
78
FEBRUARY 2018 www.ajmc.com
POLICY
I
nstances in which private information has been breached
are becoming more commonplace in the United States,
1
making the security of this type of information a signicant
concern.
2
Healthcare information is particularly vulnerable,
due to the sensitivity of these data and how they can be used
by criminals.
3
Demographic data, Social Security numbers, and
clinical information, including medical diagnoses, are housed
in both paper and electronic health records (EHRs).
3
For these
reasons, multiple attempts have been made through federal
legislation to help curtail the occurrences of healthcare privacy
breaches, including the 1996 Health Insurance Portability and
Accountability Act (HIPAA), the Health Information Technology
for Economic and Clinical Health Act of 2009, and the Omnibus
Final Rule in 2013.
4-6
Despite these initiatives, however, large data
breaches are still occurring in US hospitals.
The adoption of EHRs among hospitals has increased rapidly
over the past several years.
7,8
As healthcare systems digitized to keep
up, the healthcare sector was unable to adopt electronic security
components at the same pace, leading to vulnerabilities in record
systems.
7
In some cases, technology purposed to assist healthcare
delivery processes are now having costly diculties.
9,10
The majority
of small- and medium-size health organizations do not possess the
nancial or personnel resources necessary for sucient information
technology (IT) and security investments.
11,12
This, along with their
highly valuable data, has left hospitals vulnerable to breaches of
sensitive information.
13,14
Hospitals have begun to implement strategies to help prevent data
breaches that most often occur through theft, loss, unauthorized
access, or hacking.
15
Strategies include the adoption of systems
that include 2-factor authentication requirements to ensure that
patients’ health information is only accessible to and usable by
those with rights to access it.
16
Two-factor authentication often
incorporates a biometric component to verify the user’s identity,
such as a ngerprint, voice recognition, or iris scan, along with a
password, personal identication number, or physical verication
object, such as a token or key.
Data Breach Locations, Types, and Associated
Characteristics Among US Hospitals
Meghan Hufstader Gabriel, PhD; Alice Noblin, PhD, RHIA, CCS; Ashley Rutherford, PhD, MPH;
Amanda Walden, MSHSA, RHIA, CHDA; and Kendall Cortelyou-Ward, PhD
ABSTRACT
OBJECTIVES: The objectives of this study were to describe
the locations in hospitals where data are breached, the types
of breaches that occur most often at hospitals, and hospital
characteristics, including health information technology (IT)
sophistication and biometric security capabilities, that may
be predicting factors of large data breaches that affect 500
or more patients.
STUDY DESIGN: The Office of Civil Rights breach data from
healthcare providers regarding breaches that affected 500 or
more individuals from 2009 to 2016 were linked with hospital
characteristics from the Health Information Management
Systems Society and the American Hospital Association
Health IT Supplement databases.
METHODS: Descriptive statistics were used to characterize
hospitals with and without breaches, data breach type, and
location/mode of data breaches in hospitals. Multivariate
logistic regression analysis explored hospital characteristics
that were predicting factors of a data breach affecting at
least 500 patients, including area characteristics, region,
health system membership, size, type, biometric security
use, health IT sophistication, and ownership.
RESULTS: Of all types of healthcare providers, hospitals
accounted for approximately one-third of all data breaches and
hospital breaches affected the largest number of individuals.
Paper and films were the most frequent location of breached
data, occurring in 65 hospitals during the study period,
whereas network servers were the least common location but
their breaches affected the most patients overall. Adjusted
multivariate results showed significant associations among
data breach occurrences and some hospital characteristics,
including type and size, but not others, including health IT
sophistication or biometric use for security.
CONCLUSIONS: Hospitals should conduct routine audits
to allow them to see their vulnerabilities before a breach
occurs. Additionally, information security systems should
be implemented concurrently with health information
technologies. Improving access control and prioritizing patient
privacy will be important steps in minimizing future breaches.
Am J Manag Care. 2018;24(2):78-84

THE AMERICAN JOURNAL OF MANAGED CARE
®
VOL. 24, NO. 2
79
A False Sense of Security
The objectives of this study were to describe
the locations in hospitals where data are
breached, the types of breaches that occur most
often at hospitals, and hospital characteristics,
including health IT sophistication and biometric
security capabilities, that may be predicting
factors of large data breaches that aect 500
or more patients. In spite of these health IT
strategies, it is unclear what the most common
types of breaches are and where patients’ health
information is most vulnerable. Under federal
legislation, if a healthcare privacy breach aects
500 or more patients it must be reported to the
Oce of Civil Rights (OCR). Then, information
regarding the breach is publicly posted on the
OCR data breach portal.
