
MACStats:
Medicaid and
CHIP Data Book
DECEMBER 2023
Medicaid and CHIP Payment
and Access Commission

About MACPAC
The Medicaid and CHIP Payment and Access Commission (MACPAC) is a non-partisan legislative branch
agency that provides policy and data analysis and makes recommendations to Congress, the Secretary
of the U.S. Department of Health and Human Services, and the states on a wide array of issues aecting
Medicaid and the State Children’s Health Insurance Program (CHIP). The U.S. Comptroller General appoints
MACPAC’s 17 commissioners, who come from diverse regions across the United States and bring broad
expertise and a wide range of perspectives on Medicaid and CHIP.
MACPAC serves as an independent source of information on Medicaid and CHIP, publishing issue
briefs and data reports throughout the year to support policy analysis and program accountability.
The Commission’s authorizing statute, Section 1900 of the Social Security Act, outlines a number of areas
for analysis, including:
• payment;
• eligibility;
• enrollment and retention;
• coverage;
• access to care;
• quality of care; and
• the programs’ interaction with Medicare and the health care system generally.
MACPAC’s authorizing statute also requires the Commission to submit reports to Congress by March 15
and June 15 of each year. In carrying out its work, the Commission holds public meetings and regularly
consults with state ocials, congressional and executive branch sta, beneciaries, health care providers,
researchers, and policy experts.

MACStats:
Medicaid and
CHIP Data Book
DECEMBER 2023
Medicaid and CHIP Payment
and Access Commission

MACStats: Medicaid and CHIP Data Book
v
Commission Members and Terms
Commission Members and Terms
Melanie Bella, MBA, Chair
Philadelphia, PA
Robert Duncan, MBA, Vice Chair
Prospect, CT
Term Expires April 2024
Verlon Johnson, MPA
Acentra Health
Olympia Fields, IL
John B. McCarthy, MPA
Speire Healthcare Strategies
Nashville, TN
Katherine Weno, DDS, JD
Independent Public Health Consultant
Iowa City, IA
Heidi L. Allen, PhD, MSW
Columbia University School of Social Work
New York, NY
Melanie Bella, MBA
Cressey & Company
Philadelphia, PA
Robert Duncan, MBA
Connecticut Children’s–Hartford
Prospect, CT
Term Expires April 2025
Sonja L. Bjork, JD
Partnership HealthPlan of California
Faireld, CA
Tricia Brooks, MBA
Georgetown University Center for Children
and Families
Bow, NH
Jennifer L. Gerstor, FSA, MAAA
Milliman
Seattle, WA
Angelo P. Giardino, MD, PhD, MPH
The University of Utah
Salt Lake City, UT
Dennis Heaphy, MPH, MEd, MDiv
Massachusetts Disability Policy Consortium
Boston, MA
Rhonda M. Medows, MD
Renton, WA
Term Expires April 2026
Timothy Hill, MPA
American Institutes for Research
Columbia, MD
Carolyn Ingram, MBA
Molina Healthcare, Inc.
Santa Fe, NM
Patti Killingsworth
CareBridge
Nashville, TN
Adrienne McFadden, MD, JD
Buoy Health, Inc.
Tampa, FL
Jami Snyder, MA
JSN Strategies, LLC
Phoenix, AZ

December 2023
vi
Commission Sta
Commission Sta
Kate Massey, MPA, Executive Director Kiswana Williams, Executive Assistant
Communications
Caroline Broder, Director of Communications
Carolyn Kaneko, Graphic Designer
Melanie Raible-Tocci, Communications Specialist
Policy Directors
Kirstin Blom, MIPA
Policy Director
Joanne Jee, MPH
Policy Director and Congressional Liaison
Chris Park, MS
Policy Director and Data Analytics Advisor
Principal Analysts
Martha Heberlein, MA
Principal Analyst and Research Advisor
Robert Nelb, MPH
Aaron Pervin, MPH
Principal Analyst and Contracting Ocer
Melinda Becker Roach, MS
Melissa Schober, MPM
Amy Zettle, MPP
Senior Analysts
Asmaa Albaroudi, MSG
Lesley Baseman, MPH
Tamara Huson, MSPH
Linn Jennings, MS
Audrey Nuamah, MPH
Analysts
Drew Gerber, MPH Jerry Mi
Research Assistants
Gabby Ballweg Ava Williams
Operations and Finance
Annie Andrianasolo, MBA,
Chief Administrative Ocer
Nick Ngo, Chief Information Ocer
Kevin Ochieng, Senior IT Specialist
Steve Pereyra, Financial Management Analyst
Ken Pezzella, CGFM, Chief Financial Ocer
Erica Williams, Human Resources Specialist

MACStats: Medicaid and CHIP Data Book
vii
Table of Contents
Table of Contents
Commission Members and Terms .............................................................................................................v
Commission Staff .....................................................................................................................................vi
Introduction ............................................................................................................................................... xi
SECTION 1: Overview—Key Statistics ................................................................................................. 1
Key Points .............................................................................................................................................2
EXHIBIT 1. Medicaid and CHIP Enrollment as a Percentage of the U.S. Population,
2022 (millions) ......................................................................................................................3
EXHIBIT 2. Characteristics of Non-Institutionalized Individuals by Age and Source
of Health Coverage, 2022 ....................................................................................................4
EXHIBIT 3. National Health Expenditures by Type and Payer, 2021 ...................................................... 9
EXHIBIT 4. Major Health Programs and Other Components of Federal Budget as
a Share of Federal Outlays, FYs 1965–2022 ..................................................................... 12
EXHIBIT 5. Medicaid as a Share of States’ Total Budgets and State-Funded Budgets,
SFY 2021 ........................................................................................................................... 14
EXHIBIT 6. Federal Medical Assistance Percentages and Enhanced FMAPs by State,
FYs 2021–2024 .................................................................................................................. 17
SECTION 2: Trends ................................................................................................................................21
Key Points ...........................................................................................................................................22
EXHIBIT 7. Medicaid Beneciaries (Persons Served) by Eligibility Group,
FYs 1975–2021 (thousands) ..............................................................................................23
EXHIBIT 8. Medicaid Enrollment and Spending, FYs 1972–2022 ........................................................ 25
EXHIBIT 9. Annual Growth in Medicaid Enrollment and Spending, FYs 1982–2022 ........................... 26
EXHIBIT 10. Medicaid Enrollment and Total Spending Levels and Annual Growth,
FYs 1972–2022 ..................................................................................................................27
EXHIBIT 11. Full-Benet Medicaid and CHIP Enrollment, Selected Months in 2013–2023 ...................29
EXHIBIT 12. Historical and Projected National Health Expenditures by Payer for Selected
Years, CYs 1970–2031 .......................................................................................................32

December 2023
viii
Table of Contents
EXHIBIT 13. Medicaid as a Share of State Budgets Including and Excluding Federal Funds,
SFYs 1995 –2021 ...............................................................................................................34
SECTION 3: Program Enrollment and Spending ............................................................................... 37
Key Points ...........................................................................................................................................38
EXHIBIT 14. Medicaid Enrollment by State, Eligibility Group, and Dually Eligible Status,
FY 2021 (thousands) .......................................................................................................... 39
EXHIBIT 15. Medicaid Full-Year Equivalent Enrollment by State and Eligibility Group,
FY 2021 (thousands) ..........................................................................................................42
EXHIBIT 16. Medicaid Spending by State, Category, and Source of Funds,
FY 2022 (millions) ..............................................................................................................45
EXHIBIT 17. Total Medicaid Benet Spending by State and Category,
FY 2022 (millions) ..............................................................................................................48
EXHIBIT 18. Distribution of Medicaid Benet Spending by Eligibility Group and
Service Category, FY 2021 ................................................................................................ 51
EXHIBIT 19. Medicaid Benet Spending Per Full-Year Equivalent Enrollee (FYE)
by Eligibility Group and Service Category, FY 2021 .......................................................... 52
EXHIBIT 20. Distribution of Medicaid Enrollment and Benet Spending by Users
and Non-Users of Long-Term Services and Supports, FY 2021 .......................................53
EXHIBIT 21. Medicaid Spending by State, Eligibility Group, and Dually Eligible Status,
FY 2021 (millions)...............................................................................................................54
EXHIBIT 22. Medicaid Benet Spending Per Full-Year Equivalent Enrollee (FYE)
by State and Eligibility Group, FY 2021 .............................................................................57
EXHIBIT 23. Medicaid Benet Spending per Full-Year Equivalent Enrollee for
Newly Eligible Adult and All Enrollees by State, FY 2022 ..................................................60
EXHIBIT 24. Medicaid Supplemental Payments to Hospital Providers by State,
FY 2022 (millions) ..............................................................................................................63
EXHIBIT 25. Medicaid Supplemental Payments to Non-Hospital Providers by State,
FY 2022 (millions) ..............................................................................................................65
EXHIBIT 26. Medicaid Gross Spending for Drugs by Delivery System and Brand
or Generic Status, FY 2022 (millions) ................................................................................68
EXHIBIT 27. Medicaid Drug Prescriptions by Delivery System and Brand or
Generic Status, FY 2022 (thousands) ................................................................................ 71

MACStats: Medicaid and CHIP Data Book
ix
Table of Contents
EXHIBIT 28. Medicaid Gross Spending and Rebates for Drugs by Delivery System,
FY 2022 (millions) .............................................................................................................. 74
EXHIBIT 29. Percentage of Medicaid Enrollees in Managed Care by State, July 1, 2021 .....................77
EXHIBIT 30. Percentage of Medicaid Enrollees in Managed Care by State and
Eligibility Group, FY 2021 ...................................................................................................80
EXHIBIT 31. Total Medicaid Administrative Spending by State and Category,
FY 2022 (millions) ..............................................................................................................85
EXHIBIT 32. Child Enrollment in CHIP and Medicaid by State, FY 2022 (thousands) ...........................88
EXHIBIT 33. CHIP Spending by State, FY 2022 (millions) .....................................................................90
EXHIBIT 34. Federal CHIP Allotments, FYs 2021–2023 (millions) .........................................................93
SECTION 4: Medicaid and CHIP Eligibility ......................................................................................... 95
Key Points ...........................................................................................................................................96
EXHIBIT 35. Medicaid and CHIP Income Eligibility Levels as a Percentage of the FPL
for Children and Pregnant Women by State, July 2023 ..................................................... 97
EXHIBIT 36. Medicaid Income Eligibility Levels as a Percentage of the Federal Poverty
Level for Non-Aged, Non-Disabled, Non-Pregnant Adults by State, July 2023 ...............100
EXHIBIT 37. Medicaid Income Eligibility Levels as a Percentage of the Federal Poverty
Level for Individuals Age 65 and Older and Persons with Disabilities
by State, 2023 ..................................................................................................................103
EXHIBIT 38. Income as a Percentage of the Federal Poverty Level (FPL) for Various
Family Sizes, 2023 ........................................................................................................... 106
SECTION 5: Beneciary Health, Service Use, and Access to Care ...............................................109
Key Points ......................................................................................................................................... 110
EXHIBIT 39. Coverage, Demographic, and Health Characteristics of Non-Institutionalized
Individuals Age 0–18 by Primary Source of Health Coverage, 2022 ................................111
EXHIBIT 40. Use of Care among Non-Institutionalized Individuals Age 0–18 by Primary
Source of Health Coverage, 2022, NHIS Data ................................................................ 115
EXHIBIT 41. Use of Care among Non-Institutionalized Individuals Age 0–18 by Primary
Source of Health Coverage, 2021, MEPS Data ............................................................... 117
EXHIBIT 42. Measures of Access to Care among Non-Institutionalized Individuals
Age 0–18 by Primary Source of Health Coverage, 2022, NHIS Data .............................. 119

December 2023
x
Table of Contents
EXHIBIT 43. Access to and Experience of Care among Non-Institutionalized Individuals
Age 0–18 by Primary Source of Health Coverage, 2021, MEPS Data ............................ 121
EXHIBIT 44. Coverage, Demographic, and Health Characteristics of Non-Institutionalized
Individuals Age 19–64 by Primary Source of Health Coverage, 2022 ............................ 123
EXHIBIT 45. Use of Care among Non-Institutionalized Individuals Age 19–64 by Primary
Source of Health Coverage, 2022, NHIS Data ................................................................ 129
EXHIBIT 46. Use of Care among Non-Institutionalized Individuals Age 19–64 by Primary
Source of Health Coverage, 2021, MEPS Data ............................................................... 132
EXHIBIT 47. Measures of Access to Care among Non-Institutionalized Individuals
Age 19–64 by Primary Source of Health Coverage, 2022, NHIS Data ........................... 135
EXHIBIT 48. Access to and Experience of Care among Non-Institutionalized Individuals
Age 19–64 by Primary Source of Health Coverage, 2021, MEPS Data .......................... 137
SECTION 6: Technical Guide to MACStats .......................................................................................141
Interpreting Medicaid and CHIP Enrollment and Spending Numbers ...................................................... 143
Understanding Data on Health and Other Characteristics of Medicaid and CHIP Populations ............... 145
Methodology for T-MSIS Analysis ............................................................................................................ 146
EXHIBIT 49. MACPAC Assignment of T-MSIS Eligibility Groups ......................................................... 147
Methodology for Adjusting Benet Spending Data ................................................................................... 148
EXHIBIT 50. Medicaid Benet Spending in T-MSIS and CMS-64 Data by State,
FY 2021 (millions).............................................................................................................150
EXHIBIT 51. Service Categories Used to Adjust FY 2021 Medicaid Benet Spending in
T-MSIS to Match CMS-64 Totals ..................................................................................... 152
Understanding Managed Care Enrollment and Spending Data ............................................................... 155
Endnotes .........................................................................................................................................156

MACStats: Medicaid and CHIP Data Book
xi
Introduction
Introduction
This 2023 edition of the MACStats: Medicaid and
CHIP Data Book presents the most current data
available on Medicaid and the State Children’s Health
Insurance Program (CHIP), two programs that provide
a safety net for low-income populations who otherwise
would not have access to health care coverage and
that cover services other payers often do not cover.
The MACStats data book compiles the broad range of
Medicaid and CHIP statistics that MACPAC regularly
updates on macpac.gov into a single, end-of-year
publication. Our purpose is to bring together in one
place federal and state data on Medicaid and CHIP
that come from multiple data sources and are often
dicult to nd.
The data book provides context for understanding
these programs and how they t in the larger health
care system. Medicaid and CHIP covered more than
30 percent of the U.S. population in 2022 (Exhibit
1). Spending and enrollment in Medicaid typically
grow around recessions and slow when the economy
improves. As of July 2023, 91.5 million people were
enrolled in Medicaid and CHIP. While enrollment is
higher than July 2022, it has been decreasing from
its peak as states begin to disenroll beneciaries
following the end of the continuous coverage
requirement that was attached to the federal medical
assistance percentage (FMAP) increase under the
Families First Coronavirus Response Act (FFCRA, P.L.
116-127) (Exhibit 11).
Although the share of the federal budget devoted to
Medicaid and Medicare has grown steadily since the
programs were enacted in 1965, Medicaid and CHIP
spending combined continue to account for a small
share of the federal budget. In scal year (FY) 2022,
the share of federal spending on Medicaid and CHIP
increased from the prior scal year. This increase
reects both an increase in federal Medicaid spending
as enrollment and the federal share of Medicaid
increased under the provisions of the FFCRA, as well
as a large decrease in other federal spending related
to pandemic-related relief (Exhibit 4).
Total Medicaid spending was $830.6 billion in FY
2022 (Exhibit 16). Spending for CHIP was $22.3
billion (Exhibit 33). Medicaid spending increased 10.2
percent in FY 2022. This increase was largely driven by
increased enrollment under the continuous coverage
requirement during the public health emergency as
spending per full-year equivalent enrollee only increased
1.0 percent (Exhibit 10). In FY 2021, individuals eligible
on the basis of disability and enrollees age 65 and older
accounted for about 21 percent of Medicaid enrollees but
about 52 percent of program spending (Exhibits 14 and
21). Many of these individuals were users of long-term
services and supports.
MACStats continues to include tables on access to
and experience of care among non-institutionalized
individuals. These data show that Medicaid enrollees
were as likely to report not having diculty reaching
their usual medical provider by phone during business
hours as those covered by private insurance but
were more likely to report having a dicult time
reaching their usual medical provider after hours
for urgent medical needs compared to those with
private insurance (Exhibits 43 and 48). As in prior
years, Medicaid and CHIP enrollees of all ages were
more likely to be persons of color and to report fair
or poor health than individuals who were covered by
private insurance (Exhibit 2). Children whose primary
coverage source is Medicaid or CHIP are as likely to
report seeing a doctor or having a wellness visit within
the past year as those with private coverage and more
likely than those who are uninsured (Exhibit 40).
The pages that follow are divided into six sections:
•
an overview with key statistics on Medicaid and
CHIP;
•
trends in Medicaid spending, enrollment, and
share of state budgets;
•
Medicaid and CHIP enrollment and spending,
with information presented by state, service
category, and eligibility group;
•
Medicaid and CHIP eligibility;
•
measures of beneciary health, use of services,
and access to care; and
•
a technical guide regarding data sources,
methods, and guidance for interpreting exhibits.
We would like to thank sta at the Centers for Medicare
& Medicaid Services and our contractors—the State
Health Access Data Assistance Center at the University
of Minnesota and Acumen, LLC—who provided insights
and assistance. We would also like to thank Lori
Michelle Ryan for providing copyediting services.


SECTION 1:
Overview—
Key Statistics

Section 1: Overview—Key Statistics
December 2023
2
Section 1: Overview—Key Statistics
Key Points
•
In 2022, more than 30 percent of the U.S. population was enrolled in Medicaid or the State
Children’s Health Insurance Program (CHIP) at some point during the year: 93.8 million in Medicaid
and 8.3 million in CHIP (Exhibit 1). About 39 percent of children had Medicaid or CHIP coverage in
2022 (Exhibit 2).
•
About 34 percent of individuals enrolled in Medicaid or CHIP in 2022 had family incomes below
100 percent of the federal poverty level (FPL). Over half of all individuals (53.5 percent) enrolled
in Medicaid or CHIP had incomes of less than 138 percent FPL, the threshold used to determine
eligibility for Medicaid in states that have expanded Medicaid to low-income adults (Exhibit 2).
•
Medicaid and CHIP enrollees of all ages were more likely to be in fair or poor health than
individuals who were covered by private insurance or who were uninsured (Exhibit 2).
•
Medicaid and CHIP together accounted for 17.8 percent of national health expenditures in calendar
year 2021, less than either Medicare (21.2 percent) or private insurance (28.5 percent) (Exhibit 3).
•
In general, the share of the federal budget devoted to Medicaid and Medicare has grown steadily
since the programs were enacted in 1965. In scal year (FY) 2022, the share of federal spending
on Medicaid and CHIP (9.7 percent) increased from the prior scal year (7.8 percent) due to the
increase in the federal medical assistance percentage (FMAP) and enrollment growth under the
continuous coverage requirement under the Families First Coronavirus Response Act (FFCRA, P.L.
116-127) as well as a large decrease in other federal spending related to pandemic-related relief
(Exhibit 4).
•
In FY 2022, Medicaid continued to account for a smaller share of the federal budget (9.4 percent)
than Medicare (11.9 percent) (Exhibit 4).
•
Medicaid spending as a share of state budgets varies depending on whether federal funds are
included. Considering only the state-funded portion of state budgets (i.e., the portion states must
nance on their own through taxes and other means), Medicaid’s share was 14.4 percent in state
scal year (SFY) 2021. When federal funds are included, Medicaid’s share was 26.8 percent in SFY
2021 (Exhibit 5).

MACStats: Medicaid and CHIP Data Book
3
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 1. Medicaid and CHIP Enrollment as a Percentage of the U.S. Population, 2022 (millions)
Population Ever during FY 2022 Point in time during FY 2022 Point in time during CY 2022
Estimates based on administrative data (CMS)
1
Survey data (NHIS)
2
Medicaid enrollees 93.8
3
87.1
3
Not available
CHIP enrollees 8.3
4
7.2
5
Not available
Totals for Medicaid and CHIP 102.0 94.3 63.8
U.S. Census Bureau data Survey data (NHIS)
2
U.S. population 333.6
6
332.9
6
326.8
Administrative and Census Bureau data Survey data (NHIS)
2
Medicaid and CHIP enrollment as a
percentage of U.S. population
30.6%
1
28.3% 19.5%
Notes: FY is scal year. CY is calendar year. NHIS is National Health Interview Survey. Excludes the territories. Medicaid and CHIP enrollment numbers can
vary for reasons including dierences in the sources of data (e.g., administrative records versus survey interviews), categories of individuals included in the data
(e.g., those receiving full versus limited benets, those who are living in the community versus an institution such as a nursing facility), and the enrollment period
examined (e.g., ever during the year versus at a point in time). For a more detailed discussion of enrollment numbers, see https://www.macpac.gov/macstats/data-
sources-and-methods/.
¹ Estimates based on administrative data are from Transformed Medicaid Statistical Information System (T-MSIS), CHIP Statistical Enrollment Data System
(SEDS), and the president’s budget. Medicaid and CHIP enrollment numbers obtained from administrative data include individuals who received limited benets
(e.g., emergency services only). Combining administrative totals from Medicaid and CHIP may cause some individuals to be double counted if they were enrolled
in both programs during the year. Overcounting of enrollees in the administrative data may occur for other reasons—for example, individuals may move and be
enrolled in two states’ Medicaid programs during the year. Excludes about 1.6 million individuals in the territories.
² NHIS data exclude individuals in active-duty military and in institutions such as nursing facilities; in addition, surveys such as the NHIS generally do not classify
limited benets as Medicaid or CHIP coverage, and respondents are known to underreport Medicaid and CHIP coverage.
³ Medicaid enrollment estimates based on administrative data are from MACPAC analysis of FY 2022 T-MSIS data as of February 2023.
⁴ CHIP enrollment estimates from administrative data in the ever-enrolled column are from MACPAC analysis of CHIP SEDS data (see Exhibit 32).
⁵ CHIP enrollment estimates from administrative data in the point-in-time column are from the FY 2024 president's budget.
⁶ The Census Bureau number in the ever-enrolled column was the estimated U.S. resident population as of September 2022 (the month with the largest count
in FY 2022); the number of residents ever living in the United States during the year is not available. The Census Bureau point-in-time number is the average
estimated monthly number of U.S. residents for FY 2022.
Sources: MACPAC, 2023, analysis of the following: T-MSIS data as of February 2023; CHIP SEDS data as of August 14, 2023; HHS, 2023, FY 2024 president's
budget for HHS, Baltimore, MD, https://www.hhs.gov/sites/default/les/fy-2024-budget-in-brief.pdf; NHIS data; and U.S. Census Bureau, 2023, Monthly population
estimates for the United States: April 1, 2020 to December 1, 2023 (NA-EST2022-POP) https://www2.census.gov/programs-surveys/popest/tables/2020-2022/
national/totals/NA-EST2022-POP.xlsx.

December 2023
4
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 2. Characteristics of Non-Institutionalized Individuals by Age and Source of Health Coverage, 2022
Characteristic
Selected coverage source at
time of interview, all ages
1
Selected coverage source at time of
interview, age 0–18
1
Total Medicare Private
2
Medicaid
or CHIP
3
Uninsured
4
Total Private
2
Medicaid
or CHIP
3
Uninsured
4
Total (percent distribution across
coverage sources)
5
100.0% 24.0% 60.8% 19.5% 8.6% 100.0% 54.7% 38.7% 4.2%
Coverage
Length of time with any coverage during year
Full year 89.2* 99.1* 96.7 96.3 – 94.6* 98.2 98.0 –
Part year 5.0* 0.9* 3.3 3.7 26.6* 3.1* 1.8 2.0 35.3*
No coverage during year 5.8* – – – 73.4* 2.3* – – 64.7*
Multiple coverage sources at time of interview
Yes, any Medicare and Medicaid/
CHIP combination
6
1.9* 10.2 – 9.7 – – – – –
Yes, any private and Medicaid/CHIP
combination
0.8* – 1.3* 4.2 – 1.9* 3.4* 4.8 –
Yes, any other combination 7.6* 40.6* 12.5* 1.2 – – – – –
No 89.7* 49.2* 86.2* 84.9 100.0* 98.1* 96.6* 95.2 100.0*
Demographics
Age
0–18 23.6* † 21.2* 46.7 11.7* 100.0 100.0 100.0 100.0
19–64 59.1* 13.2* 65.7* 45.9 86.9* – –
– –
65 or older
17.4* 86.7* 13.1* 7.4 1.4* – – – –
Gender
Male 49.2* 45.6 50.0* 44.1 56.3* 51.1 51.8 50.8 52.0
Female 50.8* 54.4 50.0* 55.9 43.7* 48.9 48.2 49.2 48.0
Race
Hispanic 19.1* 8.7* 13.8* 29.3 44.4* 25.6* 16.8* 36.3 43.0
White, non-Hispanic 59.6* 74.8* 67.3* 39.6 35.7* 51.0* 64.2* 34.0 41.2
Black, non-Hispanic 12.0* 10.4* 9.4* 20.0 12.7* 12.4* 7.5* 20.0 7.0*
Native Indian, non-Hispanic 0.8 † 0.5 † 1.4 † † † †
Asian, non-Hispanic 5.7 4.4 6.3 5.3 3.7* 4.6* 5.5* 3.3 5.0
Other single and multiple races,
non-Hispanic
2.8* 1.0* 2.7* 3.8 2.0* 5.4 5.6 4.9 †

MACStats: Medicaid and CHIP Data Book
5
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 2. (continued)
Characteristic
Selected coverage source at
time of interview, age 19–64
1
Selected coverage source at time of
interview, age 65 or older
1
Total Medicare Private
2
Medicaid
or CHIP
3
Uninsured
4
Total Medicare Private
2
Medicaid
or CHIP
3
Total (percent distribution
across coverage sources)
5
100.0% 4.2% 67.6% 15.2% 12.6% 100.0% 93.2% 45.7% 8.3%
Coverage
Length of time with any coverage during year
Full year 84.2* 97.9* 95.6* 94.2 – 98.6 99.2 99.5 98.5
Part year 7.1* 2.1* 4.4* 5.8 25.8* 0.8 0.8 † †
No coverage during year 8.7* – – – 74.2* 0.6* – – –
Multiple coverage sources at time of interview
Yes, any Medicare and Medicaid/
CHIP combination
6
1.3* 31.2* – 8.6 – 6.5* 7.0* – 78.4
Yes, any private and Medicaid/
CHIP combination
0.6* – 0.9* 4.1 – † – † †
Yes, any other combination 0.8 19.7* 1.2* 0.7 – 40.9* 43.8* 89.6* 11.6
No 97.2* 49.1* 97.9 86.6 100.0* 52.6* 49.2* 10.3 9.4
Demographics
Age
0–18 – – – – – – – – –
19–64 100.0 100.0 100.0 100.0 100.0 – – –
–
65 or older
– – – – – 100.0 100.0 100.0 100.0
Gender
Male 49.5* 50.0* 50.1* 38.1 57.3* 45.6* 44.9* 46.2* 38.8
Female 50.5* 50.0* 49.9* 61.9 42.7* 54.4* 55.1* 53.8* 61.2
Race
Hispanic 19.4* 12.1* 14.3* 22.9 44.0* 9.4* 8.2* 6.4* 25.9
White, non-Hispanic 58.6* 64.2* 65.5* 45.1 35.4* 74.6* 76.5* 81.7* 41.0
Black, non-Hispanic 12.6* 16.7 10.5* 20.2 13.6* 9.6* 9.5* 6.9* 18.5
American Indian or Alaska Native,
non-Hispanic
0.8 † 0.4 † 1.4 † † 0.4 †
Asian, non-Hispanic 6.4 3.9* 7.1 6.2 3.5* 5.0* 4.5* 3.6* 12.4
Other single and multiple races,
non-Hispanic
2.3* 2.3 2.2* 3.3 2.0* 0.8 0.8 1.0 †

December 2023
6
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 2. (continued)
Characteristic
Selected coverage source at
time of interview, all ages
1
Selected coverage source at time of
interview, age 0–18
1
Total Medicare Private
2
Medicaid
or CHIP
3
Uninsured
4
Total Private
2
Medicaid
or CHIP
3
Uninsured
4
Education
7
Less than high school 10.3%* 13.4%* 4.9%* 22.6% 25.7% – – – –
High school diploma/GED 27.0* 30.7* 22.5* 37.8 37.9 – – – –
Some college 29.6 28.6 29.9 30.0 24.5* – – – –
College or graduate degree 33.2* 27.3* 42.8* 9.5 11.9* – – – –
Marital status
7
Married 52.7* 55.1* 59.5* 28.6 37.4* – – – –
Widowed 5.9 19.0* 3.9* 5.8 2.0* – – – –
Divorced or separated 10.1* 14.6 8.2* 14.8 9.2* – – – –
Living with partner 9.0* 3.3* 8.1* 12.5 18.2* – – – –
Never married 22.3* 8.0* 20.3* 38.3 33.1* – – – –
Family income
Has income less than 138 percent FPL 18.8* 19.2* 6.1* 53.5 33.2* 25.3%* 5.4%* 53.8% 32.5%*
Has income in ranges shown below
Less than 100 percent FPL 11.0*
10.3* 3.1* 33.9
19.8* 15.4* 2.9* 33.2 21.6*
100–199 percent FPL 18.7* 22.1* 9.9* 38.2 30.6* 22.1* 9.2* 40.2 25.1*
200–399 percent FPL 29.1* 31.3* 29.7* 21.7 34.1* 29.0* 32.9* 21.7 37.6*
400 percent FPL or higher 41.2* 36.2* 57.2* 6.2 15.5* 33.5* 55.0* 4.9 15.7*
Other demographic characteristics
Citizen of United States 93.1 97.5* 95.6* 93.5 68.7* 97.1 98.5* 97.2 80.2*
Parent of a dependent child
7
26.4* 2.1* 27.7* 34.8 35.5 – – – –
Currently working
7
63.7* 16.6* 75.5* 44.3 71.5* – – – –
Veteran
7
7.7* 15.2* 5.8* 2.3 2.9 – – – –
Family receives SSI or SSDI 8.3* 17.6* 4.2* 20.1 5.0* 6.1* 2.5* 11.8 †
Health
Current health status
Excellent or very good 62.8* 39.8* 68.5* 56.8 58.7 86.0* 90.6* 79.1 81.1
Good 25.3 32.8* 23.7 25.1 28.7* 11.2* 7.9* 15.7 16.0
Fair or poor 11.9* 27.4* 7.9* 18.1 12.6* 2.8* 1.4* 5.1 †

MACStats: Medicaid and CHIP Data Book
7
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 2. (continued)
Characteristic
Selected coverage source at
time of interview, age 19–64
1
Selected coverage source at time of
interview, age 65 or older
1
Total Medicare Private
2
Medicaid
or CHIP
3
Uninsured
4
Total Medicare Private
2
Medicaid
or CHIP
3
Education
7
Less than high school 9.5%* 19.4% 4.2%* 20.0% 25.1%* 13.1%* 12.5%* 8.2%* 39.5%
High school diploma/GED 26.4* 39.6 21.4* 38.7 38.3 28.9 29.3 27.6* 32.2
Some college 29.9 28.1 30.2 31.3 24.7* 28.4* 28.7* 28.5* 21.5
College or graduate degree 34.2* 12.9* 44.2* 10.0 11.9 29.6* 29.5* 35.7* 6.7
Marital status
7
Married 51.2* 41.4* 58.5* 28.3 37.7* 57.5* 57.1* 64.8* 30.8
Widowed 1.7* 6.1* 1.2* 2.7 1.7* 20.3* 21.0 17.6* 24.9
Divorced or separated 9.0* 19.0* 7.6* 13.1 9.1* 13.9* 14.0* 11.0* 25.5
Living with partner 10.9* 7.0* 9.2* 13.8 18.3* 2.9 2.8 2.4* 4.7
Never married 27.3* 26.6* 23.5* 42.2 33.2* 5.4* 5.1* 4.2* 14.1
Family income
Has income less than 138 percent FPL 17.0* 40.5* 6.1* 51.8 33.3* 16.0* 16.0* 7.6* 62.4
Has income in ranges shown below
Less than 100 percent FPL 10.1* 24.4*
3.2* 33.3
19.5* 8.3* 8.2* 3.3* 42.3
100–199 percent FPL 16.9* 33.5 9.3* 36.6 31.2* 20.3* 20.4* 14.3* 34.6
200–399 percent FPL 28.3* 25.3 28.4* 22.3 33.6* 31.9* 32.2* 31.2* 17.7
400 percent FPL or higher 44.7* 16.8* 59.1* 7.8 15.7* 39.5* 39.2* 51.1* 5.4
Other demographic characteristics
Citizen of United States 90.4 95.9* 94.1* 90.6 67.7* 96.6* 97.7* 98.3* 86.4
Parent of a dependent child
7
34.0* 12.4* 33.1* 40.2 36.1* 0.7 0.5 0.9 †
Currently working
7
76.9* 16.4* 85.6* 50.2 72.3* 19.4* 16.6* 24.9* 7.9
Veteran
7
5.2* 6.9* 4.1* 2.0 2.9 16.3* 16.4* 14.6* 4.4
Family receives SSI or SSDI 8.8* 70.9* 4.3* 26.5 5.2* 9.4* 9.6* 6.3* 36.0
Health
Current health status
Excellent or very good 59.3* 17.8* 65.4* 40.0 56.2* 43.3* 43.1* 48.3* 20.1
Good
28.6*
29.6 27.0* 33.5 30.5 33.4 33.3 32.5 32.4
Fair or poor
12.1*
52.7* 7.7* 26.5 13.3* 23.3* 23.6* 19.2* 47.4

December 2023
8
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 2. (continued)
Notes: GED is general educational development test. FPL is federal poverty level. SSI is Supplemental Security Income. SSDI is Social Security Disability
Insurance. Percentage calculations for each item in the exhibit exclude individuals with missing and unknown values. Standard errors are available in the Excel
version of this exhibit at https://www.macpac.gov/publication/characteristics-of-non-institutionalized-individuals-by-source-of-health-insurance/. The individual
components listed under the subcategories are not always mutually exclusive and may not add to 100 percent. Due to dierences in methodology (such as the
wording of questions, length of recall periods, and prompts or probes used to elicit responses), estimates obtained from dierent survey data sources will vary.
For example, the National Health Interview Survey (NHIS) is known to produce higher estimates of service use than the Medical Expenditures Panel Survey
(MEPS). For purposes of comparing groups of individuals (as in this exhibit), the NHIS provides the most recent information available. For other purposes, such as
measuring levels of use relative to a particular benchmark or goal, it may be appropriate to consult estimates from MEPS or another source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
*Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
– Dash indicates zero.
1
Total includes all non-institutionalized individuals, regardless of coverage source. In this exhibit, the values across health insurance coverage types may not
sum to 100 percent for each age group because individuals may have multiple sources of coverage and because not all types of coverage are displayed. Other
MACStats exhibits apply a hierarchy to assign individuals with multiple coverage sources to a primary source and may therefore have dierent results than those
shown here. Coverage source is dened as of the time of the survey interview. Since an individual may have multiple coverage sources or changes over time,
responses to survey questions may reect characteristics or experiences associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state-sponsored or other government-
sponsored health plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or only a private plan that paid
for one type of service, such as accidents or dental care.
5
Components may not sum to 100 percent because individuals may have multiple sources of coverage and because not all types of coverage are displayed.
6
NHIS and other survey data underestimate the number of individuals dually enrolled in Medicare and Medicaid, in part because most surveys do not count those
whose only Medicaid benet is payment of Medicare premiums and cost sharing as having Medicaid coverage.
7
Information is limited to those age 19 or older.
Source: MACPAC, 2023, analysis of NHIS data.

MACStats: Medicaid and CHIP Data Book
9
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 3. National Health Expenditures by Type and Payer, 2021
Type of expenditure
Payer amount (millions) and share of total
Total Medicaid CHIP Medicare
Private
insurance
Other
health
insurance
1
Other
third-
party
payers
2
Out of
pocket
Total payer expenditures $4,255,127 $734,011 $22,254 $900,787 $1,211,431 $149,883 $803,608 $433,153
Hospital care 1,323,912 245,307 5,591 350,726 448,778 86,091 153,335 34,083
Physician and clinical services 864,563 99,332 4,874 222,082 328,077 38,768 105,860 65,570
Dental services 161,777 15,263 2,586 4,729 64,934 2,109 8,720 63,436
Other professional services
3
130,647 9,494 480 36,240 37,490 – 17,453 29,490
Home health care 125,195 42,788 64 46,583 15,926 698 6,242 12,895
Other non-durable medical products
4
97,387 – – 2,332 – – – 95,055
Prescription drugs 377,987 39,624 2,281 119,923 151,680 10,146 4,495 49,839
Durable medical equipment
5
67,126 9,102 222 12,357 13,087 – 984 31,374
Nursing care facilities and continuing
care retirement communities
6
181,314 54,267 18 40,589 16,281 6,796 18,972 44,391
Other health, residential, and
personal care services
7
223,479 129,641 1,966 4,302 14,773 924 64,852 7,020
Administration
8
307,106 89,191 4,172 60,925 120,405 4,350 28,062 –
Public health activity 187,604 – – – – – 187,604 –
Investment 207,031 – – – – – 207,029 –

December 2023
10
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 3. (continued)
Type of expenditure
Payer amount (millions) and share of total
Total Medicaid CHIP Medicare
Private
insurance
Other
health
insurance
1
Other
third-
party
payers
2
Out of
pocket
Total payer share of expenditures 100.0% 17.3% 0.5% 21.2% 28.5% 3.5% 18.9% 10.2%
Hospital care 100.0 18.5 0.4 26.5 33.9 6.5 11.6 2.6
Physician and clinical services 100.0 11.5 0.6 25.7 37.9 4.5 12.2 7.6
Dental services 100.0 9.4 1.6 2.9 40.1 1.3 5.4 39.2
Other professional services
3
100.0 7.3 0.4 27.7 28.7 – 13.4 22.6
Home health care 100.0 34.2 0.1 37.2 12.7 0.6 5.0 10.3
Other non-durable medical products
4
100.0 – – 2.4 – – – 97.6
Prescription drugs 100.0 10.5 0.6 31.7 40.1 2.7 1.2 13.2
Durable medical equipment
5
100.0 13.6 0.3 18.4 19.5 – 1.5 46.7
Nursing care facilities and continuing
care retirement communities
6
100.0 29.9 0.0 22.4 9.0 3.7 10.5 24.5
Other health, residential, and
personal care services
7
100.0 58.0 0.9 1.9 6.6 0.4 29.0 3.1
Administration
8
100.0 29.0 1.4 19.8 39.2 1.4 9.1 –
Public health activity 100.0 – – – – – 100.0 –
Investment 100.0 – – – – – 100.0 –
Notes: Every ve years National Health Expenditure Accounts undergo a comprehensive revision that includes the incorporation of newly available source data,
methodological and denitional changes, and benchmark estimates from the U.S. Census Bureau’s quinquennial Economic Census. The values shown here reect
the comprehensive revision made in 2019, and thus, the gures shown here may reect methodological and denitional shifts within payer and service categories
from prior publications of MACStats. For example, the 2019 methodology improved the allocation of Medicaid managed care premiums to the goods and services
categories for some states by the additional use of Medicaid Drug Rebate System data. This change caused a downward revision to retail prescription drug
spending and an upward revision for most of the other service categories.

