
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
SAFETY & ENVIRONMENT OF CARE
COMPREHENSIVE Training for KP Staff Who Work in Hospitals
MEETS INITIAL TRAINING REQUIREMENTS IN THE FOLLOWING PROGRAM AREAS:
PLEASE NOTE:
MUCH OF THIS TRAINING REQUIRES ORIENTATION TO, AND ADDITIONAL TRAINING ON, DEPARTMENT-SPECIFIC AND FACILITY-
SPECIFIC POLICIES AND PROCEDURES. SEE THE BEGINNING OF EACH SECTION FOR ADDITIONAL INFORMATION.
PERSONAL SAFETY
Injury & Illness Prevention
Ergonomics
Security/Violence in the Workplace
Personal Protective Equipment
INFECTION PREVENTION & CONTROL
Aerosol Transmissible Disease/Tuberculosis
Bloodborne Pathogens
CHEMICAL SAFETY
Hazard Communication
Managing Hazardous Materials
WASTE MANAGEMENT
EMERGENCY RESPONSE
Fire Safety & Fire Extinguishers
Emergency Preparedness
ELECTRICAL & EQUIPMENT SAFETY
Lockout/Tagout (for Affected & Other Employees)
Medical Equipment
Utilities Safety
NOTIFICATIONS
Access to Medical Records
Ver. 2015-005
CALIFORNIA

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Welcome to Safety & Environment of Care Training!
INTRODUCTION
Facility-Specific Information
There will be times when the information in this training must be supplemented
with region-specific or facility-specific material.
There is a page following the test for this course with a link to this
supplemental information.
The last slide of this training contains a link to provide feedback on this module.
Please help us to improve this training by providing us with your feedback.
Finally, there is a quiz on this material at the end of the course – you must pass
the quiz to receive credit for the course.

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
PERSONAL SAFETY
Injury & Illness Prevention & Workplace Safety
Ergonomics
Security/Violence in the Workplace
Personal Protective Equipment
SECTION 1: PERSONAL SAFETY
This section provides information on how employees can prevent repetitive strain injuries and provides education and training needed to
comply with Cal/OSHA Standard 8 CCR § 5110
This section provides information on how KP employees can maintain a safe work environment for staff and provides education and
training on Illness and Injury Prevention needed to comply with Cal/OSHA Standard 8 CCR 3203 and Joint Commission Standards
EC.02.01.01, EC.03.01.01 and HR.01.04.01.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
IIPP – Workplace Safety, Hazard Reporting
Workplace Safety
The Workplace Safety program (WPS) is a Kaiser Permanente initiative to promote a safe work
environment with the ultimate goal of eliminating workplace injuries.
WPS seeks to create a culture of safety that encourages every employee to take proactive responsibility
for safety in their workplace.
Hazard Reporting
Employees at all levels should report any unsafe conditions or practices they observe. Hazards at your
worksite can be reported without fear of reprisal.
Unsafe conditions or practices can be reported to:
An immediate supervisor or to the EH&S or WPS Office
A member of the Integrated Safety Committee
The hotline established at your facility to report hazards anonymously/confidentially.
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training tells you how to report unsafe
conditions at YOUR facility.
INJURY & ILLNESS PREVENTION PROGRAM (IIPP)
EC.02.01.01, 8 CCR 3203

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Injury Reporting
If you are injured on the job you must report the injury immediately!
Specific procedures will vary by facility. However, as general rules…
Notify your supervisor right away - no later than the end of your shift! Call from home if you
discover a
problem after you
leave work.
Your supervisor will direct you to the appropriate department for treatment. For injuries that you
and/or your supervisor believe are 'emergent',
go to the Emergency Department.
Complete an injury report with your supervisor within 24 hours of the injury.
Assist your manager with evaluation of the root cause of the injury. Why did it happen? What were
the practices
or environmental factors which ma
y have caused or contributed to the injury?
If y
ou are injured…
Be prepared to provide ideas for preventing similar injuries. What can other employees learn that might
keep them safe? What can be done to reduce the injury risk?
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training provides additional
information on injury reporting at YOUR facility.
INJURY & ILLNESS PREVENTION PROGRAM (IIPP)
EC.02.01.01, 8 CCR 3203

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Strain Injuries
Strain accounts for the greatest number of employee injuries in a health care setting.
All strain injuries are preventable!
Causes of Upper Extremity Strain Injuries include:
Improper materials handling
Incorrect moving of cart by pulling it
Overloaded carts making them too heavy or unstable
Improper patient handling
Common causes of general pain when lifting, and ways to prevent strain include:
Incorrect Reaching: To get objects from a high shelf, use a sturdy stool or ladder. Keep your
shoulders, hips and feet facing the object avoid twisting to reach things to the side.
Incorrect Lifting: To properly lift an item such as a box, stand directly in front of the item and lift
with your legs. Don’t lift if you are bending or twisting at the waist.
Load Too Heavy: Before lifting, test the weight of the object by tipping one corner. If it’s too heavy
then get help or use a material handling device!
INJURY & ILLNESS PREVENTION PROGRAM (IIPP)
EC.02.01.01, 8 CCR 3203

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Workplace Safety - Back Care
Tips that will help you avoid back strain from lifting:
Perform squat lifts bending your knees, not your back.
If you can’t move an object easily with your foot, it’s
probably too heavy to lift by yourself.
Keep the object close to your body.
Don’t twist when lifting. Move your feet instead.
Lift objects only chest high.
Do not reach or stretch while attempting to lift an
object.
Whenever possible, use mechanical help such as a
hand-truck or cart.
Don’t pull heavy loads - push instead.
INJURY & ILLNESS PREVENTION PROGRAM (IIPP)
EC.02.01.01, 8 CCR 3203

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Workplace Safety - Slips, Trips and Falls
Other common preventable injuries include those caused by slips,
trips or falls.
Slips, Trips and Falls can be prevented by:
Taking personal responsibility for spills or tripping
hazards. Wipe up any non-hazardous liquid spilled on the
floor—don’t wait for EVS/housekeeping. Don’t store something
on the floor where it will create a trip hazard.
If you cannot eliminate the hazard from things like spilled
liquids, items on the floor and other objects, notify the
appropriate parties right away.
Many slips can be prevented by wearing the proper shoes or
shoe-covers. Wear enclosed shoes or shoe covers with slip-
resistant soles.
INJURY & ILLNESS PREVENTION PROGRAM (IIPP)
EC.02.01.01, 8 CCR 3203
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
The goal of the Ergonomics Program is to reduce work-related
Musculoskeletal Disorders (MSDs).
The following materials, tools, and training programs are
available from your supervisor, EH&S or WPS, to help you set up
your work area and address your own specific ergonomic issues:
The pamphlet “Ergonomics for the Computer User”
The KP Ergonomic Standard Guidance Document and
Toolbox
Self-assessment questionnaires and software tool
Standard Equipment Lists
Instructional Videos
Stretch cards
ErgoINFO Interactive Website
More information on the Ergonomics Program can be found on
the National WorkPlace Safety Ergonomics Page
The KP Ergonomics Program
ERGONOMICS
8 CCR § 5110
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Risk Factors and Symptoms
ERGONOMICS is the science of designing work
environments and technology to fit the employee
rather than requiring the employee to adapt to the
environment and technology.
Ergonomic Risk Factors include:
Repetition
Extended Duration
Excessive Force
Awkward Positions
Over Reaching
Poor Environment
Individual Factors
What happens when you, your task and the
environment don’t fit?
Musculoskeletal Disorders (MSDs) can occur!
Decreased range of motion in joints;
decreased strength in
extremity performance
Swelling of joints, extremities, digits
Numbness or tingling in extremities or digits
Pain!!!
8 CCR § 5110
ERGONOMICS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Computer Workstation Ergonomics and ergoINFO
ERGONOMICS
8 CCR § 5110
If you work at a computer most of the day -
At most workstations, correcting ergonomic problems is
simple and is something that you can do yourself. This link
has instructions on how to make ergonomic adjustments to
your workstation.
If you cannot adjust your workstation so that it is comfortable
for you, or if you are experiencing pain which you believe is
caused by incorrect ergonomics, it is important that you notify
your supervisor and find out how to request an ergonomic
evaluation at your facility.
ProWorkstation Safety Plus (WSP) and Manual Handling
Plus (MHP) are online e-learning tools designed to help
Kaiser Permanente employees effectively manage ergonomic
risk
WPS has developed the interactive ergoINFO tool
http://insidekp.kp.org/ergoinfo/

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
If you are injured at work:
Notify your supervisor right away (no later than the end of your shift)
Be prepared to provide ideas for preventing similar injuries.
Remind your supervisor to complete your injury report within 24 hours
All of the above are correct
B
A
C
D
Q&A: Injury Reporting
INJURY & ILLNESS PREVENTION PROGRAM (IIPM)
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
If you are injured at work :
Notify your supervisor right away (no later than the end of your shift)
Be prepared to provide ideas for preventing similar injuries.
Remind your supervisor to complete your injury report within 24 hours
All of the above are correct
Q&A: Injury Reporting
The correct answer is D.
B
A
C
D
INJURY & ILLNESS PREVENTION PROGRAM (IIPM)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Security
As employees, there are many things we can do to help maintain a high level of security for ourselves and
our patients and members.
Basic Security Tips for Personal Safety…
Be alert at all times
Use common sense
Follow designated practices and procedures
Report any suspicious behavior to authorities
Call Security or authorities according to your facility's policy, if you need assistance
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training has information on contacting
Security at your facility.
Introduction
SECURITY/VIOLENCE IN THE WORKPLACE
EC.02.01.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Your Responsibilities
There are things you can do as a Kaiser Permanente employee to increase security:
Kaiser Employee Identification Badges must be worn at all times while at work.
They
should be worn above the waist, on the outermost garment, and clearly visible
.
This helps identify
staff.
Protect personal property. Don’t keep personal items in public areas. Do not bring valuables to work or
leave them at your workstation. Lock personal items in
your vehicle’s trunk, or alternatively, a
desk,
locker
or file cabinet when you leave your immediate work area.
Do not share your computer password, keys or access badges with another employee. This may lead
to disciplinary action
or termination.
SECURITY/VIOLENCE IN THE WORKPLACE
EC.02.01.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Kaiser Permanente’s Zero Tolerance Policy of Threatening Behavior
Kaiser Permanente has a policy of zero tolerance with regard to violent or threatening behavior.
This applies to all Kaiser Permanente employees, visitors and members!
Threats, harassment, intimidation, assault, battery and disturbances are all examples of behavior that is
unacceptable.
All Kaiser Permanente employees have a duty to report all incidents of violent behavior.
Threatening behavior should be immediately reported to Security Services along with a request for
assistance regardless of the threat source.
Watch for verbal signs to identify threats of violence:
Angry or threatening tone of voice
Shouting, screaming, cursing
Making threats or sexual comments
Challenging rules or authority
Making unreasonable demands
Expressing irrational thinking
Talking about weapons
SECURITY/VIOLENCE IN THE WORKPLACE
EC.02.01.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Wearing Your ID Badge
An identification Badge can hang from an employee’s belt so long as it is worn at all
times while at work and clearly visible.
True
False
A
B
SECURITY/VIOLENCE IN THE WORKPLACE

