Price, J. A., Schumm, J. A. (2008). Change in posttrau-
matic stress disorder symptoms: Do clinicians and patients
agree? Psychological Assessment, 20, 131–138.
Monson, C. M., Price, J. L., & Ranslow, E. (2005, October).
Treating combat PTSD through cognitive processing ther-
apy. Federal Practitioner, 22(10), 75–83.
Monson, C. M., Schnurr, P. P., Resick, P. A., Friedman, M. J.,
Young-Xu, Y., & Stevens, S. P. (2006). Cognitive process-
ing therapy for veterans with military-related posttrau-
matic stress disorder. Journal of Consulting and Clinical
Psychology, 74, 898–907.
Morland, L. A., Hynes, A. K., Mackintosh, M., Resick, P.
A., & Chard, K. M. (2011). Group cognitive processing
therapy delivered to veterans via telehealth: A pilot cohort.
Journal of Traumatic Stress, 24, 465–469.
Mowrer, O. H. (1947). On the dual nature of learning—a re-
interpretation of “conditioning” and “problem-solving.”
Harvard Educational Review, 14, 102–148.
National Institute of Clinical Excellence. (2005). Post-
traumatic stress disorder (PTSD): The treatment of PTSD
in adults and children. London: Author.
Neuner, F., Schauer, M., Klaschik, C., Karunakara, U., &
Elbert, T. (2004). A comparison of narrative exposure
therapy, supportive counseling, and psychoeducation for
treating posttraumatic stress disorder in an African refu-
gee settlement. Journal of Consulting and Clinical Psy-
chology, 72, 579–587.
Norris, F. H. (1990). Screening for traumatic stress: A scale
for use in the general population. Journal of Applied So-
cial Psychology, 20, 1704–1718.
Norris, F. H. (1992). Epidemiology of trauma: Frequency and
impact of different potentially traumatic events on differ-
ent demographic groups. Journal of Consulting and Clini-
cal Psychology, 60, 409–418.
Oquendo, M. A., Friend, J. M., Halberstam, B., Brodsky, B.
S., Burke, A. K., Grunebaum, M. F., et al. (2003). Associa-
tion of comorbid posttraumatic stress disorder and major
depression with greater risk for suicidal behavior. Ameri-
can Journal of Psychiatry, 160, 580–582.
Orr, S. P., Lasko, N. B., Metzger, L. J., Berry, N. J., Ahern,
C. E., & Pitman, R. K. (1998). Psychophysiologic assess-
ment of women with posttraumatic stress disorder result-
ing from childhood sexual abuse. Journal of Consulting
and Clinical Psychology, 66, 906–913.
Orr, S. P., Metzger, L. J., Miller, M. W., & Kaloupek, D. G.
(2004). Psychophysiological assessment of PTSD. In J.
P. Wilson & T. M. Keane (Eds.), Assessing psychologi-
cal trauma and PTSD (2nd ed., pp. 289–343). New York:
Guilford Press.
Pitman, R. K., Orr, S. P., Altman, B., Longpre, R. E., Poire, R.
E., & Macklin, M. L. (1996). Emotional processing during
eye movement desensitization and reprocessing therapy of
Vietnam veterans with chronic posttraumatic stress disor-
der. Comprehensive Psychiatry, 37, 419–429.
Pitman, R. K., Orr, S. P., Forgue, D. F., & Altman, B. (1990).
Psychophysiologic responses to combat imagery of Viet-
nam veterans with posttraumatic stress disorder versus
other anxiety disorders. Journal of Abnormal Psychology,
99, 49–54.
Pitman, R. K., Orr, S. P., Forgue, D. F., de Jong, J., & Clai-
born, J. M. (1987). Psychophysiologic assessment of post-
traumatic stress disorder imagery in Vietnam combat vet-
erans. Archives of General Psychiatry, 44, 970–975.
Power, K., McGoldrick, T., Brown, K., Buchanan, R., Sharp,
D., & Swanson, V. (2002). A controlled comparison of
eye movement desensitization and reprocessing versus ex-
posure plus cognitive restructuring versus wait list in the
treatment of posttraumatic stress disorder. Clinical Psy-
chology and Psychotherapy, 9, 299–318.
Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan,
S. J., & Foa, E. B. (2010). A meta-analytic review of pro-
longed exposure for posttraumatic stress disorder. Clinical
Psychology Review, 30, 635–641.