MACStats: Medicaid and CHIP Data Book
11
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 3. (continued)
– Dash indicates zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
U.S. Department of Defense and U.S. Department of Veterans Aairs.
2
Includes all other public and private programs and expenditures except for out-of-pocket amounts.
3
The other professional services category includes services provided in establishments operated by health practitioners other than physicians and dentists,
including those provided by private-duty nurses; chiropractors; podiatrists; optometrists; and physical, occupational, and speech therapists.
4
The other non-durable medical products category includes the retail sales of non-prescription drugs and medical sundries.
5
The durable medical equipment category includes retail sales of items such as contact lenses, eyeglasses, and other ophthalmic products; surgical and
orthopedic products; hearing aids; wheelchairs; and medical equipment rentals.
6
The nursing care facilities and continuing care retirement communities category includes nursing and rehabilitative services provided in freestanding nursing
home facilities that are generally provided for an extended period of time by registered or licensed practical nurses and other sta.
7
The other health, residential, and personal care category includes spending for Medicaid home- and community-based waivers, care provided in residential
facilities for people with intellectual disabilities or mental health and substance abuse disorders, ambulance services, school health, and worksite health care.
8
The administrative category includes the administrative cost of health care programs (e.g., Medicare and Medicaid) and the net cost of private health insurance
(administrative costs as well as additions to reserves, rate credits and dividends, premium taxes, and plan prots or losses).
Sources: Oce of the Actuary (OACT), CMS, 2022, National health expenditures by type of service and source of funds: Calendar years 1960–2021, Baltimore,
MD: OACT, https://www.cms.gov/les/zip/national-health-expenditures-type-service-and-source-funds-cy-1960-2021.zip. OACT, 2022, National health expenditure
accounts: Methodology paper, 2021, Baltimore, MD: OACT, https://www.cms.gov/les/document/denitions-sources-and-methods.pdf. OACT, 2020, Summary
of 2019 comprehensive revision to the national health expenditure accounts, Baltimore, MD: OACT, https://www.cms.gov/les/document/summary-benchmark-
changes-2019.pdf.

December 2023
12
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 4. Major Health Programs and Other Components of Federal Budget as a Share of Federal Outlays,
FYs 1965–2022
Medicaid
Medicare
Social Security
Net interest
Discretionary,
non-defense
Discretionary,
defense
Other mandatory
programs
Exchang
e
subsidies
CHIP

MACStats: Medicaid and CHIP Data Book
13
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 4. (continued)
Fiscal year
Mandatory programs Discretionary programs
Net interest
Medicaid CHIP Medicare
Exchange
subsidies
Social
Security Other Defense
Non-
defense
1965
0.2% – – – 14.4% 12.3% 43.2% 22.6% 7.3%
1970
1.4 – 3.0% – 15.2 11.6 41.9 19.6 7.3
1975
2.1 – 3.7 – 19.1 20.6 26.4 21.2 7.0
1980
2.4 – 5.2 – 19.8 16.9 22.8 24.0 8.9
1985
2.4 – 6.8 – 19.7 13.5 26.7 17.2 13.7
1990
3.3 – 7.6 – 19.7 14.7 24.0 16.0 14.7
1995
5.9 – 10.4 – 22.0 10.5 18.0 17.9 15.3
2000
6.6 0.1% 10.9 – 22.7 13.0 16.5 17.9 12.5
2005
7.4 0.2 11.9 – 21.0 12.9 20.0 19.2 7.4
2006
6.8 0.2 12.2 – 20.5 13.4 19.6 18.7 8.5
2007
7.0 0.2 13.6 – 21.3 11.0 20.1 18.1 8.7
2008
6.8 0.2 12.9 – 20.5 13.0 20.5 17.5 8.5
2009
7.1 0.2 12.1 – 19.3 20.8 18.7 16.5 5.3
2010
7.9 0.2 12.9 – 20.3 14.1 19.9 19.0 5.7
2011
7.6 0.2 13.3 – 20.1 14.9 19.4 18.0 6.4
2012
7.1 0.3 13.2 – 21.8 15.2 19.0 17.2 6.2
2013
7.7 0.3 14.2 – 23.4 13.2 18.1 16.7 6.4
2014
8.6 0.3 14.4 0.4% 24.1 12.1 17.0 16.6 6.5
2015
9.5 0.3 14.6 0.7 23.9 13.2 15.8 15.9 6.0
2016
9.6 0.4 15.3 0.8 23.6 13.4 15.2 15.6 6.2
2017
9.4 0.4 14.9 1.0 23.6 14.0 14.8 15.3 6.6
2018
9.5 0.4 14.2 1.1 23.9 12.3 15.2 15.5 7.9
2019
9.2 0.4 14.5 1.1 23.4 13.0 15.2 14.9 8.4
2020
7.0 0.3 11.7 0.8 16.6 33.5 10.9 13.9 5.3
2021
7.6 0.2 10.1 0.9 16.5 35.4 10.9 13.1 5.2
2022
9.4 0.3 11.9 1.3 19.3 23.7 12.0 14.5 7.6
Notes: FY is scal year.
– Dash indicates zero.
Source: MACPAC, 2023, analysis of Oce of Management and Budget (OMB), Tables 6.1, 8.5, and 8.7, in Historical tables, budget of the United States
Government, scal year 2024, Washington, DC: OMB, https://www.govinfo.gov/app/details/BUDGET-2024-TAB/context.

December 2023
14
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 5. Medicaid as a Share of States’ Total Budgets and State-Funded Budgets, SFY 2021
State
Total budget (including state and federal funds) State-funded budget
Dollars
(millions)
Total spending as a share
of total budget
1
Dollars
(millions)
State-funded spending as a share
of state-funded budget
1
Medicaid
Elementary
and secondary
education
Higher
education Medicaid
Elementary
and secondary
education
Higher
education
Total $2,678,389 26.8% 18.7% 8.5% $1,585,532 14.4% 24.3% 12.2%
Alabama 31,918 24.0 19.9 19.8 19,303 8.9 27.8 26.1
Alaska 11,700 17.8 11.2 4.9 6,817 7.8 19.0 6.1
Arizona 66,826 24.0 10.9 11.1 50,556 6.1 11.4 12.5
Arkansas 31,052 26.1 12.8 12.2 18,727 8.4 16.6 20.2
California 498,883 22.7 18.0 4.9 226,589 16.8 28.2 7.9
Colorado 31,776 37.9 18.5 9.7 21,247 21.0 24.0 12.4
Connecticut 37,305 23.7 12.6 10.4 27,988 16.3 13.4 13.1
Delaware 13,257 19.5 22.1 3.6 9,301 8.1 27.9 4.4
District of Columbia 16,180 21.9 18.9 3.3 10,637 7.2 25.8 2.7
Florida 93,718 31.3 18.3 8.8 58,112 18.2 23.7 14.1
Georgia 64,286 21.0 28.5 16.7 39,581 9.1 28.0 25.7
Hawaii 24,401 11.5 9.6 5.4 19,150 4.6 9.9
6.8
Idaho 10,206 24.1 23.7 8.7 5,504 13.5 36.8 13.5
Illinois 115,535 22.5 11.3 1.9 88,855 10.3 11.0 2.3
Indiana 44,682 34.9 23.9 4.5 24,363 15.5 38.4 8.3
Iowa 28,522 23.2 15.6 23.1 18,102 12.8 19.8 33.0
Kansas 21,808 18.6 26.1 14.2 14,883 9.6 33.8 17.1
Kentucky 42,377 33.3 14.4 18.0 20,899 12.6 23.0 31.1
Louisiana 34,717 44.4 16.8 8.6 18,123 17.3 23.3 16.3
Maine 12,103 28.9 16.5 2.9 6,485 16.1 23.1 5.3
Maryland 55,058 21.5 18.0 13.0 33,313 12.0 23.5 17.5
Massachusetts 67,221 28.8 14.1 2.2 47,739 19.7 16.1 3.2
Michigan 68,420 31.1 23.4 3.7 38,325 14.5 35.5 6.3
Minnesota 48,019 28.8 24.0 3.9 30,011 17.9 33.4 6.3
Mississippi 22,231 24.4 15.8 18.1 11,948 8.7 21.5 31.1

MACStats: Medicaid and CHIP Data Book
15
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 5. (continued)
State
Total budget (including state and federal funds) State-funded budget
Dollars
(millions)
Total spending as a share
of total budget
1
Dollars
(millions)
State-funded spending as a share
of state-funded budget
1
Medicaid
Elementary
and secondary
education
Higher
education Medicaid
Elementary
and secondary
education
Higher
education
Missouri $29,779 37.5% 21.3% 4.3% $18,305 29.1% 27.4% 5.4%
Montana 11,133 20.5 10.1 6.2 5,187 8.9 17.8 13.0
Nebraska 15,067 19.1 12.3 20.5 9,986 10.5 13.6 25.0
Nevada 15,671 29.3 15.6 6.0 10,193 9.9 20.4 9.2
New Hampshire 7,535 32.1 18.1 2.0 3,953 22.8 29.3 3.8
New Jersey 78,706 22.9 25.1 8.5 54,250 10.4 28.8 11.9
New Mexico 24,727 29.0 16.0 12.5 12,185 10.2 27.5 20.4
New York 186,588 35.2 17.2 6.1 114,903 18.7 25.1 9.5
North Carolina 59,445 28.9 22.6 18.0 36,999 14.8 29.5 18.8
North Dakota 8,590 15.2 16.3 17.0 5,590 7.9 19.8 23.6
Ohio 81,216 39.3 15.9 4.0 46,865 18.2 22.0 6.2
Oklahoma 27,768 20.7 15.9 20.1 16,984 10.7 19.4 27.3
Oregon 66,771 16.7 10.0 3.5 44,586 5.9 13.1
5.1
Pennsylvania 103,258 36.6 18.3 2.0 60,200 23.7 22.5 3.4
Rhode Island 13,352 22.0 12.2 8.9 6,787 14.9 19.9 17.2
South Carolina 29,958 24.3 19.2 17.9 17,910 10.0 24.5 28.9
South Dakota 6,779 13.7 15.9 13.5 3,231 10.0 18.4 24.9
Tennessee 39,984 32.3 17.7 12.5 21,554 19.9 25.4 22.6
Texas 135,187 30.8 37.4 14.8 64,314 16.8 43.9 19.8
Utah 19,777 19.8 24.2 12.3 13,461 8.5 31.2 18.1
Vermont 7,290 22.6 29.8 2.4 4,028 14.6 48.1 3.2
Virginia 74,658 21.5 12.5 11.2 47,179 12.0 16.6 14.8
Washington 60,536 25.8 26.3 12.6 41,922 12.3 35.1 17.9
West Virginia 17,438 26.0 15.0 10.6 11,965 6.5 17.8 14.8
Wisconsin 59,355 21.3 15.2 11.7 41,782 12.9 19.2 12.3
Wyoming 5,620 11.2 16.2 6.5 4,654 6.2 19.6 7.9

December 2023
16
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 5. (continued)
Notes: SFY is state scal year. Total budget includes federal and all other funds. State-funded budget includes state general funds, other state funds, and bonds.
Other state funds are amounts from revenue sources that are restricted by law for particular government functions or activities, which for Medicaid includes
provider taxes and local funds. Medicaid, elementary and secondary education, and higher education represent the largest total budget shares among functions
broken out separately by the National Association of State Budget Ocers (NASBO). Functions not shown here are transportation, corrections, public assistance,
and all other (includes hospitals, economic development, housing environmental programs, CHIP, parks and recreation, natural resources, and air and water
transportation). Medicaid spending amounts exclude administrative costs but include Medicare Part D phased-down state contribution (also referred to as
clawback) payments.
1
Total and state-funded budget shares should be viewed with caution because they reect varying state practices. For example, in Ohio, federal reimbursements
for Medicaid expenditures funded from the General Revenue Fund (GRF) are deposited into the GRF. In prior reports, this practice made Ohio's general revenue
expenditures look higher and conversely made its federal expenditures look lower relative to most other states that do not follow this practice. In the 2019–2022
reports, NASBO removed the federal funds from the GRF number to be consistent with budget presentations in other NASBO surveys, and thus, Ohio's state-
funded Medicaid spending is less than what was reported in prior years. In addition, in many states, some functions—particularly elementary and secondary
education—may be partially funded outside of the state budget by local governments.
Source: NASBO, 2022, 2022 State expenditure report: scal years 2020–2022, Washington, DC: NASBO, https://www.nasbo.org/reports-data/state-expenditure-
report/state-expenditure-archives.

MACStats: Medicaid and CHIP Data Book
17
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 6. Federal Medical Assistance Percentages and Enhanced FMAPs by State, FYs 2021–2024
State
FMAPs for Medicaid
1
E-FMAPs for CHIP
FY 2021
(Emergency)
2, 3
FY 2022
(Emergency)
2, 3
FY 2023 Q1-2
(Emergency)
2, 4
FY 2023 Q3
(Emergency)
2, 4
FY 2023 Q4
(Emergency)
2, 4
FY 2024
5
FY 2021
(Emergency)
3, 6
FY 2022
(Emergency)
3, 6
FY 2023 Q1-2
(Emergency)
4, 6
FY 2023 Q3
(Emergency)
4, 6
FY 2023 Q4
(Emergency)
4, 6
FY 2024
5, 6
Alabama 78.78% 78.57% 78.63% 77.43% 74.93% 73.12% 85.15% 85.00% 85.04% 84.20% 82.45% 81.18%
Alaska 56.20 56.20 56.20 55.00 52.50 50.01 69.34 69.34 69.34 68.50 66.75 65.01
Arizona 76.21 76.21 75.76 74.56 72.06 66.29 83.35 83.35 83.03 82.19 80.44 76.40
Arkansas 77.43 77.82 77.51 76.31 73.81 72.00 84.20 84.47 84.26 83.42 81.67 80.40
California 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
Colorado 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34
69.34 68.50 66.75 65.00
Connecticut 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
Delaware 63.94 63.92 64.69 63.49 60.99 59.71 74.76 74.74 75.28 74.44 72.69 71.80
District of
Columbia
76.20 76.20 76.20 75.00 72.50 70.00 83.34 83.34 83.34 82.50 80.75 79.00
Florida 68.16 67.23 66.25 65.05 62.55 57.96 77.71 77.06 76.38 75.54 73.79 70.57
Georgia 73.23 73.05 72.22 71.02 68.52 65.89 81.26 81.14 80.55 79.71 77.96 76.12
Hawaii 59.22 59.84 62.26 61.06 58.56 58.56 71.45 71.89 73.58 72.74 70.99 70.99
Idaho 76.61 76.41 76.31 75.11 72.61 69.72 83.63 83.49 83.42 82.58 80.83 78.80
Illinois 57.16 57.29 56.20 55.00 52.50 51.09 70.01 70.10 69.34 68.50 66.75 65.76
Indiana 72.03 72.50 71.86 70.66 68.16 65.62 80.42 80.75 80.30 79.46 77.71 75.93
Iowa 67.95 68.34 69.33 68.13 65.63 64.13 77.57 77.84 78.53 77.69 75.94
74.89
Kansas 65.88 66.36 65.96 64.76 62.26 60.97 76.12 76.45 76.17 75.33 73.58 72.68
Kentucky 78.25 78.95 78.37 77.17 74.67 71.78 84.78 85.27 84.86 84.02 82.27 80.25
Louisiana 73.62 74.22 73.48 72.28 69.78 67.67 81.53 81.95 81.44 80.60 78.85 77.37
Maine 69.89 70.20 69.49 68.29 65.79 62.65 78.92 79.14 78.64 77.80 76.05 73.86
Maryland 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
Massachusetts 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
Michigan 70.28 71.68 70.91 69.71 67.21 64.94 79.20 80.18 79.64 78.80 77.05 75.46
Minnesota 56.20 56.71 56.99 55.79 53.29 51.49 69.34 69.70 69.89 69.05 67.30 66.04
Mississippi 83.96 84.51 84.06 82.86 80.36 77.27 88.77 89.16 88.84 88.00 86.25 84.09
Missouri 71.16 72.56 72.01 70.81 68.31 66.07 79.81 80.79 80.41 79.57 77.82 76.25
Montana 71.80 71.10
70.32 69.12 66.62 63.91 80.26 79.77 79.22 78.38 76.63 74.74
Nebraska 62.67 64.00 64.07 62.87 60.37 58.60 73.87 74.80 74.85 74.01 72.26 71.02

December 2023
18
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 1
EXHIBIT 6. (continued)
State
FMAPs for Medicaid
1
E-FMAPs for CHIP
FY 2021
(Emergency)
2, 3
FY 2022
(Emergency)
2, 3
FY 2023 Q1-2
(Emergency)
2, 4
FY 2023 Q3
(Emergency)
2, 4
FY 2023 Q4
(Emergency)
2, 4
FY 2024
5
FY 2021
(Emergency)
3, 6
FY 2022
(Emergency)
3, 6
FY 2023 Q1-2
(Emergency)
4, 6
FY 2023 Q3
(Emergency)
4, 6
FY 2023 Q4
(Emergency)
4, 6
FY 2024
5, 6
Nevada 69.50% 68.79% 68.85% 67.65% 65.15% 60.77% 78.65% 78.15% 78.20% 77.36% 75.61% 72.54%
New Hampshire 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
New Jersey 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
New Mexico 79.66 79.91 79.46 78.26 75.76 72.59 85.76 85.94 85.62 84.78 83.03 80.81
New York 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
North Carolina 73.60 73.85 73.91 72.71 70.21 65.91 81.52 81.70
81.74 80.90 79.15 76.14
North Dakota 58.60 59.79 57.75 56.55 54.05 53.82 71.02 71.85 70.43 69.59 67.84 67.67
Ohio 69.83 70.30 69.78 68.58 66.08 64.30 78.88 79.21 78.85 78.01 76.26 75.01
Oklahoma 74.19 74.51 73.56 72.36 69.86 67.53 81.93 82.16 81.49 80.65 78.90 77.27
Oregon 67.04 66.42 66.52 65.32 62.82 59.31 76.93 76.49 76.56 75.72 73.97 71.52
Pennsylvania 58.40 58.88 58.20 57.00 54.50 54.12 70.88 71.22 70.74 69.90 68.15 67.88
Rhode Island 60.29 61.08 60.16 58.96 56.46 55.01 72.20 72.76 72.11 71.27 69.52 68.51
South Carolina 76.83 76.95 76.78 75.58 73.08 69.53 83.78 83.87 83.75 82.91 81.16 78.67
South Dakota 64.48 64.89 62.94 61.74 59.24 54.98 75.14 75.42 74.06 73.22 71.47 68.49
Tennessee 72.30 72.56 72.30 71.10 68.60 65.28 80.61 80.79 80.61 79.77 78.02 75.70
Texas 68.01 67.00 66.07 64.87 62.37 60.15 77.61 76.90 76.25 75.41 73.66 72.11
Utah 73.72 73.03 72.10 70.90 68.40 65.90 81.60 81.12 80.47 79.63 77.88 76.13
Vermont 60.77 62.67 62.02 60.82 58.32 56.75 72.54 73.87 73.41 72.57 70.82 69.73
Virginia 56.20 56.20 56.85 55.65 53.15 51.22 69.34 69.34 69.80 68.96 67.21 65.85
Washington 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
West Virginia 81.19 80.88 80.22 79.02 76.52 74.10 86.83 86.62 86.15 85.31 83.56 81.87
Wisconsin 65.57 66.08 66.30 65.10 62.60 60.66 75.90 76.26 76.41 75.57 73.82 72.46
Wyoming 56.20 56.20 56.20 55.00 52.50 50.00 69.34 69.34 69.34 68.50 66.75 65.00
American
Samoa
7
89.20 89.20 89.20 88.00 85.50 83.00 92.44 92.44 92.44 91.60 89.85 88.10
Guam
7
89.20 89.20 89.20 88.00 85.50 83.00 92.44 92.44 92.44 91.60 89.85 88.10
N. Mariana
Islands
7
89.20 89.20 89.20 88.00 85.50 83.00 92.44 92.44 92.44 91.60 89.85 88.10
Puerto Rico
7
82.20 82.20 82.20 81.00 78.50 76.00 87.54 87.54 87.54 86.70 84.95 83.20
Virgin Islands
7
89.20 89.20 89.20 88.00 85.50 83.00 92.44 92.44 92.44 91.60 89.85 88.10

MACStats: Medicaid and CHIP Data Book
19
Section 1: Overview—Key Statistics
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 1
EXHIBIT 6. (continued)
Notes: FY is scal year. FMAP is federal medical assistance percentage. E-FMAP is enhanced FMAP. Q is quarter. The federal government’s share of most Medicaid service
costs is determined by the FMAP, with some exceptions. For Medicaid administrative costs, the federal share does not vary by state and is generally 50 percent. The E-FMAP
determines the federal share of both service and administrative costs for CHIP, subject to the availability of funds from a state’s federal allotments for CHIP.
FMAPs for Medicaid are generally calculated based on a formula that compares each state’s per capita income to U.S. per capita income and provides a higher federal match
for states with lower per capita incomes, subject to a statutory minimum (50 percent) and maximum (83 percent). The general formula for a given state is: FMAP = 1 – [(state
per capita income squared ÷ U.S. per capita income squared) × 0.45].
Medicaid exceptions to this formula include the District of Columbia (set in statute at 70 percent) and the territories (set in statute at 55 percent). Other Medicaid exceptions
apply to certain services, providers, or situations (e.g., services provided through an Indian Health Service facility receive an FMAP of 100 percent). E-FMAPs for CHIP are
calculated by reducing the state share under regular FMAPs for Medicaid by 30 percent.
1
For certain newly eligible individuals under the Medicaid expansion beginning in 2014, there is an increased FMAP (100 percent in 2014 through 2016, phasing down to 90
percent in 2020 and subsequent years). An increased FMAP is also available for certain states that expanded eligibility to low-income parents and non-pregnant adults without
children before enactment of the Patient Protection and Aordable Care Act (ACA, P.L. 111-148, as amended).
2
The Families First Coronavirus Response Act of 2020 (FFCRA, P.L. 116-127) provides a temporary 6.2 percentage point FMAP increase during a public health emergency for
each calendar quarter occurring during the period beginning on the rst day of the public health emergency period, as dened in Section 1135(g)(1)(B) of the Social Security Act
(the Act), and ending on the last day of the calendar quarter in which the last day of such emergency period occurs. The Secretary of the U.S. Department of Health and Human
Services declared a public health emergency on January 31, 2020, with an eective date of January 27, 2020, meaning the FMAP increase is eective January 1, 2020. States,
including the District of Columbia and the territories, must meet certain maintenance-of-eort requirements to qualify for the FMAP increase. The FMAP increase does not apply
to the Medicaid expansion population or other services such as those received at an Indian Health Service facility that already receive a higher matching rate.
3
Because the public health emergency period was in eect for all of FYs 2021 and 2022, this exhibit displays only the FY 2021 and 2022 FMAPs and E-FMAPs with the 6.2
percentage point increase under the FFCRA.
4
Section 5131(a) of the Consolidated Appropriations Act, 2023 (P.L. 117-328) subsequently amended the FFCRA to phase down the FMAP increase during calendar year
2023. For the quarter beginning April 1, 2023, and ending June 30, 2023 (Q3 of FY 2023), the FMAP increase is 5 percentage points. For the quarter beginning July 1, 2023,
and ending September 30, 2023, the FMAP increase is 2.5 percentage points (Q4 of FY 2023). For the quarter beginning October 1, 2023, and ending December 31, 2023 (Q1
for FY 2024), the FMAP increase is 1.5 percentage points. Section 5131(b) of the Consolidated Appropriations Act, 2023 added a new §1902(tt) of the Act that requires states
submit to CMS certain monthly data about activities related to eligibility redeterminations conducted during the period from April 1, 2023, to June 30, 2024. If a state does not
satisfy the reporting requirements in §1902(tt) during the period from July 1, 2023, to June 30, 2024, CMS shall reduce the FMAP for the state by the number of percentage
points (not to exceed 1 percentage point) equal to the product of 0.25 percentage points and the number of scal quarters during such period for which the state has failed to
satisfy the reporting requirements.
5
The FMAPs displayed for FY 2024 are the percentages that are in eect for January 1, 2024, to September 30, 2024. The FMAPs for the rst quarter of FY 2024 would
receive a 1.5 percentage point increase under the Consolidated Appropriations Act, 2023 (see footnote 4).
6
Because the E-FMAP in Section 2105(b) of the Act is calculated based on the FMAP, the E-FMAP is also higher for states, though not in the same amount, for the duration of
the public health emergency period.
7
Under numerous legislation that was subsequently consolidated under the Consolidated Appropriations Act, 2023 (P.L. 117-328), American Samoa, Guam, Northern Mariana
Islands, and the Virgin Islands receive an FMAP of 83 percent beginning December 21, 2019, and Puerto Rico receives an FMAP of 76 percent from December 21, 2019,
through December 3, 2021, and January 1, 2022, through September 30, 2027, but would receive its normal FMAP of 55 percent between December 4, 2021, and December
31, 2021. The E-FMAPs for FYs 2021–2024 were calculated o these increased FMAPs.
Sources: U.S. Department of Health and Human Services, Federal Register notices for FYs 2021–2024; Consolidated Appropriations Act, 2023 (P.L. 117-328);
Centers for Medicare & Medicaid Services, Families First Coronavirus Response Act – Increased FMAP FAQs, March 24, 2020, https://www.medicaid.gov/state-
resource-center/downloads/covid-19-section-6008-faqs.pdf; Center for Medicaid and CHIP Services, CMS, 2020, E-mail to MACPAC, March 27 and March 30.


SECTION 2:
Trends

December 2023
22
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
Section 2: Trends
Key Points
•
Medicaid spending and enrollment are aected by federal and state policy choices as well as
economic factors (Exhibits 8–10). For example:
– Spending and enrollment both grew around the recessions of 2001 and 2007 through 2009 and
then slowed as economic conditions improved.
– Large increases in Medicaid enrollment and spending in scal years (FYs) 2014 and 2015 were
primarily due to expanded eligibility under the Patient Protection and Aordable Care Act (ACA,
P.L. 111-148, as amended).
– Enrollment continues to increase since 2020 due to the continuous coverage requirement
attached to the federal medical assistance percentage (FMAP) increase under the Families
First Coronavirus Response Act (FFCRA, P.L. 116-127). From July 2022 to July 2023,
enrollment in Medicaid and the State Children’s Health Insurance Program (CHIP) increased
by 1.6 percent. While enrollment is higher than in 2022, it has been decreasing from its
peak as states begin to disenroll beneciaries following the end of the continuous coverage
requirement. Enrollment decreased in 20 states in 2022 (Exhibit 11).
•
Medicaid enrollment trends vary by eligibility group (Exhibit 7).
– Adults (excluding those eligible on the basis of disability) generally experience larger enrollment
increases during periods of economic recession than other eligibility groups. For example,
from FY 2008 through FY 2013, enrollment for adults grew on average 5.8 percent annually,
compared with 3.0 percent annually for children (excluding those eligible on the basis of
disability) and individuals qualifying for Medicaid on the basis of disability.
– Enrollment for adults has grown substantially due to the expansion of Medicaid under the ACA,
increasing at an average annual rate of 9.2 percent from FY 2013 through FY 2021.
– Individuals age 65 and older generally have the slowest growth rate regardless of time period.
•
Medicaid’s share of state-funded budgets (excluding federal funds) and total state budgets (including
federal funds) has varied over time. In state scal year 2015, Medicaid’s share of total state budgets
increased, but its share of state-funded budgets decreased slightly—the decrease can be attributed
to 100 percent federal funding made available for low-income adults not otherwise eligible on the
basis of disability, who became newly eligible for Medicaid under the ACA. Most recently, Medicaid’s
share of state-funded budgets has decreased from 2018 to 2021 due to additional states expanding
Medicaid and the FMAP increase under the FFCRA (Exhibit 13).
•
Medicaid and CHIP expenditures as a share of national health expenditures are projected to
decrease from 17.8 percent in 2021 to about 17.3 percent in 2031. Medicare’s share is projected to
increase from 21.2 percent to 25.8 percent during the same time period (Exhibit 12).

MACStats: Medicaid and CHIP Data Book
23
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
EXHIBIT 7. Medicaid Beneciaries (Persons Served) by Eligibility Group, FYs 1975–2021 (thousands)
Fiscal year Total Child Adult
1
Disabled Aged Unknown
1975 22,007 9,598 4,529 2,464 3,615 1,801
1976 22,815 9,924 4,773 2,669 3,612 1,837
1977 22,832 9,651 4,785 2,802 3,636 1,958
1978 21,965 9,376 4,643 2,718 3,376 1,852
1979 21,520 9,106 4,570 2,753 3,364 1,727
1980 21,605 9,333 4,877 2,911 3,440 1,044
1981 21,980 9,581 5,187 3,079 3,367 766
1982 21,603 9,563 5,356 2,891 3,240 553
1983 21,554 9,535 5,592 2,921 3,372 134
1984 21,607 9,684 5,600 2,913 3,238 172
1985 21,814 9,757 5,518 3,012 3,061 466
1986 22,515 10,029 5,647 3,182 3,140 517
1987 23,109 10,168 5,599 3,381 3,224 737
1988 22,907 10,037 5,503 3,487 3,159 721
1989 23,511 10,318 5,717 3,590 3,132 754
1990 25,255 11,220 6,010 3,718 3,202 1,105
1991 27,967 12,855 6,703 4,033 3,341 1,035
1992 31,150 15,200 7,040 4,487 3,749 674
1993 33,432 16,285 7,505 5,016 3,863 763
1994 35,053 17,194 7,586 5,458 4,035 780
1995 36,282 17,164 7,604 5,858 4,119 1,537
1996 36,118 16,739 7,127 6,221 4,285 1,746
1997 34,872 15,791 6,803 6,129 3,955 2,195
1998 40,096 18,969 7,895 6,637 3,964 2,631
1999 39,748 18,233 7,446 6,690 3,698 3,682
2000 41,212 18,528 8,538 6,688 3,640 3,817
2001 45,164 20,181 9,707 7,114 3,812 4,349
2002 46,839 21,487 10,847 7,182 3,789 3,534
2003 50,716 23,742 11,530 7,664 4,041 3,739

December 2023
24
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
EXHIBIT 7. (continued)
Fiscal year Total Child Adult
1
Disabled Aged Unknown
2004 54,250 25,415 12,325 8,123 4,349 4,037
2005 56,276 25,979 12,431 8,205 4,395 5,266
2006 56,264 26,358 12,495 8,334 4,374 4,703
2007 55,210 26,061 12,264 8,423 4,044 4,418
2008 56,962 26,479 12,739 8,685 4,147 4,912
2009 60,880 28,344 14,245 9,031 4,195 5,066
2010 63,730 30,024 15,368 9,341 4,289 4,709
2011 65,831 30,175 16,069 9,609 4,331 5,646
2012 65,584 30,467 16,483 9,836 4,376 4,423
2013 67,516 30,703 16,889 10,123 4,500 5,301
2018
2
82,940 30,769 28,870 9,062 6,086 8,153
2019 81,655 29,998 29,792 8,811 6,265 6,789
2020 81,316 30,126 30,830 8,703 6,574 5,083
2021 85,007 31,458 34,225 8,728 6,846 3,749
Notes: FY is scal year. Excludes Medicaid-expansion CHIP and the territories. Beneciaries (enrollees for whom payments are made) are shown here because
they provide the only historical time series data directly available before FY 1990. Most current analyses of individuals in Medicaid reect enrollees. For additional
discussion, see https://www.macpac.gov/macstats/data-sources-and-methods/. The increase in FY 1998 reects a change in how Medicaid beneciaries are
counted: beginning in FY 1998, a Medicaid-eligible person who received only coverage for managed care benets was included in this series as a beneciary.
Children and adults who qualify for Medicaid on the basis of a disability are included in the disabled category. In addition, although disability is not a basis of
eligibility for aged individuals, states may report some enrollees age 65 and older in the disabled category. For FYs 1975–2013, this exhibit does not recode
individuals age 65 and older who are reported as disabled, due to lack of detail in the historical data (unlike the majority of MACStats). Due to the way eligibility
is reported in Transformed Medicaid Statistical Information System (T-MSIS), age must be used to separate beneciaries eligible on the basis of age from those
eligible based on disability. This means that the beneciary count for the disabled category in 2018 and subsequent years no longer includes anyone age 65 and
older. Generally, individuals whose eligibility group is unknown are persons who were enrolled in the prior year but had a Medicaid claim paid in the current year.
For MACPAC's analysis, Medicaid enrollees were assigned a unique national identication (ID) number using an algorithm that incorporates state-specic ID
numbers and beneciary characteristics such as date of birth and gender. The national enrollment counts shown here are unduplicated using this national ID.
1
Includes the new adult group made eligible under Section 1902(a)(10)(A)(i)(VIII) of the Social Security Act by the Patient Protection and Aordable Care Act (P.L.
111-148, as amended).
2
Due to the transition from the Medicaid Statistical Information System (MSIS) to T-MSIS, complete and valid data are not available for all states for several years.
We jumped to FY 2018 because this was the most complete year of data available to develop our MACStats exhibits.
Sources: For FY 2021: MACPAC, 2023, analysis of T-MSIS data as of February 2023. For FY 2020: MACPAC, 2022, analysis of T-MSIS data as of February
2022. For FY 2019: MACPAC, 2021, analysis of T-MSIS data as of December 2020. For FY 2018: MACPAC, 2020, analysis of T-MSIS data as of April 2020;
for FYs 1999–2013: MACPAC, 2017, analysis of MSIS data; for FYs 1975–1998: Centers for Medicare & Medicaid Services, Medicare & Medicaid statistical
supplement, 2010 edition, Table 13.4, https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareMedicaidStatSupp/
Downloads/2010_Section13.pdf#Table%2013.4.