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
An identification Badge can hang from an employee’s belt so long as it is worn at all
times while at work and clearly visible.
True
False
*Remember - if your badge is hanging from your belt, it is below your waist!
A
B
The correct answer is B*.
Q&A: Wearing Your ID Badge
SECURITY/VIOLENCE IN THE WORKPLACE
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Personal Protective Equipment - Introduction: Types of PPE
Different PPE is used to protect different parts of the body, including the eyes, face, head, feet, hands,
arms and lungs.
Examples of PPE commonly used by health care workers include Gloves (Nitrile or Non-Latex/Latex
Exam) and Protective Clothing (Moisture Resistant Gowns)
Other examples of uses for PPE and the type of equipment used are:
Respiratory Protection:
N95 particulate respirators
PAPR (Powered Air Purifying Respirator)
Eye Protection:
Safety Glasses w/Side Shields
Goggles
Faceshield
Shaded Laser Glasses
PERSONAL PROTECTIVE EQUIPMENT (PPE)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
When is PPE Necessary?
PPE is necessary when hazards (like exposure to infectious materials or harmful chemicals) cannot be
eliminated through engineering or administrative controls. You select PPE based on the type of exposure
you expect to encounter.
Hazards in a health care setting that would require PPE are:
Biohazards (potentially infectious body fluids)
Penetration hazards (sharp objects, broken glass)
Chemical hazards – through exposure to skin or vapors
Non-ionizing radiation (lasers )
Noise hazards (lawn mowers, generators)
Other factors to consider when selecting appropriate PPE include:
Durability and appropriateness for the task: PPE is only effective if it stops infectious
material, chemicals or other hazards from penetrating for the entire time it is used.
Fit: PPE that fits poorly won’t provide much protection. In some cases (like N95-type
respirators) you must be fit tested prior to use in order to ensure protection
1910.132(f)(1)(i)
PERSONAL PROTECTIVE EQUIPMENT (PPE)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
What PPE is necessary?
You can access a list of commonly performed procedures and the PPE required by clicking here:
REF DOC: PPE Matrix.
1910.132(f)(1)(ii)
PERSONAL PROTECTIVE EQUIPMENT (PPE)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
The limitations of the PPE
All PPE has limitations - for example, gloves may develop small holes. Even appropriate PPE does not
provide a foolproof guarantee of safety.
Always use the right PPE for the job. OSHA requires that chemicals’ Safety Data Sheets (SDS) list
information about the appropriate PPE for the use with the product. Refer to the SDS if you have
questions about the appropriate PPE for handling a chemical.
Make sure you know where your PPE is! (It can’t help you if you can’t find it when you need it, right?)
PPE has limitations…
Make sure the size is right.
N95-type respirators require fit testing and even when fit tested and appropriately used,
N95
masks will only provide protection against particulates. They provide no
protection
from chemical vapors.
In those situations a different kind of respirator is required.
1910.132(f)(1)(iv)
PERSONAL PROTECTIVE EQUIPMENT (PPE)
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Maintenance, useful life and disposal
PPE should be disposed of when damaged or soiled.
Employees must inspect all PPE prior to use for evidence of damage, missing or defective parts,
correctness of size/fit, and any other condition which could affect its use. Any PPE with worn or defective
parts must be repaired or replaced prior to use.
PPE which isn’t discarded after single use should be cleaned and/or disinfected, depending on the
condition, use and type of the PPE.
Clean PPE must be stored in a location and in a way which will keep it clean between uses.
Goggles, non-disposable gloves, hard-hats, and other PPE shouldn’t be exchanged among employees for
use unless they’ve been cleaned and sanitized.
1910.132(f)(1)(v)
PERSONAL PROTECTIVE EQUIPMENT (PPE)

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
INFECTION PREVENTION & CONTROL
Aerosol Transmissible Disease
Bloodborne Pathogens
This section is for CALIFORNIA.
SECTION 2: INFECTION PREVENTION & CONTROL
When completed in conjunction with orientation to job specific and site specific policies and procedures this section meets the training
requirements with regard to bloodborne pathogens as described in Federal standard 29 CFR 1910.1030 and California 8 CCR §5193.
When combined with orientation to facility-specific information on the ATD Exposure Control Plan, Respiratory Protection training, PAPR
usage instruction and the Facility Surge Plan, completion of this section complies with the training requirements of California Aerosol
Transmissible Diseases Standard 8 CCR §5199.
This section is for Kaiser Permanente staff who work in Northern California or Southern California.
Are you in the wrong state?
Use the button below to jump to material for Hawaii region:

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Before getting started… Questions?
Aerosol Transmissible Diseases
The law requires that you have an opportunity for interactive questions and answers during this training.
If you reach a point in this training when you do have a question, STOP and contact your local
Infection Prevention-Control or Employee Health department.
If you do not know how to contact them, click here:
Environmental, Health & Safety, Infection Prevention-Control, Employee Health Contacts.
If you close this course and return to it at a later time, you will have the option to start again where you left
off.
In addition, Cal/OSHA’s ATD Standard requires that our records include a summary of the training content and the names and qualifications of
the trainers. KP’s ATD training was created by National EH&S and content was developed by our national Subject Matter Expert (SME) for
Aerosol Transmissible Diseases. Onsite support is provided by your local EH&S and Infection Control departments.
The Training Addendum at the link below provides a summary of elements included in this course and the qualifications of our national SME.
http://kpnet.kp.org/ehs/training/ed_Aerosol_Transmissible_Disease_Training_Addendum.pdf
8 CCR §5199 (i)(5)
By clicking the Forward button below, I understand that I have the right to get answers to
questions about this material; and because this training is delivered online, that means
contacting my Infection Prevention-Control and/or Employee Health Department.
AEROSOL TRANSMISSIBLE DISEASES (ATD)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Introduction – ATD Standard
The California Occupational Health and Safety Division (Cal/OSHA) adopted the Aerosol Transmissible
Diseases Standard in August 2009.
Some of the things the ATD Standard requires hospitals to do is:
Develop plans and procedures to protect employees and visitors from ATDs.
Provide employees with appropriate personal protective equipment (including respirators).
Provide any employee who does get an ATD with medical care.
Make sure employees receive initial and annual ATD training - like this!
And a lot more…
You can get more detailed information by reading through the ATD standard using the link below.
Click here to access a copy of the Cal/OSHA ATD standard, 8 CCR 5199.
8 CCR §5199 (i)(4)(A)
AEROSOL TRANSMISSIBLE DISEASES (ATD)
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is an ATD?
An Aerosol Transmissible Disease (or ATD) is a disease or pathogen that requires droplet or airborne
precautions to prevent exposure.
“Droplets” are relatively large in size and can result from coughing, sneezing or talking.
“Airborne” refers to relatively small particles, which can remain suspended in the air and can
travel great distances.
The infectious organisms that cause ATDs
can be spread by either of these!
Signs and Symptoms of ATDs that require further medical evaluation include:
Fever with rash
Fever with cough
Headache or neck stiffness or sensitivity to light
8 CCR §5199 (i)(4)(B)
© Kaiser Foundation Health Plan, Inc.
AEROSOL TRANSMISSIBLE DISEASES (ATD)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Modes of transmission and source control procedures
Modes of Transmission:
Droplet ATDs are spread by large respiratory droplets that generally do not travel very far.
Examples: Diphtheria, Mumps, Pertussis, Rubella, N. meningitidis
Airborne ATDs are spread by very small infectious particles that can stay suspended in air and may
travel long distances carried by air currents.
Examples: Chicken Pox, Measles, Tuberculosis, novel or unknown pathogens (treated as
airborne until they are further characterized)
Source Control Procedures:
Educate visitors and patients to cover nose and mouth with a tissue when they cough or sneeze,
using posters and/or direct communication.
Provide respiratory “etiquette stations” at facility entrances and public waiting areas, stocked with
hand sanitizer and tissue and/or surgical masks.
8 CCR §5199 (i)(4)(C)
© Kaiser Foundation Health Plan, Inc.
AEROSOL TRANSMISSIBLE DISEASES (ATD)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
ATD Exposure Control Plan
Your facility’s ATD Exposure Control Plan:
Describes specific methods the facility uses to control exposures
Identifies job classifications at risk of exposure
Describes procedures to be followed in the event of an exposure including medical follow up and
incident investigation
Describes procedures for training and recordkeeping
A link to your facility’s ATD Exposure Control Plan can be found in your facility-specific training (link at
the end of this module). Or you can contact the Department Manager or Environmental, Health &
Safety, Infection Prevention and/or Employee Health.
Employees are invited to provide input as to the Plan’s effectiveness - use the link above to determine
the appropriate contacts at your medical center.
8 CCR §5199 (i)(4)(D)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Activities that may expose you to an ATD
8 CCR §5199 (i)(4)(E)
© Kaiser Foundation Health Plan, Inc.
AEROSOL TRANSMISSIBLE DISEASES
Exposure to an ATD may occur when:
You are in the same room or within 6 feet (in
open space) of a suspected or confirmed ATD
patient or handling patient materials that may
be contaminated with infectious particles.
You are performing or present during a task
that may generate aerosolized ATD pathogens,
including tasks performed on specimens in a
lab or at autopsy.
You enter the room of a patient on Airborne
Isolation Precautions within an hour after the
patient has left the room.
For more information, see the NEH&S matrix of
tasks and procedures involving ATD exposure:
ATD Matrix