13,17
Although several studies have examined
OCR data breach information,
11-13
none have specically focused on
pediatric, academic, and nonfederal acute care hospitals, which
house millions of patient records.
METHODS
Data Sources
The OCR data breach portal provides an online database describing
data breaches of protected health information (PHI) that aect 500
or more individuals.
15,18
This portal provides users the option of
examining breach information from 3 types of covered entities:
health plans, healthcare clearing houses, and healthcare providers.
As of July 2016, the OCR portal included 1085 healthcare providers
that had PHI breaches aecting 500 or more individuals between
October 2009 and July 2016. Of these, 185 were nonfederal acute care
hospitals and 27 were Veterans Aairs (VA) hospitals. Nonfederal
acute care hospital breach information was linked with the 2015
Health Information and Management Systems Society (HIMSS)
analytic data le (HIMSS Analytics, unpublished data) and informa-
tion from the 2015 American Hospital Association (AHA) Health IT
Supplement Survey regarding the use of 2-factor authentication.
19
Variables to Characterize Data Breaches
Hospital data breaches of PHI that aected 500 or more individuals
were characterized by: 1) type of breach and 2) location or mode
of breached information. Data breach types included 6 categories:
1) hacking/IT incident, 2) improper disposal, 3) loss, 4) other/unknown,
5) theft, and 6) unauthorized access/disclosure. Data breach loca-
tions or modes included 7 categories: 1) desktop computer, 2) EHR,
3) email, 4) laptop computer, 5) network server, 6) paper/lms, and
7) other location. To gain a more detailed view of which provider
types were most frequently breached and had the most individuals
aected, the OCR data were further categorized by “name of covered
entity” into 9 health provider categories: 1)colleges/universities;
2)emergency response; 3)government; 4)group/physician practices;
5)health systems; 6)hospitals; 7)nursing homes, home/hospice care,
and treatment facilities; 8)pharmacies; and 9)research facilities,
laboratories, and medical supply companies.
Inclusion/Exclusion Criteria
Only nonfederal acute care hospitals, which include children’s,
teaching, and public or private hospitals, were included in this study.
All other health provider categories were excluded.
Variables to Characterize Hospitals
Variables to characterize hospitals included area characteristics,
region, bed size, health system membership, hospital type, health
IT sophistication, hospital governance, and market concentration
at the hospital referral region (HRR) level. A binomial variable for
area characteristics was created that assessed whether the hospital
was located in a rural or urban area; hospitals were considered to be
urban if they were located in a metropolitan core–based statistical
area. Regions (Northeast, Midwest, South, and West) were categorized
based upon the US Census Bureau classication system. Hospitals
were categorized into small (<100 staed beds), medium (100 to 399
staed beds), and large (≥400 staed beds). Hospital types included
academic, general medical and surgical, pediatric, critical access,
and other specialty. A second binomial variable was created to
measure health IT sophistication, and high levels were dened as
having a HIMSS Electronic Medical Record Adoption Model (EMRAM)
score of 6 or 7. The EMRAM score ranges from Stage 0, which is
paper-chart–based, to Stage 7, which is dened by a complete EHR
system.
16
A third binomial variable characterizing biometric security
use was created by combining the hospitals that used biometric
technology for security on the HIMSS analytics survey and/or the
hospitals that answered that they supported an infrastructure for
2-factor authentication, including biometrics, in the AHA Health IT
Supplement Survey. Hospital governance characteristics included
TAKEAWAY POINTS
›
Even with sophisticated health information technology (IT) systems in place, security breach-
es continue to affect hundreds of hospitals and compromise thousands of patients’ data; this
gives cause to believe that other hospital factors, such as area characteristics, region, bed
size, health system membership, hospital type, hospital governance, and market concentra-
tion, may play a vital role in breach risk.
›
This study's results showed that of all types of healthcare providers, hospitals accounted
for approximately one-third of all data breaches and hospital breaches affected the largest
number of individuals.
›
Paper and films were the most frequent mode or location of data breaches. However,
although network servers were among the most infrequent locations of data breaches,
breaches of this type impacted the most patients overall.
›
Adjusted multivariate results showed significant associations among data breach occur-
rences and some hospital characteristics, including type and size, but not others, including
health IT sophistication or biometric use for security.