MACStats: Medicaid and CHIP Data Book
25
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
Spending
FYE enrollment
0
5
10
15
20
25
30
35
40
45
50
55
60
65
70
75
80
85
90
95
$0
$50
$100
$150
$200
$250
$300
$350
$400
$450
$500
$550
$600
$650
$700
$750
$800
$850
$900
$950
1972
1974
1976
1978
1980
1982
1984
1986
1988
1990
1992
1994
1996
1998
2000
2002
2004
2006
2008
2010
2012
2014
2016
2018
2020
2022
FYE enrollment (millions)
Spending (billions)
Fiscal year
Notes: FY is scal year. FYE is full-year equivalent, which also may be referred to as average monthly enrollment. All numbers
exclude CHIP-nanced coverage. Data before FY 1977 have been adjusted to the current federal scal year basis (October
1 to September 30). The amounts shown in this exhibit may dier from those published elsewhere due to slight dierences
in the timing of data and the treatment of certain adjustments. The amounts may also dier from prior versions of MACStats
due to changes in methodology by the CMS Oce of the Actuary (OACT). Spending consists of federal and state Medicaid
expenditures for benets and administration, excluding the Vaccines for Children program. Enrollment counts are FYEs and,
for scal years before FY 1990, have been estimated from counts of persons served (see https://www.macpac.gov/macstats/
data-sources-and-methods/ for a discussion of how enrollees are counted). Enrollment data for FYs 2013–2020 are projected.
Enrollment for FYs 1999–2022 include estimates for the territories.
Sources: For FY 2022: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64
enrollment reports as of October 25, 2023. For FY 2021: MACPAC, 2022, analysis of CMS-64 FMR net expenditure data as
of June 8, 2022, and CMS-64 enrollment reports as of October 24, 2022. For FYs 2019 and 2020: OACT, CMS, 2021, data
compilation provided to MACPAC, September 21. OACT, CMS, 2020, data compilation provided to MACPAC, October 19.
EXHIBIT 8. Medicaid Enrollment and Spending, FYs 1972–2022

December 2023
26
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
-5%
0%
5%
10
%
15
%
20
%
25
%
30
%
1982
1984
1986
1988
1990
1992
1994
1996
1998
2000
2002
2004
2006
2008
2010
2012
2014
2016
2018
2020
2022
Fiscal year
Spending
FYE enrollment
Notes: FY is scal year. FYE is full-year equivalent, which also may be referred to as average monthly enrollment. All numbers
exclude CHIP-nanced coverage. The amounts shown in this exhibit may dier from those published elsewhere due to slight
dierences in the timing of data and the treatment of certain adjustments. The amounts may also dier from prior versions of
MACStats due to changes in methodology by the CMS Oce of the Actuary (OACT). Spending consists of federal and state
Medicaid expenditures for benets and administration, excluding the Vaccines for Children program. Enrollment counts are full-
year equivalents and, for scal years before FY 1990, have been estimated from counts of persons served (see https://www.
macpac.gov/macstats/data-sources-and-methods/ for a discussion of how enrollees are counted). Enrollment data for FYs
2013–2020 are projected. Enrollment for FYs 1999–2022 include estimates for the territories.
Sources: For FY 2022: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64
enrollment reports as of October 25, 2023. For FY 2021: MACPAC, 2022, analysis of CMS-64 FMR net expenditure data as
of June 8, 2022, and CMS-64 enrollment reports as of October 24, 2022. For FYs 2019 and 2020: OACT, CMS, 2021, data
compilation provided to MACPAC, September 21. OACT, CMS, 2020, data compilation provided to MACPAC, October 19.
EXHIBIT 9. Annual Growth in Medicaid Enrollment and Spending, FYs 1982–2022

MACStats: Medicaid and CHIP Data Book
27
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
EXHIBIT 10. Medicaid Enrollment and Total Spending Levels and Annual Growth, FYs 1972–2022
Fiscal year
Spending
(billions)
FYE enrollment
(millions)
Spending per
FYE enrollee
Annual growth
Spending FYE enrollment
Spending per
FYE enrollee
1972 $8 $16.5 $484 22.4% 1.3% 20.9%
1973 9 17.6 534 17.0 6.2 10.2
1974 11 19.0 567 15.1 8.3 6.3
1975 13 20.2 651 21.8 6.1 14.8
1976 15 20.7 720 13.6 2.7 10.6
1977 17 20.7 830 15.3 0.1 15.3
1978 19 20.0 959 11.2 -3.8 15.6
1979 22 19.6 1,115 14.0 -2.0 16.3
1980 25 19.6 1,285 15.7 0.4 15.2
1981 30 20.0 1,493 18.2 1.7 16.2
1982 32 19.6 1,620 6.7 -1.7 8.5
1983 35 19.6 1,779 9.6 -0.2 9.9
1984 37 19.8 1,890 7.4 1.2 6.2
1985 41 19.8 2,081 10.2 0.0 10.2
1986 44 20.5 2,172 7.7 3.2 4.4
1987 50 21.0 2,382 12.5 2.6 9.6
1988 54 20.8 2,609 8.6 -0.9 9.5
1989 61 21.4
2,850 12.1 2.6 9.3
1990 72 22.9 3,147 18.6 7.4 10.4
1991 94 26.3 3,587 30.6 14.6 14.0
1992 120 28.9 4,161 27.4 9.8 16.0
1993 131 31.2 4,182 8.7 8.1 0.5
1994 144 32.4 4,434 10.1 3.9 6.0
1995 159 33.4 4,779 10.9 2.9 7.8
1996 160 33.2 4,804 0.1 -0.4 0.5
1997 166 33.0 5,025 3.9 -0.6 4.6
1998 177 32.5 5,462 6.8 -1.7 8.7
1999 190 32.1 5,924 7.1 -1.2 8.5
2000 206 34.5 5,972 8.6 7.7 0.8
2001 229 36.9 6,213 11.0 6.7 4.0
2002 258 40.5 6,380 12.8 9.8 2.7
2003 276 43.5 6,352 6.9 7.4 -0.4
December 2023
28
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
EXHIBIT 10. (continued)
Fiscal year
Spending
(billions)
FYE enrollment
(millions)
Spending per
FYE enrollee
Annual growth
Spending FYE enrollment
Spending per
FYE enrollee
2004 $296 $45.2 $6,560 7.3% 3.9% 3.3%
2005 316 46.3 6,819 6.6 2.6 3.9
2006 315 46.7 6,751 -0.3 0.7 -1.0
2007 332 46.4 7,157 5.4 -0.5 6.0
2008 352 47.7 7,383 5.9 2.7 3.2
2009 379 50.9 7,443 7.6 6.7 0.8
2010 402 54.5 7,361 6.1 7.2 -1.1
2011 427 56.3 7,582 6.3 3.2 3.0
2012 431 58.9 7,313 0.9 4.6 -3.5
2013 456 59.8 7,622 5.8 1.5 4.2
2014 495 65.1 7,599 8.5 8.8 -0.3
2015 549 69.8 7,866 11.0 7.2 3.5
2016 577 72.1 8,003 5.1 3.3 1.7
2017 600 73.4 8,179 3.9 1.7 2.2
2018 616 73.9 8,339 2.7 0.7 2.0
2019 627 73.9 8,487 1.8 0.0 1.8
2020 683 75.3 9,070 8.9 1.9 6.9
2021 748 86.3
8,672 9.6 14.6
-4.4
2022 824 94.1 8,757 10.2 9.1 1.0
Notes: FY is scal year. FYE is full-year equivalent, which also may be referred to as average monthly enrollment. All numbers exclude CHIP-nanced coverage.
Data before FY 1977 have been adjusted to the current federal scal year basis (October 1 to September 30). The amounts shown in this exhibit may dier from
those published elsewhere due to slight dierences in the timing of data and the treatment of certain adjustments. The amounts may also dier from prior versions
of MACStats due to changes in methodology by the CMS Oce of the Actuary (OACT). Spending consists of federal and state Medicaid expenditures for benets
and administration, excluding the Vaccines for Children program. Enrollment counts are full-year equivalents and, for scal years before FY 1990, have been
estimated from counts of persons served (see https://www.macpac.gov/macstats/data-sources-and-methods/ for a discussion of how enrollees are counted).
Enrollment data for FYs 2013–2020 are projected. Enrollment data for FYs 1999–2022 include estimates for the territories.
Sources: For FY 2022: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64 enrollment reports as of October 25,
2023. For FY 2021: MACPAC, 2022, analysis of CMS-64 FMR net expenditure data as of June 8, 2022, and CMS-64 enrollment reports as of October 24, 2022.
For FYs 2019 and 2020: OACT, CMS, 2021, data compilation provided to MACPAC, September 21. OACT, CMS, 2020, data compilation provided to MACPAC,
October 19.

MACStats: Medicaid and CHIP Data Book
29
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
EXHIBIT 11. Full-Benet Medicaid and CHIP Enrollment, Selected Months in 2013–2023
State
Number of individuals enrolled Annual and cumulative growth
July–September
2013 average July 2020 July 2021 July 2022 July 2023
July 2020–
July 2021
July 2021–
July 2022
July 2022–
July 2023
July–September
2013 average to
July 2023
Total 56,511,799
1
76,003,528 83,999,081 90,069,484 91,521,722 10.5% 7.2% 1.6% 59.5%
2
Alabama 799,176
3
959,675 1,055,463 1,138,406 1,186,358 10.0 7.9 4.2 42.4
Alaska 122,334 233,334 251,024 261,816 261,521 7.6 4.3 -0.1 114.0
Arizona 1,201,770 1,862,408 2,072,102 2,227,971 2,134,921 11.3 7.5 -4.2 85.4
Arkansas 556,851 843,515 934,944 1,012,769 906,259 10.8 8.3 -10.5 81.9
California 7,755,381 12,016,056 12,983,442 13,744,043 14,325,437 8.1 5.9 4.2 77.2
Colorado 783,420 1,357,050 1,532,326 1,646,836 1,640,664 12.9 7.5 -0.4 110.2
Connecticut – 885,365 960,844 979,293 995,155 8.5 1.9 1.6 –
Delaware 223,324 243,349 271,159 290,979 310,479 11.4 7.3 6.7 30.3
District of Columbia 235,786
4, 5
253,009 270,938 286,672 289,252 7.1 5.8 0.9 21.6
Florida 3,695,306 3,930,734 4,350,511 4,734,996 4,521,012 10.7 8.8 -4.5 28.1
Georgia
1,535,090 1,970,507 2,214,237 2,405,477 2,511,096 12.4 8.6 4.4 56.7
Hawaii 288,357 363,958 424,531 452,696 438,044 16.6 6.6 -3.2 57.0
Idaho 238,150 347,777 399,433 430,307 359,738 14.9 7.7 -16.4 80.7
Illinois 2,626,943 3,139,748 3,440,508 3,675,203 3,863,904 9.6 6.8 5.1 39.9
Indiana 1,120,674 1,543,368 1,786,580 1,954,908 1,960,430 15.8 9.4 0.3 74.4
Iowa 493,515 711,187 786,223 828,281 793,857 10.6 5.3 -4.2 67.8
Kansas 378,160 406,698 450,537 491,794 474,225 10.8 9.2 -3.6 30.0
Kentucky 606,805 1,465,221 1,489,474 1,576,193 1,578,173 1.7 5.8 0.1 159.8
Louisiana 1,019,787 1,608,573 1,766,777 1,858,130 1,885,983 9.8 5.2 1.5 82.2
Maine – 291,569 325,876 355,437 377,328 11.8 9.1 6.2 –
Maryland 856,297 1,392,038 1,534,076 1,645,951 1,691,568 10.2 7.3 2.8 92.2
Massachusetts 1,296,359 1,647,914 1,797,825 1,923,683 1,998,111 9.1 7.0 3.9 48.4
Michigan 1,912,009 2,487,485 2,777,203 2,965,223 3,113,849 11.6 6.8 5.0 55.1
Minnesota 873,040
6
1,108,531 1,239,326 1,332,742 1,401,089 11.8 7.5 5.1 52.7
Mississippi 615,556 645,270 712,012 747,701 766,340 10.3 5.0 2.5 21.5

December 2023
30
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
EXHIBIT 11. (continued)
State
Number of individuals enrolled Annual and cumulative growth
July–September
2013 average July 2020 July 2021 July 2022 July 2023
July 2020–
July 2021
July 2021–
July 2022
July 2022–
July 2023
July–September
2013 average to
July 2023
Missouri 846,084 951,731 1,093,102 1,349,254 1,481,081 14.9% 23.4% 9.8% 59.5%
Montana 148,974 259,433 291,578 313,837 294,114 12.4 7.6 -6.3 110.7
Nebraska 244,600 261,168 335,065 374,026 393,843 28.3 11.6 5.3 52.9
Nevada 332,560 695,931 800,436 868,971 835,888 15.0 8.6 -3.8 161.3
New Hampshire 127,082 197,601 225,025 242,720 191,087 13.9 7.9 -21.3 91.0
New Jersey 1,283,851 1,806,736 2,007,346 2,148,004 2,281,227 11.1 7.0 6.2 67.3
New Mexico 457,678 782,159 847,066 876,177 823,720 8.3 3.4 -6.0 91.4
New York 5,678,417 6,349,834 6,910,492 7,249,900 7,535,276 8.8 4.9 3.9 27.7
North Carolina 1,595,952 1,900,966 2,125,427 2,283,904 2,279,059 11.8 7.5 -0.2 43.1
North Dakota 69,980
7
98,657 113,589 123,776 124,926 15.1 9.0 0.9 76.9
Ohio 2,130,322 2,819,633 3,086,656 3,270,899 3,295,451 9.5 6.0 0.8 53.5
Oklahoma 790,051 809,286 1,020,015 1,231,239
1,267,103 26.0 20.7 2.9 55.8
Oregon 626,356
8
1,069,272 1,219,271 1,334,459 1,456,893 14.0 9.4 9.2 113.1
Pennsylvania 2,386,046 3,149,552 3,422,966 3,621,759 3,635,220 8.7 5.8 0.4 51.8
Rhode Island 190,833 309,281 338,291 353,502 372,618 9.4 4.5 5.4 85.2
South Carolina 889,744 1,077,781 1,185,531
9
1,269,341 1,243,371 10.0 7.1 -2.0 42.7
South Dakota 115,501 115,715 129,870 140,676 116,043 12.2 8.3 -17.5 21.8
Tennessee 1,244,516 1,512,194 1,642,482 1,736,570 1,814,919 8.6 5.7 4.5 39.5
Texas 4,203,449 4,531,429 5,077,158 5,512,172 5,526,633 12.0 8.6 0.3 31.1
Utah 294,029
5
349,201 420,000
5
465,497
5
431,137 20.3 10.8 -7.4 58.3
Vermont 161,081 163,055 180,359 189,194 182,446 10.6 4.9 -3.6 17.5
Virginia 935,434 1,529,228 1,750,410 1,934,368 2,008,101 14.5 10.5 3.8 106.8
Washington 1,117,576 1,811,777 1,993,221 2,120,740 2,038,345 10.0 6.4 -3.9 89.8
West Virginia 354,544 538,836 593,834 631,256 596,525 10.2 6.3 -5.5 78.0
Wisconsin 985,531
10
1,137,130 1,292,431 1,380,418 1,427,922 13.7 6.8 3.4 40.1
Wyoming 67,518 61,603 70,089 79,318 83,981 13.8 13.2 5.9 17.5

MACStats: Medicaid and CHIP Data Book
31
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
EXHIBIT 11. (continued)
Notes: Enrollment excludes individuals with limited benets, such as those who receive only Medicaid coverage of Medicare premiums and cost sharing, family
planning services, or emergency coverage due to non-citizen status (state-specic exceptions are noted below). The July–September 2013 period shown here
serves as a baseline from before the Patient Protection and Aordable Care Act (P.L. 111-148, as amended) was implemented, representing the number of people
covered by Medicaid and CHIP before the start of open enrollment for exchange plans in October 2013 and the state expansions of Medicaid for adults that began
in January 2014. Some data are preliminary or estimated, and all data are subject to change as states may revise their submissions at any time. See data sources
for full details.
– Dash indicates that state did not report data.
1
Excludes two states not reporting data.
2
Percentage calculated based only on states reporting data for both periods.
3
Data are for September 2013 only.
4
Includes limited-benet enrollees.
5
Includes enrollees in other nancial assistance programs not enrolled in Medicaid or CHIP.
6
May include duplicates.
7
Data are for July 2013 only.
8
Includes emergency Medicaid population.
9
Includes retroactive enrollment.
10
Excludes retroactive enrollment.
Source: MACPAC, 2023, analysis of CMS, 2023, State Medicaid and CHIP applications, eligibility determinations, and enrollment data, accessed on October 31,
2023, https://www.medicaid.gov/medicaid/national-medicaid-chip-program-information/medicaid-chip-enrollment-data/monthly-medicaid-chip-application-eligibility-
determination-and-enrollment-reports-data/index.html.

December 2023
32
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
EXHIBIT 12. Historical and Projected National Health Expenditures by Payer for Selected Years, CYs 1970–2031
Calendar
year
Total
(billions)
Payer amount (billions) and share of total
Medicaid
and CHIP Medicare
Private
insurance
Other health
insurance
1
Other third-
party payers
2
Out of pocket
Historical
1970 $74 $5 7.1% $8 10.4% $15 20.4% $3 4.5% $19 25.0% $24 32.7%
1975 133 13 10.1 16 12.3 30 22.4 6 4.5 31 23.5 36 27.2
1980 253 26 10.3 37 14.8 67 26.5 10 3.8 58 22.8 55 21.8
1985 440 41 9.3 72 16.3 127 28.8 15 3.5 94 21.3 92 20.8
1990 719 74 10.2 110 15.3 226 31.4 21 3.0 154 21.4 134 18.6
1995 1,020 145 14.2 184 18.1 315 30.9 27 2.6 208 20.4 141 13.8
2000 1,366 203 14.9 225 16.5 441 32.3 33 2.4 270 19.8 194 14.2
2005 2,027 317 15.6 340 16.8 671 33.1 56 2.8 378 18.7 264 13.1
2010 2,590 409 15.8 520 20.1 820 31.7
84 3.2 456 17.6 301 11.6
2011 2,677 419 15.6 545 20.3 851 31.8 88 3.3 464 17.3 310 11.6
2012 2,783 435 15.6 568 20.4 878 31.5 90 3.2 489 17.6 323 11.6
2013 2,857 458 16.0 589 20.6 880 30.8 92 3.2 506 17.7 331 11.6
2014 3,003 511 17.0 617 20.6 923 30.7 99 3.3 511 17.0 341 11.4
2015 3,165 558 17.6 648 20.5 977 30.9 106 3.4 523 16.5 354 11.2
2016 3,307 582 17.6 676 20.4 1,031 31.2 109 3.3 544 16.5 366 11.1
2017 3,446 597 17.3 705 20.5 1,080 31.3 114 3.3 578 16.8 373 10.8
2018 3,604 615 17.1 750 20.8 1,130 31.3 118 3.3 605 16.8 387 10.7
2019 3,757 635 16.9 802 21.3 1,158 30.8 125 3.3 635 16.9 403 10.7
2020 4,144 693 16.7 831 20.1 1,145 27.6 136 3.3 946 22.8 392 9.5
2021 4,255 756 17.8 901 21.2 1211 28.5 150 3.5 804 18.9 433 10.2
Projected
2022 $4,440 $828 18.7% $944 21.3% $1,248 28.1% $160 3.6% $808 18.2% $452 10.2%
2023 4,666 860 18.4 1,020 21.8 1,345 28.8 179 3.8 788 16.9 475 10.2

MACStats: Medicaid and CHIP Data Book
33
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
EXHIBIT 12. (continued)
Calendar
year
Total
(billions)
Payer amount (billions) and share of total
Medicaid
and CHIP Medicare
Private
insurance
Other health
insurance
1
Other third-
party payers
2
Out of pocket
2024 $4,898 $844 17.2% $1,093 22.3% $1,447 29.5% $191 3.9% $825 16.8% $498 10.2%
2025 5,185 883 17.0 1,190 23.0 1,532 29.5 201 3.9 859 16.6 520 10.0
2026 5,462 933 17.1 1,290 23.6 1,597 29.2 211 3.9 893 16.3 539 9.9
2027 5,774 989 17.1 1,394 24.1 1,682 29.1 220 3.8 930 16.1 560 9.7
2028 6,106 1,051 17.2 1,504 24.6 1,769 29.0 229 3.7 971 15.9 583 9.6
2029 6,449 1,110 17.2 1,621 25.1 1,858 28.8 238 3.7 1,016 15.8 607 9.4
2030 6,804 1,173 17.2 1,731 25.4 1,957 28.8 247 3.6 1,063 15.6 633 9.3
2031 7,175 1,239 17.3 1,849 25.8 2,059 28.7 256 3.6 1,112 15.5 659 9.2
Notes: CY is calendar year. Components may not sum to total due to rounding. The latest projections begin after the latest historical year (2021) and go through 2031.
¹ U.S. Department of Defense and U.S. Department of Veterans Aairs.
² Includes all other public and private programs and expenditures except for out-of-pocket amounts.
Sources: For historical data: MACPAC, 2023, analysis of Oce of the Actuary (OACT), CMS, 2022, National health expenditures by type of service and source of
funds: Calendar years 1960–2021, https://www.cms.gov/les/zip/national-health-expenditures-type-service-and-source-funds-cy-1960-2021.zip. For projected data:
MACPAC, 2023, analysis of OACT, 2023, National health expenditures by type of expenditure and source of funds: Calendar years 1960 to 2031, https://www.cms.
gov/les/zip/nhe-historical-and-projections-data.zip; and OACT, 2023, Table 17: Health insurance enrollment and enrollment growth rates, calendar years, 2013–2031,
https://www.cms.gov/les/zip/nhe-projections-tables.zip.

December 2023
34
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 2
EXHIBIT 13. Medicaid as a Share of State Budgets Including and Excluding Federal Funds, SFYs 1995–2021
Including all
federal and
state funds
Including state
general funds only
(no federal funds)
Including all
state funds
(no federal funds)
19.8%
20.1%
19.5%
19.7%
22.0%
22.3%
20.9%
21.9%
23.8%
24.3%
27.9%
28.9%
28.9%
26.9%
14.4%
14.7%
14.4%
15.2%
17.2%
17.1%
16.6%
16.4%
16.5%
19.3%
19.5%
19.9%
18.9%
17.9%
11.6%
11.6%
11.4%
11.7%
13.1%
13.5%
12.8%
12.3%
13.3%
15.2%
15.6%
16.0%
15.6%
14.4%
0%
5%
10%
15%
20%
25%
30%
1995
1997
1999
2001
2003
2005
2007
2009
2011
2013
2015
2017
2019
2021

MACStats: Medicaid and CHIP Data Book
35
Section 2: Trends
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 2
EXHIBIT 13. (continued)
State scal year
Medicaid as a share of all
federal and state funds
Medicaid as a share of
state general funds only
Medicaid as a share of
all state funds
1995 19.8% 14.4% 11.6%
1996 19.9 14.7 11.7
1997 20.1 14.7 11.6
1998 19.6 14.8 11.5
1999 19.5 14.4 11.4
2000 19.1 15.0 11.0
2001 19.7 15.2 11.7
2002 20.7 15.8 12.2
2003 22.0 17.2 13.1
2004 22.1 16.9 12.9
2005 22.3 17.1 13.5
2006 21.4 17.4 13.3
2007 20.9 16.6 12.8
2008 20.5 16.0 12.5
2009 21.9 16.4 12.3
2010 22.2 14.8 11.6
2011 23.8 16.5 13.3
2012 23.9 19.2 14.8
2013 24.3 19.3 15.2
2014 26.5 20.0 15.8
2015 27.9 19.5 15.6
2016 28.8 19.6 15.8
2017 28.9 19.9 16.0
2018 29.3 20.3 16.5
2019 28.9 18.9 15.6
2020 28.4 19.1 15.1
2021 26.9 17.9 14.4
Notes: SFY is state scal year. Amounts shown here reect the most recent information available in cases in which data for a
given year were published and then updated in a subsequent report.
The all federal and state funds category reects amounts from any source. The state general funds only category reects
amounts from revenues raised through income, sales, and other broad-based state taxes and excludes federal funds. The
all state funds category reects amounts from any non-federal source; these include state general funds, other state funds
(amounts from revenue sources that are restricted by law for particular government functions or activities, which for Medicaid
includes provider taxes and local funds), and bonds (expenditures from the sale of bonds, generally for capital projects) and
excludes federal funds.
Source: MACPAC, 2023, analysis of state expenditure reports from the National Association of State Budget Ocers,
http://nasbo.org/mainsite/reports-data/state-expenditure-report/state-expenditure-archives/.


SECTION 3:
Program Enrollment
and Spending

December 2023
38
Section 3: Program Enrollment and Spending
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
Section 3: Program Enrollment and Spending
Key Points
•
Total Medicaid spending was $830.6 billion in scal year (FY) 2022 (Exhibit 16). Spending for the
State Children’s Health Insurance Program (CHIP) was $22.3 billion (Exhibit 33).
•
The federal share was 71.4 percent of total Medicaid benet spending in FY 2022, compared with an
average federal share of approximately 63 percent to 64 percent since 2015. This increase in federal
spending is due to the 6.2 percentage point increase in the federal medical assistance percentage
(FMAP) under the Families First Coronavirus Response Act (P.L. 116-127) that was retroactively
applied back to January 1, 2020 (Exhibit 16).
•
In FY 2021, individuals eligible on the basis of disability and enrollees age 65 and older accounted
for about 21 percent of Medicaid enrollees but about 52 percent of program spending (Exhibits 14
and 21). Many of these individuals were users of long-term services and supports (LTSS). LTSS
users accounted for only 4.9 percent of Medicaid enrollees but more than one-quarter of all Medicaid
spending (Exhibit 20).
•
The new adult group, which includes those individuals eligible under Section 1902(a)(10)(A)(i)(VIII)
of the Social Security Act (the Act), accounted for 25 percent of enrollees and 22 percent of spending
in FY 2021 (Exhibits 14 and 21). This group is composed primarily of those newly eligible under the
Patient Protection and Aordable Care Act (ACA, P.L. 111-148, as amended) but includes some
adults who were previously eligible in states that expanded Medicaid before the ACA.
•
More than half of Medicaid spending for enrollees was for capitation payments to managed care
plans (Exhibits 17 and 18). Spending for enrollees who are eligible on the basis of disability and
enrollees age 65 and older has been shifting to managed care. More than half (52.9 percent)
of enrollees who are eligible on the basis of disability and more than one-third (36.8 percent) of
enrollees age 65 and older were enrolled in comprehensive managed care in FY 2021, including in
plans that provide managed LTSS (Exhibit 30).
•
Medicaid benet spending per enrollee varies substantially across states (Exhibit 22). This variation
reects many factors, including the underlying costs of delivering health care services in specic
geographic areas, the breadth of covered benets, and enrollee characteristics, such as health
status, that aect their use of services.
•
Drug rebates reduced gross drug spending by more than half (52.9 percent) in FY 2022 (Exhibit 28).
About two-thirds (64.1 percent) of Medicaid gross spending for drugs occurred under managed care
in FY 2022 (Exhibit 26).
•
Disproportionate share hospital (DSH), upper payment limit, and other types of supplemental
payments accounted for more than half (52.3 percent) of fee-for-service payments to hospitals in FY
2022 (Exhibit 24).

MACStats: Medicaid and CHIP Data Book
39
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 14. Medicaid Enrollment by State, Eligibility Group, and Dually Eligible Status, FY 2021 (thousands)
State Total
Basis of eligibility
1
Dually eligible status
2
All dually eligible
enrollees
Dually eligible
with full benets
Dually eligible
with limited
benets
Child
New adult
group
3
Other
adult
4
Disabled Aged Total Age 65+ Total Age 65+ Total Age 65+
Total
87,979 32,132 22,377 15,296 9,568 8,606 13,167 8,195 9,770 5,969 3,397 2,226
Alabama 1,162
571 – 233 219 138 242 138 98 53 144 85
Alaska 255
102 71 52 16 14 24 14 23 13 1 1
Arizona 2,266
780 664 447 182 194 298 185 240 144 57 41
Arkansas 1,045
459 352 2 151 82 157 85 88 51 70 34
California⁵ 13,918
3,651 4,727 3,149 900 1,491 1,774 1,356 1,737 1,325 37 31
Colorado⁶ 1,551
533 689 127 110 91 158 98 113 65 46 33
Connecticut 1,177
366 354 236 65 157 213 152 79 46 134 106
Delaware 292
107 84 54 26 20 33 20 16 9 18 11
District of Columbia⁷ 278
78 82 57 32 29 41 28 29 19 12 10
Florida 5,054
2,517 – 1,111 679 747 1,058 737 625 428 433 309
Georgia 2,448
1,324 – 486 367 271 414 265 178 110 236 156
Hawaii 429
140 168 56 22 43 58 39 51 34 7 5
Idaho 436
178 129 42 53 34 58 32 35 17 23 14
Illinois⁷ 3,371
693 2,026 128 206 317 450 277 400 244 50 34
Indiana⁶ 1,932
726 477 406 186 136 253 134 183 93 70 41
Iowa 791
289 246 122 85 50 107 52 84 37 22 15
Kansas 452
248 – 77 81 46 87 45 58 29 28 16
Kentucky 1,734
477 761 165 218 112 247 128 152 80 95 48
Louisiana⁶ 1,823
608 710 104 241 159 284 160 162 86 122 74
Maine 422
115 95 86 64 63 103 59 63 29 40 30
Maryland 1,548
570 425 301 146 106 185 108 114 62 71 46
Massachusetts 1,980
450 429 512 350 239 395 217 360 184 35 33
Michigan 3,001
1,038 986 420 352 205 384 201 336 173 48 27
Minnesota 1,338
604 277 242 120 96 161 89 146 79 15 10
Mississippi 827
425 – 132 165 104 182 103 89 49 93 54

December 2023
40
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 14. (continued)
State Total
Basis of eligibility
1
Dually eligible status
2
All dually eligible
enrollees
Dually eligible
with full benets
Dually eligible
with limited
benets
Child
New adult
group
3
Other
adult
4
Disabled Aged Total Age 65+ Total Age 65+ Total Age 65+
Missouri 1,240
673 60 190 201 116 224 109 186 87 39 22
Montana 289
105 114 28 23 18 35 20 25 14 9 6
Nebraska 331
158 59 47 41 27 47 25 41 21 6 4
Nevada 880
330 340 85 64 61 100 61 46 25 54 36
New Hampshire 249
86 88 28 27 19 42 18 28 12 13 6
New Jersey 1,923
672 739 176 174 163 262 157 262 157 – –
New Mexico 962
348 311 162 76 66 115 71 62 34 54 37
New York 7,253
1,968 2,670 1,139 625 850 1,200 824 1,017 684 182 140
North Carolina 2,535
1,076 – 878 361 220 372 212 287 157 85 55
North Dakota⁵ 125
52 34 16 13 11 19 11 16 9 3 2
Ohio 3,146
1,108 860 525 403 249 420 221 282 147 138 74
Oklahoma 1,109
563 184 166 118 78 139 74 110 59 29 15
Oregon⁶ 1,275
332 680 40 115 108 163 103 103 63 60 39
Pennsylvania 3,390
1,032 1,093 342 600 322 582 324 484 264 98 60
Rhode Island 335
97 101 67 40 29 57 32 48 27 8 6
South Carolina 1,377
631 – 461 175 109 191 104 180 97 11 7
South Dakota 132
75 – 23 21 14 23 13 15 8 9 5
Tennessee 1,787
912 – 443 269 162 314 162 185 82 129 80
Texas⁸ 5,628
3,354 0 992 707 575 821 547 430 280 391 267
Utah⁵ 446
200 109 65 47 24 43 22 39 20 4 2
Vermont 198
69 74 13 20 22 31 18 23 12 8 6
Virginia 1,845
629 608 277 185 146 220 127 151 88 69 39
Washington 2,153
844 803 176 183 147 240 138 173 98 68 40
West Virginia 632
202 223 62 93 53 110 54 64 31 45 23
Wisconsin 1,414
510 – 556 193 155 204 106 189 95 15 11
Wyoming 81
45 – 15 12 9 14 8 9 5 5 3

MACStats: Medicaid and CHIP Data Book
41
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 14. (continued)
Notes: FY is scal year. Enrollment numbers generally include individuals ever enrolled in Medicaid-nanced coverage during the year, even if for a single month.
However, in the event individuals were also enrolled in CHIP-nanced Medicaid coverage (i.e., Medicaid-expansion CHIP) during the year, they are excluded if
their most recent enrollment month was in Medicaid-expansion CHIP. Numbers exclude individuals enrolled only in Medicaid-expansion CHIP during the year and
enrollees in the territories. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between the Transformed
Medicaid Statistical Information System (T-MSIS) and the Medicaid Statistical Information System (MSIS).
For MACPAC's analysis, Medicaid enrollees were assigned a unique national identication (ID) number using an algorithm that incorporates state-specic ID
numbers and beneciary characteristics such as date of birth and gender. The state and national enrollment counts shown here are unduplicated using this
national ID. Categories may not sum to the total for each state due to rounding. In addition, the sum of the state totals exceeds the national total because
individuals may be enrolled in more than one state during the year.
– Dash indicates zero; 0 indicates an amount less than 500 that rounds to zero.
¹ Children and adults under age 65 who qualify for Medicaid on the basis of disability are included in the disabled category. Individuals age 65 and older eligible
through an aged, blind, or disabled pathway are included in the aged category.
² Dually eligible enrollees are covered by both Medicaid and Medicare. Those with limited benets receive only Medicaid assistance with Medicare premiums and
cost sharing.
³ Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Social Security Act (the Act). Newly eligible
adults include those who are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who
would have previously been eligible for Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to
adults with incomes greater than 100 percent of the federal poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
⁴ Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers,
pregnancy).
⁵ State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children that
would have, before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied
in the T-MSIS data. Because the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these
states based on the proportion reported in their SPA. Correspondingly, we reduced California's child enrollment by approximately 250,000, North Dakota's child
enrollment by approximately 3,000, and Utah's child enrollment by approximately 12,000.
⁶ State reported a large shift of enrollees between eligibility groups from the prior year. Colorado reported a 35 percent increase in the new adult group and a 46
percent decrease for the other adult group. Indiana reported a 16 percent decrease for the new adult group and a 60 percent increase for the other adult group.
Louisiana reported a 15 percent increase in the new adult group and a 10 percent decrease in the other adult group. Oregon reported a 33 percent increase in the
new adult group, a 69 percent decrease in the other adult group, a 102 percent increase in the disabled group, and a 53 percent increase in the aged group.
⁷ State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The
District of Columbia's average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than
the benchmark.
⁸ State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
Source: MACPAC, 2023, analysis of T-MSIS data as of February 2023.

December 2023
42
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 15. Medicaid Full-Year Equivalent Enrollment by State and Eligibility Group, FY 2021 (thousands)
State
Total Child New adult group
1
Other adult
2
Disabled Aged
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
Total
80,838 74,023 29,688 29,567 20,360 19,786 13,744 10,868 9,192 8,079 7,855 5,723
Alabama 1,072 865 524 524 – – 214 140 209 154 126 48
Alaska 237 236 94 94 66 66 48 48 16 15 13 12
Arizona 2,096 1,917 718 708 608 570 418 345 173 158 178 135
Arkansas 956 890 418 418 319 319 1 1 145 111 74 42
California⁴ 12,702 11,171 3,371 3,337 4,321 3,918 2,740 1,717 875 869 1,396 1,330
Colorado⁵ 1,417 1,374 490 490 625 625 116 115 105 93
82 53
Connecticut 1,087 942 341 340 330 329 209 192 63 35 145 46
Delaware 268 241 99 97 76 76 50 40 25 19 19 8
District of Columbia⁶ 262 250 72 72 76 76 55 55 32 29 27 18
Florida 4,648 4,153 2,355 2,353 – – 978 893 628 510 686 397
Georgia 2,229 1,924 1,211 1,211 – – 433 343 342 268 244 103
Hawaii 393 386 130 130 151 151 51 51 21 20 40 35
Idaho 382 360 155 155 111 111 37 37 50 41 30 17
Illinois⁶ 3,059 2,988 655 654 1,818 1,818 108 83 196 182 282 251
Indiana⁵ 1,752 1,601 664 653 426 415 359 300 180 152 122 81
Iowa 714 689 257 257 223 222 108 105 82 75 44 30
Kansas 408 379 227 227 – – 67 65 74 62 40 26
Kentucky 1,591 1,497 442 442 677 676 156 155 213 167 103 58
Louisiana⁴ 1,707 1,589 572 572 659 659 96 94 233 187 147 77
Maine 380 305 100 97 84 83 77 48 61 51 57 26
Maryland 1,440 1,354 537 536 391 391 275 256 141 117 96 54
Massachusetts 1,819 1,566 409 380 387 366 467 314 334 332 222 175
Michigan 2,783 2,708 957 954 908 894 391 380 341 322 185 159
Minnesota 1,227 1,199 563 562 249 247 214 204 116 111 85 76
Mississippi 770 653 398 398 – – 120 92 157 119 96 45

MACStats: Medicaid and CHIP Data Book
43
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 15. (continued)
State
Total Child New adult group
1
Other adult
2
Disabled Aged
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
All
enrollees
Full-
benet
enrollees
3
Missouri 1,101 1,066 626 626 15 15 168 168 189 174 102 82
Montana 266 256 98 98 104 104 25 24 22 19 17 11
Nebraska 289 284 143 143 44 44 40 40 38 36 24 20
Nevada 785 733 295 295 302 302 73 71 60 43 55 21
New Hampshire 225 204 80 79 78 78 25 17 26 20 17 11
New Jersey 1,750 1,749 615 615 670 669 150 148 168 168 148 148
New Mexico 887 799 314 314 289 283 151 122 72 54 61 26
New York 6,677 6,506 1,821 1,820 2,466 2,465 1,007 1,003 605 566 778 651
North Carolina 2,275 1,791 953 948 – – 780 384 343 311 199 148
North Dakota⁴ 107 104 44 44 28 28 14 14 12 11 9 7
Ohio 2,929 2,798 1,037 1,036 785 785 493 493 391 330 224 154
Oklahoma 883 808 453 453 114 84 136 116 111 100 69 55
Oregon⁵ 1,100 999 281 280 609 579 35 12 93 77 82 51
Pennsylvania 3,103 2,989 935 930 989 985 315 301 576 539 288 234
Rhode Island 310 301 87 87 93 93 63 62 39 37 27 22
South Carolina 1,296 1,068 597 593 – – 432 222 167 162 100 91
South Dakota 119 111 68 68 – – 20 20 19 16 12 7
Tennessee 1,625 1,505 802 802 – – 418 418 258 212 147 73
Texas⁷ 5,173 4,413 3,110 3,109 0 0 872 477 672 555 519 272
Utah⁴ 392 379 179 178 93 93 54 47 45 43 21 19
Vermont 184 177 65 65 68 68 12 12 20 18 20 14
Virginia 1,667 1,548 562 562 547 539 249 203 178 149 131 95
Washington 1,957 1,888 776 775 722 722 150 145 176 150 133 96
West Virginia 583 540 186 186 203 201 56 55 89 70 48 27
Wisconsin 1,303 1,242 470 468 – – 507 463 186 183 139 129
Wyoming 70 65 40 40 – – 12 12 11 9 7 4

December 2023
44
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 15. (continued)
Notes: FY is scal year. Full-year equivalent (FYE) may also be referred to as average monthly enrollment. Enrollment numbers generally include individuals ever
enrolled in Medicaid-nanced coverage during the year, even if for a single month. However, in the event individuals were also enrolled in CHIP-nanced Medicaid
coverage (i.e., Medicaid-expansion CHIP) during the year, they are excluded if their most recent enrollment month was in Medicaid-expansion CHIP. Numbers
exclude individuals enrolled only in Medicaid-expansion CHIP during the year and enrollees in the territories. Children and adults under age 65 who qualify
for Medicaid on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through an aged, blind, or disabled pathway
are included in the aged category. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between the
Transformed Medicaid Statistical Information System (T-MSIS) and the Medicaid Statistical Information System (MSIS).
For MACPAC's analysis, Medicaid enrollees were assigned a unique national identication (ID) number using an algorithm that incorporates state-specic ID
numbers and beneciary characteristics such as date of birth and gender. The state and national enrollment counts shown here are unduplicated using this
national ID. Categories may not sum to the total for each state due to rounding. In addition, the sum of the state totals exceeds the national total because
individuals may be enrolled in more than one state during the year.
– Dash indicates zero; 0 indicates an amount less than 500 that rounds to zero.
¹ Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Social Security Act (the Act). Newly eligible
adults include those who are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who
would have previously been eligible for Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to
adults with incomes greater than 100 percent of the federal poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
² Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers,
pregnancy).
³ In this exhibit, full-benet enrollees columns exclude enrollees reported by states in T-MSIS as receiving coverage of only emergency services, family planning
services, COVID-19 diagnostic products or testing-related services, or assistance with Medicare premiums and cost sharing.
⁴ State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children that
would have, before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in
the T-MSIS data. Because the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states
based on the proportion reported in their SPA. Correspondingly, we reduced California's child FYE enrollment by approximately 229,000, North Dakota's child FYE
enrollment by approximately 2,600, and Utah's child FYE enrollment by approximately 10,900.
⁵ State reported a large shift of enrollees between eligibility groups from the prior year. Colorado reported a 54 percent increase in the new adult group and a 41
percent decrease for the other adult group. Indiana reported a 1.2 percent increase for the new adult group and an 80 percent increase for the other adult group.
Louisiana reported a 28 percent increase in the new adult group and a 0.5 percent increase in the other adult group. Oregon reported a 45 percent increase in the
new adult group, a 67 percent decrease in the other adult group, a 76 percent increase in the disabled group, and a 32 percent increase in the aged group.
⁶ State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The
District of Columbia's average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than
the benchmark.
⁷ State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
Source: MACPAC, 2023, analysis of T-MSIS data as of February 2023.