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Methods to prevent exposure – Hierarchy of Controls
The next slides contain
more information on PPE
8 CCR §5199 (i)(4)(F)
AEROSOL TRANSMISSIBLE DISEASES
Click here for more information
on Work Practice Controls
Click here for more information
on Engineering Controls
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Personal Protective Equipment (PPE)
Use: Protects wearer from exposure to ATD pathogens.
Limitations: PPE is only effective if appropriately selected, correctly and consistently worn, and
properly cleaned, stored or discarded. Contaminated PPE may be a source of infection.
Basis for selection: PPE creates physical barrier protection from exposure to ATD pathogens,
including facial protection for droplets and respiratory protection for airborne particles. Examples of types
of PPE:
Gloves
Gown or apron (impermeable)
Surgical mask for ATDs requiring Droplet Precautions
Respirator (N95 or PAPR) for ATDs requiring Airborne Precautions
Your facility’s ATD Exposure Control Plan includes a “Matrix of Tasks and Procedures Involving
Occupational Exposure and Exposure Controls”, which show the work practices and PPE required for
each task that has potential for exposure to an ATD or bloodborne pathogen.
Your department manager is responsible for maintaining an adequate supply of respirators and other
protective gear to prevent employee exposure and for informing you of the proper use, location, removal,
handling, cleaning, decontamination and disposal of PPE used at your worksite.
8 CCR §5199 (i)(4)(G)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Decontamination and disposal of PPE
Remove any PPE before leaving the patient
room/work area or when the PPE becomes
contaminated or torn and place it in appropriate
containers for storage, washing, decontamination
or disposal.
The exception is your respirator, which must be
removed after leaving the patient room.
Consider the front of the respirator and facemask
contaminated after use. Dispose of your N95 in
regular trash after use.
Decontaminate and store PAPRs according to
your facility and/or departmental procedures.
Always wash your hands after the removal of PPE!
8 CCR §5199 (i)(4)(F),(G)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Methods to prevent exposure – Respiratory Protection
N95: Use an N95 or equivalent respirator with a known or suspected TB or other Airborne ATD
patient when entering room of a patient on Airborne Isolation Precautions, or within an hour of when
the room was occupied by patient.
Note: In order to correctly choose and wear an N-95 respirator, you must be fit tested for that type of
respirator.
Powered Air Purifying Respirator (PAPR) means an air-purifying respirator that uses a blower to
force the ambient air through air-purifying filter to remove airborne contaminants and deliver filtered air
to the user.
Employees who participate in high hazard procedures on patients suspected or confirmed to have an
Airborne Infectious Disease must wear a PAPR or equivalent protection during the procedure,
including when the procedure is performed in a negative pressure isolation room.
High hazard procedures are aerosol-generating procedures performed on an individual who has a
suspected or confirmed ATD, including: sputum induction, bronchoscopy, intubation, aerosolized
administration of Pentamidine or other medications, and autopsy, clinical, surgical and laboratory
procedures that may generate aerosols.
8 CCR §5199 (i)(4)(F),(G)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
TB surveillance
Employee Health Services is responsible for
performing TB surveillance:
All health care workers are screened
initially upon hire and annually thereafter.
Medical follow-up is provided for TB
conversions.
Screenings are conducted every three
months if two or more conversions
occur in one department or group.
Note that immune-compromised
individuals can have a false negative TB
test result.
8 CCR §5199 (i)(4)(H)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Respiratory Protection Training
If you are assigned to wear an N95 or PAPR respirator for protection from exposure to ATDs, you
must complete initial and annual respiratory protection training.
For information regarding your facility’s method for providing this training, talk to your Supervisor or
contact Environmental, Health & Safety, Infection Prevention or Employee Health.
8 CCR §5199 (i)(4)(I)
Example of an N95 Particulate Respirator
3M 1860
Example of Powered Air Purifying Respirator
3M Air-Mate™ PAPR
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Vaccines for ATDs
Employee Health Services is responsible for administering vaccinations:
Vaccines are a safe and an effective means of preventing some ATD transmission
Vaccinations are available at no cost to employees
If you don’t have your vaccination records, a simple blood test will determine if you have immunity
The following links will give you more information* on specific vaccines:
Click for information about the Tetanus, Diphtheria (Td) with Pertussis (Tdap) vaccine
Click for information about the Varicella (Var) vaccine
Click for information about the Influenza, trivalent inactivated (TIV) vaccine
Click for information about the Influenza, live, attenuated (LAIV) vaccine
Click for information about the Measles, mumps, rubella (MMR) vaccine
* From the VIS (Vaccine Information Statements) web site: http://www.immunize.org/vis/
8 CCR §5199 (i)(4)(J)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
ATD Exposure Incident: Reporting and medical follow-up
Reporting an ATD Exposure Incident:
ALL exposure incidents must be reported to your manager immediately.
Proceed to Employee Health as soon as possible for appropriate evaluation and medical follow-up.
Post-Exposure Evaluation:
A Post-Exposure Evaluation is performed to determine the nature and extent of exposure, including
circumstances of event, source patient information and other details. It may also involve testing of
exposed employee or physician.
Medical follow-up may involve:
Testing
Preventive therapy: medications or vaccinations
Other procedures if indicated (for example, a chest x-ray)
8 CCR §5199 (i)(4)(K)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Facility Surge Plan
Epidemics or other events may create a surge situation. For this training to be compliant, you must
know your facility’s procedures under these circumstances, including the plan for:
1. Surge receiving and treatment of patients
2. Patient isolation procedures
3. Surge procedures for handling of specimens, including specimens from persons who may have
been contaminated as a result of a release of a biological agent
4. How to access supplies needed for the response including PPE and respirators
5. Decontamination facilities and procedures
6. How to coordinate with emergency response personnel from other agencies
These procedures will be covered during your facility’s disaster drills, which will include a surge scenario at
least annually.
To access YOUR facility’s Emergency Operations Plan and find specific information regarding the items
listed above, talk to your Department Manager or contact Environmental, Health & Safety, Infection
Prevention and/or Employee Health.
8 CCR §5199 (i)(4)(L)
AEROSOL TRANSMISSIBLE DISEASES
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
An Aerosol Transmissible Disease (or ATD) is a disease or pathogen that requires droplet or
airborne precautions to prevent exposure, and your facility’s ATD Exposure Control Plan
describes procedures to be followed in the event of an exposure.
True
False
A
B
Q&A: What is an ATD? What does the Exposure Control Plan do?
AEROSOL TRANSMISSIBLE DISEASES (ATD)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
An Aerosol Transmissible Disease (or ATD) is a disease or pathogen that requires droplet or
airborne precautions to prevent exposure, and your facility’s ATD Exposure Control Plan
describes procedures to be followed in the event of an exposure.
True
False
A
B
The correct answer is A.
Q&A: What is an ATD? What does the Exposure Control Plan do?
AEROSOL TRANSMISSIBLE DISEASES (ATD)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Before getting started… Questions?
The law requires that you have an opportunity for interactive questions and answers about this
material. If you reach a point in this training when you do have a question, STOP and contact your
local Infection Control or Employee Health department.
If you do not know how to contact them, you can find contact numbers by clicking SafetyNet -
Environmental, Health & Safety, Infection Prevention-Control, Employee Health Contacts.
(If you close this course and return to it at a later time, you will have the option to start again where
you left off.)
In addition, OSHA’s BBP Standard requires that our records include a summary of the training content and the
names and qualifications of the trainers. KP’s BBP training was created by National EH&S and content was
developed by our national Subject Matter Expert (SME) for Bloodborne Pathogens. Onsite support is provided by
your local EH&S and Infection Control departments.
The Training Addendum at the link below provides a summary of elements included in this course and the
qualifications of our national SME.
http://kpnet.kp.org/ehs/training/ed_Bloodborne_Pathogens_Awareness_Training_Addendum.pdf
Questions?
By clicking the Forward button below, I understand that I have the right to get answers to
questions about this material; and because this training is delivered online, that means
contacting my Infection Control and/or Employee Health Department.
BLOODBORNE PATHOGENS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
OSHA’s Bloodborne Pathogens Standard
The Bloodborne Pathogen (BBP) Standard aims to minimize your exposure to bloodborne pathogens.
Employers must select and implement appropriate engineering controls to prevent employee exposure to
BBPs. The standard requires that those at risk of BBP exposure be included in the process of evaluation
and selection of these devices.
A hands-on demonstration in the use of the approved safety devices used in your work area is required.
Employees are required to use safe devices that are provided by the employer
Talk to your Department Manager for more information on specific procedures performed or
devices approved for use in your department.
For your reference, a copy of the Federal (national) standard can be accessed by clicking 29 CFR 1910.1030
The California standard can be accessed here: California Standard
BLOODBORNE PATHOGENS
1910.1030(g)(2)(vii)(A)
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Epidemiology and Symptoms of BBPs
BBPs may include HIV, Hepatitis B (HBV), Hepatitis C (HCV) or other pathogens:
Infection by HIV causes the progressive loss of immune system function. Acquired
Immunodeficiency Syndrome (AIDS) can result from HIV infection and is characterized by
opportunistic infections, cancers, neurologic disorders and other syndromes.
The time from infection by HIV to clinical diagnosis can be as long as 14 years.
Hepatitis is an inflammation of the liver caused by a virus. Hepatitis B and C are the more serious viral
forms and are spread through contact with human blood and perhaps through contact with other body
fluids. They can result in chronic, debilitating and potentially fatal liver disease. You can have Hepatitis B
or C for many years before you even know you have the virus. However, by then your liver may already be
damaged. You can be infectious weeks before the onset of symptoms, and you will stay infectious while
you are sick. Many people remain infectious indefinitely.
1910.1030(g)(2)(vii)(B)
BLOODBORNE PATHOGENS
Symptoms of infection from Hepatitis B and C include, but are not limited to:
Loss of appetite Abdominal discomfort
Nausea and vomiting Joint pain and rash
Jaundice (yellowing of the skin and eyes) Flu-like symptoms
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
BBP Modes of Transmission
The modes of BBP transmission to
healthcare workers are:
1. Needlesticks/punctures
2. Splashes to the eyes or
mucous membranes
3. Cuts or contact with non-
intact skin (percutaneous)
1910.1030(g)(2)(vii)(C)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
The BBP Exposure Control Plan
1910.1030(g)(2)(vii)(D)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.
Each Kaiser facility maintains a
Bloodborne Pathogen Exposure Control Plan.
Your Facility’s plan…
Describes Kaiser’s role in protecting
employees and your obligation to use
protective measures.
Identifies the procedures that put employees
at risk and the protective measures to be
taken.
Describes the procedure for reporting BBP
Exposure and Post-Exposure Prophylaxis.
There will be a link to a copy of your facility’s BBP
Exposure Control Plan in your facility-specific training.
Or a copy can be obtained from Environmental Health &
Safety, Infection Prevention or Employee Health Services
(click here to locate).

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Activities That May Involve BBP Exposure
Examples of tasks that could involve exposure to
Bloodborne Pathogens or Other Potentially
Infectious Materials (OPIM) include any assigned
duties during which skin, eye, mucous membrane, or
parenteral contact with blood or OPIM can be
reasonably anticipated.
Including:
Blood drawing
Suctioning
Cleaning up blood or body fluid spill
Click here for a list of commonly performed
procedures that may lead to exposure to BBPs.
1910.1030(g)(2)(vii)(E)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Prevention of BBP Exposure
In order to prevent and reduce exposure to Bloodborne Pathogens, employees must:
Handle blood/body fluids of all patients as potentially infectious.
Decontaminate hands between all patient contact, after specimen contact and after removal
of gloves.
Use safe needle devices for injection, IV starts, blood draws, and use the needleless IV
tubing systems. Use of safe needle devices is required by OSHA with only a few exceptions.
A limitation of safe needle devices is that the majority of devices have safety features that
must be actively engaged by the employee in order to be effective.
Employees are required to use safe devices that are provided by the employer!
Place used sharps in sharps container immediately after use. Do not recap or manipulate
needles.
In addition…
Handle all laboratory specimens as potentially infectious
Hepatitis B vaccine must be offered to all employees at risk for blood or body fluid contact,
and is strongly recommended for all employees. A declination form (available from Employee
Health Services) must be signed if you choose to refuse the vaccine.
Do not eat, drink, apply cosmetics or lip balm, or handle contact lenses in patient care areas
or laboratory processing areas.
Protect your non-intact skin (i.e. chapped or abraded skin) from contact with blood or body
fluids.
1910.1030(g)(2)(vii)(F)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Personal Protective Equipment (PPE)
PPE protects the skin, eyes, mouth or other mucous membranes during normal use and during the entire length of
time the PPE is worn.
Examples of PPE are:
Gloves
Gowns and/or disposable plastic aprons
Masks
Face shields
Protective eyewear
Click here for a list of commonly performed procedures and the PPE required.
Or http://kpnet.kp.org/ehs/training/deeplinks/redirects/kpl_bbp_ppe_matrix.htm
Also note:
Disposable gloves cannot be washed or decontaminated for reuse.
Employees must remove any PPE when it becomes torn or damaged, before leaving the work area, or
when the PPE becomes contaminated, and place it in appropriate containers for decontamination or
disposal. Disposable PPE, when dripping or caked with blood or other infectious material, should be
discarded in a biohazard container (or in a chemo container if the PPE is contaminated by
chemotherapeutic agents).
All PPE has limitations—gloves may develop small holes. Even appropriate PPE does not provide a foolproof
guarantee of safety. Your department manager is responsible for maintaining an adequate supply of
protective gear to prevent employee exposure and for informing you of the proper use, location, removal,
handling, cleaning, decontamination and disposal of PPE used at your worksite.
1910.1030(g)(2)(vii)(G)
BLOODBORNE PATHOGENS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Explanation for Selection of PPE
Your supervisor will need to review your job responsibilities for
areas that may involve exposure to bloodborne pathogens.
Selection of Personal Protective Equipment (PPE) is based on
the type and degree of risk associated with the task being
performed. Your facility EH&S and/or Infection Prevention-
Control Departments can help with selection and evaluation of
PPE.
Any concerns about PPE (what type to use, proper training,
etc.) should be discussed with your supervisor or contact your
EH&S Department for more information.
1910.1030(g)(2)(vii)(H)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Hepatitis B Vaccine
KP offers hepatitis B vaccine to all employees. The vaccine can be obtained free of charge from
Employee Health Services. The benefit of being vaccinated against hepatitis B is that it will prevent
infection and liver disease associated with exposure to the hepatitis B virus.
The vaccine:
is highly effective and safe
is recommended for all employees
does not expose the recipient to bloodborne pathogen diseases
is given in three injections in the arm at day 0, 1 month and 6 months
Adverse reactions to the hepatitis B vaccine are rare but include:
injection site reactions, including redness, soreness, swelling
fatigue/weakness
headache
malaise
irritability
This link will give you more information on the vaccine: http://www.immunize.org/vis/hepatitis_b.pdf
If you decide not to receive the immunization, you must sign a declination form. You may decide later to be
immunized.
1910.1030(g)(2)(vii)(I)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Actions to take in an Emergency
Skin (intact or non-intact) should be washed IMMEDIATELY
with soap and water.
Exposed mucous membranes should be flushed with
water only.
In CALIFORNIA Regions: Notify your department manager and
go to Employee Health or the Emergency Department
IMMEDIATELY (within the first 2 hours of exposure).
In HAWAII Region: notify your department manager (or person
in charge) IMMEDIATELY, then go to Workplace Incident
Reporting on the Kaiser Home Page and follow the
instructions.
Employees who have had an exposure are offered a medical
evaluation immediately with appropriate follow-up. The most
obvious exposure incident is a needlestick. However, when
blood or other infectious material come in contact with your
eyes, nose, mouth, other mucous membrane, or non-intact
skin, this is also considered an exposure incident and should
be reported to your department manager immediately.
1910.1030(g)(2)(vii)(J)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Post-Exposure Procedure
In the event you are exposed to any blood or other infectious materials, it is CRUCIAL that you report
any exposure incident to your department manager within the first 2 hours of exposure to facilitate
immediate intervention that can deter the development of HBV, HIV other potential infections.
Information which will be needed to report BBP exposure includes…
The name and medical record number of the source patient (if known)
The type and level of exposure
What protective equipment or clothing you were wearing at the time of exposure
Information on the device involved (including: name, brand, manufacturer, volume, gauge and length)
Whether or not a safety feature was utilized
Employees who have had an exposure are offered an immediate medical evaluation with appropriate
follow-up. The most obvious exposure incident is a needlestick. However, when blood or OPIM come in
contact with your eyes, nose, mouth, other mucous membrane, or non-intact skin, this is also considered
an exposure incident and should be reported to your supervisor immediately.
Employee Health Services enters information provided by the employee regarding the exposure incident
into the National BBP Exposure Incident database. The Sharps Injury Log for each facility is generated
from this database.
1910.1030(g)(2)(vii)(K)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Post-Exposure Medical Evaluation
During the post-exposure medical evaluation, you will be
provided with…
Counseling
Appropriate lab work and treatment in line with
current US Public Health Service recommendations
and regional policies and procedures
Evaluation of any reported illness in the future to
determine if the symptoms may be related to HIV or
HBV development
Chemoprophylaxis (drug therapy) is recommended
after a high risk exposure.
The recommended post exposure testing interval
for HIV is at the time of exposure (baseline), 6
weeks, 12 weeks and 6 months.
1910.1030(g)(2)(vii)(L)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Biohazard Labeling
Biohazard warning labels must be affixed to
containers of biohazardous materials. Labels
must include the universal biohazard symbol and
the legend "BIOHAZARD" or in the case of
sharps containers and regulated waste
"BIOHAZARDOUS WASTE" or "SHARPS
WASTE.“
Labels are fluorescent orange or orange-red, with
lettering and symbols in a contrasting color.
1910.1030(g)(2)(vii)(M)
BLOODBORNE PATHOGENS
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Exposure to Blood or OPIM
In order to prevent and reduce exposure to Bloodborne Pathogens, employees must:
Handle blood/body fluids of all patients as potentially infectious
Decontaminate hands between all patient contact, after specimen contact and after
removal of gloves
Place used sharps in sharps container immediately after use. Do not recap or
manipulate needles
All of the above are correct
A
B
C
D
BLOODBORNE PATHOGENS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
In order to prevent and reduce exposure to Bloodborne Pathogens, employees must:
Handle blood/body fluids of all patients as potentially infectious
Decontaminate hands between all patient contact, after specimen contact and after
removal of gloves
Place used sharps in sharps container immediately after use. Do not recap or
manipulate needles
All of the above are correct
© Kaiser Foundation Health Plan, Inc.
The correct answer is D.
A
B
C
D
Q&A: Exposure to Blood or OPIM
BLOODBORNE PATHOGENS