80
FEBRUARY 2018 www.ajmc.com
POLI CY
hospital status, such as not-for-prot, investor-owned (for-prot),
and government (nonfederal). In addition, a hospital was considered
to be a member of a hospital system if it belonged to an integrated
healthcare delivery system. Market concentration was measured
by the Herndahl-Hirschman Index,
20
constructed on bed shares
within systems at the HRR level.
21
Data Analysis
Descriptive analyses to characterize provider facility, data breach
type, and location/mode in hospitals were performed. Number of
patients aected by data breaches was log transformed and a factorial
2-way analysis of variance (ANOVA) was conducted to examine the
dierences between data location/mode and type of breach and the
number of patients aected by data breaches. Univariate analyses
were conducted on hospital and area characteristics. To explore
factors associated with hospitals having a data breach aecting
500 or more individuals, multivariate logistic regression analyses
were performed using SAS Enterprise Guide (SAS Institute Inc; Cary,
North Carolina). Signicance was determined at the P <.05 level.
RESULTS
In total, 215 breaches, each aecting 500 or more individuals,
occurred at 185 nonfederal acute care hospitals that reported to
the OCR during the study period. Thirty hospitals had multiple
breaches during that time. Twenty-four hospitals had 2 breaches,
5 hospitals had 3 breaches, and 1 hospital had 4 breaches (Table 1).
Descriptive Results
Signicant dierences were found between hospitals that had at
least 1 breach and hospitals that did not have a breach aecting 500
or more individuals during the study period (Table 2). Bivariate
descriptive statistics comparing hospitals with and without data
breaches showed unadjusted dierences in terms of hospital
type, size, and ownership. Specically, teaching hospitals (18%
with a data breach vs 3% without a breach) and pediatric hospitals
(6% with a breach vs 2% without) had higher percentages of data
breaches. Larger hospitals also had a higher percentage of data
breaches (26% with a data breach vs 10% without). In addition, a
lower percentage of investor-owned (for-prot) hospitals (15% with
a data breach vs 22% without) and other specialty hospitals (6%
with a data breach vs 12% without) had at least 1 data breach. In
bivariate descriptive analyses, health IT sophistication, biometric
security use, health system membership, hospital region, and
area characteristics were not signicantly dierent in terms of
data breach percentages.
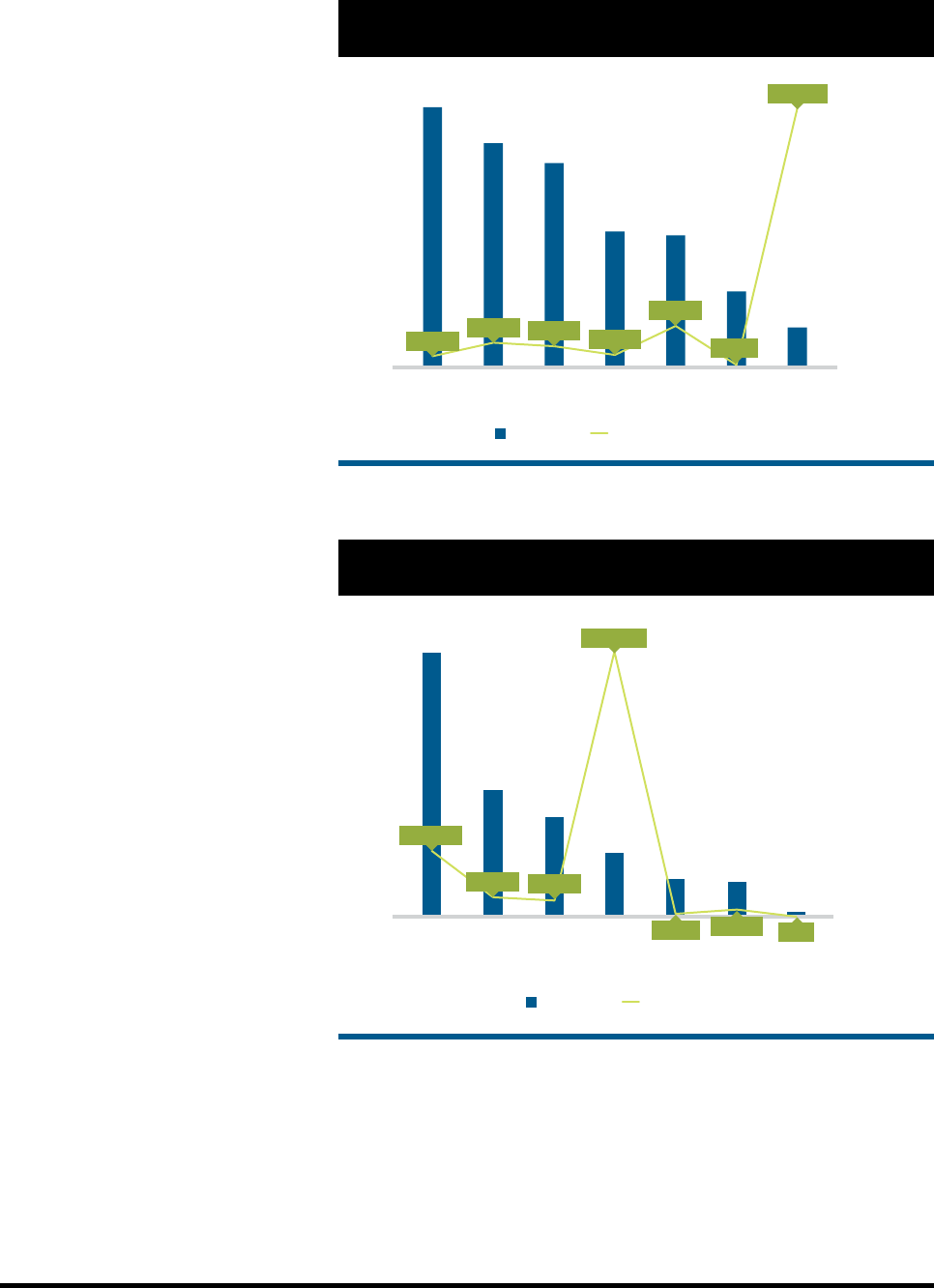
Location of Data Breaches in Hospitals
The location of breached data and the number of individuals aected