MACStats: Medicaid and CHIP Data Book
45
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 16. Medicaid Spending by State, Category, and Source of Funds, FY 2022 (millions)
State
1
Benets State program administration Total Medicaid
Total Federal State Total Federal State Total Federal State
Alabama $7,166 $5,685 $1,481 $241 $144 $96 $7,407 $5,829 $1,578
Alaska 2,436 1,911 525 157 95 62 2,592 2,006 587
Arizona 20,258 16,932 3,325 331 205 126 20,589 17,137 3,452
Arkansas 8,533 7,022 1,511 442 289 153 8,975 7,311 1,664
California 117,885 80,358 37,527 7,190 4,323 2,867 125,075 84,681 40,393
Colorado 11,874 7,966 3,908 551 334 217 12,425 8,300 4,125
Connecticut 9,672 6,285 3,387 353 226 127 10,025 6,511 3,514
Delaware 3,137 2,255 882 103 64 39 3,240 2,319 921
District of Columbia 3,648 2,902 745 281 183 98 3,929 3,086 843
Florida 32,667 22,212 10,455 606 365 241 33,274 22,577 10,697
Georgia 14,340 10,664 3,676 536 338 198 14,876 11,002 3,874
Hawaii 2,990 2,130 860 113 74 39 3,103 2,204 898
Idaho 3,195 2,551 644 135 87 48 3,330 2,638 692
Illinois 25,956 17,225 8,731 1,017 626 390 26,973 17,851 9,122
Indiana 16,851 13,042 3,809 471 280 191 17,322 13,322 4,000
Iowa 6,614 4,906 1,708 163 110 53 6,777 5,016 1,761
Kansas 4,301 2,957 1,344 250 166 85 4,551 3,122 1,429
Kentucky 14,590 12,164 2,426 286 193 93 14,877 12,357 2,520
Louisiana 14,674 11,790 2,884 365 240 125 15,039 12,030 3,009
Maine 3,786 2,879 906 167 111 55 3,952 2,991 962
Maryland 14,344 9,609 4,735 501 322 178 14,844 9,931 4,913
Massachusetts 20,865 13,428 7,437 1,159 678 480 22,023 14,106 7,918
Michigan 21,023 16,123 4,900 673 424 248 21,696 16,547 5,149
Minnesota 16,159 10,708 5,451 738 427 311 16,897 11,135 5,762
Mississippi 5,944 5,062 881 198 131 67 6,142 5,193 949
Missouri 13,013 10,303 2,710
427 260 167 13,440 10,563 2,877

December 2023
46
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
State
1
Benets State program administration Total Medicaid
Total Federal State Total Federal State Total Federal State
Montana $2,344 $1,929 $414 $105 $73 $31 $2,448 $2,003 $446
Nebraska 3,296 2,354 942 185 125 61 3,481 2,479 1,003
Nevada 5,053 3,976 1,076 218 134 85 5,271 4,110 1,161
New Hampshire 2,461 1,601 860 151 102 49 2,612 1,703 909
New Jersey 20,873 14,229 6,643 1,013 616 397 21,886 14,845 7,041
New Mexico 8,258 7,074 1,184 287 192 95 8,545 7,266 1,279
New York 80,518 52,155 28,363 2,046 1,180 866 82,565 53,336 29,229
North Carolina 18,404 13,967 4,437 1,063 679 384 19,467 14,646 4,822
North Dakota 1,524 1,076 448 97 66 30 1,621 1,143 478
Ohio 30,025 23,179 6,846 1,035 622 413 31,060 23,802 7,258
Oklahoma 7,523 6,353 1,170 218 128 90 7,741 6,482 1,260
Oregon 13,083 10,174 2,909 613 352 261 13,696 10,526 3,170
Pennsylvania 41,178 28,126 13,052 1,117 708 408 42,295 28,835 13,460
Rhode Island 3,393 2,394 999 191 123 69 3,584 2,517 1,067
South Carolina 7,544 5,887 1,657 382 240 142 7,926 6,127 1,800
South Dakota 1,246 886 360 74 47 27 1,320 933 387
Tennessee 11,265 8,323 2,942 819 573 245 12,083 8,896 3,187
Texas 54,942 37,497 17,444 1,627 982 645 56,569 38,479 18,090
Utah 4,211 3,304 907 186 123 63 4,398 3,428 970
Vermont 1,884 1,304 581 165 109 56 2,049 1,412 637
Virginia 17,824 12,252 5,572 439 275 164 18,263 12,527 5,736
Washington 17,141 12,133 5,007 1,073 582 490 18,213 12,716 5,498
West Virginia 5,184 4,389 795 209 152 56 5,393 4,542 851
Wisconsin 11,429 7,982 3,447 524 343 181 11,953 8,325 3,628
Wyoming 668 410 259 75 53 22 744 463 281
Subtotal (states) $787,191 $562,025
$225,165
$31,365 $19,278 $12,087 $818,555 $581,303 $237,252
EXHIBIT 16. (continued)

MACStats: Medicaid and CHIP Data Book
47
Section 3: Program Enrollment and Spending—Medicaid Overall
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 16. (continued)
State
1
Benets State program administration Total Medicaid
Total Federal State Total Federal State Total Federal State
American Samoa $68 $59 $10 $2 $2 $1 $71 $60 $11
Guam 167 150 17 4 2 2 171 152 19
Northern Mariana Islands 73 66 8 5 4 1 78 70 8
Puerto Rico 5,098 3,368 1,730 102 75 27 5,200 3,443 1,757
Virgin Islands 137 121 16 24 16 8 161 137 24
Subtotal (states and
territories)
$792,734 $565,788 $226,946 $31,502 $19,377 $12,125 $824,236 $585,165 $239,071
State Medicaid Fraud Control
Units
– – – 409 307 102 409 307 102
Medicaid survey and certication
of nursing and intermediate care
facilities
– – – 400 300 100 400 300 100
Vaccines for Children program – – – – – – 5,540 5,540 –
Total $792,734 $565,788 $226,946 $32,311 $19,983 $12,327 $830,585
2
$591,312
2
$239,273
Notes: FY is scal year. Total federal spending shown here ($591,312 million) will dier from total federal outlays shown in FY 2024 budget documents due to
slight dierences in the timing of data for the states and the treatment of certain adjustments. Federal spending in the territories is capped; however, territories
report their total spending regardless of whether they have reached their caps. As a result, federal spending shown here may exceed the amounts actually paid
to the territories. State shares for Medicaid Fraud Control Units (MFCUs) and survey and certication are MACPAC estimates based on 75 percent federal match.
State-level estimates for these items are available but are not shown here. The Vaccines for Children (VFC) program is authorized in the Medicaid statute but is
operated as a separate program; 100 percent federal funding nances the purchase of vaccines for children who are enrolled in Medicaid, uninsured, or privately
insured without vaccine coverage. Spending on administration is only for state programs; federal oversight spending is not included.
– Dash indicates zero; $0 indicates an amount less than $0.5 million that rounds to zero.
1
All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
2
Amounts exceed the sum of benets and state program administration columns due to the inclusion of the VFC program.
Sources: For state and territory spending: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023. For all other spending (MFCUs,
survey and certication, VFC program): CMS, 2023, Fiscal year 2024 justication of estimates for appropriations committees, Baltimore, MD, https://www.cms.gov/
les/document/cms-fy-2024-congressional-justication-estimates-appropriations-committees.pdf-0.

December 2023
48
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 17. Total Medicaid Benet Spending by State and Category, FY 2022 (millions)
State
1
Total
spending
on
benefits
Fee for service
Managed
care and
premium
assistance
Medicare
premiums
and
coinsurance CollectionsHospital Physician Dental
Other
practitioner
Clinic
and
health
center
Other
acute Drugs
Institutional
LTSS
Home- and
community-
based LTSS
Alabama
$7,166 $2,835 $483 $89 $108 $126 $712 $432 $1,172 $656 $140 $450 -$37
Alaska
2,436 755 173 94 41 499 184 106 235 329 1 43 -24
Arizona
20,258 1,377 62 5 18 375 1,242 230 105 8 16,327 509 -0
Arkansas
8,533 1,371 359 1 31 88 765 103 934 400 4,111 408 -38
California²
117,885 10,370 1,074 1,614 -45 4,058 12,640 6,786 3,893 23,408 51,517 3,572 -1,002
Colorado²
11,874 3,611 380 342 -0 874 351 471 854 2,396 2,464 244 -115
Connecticut
9,672 2,860 541 149 298 391 604 462 1,615 2,085 136 629 -96
Delaware³
3,137 87 9 53 1 3 116 -10 74 246 2,518 44 -4
District of
Columbia
3,648 287 23 5 5 164 328 96 442 646 1,575 81 -5
Florida
32,667 2,921 289 406 69 271 656 140 1,863 1,856 22,218 2,398 -421
Georgia
14,340 2,877 379 17 73 20 843 350 1,807 1,829 5,525 703 -84
Hawaii
2,990 37 0 33 0 27 34 0 10 156 2,688 52 -48
Idaho
3,195 824 186 – 54 54 267 189 200 527 829 95 -31
Illinois
25,956 2,590 184 16 29 74 1,090 1 1,106 1,170 19,017 765 -86
Indiana
16,851 1,438 220 23 11 197 794 161 3,039 2,250 8,369 409 -61
Iowa³
6,614 101 15 0 2 71 128 -2 38 56 6,092 196 -84
Kansas³
4,301 98 4 0 0 1 68 -1 81 0 3,927 145 -22
Kentucky
14,590 477 46 2 10 345 418 25 1,457 1,228 10,268 341 -27
Louisiana
14,674 1,349 39 – 1 32 334 51 1,602 914 9,918 518 -83
Maine
3,786 944 126 21 92 198 564 153 554 945 11 266 -86
Maryland
14,344 1,245 140 150 151 209 1,510 264 1,576 2,120 6,614 468 -102
Massachusetts
20,865 2,716 366 373 38 277 1,414 407 1,624 4,236 8,829 774 -189
Michigan
21,023 1,368 258 27 18 246 751 609 2,129 1,059 14,068 786 -297
Minnesota³
16,159 612 170 21 125 174 1,016 -314 1,172 4,920 8,122 279 -138
Mississippi
5,944 781 150 5 31 65 306 72 1,092 556 2,574 337 -26
Missouri
13,013 2,847 12 4 14 458 872 585 1,455 2,788 3,595 463 -79
Montana
2,344 938 158 61 84 85 299 135 188 303 53 63 -23
Nebraska³
3,296 39 2 0 0 0 56 -0 534 642 2,014 59 -50
Nevada
5,053 637 161 76 39 76 412 137 387 396 2,512 254 -35
New Hampshire³
2,461 248 4 22 1 4 164 -90 433 494 1,135 55 -9

MACStats: Medicaid and CHIP Data Book
49
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 17. (continued)
State
1
Total
spending
on
benefits
Fee for service
Managed
care and
premium
assistance
Medicare
premiums
and
coinsurance CollectionsHospital Physician Dental
Other
practitioner
Clinic
and
health
center
Other
acute Drugs
Institutional
LTSS
Home- and
community-
based LTSS
New Jersey
$20,873 $1,285 $54 $0 $18 $518 $1,178 $7 $1,372 $2,376 $13,759 $587 $-281
New Mexico
8,258 503 22 8 51 6 120 2 40 706 6,606 209 -15
New York³
80,518 8,752 277 14 155 1,189 4,262 -3,578 8,605 9,947 51,134 2,487 -2,727
North Carolina
18,404 2,388 325 350 55 160 1,076 212 2,111 1,131 10,104 670 -179
North Dakota
1,524 164 40 15 22 17 64 49 423 283 433 23 -9
Ohio
30,025 924 155 29 15 166 824 135 2,656 4,676 19,843 834 -232
Oklahoma
7,523 2,817 730 175 46 703 601 1,107 970 763 108 236 -731
Oregon
13,083 414 23 5 19 407 486 90 585 2,981 7,797 341 -65
Pennsylvania
41,178 1,884 33 6 1 62 509 12 1,362 3,924 32,617 976 -209
Rhode Island
3,393 366 10 4 0 18 245 2 295 417 1,963 88 -15
South Carolina
7,544 1,234 129 139 16 85 422 143 971 928 3,440 332 -294
South Dakota
1,246 309 68 24 7 65 100 87 231 317 1 47 -11
Tennessee
11,265 612 30 152 0 99 348 542 268 754 7,984 567 -90
Texas
54,942 8,384 122 12 2,305 24 2,474 448 1,693 2,933 37,585 1,725 -2,762
Utah
4,211 477 129 24 14 22 363 113 478 506 2,051 71 -36
Vermont³
1,884 100 15 7 13 9 1,360 -91 149 303 – 19 -1
Virginia³
17,824 3,044 241 279 6 90 366 -18 383 2,892 10,946 432 -838
Washington
17,141 877 92 191 10 1,068 914 620 1,097 4,279 12,369 565 -4,941
West Virginia
5,184 216 27 5 30 14 354 293 929 713 2,439 203 -40
Wisconsin
11,429 804 31 101 34 368 1,050 616 777 1,348 5,958 431 -89
Wyoming
668 142 70 12 2 49 30 42 139 166 2 23 -9
Subtotal
$787,191 $84,336 $8,639 $5,160 $4,115 $14,602 $46,085 $12,382 $57,205 $100,961 $444,305 $26,275 -$16,876
American Samoa
68 38 1 – – 7 21 0 – 0 – 2 –
Guam
167 83 18 3 0 2 37 22 1 1 – 2 –
N. Mariana
Islands
73 46 – 5 – 10 7 4 – 1 – 1 –
Puerto Rico
5,098 – – – – 60 31 323 – – 4,678 – 6
Virgin Islands
137 41 10 15 4 14 12 33 0 2 – 1 6
Total
$792,734 $84,544 $8,668 $5,183 $4,119 $14,694 $46,193 $12,764 $57,206 $100,964 $448,983 $26,281 -$16,865
Percent of total,
exclusive of
collections
– 10.4% 1.1% 0.6% 0.5% 1.8% 5.7% 1.6% 7.1% 12.5% 55.5% 3.2% –

December 2023
50
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 17. (continued)
Notes: FY is scal year. LTSS is long-term services and supports. Includes federal and state funds. Service category denitions and spending amounts shown
here may dier from other CMS data sources, such as the Transformed Medicaid Statistical Information System (T-MSIS). The specic services included in each
category have changed over time and therefore may not be directly comparable to earlier editions of MACStats. Collections include third-party liability, estate, and
other recoveries.
– Dash indicates zero; $0 or -$0 indicates an amount between $0.5 and -$0.5 million that rounds to zero.
Additional detail on categories:
• Hospital includes inpatient, outpatient, critical access hospital, and emergency hospital services as well as related disproportionate share hospital payments.
• Physician includes physician and surgical services.
• Clinic and health center includes non-hospital outpatient clinic, rural health clinic, federally qualied health center (FQHC), and freestanding birth center.
• Other acute includes lab or X-ray; sterilizations; abortions; early and periodic screening, diagnostic, and treatment (EPSDT) screenings; emergency services
for unauthorized aliens; non-emergency transportation; physical, occupational, speech, and hearing therapy; prosthetics, dentures, and eyeglasses; U.S.
Preventive Services Task Force (USPSTF) grade A or B preventive services and Advisory Committee on Immunization Practices (ACIP) vaccines; other
diagnostic screening and preventive services; school-based services; health home with chronic conditions; tobacco cessation for pregnant women; private
duty nursing; case management (excluding primary care case management); rehabilitative services; hospice; health home with substance use disorder; opioid
use disorder (OUD) medication assisted treatment (MAT) services; COVID-19 vaccine and administration; and other care not otherwise categorized.
• Drugs (including OUD MAT drugs) are net of rebates.
• Institutional LTSS includes nursing facility, intermediate care facility for individuals with intellectual disabilities, and mental health facility.
• Home- and community-based LTSS includes home health, waiver and state plan services, personal care, and certied community behavioral health clinic.
• Managed care and premium assistance includes comprehensive and limited-benet managed care plans, primary care case management, employer-
sponsored premium assistance programs, and Programs of All-Inclusive Care for the Elderly. Comprehensive plans account for more than 90 percent of
spending in the managed care category. Managed care also includes rebates for drugs (including OUD MAT drugs) provided by managed care plans and
managed care payments associated with the Community First Choice option, USPSTF grade A or B preventive services, ACIP vaccines, certied community
behavioral health clinic, and services subject to electronic visit verication requirements.
¹ All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
² State or territory reports negative spending in a category due to prior period adjustments. California and Colorado report negative spending for other practitioners.
³ State reports negative fee-for-service (FFS) drug spending after the application of drug rebates. The negative net amount may reect prior period adjustments,
a dierence in the timing of payments and rebates after a shift of some FFS drug spending into Medicaid managed care, or the state not separately reporting the
FFS and managed care drug rebates. Vermont shows negative drug spending because it reports most of its benet spending under other care services in its CMS-
64 submission.
Source: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023.

MACStats: Medicaid and CHIP Data Book
51
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
Notes: FY is scal year. LTSS is long-term services and supports. Includes federal and state funds. Excludes spending for
administration, the territories, and Medicaid-expansion CHIP enrollees. Children and adults under age 65 who qualify for Medicaid
on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through an aged, blind, or
disabled pathway are included in the aged category. Amounts are fee for service unless otherwise noted. Benet spending from
Transformed Medicaid Statistical Information System (T-MSIS) data has been adjusted to reect CMS-64 totals. With regard to
methods, spending totals exclude disproportionate share hospital (DSH) and certain incentive and uncompensated care pool
payments made under waiver expenditure authority of Section 1115 of the Social Security Act (the Act), which were previously
included before the December 2015 data book. See https://www.macpac.gov/macstats/data-sources-and-methods/ for additional
information. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between
T-MSIS and the Medicaid Statistical Information System (MSIS).
* Values less than 0.1 percent are not shown.
1
California, North Dakota, and Utah have a state plan amendment (SPA) that allows the state to receive the CHIP enhanced federal
medical assistance percentage (FMAP) for Medicaid children who would have, before January 1, 2014, been enrolled in CHIP if
not for the elimination of the Medicaid asset test. These children cannot be separately identied in the T-MSIS data. Because the
state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states
based on the proportion reported in their SPA. Correspondingly, we reduced child spending by $724.7 million.
2
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act. Newly
eligible adults include those who are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not
newly eligible adults include those who would have previously been eligible for Medicaid under the rules that a state had in place on
December 1, 2009; this includes states that had already expanded to adults with incomes greater than 100 percent of the federal
poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
3
Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g.,
parents and caretakers, pregnancy).
Sources: MACPAC, 2023, analysis of T-MSIS data as of February 2023 and analysis of CMS-64 nancial management report net
expenditure data as of June 2022.
Medicare premiums
LTSS institutional
LTSS non-institutiona
l
Managed care
Drugs
Non-hospital acute
Inpatient and
outpatient hospital
9.6%
11.4%
12.2%
16.1%
8.5%
4.0%
8.8%
15.8%
7.1%
10.6%
8.6%
4.9%
1.4%
1.4%
1.3%
2.4%
1.9%
0.2%
57.0%
68.8%
77.1%
68.5%
43.0%
42.6%
12.6%
1.5%
0.9% 1.1%
27.1%
16.8%
7.4%
1.0%
0.7%
0.7%
7.6%
22.2%
3.2%
*
0.6%
0.7%
3.3%
9.2%
EXHIBIT 18. Distribution of Medicaid Benet Spending by Eligibility Group and Service Category, FY 2021

December 2023
52
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
Notes: FY is scal year. LTSS is long-term services and supports. Includes federal and state funds. Excludes spending for
administration, the territories, and Medicaid-expansion CHIP enrollees. Children and adults under age 65 who qualify for Medicaid
on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through an aged, blind, or
disabled pathway are included in the aged category. Amounts are fee for service unless otherwise noted, and they reect all
enrollees, including those with limited benets. Benet spending from Transformed Medicaid Statistical Information System
(T-MSIS) data has been adjusted to reect CMS-64 totals. With regard to methods, spending totals exclude disproportionate share
hospital (DSH) and certain incentive and uncompensated care pool payments made under waiver expenditure authority of Section
1115 of the Social Security Act (the Act), which were previously included before the December 2015 data book. See https://www.
macpac.gov/macstats/data-sources-and-methods/ for additional information. Additionally, gures shown here may not be directly
comparable to prior years due to dierences in reporting between T-MSIS and the Medicaid Statistical Information System (MSIS).
1
California, North Dakota, and Utah have a state plan amendment (SPA) that allows the state to receive the CHIP enhanced
federal medical assistance percentage (FMAP) for Medicaid children who would have, before January 1, 2014, been enrolled
in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in the T-MSIS data.
Because the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending
in these states based on the proportion reported in their SPA. Correspondingly, we reduced child FYE by 242,500 and child
spending by $724.7 million.
2
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act. Newly
eligible adults include those who are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not
newly eligible adults include those who would have previously been eligible for Medicaid under the rules that a state had in place
on December 1, 2009; this includes states that had already expanded to adults with incomes greater than 100 percent of the
federal poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
3
Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g.,
parents and caretakers, pregnancy).
Sources: MACPAC, 2023, analysis of T-MSIS data as of February 2023 and analysis of CMS-64 nancial management report net
expenditure data as of June 2022.
LTSS institutional
LTSS non-institutional
Managed care
Drugs
Non-hospital acute
Inpatient and outpatient hospital
Medicare premiums
$832
$410
$915
$881
$2,024
$733
$764
$567 $535
$577
$2,062
$914
$120
$49 $96$131
$456
$42
$4,932
$2,465
$5,771
$3,739
$10,299
$7,893
$1,089
$55 $70$58
$6,492
$3,116
$639
$37 $55$36
$1,813
$4,114
$274
$1 $44$40
$790
$1,703
Allenrollees
$8,651
Child
1
$3,584
Newadult
group
2
$7,486
Otheradult
3
$5,462
Disabled
$23,935
Aged
$18,514
EXHIBIT 19. Medicaid Benet Spending Per Full-Year Equivalent Enrollee (FYE) by Eligibility Group and Service
Category, FY 2021

MACStats: Medicaid and CHIP Data Book
53
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
All enrollees
88.0 million
Benefit spending for LTSS
and all other services
$699.3 billion
Not using LTSS
Using LTSS: Non-institutional only,
no services under HCBS waiver
1
Using LTSS: Non-institutional only,
some with services under HCBS waiver
1
Using LTSS: Institutional only
Using LTSS: Both institutional and
non-institutional
4.9% of enrolles
(4.3 million) are
LTSS users
28.5% of spending ($199.1 billion)
is for LTSS users
0.2%
1.5%
1.0%
8.3%
2.0%
12.8%
1.8%
5.9%
95.1%
71.5%
Notes: FY is scal year. LTSS is long-term services and supports. HCBS is home- and community-based services. Includes
federal and state funds. Excludes spending on administration, the territories, and Medicaid-expansion CHIP enrollees. Benet
spending from Transformed Medicaid Statistical Information System (T-MSIS) data has been adjusted to reect CMS-64 totals,
and enrollment counts are unduplicated using unique national identication numbers. With regard to methods, spending totals
exclude disproportionate share hospital (DSH) and certain incentive and uncompensated care pool payments made under waiver
expenditure authority of Section 1115 of the Social Security Act (the Act), which were previously included before the December
2015 data book. See https://www.macpac.gov/macstats/data-sources-and-methods/ for additional information. Additionally,
gures shown here may not be directly comparable to prior years due to dierences in reporting between T-MSIS and the
Medicaid Statistical Information System (MSIS).
LTSS users are dened here as enrollees using at least one LTSS service during the year under a fee-for-service
arrangement. For example, an enrollee with a short stay in a nursing facility for rehabilitation following a hospital discharge and
an enrollee with permanent residence in a nursing facility would both be counted as LTSS users.
California, North Dakota, and Utah have a state plan amendment (SPA) that allows the state to receive the enhanced federal
medical assistance percentage (FMAP) for Medicaid children who would have, before January 1, 2014, been enrolled in CHIP
if not for the elimination of the Medicaid asset test. These children cannot be separately identied in the T-MSIS data. Because
the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in
these states based on the proportion reported in their SPA. Correspondingly, we reduced child enrollment by 242,500 and
spending by $724.7 million.
1
All states have HCBS waiver programs that provide a range of LTSS for targeted populations of non-institutionalized
enrollees who require institutional levels of care. The number of HCBS waiver enrollees and associated spending may
be dierent from other sources, such as the CMS-372 report (a state-reported source containing aggregate spending and
enrollment for HCBS waivers).
Sources: MACPAC, 2023, analysis of T-MSIS data as of February 2023 and analysis of CMS-64 nancial management report
net expenditure data as of June 2022.
EXHIBIT 20. Distribution of Medicaid Enrollment and Benet Spending by Users and Non-Users of Long-Term
Services and Supports, FY 2021

December 2023
54
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 21. Medicaid Spending by State, Eligibility Group, and Dually Eligible Status, FY 2021 (millions)
State Total
Basis of eligibility
1
Dually eligible status
2
All dually eligible
enrollees
Dually eligible with
full benets
Dually eligible with
limited benets
Child
New adult
group
3
Other
adult
4
Disabled Aged Total Age 65+ Total Age 65+ Total Age 65+
Total $699,301 15.2% 21.8% 10.7% 31.5% 20.8% $222,573 60.8% $213,571 60.7% $9,002 62.5%
Alabama 6,257 22.1 – 11.9 44.9 21.1 2,017 64.7 1,725 65.9 292 57.7
Alaska 2,146 22.5 25.3 15.9 23.4 13.0 496 52.5 494 52.4 2 76.1
Arizona
5
17,403 14.6 32.0 14.2 28.9 10.2 3,322 48.6 3,223 48.0 99 67.8
Arkansas 7,162 23.7 32.0 0.1 30.4 13.8 1,782 56.4 1,609 57.5 173 45.6
California
6
105,889 11.7 26.0 13.7 26.1 22.6 29,695 70.6 29,301 70.6 394 74.8
Colorado
7
10,568 14.3 33.9 6.2 29.7 15.8 2,667 61.4 2,585 61.2 82 67.4
Connecticut 9,180 13.2 26.7 12.4 22.8 24.9 3,416 60.1 3,019 58.6 397 71.4
Delaware 2,422 18.4 25.3 16.1
26.6 13.6 581 55.0 552 54.7 29 60.0
District of Columbia
8
3,254 10.4 16.9 11.9 38.6 22.2 1,002 66.5 969 66.2 33 75.2
Florida 26,723 22.1 – 13.1 36.1 28.7 11,026 66.7 9,889 67.0 1,138 63.9
Georgia 11,850 25.3 – 15.4 38.7 20.6 3,467 67.2 3,034 67.6 433 64.5
Hawaii
9
2,823 16.8 33.4 9.8 19.5 20.5 802 62.2 795 62.1 7 77.6
Idaho 2,876 16.9 23.6 8.1 38.0 13.4 808 42.4 753 41.6 55 53.5
Illinois
8
26,392 10.2 53.9 2.5 12.1 21.2 6,192 65.8 6,087 65.8 105 66.3
Indiana
7
15,506 12.4 24.8 21.8 22.7 18.3 4,793 62.1 4,622 62.5 171 53.3
Iowa 5,934 13.4 24.7 11.3 34.4 16.1 2,038 47.4 1,982 46.8 56 66.8
Kansas 3,934 20.9 – 11.6 45.3 22.2 1,630 49.2 1,560 49.2 71 48.5
Kentucky
5
14,238 14.2 38.2 8.9 28.4 10.3 2,649 54.7 2,432 55.6 216 43.9
Louisiana
7
12,489 14.7 37.6 5.1 29.8 12.8 2,706 56.2 2,408 56.3 298 55.3
Maine 3,398 14.0 16.1 8.1 40.7 21.1 1,457 48.6 1,354 47.0 103 69.3
Maryland 13,278 14.5 25.7 13.4 30.9 15.6 3,676 54.1 3,467 53.6 209 60.8
Massachusetts 19,038 9.0 15.6 11.3 38.0 26.1 8,513 55.2 8,443 54.9 69 95.6
Michigan 20,635 12.8 28.3 9.8 30.9 18.2 6,459 58.0 6,366 58.1 94 55.0
Minnesota 14,912 14.9 17.7 10.0 37.5 20.0 5,417 50.6 5,387 50.5 30 68.1
Mississippi 5,523 24.1 – 11.3 42.9 21.7 1,977 60.0 1,735 60.9 242 53.6

MACStats: Medicaid and CHIP Data Book
55
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 21. (continued)
State Total
Basis of eligibility
1
Dually eligible status
2
All dually eligible
enrollees
Dually eligible with
full benets
Dually eligible with
limited benets
Child
New adult
group
3
Other
adult
4
Disabled Aged Total Age 65+ Total Age 65+ Total Age 65+
Missouri $10,607 25.4% 0.9% 9.8% 46.1% 17.8% $3,894 42.9% $3,827 42.7% $67 54.7%
Montana 2,183 19.0 38.1 8.5 21.1 13.4 541 55.7 515 55.5 25 60.7
Nebraska
5
3,035 17.2 14.3 10.5 36.6 21.5 1,044 53.8 1,031 53.7 13 58.6
Nevada 4,666 15.9 41.8 8.2 22.5 11.6 873 58.8 744 58.1 129 63.0
New Hampshire 2,152 16.7 26.0 5.3 29.5 22.6 893 51.8 861 52.1 32 42.6
New Jersey 17,990 12.3 27.0 6.4 33.3 21.0 6,523 53.6 6,523 53.6 – –
New Mexico 6,844 19.7 30.8 13.2 24.6 11.7 1,438 56.3 1,324 55.6 114 64.6
New York 71,252 8.5 24.1 8.4 28.5 30.5 30,300 68.9 29,865 68.8 436 76.7
North Carolina 16,436
19.9 – 16.8 43.9 19.4
5,147 60.0 5,001 59.9 146 64.2
North Dakota
6
1,378 13.4 2.9 5.5 40.6 37.6 890 58.0 817 56.6 72 74.3
Ohio 26,956 13.7 23.2 11.3 33.8 18.0 7,827 51.3 7,503 51.3 324 51.6
Oklahoma 5,788 30.3 9.1 11.1 32.9 16.7 1,607 54.3 1,560 54.5 47 49.3
Oregon
7
11,165 10.6 42.2 1.4 21.5 24.4 3,506 74.0 3,373 74.5 133 62.0
Pennsylvania 36,392 11.1 20.5 5.7 40.3 22.4 14,238 57.1 14,039 57.1 198 60.6
Rhode Island 2,809 21.3 24.7 11.7 31.5 10.8 944 58.4 929 58.4 15 64.1
South Carolina 6,726 22.7 – 16.7 41.4 19.1 2,261 55.4 2,226 55.3 35 64.9
South Dakota 1,004 19.7 – 12.2 46.6 21.5 406 51.9 382 51.9 24 52.8
Tennessee 10,671 27.6 – 20.2 34.2 18.0 3,423 54.8 3,190 54.4 233 60.6
Texas
10
39,271 29.4 – 11.2 39.0 20.4 11,598 65.4 10,010 65.2 1,589 66.1
Utah
6
3,528 18.5 22.0 10.6 36.0 13.0 980 44.6 924 44.9 57 39.8
Vermont 1,533
11 11 11 11 11 11 11 11 11 11 11
Virginia 16,008 13.3 28.7 7.3 34.2 16.5 4,540 48.1 4,360 47.9 181 52.7
Washington 21,652 15.1 36.3 7.6 26.2 14.7 4,941 55.1 4,772 55.0 169 58.0
West Virginia 4,575 14.3 29.0 8.3 27.4 21.0 1,555 61.7 1,433 63.3 122 42.9
Wisconsin 10,253 14.1 – 24.4 40.6 21.0 3,933 52.3 3,910 52.1 23 74.8
Wyoming 598 21.8 – 12.7 41.7 23.8 259 54.1 249 54.1 10 52.5

December 2023
56
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 21. (continued)
Notes: FY is scal year. Includes federal and state funds. Excludes spending for administration, the territories, and Medicaid-expansion CHIP enrollees. Benet
spending from Transformed Medicaid Statistical Information System (T-MSIS) data has been adjusted to reect CMS-64 totals. With regard to methods, spending totals
exclude disproportionate share hospital (DSH) and certain incentive and uncompensated care pool payments made under waiver expenditure authority of Section 1115
of the Social Security Act (the Act), which were previously included before the December 2015 data book. See https://www.macpac.gov/macstats/data-sources-and-
methods/ for additional information. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between T-MSIS and
the Medicaid Statistical Information System (MSIS).
– Dash indicates zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
Children and adults under age 65 who qualify for Medicaid on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through
an aged, blind, or disabled pathway are included in the aged category.
2
Dually eligible enrollees are covered by both Medicaid and Medicare. Those with limited benets receive only Medicaid assistance with Medicare premiums and cost
sharing.
3
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act. Newly eligible adults include those who are
not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who would have previously been eligible
for Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to adults with incomes greater than 100
percent of the federal poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
4
Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers, pregnancy).
5
State reported CMS-64 spending that shows a dierence greater than 20 percent when compared to the prior year. Arizona's spending on the CMS-64 was 23.0
percent higher compared with 2020. Kentucky's spending on the CMS-64 was 21.4 percent higher compared with 2020. Nebraska's spending on the CMS-64 was 33.9
percent higher compared with 2020.
6
State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children who
would have, before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in the
T-MSIS data. Because the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states based
on the proportion reported in their SPA. Correspondingly, we reduced California's child spending by approximately $681.9 million, North Dakota's child spending by
approximately $9.3 million, and Utah's child spending by approximately $33.5 million.
7
State reported a large shift of enrollees between eligibility groups. Colorado reported a 35 percent increase in the new adult group and a 46 percent decrease for
the other adult group. Indiana reported a 16 percent decrease for the new adult group and a 60 percent increase for the other adult group. Louisiana reported a 15
percent increase in the new adult group and a 10 percent decrease in the other adult group. Oregon reported a 33 percent increase in the new adult group, a 69 percent
decrease in the other adult group, a 102 percent increase in the disabled group, and a 53 percent increase in the aged group.
8
State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The District of
Columbia's average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than the benchmark.
9
Spending total excludes a small amount of fee-for-service (FFS) drug spending reported on the CMS-64 because there were no FFS drug claims reported in T-MSIS.
10
State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
11
Due to large dierences in the way spending is reported by Vermont in CMS-64 and T-MSIS data, MACPAC’s adjustment methodology is applied only to total
Medicaid spending.
Sources: MACPAC, 2023, analysis of T-MSIS data as of February 2023 and analysis of CMS-64 nancial management report net expenditure data as of June 2022.