Prins, A., Ouimette, P., Kimerling, R., Camerond, R. P., Hu-
gelshofer, D. S., Shaw-Hegwer, J., et al. (2004). The Pri-
mary Care PTSD Screen (PC-PTSD): Development and
operating characteristics. Primary Care Psychiatry, 9, 9–
14.
Renfrey, G., & Spates, C. R. (1994). Eye movement desensi-
tization: A partial dismantling study. Journal of Behavior
Therapy and Experimental Psychiatry, 25, 231–239.
Resick, P. A., Galovski, T. E., Uhlmansiek, M. O., Scher, C.
D., Clum, G., & Young-Xu, Y. (2008). A randomized clini-
cal trial to dismantle components of cognitive processing
therapy for posttraumatic stress disorder in female victims
of interpersonal violence. Journal of Consulting and Clin-
ical Psychology, 76, 243–258.
Resick, P. A., Jordan, C. G., Girelli, S. A., Hutter, C. K., &
Marhoeder-Dvorak, S. (1988). A comparative outcome
study of behavioral group therapy for sexual assault vic-
tims. Behavior Therapy, 19, 385–401.
Resick, P. A., & Markaway, B. E. (1991). Clinical treatment of
adult female victims of sexual assault. In C. R. Hollin & K.
Howells (Eds.), Clinical approaches to sex offenders and
their victims (pp. 261–284). London: Wiley.
Resick, P. A., Monson, C. M., & Chard, K. M. (2007). Cogni-
tive processing therapy: Veteran/military version. Wash-
ington, DC: Department of Veterans Affairs.
Resick, P. A., Nishith, P., & Griffin, M. G. (2003). How well
does cognitive-behavioral therapy treat symptoms of com-
plex PTSD?: An examination of child sexual abuse survi-
vors within a clinical trial. CNS Spectrums, 8, 340–355.
Resick, P. A., Nishith, P., Weaver, T. L., Astin, M. C., &
Feuer, C. A. (2002). A comparison of cognitive process-
ing therapy, prolonged exposure and a waiting condition
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
112 CLINICAL HANDBOOK OF PSYCHOLOGICAL DISORDERS
for the treatment of posttraumatic stress disorder in female
rape victims. Journal of Consulting and Clinical Psychol-
ogy, 70, 867–879.
Resick, P. A., & Schnicke, M. K. (1992). Cognitive process-
ing therapy for sexual assault victims. Journal of Consult-
ing and Clinical Psychology, 60, 748–756.
Resick, P. A., & Schnicke, M. K. (1993). Cognitive process-
ing therapy for rape victims: A treatment manual. New-
bury Park, CA: Sage.
Resick, P. A., Williams, L. F., Suvak, M. K., Monson, C. M.,
& Gradus, J. L. (2012). Long-term outcomes of cognitive-
behavioral treatments for posttraumatic stress disorder
among female rape survivors. Journal of Consulting and
Clinical Psychology, 80, 201–210.
Resnick, H. S., Kilpatrick, D. G., Dansky, B. S., Saunders, B.
E., & Best, C. L. (1993). Prevalence of civilian trauma and
posttraumatic stress disorder in a representative national
sample of women. Journal of Consulting and Clinical
Psychology, 61, 984–991.
Resnick, H. S., Kilpatrick, D. G., & Lipovsky, J. A. (1991).
Assessment of rape-related posttraumatic stress disorder:
Stressor and symptom dimensions. Psychological Assess-
ment, 3, 561–572.
Robins, L. N., Helzer, J. E., Croughan, J., & Ratcliff, K. S.
(1981). National Institute of Mental Health Diagnostic In-
terview Schedule: Its history, characteristics, and validity.
Archives of General Psychiatry, 38, 381–389.
Rosenheck, R., & Fontana, A. (1996). PTSD and community-
based treatment: A commentary on “PTSD diagnosis and
treatment for mental health clinicians.” Community Men-
tal Health Journal, 32, 191–193.
Rosenheck, R., Fontana, A., & Cottrol, C. (1995). Effect of
clinician–veteran racial pairing in the treatment of post-
traumatic stress disorder. American Journal of Psychiatry,
152, 555–563.