varied greatly among hospitals (Figure 1). Data breaches of paper/
TABLE 1. Number of Data Breaches Affecting 500 or More
Individuals Among US Hospitals, 2009-2016
Number of Breaches Number of Hospitals
1 185
2 24
3 5
4 1
TABLE 2. Characteristics of US Hospitals With and Without
Data Breaches Affecting 500 or More Individuals, 2009-2016
Variable
Hospitals
Without
Breaches
n = 5295
Hospitals
With
≥
1
Breach
n = 185 P
Area Characteristics
Rural 21% 17% .205
Urban 79% 83% .205
Hospital Region
West 19% 23% .111
Midwest 29% 27% .786
South 40% 36% .764
Northeast 13% 14% .555
Health System Membership
(yes/no)
Health system membership
(yes)
69% 68% .762
Hospital Size
Small 53% 37% .572
Medium 36% 36% .928
Large 10% 26% <.001
Hospital Type
General medical and surgical 58% 48% .758
Teaching hospital 3% 18% <.001
Critical access hospital 25% 21% .322
Other specialty hospital 12% 6% <.001
Pediatric hospital 2% 6% <.001
Biometric Security Use (yes/no)
Biometric security use (yes) 39% 42% .746
Health IT Sophistication
(high/low)
High health IT sophistication 30% 33% .611
Hospital Ownership
Government, nonfederal 19% 18% .744
Not-for-profit 58% 67% .398
Investor-owned, for-profit 22% 15% .003
IT indicates information technology.
THE AMERICAN JOURNAL OF MANAGED CARE
®
VOL. 24, NO. 2
81
A False Sense of Security
lms occurred most frequently (65 hospitals).
Data located in “other locations” (eg, breaches
not from paper/lms, laptop computers, email,
desktop computers, EHRs, or network servers,
which were reported in 56 hospitals) and in
laptops (in 51 hospitals) were the second and
third most prevalent, respectively. The numbers
of unsecured PHI breaches from email (in
34 hospitals) and desktop computers (in 33
hospitals) were approximately equal during
the study period. EHR data were breached in
19 hospitals. Although network server breaches
occurred most infrequently (in 10 hospitals),
these breaches compromised the highest num-
ber of individuals (4,613,858 aected).
Types of Data Breaches in Hospitals
Types of data breaches and the number of indi-
viduals aected by those types of breaches varied
signicantly among hospitals (Figure 2). Thefts
occurred most frequently (in 112 hospitals),
followed by unauthorized access/disclosure
(in 54 hospitals), whereas hacking/IT incidents
from 27 hospitals aected the most individuals
(4,685,426).
Two-way ANOVA indicated no statistically
signicant dierences in the number of patients
aected between data location/mode (P = .455)
or type of breach (P = .443). There were, however,
statistically signicant dierences between
frequency of data breaches occurring from
network servers and EHRs (P = .018) and between
network servers and paper lms (P = .003).