MACStats: Medicaid and CHIP Data Book
57
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
Notes: FY is scal year. Includes federal and state funds. Excludes spending for administration, the territories, and Medicaid-expansion CHIP enrollees. Benet
spending from Transformed Medicaid Statistical Information System (T-MSIS) data has been adjusted to reect CMS-64 totals. With regard to methods, spending totals
exclude disproportionate share hospital (DSH) and certain incentive and uncompensated care pool payments made under waiver expenditure authority of Section 1115
of the Social Security Act (the Act), which were previously included before the December 2015 data book. See https://www.macpac.gov/macstats/data-sources-and-
methods/ for additional information. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between T-MSIS and
the Medicaid Statistical Information System (MSIS).
– Dash indicates zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
Children and adults under age 65 who qualify for Medicaid on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through
an aged, blind, or disabled pathway are included in the aged category.
2
Dually eligible enrollees are covered by both Medicaid and Medicare. Those with limited benets receive only Medicaid assistance with Medicare premiums and cost
sharing.
3
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act. Newly eligible adults include those who are
not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who would have previously been eligible
for Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to adults with incomes greater than 100
percent of the federal poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
4
Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers, pregnancy).
5
State reported CMS-64 spending that shows a dierence greater than 20 percent when compared to the prior year. Arizona's spending on the CMS-64 was 23.0
percent higher compared with 2020. Kentucky's spending on the CMS-64 was 21.4 percent higher compared with 2020. Nebraska's spending on the CMS-64 was 33.9
percent higher compared with 2020.
6
State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children who
would have, before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in the
T-MSIS data. Because the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states based
on the proportion reported in their SPA. Correspondingly, we reduced California's child spending by approximately $681.9 million, North Dakota's child spending by
approximately $9.3 million, and Utah's child spending by approximately $33.5 million.
7
State reported a large shift of enrollees between eligibility groups. Colorado reported a 35 percent increase in the new adult group and a 46 percent decrease for
the other adult group. Indiana reported a 16 percent decrease for the new adult group and a 60 percent increase for the other adult group. Louisiana reported a 15
percent increase in the new adult group and a 10 percent decrease in the other adult group. Oregon reported a 33 percent increase in the new adult group, a 69 percent
decrease in the other adult group, a 102 percent increase in the disabled group, and a 53 percent increase in the aged group.
8
State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The District of
Columbia's average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than the benchmark.
9
Spending total excludes a small amount of fee-for-service (FFS) drug spending reported on the CMS-64 because there were no FFS drug claims reported in T-MSIS.
10
State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
11
Due to large dierences in the way spending is reported by Vermont in CMS-64 and T-MSIS data, MACPAC’s adjustment methodology is applied only to total
Medicaid spending.
Sources: MACPAC, 2023, analysis of T-MSIS data as of February 2023 and analysis of CMS-64 nancial management report net expenditure data as of June 2022.
EXHIBIT 22. Medicaid Benet Spending Per Full-Year Equivalent Enrollee (FYE) by State and Eligibility Group, FY 2021
State
Total Child New adult group
1
Other adult
2
Disabled Aged
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
Total $8,651 $9,175 $3,584 $3,591 $7,486 $7,508 $5,462 $6,388 $23,935 $26,762 $18,514 $24,247
Alabama 5,835 6,848 2,641 2,641 – – 3,474 5,032 13,451 17,454 10,497 24,247
Alaska 9,050 9,083 5,110 5,110 8,205 8,205 7,093 7,093 32,182 32,698 21,447 22,789
Arizona
4
8,305 8,921 3,543 3,584 9,163 9,613 5,916 6,930 29,098 31,658 9,955 12,484
Arkansas 7,490 7,850 4,062 4,061 7,191 7,190 5,957 5,957 15,013 18,711 13,456 21,862
California
5
8,336 8,811 3,667 3,674 6,367 6,222 5,283 6,562 31,553 31,649 17,137 17,311
Colorado
6
7,460 7,629 3,095 3,095 5,743 5,743 5,689 5,732 29,966 33,521 20,403 30,725
Connecticut 8,444 9,249 3,565 3,567 7,421 7,325 5,431 5,790 33,499 55,991 15,772 43,581
Delaware 9,031 9,877 4,506 4,546 8,029 8,031 7,840 9,313 25,866 34,100 17,814 38,115
District of Columbia
7
12,434 12,871 4,698 4,698 7,205 7,205 7,070 7,049 39,815 42,989 26,788 38,954
Florida 5,750 6,124 2,507 2,508 – – 3,587 3,814 15,344 18,059 11,182 17,444
Georgia 5,315 5,830 2,474 2,470 – – 4,204 4,894 13,416 16,442 10,029 20,822
Hawaii
8
7,185 7,247 3,644 3,644 6,252 6,178 5,485 5,461 25,720 27,420 14,502 16,311
Idaho 7,529 7,827 3,142 3,142 6,113 6,113 6,364 6,365 22,037 26,007 12,858 20,993
Illinois
7
8,629 8,731 4,130 4,133 7,831 7,822 6,217 6,051 16,289 17,332 19,816 21,946
Indiana
6
8,852 9,390 2,883 2,921 9,020 9,112 9,424 10,642 19,590 22,634 23,217 33,463
Iowa 8,307 8,490 3,094
3,094 6,572 6,548 6,238 6,296 25,040 27,011 21,614 30,537
Kansas 9,653 10,096 3,634 3,634 – – 6,813 6,488 23,988 28,112 21,861 32,651
Kentucky
4
8,949 9,342 4,578 4,574 8,034 8,016 8,172 8,175 19,000 23,496 14,132 23,608
Louisiana
6
7,315 7,657 3,212 3,210 7,121 7,123 6,617 6,711 15,969 19,166 10,885 18,475
Maine 8,938 10,772 4,723 4,894 6,477 6,573 3,596 5,670 22,640 26,318 12,500 24,564
Maryland 9,220 9,555 3,574 3,560 8,721 8,724 6,444 6,449 29,182 34,388 21,509 36,207
Massachusetts 10,466 11,879 4,203 4,494 7,656 8,019 4,624 6,082 21,626 21,747 22,355 27,633
Michigan 7,416 7,558 2,756 2,764 6,439 6,488 5,167 5,272 18,696 19,657 20,283 23,295
Minnesota 12,150 12,367 3,956 3,961 10,584 10,572 6,933 7,210 48,296 50,230 34,844 38,879
Mississippi 7,171 8,044 3,339 3,340 – – 5,217 6,557 15,134 18,947 12,497 23,750
Missouri 9,634 9,889 4,309
4,309 6,043
6,034 6,202 6,202 25,841 27,939 18,457 22,470
Montana 8,219 8,432 4,241 4,241 8,015 8,013 7,279 7,664 20,520 23,228 17,686 24,912
Nebraska
4
10,509 10,654 3,651 3,649 9,765 9,749 8,028 8,019 28,948 30,430 27,701 31,744

December 2023
58
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 22. (continued)
State
Total Child New adult group
1
Other adult
2
Disabled Aged
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
All
enrollees
Full-
benefit
enrollees
3
Nevada $5,943 $6,141 $2,522 $2,522 $6,451 $6,446 $5,222 $5,045 $17,430 $23,038 $9,865 $21,031
New Hampshire 9,563 10,383 4,494 4,522 7,182 7,185 4,659 6,704 24,151 31,498 29,170 44,119
New Jersey 10,278 10,201 3,594 3,585 7,263 7,166 7,672 7,374 35,749 35,725 25,462 25,340
New Mexico 7,716 8,332 4,284 4,287 7,301 7,360 5,968 7,231 23,305 29,934 13,246 27,521
New York 10,670 10,884 3,325 3,326 6,968 6,969 5,950 5,972 33,555 35,689 27,920 32,830
North Carolina 7,223 8,881 3,437 3,450 – – 3,542 6,541 21,011 22,626 15,996 20,859
North Dakota
5
12,921 12,535 4,221 4,221 1,417 1,389 5,591 5,590 46,190 47,806 56,783 62,878
Ohio 9,202 9,508 3,560 3,557 7,980 7,964 6,163 6,142 23,281 27,105 21,753 30,555
Oklahoma 6,553 6,986 3,865 3,865 4,588 5,445 4,706 5,260 17,174 18,886 14,010 17,039
Oregon
6
10,154 10,969 4,222 4,236 7,737 8,046 4,327 10,692 25,846 30,570 33,065 51,801
Pennsylvania 11,726 12,102 4,312 4,334 7,544 7,556 6,611 6,902 25,483 27,066 28,234 34,349
Rhode Island 9,062 9,264 6,899 6,900 7,431 7,430 5,176 5,250 22,542 23,984 11,162 13,303
South Carolina 5,191 6,150 2,562 2,572 – – 2,609 4,668 16,681 16,947 12,829 13,834
South Dakota 8,439 8,824 2,896 2,896 – – 6,179 6,179 24,254 28,979 18,523 28,012
Tennessee 6,567 6,933 3,669 3,669 – – 5,152 5,152 14,165 16,802 13,099 24,356
Texas
9
7,592 8,379 3,709 3,700 2,817 2,817 5,052 8,381 22,814 26,417 15,404 25,052
Utah
5
8,989 9,063 3,634 3,663 8,335 8,343 6,837 7,578 28,481 28,703 21,669 22,326
Vermont 8,313
10 10 10 10 10 10 10 10 10 10 10
Virginia 9,603 10,164 3,789 3,789 8,410 8,388 4,689 5,667 30,747 36,146 20,085 26,790
Washington 11,064 11,272 4,227 4,229 10,887 10,885 11,014 10,278 32,223 37,329 23,961 31,820
West Virginia 7,845 8,247 3,501 3,501 6,529 6,465 6,790 6,870 14,011 17,199 20,019 33,795
Wisconsin 7,868 8,179 3,066 3,072 – – 4,934 5,286 22,343 22,740 15,407 16,508
Wyoming 8,544 8,996 3,257 3,258 – – 6,207 6,201 22,285 26,549 21,787 34,656
Notes: FY is scal year. Full-year equivalent (FYE) may also be referred to as average monthly enrollment. Includes federal and state funds. Excludes spending
for administration, the territories, and Medicaid-expansion CHIP enrollees. Children and adults under age 65 who qualify for Medicaid on the basis of disability
are included in the disabled category. Individuals age 65 and older eligible through an aged, blind, or disabled pathway are included in the aged category. Benet
spending from Transformed Medicaid Statistical Information System (T-MSIS) data has been adjusted to reect CMS-64 totals. With regard to methods, spending
totals exclude disproportionate share hospital (DSH) and certain incentive and uncompensated care pool payments made under waiver expenditure authority of
Section 1115 of the Social Security Act (the Act), which were previously included before the December 2015 data book. See https://www.macpac.gov/macstats/
data-sources-and-methods/ for additional information. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting
between T-MSIS and the Medicaid Statistical Information System (MSIS).

MACStats: Medicaid and CHIP Data Book
59
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 22. (continued)
– Dash indicates zero.
1
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act. Newly eligible adults include those who
are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who would have previously
been eligible for Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to adults with incomes
greater than 100 percent of the federal poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
2
Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers,
pregnancy).
3
In this table, full-benet enrollees excludes those reported by states in T-MSIS as receiving coverage of only family planning services, assistance with Medicare
premiums and cost sharing, emergency services, or COVID-19 diagnostic products or testing-related services.
4
State reported CMS-64 spending that shows a dierence greater than 20 percent when compared to the prior year. Arizona's spending on the CMS-64 was 23.0
percent higher compared with 2020. Kentucky's spending on the CMS-64 was 21.4 percent higher compared with 2020. Nebraska's spending on the CMS-64 was
33.9 percent higher compared with 2020.
5
State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children who
would have, before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in
the T-MSIS data. Because the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states
based on the proportion reported in their SPA. Correspondingly, we reduced California's child FYE enrollment by approximately 229,000 and spending by $681.9
million, North Dakota's child FYE enrollment by approximately 2,600 and spending by $9.3 million, and Utah's child FYE enrollment by approximately 10,900 and
spending by $33.5 million.
6
State reported a large shift of enrollees between eligibility groups. Colorado reported a 54 percent increase in the new adult group and a 41 percent decrease for
the other adult group. Indiana reported a 1.2 percent increase for the new adult group and an 80 percent increase for the other adult group. Louisiana reported a
28 percent increase in the new adult group and a 0.5 percent increase in the other adult group. Oregon reported a 45 percent increase in the new adult group, a 67
percent decrease in the other adult group, a 76 percent increase in the disabled group, and a 32 percent increase in the aged group.
7
State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The
District of Columbia's average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than
the benchmark.
8
Spending total excludes a small amount of fee-for-service (FFS) drug spending reported on the CMS-64 because there were no FFS drug claims reported in
T-MSIS.
9
State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
10
Due to large dierences in the way spending is reported by Vermont in CMS-64 and T-MSIS data, MACPAC’s adjustment methodology is applied only to total
Medicaid spending.
Sources: MACPAC, 2023, analysis of T-MSIS data as of February 2023 and analysis of CMS-64 nancial management report net expenditure data as of June 2022.

December 2023
60
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 23. Medicaid Benet Spending per Full-Year Equivalent Enrollee for Newly Eligible Adult and All Enrollees by State, FY 2022
State
1
All Medicaid enrollees Newly eligible adults
2
FYE enrollees
Medicaid benet
spending
Spending per
FYE enrollee FYE enrollees
Medicaid benet
spending
Spending per
FYE enrollee
Alabama 1,263,175 $7,166,453,694 $5,673 – – –
Alaska 251,282 2,435,528,905 9,692 70,665 $642,524,948 $9,093
Arizona 2,325,631 20,257,896,179 8,711 190,602 1,074,112,696 5,635
Arkansas 1,017,974 8,533,079,808 8,382 326,938 2,852,307,635 8,724
California 14,339,675 117,884,562,290 8,221 4,713,543 31,626,470,705 6,710
Colorado 1,599,514 11,873,695,582 7,423 574,326 2,969,913,633 5,171
Connecticut 1,126,626 9,671,697,756 8,585 334,448 2,191,679,409 6,553
Delaware 273,247 3,136,940,055 11,480 13,861 116,549,173 8,409
District of Columbia 291,798 3,647,665,830 12,501 85,249 598,847,121 7,025
Florida 5,186,843 32,667,454,330 6,298 – – –
Georgia 2,464,300 14,339,599,611 5,819 – – –
Hawaii 446,691 2,990,024,469 6,694 30,443 916,051,591 30,091
Idaho 440,396 3,195,270,944 7,255 119,719 722,183,050 6,032
Illinois 3,276,552 25,956,045,305 7,922 849,801 7,004,360,250 8,242
Indiana 1,937,898 16,850,885,790 8,695 550,604 4,028,880,849 7,317
Iowa 754,159 6,614,098,328 8,770 192,808 1,320,326,430 6,848
Kansas 444,559 4,301,338,042 9,676 – – –
Kentucky 1,514,661 14,590,469,639 9,633
604,721 5,017,487,034 8,297
Louisiana 2,511,066 14,673,978,206 5,844 1,278,115 5,329,608,850 4,170
Maine 371,823 3,785,788,570 10,182 78,104 – –
Maryland 1,851,480 14,343,522,494 7,747 764,001 3,659,001,179 4,789
Massachusetts 2,079,423 20,864,779,727 10,034 – – –
Michigan 2,945,520 21,023,267,979 7,137 929,409 5,616,414,579 6,043
Minnesota 1,316,731 16,158,756,247 12,272 285,383 3,024,984,462 10,600
Mississippi 806,859 5,943,740,111 7,367 – – –
Missouri 1,234,226 13,013,125,297 10,544 130,329 1,010,444,979 7,753

MACStats: Medicaid and CHIP Data Book
61
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 23. (continued)
State
1
All Medicaid enrollees Newly eligible adults
2
FYE enrollees
Medicaid benet
spending
Spending per
FYE enrollee FYE enrollees
Medicaid benet
spending
Spending per
FYE enrollee
Montana 294,335 $2,343,639,013 $7,962 114,925 $1,025,685,648 $8,925
Nebraska 366,346 3,295,908,995 8,997 66,223 671,513,915 10,140
Nevada 799,602 5,052,662,737 6,319 343,249 2,038,489,951 5,939
New Hampshire 229,868 2,460,870,676 10,706 87,629 475,895,902 5,431
New Jersey 1,997,102 20,872,611,334 10,451 730,318 6,091,175,975 8,340
New Mexico 967,813 8,257,965,730 8,533 293,868 2,361,892,528 8,037
New York 7,436,108 80,518,406,335 10,828 431,234 2,572,447,961 5,965
North Carolina 2,737,528 18,403,697,744 6,723 – – –
North Dakota 122,969 1,524,148,076 12,395 30,645 441,551,499 14,409
Ohio 3,432,005 30,024,849,008 8,748 820,796 7,315,239,420 8,912
Oklahoma 1,121,392 7,523,240,743 6,709 275,791 2,012,618,979 7,298
Oregon 1,240,155 13,083,208,627 10,550 582,360 4,450,926,990 7,643
Pennsylvania 3,484,071 41,178,251,107 11,819 1,046,001 7,744,544,458 7,404
Rhode Island 343,092 3,392,593,755 9,888 94,233 826,871,497 8,775
South Carolina 1,514,365 7,544,266,509 4,982 – – –
South Dakota 129,088 1,246,309,725 9,655 – – –
Tennessee 1,793,620 11,264,609,657 6,280 – – –
Texas 5,675,484 54,941,921,302 9,681
– – –
Utah 479,778 4,211,452,614 8,778 119,798 1,069,685,545 8,929
Vermont 197,893 1,884,369,967 9,522 – – –
Virginia 1,819,324 17,823,746,172 9,797 641,093 5,713,323,393 8,912
Washington 2,082,453 17,140,713,645 8,231 776,271 7,232,054,375 9,316
West Virginia 634,581 5,183,933,490 8,169 228,404 1,351,794,647 5,918
Wisconsin 1,495,312 11,429,134,969 7,643 – – –
Wyoming 79,222 668,371,415 8,437 – – –
Subtotal (states) 92,545,614 $787,190,548,533 $8,506 18,805,907 $133,117,861,256 $7,079

December 2023
62
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 23. (continued)
State
1
All Medicaid enrollees Newly eligible adults
2
FYE enrollees
Medicaid benet
spending
Spending per
FYE enrollee FYE enrollees
Medicaid benet
spending
Spending per
FYE enrollee
American Samoa 31,434 $68,475,260 $2,178 – – –
Guam 38,927 167,053,407 4,291 – – –
Northern Mariana Islands 17,971 73,254,850 4,076 – – –
Puerto Rico 1,454,462 5,097,773,472 3,505 – – –
Virgin Islands 36,311 137,287,976 3,781 – – –
Total (states and
territories)
94,124,719 $792,734,393,498 $8,422 18,805,907 $133,117,861,256 $7,079
Notes: FY is scal year. FYE is full-year equivalent. FYE may also be referred to as average monthly enrollment. Includes federal and state funds. Excludes
spending for administration and Medicaid-expansion CHIP enrollees. Enrollment counts come from CMS-64 enrollment data and may dier from other data
sources. Quarterly enrollment was tabulated from the most recent non-zero CMS-64 submission to account for any lag in reporting; this typically is the report
submitted three quarters later (e.g., January–March 2022 enrollment was taken from the submission quarter ending December 31, 2022). Unlike other MACStats
exhibits that show spending per FYE, this exhibit includes spending for disproportionate share hospital (DSH) and certain incentive and uncompensated care pool
payments made under waiver expenditure authority of the Social Security Act (the Act).
– Dash indicates zero.
1
All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
2
Newly eligible adults include those enrollees who are newly eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act and receive a federal matching rate of 90
percent in FY 2022.
Source: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64 enrollment reports as of October 25, 2023.

MACStats: Medicaid and CHIP Data Book
63
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 24. Medicaid Supplemental Payments to Hospital Providers by State, FY 2022 (millions)
State
1
Inpatient and outpatient hospitals
2
Total Medicaid
payments DSH payments
Non-DSH supplemental
payments
Section 1115 waiver
authority payments
Supplemental payments
as % of total
Total $87,955.0 $14,971.3 $20,773.6 $10,223.6 52.3%
Alabama 2,835.4 308.8 1,437.5 – 61.6
Alaska
3
754.5 -0.5 – – -0.1
Arizona
4
1,377.4 127.2 391.2 23.9 39.4
Arkansas 1,371.3 26.6 493.2 – 37.9
California
5, 6
13,698.8 595.7 4,804.9 3,329.0 63.7
Colorado 3,611.0 210.1 1,457.8 – 46.2
Connecticut 2,859.5 79.1 600.0 – 23.8
Delaware 87.5 25.3 – – 29.0
District of Columbia 287.3 121.4 – – 42.3
Florida
6
2,920.8 239.8 780.7 1,147.5 74.2
Georgia 2,876.8 564.2 666.0 – 42.8
Hawaii 37.0 – 0.7 – 1.8
Idaho 824.4 27.8 24.3 – 6.3
Illinois 2,589.9 507.9 560.6 – 41.3
Indiana 1,438.1 619.4 39.4 – 45.8
Iowa 100.8 10.0 52.6 – 62.1
Kansas
5, 6
98.0 65.5 0.2 13.8 81.2
Kentucky 477.1 13.6 258.5 – 57.0
Louisiana 1,349.2 1,074.4 87.5 – 86.1
Maine 943.5 – 124.7 – 13.2
Maryland 1,244.9 136.2 26.5 – 13.1
Massachusetts
4, 5, 6
3,000.7 – 177.5 576.8 25.1
Michigan 1,368.0 445.2 471.5 – 67.0
Minnesota 611.7 49.9 191.4 – 39.4
Mississippi 780.5 245.7 40.3 – 36.6
Missouri 2,846.7 628.0 211.7 – 29.5
Montana 937.7 – 393.2 – 41.9
Nebraska 39.3 39.9 – – 101.6
Nevada 636.8 144.9 159.5 – 47.8
New Hampshire
5
248.1 197.1 29.5 0.3 91.5
New Jersey 1,284.7 570.8 242.0 – 63.3
New Mexico
5
503.0 33.6 228.2 12.0 54.4
New York 8,752.2 3,321.2 121.4 – 39.3
North Carolina 2,388.0 434.4 345.8 – 32.7
North Dakota 164.0 0.5 1.9 – 1.5
Ohio 923.8 117.6 – – 12.7
Oklahoma 2,816.8 61.7 1,111.3 – 41.6

December 2023
64
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 24. (continued)
State
1
Inpatient and outpatient hospitals
2
Total Medicaid
payments DSH payments
Non-DSH supplemental
payments
Section 1115 waiver
authority payments
Supplemental payments
as % of total
Oregon $414.0 $68.2 $129.3 – 47.7%
Pennsylvania 1,884.0 919.6 571.1 – 79.1
Rhode Island
4
366.6 160.0 36.8 $17.3 58.4
South Carolina 1,234.2 529.7 150.8 – 55.1
South Dakota 309.2 0.9 3.1 – 1.3
Tennessee 611.7 71.9 502.5 – 93.9
Texas
5, 6
8,385.4 1,565.9 838.4 5,100.1 89.5
Utah 477.4 33.7 63.6 – 20.4
Vermont
5
103.2 46.4 – 2.9 47.7
Virginia 3,044.1 42.3 2,690.8 – 89.8
Washington 877.2 277.0 153.7 – 49.1
West Virginia 216.1 69.0 14.6 – 38.7
Wisconsin 804.5 143.1 52.8 – 24.3
Wyoming 142.2 0.5 34.4 – 24.6
Notes: FY is scal year. DSH is disproportionate share hospital. Includes federal and state funds. Section 1115 refers to Section 1115 of the Social Security Act
(the Act). Excludes payments made under managed care arrangements. All amounts in this table are as reported by states in CMS-64 data during the scal year to
obtain federal matching funds; amounts include expenditures for the current scal year and adjustments to expenditures for prior scal years that may be positive
or negative. Amounts reported by states for any given category (e.g., inpatient hospital) sometimes show substantial annual uctuations. Some uctuation in
supplemental payments may reect the fact that states may not consistently classify payments in the same way over time.
– Dash indicates zero. $0.0 or -$0.0 indicates a value between $0.05 million and -$0.05 million that rounds to zero. 0.0% or -0.0% indicates a value between 0.05%
and -0.05% that rounds to zero.
1
All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
2
Includes inpatient, outpatient, critical access hospital, and emergency hospital categories in the CMS-64 data. The CMS-64 instructions to states note that DSH
payments are those made in accordance with Section 1923 of the Act. Non-DSH supplemental payments are described in the CMS-64 instructions to states as those
made in addition to the standard fee schedule or other standard payment for a given service. They include payments made under institutional upper payment limit
rules and payments to hospitals for graduate medical education. Section 1115 waiver expenditure authority payments include those made under uncompensated
care pools, delivery system reform incentive payments (DSRIP), and other non-DSH supplemental payments that have been authorized under Section 1115 waivers.
Because the majority of DSRIP payments go to hospitals, DSRIP payments that were reported as other care services on the CMS-64 were included in the Section
1115 waiver expenditure category and the total hospital payment category.
3
State reports negative DSH payments due to prior period adjustments.
4
State made other supplemental payments under Section 1115 waiver expenditure authority.
5
State made supplemental payments through a DSRIP or DSRIP-like program under Section 1115 waiver expenditure authority.
6
State made supplemental payments through an uncompensated care pool under Section 1115 waiver expenditure authority.
Source: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64 Schedule C waiver report data as of September 29, 2023.

MACStats: Medicaid and CHIP Data Book
65
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
State
1
Inpatient and outpatient hospitals
2
Total Medicaid
payments DSH payments
Non-DSH supplemental
payments
Section 1115 waiver
authority payments
Supplemental payments
as % of total
Oregon $414.0 $68.2 $129.3 – 47.7%
Pennsylvania 1,884.0 919.6 571.1 – 79.1
Rhode Island
4
366.6 160.0 36.8 $17.3 58.4
South Carolina 1,234.2 529.7 150.8 – 55.1
South Dakota 309.2 0.9 3.1 – 1.3
Tennessee 611.7 71.9 502.5 – 93.9
Texas
5, 6
8,385.4 1,565.9 838.4 5,100.1 89.5
Utah 477.4 33.7 63.6 – 20.4
Vermont
5
103.2 46.4 – 2.9 47.7
Virginia 3,044.1 42.3 2,690.8 – 89.8
Washington 877.2 277.0 153.7 – 49.1
West Virginia 216.1 69.0 14.6 – 38.7
Wisconsin 804.5 143.1 52.8 – 24.3
Wyoming 142.2 0.5 34.4 – 24.6
Notes: FY is scal year. DSH is disproportionate share hospital. Includes federal and state funds. Section 1115 refers to Section 1115 of the Social Security Act
(the Act). Excludes payments made under managed care arrangements. All amounts in this table are as reported by states in CMS-64 data during the scal year to
obtain federal matching funds; amounts include expenditures for the current scal year and adjustments to expenditures for prior scal years that may be positive
or negative. Amounts reported by states for any given category (e.g., inpatient hospital) sometimes show substantial annual uctuations. Some uctuation in
supplemental payments may reect the fact that states may not consistently classify payments in the same way over time.
– Dash indicates zero. $0.0 or -$0.0 indicates a value between $0.05 million and -$0.05 million that rounds to zero. 0.0% or -0.0% indicates a value between 0.05%
and -0.05% that rounds to zero.
1
All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
2
Includes inpatient, outpatient, critical access hospital, and emergency hospital categories in the CMS-64 data. The CMS-64 instructions to states note that DSH
payments are those made in accordance with Section 1923 of the Act. Non-DSH supplemental payments are described in the CMS-64 instructions to states as those
made in addition to the standard fee schedule or other standard payment for a given service. They include payments made under institutional upper payment limit
rules and payments to hospitals for graduate medical education. Section 1115 waiver expenditure authority payments include those made under uncompensated
care pools, delivery system reform incentive payments (DSRIP), and other non-DSH supplemental payments that have been authorized under Section 1115 waivers.
Because the majority of DSRIP payments go to hospitals, DSRIP payments that were reported as other care services on the CMS-64 were included in the Section
1115 waiver expenditure category and the total hospital payment category.
3
State reports negative DSH payments due to prior period adjustments.
4
State made other supplemental payments under Section 1115 waiver expenditure authority.
5
State made supplemental payments through a DSRIP or DSRIP-like program under Section 1115 waiver expenditure authority.
6
State made supplemental payments through an uncompensated care pool under Section 1115 waiver expenditure authority.
Source: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64 Schedule C waiver report data as of September 29, 2023.
EXHIBIT 25. Medicaid Supplemental Payments to Non-Hospital Providers by State, FY 2022 (millions)
State
1
Mental health facilities
2
Nursing facilities and ICF/IDs
3
Physicians and other practitioners
4
Total
Medicaid
payments
Supplemental
payments
Supplemental
payments as
% of total
Total
Medicaid
payments
Supplemental
payments
Supplemental
payments as
% of total
Total
Medicaid
payments
Supplemental
payments
Supplemental
payments as
% of total
Total $6,758.8 $3,095.5 45.8% $50,446.7 $3,058.9 6.1% $12,315.2 $4,087.0 33.2%
Alabama 67.6 3.2 4.8 1,103.9 – – 514.3 – –
Alaska 30.6 11.5 37.7 204.7 – – 214.2 – –
Arizona 36.4 28.5 78.3 68.4 12.9 18.9 69.6 – –
Arkansas 14.1 – – 919.9 – – 385.6 41.0 10.6
California 599.6 0.1 0.0 3,293.7 205.2 6.2 1,025.4 609.3 59.4
Colorado 9.6 – – 844.9 165.8 19.6 380.2 173.8 45.7
Connecticut 263.7 105.6 40.0 1,351.2 – – 838.7 29.4 3.5
Delaware 31.2 17.3 55.5 42.3 – – 9.7 – –
District of Columbia 29.1 3.8 13.0 412.8 2.5 0.6 24.8 4.5
18.1
Florida
5
1,302.8 128.2 9.8 560.3 – – 357.1 207.3 58.0
Georgia 7.1 – – 1,800.2 259.9 14.4 452.0 97.4 21.5
Hawaii – – – 10.4 – – 0.1 – –
Idaho 5.0 – – 195.1 92.1 47.2 240.0 – –
Illinois 118.4 89.4 75.5 987.8 – – 199.6 – –
Indiana
6
39.6 -41.2 -104.1 2,999.3 1,013.0 33.8 229.6 28.9 12.6
Iowa 1.2 – – 37.2 – – 16.3 5.8 35.7
Kansas 18.1 18.1 99.8 63.2 – – 4.0 0.2 6.1
Kentucky 39.4 35.6 90.2 1,417.5 0.6 0.0 51.1 20.0 39.2
Louisiana 104.0 97.8 94.0 1,497.6 2.7 0.2 39.7 9.2 23.1
Maine 129.2 58.5 45.3 424.8 – – 191.5 1.3 0.7
Maryland 287.5 61.6 21.4 1,288.2 – – 234.3 – –
Massachusetts
7
207.4 169.4 81.7 1,416.4 58.4 4.1 368.8 2.2 0.6
Michigan 211.7 163.4 77.2 1,917.7 369.6 19.3 266.6 142.3 53.4
Minnesota 82.8 0.4 0.5 1,089.4 – – 270.0 55.9 20.7
Mississippi 26.6 – – 1,065.1 14.7 1.4 153.0 13.0 8.5

December 2023
66
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 25. (continued)
State
1
Mental health facilities
2
Nursing facilities and ICF/IDs
3
Physicians and other practitioners
4
Total
Medicaid
payments
Supplemental
payments
Supplemental
payments as
% of total
Total
Medicaid
payments
Supplemental
payments
Supplemental
payments as
% of total
Total
Medicaid
payments
Supplemental
payments
Supplemental
payments as
% of total
Missouri $232.1 $207.2 89.3% $1,222.6 $5.4 0.4% $25.6 – –
Montana 22.3 – – 165.8 10.9 6.6 239.4 – –
Nebraska – – – 533.8 24.8 4.6 2.5 $1.3 52.6%
Nevada 40.1 – – 346.7 126.0 36.3 174.1 3.5 2.0
New Hampshire 49.1 48.4 98.6 384.2 80.5 21.0 4.6 – –
New Jersey 505.3 357.4 70.7 867.1 10.7 1.2 59.3 – –
New Mexico 5.0 – – 34.6 – – 73.1 3.8 5.2
New York 884.1 605.0 68.4 7,721.1 125.0 1.6 431.5 – –
North Carolina 28.3 27.5 97.2 2,082.9 – – 333.0 41.4 12.4
North Dakota 18.0 1.2 6.9 404.9 – – 54.9 –
–
Ohio 101.2 93.4 92.3 2,555.1 – – 169.9 51.9 30.5
Oklahoma 84.1 3.3 3.9 886.3 151.2 17.1 773.9 9.7 1.3
Oregon 24.1 21.1 87.6 560.7 – – 36.1 2.0 5.7
Pennsylvania 389.4 304.6 78.2 972.7 34.8 3.6 33.4 – –
Rhode Island
5, 7, 8
0.6 0.4 68.9 294.0 4.1 1.4 10.2 0.7 6.7
South Carolina 64.7 62.5 96.7 906.0 13.9 1.5 138.9 33.8 24.4
South Dakota 2.5 0.8 30.1 228.0 – – 74.8 – –
Tennessee 53.8 – – 214.1 – – 30.5 – –
Texas
5
291.4 289.2 99.2 1,401.3 7.0 0.5 2,415.2 2,229.1 92.3
Utah 18.9 0.9 5.0 458.9 143.5 31.3 132.6 44.7 33.7
Vermont 1.3 – – 147.7 – – 28.5 – –
Virginia 91.2 – – 291.9 15.5 5.3 246.9 195.1 79.0
Washington 130.6 100.1 76.6 966.6 5.3 0.5 101.4 5.4 5.3
West Virginia
30.3 21.2 69.8 899.0 – – 53.4 – –
Wisconsin 21.6 – – 755.6 58.8 7.8 64.5 – –
Wyoming 6.2 – – 133.0 44.1 33.1 70.6 23.2 32.9

MACStats: Medicaid and CHIP Data Book
67
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 25. (continued)
Notes: FY is scal year. ICF/ID is intermediate care facility for persons with intellectual disabilities. Includes federal and state funds. Excludes payments made
under managed care arrangements. All amounts in this table are as reported by states in CMS-64 data during the scal year to obtain federal matching funds;
amounts include expenditures for the current scal year and adjustments to expenditures for prior scal years that may be positive or negative. Amounts reported
by states for any given category (e.g., nursing facility) sometimes show substantial annual uctuations. Some uctuation in supplemental payments may reect the
fact that states may not consistently classify payments in the same way over time.
– Dash indicates zero; $0.0 indicates an amount between zero and $0.05 million that rounds to zero; 0.0% indicates an amount between zero and 0.05% that
rounds to zero.
1
All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
2
Includes inpatient psychiatric services for individuals under age 21 and inpatient hospital or nursing facility services for individuals age 65 and older in an
institution for mental diseases. Supplemental payments include disproportionate share hospital (DSH) payments made in accordance with Section 1923 of the
Social Security Act (the Act) as well as uncompensated care pool and other non-DSH supplemental payments made under waiver expenditure authority of Section
1115 of the Act. States are not instructed to break out non-DSH supplemental payments for mental health facilities.
3
Supplemental payments to nursing facilities and ICF/IDs include those made in addition to the standard fee schedule or other standard payments for a given
service, including payments made under institutional upper payment limit rules as well as other non-DSH supplemental payments made under waiver expenditure
authority of Section 1115 of the Act.
4
Includes the physician and other practitioner categories in CMS-64 data; excludes additional categories (e.g., dental, nurse-midwife, nurse practitioner) for which
states are not instructed to break out supplemental payments. Supplemental payments include those made in addition to the standard fee schedule payment as
well as uncompensated care pool, delivery system reform incentive payments (DSRIP), and other non-DSH supplemental payments made under Section 1115
waiver expenditure authority. There is no regulatory upper payment limit for physicians and other practitioners (as there is for institutional providers).
5
State made payments to physicians and other practitioners through an uncompensated care pool, DSRIP, or other non-DSH supplemental payments under
Section 1115 waiver expenditure authority.
6
State reports negative supplemental payments to mental health facilities due to prior period adjustments.
7
State made non-DSH payments to mental health facilities through an uncompensated care pool or other non-DSH supplemental payments under Section 1115
waiver expenditure authority.
8
State made non-DSH payments to nursing facilities through other non-DSH supplemental payments under Section 1115 waiver expenditure authority.
Source: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023, and CMS-64 Schedule C waiver report data as of September 29,
2023.