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
CHEMICAL SAFETY
Hazard Communication
Managing Hazardous Materials
SECTION 3: CHEMICAL SAFETY
When completed in conjunction with on-site departmental and job-specific orientation to the Hazardous Materials in use in the work area,
this training meets the requirements of Federal Hazard Communication Standard 29 CFR 1910.1200 and California 8 CCR §5194.
This section provides information on how employees can create a safe and secure working environment for staff and members and
provides education and training needed to comply with Joint Commission Standard EC.02.02.01

HOSPITAL – COMPREHENSIVE/INITIAL
Information
HAZARD COMMUNICATION
The Federal Hazard Communication Standard requires a hazard communication program for the workplace, and
this program should cover:
Identification of chemicals in the work area (chemical inventory)
Labeling of hazardous chemicals to provide hazard warnings
Safety Data Sheets (SDS) for all hazardous chemicals to be readily accessible
Training to be provided to all staff coming in contact with hazardous chemicals.
You will need to know……
All of the operations in your work where hazardous chemicals are present
How to access facility chemical inventories
How to access the Safety Data Sheets (SDS) for these chemicals
How to access a copy of your facility’s Hazard Communication Program.
If you do not currently know the above information, you MUST get this information from your department
manager/supervisor and/or your EH&S department.
Or, wait until the FACILITY-SPECIFIC SUPPLEMENT page at the end of this training for information on
how to access hazardous chemical information for YOUR facility.
1910.1200(h)(2)
© Kaiser Foundation Health Plan, Inc.
By clicking the Forward button below, I agree to learn where hazardous chemicals are present in
my work area; how to access my Hazard Communication Plan; the chemical inventory for my
work area; and how to access Safety Data Sheets.

HOSPITAL – COMPREHENSIVE/INITIAL
1910.1200(h)(3)(ii)
The types of hazardous chemicals you will work with depends on the operations in your work area.
Click on the link below and select your department, you will find examples of chemicals typically found in
different departments and the associated hazards, such as physical, health, simple asphyxiation, and
combustible dust hazards, as well as hazards not otherwise classified.
CLICK HERE!
You will require orientation on the specific processes and procedures for safe handling and use of
chemicals at your worksite (Department Specific Training by your supervisor and/or EH&S Department is
required), as well as information on the location and the hazards associated with chemicals in the work
area. If a new chemical hazard is introduced, you will need training on that chemical and its specific
hazards.
Chemical Hazards In the Work Area
HAZARD COMMUNICATION
© Kaiser Foundation Health Plan, Inc.

HOSPITAL – COMPREHENSIVE/INITIAL
Labeling Systems: Primary and Secondary Labels
Primary Labels are those which are affixed to the product’s original container
and provided by the manufacturer/distributors, which must include:
Product identifier;
Signal word, either “danger" or "warning";
Hazard statement(s);
Pictogram(s), presented on the next slide;
Precautionary statement(s); and,
Name, address, and telephone number of the chemical manufacturer,
importer, or other responsible party.
You may find in your workplace some primary labels with an older format, which do not have the
pictograms or signal words. These older primary labels provide very similar hazard information. If there
are currently such labels, they will be replaced by the newer primary labels before mid year 2016
When hazardous chemicals are transferred from a primary container into a
secondary container, the secondary container must be labeled with the
following:
Product identifier
General hazard information by words, pictures and/or symbols
The original manufacturer’s label and SDS are used as sources of information.
1910.1200(f), (h)(3)(iv)
HAZARD COMMUNICATION
© Kaiser Foundation Health Plan, Inc.
Examples of secondary labels

HOSPITAL – COMPREHENSIVE/INITIAL
HAZARD COMMUNICATION
1910.1200(f); (h)(3)(iv)
Pictograms and Hazards
© Kaiser Foundation Health Plan, Inc.

HOSPITAL – COMPREHENSIVE/INITIAL
Safety Data Sheets (SDS)
Safety Data Sheets, or SDSs, are important components of a hazard communication program.
Standardized SDS will include the following required sections:
Section 1, Identification
Section 2, Hazards(s) identification
Section 3, Composition/information on ingredients
Section 4, First-aid measures
Section 5, Fire-fighting measures
Section 6, Accidental release measures
Section 7, Handling and storage
Section 8, Exposure controls/personal protection
Section 9, Physical and chemical properties
Section 10, Stability and reactivity
Section 11, Toxicological information
Section 16, Other information
SDSs can be available electronically or as hard copies. If you are not sure how to access an SDS, contact
your supervisor or your facility EH&S Department.
You may find an older format of an SDS, called an MSDS, in your workplace. These MSDSs provide similar information. If there is an MSDS, it will be
replaced by the SDS before mid year 2016.
1910.1200(g), (h)(3)(iv)
HAZARD COMMUNICATION
© Kaiser Foundation Health Plan, Inc.

HOSPITAL – COMPREHENSIVE/INITIAL
Methods of Detecting a Chemical Presence or Release
You may learn about the presence of a hazardous chemical by
Air sampling reports, for example, Kaiser Permanente's National Environmental, Health &
Safety department will conduct periodic monitoring for formaldehyde.
Continuous monitoring devices, such as those installed for EtO when needed
It is important that you stay alert to the signs of a chemical spill or release, by such signs:
Is there an unusual or unusually strong smell?
Is there a pool of an unidentifiable substance in an area where chemicals are being
used?
Are there leaks in the chemical containers?
You will need orientation and training on how to detect a spill or accidental chemical release -
which is specific to those chemicals in use in your work area.
Additional training may be required. Your facility’s EH&S Department will identify those
employees who require additional training.
1910.1200(h)(3)(i)
HAZARD COMMUNICATION
© Kaiser Foundation Health Plan, Inc.

HOSPITAL – COMPREHENSIVE/INITIAL
Work practice controls and Personal Protective Equipment (PPE)
Work practice controls are an effective way to prevent exposure to chemical hazards.
Examples of safe work practices include:
Follow the precautionary statements printed in the SDS and labels
Do not eat, drink, or chew gums near chemicals
Use well-ventilated work area
Proper use of Personal Protective Equipment (PPE)
Washing your hands after handling chemicals
Consistent and proper use of the correct PPE is another crucial part of safe handling of
Hazardous Materials.
Make sure everyone, including visitors, wears appropriate eye protection
where chemicals are handled.
Wear appropriate gloves (such as Nitrile) to avoid potential contact with
toxic materials; inspect the gloves before each use, wash them before
removal, and replace them periodically or between procedures.
Contact your manager/supervisor for PPE options
1910.1200(h)(3)(iii)
HAZARD COMMUNICATION
© Kaiser Foundation Health Plan, Inc.