Multivariate Results
Adjusted results showed similar associa-
tions among biometric use for security and
hospital characteristics, including type and
size. Pediatric hospitals (odds ratio [OR], 5.1;
95% CI, 2.5-10.2) and teaching hospitals (OR,
5.0; 95% CI, 2.9-8.4) were associated with an
increased risk of data breaches compared with
other types of hospitals. In addition, small
(OR, 0.3; 95% CI, 0.2-0.6) and medium (OR,
0.6; 95% CI, 0.3-0.9) hospitals by bed size were associated with a
decreased risk for data breaches compared with larger hospitals.
Hospital setting, health system membership, health IT sophistica-
tion, federal status, market concentration, and ownership status
were not predicting factors of a data breach aecting 500 or more
patients (Table 3).
DISCUSSION
Approximately one-third of all healthcare data breaches occurred
in hospitals, and the most individual patients were impacted when
hospitals were breached compared with other types of healthcare
providers, such as doctors, nurses, and social workers. Therefore,
65
56
51
34
33
19
10
-
500,000
1,000,000
1,500,000
2,000,000
2,500,000
3,000,000
3,500,000
4,000,000
4,500,000
5,000,000
0
10
20
30
40
50
60
70
Paper/Films Other Laptop Email Desktop
Computer
EHR Network
Server
# of Individuals Affected
# of Hospitals
# Hospitals # Individuals Affected
200,150
445,411
380,669
226,240
740,072
44,805
4,613,858
FIGURE 1. US Hospital Data Breaches Affecting 500 or More Individuals
by Data Location, 2009-2016
EHR indicates electronic health record.
1 column
112
54
42
27
16
15
2
Theft Unauthorized
Access
Loss Hacking/
IT Incident
Improper
Disposal
Other
Unknown
-
1,000,000
2,000,000
3,000,000
4,000,000
500,000
1,500,000
2,500,000
3,500,000
4,500,000
5,000,000
0
20
40
60
80
100
120
# of Individuals Affected
Frequency
Frequency # Individuals Affected
1,161,476
345,318
283,209
4,685,426
47,971
126,198
1607
FIGURE 2. US Hospital Data Breaches Affecting 500 or More Individuals
by Type of Breach, 2009-2016
IT indicates information technology.

82
FEBRUARY 2018 www.ajmc.com
POLI CY
despite the the high level of hospital adoption of EHRs and the
federal incentives to do so,
7
the most common type of data breach
in hospitals occurred with paper records and lms. These paper
and lm breaches occurred mostly due to theft, improper disposal,
and unauthorized access. However, the overall number of patients
aected by these breaches was relatively small. Conversely, network
servers were found to be the least frequent location of data breaches,
but these breaches impacted the most patients overall. In addition,
this study found that there were large numbers of thefts of laptops,
which can easily be physically removed and stolen regardless of
EHR or biometric security system implementation. Adjusted results
showed signicant associations among data breach occurrences
and hospital characteristics, including type and size. Pediatric
hospitals and teaching hospitals were found to be at increased
risk for breaches. The presence of capability and infrastructure
support for biometrics and high health IT sophistication were not
signicantly associated with data breach risk.
Medical identity theft has long-lasting repercussions that can
aect an individual’s health and nancial well-being; it cannot be
remedied by closing an account, as one would do with a nancial
breach of a credit card number, for instance. Hospitals are vulner-
able to data breaches, but investment in data security is lacking.
12
Although hospital investments in technology have been implemented
to meet Meaningful Use and other federal requirements, protecting
digitized patient data has not been a central focus. The ndings of
this study point to a need to integrate security measures in areas
where patient information is kept to reduce the theft risk for both
paper les and computers with PHI.
As shown by the ndings of this study and others, computers
have served as a source of data breaches because generic usernames
and passwords make them easily accessible.
13,21
Hospital unit
computers are easy targets because they contain patient and sta
information, such as referral letters, nursing reports, patient charts,
audits, handovers, and sta sick leave lists, directly on the desktop.
Biometric technology is a valuable means of reducing username
and password reliance by utilizing ngerprint, gesture, eye, facial,
and voice recognition modalities. This is further strengthened via
2-factor authentication protocols, which often combine a username
and password with a physical biometric scan to grant access.
20,22
Given that the most common location of breaches in a hospital is
currently paper les/lms, the addition of biometric technology
is not likely to impact this number. However, as the diusion of
EHR technology continues in the United States and cyber threats
become more prevalent, these hard-copy breaches will presumably
continue to be minimized as long as necessary security policies are
upheld and security audits are practiced.