December 2023
68
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 26. Medicaid Gross Spending for Drugs by Delivery System and Brand or Generic Status, FY 2022 (millions)
State
Total Fee for service Managed care
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Total
4
$91,708.2 84.6% 15.2% 0.2% $32,918.3 86.4% 13.5% 0.1% $58,789.9 83.5% 16.2% 0.3%
Alabama 1,007.0 87.0 12.9 0.0 1,007.0 87.0 12.9 0.0 – – – –
Alaska 196.7 85.1 14.8 0.1 196.7 85.1 14.8 0.1 – – – –
Arizona 1,814.0 85.4 14.5 0.1 28.8 79.0 20.8 0.2 1,785.2 85.5 14.4 0.1
Arkansas 473.2 83.5 16.4 0.1 381.4 82.8 17.1 0.1 91.8 86.6 13.3 0.1
California 10,756.3 84.3 15.7 0.1 9,324.0 84.4 15.5 0.1 1,432.3 83.4 16.4 0.2
Colorado 1,378.2 89.9 9.9 0.1 1,327.4 90.2 9.7 0.1 50.7 84.2 15.8 0.0
Connecticut 1,650.2 90.1 9.8 0.1 1,650.2 90.1 9.8 0.1 – – – –
Delaware 296.2 88.9 10.9 0.2 1.6 94.6 5.4 – 294.7 88.9 11.0 0.2
District of Columbia 244.0 91.5 8.5 0.0 148.1 98.0 2.0 0.0 95.9 81.4 18.5 0.1
Florida 3,645.6 89.5 10.5 0.0 265.5 94.2 5.7 0.0 3,380.0 89.1 10.9 0.0
Georgia 1,380.3 84.6 15.3 0.1 868.5 89.5 10.5 0.0 511.8 76.4 23.5 0.1
Hawaii 222.8 83.4 16.5 0.0 0.1 – 100.0 – 222.8 83.5 16.5 0.0
Idaho 528.1 89.1 10.9 0.0 528.1 89.1 10.9 0.0 – – – –
Illinois 3,252.9 88.7 11.3 0.0 128.0 85.9 14.1 0.0 3,124.9 88.8 11.2 0.0
Indiana 2,485.5 86.2 13.8 0.0 479.2 91.2 8.7 0.1 2,006.3 85.0 15.0 0.0
Iowa 757.7 91.8 8.2 0.0 5.2 86.6 13.3 0.0 752.5 91.9 8.1 0.0
Kansas 287.5 83.4 16.6 0.0 0.4 78.5 21.5 – 287.1 83.4 16.6 0.0
Kentucky 1,960.8 89.7 10.0 0.3 76.5 80.1 19.7 0.3 1,884.3 90.1 9.6 0.3
Louisiana 2,358.4 85.9 14.0 0.1 49.3 81.4 18.4 0.2 2,309.1 86.0 13.9 0.1
Maine 439.5 90.2 9.8 0.0 439.5 90.2 9.8 0.0 – – – –
Maryland 1,598.9 88.4 11.5 0.0 544.3 86.5 13.5 0.0 1,054.6 89.5 10.5 0.0
Massachusetts 2,122.9 87.7 12.1 0.2 990.0 88.4 11.4 0.2 1,132.8 87.1 12.8 0.2
Michigan 3,289.6 88.7 11.2 0.1 1,418.9 88.3 11.6 0.0 1,870.7 89.0 10.9 0.1
Minnesota 1,318.6 84.9 14.9 0.3 168.2 72.5 26.7 0.8 1,150.4 86.7 13.2 0.2
Mississippi 509.9 82.5 17.5 0.0 150.0 80.3 19.7 0.0 359.8 83.5 16.5 0.0

MACStats: Medicaid and CHIP Data Book
69
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 26. (continued)
State
Total Fee for service Managed care
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Missouri $1,437.4 86.1% 13.9% 0.1% $1,437.4 86.1% 13.9% 0.1% – – – –
Montana 388.2 87.7 12.3 0.0 388.2 87.7 12.3 0.0 – – – –
Nebraska 411.9 86.2 13.7 0.1 0.0 – 100.0 – $411.9 86.2% 13.7% 0.1%
Nevada 549.5 83.1 16.2 0.7 295.0 82.1 16.9 1.0 254.5 84.2 15.4 0.4
New Hampshire 261.6 84.2 15.7 0.1 2.8 95.9 3.2 1.0 258.8 84.1 15.8 0.1
New Jersey 1,803.5 86.3 13.7 0.0 12.1 85.0 15.0 0.0 1,791.4 86.3 13.7 0.0
New Mexico 488.6 71.8 28.1 0.1 99.9 33.1 66.9 0.1 388.7 81.8 18.1 0.1
New York 7,109.8 86.2 13.7 0.2 721.4 79.6 20.3 0.1 6,388.4 86.9 12.9 0.2
North Carolina 2,319.6 89.1 10.9 0.0 846.8 89.0 11.0 0.0 1,472.8 89.2 10.8 0.0
North Dakota 97.6 85.9 14.1 0.0 93.2 86.0 14.0 0.0 4.4 84.2 15.7 0.1
Ohio 4,301.9 84.6 15.4 0.0 316.1 82.8 17.2 0.0 3,985.8 84.7 15.3 0.0
Oklahoma 811.9 84.5 15.5 0.0 811.9 84.5 15.5 0.0 – – – –
Oregon 817.9 82.1 17.9 0.0 139.3 77.8 22.2 0.0 678.6 83.0 17.0 0.1
Pennsylvania 4,253.0 85.0 15.0 0.0 27.6 78.1 21.9 0.0 4,225.4 85.1 14.9 0.0
Rhode Island 327.8 82.1 17.9 0.0 6.5 86.0 14.0 – 321.3 82.0 18.0 0.0
South Carolina 740.9 87.1 12.8 0.1 117.7 87.7 12.0 0.3 623.3 87.0 13.0 0.1
South Dakota 166.6 68.7 30.6 0.7 166.6 68.7 30.6 0.7 – – – –
Tennessee 1,467.3 87.7 12.1 0.2 1,331.9 86.8 13.0 0.2 135.4 95.8 4.0 0.2
Texas 3,882.2 85.6 14.4 0.0 43.9 82.4 17.5 0.0 3,838.4 85.6 14.4 0.0
Utah 491.9 89.4 10.5 0.0 209.7 88.7 11.2 0.0 282.2 90.0 10.0 0.0
Vermont 194.9 88.6 11.4 0.0 194.8 88.6 11.4 0.0 0.0 99.2 0.8 –
Virginia
5
5,312.1 52.0 45.6 2.4 12.5 81.9 17.8 0.3 5,299.6 51.9 45.7 2.4
Washington 1,533.9 90.0 9.9 0.1 99.5 92.5 7.5 0.0 1,434.5 89.8 10.0 0.1
West Virginia 845.8 87.0 13.0 0.0 822.0 86.7 13.3 0.0 23.8 97.2 2.7 0.0
Wisconsin 1,932.9 87.5 12.4 0.1 1,932.9 87.5 12.4 0.1 – – – –
Wyoming 43.6 86.5 13.5 0.0 43.6 86.5 13.5 0.0 – – – –

December 2023
70
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 26. (continued)
Notes: FY is scal year. Amounts include federal and state funds. Gross spending reects expenditures before the application of manufacturer rebates. Drug
expenditures in this exhibit use information from the state drug utilization data that states submit to CMS for rebate purposes and are dierent from the CMS-
64 Financial Management Report and Transformed Medicaid Statistical Information System (T-MSIS) data that serve as our usual sources of expenditure data.
Spending shown in the drug utilization data may dier from these other sources due to dierences in timing and run-out of data used. In addition, the drug
utilization data may include physician-administered drugs for which rebates are available; these drugs are typically reported under the physician services category
instead of the outpatient prescription drug category in other data. The state drug utilization data provide both fee-for-service (FFS) and managed care drug
utilization and spending information at the national drug code (NDC) level. To assign brand and generic status, we linked the quarterly state drug utilization data to
the quarterly Medicaid drug product data from CMS using the NDC code. Brand and generic status was assigned using the drug category indicator from the drug
product le.
The state drug utilization data are available at https://www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/index.html, and the drug product
data are available at https://www.medicaid.gov/medicaid/prescription-drugs/medicaid-drug-rebate-program/data/index.html.
Since October 2016, CMS has suppressed all records in the state drug utilization data that are less than 11 counts, as obligated by the Privacy Act of 1974 (5
U.S.C. § 552a) and the HIPAA Privacy Rule (45 C.F.R. Parts 160 and 164). The dierent brand and generic proportions under FFS and managed care may reect
dierences in the populations and specic drugs covered under each delivery system (e.g., behavioral health drugs carved out of managed care) as well as
dierences in how the state and participating health plans managed the drug benet.
– Dash indicates zero; 0.0 indicates an amount less than $0.05 million that rounds to zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
For this exhibit, brand drugs were dened as single source drugs and innovator, multiple source drugs as indicated in that quarter’s Medicaid drug product data.
2
For this exhibit, generic drugs were dened as non-innovator, multiple source drugs as indicated in that quarter’s Medicaid drug product le.
3
For this exhibit, unknown drugs were those drugs whose NDC did not have a match in that quarter’s Medicaid drug product le.
4
The national total does not equal the sum of the states due to the suppression of records. Records for drugs that were suppressed at the state level were not
necessarily suppressed once the individual state data were rolled up into the national le. Although the amount of suppressed spending in the FY 2022 national
le is not known, comparison of totals from previous years may be instructive. A comparison of the updated FY 2014 les with data suppression to prior versions
without suppression indicates that about $370 million, or 0.9 percent of gross spending, was suppressed in the FY 2014 data.
5
Virginia reports an atypical proportion of spending on generic drugs; this may indicate data anomalies in the payment amount for these drugs.
Source: MACPAC, 2023, analysis of Medicaid drug product data and state drug rebate utilization data as of September 2023.

MACStats: Medicaid and CHIP Data Book
71
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 27. Medicaid Drug Prescriptions by Delivery System and Brand or Generic Status, FY 2022 (thousands)
State
Total Fee for service Managed care
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Total
4
758,504 14.4% 85.2% 0.4% 237,498 15.4% 84.1% 0.4% 521,006 13.9% 85.7% 0.4%
Alabama 7,870 16.7 83.1 0.2 7,870 16.7 83.1 0.2 – – – –
Alaska 1,406 15.9 83.7 0.4 1,406 15.9 83.7 0.4 – – – –
Arizona 15,871 13.8 85.7 0.5 206 15.6 83.8 0.6 15,664 13.8 85.7 0.5
Arkansas 5,442 15.4 84.3 0.3 4,396 15.4 84.4 0.3 1,046 15.7 84.1 0.2
California 85,576 14.3 85.4 0.2 64,447 13.3 86.5 0.2 21,129 17.4 82.2 0.4
Colorado 8,436 17.5 82.3 0.3 7,971 17.7 82.0 0.3 464 14.1 85.8 0.1
Connecticut 9,299 21.4 78.3 0.3 9,299 21.4 78.3 0.3 – – – –
Delaware 2,686 14.9 84.8 0.3 7 49.4 50.6 – 2,679 14.8 84.9 0.3
District of Columbia 1,434 15.4 84.4 0.2 251 30.4 69.5 0.1 1,183 12.2 87.6 0.2
Florida 29,323 16.1 83.6 0.3 991 18.9 80.7 0.4 28,332 16.0 83.7 0.3
Georgia 16,995 12.3 87.4 0.3 7,213 16.2 83.6 0.1 9,782 9.3 90.2 0.5
Hawaii 2,013 11.9 87.7 0.5 5 – 100.0 – 2,008 11.9 87.6 0.5
Idaho 4,276 16.4 83.2 0.4 4,276 16.4 83.2 0.4 – – – –
Illinois 27,602 13.8 86.2 0.1 1,523 15.4 84.5 0.0 26,079 13.7 86.3 0.1
Indiana 20,171 14.2 85.5 0.3 2,796 14.8 84.8 0.4 17,375 14.2 85.6 0.2
Iowa 8,156 14.4 85.5 0.1 67 18.0 82.0 0.0 8,089 14.4 85.5 0.1
Kansas 3,542 14.7 85.1 0.1 8 10.9 89.1 – 3,534 14.8 85.1 0.1
Kentucky 23,851 12.3 87.1 0.6 1,089 9.0 89.4 1.6 22,763 12.4 87.0 0.6
Louisiana 21,158 12.7 86.9 0.4 599 12.6 86.9 0.5 20,559 12.7 86.9 0.4
Maine 2,845 25.7 74.2 0.2 2,845 25.7 74.2 0.2 – – – –
Maryland 14,893 15.5 84.4 0.1 5,008 18.7 81.2 0.0 9,885 13.9 86.0 0.1
Massachusetts 16,419 17.5 80.9 1.6 7,873 16.7 81.6 1.7 8,546 18.2 80.3 1.5
Michigan 30,775 13.8 85.7 0.5 9,598 14.5 85.3 0.2 21,176 13.5 85.9 0.6
Minnesota 12,135 14.7 81.6 3.7 1,638 12.9 78.8 8.3 10,497 15.0 82.0 3.0
Mississippi 5,256 12.4 87.4 0.2 1,715 11.2 88.7 0.1 3,541 13.0 86.8 0.2
Missouri 13,239 15.8 84.0 0.3 13,239 15.8 84.0 0.3 – – – –

December 2023
72
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 27. (continued)
State
Total Fee for service Managed care
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Total Brand
1
Generic
2
Unknown
3
Montana 3,115 15.6% 84.3% 0.2% 3,115 15.6% 84.3% 0.2% – – – –
Nebraska 4,151 15.5 84.2 0.3 0 – 100.0 – 4,151 15.5% 84.2% 0.3%
Nevada 5,293 11.8 87.2 0.9 2,025 14.8 84.4 0.7 3,267 10.0 89.0 1.1
New Hampshire 2,403 13.2 86.5 0.3 8 20.9 70.0 9.1 2,395 13.1 86.6 0.3
New Jersey 21,635 11.2 88.7 0.0 168 17.4 82.5 0.1 21,467 11.2 88.8 0.0
New Mexico 5,291 12.1 87.7 0.2 278 21.2 78.6 0.2 5,012 11.6 88.2 0.2
New York 78,804 12.3 86.8 0.9 9,933 12.3 86.7 1.0 68,871 12.3 86.8 0.9
North Carolina 15,638 19.7 80.0 0.2 5,275 22.0 77.7 0.3 10,364 18.6 81.2 0.2
North Dakota 998 16.6 83.0 0.3 920 15.8 84.0 0.2 78 26.4 71.2 2.3
Ohio 43,117 14.5 85.4 0.1 3,442 11.8 88.1 0.1 39,674 14.7 85.2 0.1
Oklahoma 7,612 11.7 88.2 0.1 7,612 11.7 88.2 0.1 – – – –
Oregon 10,340 12.1 87.7 0.2 2,376 5.9 94.0 0.0 7,964 14.0 85.8 0.2
Pennsylvania 36,233 13.5 86.5 0.0 490 10.7 89.2 0.0 35,743 13.5 86.4 0.0
Rhode Island 3,840 10.7 89.3 0.0 105 11.0 89.0 – 3,735 10.7 89.3 0.0
South Carolina 6,999 14.0 85.5 0.5 983 15.8 82.9 1.3 6,016 13.7 86.0 0.3
South Dakota 928 14.9 84.3 0.8 928 14.9 84.3 0.8 – – – –
Tennessee 14,511 17.2 81.9 0.9 12,855 14.3 84.8 0.9 1,656 40.0 58.7 1.3
Texas 34,239 14.1 85.9 0.0 502 20.2 79.7 0.1 33,737 14.0 86.0 0.0
Utah 3,508 16.6 83.3 0.1 1,512 17.9 82.0 0.1
1,996 15.5 84.3 0.1
Vermont 1,650 23.1 76.9 0.0 1,635 23.1 76.9 0.0 15 23.0 76.7 0.4
Virginia 22,581 14.0 85.2 0.8 216 15.5 82.0 2.4 22,365 14.0 85.2 0.7
Washington 14,682 12.6 87.1 0.2 996 13.4 86.4 0.2 13,686 12.6 87.2 0.2
West Virginia 8,928 16.9 82.9 0.2 8,639 16.6 83.2 0.2 288 25.5 74.3 0.2
Wisconsin 12,342 18.7 81.0 0.4 12,342 18.7 81.0 0.4 – – – –
Wyoming 419 15.1 84.8 0.1 419 15.1 84.8 0.1 – – – –

MACStats: Medicaid and CHIP Data Book
73
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 27. (continued)
Notes: FY is scal year. Drug utilization in this exhibit reects the number of prescriptions reported in the state drug utilization data that states submit to CMS
for rebate purposes and are dierent from Transformed Medicaid Statistical Information System (T-MSIS) data that serve as our usual source of utilization data.
Utilization shown in the drug utilization data may dier from these other sources due to dierences in timing and run-out of data used. In addition, the drug
utilization data may include physician-administered drugs for which rebates are available; these drugs are typically reported under the physician services category
instead of the outpatient prescription drug category in other data. The state drug utilization data provide both fee-for-service (FFS) and managed care drug
utilization and spending information at the national drug code (NDC) level. To assign brand and generic status, we linked the quarterly state drug utilization data to
the quarterly Medicaid drug product data from CMS using the NDC code. Brand and generic status was assigned using the drug category indicator from the drug
product le.
The state drug utilization data are available at https://www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/index.html, and the drug product
data are available at https://www.medicaid.gov/medicaid/prescription-drugs/medicaid-drug-rebate-program/data/index.html.
Since October 2016, CMS has suppressed all records in the state drug utilization data that are less than 11 counts, as obligated by the Privacy Act of 1974 (5
U.S.C. § 552a) and the HIPAA Privacy Rule (45 C.F.R. Parts 160 and 164). The dierent brand and generic proportions under FFS and managed care may reect
dierences in the populations and specic drugs covered under each delivery system (e.g., behavioral health drugs carved out of managed care) as well as
dierences in how the state and participating health plans managed the drug benet.
– Dash indicates zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
For this exhibit, brand drugs were dened as single source drugs and innovator, multiple source drugs as indicated in that quarter’s Medicaid drug product data.
² For this exhibit, generic drugs were dened as non-innovator, multiple source drugs as indicated in that quarter’s Medicaid drug product le.
³ For this exhibit, unknown drugs were those drugs whose NDC did not have a match in that quarter’s Medicaid drug product le.
⁴ The national total does not equal the sum of the states due to the suppression of records. Records for drugs that were suppressed at the state level were not
necessarily suppressed once the individual state data were rolled up into the national le. Although the number of suppressed prescriptions in the FY 2022 national
le is not known, a comparison of totals from previous years may be instructive. A comparison of the updated FY 2014 les with data suppression to prior versions
without suppression indicates that about 4 million prescriptions, or 0.7 percent of prescriptions, were suppressed in the FY 2014 data.
Source: MACPAC, 2023, analysis of Medicaid drug product data and state drug rebate utilization data as of September 2023.

December 2023
74
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 28. Medicaid Gross Spending and Rebates for Drugs by Delivery System, FY 2022 (millions)
State
Gross spending Rebates
Total Fee for service Managed care Total Fee for service Managed care
Total
1
$91,708.2 $32,918.3 $58,789.9 -$48,495.2 -$21,317.5 -$27,177.7
Alabama 1,007.0 1,007.0 – -547.7 -547.7 –
Alaska 196.7 196.7 – -120.1 -120.1 –
Arizona 1,814.0 28.8 1,785.2 -1,171.4 -65.6 -1,105.8
Arkansas
2
473.2 381.4 91.8 -320.4 -320.4 –
California
3
10,756.3 9,324.0 1,432.3 -4,223.7 -2,442.2 -1,781.5
Colorado 1,378.2 1,327.4 50.7 -932.5 -902.3 -30.2
Connecticut
4
1,650.2 1,650.2 – -1,142.1 -1,277.7 135.6
Delaware 296.2 1.6 294.7 -226.9 -11.1 -215.8
District of Columbia 244.0 148.1 95.9 -144.1 -74.7 -69.4
Florida 3,645.6 265.5 3,380.0 -2,369.3 -151.3 -2,218.0
Georgia 1,380.3 868.5 511.8 -749.3 -540.3 -209.0
Hawaii 222.8 0.1 222.8 -119.0 -0.8 -118.2
Idaho 528.1 528.1 – -339.5 -339.5 –
Illinois 3,252.9 128.0 3,124.9 -2,047.2 -114.7 -1,932.6
Indiana 2,485.5 479.2 2,006.3 -1,360.9 -315.6 -1,045.3
Iowa 757.7 5.2 752.5 -494.1 -15.7 -478.4
Kansas 287.5 0.4 287.1 -207.1 -2.7 -204.4
Kentucky 1,960.8 76.5 1,884.3 -1,302.0 -96.5 -1,205.5
Louisiana 2,358.4 49.3 2,309.1 -1,214.4 -46.3 -1,168.1
Maine 439.5 439.5 – -312.7 -312.7 –
Maryland 1,598.9 544.3 1,054.6 -810.7 -315.8 -494.9
Massachusetts 2,122.9 990.0 1,132.8 -1,457.5 -749.4 -708.1
Michigan 3,289.6 1,418.9 1,870.7 -2,263.4 -903.8 -1,359.6
Minnesota 1,318.6 168.2 1,150.4 -899.7 -513.1 -386.7
Mississippi 509.9 150.0 359.8 -363.2 -125.9 -237.3

MACStats: Medicaid and CHIP Data Book
75
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 28. (continued)
State
Gross spending Rebates
Total Fee for service Managed care Total Fee for service Managed care
Missouri $1,437.4 $1,437.4 – -$926.3 -$926.3 –
Montana 388.2 388.2 – -259.5 -259.5 –
Nebraska 411.9 0.0 $411.9 -207.7 -0.2 -$207.5
Nevada 549.5 295.0 254.5 -503.8 -243.3 -260.4
New Hampshire 261.6 2.8 258.8 -166.3 -91.3 -74.9
New Jersey 1,803.5 12.1 1,791.4 -787.2 -11.4 -775.8
New Mexico 488.6 99.9 388.7 -218.0 -30.1 -187.9
New York
4
7,109.8 721.4 6,388.4 -4,307.6 -4,307.6 0.0
North Carolina 2,319.6 846.8 1,472.8 -1,461.9 -673.3 -788.6
North Dakota 97.6 93.2 4.4 -79.5 -76.2 -3.4
Ohio 4,301.9 316.1 3,985.8 -2,535.0 -204.2 -2,330.8
Oklahoma 811.9 811.9 – -500.6 -500.6 –
Oregon 817.9 139.3 678.6 -448.3 -100.0 -348.2
Pennsylvania 4,253.0 27.6 4,225.4 -2,638.6 -41.3 -2,597.3
Rhode Island 327.8 6.5 321.3 -149.2 -6.7 -142.5
South Carolina 740.9 117.7 623.3 -372.1 -18.6 -353.5
South Dakota 166.6 166.6 – -54.9 -54.9 -0.0
Tennessee
2
1,467.3 1,331.9 135.4 -990.5 -990.5 –
Texas 3,882.2 43.9 3,838.4 -2,108.5 -51.0 -2,057.4
Utah 491.9 209.7 282.2 -269.9 -141.8 -128.1
Vermont 194.9 194.8 0.0 -155.6 -155.6 –
Virginia
5
5,312.1 12.5 5,299.6 -1,261.5 -33.9 -1,227.5
Washington 1,533.9 99.5 1,434.5 -1,046.0 -198.8 -847.3
West Virginia 845.8 822.0 23.8 -613.5 -600.1 -13.4
Wisconsin
4
1,932.9 1,932.9 – -1,254.3 -1,254.3 0.0
Wyoming 43.6 43.6 – -40.2 -40.2 –

December 2023
76
Section 3: Program Enrollment and Spending—Medicaid Benets
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 28. (continued)
Notes: FY is scal year. Amounts include federal and state funds. Gross spending reects expenditures before the application of manufacturer rebates. The gross
drug expenditures in this exhibit use information from the state drug utilization data that states submit to CMS for rebate purposes and are dierent from the CMS-
64 Financial Management Report (FMR) and Transformed Medicaid Statistical Information System (T-MSIS) data that serve as our usual sources of expenditure
data. Spending shown in the drug utilization data may dier from these other sources due to dierences in timing and run-out of data used. In addition, the drug
rebate data may include physician-administered drugs for which rebates are available; the spending for these drugs are typically reported under the physician
services category instead of the outpatient prescription drug category in other data. The state drug utilization data provide both fee-for-service (FFS) and managed
care drug utilization and spending information at the national drug code (NDC) level, which is not available in CMS-64 data. The state drug utilization data are
available at https://www.medicaid.gov/medicaid/prescription-drugs/state-drug-utilization-data/index.html.
Since October 2016, CMS has suppressed all records in the state drug utilization data that are less than 11 counts, as obligated by the Privacy Act of 1974
(5 U.S.C. § 552a) and the HIPAA Privacy Rule (45 C.F.R. Parts 160 and 164). The drug rebate information comes from the CMS-64 and does allow states to
separately identify FFS and managed care drug rebates. The rebate totals shown here include federal rebates, state supplemental rebates, and the rebate
increases attributable to the Patient Protection and Aordable Care Act (P.L. 111-148, as amended), including rebates for opioid use disorder medication assisted
treatment.
Due to the time it takes to collect the drug utilization information and invoice drug manufacturers for the rebate, the rebates collected in any particular quarter
are generally attributable to drugs purchased in prior quarters; thus, the gross spending and rebate dollars for a given time period are not necessarily aligned.
Changes in covered populations or benet design (e.g., managed care expansion or pharmacy carve-in) can create distortions in the data, because changes will
be reected in gross spending before they are reected in rebates collected.
– Dash indicates zero; $0.0 or -$0.0 indicates an amount between -$0.05 and $0.05 million that rounds to zero.
1
The national total does not equal the sum of the states due to the suppression of records. Records for drugs that were suppressed at the state level were not
necessarily suppressed once the individual state data were rolled up into the national le. Although the amount of suppressed spending in the FY 2022 national
le is not known, comparison of totals from previous years may be instructive. A comparison of the updated FY 2014 les with data suppression to prior versions
without suppression indicates that about $370 million, or 0.9 percent of gross spending, was suppressed in the FY 2014 data.
2
State generally carves out prescription drugs from the managed care program. State managed care spending may reect physician-administered drugs; however,
minimal or no rebates for these managed care expenditures have been reported in the CMS-64 data and are likely to have been reported with the FFS rebates.
3
California carved prescription drugs out of managed care beginning January 1, 2022, resulting in anomalous distributions in spending and rebates between FFS
and managed care.
4
Connecticut, New York, and Wisconsin reported prior period adjustments for managed care that ultimately resulted in a positive managed care rebate amount.
5
Virginia reports an atypical proportion of spending on generic drugs; this may indicate data anomalies in the payment amount for these drugs.
Source: MACPAC, 2023, analysis of Medicaid state drug rebate utilization data as of September 2023 and CMS-64 FMR net expenditure data as of May 30, 2023.

MACStats: Medicaid and CHIP Data Book
77
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 29. Percentage of Medicaid Enrollees in Managed Care by State, July 1, 2021
State
Total Medicaid
enrollees
Percentage in managed care
Comprehensive
managed care
1
Limited-benet plans
PCCMMLTSS
BHO (PIHP
and/or PAHP) Dental Transportation Other
Total 89,018,035 74.3% 0.6% 9.0% 16.9% 16.0% 2.0% 6.0%
Alabama 1,198,510 0.0 – – – – – 79.3
Alaska
2
242,176 – – – – – – –
Arizona 2,244,273 80.0 2.8 2.8 – – – –
Arkansas 1,069,577 4.7 – – 67.6 85.1 26.9 42.4
California 14,150,266 82.4 – – 6.3 – – –
Colorado
3
1,499,303 10.6 – – – – – 84.3
Connecticut
4
1,106,169 – – – – – – –
Delaware 276,475 87.1 – – – 88.6 – –
District of Columbia 285,297 81.1 – – – 12.9 – –
Florida 4,871,362 78.3 2.5 – 83.1 – – –
Georgia 2,539,039 72.1 – – – 78.4 2.5 –
Hawaii 420,033 100.0 – – – – – –
Idaho 421,589 5.6 – 87.2 92.8 92.8 – 80.8
Illinois 3,467,588 75.4 1.9 – – – – –
Indiana 1,870,171 78.8 – – – – – –
Iowa 749,862 93.9 – – 94.8 – – –
Kansas 461,405 88.1 – – – – – –
Kentucky 1,584,976 89.4 – – – 99.8 – –
Louisiana 1,894,676 85.3 – 7.3 92.8 – – –
Maine 331,396 – – – – 98.6 – 68.9
Maryland 1,780,886 85.4 – – – – – –
Massachusetts 2,091,955 40.5 – 29.9 – – – 26.9
Michigan
5
2,900,801 100.5 0.4 93.1 28.1 – – –
Minnesota 1,253,815 86.7 – – – – – –
Mississippi 776,482 61.2 – – – – – –
Missouri 1,048,083 74.2 – – – 25.5 – –

December 2023
78
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 29. (continued)
State
Total Medicaid
enrollees
Percentage in managed care
Comprehensive
managed care
1
Limited-benet plans
PCCMMLTSS
BHO (PIHP
and/or PAHP) Dental Transportation Other
Montana 309,776 – – – – – – 79.2%
Nebraska 336,290 99.6% – – 88.1% – – –
Nevada 847,650 75.6 – – 77.1 90.9% – –
New Hampshire 239,439 91.3 – – – – – –
New Jersey 1,892,091 96.2 – – – 96.2 – –
New Mexico 941,830 83.0 – – – – – –
New York 7,145,884 75.2 3.4% – – – – –
North Carolina 2,557,593 60.6 – 19.6% – – – 20.3
North Dakota 125,354 27.0 – – – – – 41.8
Ohio 3,238,849 85.9 – – – – – –
Oklahoma 1,065,121 0.1 – – – 97.6 – 58.4
Oregon
6
1,286,095 85.8 – – 4.7 – – –
Pennsylvania
7
3,292,313 93.9 – 94.5 – 21.4 0.0% –
Rhode Island 339,276 84.6 – – 37.7 98.8 – –
South Carolina 1,446,070 66.6 – – – 100.0 – 0.1
South Dakota 137,268 – – – – – – 61.1
Tennessee
8
1,717,984 92.9 – – 54.1 – 83.7 –
Texas 4,928,655 81.7 – – 69.6 – – –
Utah 424,565 82.9 – 79.0 51.1 80.6 – –
Vermont
9
191,240 68.5 – – – – – –
Virginia 1,852,563 91.3 – – – – – –
Washington 2,008,655 88.3 – 8.3 – 100.0 0.6 0.2
West Virginia 599,336 81.4 – – – – – –
Wisconsin 1,484,746 69.1 3.5 0.1 – – 0.2 –
Wyoming
10
73,227 – – – – – – –

MACStats: Medicaid and CHIP Data Book
79
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 29. (continued)
Notes: MLTSS is managed long-term services and supports. BHO is behavioral health organization. PIHP is prepaid inpatient health plan. PAHP is prepaid
ambulatory health plan. PCCM is primary care case management. Excludes the territories. This exhibit includes Medicaid-expansion CHIP enrollees. Medicaid
beneciaries may be enrolled concurrently in more than one type of managed care program (e.g., a comprehensive plan and a BHO), so the sum of enrollment in
each program type as a percentage of total Medicaid enrollment may be greater than 100 percent.
– Dash indicates zero. 0.0% indicates an amount less than 0.05% that rounds to zero.
1
Includes comprehensive managed care and Programs of All-Inclusive Care for the Elderly (PACE). Comprehensive managed care organizations (MCOs) cover
acute, primary, and specialty medical care services; they may also cover behavioral health, long-term services and supports, and other benets in some states.
2
Alaska's total Medicaid enrollment as of July 1, 2021, was taken from the July–September 2021 enrollment data collected through the Medicaid Budget and
Expenditure System, updated January 2023 and accessed April 2, 2023.
3
Colorado did not provide plan level enrollment for plans that had fewer than 30 beneciaries. As a result, reported Medicaid enrollment in comprehensive
managed care may be lower than actual enrollment.
4
Connecticut's total Medicaid enrollment as of July 1, 2021, was taken from the July–September 2021 enrollment data collected through the Medicaid Budget and
Expenditure System, updated January 2023 and accessed April 2, 2023.
5
Michigan has two programs that provide home- and community-based service waiver services under capitation: MI Choice and the Specialty Prepaid Inpatient
Health Plan (SPIHP). MI Choice is reported as an MLTSS program and SPIHP is reported as a BHO.
6
Some plans that appear to be limited-benet plans (dental, BHO, or other managed care) were classied as comprehensive managed care in the CMS report.
The values shown here use plan-level information in the CMS report to recategorize enrollment in Advantage Dental Services, Capitol Dental Care, Family Dental
Care, Managed Dental Care of Oregon, and ODS Community Health as dental.
7
Pennsylvania did not provide enrollment counts for plans with fewer than 11 beneciaries. As a result, reported Medicaid enrollment in comprehensive managed
care may be lower than actual enrollment.
8
Some plans that appear to be limited-benet plans (dental, BHO, or other managed care) were classied as comprehensive managed care in the CMS report.
The values shown here use plan-level information in the CMS report to recategorize enrollment in DentaQuest as dental and enrollment in OptumRx as other.
9
The Department of Vermont Health Access, a state agency, acts as Vermont's single MCO entity.
10
Wyoming's total Medicaid enrollment as of July 1, 2021, was taken from the July–September 2021 enrollment data collected through the Medicaid Budget and
Expenditure System, updated January 2023 and accessed April 2, 2023.
Source: MACPAC, 2023, analysis of data from CMS, Medicaid managed care enrollment and program characteristics, 2021, Baltimore, MD: CMS, https://www.
medicaid.gov/medicaid/managed-care/enrollment-report/index.html.

December 2023
80
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 30. Percentage of Medicaid Enrollees in Managed Care by State and Eligibility Group, FY 2021
State
Total
Medicaid
enrollees
(thousands)
Percentage of enrollees in managed care
Comprehensive managed care
1
Limited-benet plans
2
Total Child
New adult
group
4
Other
adult
5
Disabled Aged Total Child
New adult
group
4
Other
adult
5
Disabled Aged
Total 87,979 72.4% 85.0% 81.5% 64.9% 52.9% 36.8% 42.1% 51.3% 32.4% 36.0% 49.7% 35.6%
Alabama 1,162 0.0 – – – 0.0 0.1 7.5 0.0 – 0.1 18.8 33.4
Alaska 255 – – – – – – – – – – – –
Arizona 2,266 91.1 98.6 93.6 83.2 91.1 71.1 0.0 – 0.0 0.0 – –
Arkansas 1,045 0.1 – 0.0 – 0.0 0.6 88.9 96.9 96.2 77.3 73.4 41.4
California
6
13,918 78.6 90.2 84.5 56.9 85.1 73.0 6.1 6.2 7.6 4.7 6.5 3.6
Colorado
7
1,551 12.1 8.7 14.6 12.4 10.7 13.7 95.2 99.3 98.7 92.8 87.5 57.9
Connecticut 1,177 0.0 – 0.0 – – – 86.1 99.3 100.0 85.6 59.1 35.8
Delaware 292 86.8 96.1 94.7 78.7 72.8 44.8 88.6 96.9 98.5 80.3 74.1 44.1
District of Columbia
8
278 81.5 94.6 94.8 96.9 54.9 7.6 22.2 11.4 17.7 11.3 43.4 62.0
Florida 5,054 78.9 97.5 – 76.6 62.8 34.3 92.2 99.5 – 92.8 85.8 72.6
Georgia 2,448 72.3 98.3 – 93.6 3.4 0.0 83.3 97.8 – 79.5 67.8 40.0
Hawaii 429 98.3 99.9 99.8 99.8 93.4 87.7 1.3 0.0 0.9 0.4 13.1 2.2
Idaho 436 – – – – – – 94.5 99.9 99.7 98.3 83.6 58.8
Illinois
8
3,371 81.1 92.1 87.4 59.7 49.8 45.9 – – – – – –
Indiana
7
1,932 78.4 91.5 100.0 76.4 29.4 6.5 19.9 17.2 0.2 13.5 61.6 65.1
Iowa 791 94.0 98.2 96.4 92.2 89.5 70.3 94.1 95.3 98.1 94.9 91.2 70.5
Kansas 452 93.5 100.0 – 96.7 85.4 67.7 – – – – – –
Kentucky 1,734 87.8 97.8 93.0 95.2 69.2 36.2 92.5 98.3 96.5 96.8 80.2 58.5
Louisiana
7
1,823 93.0 99.9 98.9 93.8 81.9 56.7 93.3 99.9 98.9 94.1 83.6 57.2
Maine 422 – – – – – – – – – – – –
Maryland 1,548 84.9 98.6 95.4 86.8 57.0 2.0 – – – – – –
Massachusetts 1,980 41.8 49.7 52.0 36.5 31.8 34.2 33.3 44.7 42.3 28.8 35.8 2.0
Michigan 3,001 78.1 86.1 84.4 81.0 62.1 28.7 96.1 99.0 96.9 95.0 93.9 84.2
Minnesota 1,338 85.6 89.7 94.3 85.2 53.6 75.1 – – – – – –
Mississippi 827 66.3 92.7 – 62.1 42.6 1.4 – – – – – –

MACStats: Medicaid and CHIP Data Book
81
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 30. (continued)
State
Total
Medicaid
enrollees
(thousands)
Percentage of enrollees in managed care
Comprehensive managed care
1
Limited-benet plans
2
Total Child
New adult
group
4
Other
adult
5
Disabled Aged Total Child
New adult
group
4
Other
adult
5
Disabled Aged
Missouri 1,240 65.6% 97.0% 0.5% 84.2% 0.4% 0.0% 95.2% 100.0% 98.9% 91.6% 89.8% 80.7%
Montana 289 – – – – – – – – – – – –
Nebraska 331 97.9 99.8 99.1 99.3 94.8 86.5 87.1 99.6 39.1 98.9 94.6 85.6
Nevada 880 74.8 86.1 88.0 83.9 4.1 2.0 92.3 99.5 98.2 94.3 72.5 37.4
New Hampshire 249 87.6 98.4 97.2 63.6 66.9 59.6 0.7 0.1 0.8 0.7 1.7 1.9
New Jersey 1,923 94.5 95.8 94.8 85.9 97.0 94.1 100.0 100.0 100.0 100.0 100.0 100.0
New Mexico 962 83.3 92.3 91.2 70.5 71.4 43.3 – – – – – –
New York 7,253 75.2 94.6 92.1 61.5 50.2 13.8 3.9 0.0 0.5 0.5 7.0 26.2
North Carolina 2,535 55.2 86.0 – 41.8 28.3 2.7 78.0 95.8 – 52.6 90.7 71.6
North Dakota
6
125 29.5 0.1 99.5 14.8 5.0 4.4 – – – – – –
Ohio 3,146 83.5 98.3 94.9 94.7 49.6 10.1 5.1 0.0 0.0 2.0 15.8 34.6
Oklahoma 1,109 0.1 – – – 0.2 0.8 – – – – – –
Oregon
7
1,275 84.0 92.7 88.7 32.5 75.0 56.6 7.2 7.2 7.7 6.4 6.9 4.0
Pennsylvania 3,390 88.2 94.4 87.3 89.7 83.7 78.4 93.7 97.6 96.5 93.3 91.0 77.6
Rhode Island 335 82.4 83.8 97.1 88.9 69.2 28.8 92.1 91.4 99.0 91.6 92.9 69.7
South Carolina 1,377 67.0 94.6 – 49.8 41.3 20.6 81.6 99.2 – 52.9 93.9 80.9
South Dakota 132 – – – – – – – – – – – –
Tennessee 1,787 92.2 99.3 – 99.4 81.4 50.3 – – – – – –
Texas
9
5,628 81.2 97.1 – 56.1 72.1 42.5 80.2 96.2 – 50.6 74.2 45.1
Utah
6
446 80.4 87.2 75.9 71.4 81.4 67.1 90.5 98.0 80.0 81.6 96.3 89.2
Vermont 198 – – – – – – – – – – – –
Virginia 1,845 73.8 97.4 86.7 75.7 1.9 5.1 16.4 0.2 9.1 1.6 80.7 62.9
Washington 2,153 86.2 96.7 96.6 90.0 52.4 6.5 8.8 1.0 2.4 2.3 32.5 67.3
West Virginia 632 82.6 98.9 97.4 94.7 49.2 3.4 44.3 46.2 60.0 57.8 8.9 17.8
Wisconsin 1,414 72.3 91.9 – 86.0 31.5 9.7 94.4 99.5 – 99.1 96.9 57.1
Wyoming 81 0.2 – – – 0.1 1.4 0.5 0.6 – 0.0 1.0 –