HOSPITAL – COMPREHENSIVE/INITIAL
Spill Response
In general, you should know:
What to do in case of an accidental spill—refer to the Rainbow Chart or
other quick reference guide on emergency procedures. You can also
refer to the SDS for accidental release measures.
Incidental or small spills should be cleaned up immediately. With the
proper training, incidental or small spills can generally be cleaned up
by departmental staff. Know what the policy is at your facility/region
Large or Emergency Response Releases, require response from
professionally trained HazMat teams.
For your reference, you may print this fact sheet with information on spill
response: Hazardous Spills Fact Sheet
1910.1200(h)(3)(iii)
HAZARD COMMUNICATION
© Kaiser Foundation Health Plan, Inc.
In addition, remember that spill clean up material may need to be disposed as
hazardous waste! (contact your EH&S Department for consultation).
HOSPITAL – COMPREHENSIVE/INITIAL
Spill Response
You should follow these procedures for response to incidental spills…
Isolate, Evacuate, Secure: Isolate the spill area. Evacuate everyone from the area surrounding the spill, (the
entire room if necessary), except those responsible for clean up of the spill. Secure the area.
Personal Protective Equipment (PPE): If not already worn, put on personal protective equipment as
needed, including: gloves, impervious foot covers and apron, chemical goggles with or without a face shield, if
splash hazard present.
Respiratory Protection: response to an incidental spill will not normally require respiratory protective
equipment.
Apply absorbents or neutralizers immediately to keep respiratory exposure within safe limits. Allow
time for neutralizers to work before cleaning up.
Some chemicals present an inhalation hazard even from small spills and would require use of
equipment such as a Powered Air-Purifying Respirator (PAPR). Those spills would be considered an
Emergency Response Release, in which case you should evacuate and secure the room containing
the spill. Contact your EH&S Department for a list of these chemicals.
Remember that N95-type respirators will not protect against chemical vapors or fumes!
N95 particulate respirators are recommended for spills of hazardous drugs (click on this link for more
information on hazardous drug spills Hazardous Drug Management).
Contain: Stop the source of the spill, if possible.
Confine: Confine spill to initial spill area.
Neutralize: See SDS for information on neutralization.
HAZARD COMMUNICATION
Large, or Emergency Response Releases, require response from Operations Level staff (employees in
EH&S or Engineering may have this training), professionally trained HazMat teams or outside contractors.
1910.1200(h)(3)(iii)
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
CALIFORNIA ONLY: Employee Rights in California, Proposition 65
In California, Title 8 of the California Code of Regulations, Section 5194 (8 CCR 5194) contains additional
notification requirements which are not in the federal standard.
California requires that employees are informed of their right:
To receive information about hazardous substances in their work environment.
For their physician or collective bargaining agent to receive that information
Against discharge or other discrimination due to the employee's exercise of these rights
To receive updated information on a timely basis when a new or revised safety data sheet is received.
This must be within 30 days if the new information indicates significantly increased risks.
California voters approved proposition 65 which requires the state to publish a list of chemicals that are
known to cause cancer, birth defects or other reproductive harm. That list is available on the California
EPA web site (http://www.oehha.ca.gov/prop65.html).
Examples of listed chemicals in health care include formaldehyde, ethylene oxide and some chemotherapy
agents. Prop. 65 also requires that warnings appear on the label of listed products and that warning signs
in the workplace be posted in conspicuous places where they’re likely to be read and understood.
For questions regarding Prop. 65, contact your facility’s EH&S department.
8 CCR 5194 (G)
(This description of Prop. 65 requirements is provided for informational purposes only.)
HAZARD COMMUNICATION

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Hazard Communication Training
So that I am compliant with the Hazard Communication regulation, I agree to learn where
hazardous chemicals are present in my work area; how to access my Hazard Communication
Plan; the chemical inventory for my work area; and how to access Safety Data Sheets
True
False
A
B
HAZARD COMMUNICATION

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
So that I am compliant with the Hazard Communication regulation, I agree to learn where
hazardous chemicals are present in my work area; how to access my Hazard Communication
Plan; the chemical inventory for my work area; and how to access Safety Data Sheets
True
False
The correct answer is A.
Q&A: Hazard Communication Training
A
B
HAZARD COMMUNICATION

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Safe Chemical Storage
It’s important to store chemicals safely. Follow any and all
recommendations of the manufacturer. These are usually
found on the chemical container, label, or safety data
sheet (SDS).
Other things to remember…
Don’t store hazardous chemicals above eye level.
Separate chemicals that could cause a hazardous
reaction if they are mixed. For instance, acids and bases
can be very reactive together.
Consider whether your chemicals need to be stored in a
special cabinet, such as a flammables or a caustics
cabinet.
Do not store chemicals in containers normally used for
other purposes—for instance a dish detergent or milk
bottle.
Chemical containers should not be stored on top of
each other or on the floor where they could accidentally
be knocked over.
Chemicals should never be stored with food.
HAZARDOUS MATERIALS
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Emergency Eyewash
Use of Emergency Eyewash Equipment
You need to know:
Chemicals you use that can cause damage to your eyes or skin
The location of the nearest eyewash Can you get there with your eyes shut?
In areas required to have an emergency eyewashes and/or shower, they must be in accessible locations
that require no more than 10 seconds for the injured person to reach (55 feet maximum).
To activate the eyewash, push or pull the activation mechanism until the water starts
Hold your eyes open and rinse for 15 minutes!
EMERGENCY EYEWASH AND SHOWER
ANSI Z358.1

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Emergency Showers
Emergency Deluge showers are needed in those areas where it is a possibility that either highly corrosive
or highly toxic chemicals may splash over substantial areas of the body.
To activate the emergency shower, pull down on the activation mechanism until the water
starts.
If your clothing is contaminated with chemicals, remove them before getting under the
shower. (The chemicals will stay on the body longer if the clothing is not removed.)
Continue under the shower for 15 minutes before seeking medical attention.
Also remember…there must always be a clear pathway to the eyewash: ensure no carts or boxes are
placed in the way.
EMERGENCY EYEWASH AND SHOWER
ANSI Z358.1

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Medical Gas Safety
Cylinders containing compressed gases
are a serious hazard when not
handled or stored correctly.
A tank which is not secured may be
knocked over. If the valve is knocked off
or the tank ruptures, the cylinder would
become a projectile causing severe
injury or even death.
A leaking oxygen cylinder can be a fire
and explosion hazard.
Leaks of compressed gases which
displace oxygen, such as nitrogen or
carbon dioxide, can put people at risk
for asphyxiation.
HAZARDOUS MATERIALS
EC.02.02.01
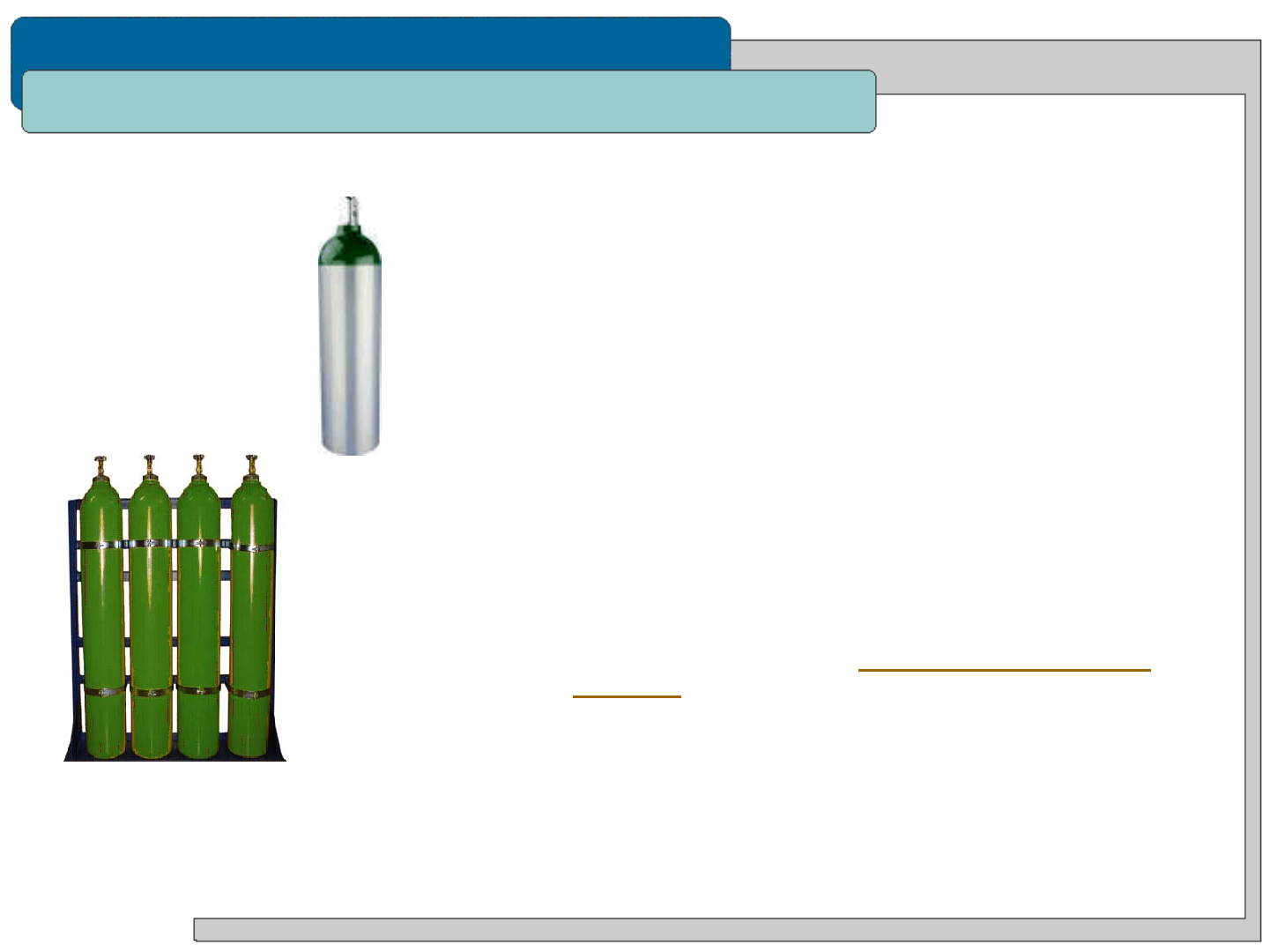
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Medical Gas Safety
Compressed Gas Cylinder Storage
All compressed gas cylinders must be upright and
secured to a fixed object, or held in a portable
transport cart/holder. Cylinders should be secured at
both the top and the bottom.
In patient areas, only 12 small “E-Cylinders” of
oxygen or one H-cylinder (a maximum of 300 cubic
feet) can be stored in a smoke compartment without
special enclosures. In use e-cylinders of oxygen may
be found on gurneys, wheelchairs or crash carts.
These in use e-cylinders are not to be included in the
smoke compartment storage count limitation.
Never store cylinders in an egress corridor!
Click on this link for more information on safe
handling and storage of compressed medical gas
cylinders
HAZARDOUS MATERIALS
EC.02.02.01
E-cylinder
H-cylinders

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
Medical Waste
Hazardous and Universal Waste
Recyclable Waste and Regular Trash (non-hazardous)
SECTION 4: WASTE MANAGEMENT
This training meets the requirements of Medical Waste Management Act - California Health and Safety Code Sections 117600 – 118360,
also Hazardous and Universal Waste Regulations - California Code of Regulations, Title 22, Division 4.5, Chapter 10 - 55.
This section provides information on how employees can create a safe and secure working environment for staff and members and
provides education and training needed to comply with Joint Commission Standard EC.02.02.01