22,23
Previous studies have reviewed the characteristics of privacy
breaches, but little research has been done since the revision of
HIPAA in 2013.
5
This policy revision represented a signicant change
in the denition of what constitutes a breach and how covered
entities and their business associates operationalize the regulations.
As hospitals are now faced with additional evolving threats to PHI,
the impact of these breaches is a signicant concern.
11
An emerging
threat includes crypto-ransomware attacks on hospitals. Instead
of stealing and selling patient data, hackers are now locking down
entire systems and threatening to damage or disable computers
unless hospitals pay a ransom. Users have the option to attempt
to restore their system data from backups, lose the data, or pay the
TABLE 3. Predicting Factors of Large Data Breaches Affecting
500 or More Individuals Among US Hospitals, 2009-2016
a
Point Estimates and 95% CIs
Variable Estimate 95% CI
Area Characteristics
Rural Ref
Urban 0.705 0.401-1.238
Hospital Region
Northeast Ref
West 1.594 0.906-2.804
Midwest 1.265 0.729-2.197
South 1.179 0.697-1.997
Health System Membership (yes/no)
Health system membership 0.804 0.547-1.183
Hospital Size
Large bed size Ref
Medium bed size 0.601 0.382-0.946
Small bed size 0.313 0.168-0.584
Hospital Type
General medical and surgical Ref
Teaching hospital 5.028 2.989-8.459
Critical access hospital 1.553 0.815-2.957
Other specialty hospital 1.103 0.531-2.290
Pediatric hospital 5.103 2.550-10.215
Biometric Security Use (yes/no)
Biometric security use 1.122 0.806-1.561
Health IT Sophistication (high/low)
High health IT sophistication 0.907 0.631-1.303
Hospital Ownership
Not-for-profit Ref
Government, nonfederal 0.761 0.478-1.212
Investor-owned, for-profit 0.887 0.533-1.475
Market Competition (HHI)
Market competition 0.670 0.189-2.370
HHI indicates Herfindahl-Hirschman Index; IT, information technology;
Ref, reference.
a
Data source: HHS, Office for Civil Rights: Breaches affecting 500 or more
individuals; HIMSS Analytics Data 2015; and American Hospital Association
Health Information Technology Supplement 2015.

THE AMERICAN JOURNAL OF MANAGED CARE
®
VOL. 24, NO. 2
83
A False Sense of Security
requested ransom.
9,11,12
Healthcare policy under HIPAA has tried
to adapt quickly to these new threats; however, OCR addressed
the issue of ransomware attacks only relatively recently, through
guidance delivered in July 2016.
24
As annual hospital budgets are planned, including a line item for
information security will be important for many reasons, including
reputation.
25
A recent review found that, on average, healthcare
organizations are spending 95% of their IT budgets on attempts to
comply with federal initiatives, such as health IT implementation
and adoption, and only 5% on security.
13
Hospitals would be judi-
cious to include a compliance plan with consistent audits to verify
who is accessing patient information. In addition, it is critical that
hospital administrators support overall plans and penalties for
those sta members who deliberately and maliciously access patient
data outside of their job requirements. Access control to protected
patient data in larger facilities is dicult to manage and adds to the
vulnerability of patient information.
11
To protect patient information
and to keep in line with the Minimum Necessary Rule under HIPAA,
which states that PHI should not be used or disclosed unless neces-
sary,
26
it is important to maintain and enforce a policy of access to
the minimum necessary information for job performance. Finally,
the Health Care Industry Cybersecurity Task Force, established in
the Cybersecurity Act of 2015, has put forth guidance for hospitals to
improve cybersecurity.
27
They recommend that insurance companies
provide incentives specically for small- and medium-size healthcare
providers to transfer patient records to more secure environments.
In addition, hospitals may consider cyber-insurance policies, which
require security audits as a condition of coverage, to help protect
their facilities from breaches and ransomware attacks.
12,27
Limitations
Although many aspects surrounding healthcare privacy and data
breaches were included in this study, not all could be accounted for.
One limitation was that the OCR only had data available on breaches
that aect 500 or more patients per case. Information on breaches
and the at-fault facilities for all breaches aecting 499 patients or
less was not accessible. In addition, the policy language around
what is considered reportable in privacy breaches is vague, so these
occurrences may have been under- or over-reported depending
on the individual facility. The OCR data did not give specic dates
and months of data breaches, only the year, and the 2016 data were
not all available when we conducted the analysis. In addition, the
survey questions used to measure biometric security systems only
measured capability and infrastructure support and did not reect
use. Furthermore, all data used for this analysis were self-reported.