Rothbaum, B. O., Astin, M. C., & Marsteller, F. (2005). Pro-
longed exposure versus eye movement desensitization and
reprocessing (EMDR) for PTSD rape victims. Journal of
Traumatic Stress, 18, 607–616.
Rothbaum, B. O., & Foa, E. B. (1992). Exposure therapy for
rape victims with post-traumatic stress disorder. Behavior
Therapist, 15, 219–222.
Rothbaum, B. O., Hodges, L. F., Ready, D., Graap, K., &
Alarcon, R. (2001). Virtual reality exposure therapy for
Vietnam veterans with PTSD. Journal of Clinical Psy-
chiatry, 62, 617–622.
Saunders, B. E., Arata, C. M., & Kilpatrick, D. G. (1990). De-
velopment of a crime-related posttraumatic stress disorder
scale for women within the Symptom Checklist–90—Re-
vised. Journal of Traumatic Stress, 3, 439–448.
Schindler, F. E. (1980). Treatment by systematic desensitiza-
tion of a recurring nightmare of a real life trauma. Journal
of Behavior Therapy and Experimental Psychiatry, 11,
53–54.
Schnurr, P. P., Friedman, M. J., Engel, C. C., Foa, E. B., Shea,
T., Chow, B. K., et al. (2007). Cognitive-behavioral thera-
py for posttraumatic stress disorder in women: A random-
ized controlled trial. Journal of the American Medical As-
sociation, 297, 820–830.
Shalev, A. Y., Orr, S. P., & Pitman, R. K. (1992). Psycho-
physiologic response during script-driven imagery as an
outcome measure in posttraumatic stress disorder. Journal
of Clinical Psychiatry, 53, 324–326.
Shapiro, F. (1989). Eye movement desensitization: A new
treatment for post-traumatic stress disorder. Journal of
Behavior Therapy and Experimental Psychiatry, 20,
211–217.
Shapiro, F. (1995). Eye movement desensitization and repro-
cessing: Basic principles, protocols, and procedures. New
York: Guilford Press.
Shay, J., & Munroe, J. (1999). Group and milieu therapy for
veterans with complex posttraumatic stress disorder. In
P. A. Saigh & J. D. Bremner (Eds.), Posttraumatic stress
disorder: A comprehensive text (pp. 391–413). Needham
Heights, MA: Allyn & Bacon.
Silverman, D. (1977). First do no more harm: Female rape
victims and the male counselor. American Journal of Or-
thopsychiatry, 47, 91–96.
Street, A. E., Gradus, J. L., Vogt, D. S., Giasson, H. L., &
Resick, P. A. (2013). Gender differences among veter-
ans deployed in support of the wars in Afghanistan and
Iraq. Journal of General Internal Medicine, 28(Suppl. 2),
556–562.
Sutker, P. B., Uddo-Crane, M., & Allain, A. N. (1991). Clini-
cal and research assessment of posttraumatic stress disor-
der: A conceptual overview. Psychological Assessment, 3,
520–530.
Tarrier, N., Pilgrim, H., Sommerfield, C., Faragher, B., Reyn-
olds, M., Graham, E., et al. (1999). A randomized trial of
cognitive therapy and imaginal exposure in the treatment
of chronic posttraumatic stress disorder. Journal of Con-
sulting and Clinical Psychology, 67, 13–18.
Tarrier, N., & Sommerfield, C. (2004). Treatment of chronic
PTSD by cognitive therapy and exposure: 5-year follow-
up. Behavior Therapy, 35, 231–246.
Taylor, S., Kuch, K., Koch, W. J., Crockett, D. J., & Passey, G.
(1998). The structure of posttraumatic stress symptoms.
Journal of Abnormal Psychology, 107, 154–160.
Taylor, S., Thordarson, D. S., Maxfield, L., Fedoroff, I. C.,
Lovell, K., & Orgodniczuk, J. (2003). Comparative effi-
cacy, speed, and adverse effects of three PTSD treatments:
Exposure therapy, EMDR, and relaxation training. Jour-
nal of Consulting and Clinical Psychology, 71, 330–338.
Tolin, D. F., & Foa, E. B. (2006). Sex differences in trauma
and posttraumatic stress disorder: A quantitative review
of 25 years of research. Psychological Bulletin, 132, 959–
992.
U.S. Department of Health and Human Services. (2001).
Mental health: A report of the Surgeon General. Wash-
ington, DC: Author.