December 2023
82
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 30. (continued)
State
Total Medicaid
enrollees
(thousands)
Percentage of enrollees in managed care
Primary care case management
3
Total Child
New adult
group
4
Other adult
5
Disabled Aged
Total 87,979 8.3% 11.2% 6.6% 7.1% 8.7% 3.1%
Alabama 1,162 78.4 97.4 – 92.9 53.1 16.0
Alaska 255 – – – – – –
Arizona 2,266 – – – – – –
Arkansas 1,045 47.2 82.5 8.5 38.6 54.4 2.8
California
6
13,918 – – – – – –
Colorado
7
1,551 94.3 98.4 97.5 91.9 86.8 57.5
Connecticut 1,177 – – – – – –
Delaware 292 – – – – – –
District of Columbia
8
278 – – – – – –
Florida 5,054 – – – – – –
Georgia 2,448 – – – – – –
Hawaii 429 – – – – – –
Idaho 436 85.6 96.1 92.4 91.7 66.6 26.3
Illinois
8
3,371 – – – – – –
Indiana
7
1,932 – – – – – –
Iowa 791 0.1 0.0 0.0 0.1 0.2 0.0
Kansas 452 – – – – – –
Kentucky 1,734 – – – – – –
Louisiana
7
1,823 – – – – – –
Maine 422 56.0 82.2 83.6 48.9 31.6 1.7
Maryland 1,548 – – – – – –
Massachusetts 1,980 28.0 34.1 41.4 27.3 23.6 1.0
Michigan 3,001 – – – – – –
Minnesota 1,338 – – – – – –
Mississippi 827 – – – – – –

MACStats: Medicaid and CHIP Data Book
83
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 30. (continued)
State
Total Medicaid
enrollees
(thousands)
Percentage of enrollees in managed care
Primary care case management
3
Total Child
New adult
group
4
Other adult
5
Disabled Aged
Missouri 1,240 – – – – – –
Montana 289 83.7% 95.4% 94.7% 83.0% 41.7% 3.1%
Nebraska 331 – – – – – –
Nevada 880 – – – – – –
New Hampshire 249 – – – – – –
New Jersey 1,923 – – – – – –
New Mexico 962 – – – – – –
New York 7,253 – – – – – –
North Carolina 2,535 67.6 91.6 – 40.1 75.9 45.9
North Dakota
6
125 52.3 89.3 10.4 96.1 2.4 0.1
Ohio 3,146 – – – – – –
Oklahoma 1,109 92.6 98.9 88.0 89.7 84.0 76.9
Oregon
7
1,275 23.3 22.0 24.7 18.1 26.2 17.9
Pennsylvania 3,390 – – – – – –
Rhode Island 335 – –
– – – –
South Carolina 1,377 0.1 0.0 – – 0.5 –
South Dakota 132 73.7 89.7 – 91.8 37.2 10.8
Tennessee 1,787 – – – – – –
Texas
9
5,628 – – – – – –
Utah
6
446 – – – – – –
Vermont 198 – – – – – –
Virginia 1,845 – – – – – –
Washington 2,153 0.2 0.2 0.1 0.2 0.3 0.0
West Virginia 632 – – – – – –
Wisconsin 1,414 – – – – – –
Wyoming 81 – – – – – –

December 2023
84
Section 3: Program Enrollment and Spending—Medicaid Managed Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 30. (continued)
Notes: FY is scal year. Enrollment numbers generally include individuals ever enrolled in Medicaid-nanced coverage during the year, even if for a single month. However, in the
event individuals were also enrolled in CHIP-nanced Medicaid coverage (i.e., Medicaid-expansion CHIP) during the year, they are excluded if their most recent enrollment month was
in Medicaid-expansion CHIP. Numbers exclude individuals enrolled only in Medicaid-expansion CHIP during the year and enrollees in the territories. Children and adults under age 65
who qualify for Medicaid on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through an aged, blind, or disabled pathway are included
in the aged category. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between the Transformed Medicaid Statistical
Information System (T-MSIS) and the Medicaid Statistical Information System (MSIS).
Individuals are counted as participating in managed care if they had at least one month indicating plan enrollment. For MACPAC's analysis, Medicaid enrollees were assigned a unique
national identication (ID) number using an algorithm that incorporates state-specic ID numbers and beneciary characteristics such as date of birth and gender. The state and national
enrollment counts shown here are unduplicated using this national ID. The sum of the state totals exceeds the national total because individuals may be enrolled in more than one state
during the year. Medicaid enrollees may be enrolled concurrently in more than one type of managed care program (e.g., a comprehensive plan and a limited-benet plan), so the sum of
enrollment across program types as a percentage of total Medicaid enrollment may be greater than 100 percent.
Figures shown here, which are based on T-MSIS data, may dier from those that use Medicaid managed care enrollment report data. Reasons for dierences include diering time
periods, state reporting anomalies, and the treatment of Medicaid-expansion CHIP enrollees (excluded here but included in enrollment report data). Although the enrollment report is a
commonly cited source, it does not provide information on the characteristics of enrollees in managed care (e.g., eligibility group).
– Dash indicates zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
Includes comprehensive managed care, health insuring organization, and Programs of All-Inclusive Care for the Elderly (PACE).
2
Includes prepaid inpatient health plan (PIHP), prepaid ambulatory health plan (PAHP), accountable care organization, and other plan types. PIHPs and PAHPs include plans covering
services for long-term services and supports, behavioral health, substance use disorder, dental, transportation, and pharmacy.
3
Primary care case management (PCCM) includes traditional PCCM, enhanced PCCM, and medical and health homes.
4
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Social Security Act (the Act). Newly eligible adults include those
who are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who would have previously been eligible for
Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to adults with incomes greater than 100 percent of the federal
poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
5
Includes adults age 19 to 64 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers, pregnancy).
6
State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children who would have,
before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in the T-MSIS data. Because
the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states based on the proportion reported in their
SPA. Correspondingly, we reduced California's child enrollment by approximately 250,000, North Dakota's child enrollment by approximately 3,000, and Utah's child enrollment by
approximately 12,000.
7
State reported a large shift of enrollees between eligibility groups. Colorado reported a 35 percent increase in the new adult group and a 46 percent decrease for the other adult
group. Indiana reported a 16 percent decrease for the new adult group and a 60 percent increase for the other adult group. Louisiana reported a 15 percent increase in the new adult
group and a 10 percent decrease in the other adult group. Oregon reported a 33 percent increase in the new adult group, a 69 percent decrease in the other adult group, a 102 percent
increase in the disabled group, and a 53 percent increase in the aged group.
8
State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The District of Columbia's
average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than the benchmark.
9
State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
Source: MACPAC, 2023, analysis of T-MSIS data as of February 2023.

MACStats: Medicaid and CHIP Data Book
85
Section 3: Program Enrollment and Spending—Medicaid Program Administration
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 31. Total Medicaid Administrative Spending by State and Category, FY 2022 (millions)
State
1
Total
spending on
administration
Spending by category
CollectionsMMIS
2
Eligibility
systems
2
EHR
incentive
program
3
Other
functions,
federal match
above 50%
4
Other
functions,
federal match
of 50%
5
Alabama $241 $43 $27 $2 $11 $157 –
Alaska 157 46 5 1 6 99 –
Arizona 331 45 130 7 11 137 –
Arkansas 442 129 93 0 24 196 -$0
California 7,190 488 2,489 23 295 3,896 -1
Colorado 551 77 140 9 19 306 -1
Connecticut 353 47 101 3 31 171 –
Delaware 103 35 9 1 2 56 –
District of Columbia 281 42 81 4 9 145 –
Florida 606 113 73 2 34 384 –
Georgia 536 132 105 2 14 284 –
Hawaii 113 22 41 1 2 47 –
Idaho 135 37 22 -2 20 58 –
Illinois 1,017
73 292
5 73 574 –
Indiana 471 66 87 3 22 293 –
Iowa 163 34 80 1 13 35 –
Kansas 250 75 67 1 4 103 –
Kentucky 286 84 80 1 18 104 –
Louisiana 365 68 130 2 6 159 -0
Maine 167 52 38 3 11 63 -0
Maryland 501 106 136 6 22 230 –
Massachusetts 1,159 141 150 5 51 812 -0
Michigan 673 165 135 4 21 348 -0
Minnesota 738 72 157 5 15 489 –
Mississippi 198 72 37 1 7 81 –
Missouri 427 70 94 3 12 248 –
Montana 105 43 17 6 7 33 -1
Nebraska 185 33 39 26 7 80 –
Nevada 218 49 71 1 11 86 –
New Hampshire 151 59 44 0 5 42 –
Notes: FY is scal year. Enrollment numbers generally include individuals ever enrolled in Medicaid-nanced coverage during the year, even if for a single month. However, in the
event individuals were also enrolled in CHIP-nanced Medicaid coverage (i.e., Medicaid-expansion CHIP) during the year, they are excluded if their most recent enrollment month was
in Medicaid-expansion CHIP. Numbers exclude individuals enrolled only in Medicaid-expansion CHIP during the year and enrollees in the territories. Children and adults under age 65
who qualify for Medicaid on the basis of disability are included in the disabled category. Individuals age 65 and older eligible through an aged, blind, or disabled pathway are included
in the aged category. Additionally, gures shown here may not be directly comparable to prior years due to dierences in reporting between the Transformed Medicaid Statistical
Information System (T-MSIS) and the Medicaid Statistical Information System (MSIS).
Individuals are counted as participating in managed care if they had at least one month indicating plan enrollment. For MACPAC's analysis, Medicaid enrollees were assigned a unique
national identication (ID) number using an algorithm that incorporates state-specic ID numbers and beneciary characteristics such as date of birth and gender. The state and national
enrollment counts shown here are unduplicated using this national ID. The sum of the state totals exceeds the national total because individuals may be enrolled in more than one state
during the year. Medicaid enrollees may be enrolled concurrently in more than one type of managed care program (e.g., a comprehensive plan and a limited-benet plan), so the sum of
enrollment across program types as a percentage of total Medicaid enrollment may be greater than 100 percent.
Figures shown here, which are based on T-MSIS data, may dier from those that use Medicaid managed care enrollment report data. Reasons for dierences include diering time
periods, state reporting anomalies, and the treatment of Medicaid-expansion CHIP enrollees (excluded here but included in enrollment report data). Although the enrollment report is a
commonly cited source, it does not provide information on the characteristics of enrollees in managed care (e.g., eligibility group).
– Dash indicates zero; 0.0% indicates an amount less than 0.05% that rounds to zero.
1
Includes comprehensive managed care, health insuring organization, and Programs of All-Inclusive Care for the Elderly (PACE).
2
Includes prepaid inpatient health plan (PIHP), prepaid ambulatory health plan (PAHP), accountable care organization, and other plan types. PIHPs and PAHPs include plans covering
services for long-term services and supports, behavioral health, substance use disorder, dental, transportation, and pharmacy.
3
Primary care case management (PCCM) includes traditional PCCM, enhanced PCCM, and medical and health homes.
4
Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Social Security Act (the Act). Newly eligible adults include those
who are not eligible for Medicaid under the rules that a state had in place on December 1, 2009. Not newly eligible adults include those who would have previously been eligible for
Medicaid under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to adults with incomes greater than 100 percent of the federal
poverty level as of March 23, 2010, and receive the expansion state transitional matching rate.
5
Includes adults age 19 to 64 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers, pregnancy).
6
State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance percentage (FMAP) for Medicaid children who would have,
before January 1, 2014, been enrolled in CHIP if not for the elimination of the Medicaid asset test. These children cannot be separately identied in the T-MSIS data. Because
the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in these states based on the proportion reported in their
SPA. Correspondingly, we reduced California's child enrollment by approximately 250,000, North Dakota's child enrollment by approximately 3,000, and Utah's child enrollment by
approximately 12,000.
7
State reported a large shift of enrollees between eligibility groups. Colorado reported a 35 percent increase in the new adult group and a 46 percent decrease for the other adult
group. Indiana reported a 16 percent decrease for the new adult group and a 60 percent increase for the other adult group. Louisiana reported a 15 percent increase in the new adult
group and a 10 percent decrease in the other adult group. Oregon reported a 33 percent increase in the new adult group, a 69 percent decrease in the other adult group, a 102 percent
increase in the disabled group, and a 53 percent increase in the aged group.
8
State reported enrollment for the new adult group that shows a dierence of greater than 20 percent when compared to the CMS-64 enrollment report. The District of Columbia's
average monthly enrollment was 36 percent less than the benchmark, and Illinois's average monthly enrollment was 113 percent more than the benchmark.
9
State reported enrollment for the new adult group even though it had not expanded coverage in FY 2021.
Source: MACPAC, 2023, analysis of T-MSIS data as of February 2023.

December 2023
86
Section 3: Program Enrollment and Spending—Medicaid Program Administration
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 31. (continued)
State
1
Total
spending on
administration
Spending by category
CollectionsMMIS
2
Eligibility
systems
2
EHR
incentive
program
3
Other
functions,
federal match
above 50%
4
Other
functions,
federal match
of 50%
5
New Jersey $1,013 $104 $281 $7 $32 $589 -$0
New Mexico 287 79 88 1 8 111 –
New York 2,046 244 193 52 55 1,502 –
North Carolina 1,063 103 405 1 69 485 –
North Dakota 97 34 31 1 2 29 -0
Ohio 1,035 165 188 2 22 659 -0
Oklahoma 218 47 11 1 21 138 –
Oregon 613 47 102 2 23 439 -0
Pennsylvania 1,117 103 413 2 25 573 –
Rhode Island 191 43 47 1 1 99 -0
South Carolina 382 75 73 2 30 202 –
South Dakota 74 13 14 1 3 44 –
Tennessee 819 280 244 1 16 279 -2
Texas 1,627
302 435 4 20 870 -5
Utah 186 49 42 2 14 79 –
Vermont 165 40 35 6 9 74 –
Virginia 439 83 111 1 25 219 –
Washington 1,073 107 99 -3 17 853 -0
West Virginia 209 69 41 0 38 60 –
Wisconsin 524 148 125 3 7 242 -1
Wyoming 75 36 17 – 4 19 -0
Subtotal (states) $31,365 $4,687 $7,964 $214 $1,229 $17,282 -$12
American Samoa 2 – – 0 – 2 –
Guam 4 0 – – 0 4 –
Northern Mariana Islands 5 4 – 0 – 1 –
Puerto Rico 102 27 34 8 – 33 –
Virgin Islands 24 7 9 0 – 8 –
Subtotal (states and territories) $31,502 $4,724 $8,007 $224 $1,229 $17,330 -$12

MACStats: Medicaid and CHIP Data Book
87
Section 3: Program Enrollment and Spending—Medicaid Program Administration
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 31. (continued)
State
1
Total
spending on
administration
Spending by category
CollectionsMMIS
2
Eligibility
systems
2
EHR
incentive
program
3
Other
functions,
federal match
above 50%
4
Other
functions,
federal match
of 50%
5
Medicaid Fraud Control Units
6
$409 – – – $409 – –
Medicaid survey and certication
of nursing and intermediate care
facilities
6
400 – – – 400 – –
Total $32,311 $4,724 $8,007 $224 $2,038 $17,330 -$12
Percent of total, exclusive of
collections
– 14.6% 24.8% 0.7% 6.3% 53.6% –
Notes: FY is scal year. MMIS is Medicaid Management Information Systems. EHR is electronic health record. Includes federal and state funds. Excludes
administrative activities performed by Medicaid managed care plans (which are included in the capitation payments that states make to these plans) and activities
that are exclusively federal, such as program oversight by CMS sta. Collections may include, for example, donations made by hospitals to compensate for the
cost of on-site stationing of state or local Medicaid agency personnel to determine eligibility or provide outreach. For more information on specic items from the
Medicaid and CHIP Budget Expenditure System (MBES CBES) noted in this exhibit, see CMS, 2014, MBES CBES category of service line denitions for the 64.10
base form, https://www.medicaid.gov/medicaid/downloads/cms-6410-admin-category-of-services-denition-2-14.pdf.
– Dash indicates zero; $0 or -$0 indicates an amount between $0.5 and -$0.5 million that rounds to zero.
1
All states had certied their CMS-64 Financial Management Report (FMR) submissions as of May 30, 2023. Figures presented in this exhibit may change if states
revise their expenditure data after this date.
2
Includes design and development of systems (90 percent federal match), operation of approved systems (75 percent), and other costs (50 percent).
3
Includes EHR incentive payments to providers (100 percent federal match) and administration of payments (90 percent).
4
Includes skilled medical professionals, preadmission screening and resident review, medical and utilization review, external independent review, survey and
certication, and Medicaid Fraud Control Units (MFCU) operations (all at 75 percent federal match); translation and interpretation services for children and
planning activities for the health home benet (both at match equal to a state's federal medical assistance percentage (FMAP)); eligibility changes associated
with the Temporary Assistance for Needy Families program (75 or 90 percent); administration of family planning services (90 percent); and immigration status
verication systems and design development and implementation of Prescription Drug Monitoring Program systems (100 percent). Excludes MMIS and eligibility
systems, which are included in their own categories.
5
Excludes MMIS and eligibility systems, which are included in their own categories.
6
State-level estimates for MFCUs and survey and certication are available but are not included in the CMS-64 data that MACPAC typically uses to analyze
Medicaid spending.
Sources: For state and territory spending: MACPAC, 2023, analysis of CMS-64 FMR net expenditure data as of May 30, 2023. For all other spending (MFCUs,
survey and certication, VFC program): CMS, 2023, Fiscal year 2024 justication of estimates for appropriations committees, Baltimore, MD, https://www.cms.gov/
les/document/cms-fy-2024-congressional-justication-estimates-appropriations-committees.pdf-0.

December 2023
88
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 32. Child Enrollment in CHIP and Medicaid by State, FY 2022 (thousands)
State
CHIP and Medicaid CHIP-funded coverage
Medicaid-funded
coverage
Total
Medicaid
expansion Separate CHIP Total Total
Total 46,465 5,528 2,746 8,274 38,190
Alabama 806 106 95 202 604
Alaska 126 13 – 13 113
Arizona 1,058 73 68 141 916
Arkansas 528 37 46 83 445
California 6,034 1,478 79 1,556 4,478
Colorado 537 111 32 143 393
Connecticut 412 – 18 18 394
Delaware 131 2 9 11 120
District of Columbia 102 16 – 16 85
Florida 2,914 182 151 333 2,581
Georgia 1,779 86 219 305 1,474
Hawaii 184 24 – 24 160
Idaho 230 2 41 43 187
Illinois 1,756 306 39 344 1,412
Indiana 923 87 35 121 802
Iowa 449 17 66 83 366
Kansas 349 15 47 62 287
Kentucky 674 115 13 128 545
Louisiana 884 189 11 200 684
Maine 232 25
9 34
198
Maryland 730 127 – 127 603
Massachusetts 804 124 97 221 583
Michigan 1,298 128 3 131 1,167
Minnesota 676 1 3 4 672
Mississippi 517 34 49 83 434
Missouri 743 54 54 107 636
Montana 151 7 23 29 121
Nebraska 239 56 2 58 180
Nevada 435 46 30 76 358
New Hampshire 112 23 – 23 89
New Jersey 1,014 116 152 268 746
New Mexico 794 11 – 11 783

MACStats: Medicaid and CHIP Data Book
89
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 32. (continued)
State
CHIP and Medicaid CHIP-funded coverage
Medicaid-funded
coverage
Total
Medicaid
expansion Separate CHIP Total Total
New York 2,820 295 329 624 2,196
North Carolina 1,558 234 68 302 1,255
North Dakota
1
75 3 4 7 68
Ohio 1,540 238 – 238 1,302
Oklahoma 759 231 10 241 518
Oregon 664 74 177 251 413
Pennsylvania 1,630 111 159 270 1,359
Rhode Island 145 31 3 34 111
South Carolina 767 105 – 105 662
South Dakota 100 15 4 19 81
Tennessee 1,092 11 57 69 1,023
Texas 4,453 395 263 658 3,796
Utah 289 27 11 37 251
Vermont 77 5 – 5 72
Virginia 943 95 79 174 769
Washington 935 – 82 82 853
West Virginia 257 14 20 34 224
Wisconsin 693 32 85 117 576
Wyoming 49 1 4 5 44
Notes: FY is scal year. The CHIP and Medicaid total column reects children ever enrolled in CHIP or Medicaid during the year, even if for a single month. Most
states counted children who were enrolled in multiple categories during the year (e.g., in Medicaid-funded coverage for the rst half of the year but in CHIP-
funded coverage for the second half) in the most recent category (state-specic exceptions to this rule are noted below). Medicaid-funded child enrollment shown
here includes all children, regardless of disability status; in other MACStats exhibits that break enrollment out by eligibility group, children qualifying on the basis
of disability may be counted in the disabled category rather than the child category. Data were reported by individual states as of August 14, 2023, and may be
revised at a later date.
– Dash indicates zero.
¹ North Dakota did not report the number of children with Medicaid coverage for FY 2022, so the state's FY 2021 amount was included in this exhibit.
Source: MACPAC, 2023, analysis of CHIP Statistical Enrollment Data System data as of August 14, 2023.

December 2023
90
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 33. CHIP Spending by State, FY 2022 (millions)
State
Total CHIP
Benets
State program
administration
2105(g)
spending
2
Medicaid-expansion CHIP
Separate CHIP programs and
coverage of pregnant women
1
Total Federal State Total Federal State Total Federal State Total Federal State Federal
Alabama $462.4 $392.9 $69.5 $192.3 $163.3 $29.0 $260.2 $221.2 $39.0 $9.9 $8.4 $1.5 –
Alaska 26.3 18.4 7.9 23.8 16.7 7.2 – – – 2.5 1.7 0.8 –
Arizona 407.9 339.0 68.8 217.8 180.9 36.9 178.4 148.5 30.0 11.6 9.7 2.0 –
Arkansas 232.1 196.0 36.0 100.5 84.9 15.6 126.4 106.7 19.6 5.2 4.4 0.8 –
California 4,265.9 2,973.9 1,292.0 4,028.8 2,809.2 1,219.6 147.1 102.2 44.9 90.1 62.6 27.5 –
Colorado 344.9 240.0 104.9 176.9 123.7 53.3 158.7 110.0 48.8 9.2 6.4 2.8 –
Connecticut 50.4 57.3 -6.9 – – – 45.4 31.5 13.9 5.0 3.5 1.5 $22.3
Delaware 34.8 26.0 8.9 9.3 6.9 2.3 24.3 18.1 6.2 1.2
0.9 0.3 –
District of Columbia 61.1 50.9 10.2 59.6 49.6 9.9 -0.0 -0.0 -0.0 1.5 1.3 0.3 –
Florida 787.3 606.4 180.8 448.0 345.2 102.9 307.5 236.8 70.7 31.8 24.5 7.3 –
Georgia 581.3 469.5 111.8 151.3 122.1 29.2 416.5 336.6 80.0 13.4 10.9 2.6 –
Hawaii 71.5 51.3 20.3 68.9 49.4 19.5 -0.0 -0.0 -0.0 2.6 1.9 0.7 –
Idaho 109.3 91.2 18.1 -4.1 -3.4 -0.7 109.8 91.6 18.2 3.6 3.0 0.6 –
Illinois 712.3 499.6 212.7 266.3 186.6 79.6 379.4 266.2 113.2 66.6 46.8 19.9 –
Indiana 269.3 217.5 51.8 175.3 141.5 33.8 85.1 68.8 16.3 8.9 7.2 1.7 –
Iowa 171.0 132.6 38.4 44.4 34.6 9.8 118.8 92.1 26.8 7.8 6.0 1.7 –
Kansas 180.2 137.9 42.3 38.5 29.4 9.1 124.4 95.2 29.2 17.4 13.3 4.1 –
Kentucky 412.9 350.3 62.6 238.8
202.5 36.4 160.2 136.1 24.2 13.8 11.7 2.1 –
Louisiana 509.2 418.2 91.0 401.1 329.7 71.4 88.7 72.6 16.1 19.4 15.9 3.5 –
Maine 45.3 35.8 9.5 29.6 23.4 6.2 13.9 11.0 3.0 1.8 1.4 0.4 –
Maryland 444.7 308.4 136.3 439.4 304.6 134.7 -17.8 -12.4 -5.4 23.2 16.1 7.0 –
Massachusetts 884.4 614.4 270.0 391.6 272.2 119.4 404.5 280.9 123.6 88.3 61.3 27.0 –
Michigan 337.8 270.9 66.9 305.8 245.3 60.5 7.1 5.7 1.4 24.8 19.9 4.9 –
Minnesota 20.0 73.4 -53.4 1.5 1.1 0.5 16.6 11.6 5.0 1.9 1.3 0.6 59.5
Mississippi 207.7 176.7 31.1 86.2 73.4 12.8 118.5 100.7 17.8 3.0 2.5 0.4 –
Missouri 366.3 294.1 72.2 184.0 148.6 35.3 191.6 152.9 38.7 -9.2 -7.4 -1.9 –
Montana 111.8 89.2 22.6 18.6 14.9 3.8 87.5 69.8 17.7 5.7 4.5 1.2
–
Nebraska 111.6 83.1 28.5 96.2 71.6 24.6 9.8 7.3 2.5 5.5 4.1 1.4 –
Nevada 107.0 83.6 23.4 59.7 46.6 13.0 44.2 34.6 9.7 3.1 2.4 0.7 –
New Hampshire 58.3 48.6 9.6 58.3 40.4 17.9 – – – 0.0 0.0 0.0 8.2

MACStats: Medicaid and CHIP Data Book
91
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 33. (continued)
State
Total CHIP
Benets
State program
administration
2105(g)
spending
2
Medicaid-expansion CHIP
Separate CHIP programs and
coverage of pregnant women
1
Total Federal State Total Federal State Total Federal State Total Federal State Federal
New Jersey $833.8 $580.7 $253.1 $358.9 $250.2 $108.7 $396.8 $276.1 $120.7 $78.2 $54.4 $23.8 –
New Mexico 131.0 111.3 19.8 129.9 110.3 19.6 -0.0 -0.0 -0.0 1.2 1.0 0.2 –
New York 1,816.9 1,260.1 556.7 868.1 601.9 266.2 766.9 532.0 234.9 181.9 126.2 55.7 –
North Carolina 763.9 624.2 139.7 568.0 464.2 103.8 181.7 148.4 33.3 14.2 11.6 2.6 –
North Dakota 26.7 19.1 7.6 25.0 17.9 7.1 -0.0 -0.0 -0.0 1.7 1.2 0.5 –
Ohio 694.1 552.5 141.5 658.0 524.0 134.0 – – – 36.0 28.5 7.5 –
Oklahoma 284.5 233.8 50.7 291.0 239.1 51.8 -24.0 -19.7 -4.3 17.5 14.3 3.1 –
Oregon 604.0 461.9 142.1 147.6 112.9 34.7 440.0 336.4 103.5 16.4
12.5 3.9 –
Pennsylvania 706.0 502.9 203.1 411.8 293.3 118.5 275.8 196.5 79.3 18.5 13.2 5.3 –
Rhode Island 130.6 94.9 35.7 103.5 75.2 28.3 25.6 18.6 7.0 1.4 1.0 0.4 –
South Carolina 223.5 187.5 36.1 216.1 181.2 34.9 -1.7 -1.5 -0.3 9.2 7.7 1.5 –
South Dakota 37.1 28.0 9.1 29.5 22.2 7.3 7.1 5.4 1.7 0.5 0.4 0.1 –
Tennessee 403.6 326.2 77.4 254.4 205.7 48.8 145.6 117.7 28.0 3.5 2.8 0.7 –
Texas 1,667.5 1,280.9 386.5 1,328.0 1,021.7 306.3 315.9 241.3 74.6 23.5 18.0 5.6 –
Utah 128.4 104.3 24.2 102.9 83.5 19.4 20.0 16.3 3.7 5.5 4.5 1.0 –
Vermont 16.6 15.8 0.8 15.0 11.1 3.9 -0.0 -0.0 -0.0 1.7 1.2 0.4 $3.5
Virginia 523.3 362.3 161.0 222.4 153.6 68.8 277.2 192.3 84.9 23.7 16.4 7.3 –
Washington 240.3 224.8 15.5 28.1
19.5 8.6 204.4 139.0 65.4 7.8 5.3 2.5 61.0
West Virginia 88.4 75.1 13.3 34.0 28.9 5.1 48.4 41.2 7.3 6.0 5.1 0.9 –
Wisconsin 305.3 245.4 60.0 108.5 83.2 25.4 170.6 130.4 40.2 26.2 20.0 6.2 11.8
Wyoming 9.2 6.3 2.8 8.8 6.1 2.7 0.0 0.0 0.0 0.3 0.2 0.1 –
Subtotal (states)
$22,019.3 $16,645.0 $5,374.3 $14,218.1 $10,620.5 $3,597.6 $6,856.9 $5,166.3 $1,690.6 $944.3 $691.8 $252.5 $166.4
American Samoa 8.4 7.4 0.9 8.4 7.4 0.9 – – – – – – –
Guam 1.3 1.3 – 1.3 1.3 – – – – – – – –
Northern Mariana
Islands
19.7 16.9 2.8 19.7 16.9 2.8 – – – – – – –
Puerto Rico 217.0 184.9 32.2 217.0 184.9 32.2 – – – – – – –
Virgin Islands 3.2 2.7 0.5 3.2 2.7 0.5 – – – – – – –
Total $22,268.9 $16,858.3 $5,410.6 $14,467.7 $10,833.8 $3,633.9 $6,856.9 $5,166.3 $1,690.6 $944.3 $691.8 $252.5 $166.4

December 2023
92
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
EXHIBIT 33. (continued)
Notes: FY is scal year. Components may not add to total due to rounding. Federal CHIP spending on administration is generally limited to 10 percent of a state’s
total federal CHIP spending for the year. States with Medicaid-expansion CHIP may elect to receive reimbursement for administrative spending from Medicaid
rather than CHIP funds; Medicaid funds are not shown in this exhibit.
– Dash indicates zero; $0.0 or -$0.0 indicates an amount between $0.05 million and -$0.05 million that rounds to zero.
1
Seven states (Colorado, Kentucky, Missouri, New Jersey, Rhode Island, Virginia, and West Virginia) use CHIP funds to provide coverage for pregnant women
(MACPAC uses the term "pregnant women" as this is the term used in the statute and regulations. However, other terms are being used increasingly in recognition
that not all individuals who become pregnant and give birth identify as women).
2
Section 2105(g) of the Social Security Act permits 11 qualifying states to use CHIP funds to pay the dierence between the regular Medicaid matching rate
and the enhanced CHIP matching rate for Medicaid-enrolled, Medicaid-nanced children whose family income exceeds 133 percent of the federal poverty level.
Although these are CHIP funds, they eectively reduce state spending on children in Medicaid and do not require a state match within the CHIP program. In cases
in which the sum of 2105(g) federal CHIP spending (for Medicaid enrollees) and regular federal CHIP spending (for CHIP enrollees) exceeds total spending for
CHIP enrollees, states are shown in this table as having negative state CHIP spending (Connecticut and Minnesota).
Source: MACPAC, 2023, analysis of Medicaid and CHIP Budget Expenditure System data from CMS as of October 9, 2023.

MACStats: Medicaid and CHIP Data Book
93
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 3
EXHIBIT 34. Federal CHIP Allotments, FYs 2021–2023 (millions)
State
FY 2021 federal
CHIP allotments
FY 2022 federal
CHIP allotments
1
FY 2023 federal
CHIP allotments
Alabama $368.1 $390.8 $434.9
Alaska 25.7 27.6 20.3
Arizona 248.9 264.6 375.0
Arkansas 208.8 221.2 216.8
California 3,346.6 3,548.3 3,294.1
Colorado 279.6 300.5 265.7
Connecticut 73.5 77.8 64.0
Delaware 37.4 39.6 28.7
District of Columbia 61.1 65.2 56.3
Florida 781.9 831.0 671.6
Georgia 418.6 493.8 519.4
Hawaii 55.3 59.0 56.7
Idaho 85.7 91.2 101.9
Illinois 536.0 567.9 552.6
Indiana 272.4 288.8 241.2
Iowa 166.6 185.7 146.7
Kansas 146.4 155.3 152.5
Kentucky 253.4 293.9 387.5
Louisiana 393.7 418.7 462.6
Maine 35.7 37.8 39.6
Maryland 285.4 302.4 341.1
Massachusetts 682.1 725.8 679.9
Michigan 271.5 288.8 299.7
Minnesota 114.8 121.6 81.2
Mississippi 270.8 287.6 195.6
Missouri 326.9 346.6 325.6
Montana 86.6 92.1 98.8
Nebraska 81.6 86.5 91.9
Nevada 82.6 87.6 92.5
New Hampshire 47.8 50.6 53.8
New Jersey 614.7 661.3 643.0
New Mexico 115.4
122.3 123.2
New York
1,603.9 1,699.4 1,394.0
North Carolina 555.9 590.6 690.8
North Dakota 18.4 19.6 21.1
Ohio 521.2 555.5 611.2
Oklahoma 262.6 278.4 258.6

December 2023
94
Section 3: Program Enrollment and Spending—CHIP
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 3
State
FY 2021 federal
CHIP allotments
FY 2022 federal
CHIP allotments
1
FY 2023 federal
CHIP allotments
Oregon $429.7 $455.2 $510.9
Pennsylvania 695.2 736.6 559.0
Rhode Island 75.6 80.1 105.0
South Carolina 207.9 220.7 207.5
South Dakota 29.5 31.2 30.9
Tennessee 304.4 323.4 361.3
Texas 1,355.6 1,440.7 1,417.0
Utah 127.3 135.1 115.3
Vermont 20.8 22.0 17.5
Virginia 378.6 403.3 400.8
Washington 247.7 263.5 250.7
West Virginia 78.9 83.7 83.1
Wisconsin 250.5 265.7 271.4
Wyoming 12.2 12.9 7.0
Subtotal (states) $17,951.4 $19,149.8 $18,427.7
American Samoa 6.3 7.4 8.9
Guam 30.7 32.5 1.5
Northern Mariana Islands 17.2 18.2 18.7
Puerto Rico 117.4 127.0 204.5
Virgin Islands 12.2 12.9 3.0
Total (states and territories) $18,135.2 $19,347.9 $18,664.3
Notes: FY is scal year.
1
States with approved CHIP state plans to expand eligibility for children or benets may request an increased CHIP allotment
for even-number years beginning in FY 2010 and ending in FY 2029 (§ 2104(m)(7) of the Social Security Act). The FY 2022
allotment for a state may dier from previously published allotments for the scal year because the state received such an
allotment increase.
Sources: MACPAC, 2023, analysis of Medicaid and CHIP Budget Expenditure System data as of October 10, 2023.
EXHIBIT 34. (continued)

SECTION 4:
Medicaid and
CHIP Eligibility

December 2023
96
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 4
Section 4: Medicaid and CHIP Eligibility
Key Points
•
Thirty-nine states and the District of Columbia now cover low-income adults not otherwise eligible
on the basis of disability, a new Medicaid eligibility group created under the Patient Protection and
Aordable Care Act (ACA, P.L. 111-148, as amended) (Exhibit 36). One state has approved Medicaid
expansion but has not implemented it as of July 2023.
•
Eligibility levels under Medicaid and the State Children’s Health Insurance Program (CHIP) for most
children and adults eligible on a basis other than disability are determined using uniform modied
adjusted gross income (MAGI) rules (Exhibits 35 and 36).
•
Eligibility criteria for individuals eligible for Medicaid on the basis of disability and for individuals age
65 and older, who are not subject to MAGI rules, were largely unchanged between 2022 and 2023
(Exhibit 37).
•
In 2023, in the lower 48 states and the District of Columbia, 100 percent federal poverty level (FPL)
is $14,580 for an individual plus $5,140 for each additional family member (Exhibit 38).