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Overview
Health care organizations can be subject to severe
penalties when waste is not segregated correctly by
staff. Waste typically falls into some basic categories
which are subject to regulations written and enforced by
different government agencies.
These categories include:
Medical Waste
Hazardous and Universal Waste
Recyclable Waste and Regular Trash (non-
hazardous)
In addition to this training, it is important that you know
the local regulatory requirements and facility policies for
waste segregation and disposal at your worksite.
You can contact your facility’s Environmental Health &
Safety Department if you have questions on waste.
WASTE MANAGEMENT
EC.02.02.01
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Kaiser Permanente’s medical waste streams
Medical Waste consists of:
Biohazardous Waste
Pathology Waste
Infectious Laboratory Waste
Trace Chemotherapeutic Waste
Sharps Waste
Non-Hazardous Pharmaceutical Waste
Commingled Sharps and Non-hazardous Pharmaceutical Waste
This presentation will explain what is required to manage each one of these waste streams.
Kaiser Permanente generates a number of different waste streams that are “medical waste”
© Kaiser Foundation Health Plan, Inc.
Note that, if you are involved in the packaging, shipping and transport of medical waste (for
instance—you work in the EVS department), you will need to take additional DOT training on KP
Learn: DOT Regulated Medical Waste Function Specific Training. Contact your facility’s
Environmental Health & Safety Department if you have questions on training requirements.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Why properly manage medical waste? Who is responsible?
Prevent Disease Transmission
It protects KP employees, waste handlers and communities we serve from being exposed to
potentially infectious materials.
Regulatory Compliance
Medical waste management must be properly collected for treatment and disposal. Improper
management can result in regulatory citations and financial penalties.
Affordability and Environmental Stewardship
The cost of treatment and disposal of each medical waste type varies; improperly treating medical
waste can result in unnecessary costs AND unnecessary environmental impact as treatment and
disposal processes use lots of water and energy.
The person that generates the medical waste (for example, nurse, physician, lab tech) is responsible
for knowing how to properly dispose of each type of medical waste generated from their job duties.
The medical waste generator is responsible for disposing of the medical waste into its designated
container at the point of generation.
If you not sure how to dispose of waste, or have concerns regarding container requirements,
report your concerns to your supervisor.
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Biohazardous Waste?
DEFINITION:
BIOHAZARDOUS WASTE
Fluid blood and otherwise potentially infectious body fluids
Items that are soaked with blood and body fluids that “flow”
(gauze, bandages, blood transfusion bags/tubing, etc.)
Items that contain dry blood and body fluids that when
wetted would “flow”
Suction canisters with free flowing liquids, not solidified
Any free-flowing body secretion containing blood
components (e.g. urine, stools, pleural , peritoneal,
amniotic fluids), and any other fluid visibly contaminated
with blood
Any item labeled with a “Biohazard Symbol” (e.g. specimen bags)
is considered medical waste.
WASTE CONTAINER:
Collect in a container labeled with a biohazard symbol on the
lid and sides AND lined with a red biohazard bag.
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Pathology Waste?
DEFINITION:
PATHOLOGY WASTE
Recognizable human anatomical parts
Placentas
Skin or tissue biopsies
Human surgical specimens, tissue, organs, bone
fragments, limbs, or body parts removed during
surgery, autopsy, or other medical procedures
Suction canisters with solidified fluids
WASTE CONTAINER:
Collect in a container labeled with the words “path”
or “Pathology Waste“ on the lid and sides AND lined
with a red biohazard bag.
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Infectious Laboratory Waste?
DEFINITION:
INFECTIOUS LABORATORY WASTE
Human specimen cultures from clinical laboratories
Waste cultures and stocks from the production of bacteria,
viruses, spores, discarded live and attenuated vaccines
used in human healthcare or research, and culture dishes
and devices used to transfer, inoculate and mix cultures
WASTE CONTAINER:
Collect in a container labeled with a biohazard symbol on the
lid and sides AND lined with a red biohazard bag.
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Trace Chemotherapeutic Waste?
WASTE CONTAINER:
Collect in a container usually yellow in color labeled
with the words “chemo” or “Trace Chemotherapy“ AND
“Incinerate Only” on the lid and sides.
© Kaiser Foundation Health Plan, Inc.
DEFINITION: TRACE CHEMOTHERAPEUTIC WASTE
Any device (including personal protective equipment) used in the
production or delivery that is contaminated through contact with,
or having previously contained, chemotherapeutic agents and is
EMPTY.
“Empty” is defined as a container, liner, tubing, or syringe that
has no pourable, scrapable or drainable chemotherapy drug
waste inside when tilted or inverted.
Non-empty devices, containers, or grossly contaminated
items are to be managed as RCRA hazardous waste or “bulk”
chemo waste
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Sharps Waste?
DEFINITION:
SHARPS WASTE
Devices that are designed to puncture or capable of
puncturing or cutting the skin that are contaminated
with blood or potentially infectious body fluids.
Examples include:
Needles; syringes with needles attached;
trocars; pipettes; scalpel blades; guide wires;
blood vials; broken or unbroken glassware that
has been in contact with infectious agents,
including serum bottles, and other rigid objects
© Kaiser Foundation Health Plan, Inc.
WASTE CONTAINER:
Collect in a Red or Clear sharps container, labeled
with the word “Sharps” AND the international
biohazard symbol.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Pharmaceutical Waste?
DEFINITION:
PHARMACEUTICAL WASTE
All prescription or over the counter medications that
do not require collection as trace chemotherapeutic or
hazardous waste
Departments that generate hazardous waste or
trace chemotherapy waste will have a
designated collection process approved by the
EH&S manager
Contact your EH&S Manager for questions regarding
identifying hazardous waste.
WASTE CONTAINER:
CALIFORNIA: Collect in a blue or blue lidded container
labeled with the words “Pharm” or “Pharmaceutical
Waste” AND “Incinerate Only”.
HAWAII: Return to the Pharmacy or dispose of per
department policy
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is Commingled Waste?
DEFINITION:
COMMINGLED WASTE
The collection of sharps and pharmaceutical waste into
the same container.
WASTE CONTAINER:
Collect in a blue or blue lidded container labeled with
the words “Pharm” or “Pharmaceutical Waste” AND
“Incinerate Only”
Note: hazardous or trace chemotherapy waste may not
be placed into the commingled waste container!
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
What is NOT Medical Waste?
Below are some items that are sometimes misclassified as “medical waste”
Urine, feces, saliva, sputum, nasal secretions, sweat, tears, or vomitus, unless it contains fluid blood.
Waste such as paper towels, paper products, articles containing non fluid blood, and other clinical
solid waste products commonly found in the facility.
These should all be disposed of as regular trash or into the sewer (as appropriate)!
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Why does it matter what container medical waste goes into?
NOT all medical waste is BURNED via incineration!
Proper collection and segregation of medical waste ensures proper treatment prior to disposal in a landfill.
© Kaiser Foundation Health Plan, Inc.
The following wastes are treated by
INCINERATION:
Commingled Waste
Pathology Waste
Trace Chemotherapy Waste
Pharmaceutical Waste
The following wastes are treated by
STEAM STERILIZATION:
Biohazardous Waste
Sharps
Infectious Laboratory Waste
WASTE MANAGEMENT
EC.02.02.01
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
As an example, if you find biohazardous waste in the regular trash bin, remember this:
ISOLATE the waste container
Do not attempt to remove or touch the medical waste.
REPORT the incident to your supervisor.
Supervisors should contact the EH&S or EVS Manager for further guidance
EVS will properly manage entire contents of the bin as medical waste.
© Kaiser Foundation Health Plan, Inc.
What do you do if you identify improperly disposed medical waste?
WASTE MANAGEMENT
EC.02.02.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Southern California Policy & Resources
IF YOU WORK IN SOUTHERN CALIFORNIA REGION:
The Southern California Regional Medical Waste POLICY - and your site specific policy -
detail requirements for managing medical waste. (add link to sharepoint)
The Southern California Regional Medical Waste PLAN - and your site specific plan - detail
the processes and procedures that should be used to manage medical waste.
Contact your EH&S, Infection Prevention or EVS departments for questions regarding the
policy or plan or any other needed guidance – click here for contact information.
The Southern California Regional Medical Waste Policy and Plan can be accessed here:
https://sites.sp.kp.org/teams/ehs/scal/_layouts/15/start.aspx#/Shared%20Documents
Or
http://kpnet.kp.org/ehs/training/deeplinks/redirects/scal_med_waste_policy_plan.htm
© Kaiser Foundation Health Plan, Inc.
WASTE MANAGEMENT

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Hazardous Waste and Universal Waste
In addition to Regulated Medical Waste, you may generate other types of waste, such as Hazardous
Waste or Universal Waste.
Hazardous and Universal Waste have special collection, storage, and disposal requirements that differ
from regulated medical waste requirements.
They must be segregated from other types of waste to enable proper disposal!
Examples of Hazardous Waste are Formaldehyde, Warafin, Laboratory solvents and silver nitrate
applicators.
Be aware there are many other types of hazardous waste at KP
If you package, label, ship or transport hazardous waste you are required to take additional
training. The training is available via KP Learn, search for “DOT”.
Universal Waste consists of batteries, electronic equipment, mercury, light bulbs/tubes, and non-empty
aerosol cans.
If you have questions about whether a waste is hazardous or universal waste, or how any waste
should be managed, contact your supervisor or your EH&S Department.
SafetyNet’s Hazardous and Universal Waste Resources
WASTE MANAGEMENT
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Recyclable and Regular Trash (non-hazardous)
WASTE MANAGEMENT
© Kaiser Foundation Health Plan, Inc.
At many Kaiser Permanente sites, items such as non confidential paper, cardboard,
bottles and cans, and organic food waste can be collected for recycling. Know what
items at your site can be collected for recycling, and place them in the proper recycling bin
instead of the regular trash bin whenever appropriate.
The benefits of recycling include
:
Reducing the amount of waste sent to landfills and incinerators;
Conserving natural resources such as timber, water, and minerals;
Preventing pollution by reducing the need to collect new raw materials;
Saving energy;
Reducing greenhouse gas emissions that contribute to global climate change;
Helping to sustain the environment for future generations;
Helping to create new well-paying jobs in the recycling and manufacturing industries in
the United States.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Medical Waste
Which of the following is NOT considered Medical Waste?
Biohazardous Waste
Trace Chemotherapeutic Waste
Non-Hazardous Pharmaceutical Waste
Paper towels and other paper products that don't contain fluid blood
A
B
C
D
WASTE MANAGEMENT

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Medical Waste
Which of the following is NOT considered Medical Waste?
Biohazardous Waste
Trace Chemotherapeutic Waste
Non-Hazardous Pharmaceutical Waste
Paper towels and other paper products that don't contain fluid blood
A
B
C
WASTE MANAGEMENT
D
The correct answer is D.
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
EMERGENCY RESPONSE
Fire Safety
Fire Extinguishers
Emergency Preparedness
SECTION 5: EMERGENCY RESPONSE
Completion of this section, in conjunction with on-site orientation to facility and departmental procedures with regard to Fire Response
Plans, complies with the training requirements of Joint Commission Standard EC.03.01.01 and the requirements of 29 CFR 1910.38 with
regard to staff training on Emergency Plans and Fire Prevention. This section uses "RACE“. See your facility specific supplement to
learn if you use RACE of another acronym at YOUR location.
Completion of this section in conjunction with on-site orientation to facility and departmental procedures with regard to emergency,
disaster response and evacuation complies with the training requirements of CFR 1910.38 with regard to staff training on Emergency
Plans and provides information needed to comply with Joint Commission standard EM.02.02.07.
Completion of this section in conjunction with training on facility-specific and departmental procedures complies with the requirements of
Federal Standard 29 CFR 1910.157 with regard to staff training on the use of portable Fire Extinguishers and provides education and
training needed to comply with Joint Commission Standard EC.02.03.01.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
EC.02.03.01.
FIRE SAFETY AND EXTINGUISHERS
Fire Safety
There are many things you can do to protect yourself
from fire.
In general, you should…
Use good housekeeping practices to keep
combustible material from piling up.
Keep items at least 18 inches below the bottom of
the sprinkler head. Do not hang items from the
sprinkler heads.
Keep all hallways and exits free and clear of
clutter and debris.
Do not prop doors open. Open doors will aid the
spread of the fire.
Report all faulty wiring and electrical equipment to
Engineering.
Give electrical panels 36 inches of clearance.
Don’t post paper signs in egress corridors.
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
Use the term R.A.C.E. to remember basic fire procedures.
(Note that healthcare facilities in Los Angeles DO NOT use R.A.C.E. for fire response – see next slide)
When fire or smoke is discovered remember…
R - Rescue/ Remove patients and staff from area.
A - Alarm - Pull closest fire alarm and follow your facility’s procedures for notification.
C - Confine fire by closing doors. Clear hallways of portable equipment and prepare for
evacuation.
E - Extinguish the fire if small and you have been trained to operate an extinguisher
(or Evacuate if told to do so by the Incident Commander)
FIRE SAFETY AND EXTINGUISHERS
Fire Safety – R.A.C.E.
R - Rescue/Remove patients & staff
A - Alarm
C - Confine fire/Clear hallways
E - Extinguish or Evacuate
`
CFR 1910.157, EC.02.03.01
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Code Red Response – Los Angeles Medical Centers
You must review the FACILITY-SPECIFIC SUPPLEMENT page at the end of this training for information
on the acronym used at YOUR facility/region to respond to a fire.
For example: the city of Los Angeles has additional Fire/Life Safety training requirements for Hospital staff.
Affected hospitals include:
Los Angeles/LAMC
Panorama City
South Bay
West LA
Woodland Hills
Note that healthcare facilities in Los Angeles DO NOT use R.A.C.E. for fire response.
In addition, every four years hospital staff in the city of Los Angeles must complete additional training on
how to respond to a fire, including use of first aid fire equipment and employee evacuation procedures.
You can contact your facility’s Environmental Health & Safety Department if you have questions about
fire safety.
EC.03.01.01, 29 CFR 1910.38
FIRE SAFETY