Not all hospitals in the OCR database could be matched to the
HIMSS and AHA analytics data les due to the possibility of facility
closure, unveried city of breach, or inadequate information. In
total, 15 hospitals were unable to be matched. VA hospitals were
also unable to be matched because HIMSS does not monitor VA
information. This study focused on hospitals due to the number
of individuals aected by breaches in these types of facilities.
However, other types of facilities, including physician practices,
health plans, and clearinghouses, do have breaches and should be
an area of focus for future research. Finally, it is important to note
that most states have passed additional legislation that is more or
less strict than the current federal iteration, which may or may not
impact breach reporting.
28
CONCLUSIONS
Although there are more group/physician practices within the United
States than hospitals, the overall number of individual patients
treated, and who thus have data created and stored within the
record system, is greater within hospitals. Routine audits required
by cyber-insurance coverage may help healthcare facilities recognize,
and repair, their vulnerabilities before a breach occurs. Accordingly,
information security systems should be concurrently implemented
alongside health information technologies. Improving access
control and prioritizing patient privacy will be important steps in
minimizing future breaches.
n
Author Aliations: College of Health and Public Aairs, University of
Central Florida (MHG, AW, AN, KCW), Orlando, FL; United States Air Force
(AR), Joint Base Charleston, SC.
Source of Funding: None.
Author Disclosures: The authors report no relationship or nancial
interest with any entity that would pose a conict of interest with the
subject matter of this article.
Authorship Information: Concept and design (MHG, AN, AR, AW, KCW);
acquisition of data (AR, MHG); analysis and interpretation of data (MHG,
AN, AR, KCW); drafting of the manuscript (MHG, AR, AW); critical revision
of the manuscript for important intellectual content (MHG, AN, AR, AW,
KCW); statistical analysis (MHG, AR); administrative, technical, or logistic
support (KCW); and supervision (AR, MHG).
Address Correspondence to: Meghan Hufstader Gabriel, PhD, University
of Central Florida, 4364 Scorpius St, HPAII, Rm 213, Orlando, FL 32816. Email:
REFERENCES
1. Dezenhall E. A look back at the Target breach. HuffPost. April 6, 2015. huffingtonpost.com/eric-dezenhall/a-
look-back-at-the-target_b_7000816.html. Accessed July 22, 2016.
2. Anwar M, Joshi J, Tan J. Anytime, anywhere access to secure, privacy-aware healthcare services: issues,
approaches and challenges. Health Policy Technol. 2015;4(4):299-311. doi: 10.1016/j.hlpt.2015.08.007.
3. Liginlal D, Sim I, Khansa L, Fearn P. HIPAA privacy rule compliance: an interpretive study using Norman’s
action theory. Computers & Security. 2012;31(2):206-220. doi: 10.1016/j.cose.2011.12.002.
4. Heubusch K. Little breaches: OCR releases first “small breach” data. J AHIMA. 2011;82(10):56-57.
5. Wilder M, Bennett B, Bianchi M, Peters N. HHS issues new HITECH/HIPAA rule: top ten changes. Hogan
Lovells website. ehoganlovells.com/cv/07d443ca1b960fd9814fc6ae023b59c3661538c5. Published January 22,
2013. Accessed July 22, 2016.
6. LaTour KM, Eichenwald-Maki S, eds. Health Information Management: Concepts, Principles, and Practice.
Chicago, IL: American Health Information Management Association; 2006.
7. Henry J, Pylypchuck Y, Searcy Y, Patel V. Adoption of electronic health record systems among U.S. non-
federal acute care hospitals: 2008-2015. ONC data brief no. 35. Office of the National Coordinator for Health
Information Technology website. dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-
hospital-ehr-adoption-2008-2015.php. Published May 2016. Accessed September 1, 2016.
8. Adler-Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in US hospitals:
progress continues, but challenges persist. Health Aff (Millwood). 2015;34(12):2174-2180.
doi: 10.1377/hlthaff.2015.0992.
9. Sittig DF, Singh H. A socio-technical approach to preventing, mitigating, and recovering from ransomware
attacks. Appl Clin Inform. 2016;7(2):624-632. doi: 10.4338/ACI-2016-04-SOA-0064.

84
FEBRUARY 2018 www.ajmc.com
POLI CY
10. Pal S, Biswas B, Mukhopadhyay A. Can HIT work alone? a security and socio-economic perspective of
healthcare quality. Social Science Research Network website. papers.ssrn.com/sol3/papers.cfm?abstract_
id=2740951. Published February 23, 2016. Accessed July 22, 2016.