From Clinical Handbook of Psychological Disorders, Fourth Edition, Edited by David H. Barlow, PhD
Copyright 2014 by The Guilford Press. All rights reserved.
Copyright © 2014 The Guilford Press. All rights reserved under International Copyright Convention.
No part of this text may be reproduced, transmitted, downloaded, or stored in or introduced into
any information storage or retrieval system, in any form or by any means, whether electronic or
mechanical, now known or hereinafter invented, without the written permission of The Guilford Press.
Guilford Publications
370 Seventh Ave., Ste 1200
New York, NY 10001
212-431-
9800
800-365-
7006
www.guilford.com
Posttraumatic Stress Disorder
113
U.S. Departments of Veterans Affairs and Defense. (2010).
VA/DoD clinical practice guideline for the management
of PTSD. Washington, DC: Author.
van Etten, M. L., & Taylor, S. (1998). Comparative efficacy
of treatments for post-traumatic stress disorder: A meta-
analysis. Clinical Psychology and Psychotherapy, 5,
126–144.
Vogt, D., Smith, B., Elwy, R., Martin, J., Schultz, M., Drai-
noni, M.-L., et al.(2011). Predeployment, deployment, and
postdeployment risk factors for posttraumatic stress symp-
tomatology in female and male OEF/OIF veterans. Jour-
nal of Abnormal Psychology, 120, 819–831.
Vrana, S., & Lauterbach, D. (1994). Prevalence of traumatic
events and post-traumatic psychological symptoms in a
nonclinical sample of college students. Journal of Trau-
matic Stress, 7, 289–302.
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek,
D. G., Marx, B. P., & Keane, T. M. (2013). Clinician-
Administered PTSD Scale for DSM-5. Washington, DC:
U.S. Veterans Affairs National Center for Posttraumatic
Stress Disorder.
Weathers, F., Litz, B. T., Herman, D. S., Huska, J. A., &
Keane, T. M. (1993, October). The PTSD Checklist (PCL):
Reliability, validity, and diagnostic utility. Presentation at
the International Society for Traumatic Stress Studies, San
Antonio, TX.
Weathers, F. W., & Keane, T. M. (1999). Psychological as-
sessment of traumatized adults. In P. A. Saigh & J. D.
Bremner (Eds.), Posttraumatic stress disorder: A compre-
hensive text (pp. 219–247). Boston: Allyn & Bacon.
Weathers, F. W., Keane, T. M., & Davidson, J. R. (2001).
Clinician-Administered PTSD Scale: A review of the first
ten years of research. Depression and Anxiety, 13, 132–
156.
Weathers, F. W., Litz, B., Keane, K. M., Palmieri, P. A.
, Marx, B., & Schnurr, P. P. (2013). PTSD Checklist–5.
Washington, DC: U.S. Veterans Affairs National Center
for Posttraumatic Stress Disorder.
Weathers, F. W., Ruscio, A. M., & Keane, T. M. (1999).
Psychometric properties of nine scoring rules for the
Clinician-Administered Posttraumatic Stress Disorder
Scale. Psychological Assessment, 11, 124–133.
Weiss, D. S., & Marmar, C. R. (1997). The Impact of Event
Scale—Revised. In J. P. Wilson & T. M. Keane (Eds.), As-
sessing psychological trauma and PTSD (pp. 399–411).
New York: Guilford Press.
Wilson, A. E., Calhoun, K. S., & Bernat, J. A. (1999). Risk
recognition and trauma-related symptoms among sexually
revictimized women. Journal of Consulting and Clinical
Psychology, 67, 705–710.
Wilson, D., Silver, S. M., Covi, W., & Foster, S. (1996). Eye
movement desensitization and reprocessing: Effectiveness
and automatic correlates. Journal of Behavior Therapy
and Experimental Psychiatry, 27, 219–229.
Wolf, E. J., Lunney, C. A., Miller, M. W., Resick, P. A., Fried-
man, M. J., & Schnurr, P. P. (2012). The dissociative sub-
type of PTSD: A replication and extension. Depression
and Anxiety, 29, 679–688.
Zoellner, L. A., Feeny, N. C., Fitzgibbons, L. A., & Foa, E.
B. (1999). Response of African American and Caucasian
women to cognitive behavioral therapy for PTSD. Behav-
ior Therapy, 30, 581–595.