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
P.A.S.S.
To operate a fire extinguisher, remember:
P.A.S.S.
P - Pull The Pin
A - Aim The Nozzle (at the base of the fire)
S - Squeeze The Handle
S - Sweep It Back & Forth (at the base of the fire)
Pull Aim Squeeze Sweep
PORTABLE FIRE EXTINGUISHERS
CFR 1910.157, EC.02.03.01
© Kaiser Foundation Health Plan, Inc.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Fire Extinguishers - The Hazards of Early Stage Fire Fighting
There are things to consider when assessing the risk of
trying to extinguish a fire:
Is the fire too big to use an extinguisher? Portable
extinguishers last for only a short time when
activated - less than a minute.
Is the air unsafe to breathe?
Is the area too hot or too smoky?
Is there a clear evacuation path behind you as you
extinguish the fire?
Remember:
Stand between the exit and the fire to escape if
needed.
Never place yourself or others in jeopardy by
attempting to extinguish a fire.
If it is not SAFE to extinguish a small fire, or if
smoke becomes hazardous, leave the area!
CFR 1910.157, EC.02.03.01
PORTABLE FIRE EXTINGUISHERS
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Hospital Fire Response
Hospital Smoke Compartments:
Each floor of a hospital is divided into separate Smoke Compartments. Each smoke compartment is
surrounded by walls and doors with added protection against smoke and fire, and will provide a
barrier between you and the area which is burning.
You should know the boundaries of your smoke compartment and the smoke compartments adjacent
to your unit.
If there is a fire on your unit, you would immediately evacuate yourself, coworkers, patients and
visitors into the adjacent smoke compartment. This is known as Horizontal Evacuation.
Note: stairwells in protected buildings are both smoke and fire resistant!
EC.02.03.01, 29 CFR 1910.38
FIRE SAFETY

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Hospital Fire Response and Evacuation
In the event of fire, Hospital Employees will not leave the building unless instructed to do so.
If there is a fire on the unit, Hospital Departments evacuate in the following order…
1. Horizontal Evacuation (side to side to the next safe smoke compartment on the same floor)
2. Vertical Evacuation (going down the stairs to the next safe smoke compartment)
3. Evacuate the Building - only under the direction of the fire department or the incident
commander.
Familiarize yourself with both the primary and secondary evacuation routes for your unit. Evacuation Maps
are posted throughout each facility.
EC.02.03.01, 29 CFR 1910.38
FIRE SAFETY
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Fire Drills
For COMPLIANCE with both Joint Commission Standards and NFPA Fire Code, ALL employees are
REQUIRED to participate in fire drills that are conducted regularly by EH&S or Engineering! Treat a drill
like a real Code Red: Stop work and participate in the drill – EVERY TIME!
Fire Drills are conducted at every facility as follows:
Hospitals - 1 drill per quarter per shift
Medical Office Buildings which are Accredited – 1 drill per quarter per shift
Medical Offices and other buildings – at least once per year
EC.02.03.01, 29 CFR 1910.38
FIRE SAFETY

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Fire Drills
Which of the following can you do to protect yourself from fire?
Keep all hallways and exits free and clear of clutter and debris.
Do not prop doors open because open doors will aid the spread of the fire.
Both A and B are correct.
A
B
C
FIRE SAFETY

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Which of the following can you do to protect yourself from fire?
Keep all hallways and exits free and clear of clutter and debris.
Do not prop doors open because open doors will aid the spread of the fire.
Both A and B are correct.
C
The correct answer is C.
A
B
Q&A: Fire Drills
FIRE SAFETY

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Disasters
The Joint Commission defines a “disaster” as “an unexpected or sudden event” and also “a natural or
human-made event that significantly disrupts the environment of care, or results in a sudden, significantly
changed or increased demand for the organization’s services.”
Commonly within Kaiser Permanente we define a “disaster” as any unplanned event, inside or outside
our facility, that may affect our facilities, staff, patients, or our ability to provide care.
We have a four-part program to manage disasters that includes:
Mitigation
Preparedness
Response
Recovery
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Disaster Response Codes
All facilities use disaster codes. The FACILITY-SPECIFIC SUPPLEMENT page at the end of this
training contains information about the codes for YOUR facility.
Examples of internal disasters might be: IT computer system failures, public utility outages,
hazardous materials spills, fires.
Examples of external disasters might be: earthquakes, tsunamis, hurricanes, wildfires, terrorist acts,
hazardous materials spills near your facility or infectious pandemics.
Each facility/region has developed Code Flipcharts (sometimes called Rainbow Charts) which contain
basic information on what you should do in response to an emergency.
These charts are posted throughout work areas as staff quick references.
You must familiarize yourself with the codes used at your facility for each type of emergency.
29 CFR 1910.38, EM.02.02.07
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Emergency Operations Plans
Each medical center has an Emergency Operations Plan to manage disaster response.
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training contains specific information
about YOUR facility’s plans, where they are kept and how you can get a copy if you want to read it.
Some critical departments have created department-level Emergency Operations Plans also. Familiarize
yourself with any department specific procedures for your work area.
29 CFR 1910.38, EM.02.02.07
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Roles & Responsibilities During a Disaster
Your role and responsibilities during an emergency will depend on where
you work and what you do.
You may be reassigned to new or different duties during a disaster.
See your facility’s specific information (link at the end of this section) for
what you should do in a disaster:
If you are at work when a disaster happens, or
If you are at home when a disaster happens.
Keep your manager and Human Resources current on your contact
information for any emergency call-back lists they might maintain.
Communications in a disaster are often difficult. Listen for public
information broadcasts on radio and TV, check your facility’s web page,
and call your staff hotline (if your facility has one).
29 CFR 1910.38, EM.02.02.07
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Managing the Emergency Response
Depending on your location, your facility/region will have a
A Hospital Command Center (HCC), or
An Emergency Operations Center (EOC)
This will be activated if the disaster code is called. It’s a place for leaders to gather, collect information,
make decisions, and manage the response until the crisis is over and the Code is secured.
Kaiser Permanente facilities use the Incident Command System (also known as the Hospital Incident
Command System) to manage disaster response in the HCC/EOC.
The person in charge in the HCC/EOC during a disaster is called the “Incident Commander.” Other
managers may be assigned to help in various pre-set roles as needed.
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training will tell you how to locate YOUR
HCC/EOC and its phone number.
29 CFR 1910.38, EM.02.02.07
EMERGENCY PREPAREDNESS
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Hazard Vulnerability Assessment and Drills
Medical centers conduct a
Hazard Vulnerability Assessment (HVA)
every year to determine the greatest threats, so they can focus
preparations in the right areas. HVAs are specific to each facility, its
locations, operations, and threats (internal or external).
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training
contains the top risks to YOUR medical center based on recent
vulnerability assessments.
Each hospital conducts at least two disaster drills a year (this is also a
requirement of The Joint Commission).
Drills are designed to prepare the facility for the greatest risks identified
on its HVA (Hazard Vulnerability Assessment).
29 CFR 1910.38, EM.02.02.07
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
OSHA Emergency Action Plan
Your Emergency Operations Plan also includes OSHA-required emergency evacuation procedures
including how to evacuate and accounting for all staff after an evacuation. (The plan also covers how to
evacuate patients as part of the process.)
Do not evacuate hospitalized patients until directed to do so
by overhead speaker, or
by your manager!
Posted in your facility are maps of exit paths through marked exit doors and stairs to designated areas
outside the building. When you get to your work area find these maps, learn the fire escape routes, and
ask your supervisor if you have any questions.
When you get to your work area ask your supervisor about evacuation plans and what your duties are if an
evacuation is ordered.
29 CFR 1910.38, EM.02.02.07
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Which is an “internal disaster”?
An example of an internal disaster is:
Earthquake
Wildfire
IT computer system failure
Terrorist attack
A
B
C
D
EMERGENCY PREPAREDNESS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
An example of an internal disaster is:
Earthquake
Wildfire
IT computer system failure
Terrorist attack
A
B
C
D
The correct answer is C.
Q&A: Which is an “internal disaster”?
EMERGENCY PREPAREDNESS