11. Yaraghi N. A health hack wake-up call. U.S. News & World Report. April 1, 2016. usnews.com/opinion/blogs/
policy-dose/articles/2016-04-01/ransomware-hacks-are-a-hospital-health-it-wake-up-call. Accessed July
22, 2016.
12. Yaraghi N. Hackers, phishers, and disappearing thumb drives: lessons learned from major health care
data breaches. Brookings Institution website. brookings.edu/research/papers/2016/05/05-health-care-data-
breaches-yaraghi. Published May 5, 2016. Accessed July 14, 2016.
13. Kruse CS, Frederick B, Jacobson T, Monticone DK. Cybersecurity in healthcare: a systematic review of
modern threats and trends. Technol Health Care. 2017;25(1):1-10. doi: 10.3233/THC-161263.
14. Blanke SJ, McGrady E. When it comes to securing patient health information from breaches, your
best medicine is a dose of prevention: a cybersecurity risk assessment checklist. J Healthc Risk Manag.
2016;36(1):14-24. doi: 10.1002/jhrm.21230.
15. Liu V, Musen MA, Chou T. Data breaches of protected health information in the United States. JAMA.
2015;313(14):1471-1473. doi: 10.1001/jama.2015.2252.
16. Gabriel M, Charles D, Henry J, Wilkins TL. State and national trends of two-factor authentication for non-
federal acute care hospitals. ONC data brief no. 32. Office of the National Coordinator for Health Information
Technology website. healthit.gov/sites/default/files/briefs/oncdatabrief32_two-factor_authent_trends.pdf.
Published November 2015. Accessed September 1, 2016.
17. HHS Office for Civil Rights. How OCR enforces the HIPAA privacy & security rules. HHS website. hhs.gov/
hipaa/for-professionals/compliance-enforcement/examples/how-OCR-enforces-the-HIPAA-privacy-and-
security-rules/index.html. Published 2011. Accessed February 2, 2016.
18. HHS Office for Civil Rights. Breach portal: notice to the secretary of HHS breach of unsecured protected
health information. HHS website. ocrportal.hhs.gov/ocr/breach/breach_report.jsf. Accessed September 1, 2016.
19. AHA healthcare IT database: a supplement to the AHA annual survey of hospitals. American Hospital
Association website. aha.org/research/rc/stat-studies/data-and-directories.shtml. Published January 2016.
Accessed September 1, 2016.
20. Furukawa MF, Patel V, Charles D, Swain M, Mostashari F. Hospital electronic health information exchange
grew substantially in 2008-12. Health Aff (Millwood). 2013;32(8):1346-1354. doi: 10.1377/hlthaff.2013.0010.
21. Data by region. The Dartmouth Atlas of Healthcare website. www.dartmouthatlas.org/data/region. Accessed
July 22, 2016.
22. Claunch D, McMillan M. Determining the right level for your IT security investment. Healthc Financ Manage.
2013;67(5):100-103.
23. Kwon J, Johnson ME. Security practices and regulatory compliance in the healthcare industry. J Am Med
Inform Assoc. 2013;20(1):44-51. doi: 10.1136/amiajnl-2012-000906.
24. Thiemann T. Picking the right path to mobile biometric authentication. Biometric Technology Today.
2016;2016(2):5-8. doi: 10.1016/S0969-4765(16)30034-0.
25. Hoppszallern S. Skimping on IT security is costly. Hospitals & Health Networks. May 13, 2014. hhnmag.com/
articles/4221-skimping-on-it-security-is-costly. Accessed September 1, 2016.
26. Sethi N, Lane G, Newton S, Egan P, Ghosh S. Disaster easily averted? data confidentiality and the hospital
desktop computer. Int J Med Inform. 2014;83(5):385-391. doi: 10.1016/j.ijmedinf.2014.02.002.
27. Health Care Industry Cybersecurity Task Force. Report on improving cybersecurity in the health care indus-
try. HHS Public Health Emergency website. phe.gov/Preparedness/planning/CyberTF/Documents/report2017.pdf.
Published June 2017. Accessed July 20, 2017.
28. Lopez VJ. Health data privacy: how states can fill the gaps in HIPAA. University of San Francisco Law Review.
2016. heinonline.org/HOL/LandingPage?handle=hein.journals/usflr50&div=17&id=&page=. Accessed July 22, 2016.
Full text and PDF at www.ajmc.com