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
ELECTRICAL & EQUIPMENT SAFETY
Lockout/Tagout (for Affected & Other Employees)
Medical Equipment
Utilities Safety
SECTION 6: MECHANICAL & ELECTRICAL SAFETY
Completion of this training module in conjunction with orientation and review of any facility or department-specific procedures with regard
to Utilities Management will provide employees with education and knowledge needed to comply with Joint Commission standard
EC.02.05.01.
Completion of this course in conjunction with orientation and review of any facility or department-specific procedures with regard to
Medical Equipment Management will provide employees with education and knowledge needed for compliance with Joint Commission
Standard EC.02.04.01.
Completion of this course complies with Federal requirements for training of affected and other employees with regard to controlof
hazardous energy under Federal Standard 29 CFR 1910.147 and California 8 CCR §3314.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Lockout/Tagout for Affected and Other Employees
There are machines and equipment in our workplace which require periodic servicing and maintenance.
The unexpected start-up of these machines/equipment or uncontrolled release of energy from them could
cause injury to employees (e.g., electrocution). All Kaiser Permanente facilities have implemented a
Hazardous Energy Control Program to prevent injury to employees. This program is known as
Lockout/Tagout (LOTO).
What is “Lockout/Tagout”?
Lockouts and Tagouts are the ways maintenance personnel control hazardous energy from
being released when they are working on a piece of equipment.
Sources of potentially hazardous energy include low to very high voltage electricity, compressed
air, oxygen or other gases, open flames, steam, hydraulic line forces, radiation sources including
x-ray laser light sources from laser surgical machines and spring tension.
29 CFR § 1910.147(c)(7)(i)(B)
Purpose and Use of Energy Control
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)
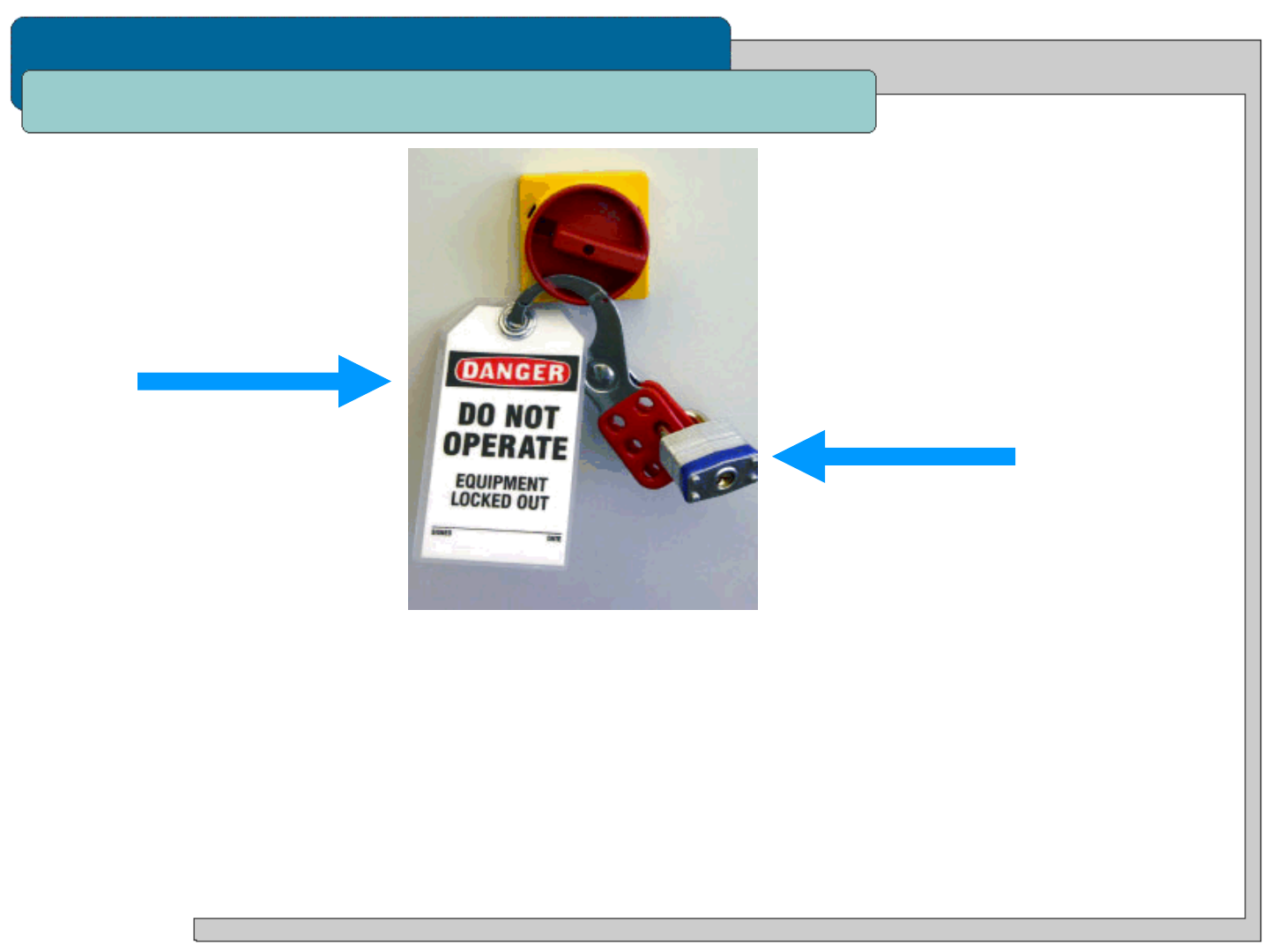
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Procedures and Prohibitions
LOCKOUT is a physical lock that
holds a switch in the off position or
holds shut a valve so hazardous
energy cannot be released while the
maintenance is occurring.
TAGOUT is a paper or
plastic tag that is placed on a
breaker/switch, or valve that
warns other people not to
operate it. Tagouts are used
when a Lockout cannot be
used.
How this applies to YOU:
Lockouts and Tagouts protect lives and ensure human safety. You may be working in or walking through an
area where a Lockout or Tagout is being used.
If you see one, DO NOT TOUCH IT! Someone’s life may be at risk!
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)
29 CFR § 1910.147(c)(7)(i)(B),(C)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
“Affected” Employees
You are an “affected” employee if…
your job requires you to operate or use a
machine or equipment on which cleaning,
repairing, servicing, maintenance, setting-up or
adjusting operations are being performed under
lockout or tagout, or
your job requires you to work in an area in
which such activities are being performed under
Lockout or Tagout.
(An example is in Radiology, if you work around
certain MRI or CT scan equipment.)
When equipment in your work area needs to be locked
out or tagged out, the appropriate department (for
example, Engineering or Kaiser Clinical Technologies)
will notify you about the upcoming work and any
other information you will need to remain safe.
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)
29 CFR § 1910.147(c)(7)(i)(B)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Limitations of Tags
Tagouts have limitations:
You should be aware that tags are essentially warning devices affixed to energy isolating
devices and do not provide the physical restraint on those devices that is provided by a lock.
The person who applied the lockout or tagout device is the ONLY person who may remove it!
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)
29 CFR § 1910.147(c)(7)(ii)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Lockout/Tagout Questions?
Questions or Problems:
If you see a problem with a tagout (e.g., torn or ripped, fallen off), inform your supervisor/team leader
and the maintenance person identified on the tag immediately.
If you have any other questions or concerns about the Lockout/Tagout program,
contact your local EH&S Department or visit the NEH&S SafetyNet Lockout/Tagout Resources page:
http://kpnet.kp.org/ehs/loto/.
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Q&A: Removing a Lockout or Tagout Device
Who is authorized to remove a lockout or tagout device?
The manager or supervisor responsible for the given area
The Environmental, Health and Safety Officer
Any employee who needs to
Only the person who applied the given lockout or tagout device
A
B
C
D
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Who is authorized to remove a lockout or tagout device?
The manager or supervisor responsible for the given area
The Environmental, Health and Safety Officer
Any employee who needs to
Only the person who applied the given lockout or tagout device
A
B
C
D
The correct answer is D.
Q&A: Removing a Lockout or Tagout Device
LOCKOUT/TAGOUT (AFFECTED AND OTHER EMPLOYEES)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Clinical Technologies
“ClinTech” is the department responsible for the management of the maintenance of all medical
equipment at Kaiser Permanente facilities - regardless of ownership.
Some of the responsibilities of these departments include:
Maintaining current, accurate inventories of all medical equipment
Monitoring and acting on medical equipment hazard notices and recalls
Conducting electrical safety testing on medical equipment
Conducting scheduled preventive maintenance of all medical equipment
Note that at most medical centers, ClinTech does not maintain or repair:
Typically these items will be maintained by the facility’s Engineering Department or an outside
contractor.
MEDICAL EQUIPMENT
Sphygmomanometers
High Level Disinfection Units
(GUS, Steris)
TVs
OR Tables
Wheel chairs
Call lights
Patient lifts
Beds
Patient Mechanical Scales
EC.02.04.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Preventive Maintenance (PM) Tags
Prior to use of medical equipment, staff must inspect the PM Tag to ensure that its preventive
maintenance is current (not expired).
Equipment with outdated PM tags must be immediately reported to your supervisor and/or ClinTech.
Remove from service and make it available for the performance of the PM.
Patient equipment should have inspection stickers. Individual pieces of Medical Equipment can be
identified by the color-coded Equipment Identification Number (EIN) Sticker, which will look similar to one
of the following:
MEDICAL EQUIPMENT
EC.02.04.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Malfunctioning Equipment Tags & Safe Medical Devices Act
Medical Equipment which malfunctions must be tagged with a malfunctioning equipment tag and
moved to a location where it will not be used.
Contact ClinTech to report the equipment malfunction. Tags on equipment should describe the exact
problem so that proper repair can be promptly arranged.
Staff should never “tag” equipment with a piece of paper marked “broken”. Be aware that “broken”
doesn’t really describe what is wrong with the equipment.
Remember that not using the tags or not following the proper procedures could jeopardize patient safety!
Safe Medical Devices Act (SMDA)
Medical Equipment failure or malfunction that causes or contributes to patient injury, illness or death must
be reported, as required by the Federal Drug Administration (FDA).
In these instances a Responsible Reporting Form (RRF) should be completed.
All equipment involved in such an incident must be sequestered by ClinTech for investigation.
MEDICAL EQUIPMENT
EC.02.04.01
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
You should:
Contact ClinTech to report the equipment malfunction.
Put tags on equipment that describe the exact problem so that proper repair can be
promptly arranged.
Never “tag” equipment with a piece of paper marked “broken”.
True
False
© Kaiser Foundation Health Plan, Inc.
Q&A: ClinTech
A
B
MEDICAL EQUIPMENT

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
You should:
Contact ClinTech to report the equipment malfunction.
Put tags on equipment that describe the exact problem so that proper repair can be
promptly arranged.
Never “tag” equipment with a piece of paper marked “broken”.
True
False
© Kaiser Foundation Health Plan, Inc.
Q&A: ClinTech
A
B
MEDICAL EQUIPMENT
The correct answer is A.
HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Utilities Failures
There are a number of utilities in use at a hospital, and any of these
may fail. Your facility may experience electrical failure,
flooding/sewer failure, medical gas failure, medical vacuum
failure, hi-pressure steam failure, elevator failure or
communications failure. These systems are maintained by the
Facility Services department at each medical center.
Review your facility’s Rainbow Chart, or contact your supervisor or
EH&S Department to learn what to do in any of these utility failure
situations.
UTILITIES
EC.02.05.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Medical Gases/Compressed Gas Cylinders
Staff in departments with piped medical gases
should know what your department’s
responsibilities are with regard to emergency
medical gas shut off.
Know the location of the shut-off valves and the
rooms they control. If unsure of your
responsibilities, discuss with your supervisor or
contact your Engineering department.
UTILITIES
EC.02.05.01

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Electrical Safety
Electricity - General Safety Tips:
Do not use “cheater” adapters or multiple adapters. Extension cords should be no longer than
10 feet and used only in temporary emergency situations.
Always disconnect plugs from wall by grasping the plug, not the cord.
Equipment in patient care areas in a Hospital must have a 3-prong plug and be plugged into a 3-
wire receptacle.
At most facilities, electrical outlets which are connected to the back-up generators are colored
RED. Red outlets are to be used primarily for life support equipment. At some hospitals, all
outlets connect to back up generators. You should know which outlets in your area connect to
back up power and your building’s emergency procedures in the event of power loss.
Don’t plug microwaves or refrigerators into power strips.
Remove equipment from service if…
There is evidence of overheating.
Someone has received a shock from the equipment.
Any wire is frayed, worn, burned, cut, or warm.
It has been dropped or is physically damaged.
Switches or knobs are loose or do not turn from one position to another, or do not consistently
produce the expected result when operated.
Liquid has been spilled on it.
If in question, do not use!
UTILITIES
EC.02.05.01

HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
NOTIFICATIONS
Right to Access Exposure Records
SECTION 7: NOTIFICATIONS
Completion of this section complies with Federal requirements for Notification of Employee Access to Exposure Records under 29 CFR
1910.1020 and California requirements for 8 CCR 3204.

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Employee Access to Exposure Records
Kaiser Permanente maintains records of any occupational exposure to harmful chemical or biological
agents (or testing for them). An example is testing for staff exposure to TB. Certain records are
maintained by the Employee Health Department, while records of any testing for occupational exposure to
hazardous chemicals will be maintained by the facility’s safety department.
Federal law requires that employers notify their employees of the existence of Employee Exposure
Records at the start of employment and at least annually thereafter.
This section is your notification!
NOTE: Before finishing this training, you must know how to contact your Employee Health Department
which is responsible for maintaining and providing access to Employee Exposure Records.
The FACILITY-SPECIFIC SUPPLEMENT page at the end of this training will tell you how to find YOUR
facility’s Employee Health Designee.
Location and Availability of Records
Responsible Persons
ACCESS TO EXPOSURE RECORDS
1910.1020(g)(1)(iii)

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Right to Access Records and the Standard
You have the right to review your relevant exposure records.
Kaiser Permanente must make available a copy of the standard and its appendices to its employees.
Click here to access a copy of OSHA Standard 29 CFR 1910.1020
Click here to access a copy of the standard’s Appendix A
Click here to access a copy of the standard’s Appendix B
1910.1020(g)(1)(iii)
Right to Access Records
Access to the Standard
ACCESS TO EXPOSURE RECORDS

HOSPITAL - INITIAL ASSIGNMENT
HOSPITAL – COMPREHENSIVE/INITIAL
© Kaiser Foundation Health Plan, Inc.
Quiz
SAFETY & ENVIRONMENT OF CARE TRAINING (INITIAL)
The following Quiz consists of 10 questions.
To receive credit for the course, you must pass the Quiz with a score of 80% or better.
If you do not pass the quiz, you may take it again.
Good Luck!