MACStats: Medicaid and CHIP Data Book
97
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 4
EXHIBIT 35. Medicaid and CHIP Income Eligibility Levels as a Percentage of the FPL for Children and Pregnant Women by State, July 2023
State
CHIP program type
1
(as of July 2023)
Medicaid coverage
2
Separate CHIP
coverage
Medicaid and
CHIP coverage
Infants under age 1 Age 1–5 Age 6–18
Birth
through
age 18
3
Unborn
children
4
Pregnant women
and deemed
newborns
5
Medicaid
funded
CHIP
funded
Medicaid
funded
CHIP
funded
Medicaid
funded
CHIP
funded
Alabama Combination 141% – 141% – 141% 107–141% 312% – 141%
Alaska Medicaid expansion 177 159–203% 177 159–203% 177 124–203 – – 200
Arizona Combination 147 – 141 – 133 104–133 200 – 156
Arkansas Combination 142 – 142 – 142 107–142 211 209% 209
California Combination 208 208–261 142 142–261 133 108–261 –
6
317 208
Colorado Combination 142 – 142 – 142 108–142 260 – 195; 260
Connecticut Separate 196 – 196 – 196 – 318 258 258
Delaware Combination 212 194–212 142 – 133 110–133 212
7
– 212
District of
Columbia
Medicaid expansion 319 206–319 319 146–319 319 112–319 – – 319
Florida Combination 206 192–206 140 – 133 112–133 210
7
– 191
Georgia Combination 205 – 149 – 133 113–133 247 – 220
Hawaii Medicaid expansion 191 191–308 139 139–308 133 105–308 – – 191
Idaho Combination 142 – 142 – 133 107–133 185 – 133
Illinois Combination 142 142–313 142 142–313 142 108–313 – 208 208
Indiana Combination 208 157–208 158 141–158 158 106–158 250 – 208
Iowa Combination 375 240–375 167 – 167 122–167 302
7
– 375
Kansas Combination 166 – 149 – 133 113–133 250 – 166
Kentucky Combination 195 195- 213 142 142–213 133 109–213 – – 195; 213
Louisiana Combination 142 142–212 142 142–212 142 108–212 250 209 133
Maine Combination 208 191-208 208 140–208 208 132–208 – 208 209
Maryland Medicaid expansion 194 194–317 138 138–317 133 109–317 – – 259
Massachusetts Combination 200 185–200 150 133–150 150 114–150 300 200 200
Michigan Combination 195 195–212 160 143–212 160 109–212 – 195 195
Minnesota Combination 275 275–283
8
275 – 275 – – 278 278
Mississippi Combination 194 – 143 – 133 107–133 209 – 194
Missouri Combination 196 – 148 148–150 148 110–150 300 300 196; 300
Montana Combination 143 – 143 – 133 109–143 261 – 157
Nebraska Combination 162 162–213 145 145–213 133 109–213 – 197 194
Nevada Combination 160 – 160 – 133 122–133 200 – 160
New Hampshire Medicaid expansion 196 196–318 196 196–318 196 196–318 – – 196

December 2023
98
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 4
EXHIBIT 35. (continued)
State
CHIP program type
1
(as of July 2023)
Medicaid coverage
2
Separate CHIP
coverage
Medicaid and
CHIP coverage
Infants under age 1 Age 1–5 Age 6–18
Birth
through
age 18
3
Unborn
children
4
Pregnant women
and deemed
newborns
5
Medicaid
funded
CHIP
funded
Medicaid
funded
CHIP
funded
Medicaid
funded
CHIP
funded
New Jersey Combination 194% – 142% – 142% 107–142% 350% – 194; 200%
New Mexico Medicaid expansion 240 200–300% 240 200–300% 190 138–240 – – 250
New York Combination 218 – 149 – 149 110–149 400 – 218
North Carolina Medicaid expansion 211 194–211 211 141–211 211 107–133 – – 196
North Dakota Medicaid expansion 147 147–170 147 147–170 133 111–170 – – 157
Ohio Medicaid expansion 156 141–206 156 141–206 156 107–206 – – 200
Oklahoma Combination 205 169–205 205 151–205 205 115–205 – 205% 133
Oregon Combination 185 133–185 133 – 133 100–133 300 185 185
Pennsylvania Combination 215 – 157 – 133 119–133 314 – 215
Rhode Island Combination 190 190–261 142 142–261 133 109–261 – 253 190; 253
South Carolina Medicaid expansion 194 194–208 143 143–208 133 107–208 – – 194
South Dakota Combination 182 147–182 182 147–182 182 111–182 204 133 133
Tennessee
9
Combination 195 – 142 – 133 109–133 250 250 195
Texas Combination 198 – 144 – 133 109–133 201 202 198
Utah Combination 139 – 139 – 133 105–133 200 – 139
Vermont Medicaid expansion 312 237–312 312 237–312 312 237–312 – – 208
Virginia Combination 143 – 143 – 143 109–143 200 200 143; 200
Washington Separate 210 – 210 – 210 – 312 193 193
West Virginia Combination 158 – 141 – 133 108–133 300 – 185; 300
Wisconsin Combination 301 – 186 – 133 101–151 301
7
301 301
Wyoming Medicaid expansion 154 154–200 154 154–200 133 119–200 – – 154
Notes: As of January 2023, 100 percent of the federal poverty level (FPL) in the lower 48 states and the District of Columbia was $14,580 for an individual plus
$5,140 for each additional family member. Before 2014, states had the exibility to disregard income sources and amounts of their choosing when determining
Medicaid and CHIP eligibility. In 2014, uniform modied adjusted gross income (MAGI) rules became mandatory for determining Medicaid and CHIP eligibility
for most children and adults under age 65 eligible for Medicaid on a basis other than disability, including the groups shown in this table. As a result, states are
now required to use MAGI-converted eligibility levels that account for the change in income-counting rules. The eligibility levels shown in this table reect these
MAGI-converted levels or another MAGI-based income limit in eect in each state for these groups as of July 2023. Under federal regulations, the eective income
limits may be 5 percentage points higher than the percentage of FPL shown in this table to account for a general income disregard that applies to an individual’s
eligibility under the group with the highest income standard, rather than for particular eligibility groups within Medicaid or CHIP.
Medicaid (Title XIX of the Social Security Act (the Act)) funding continues to nance Medicaid coverage of children under age 19 in families with incomes below
state eligibility levels in eect as of March 31, 1997. Any expansion of eligibility to uninsured children above those levels—through expansions of Medicaid or
through separate CHIP programs—is generally nanced by CHIP (Title XXI of the Act) funding. CHIP funding is not permitted for children with other coverage.

MACStats: Medicaid and CHIP Data Book
99
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 4
EXHIBIT 35. (continued)
Thus, where Medicaid coverage in this table shows overlapping eligibility levels for Medicaid funding and CHIP funding, children with no other coverage are funded
by CHIP, while children with other coverage are funded by Medicaid. Pregnant women can receive Medicaid- or CHIP-funded services through regular state plan
eligibility pathways or through waivers under Section 1115 of the Act; in addition, the unborn children of pregnant women may receive CHIP-funded coverage
under a state plan option.
– Dash indicates that state does not use this eligibility pathway.
¹ Under CHIP, states can implement Medicaid expansion, separate CHIP, or a combination program. Eleven states (Alaska, Hawaii, Maryland, New Hampshire,
New Mexico, North Carolina, North Dakota, Ohio, South Carolina, Vermont, and Wyoming) and the District of Columbia use Medicaid expansion, and two states
(Connecticut and Washington) use separate CHIP. Thirty-seven states use combination programs, although some of these are combination programs solely as
a result of the transition of children in families with income less than or equal to 133 percent FPL from separate CHIP to Medicaid. In six states with combination
programs (Illinois, Michigan, Minnesota, Nebraska, Oklahoma, and Rhode Island), separate CHIP coverage is only through the unborn child option.
² Under Medicaid-funded coverage, there is no lower threshold for income eligibility. The eligibility levels listed are the highest income levels under which each
age group of children is covered under the Medicaid state plan. The eligibility levels listed under CHIP-funded Medicaid coverage are the income levels to which
Medicaid has expanded using CHIP funds (which became available when CHIP was created in 1997). For states that set dierent CHIP-funded eligibility levels
for children age 6–13 and age 14–18, this table shows only the levels for children age 6–13. In addition, Section 2105(g) of the Act permits 11 qualifying states to
use CHIP funds to pay the dierence between the regular Medicaid matching rate and the enhanced CHIP matching rate for Medicaid-enrolled, Medicaid-nanced
uninsured children whose family income exceeds 133 percent FPL (not separately noted on this table).
³ Separate CHIP eligibility for children from birth through age 18 generally begins where Medicaid coverage ends (as shown in the previous columns).
⁴ For unborn children, there is no lower threshold for income eligibility if the mother is not eligible for Medicaid.
⁵ Deemed newborns are infants up to age one who are deemed eligible for Medicaid or CHIP—with no separate application or eligibility determination required—if
their mother was enrolled at the time of their birth. Pregnant women can be covered with Medicaid or CHIP funding (MACPAC uses the term "pregnant women" as
this is the term used in the statute and regulations. However, other terms are being used increasingly in recognition that not all individuals who become pregnant
and give birth identify as women). Under CHIP, coverage can be through a state plan option for targeted low-income pregnant women or through continuation of an
existing Section 1115 waiver. When two values are shown in this column, the rst is for Medicaid and the second is for CHIP.
⁶ In California, certain children up to age two with incomes above 261 percent FPL up to 317 percent FPL are covered statewide, and children in three counties are
covered above 261 percent FPL up to 317 percent FPL through a separate CHIP program.
⁷ In Delaware, Florida, Iowa, and Wisconsin, separate CHIP covers children age 1 through 18.
⁸ In Minnesota, infants (dened by the state as being under age two) are eligible for Medicaid-expansion CHIP up to 283 percent FPL.
⁹ Although Tennessee covers children with CHIP-funded Medicaid, coverage is available only for children under age 19 who are enrolled in Medicaid but no longer
qualify and lack access to health insurance through a parent's employer.
Source: MACPAC, 2023, analysis of CMS, 2023, Medicaid, Children's Health Insurance Program, & Basic Health Program Eligibility Levels, https://www.medicaid.
gov/medicaid/national-medicaid-chip-program-information/medicaid-childrens-health-insurance-program-basic-health-program-eligibility-levels/index.html; CMS,
2023, Medicaid state plan amendments, https://www.medicaid.gov/state-resource-center/medicaid-state-plan-amendments/index.html; CMS, 2023, CHIP state
plan amendments, https://www.medicaid.gov/chip/state-program-information/index.html; Kaiser Family Foundation (KFF), 2023, Medicaid and CHIP eligibility,
enrollment, and renewal policies as states prepare for the unwinding of the pandemic-era continuous enrollment provision, San Francisco, CA: KFF, https://les.k.
org/attachment/REPORT-Medicaid-and-CHIP-Eligibility-Enrollment-and-Renewal-Policies-as-States-Prepare-for-the-Unwinding-of-the-Pandemic-Era-Continuous-
Enrollment-Provision.pdf; and eligibility information from state websites.

December 2023
100
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 4
EXHIBIT 36. Medicaid Income Eligibility Levels as a Percentage of the Federal Poverty Level for Non-Aged, Non-
Disabled, Non-Pregnant Adults by State, July 2023
State
Parents and caretaker relatives of
dependent children
1
Additional individuals age 19–64
2
Alabama 13% –
Alaska 130 133%
Arizona 106 133
Arkansas 13 133
California 109 133
Colorado 68 133
Connecticut 155 133
Delaware 87 133
District of Columbia 216 210 (age 19–20 only: 216)
Florida 24 Age 19–20 only: 24
Georgia 28 –
Hawaii 105 133
Idaho 19 133
Illinois 133 133
Indiana 15 133
Iowa 44 133
Kansas 33 –
Kentucky 19 133
Louisiana 19 133
Maine 100 133 (age 19–20 only: 156)
Maryland 123 133
Massachusetts 133 133 (age 19–20 only: 150)
Michigan 54 133
Minnesota 133
3
133
3
Mississippi 19 –
Missouri 15 133
Montana 24 133
Nebraska 58 133
Nevada 26 133
New Hampshire 55 133
New Jersey 26 133
New Mexico 37 133
New York 133
3
133
3
North Carolina 36 Age 19–20 only: 36
North Dakota 43 133
Ohio 90 133
Oklahoma 33
4
133
5
Oregon 33 133
MACStats: Medicaid and CHIP Data Book
101
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 4
EXHIBIT 36. (continued)
State
Parents and caretaker relatives of
dependent children
1
Additional individuals age 19–64
2
Pennsylvania 33% 133%
Rhode Island 116 133
South Carolina 95 –
5
South Dakota 46 133
Tennessee 84 –
Texas 12 –
Utah 36
4
133
5
Vermont 43 133
Virginia 49 133
Washington 33 133
West Virginia 16 133
Wisconsin 95 95
Wyoming 45 –
Notes: As of January 2023, 100 percent of the federal poverty level (FPL) in the lower 48 states and the District of Columbia
was $14,580 for an individual plus $5,140 for each additional family member. Before 2014, states had the exibility to
disregard income sources and amounts of their choosing when determining Medicaid and CHIP eligibility. In 2014, uniform
modied adjusted gross income (MAGI) rules became mandatory for determining Medicaid and CHIP eligibility for most
children and adults under age 65 eligible for Medicaid on a basis other than disability, including the groups shown in this
table. As a result, states are now required to use MAGI-converted eligibility levels that account for the change in income-
counting rules. The eligibility levels shown in this table reect these MAGI-converted levels or another MAGI-based income
limit in eect in each state for these groups as of July 2023. Under federal regulations, the eective income limits may be 5
percentage points higher than the percentage of FPL shown in this table to account for a general income disregard that applies
to an individual’s eligibility under the group with the highest income standard, rather than for particular eligibility groups within
Medicaid or CHIP.
States are required to provide Medicaid coverage for parents and other caretaker relatives (and their dependent children)
at or above the state's 1988 Aid to Families with Dependent Children eligibility levels. Under regular Medicaid state plan
rules, states may opt to cover additional parents and caretaker relatives, children age 19–20, and other individuals age
19–64 who have incomes less than or equal to 133 percent FPL and are not pregnant or eligible for Medicare. Certain states
provide coverage through Section 1115 waivers, which allow them to operate their Medicaid programs with fewer statutory
requirements. As noted in this table, the covered benets under these waivers may be more limited than those provided under
regular state plan rules and might not be available to all individuals at the income levels shown.
– Dash indicates that state does not use this eligibility pathway.
¹ In states that use dollar amounts rather than percentage of FPL to determine eligibility for parents, dollar amounts were
converted to percentage of FPL, and the highest percentage was selected to reect eligibility level for the group. Parents and
caretaker relatives with income above the reported threshold for this group may be eligible for coverage under the new adult
group (under Section 1902(a)(10)(A)(i)(VIII) of the Social Security Act (the Act)) in states that have adopted the expansion.
² Reects state plan coverage under Section 1902(a)(10)(A)(i)(VIII) of the Act for individuals who are age 19–64, have incomes
less than or equal to 133 percent FPL, and are not pregnant or eligible for Medicare; state plan coverage for children age
19–20 where indicated; and Section 1115 waiver coverage that is not subject to the limitations indicated in note 5.
³ In Minnesota and New York, individuals with incomes that are greater than 133 percent FPL but do not exceed 200 percent
FPL are covered under the Basic Health Program.
⁴ Reects parent coverage under the Medicaid state plan. The state has some additional coverage above state plan eligibility
standards through a Section 1115 demonstration. The demonstration includes limitations on eligibility or benets, is not oered
to all residents of the state, or includes an enrollment cap.

December 2023
102
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 4
EXHIBIT 36. (continued)
⁵ The state has a Section 1115 demonstration that provides Medicaid coverage to some low-income adults. The demonstration
includes limitations on eligibility or benets, is not oered to all residents of the state, or includes an enrollment cap.
Source: MACPAC, 2023, analysis of CMS, 2023, Medicaid, Children's Health Insurance Program, & Basic Health Program
Eligibility Levels, https://www.medicaid.gov/medicaid/national-medicaid-chip-program-information/medicaid-childrens-
health-insurance-program-basic-health-program-eligibility-levels/index.html; CMS, 2023, Medicaid state plan amendments,
https://www.medicaid.gov/state-resource-center/medicaid-state-plan-amendments/index.html; CMS, 2023, CHIP state plan
amendments, https://www.medicaid.gov/chip/state-program-information/index.html; Kaiser Family Foundation (KFF), 2023,
Medicaid and CHIP eligibility, enrollment, and renewal policies as states prepare for the unwinding of the pandemic-era
continuous enrollment provision, San Francisco, CA: KFF, https://les.k.org/attachment/REPORT-Medicaid-and-CHIP-
Eligibility-Enrollment-and-Renewal-Policies-as-States-Prepare-for-the-Unwinding-of-the-Pandemic-Era-Continuous-Enrollmen-
t-Provision.pdf; and eligibility information from state websites.

MACStats: Medicaid and CHIP Data Book
103
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 4
EXHIBIT 37. Medicaid Income Eligibility Levels as a Percentage of the Federal Poverty Level for Individuals Age 65 and Older and Persons with
Disabilities by State, 2023
State
State eligibility
type
1
SSI recipients
2
§ 209(b) eligibility Poverty level
3
Medically needy
4
Special income
level
5
Alabama § 1634 75% – – – 226%
Alaska SSI criteria 60
6
– – – 181
Arizona § 1634 75 – – – 226
Arkansas § 1634 75 – 80% (aged only) 9% 226
California § 1634 75 – 138
7
43 –
Colorado § 1634 75 – – – 226
Connecticut § 209(b) – 58% – 58 226
Delaware § 1634 75 – – – 188
District of Columbia § 1634 75 – 100 64 226
Florida § 1634 75 – 88 15 226
Georgia § 1634 75 – – 26 226
Hawaii § 209(b) – 65 100 34 –
Idaho SSI criteria 75 – 78 – 226
Illinois § 209(b) – 100 100 100 –
Indiana § 1634 75 – 100 – 226
Iowa § 1634 75 – – 40 226
Kansas SSI criteria 75 – – 39
226
Kentucky
§ 1634 75 – – 18 226
Louisiana § 1634 75 – – 8 226
Maine § 1634 75 – 100 26 226
Maryland § 1634 75 – – 29 226
Massachusetts
8
§ 1634 75 – 100 (aged); 133 (disabled) 43 226
Michigan § 1634 75 – 100 34 226
Minnesota § 209(b) – 100 100 40 226
Mississippi § 1634 75 – – – 226
Missouri § 209(b) – 85 85 85 132
Montana § 1634 75 – 75 43 –
Nebraska SSI criteria 75 – 100 32 –

December 2023
104
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 4
EXHIBIT 37. (continued)
State
State eligibility
type
1
SSI recipients
2
§ 209(b) eligibility Poverty level
3
Medically needy
4
Special income
level
5
Nevada SSI criteria 75% – – – 226%
New Hampshire § 209(b) – 76% – 73% 226
New Jersey § 1634 75 – 100% 30 226
New Mexico § 1634 75 – – – 226
New York § 1634 75 – – 138 –
North Carolina § 1634 75 – 100 20 –
North Dakota § 209(b) – 83 – 83
9
–
Ohio § 1634 75 – – – 226
Oklahoma SSI criteria 75 – 100 – 226
Oregon SSI criteria 75 – – – 226
Pennsylvania § 1634 75 – 100 35 226
Rhode Island § 1634 75 – 100 90 226
South Carolina § 1634 75 – 100 – 226
South Dakota § 1634 75 – – – 226
Tennessee § 1634 75 – – – 226
Texas § 1634 75 – – – 226
Utah SSI criteria 75 – 100 100 226
Vermont § 1634
75 – – 96 226
Virginia § 209(b) – 75 80 50 226
Washington § 1634 75 – – 75 226
West Virginia § 1634 75 – – 16 226
Wisconsin § 1634 75 – 82 100 226
Wyoming § 1634 75 – – – 226
Notes: SSI is Supplemental Security Income. § 209(b) refers to Section 209(b) of the Social Security Act Amendments of 1972. § 1634 refers to Section 1634 of
the Social Security Act. In 2023, 100 percent of the federal poverty level (FPL) in the lower 48 states and the District of Columbia is $14,580 for an individual and
$5,140 for each additional family member. Eligibility levels shown here apply to countable income; as a result, states that use optional income disregards to reduce
countable income eectively allow more people to qualify at a given eligibility level (e.g., 100 percent FPL) than states that do not use income disregards. The
eligibility levels listed in this table are for individuals; the eligibility levels for couples dier for certain categories. In addition, income eligibility levels for individuals
who qualify based on blindness may be higher than for individuals age 65 or older or who qualify on the basis of other disabilities.

MACStats: Medicaid and CHIP Data Book
105
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 4
EXHIBIT 37. (continued)
In most states, enrollment in the SSI program for individuals age 65 and older and persons eligible on the basis of disability automatically qualies them for
Medicaid. However, Section 209(b) states may use more restrictive criteria (related to income and assets, disability, or both) than SSI when determining Medicaid
eligibility. All states have the option of covering additional people with low incomes or high medical expenses through other eligibility pathways, such as poverty
level, medically needy, and special income level.
The categories displayed in this exhibit do not include all Medicaid eligibility pathways for individuals 65 years old or those qualifying on the basis of disability.
Other eligibility groups include but are not limited to individuals who meet the income and resource requirements of the cash assistance programs; individuals
receiving only optional state supplements; individuals receiving state plan home- and community-based services; individuals who have disabilities and are earning
income; individuals who are receiving hospice services or are in the Program for All Inclusive Care for the Elderly (PACE); and other discrete eligibility groups.
– Dash indicates that state does not use this eligibility pathway.
1
SSI criteria are used to determine Medicaid eligibility in both Section 1634 and SSI-criteria states. In Section 1634 states, the federal eligibility determination
process for SSI automatically qualies an individual for Medicaid; in SSI-criteria states, individuals must submit information to the state for a separate eligibility
determination. Section 209(b) states may use eligibility criteria (related to income and assets, disability, or both) that are more restrictive than SSI program criteria,
but they may not use more restrictive criteria than those in eect in the state on January 1, 1972. If a Section 209(b) state does not have a separate medically
needy standard, it must allow individuals with higher incomes to spend down to the Section 209(b) income level shown here by deducting incurred medical
expenses from the amount of income that is counted for Medicaid eligibility purposes.
2
The SSI federal benet rate as a percent of the FPL increased from last year because the FPL increased by 7.3 percent but the SSI federal benet rate increased
by 8.7 percent.
3
Under the poverty level option (§1902(a)(10)(A)(ii)(X)), states may choose to provide Medicaid coverage to individuals who are age 65 and older or have
disabilities and whose income is above the SSI or Section 209(b) level but is less than or equal to the FPL. Some states, such as Arizona, provide coverage to
other low-income aged, blind, and disabled individuals through an income disregard. Such coverage is not included here.
4
Under the medically needy option, individuals with higher incomes can spend down to the medically needy income level shown here by deducting incurred
medical expenses from the amount of income that is counted for Medicaid eligibility purposes. Four states (Louisiana, Michigan, Vermont, and Virginia) have a
medically needy income standard that varies by location; the highest income standard is listed for each of these states.
5
Under the special income level option, states have the option to provide Medicaid benets to people who require at least 30 days of nursing facility or other
institutional care and have incomes up to 300 percent of the SSI benet rate (which was about 226 percent FPL in 2023). The income thresholds listed in this
column may be for institutional services, home- and community-based waiver services, or both.
6
The dollar amount that equals the upper income eligibility level for SSI does not vary by state; however, the dollar amount that equals the FPL is higher in Alaska,
resulting in a lower percentage.
7
California disregards income between 100 percent and 138 percent of FPL, eectively raising the poverty level income limit to 138 percent of FPL.
8
Massachusetts provides medically needy coverage for individuals who are age 65 and older and those who are eligible on the basis of disability, but the rules for
counting income and spend-down expenses vary for these groups.
9
North Dakota disregards income between the medically needy income limit ($500 per month or approximately 44 percent FPL) and 83 percent FPL for its aged,
blind, and disabled medically needy group. This eectively raises the medically needy income limit to 83 percent FPL.
Source: MACPAC, 2023, analysis of eligibility information from state websites and Medicaid state plans as of November 2023.

December 2023
106
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 4
EXHIBIT 38. Income as a Percentage of the Federal Poverty Level (FPL) for Various Family Sizes, 2023
States FPL
Annual amount Monthly amount
Family size Family size
1 2 3 4
Each
additional
person 1 2 3 4
Each
additional
person
Lower 48
states and
District of
Columbia
100% $14,580 $19,720 $24,860 $30,000 $5,140 $1,215 $1,643 $2,072 $2,500 $428
133 19,391 26,228 33,064 39,900 6,836 1,616 2,186 2,755 3,325 570
138 20,120 27,214 34,307 41,400 7,093 1,677 2,268 2,859 3,450 591
150 21,870 29,580 37,290 45,000 7,710 1,823 2,465 3,108 3,750 643
185 26,973 36,482 45,991 55,500 9,509 2,248 3,040 3,833 4,625 792
200 29,160 39,440 49,720 60,000 10,280 2,430 3,287 4,143 5,000 857
250 36,450 49,300 62,150 75,000 12,850 3,038 4,108 5,179 6,250 1,071
300 43,740 59,160 74,580 90,000 15,420 3,645 4,930 6,215 7,500 1,285
400 58,320 78,880 99,440 120,000 20,560 4,860 6,573 8,287 10,000 1,713
Alaska
100% $18,210 $24,640 $31,070 $37,500 $6,430 $1,518 $2,053 $2,589 $3,125 $536
133 24,219 32,771 41,323 49,875 8,552
2,018 2,731 3,444 4,156 713
138 25,130 34,003 42,877 51,750 8,873 2,094 2,834 3,573 4,313 739
150 27,315 36,960 46,605 56,250 9,645 2,276 3,080 3,884 4,688 804
185 33,689 45,584 57,480 69,375 11,896 2,807 3,799 4,790 5,781 991
200 36,420 49,280 62,140 75,000 12,860 3,035 4,107 5,178 6,250 1,072
250 45,525 61,600 77,675 93,750 16,075 3,794 5,133 6,473 7,813 1,340
300 54,630 73,920 93,210 112,500 19,290 4,553 6,160 7,768 9,375 1,608
400 72,840 98,560 124,280 150,000 25,720 6,070 8,213 10,357 12,500 2,143

MACStats: Medicaid and CHIP Data Book
107
Section 4: Medicaid and CHIP Eligibility
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 4
States FPL
Annual amount Monthly amount
Family size Family size
1 2 3 4
Each
additional
person 1 2 3 4
Each
additional
person
Hawaii
100% $16,770 $22,680 $28,590 $34,500 $5,910 $1,398 $1,890 $2,383 $2,875 $493
133 22,304 30,164 38,025 45,885 7,860 1,859 2,514 3,169 3,824 655
138 23,143 31,298 39,454 47,610 8,156 1,929 2,608 3,288 3,968 680
150 25,155 34,020 42,885 51,750 8,865 2,096 2,835 3,574 4,313 739
185 31,025 41,958 52,892 63,825 10,934 2,585 3,497 4,408 5,319 911
200 33,540 45,360 57,180 69,000 11,820 2,795 3,780 4,765 5,750 985
250 41,925 56,700 71,475 86,250 14,775 3,494 4,725 5,956 7,188 1,231
300 50,310 68,040 85,770 103,500 17,730 4,193 5,670 7,148 8,625 1,478
400 67,080 90,720 114,360 138,000 23,640 5,590 7,560 9,530 11,500 1,970
Notes: FPL is federal poverty level. The FPLs shown here are based on the U.S. Department of Health and Human Services (HHS) 2023 federal poverty
guidelines. These dier slightly from the U.S. Census Bureau’s federal poverty thresholds, which are used mainly for statistical purposes. The separate poverty
guidelines for Alaska and Hawaii reect Oce of Economic Opportunity administrative practice beginning in the 1966–1970 period.
Source: HHS, 2023, Annual update of the HHS poverty guidelines, Federal Register 88, no. 12 (January 19): 3424–3425.
EXHIBIT 38. (continued)


SECTION 5:
Beneficiary Health,
Service Use, and
Access to Care

Section 5: Beneciary Health, Service Use, and Access to Care
December 2023
110
Section 5: Beneciary Health, Service Use,
and Access to Care
Key Points
•
Children whose primary coverage source is Medicaid or the State Children’s Health Insurance
Program (CHIP) are less likely to be in excellent or very good health than those who have private
coverage (Exhibit 39).
•
Children whose primary coverage source is Medicaid or CHIP are as likely to report seeing a doctor
or having a wellness visit within the past year as those with private coverage and more likely than
those who are uninsured (Exhibit 40). Children whose primary coverage source is Medicaid or
CHIP are as likely to experience delayed care because of cost as children with private coverage
(Exhibit 42). However, while most children whose primary coverage source is Medicaid or CHIP
had a usual source of care, they were less likely to have one compared with children with private
coverage (Exhibits 42).
•
Children with Medicaid or CHIP are less likely than those with private coverage but more likely than
those who are uninsured to have had a dental care visit in the past 12 months (Exhibit 41).
•
Adults age 19 to 64 whose primary coverage source is Medicaid or CHIP are less likely to be in
excellent or very good health than those who have private coverage or are uninsured. Adults age
19 to 64 whose primary coverage source is Medicare, who must meet federal disability criteria
to receive coverage, report the poorest health and highest service use in this age group
(Exhibits 44–46).
•
Adults age 19 to 64 whose primary coverage is Medicaid are less likely to report having a usual
source of care than those with private and Medicare coverage (Exhibit 47). Among adults age 19 to
64 with health coverage (i.e., excluding the uninsured), adults whose primary coverage source is
Medicaid report lower rates of delayed care due to cost compared to those with Medicare coverage
but higher than those with private insurance (Exhibit 47).
•
Children and adults age 19 to 64 whose primary coverage is Medicaid or CHIP are as likely to
report not having diculty reaching their usual medical provider by phone during business hours
as those covered by private insurance but are more likely to report having a dicult time reaching
their usual medical provider after hours for urgent medical needs compared to those with private
insurance (Exhibits 43 and 48).
•
Measures of use of care for specic types of services should be interpreted with caution due to
the limitations of survey data and the characteristics of the populations examined. For example,
the results shown are unadjusted for dierences in age, health, income, race and ethnicity, and
family and household characteristics, which are known factors in explaining some of the dierences
in access and use observed between individuals with dierent coverage sources. In addition,
this section presents data based on primary source of coverage, with multiple coverage sources
narrowed down to a single source based on a hierarchy. (For selected characteristics of individuals
without the application of this hierarchy, see Exhibit 2.)

MACStats: Medicaid and CHIP Data Book
111
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 39. Coverage, Demographic, and Health Characteristics of Non-Institutionalized Individuals Age 0–18 by Primary Source of Health
Coverage, 2022
Characteristics
Primary coverage source at time of interview
1
Total Private
2
Medicaid or
CHIP
3
Uninsured
4
Total (percent distribution across coverage sources)
5
100.0% 54.6% 36.8% 4.2%
Coverage
Length of time with any coverage during the year
Full year 94.6* 98.2 97.9 –
Part year 3.1* 1.8 2.1 35.3*
No coverage during year 2.3* – – 64.7*
Demographics
Age
0–5 29.5* 27.0* 33.5 25.1*
6 –11 31.1 31.3 30.5 31.2
12–18 39.3* 41.6* 36.0 43.7*
Gender
Male 51.1 51.8 50.6 52.0
Female 48.9 48.2 49.4 48.0
Race
Hispanic 25.6* 16.8* 36.9 43.0
White, non-Hispanic 51.0* 64.2* 32.7 41.2*
Black, non-Hispanic 12.4* 7.5* 20.5 7.0*
American Indian, non-Hispanic † † † †
Asian, non-Hispanic 4.6* 5.5* 3.4 5.0
Other single and multiple races, non-Hispanic 5.4 5.6 4.9 †
Parents present in family
0 parents 2.3* 0.6* 4.8 †
1 parent 27.9* 17.8* 43.3 28.6*
2 or more parents 69.8* 81.6* 51.9 69.9*
Family income
Has income less than 138 percent FPL 25.3* 5.4* 54.9 32.5*
Has income in ranges shown below
Less than 100 percent FPL 15.4* 2.9* 34.0 21.6*
100–199 percent FPL 22.1* 9.2* 40.4 25.1*
200–399 percent FPL 29.0* 32.9* 21.2 37.6*
400 percent FPL or higher 33.5* 55.0* 4.4
15.7*

December 2023
112
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 39. (continued)
Characteristics
Primary coverage source at time of interview
1
Total Private
2
Medicaid or
CHIP
3
Uninsured
4
Other demographic characteristics
Citizen of United States 97.1% 98.5%* 97.1% 80.2%*
Born outside U.S. 4.4 2.8* 4.6 21.9*
Number of years spent in the U.S. (among those born outside U.S.)
Less than 5 years 45.4 33.9 45.0 66.1*
5–9 years 36.4 40.1 35.9 28.8
10 years or more 18.3 25.9 19.1 †
Lives in a family that receives
SSI or SSDI 6.1* 2.5* 11.7 †
SSI 3.1* 0.9* 6.7 †
SSDI 3.7* 1.8* 6.5 †
WIC 12.8* 3.1* 28.0 9.1*
SNAP 23.3* 6.1* 51.3 10.4*
Public assistance 6.8* 1.9* 14.5 †
Any school-aged child in family received free or reduced-cost
meals at school in past 12 months
59.6* 45.9* 80.9 56.5*
Health
Current health status
Excellent or very good 86.0* 90.6* 79.5 81.1
Good 11.2* 7.9* 15.5 16.0
Fair or poor 2.8* 1.4* 5.0 †
School days lost due to illness or injury, past 12 months
None 35.2* 31.3* 39.7 48.8*
1 day 7.4 8.2 6.6 †
2–5 days 34.9* 38.2* 29.4 27.5
6–10 days 13.4 14.1 12.7 13.7
11–20 days 6.4* 6.0* 7.8 †
Over 20 days 2.8* 2.3* 3.8 †
Special needs, impairments, and health conditions
Receives special education or early intervention services
6
9.9* 8.6* 12.9 †
Uses a hearing aid 0.7 0.5 1.0 †
Uses special equipment for walking 0.7 0.4* 1.0 †

MACStats: Medicaid and CHIP Data Book
113
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 39. (continued)
Characteristics
Primary coverage source at time of interview
1
Total Private
2
Medicaid or
CHIP
3
Uninsured
4
Uses glasses 25.0% 25.3% 25.2% 21.9%
Washington Group on Disability Statistics indicator for kids 2–4
7
4.3* † 6.6 †
Washington Group on Disability Statistics indicator for kids 5–17
7
13.4* 11.8* 17.2 7.9*
Ever been told he or she has selected conditions
ADHD/ADD
8
9.7 9.3 10.7 6.3*
Asthma 10.4* 9.2* 12.7 9.0
Autism
8
3.8 3.4 4.4 †
Diabetes 0.4 0.3 † –
Intellectual disability
6
1.7 1.6 1.9 †
Other developmental delay
6
5.4* 4.5* 6.7 †
Notes: FPL is federal poverty level. SSI is Supplemental Security Income. SSDI is Social Security Disability Insurance. WIC is Supplemental Nutrition Program for
Women, Infants, and Children. SNAP is Supplemental Nutrition Assistance Program, formerly referred to as food stamps. ADHD is attention decit hyperactivity
disorder. ADD is attention decit disorder. Percentage calculations for each item in the exhibit exclude individuals with missing and unknown values. The individual
components listed under the subcategories are not always mutually exclusive and may not sum to 100 percent. Standard errors are available in the Excel version
of this exhibit at https://www.macpac.gov/publication/coverage-demographic-and-health-characteristics-of-non-institutionalized-individuals-age-0-18-by-primary-
source-of-health-coverage/. Due to dierences in methodology (such as the wording of questions, length of recall periods, and prompts or probes used to elicit
responses), estimates obtained from dierent survey data sources will vary. For example, the National Health Interview Survey (NHIS) is known to produce
higher estimates of service use than the Medical Expenditures Panel Survey (MEPS). For purposes of comparing groups of individuals (as in this exhibit), the
NHIS provides the most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be
appropriate to consult estimates from MEPS or another source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
– Dash indicates zero.
1
Total includes all non-institutionalized children under age 19, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by Medicare (generally children with end-stage renal disease), any type of military health plan, or other federal government-sponsored programs.
Coverage source is dened as of the time of the survey interview. Because an individual may have multiple coverage sources or changes over time, responses to
survey questions may reect characteristics or experiences associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.

December 2023
114
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 39. (continued)
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type
of service, such as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare (which is rare for children) or private coverage. Components do not sum to 100
percent because not all coverage sources are shown.
6
Survey information is limited to children age 0–17.
7
This measure is dierent from previous measures of disability and special health care needs among children published in prior measures of MACStats.
Washington Group on Disability Statistics questions focus on several domains of functioning that identify children who are at greater risk than the general
population of experiencing restrictions in participation because of diculties performing certain universal, basic actions. See https://www.macpac.gov/macstats/
data-sources-and-methods/ for additional information.
8
Survey information is limited to children age 2–17.
Source: MACPAC, 2023, analysis of NHIS data.

MACStats: Medicaid and CHIP Data Book
115
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 40. Use of Care among Non-Institutionalized Individuals Age 0–18 by Primary Source of Health Coverage, 2022, NHIS Data
Characteristics
Primary coverage source at time of interview
1
Total Private
2
Medicaid or CHIP
3
Uninsured
4
Total (percent distribution across coverage sources)
5
100.0% 54.6% 36.8% 4.2%
Contact with health care professionals (past 12 months)
Saw selected health professional
Saw doctor or other health care professional 93.9* 94.5 95.0 75.3*
Had eye exam 40.4 42.6* 38.6 30.5*
Received counseling/therapy from mental health
professional
6
12.5 13.1 12.7 7.3*
Dental exam/cleaning
7
82.1* 85.2* 79.6 57.5*
Had at least 1 overnight hospital stay
7
2.6* 2.1* 3.5 †
Used prescription medication 35.9 35.8 37.4 23.8*
Had a medical appointment by video or phone 16.5 18.2* 15.0 10.3*
Receipt of appropriate care (past 12 months)
Interval since last wellness visit
8
Within the past year 92.5 92.7 93.6 78.5*
More than 1 year ago but less than 2 years 5.6 5.7 4.9 11.4*
More than 2 years ago 1.8 1.6 1.4 9.2*
Never † † † †
Number of emergency room visits
None 83.7* 88.0* 77.2 88.3*
At least 1 16.3* 12.0* 22.8 11.7*
1 11.0* 8.9* 14.3 8.3*
2–3 4.3* 2.6* 6.7 †
4 or more 0.9* 0.5* 1.7 †
Number of urgent care visits
None 70.9 68.5* 73.1 81.5*
At least 1 29.1 31.5* 26.9 18.5*
1 16.1* 18.2* 13.9 10.8
2–3 10.3 10.8 9.9 †
4 or more 2.7 2.5 3.2 †

December 2023
116
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 40. (continued)
Notes: NHIS is National Health Interview Survey. Percentage calculations for each item in the exhibit exclude individuals with missing and unknown values. The
individual components listed under the subcategories are not always mutually exclusive and may not sum to 100 percent. Standard errors are available in the
Excel version of this exhibit at https://www.macpac.gov/publication/use-of-care-among-non-institutionalized-individuals-age-0-18-by-primary-source-of-health-
coverage-data-from-national-health-interview-survey/. Due to dierences in methodology (such as the wording of questions, length of recall periods, and prompts
or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example, the NHIS is known to produce higher estimates
of service use than the Medical Expenditures Panel Survey (MEPS). For purposes of comparing groups of individuals (as in this exhibit), the NHIS provides the
most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be appropriate to consult
estimates from MEPS or another source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
1
Total includes all non-institutionalized children under age 19, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by Medicare (generally children with end-stage renal disease), any type of military health plan, or other federal government-sponsored programs.
Coverage source is dened as of the time of the survey interview. Because an individual may have multiple coverage sources or changes over time, responses to
survey questions may reect characteristics or experiences associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare (which is rare for children) or private coverage. Components do not sum to 100 percent
because not all coverage sources are shown.
6
Survey information is limited to children age two or older.
7
Survey information is limited to children age one or older.
8
Prior versions of MACStats reported whether an individual received a well-child visit in the past year. This version of MACStats reports the time that has elapsed
since the individual’s last well-child visit.
Source: MACPAC, 2023, analysis of NHIS data.

MACStats: Medicaid and CHIP Data Book
117
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 41. Use of Care among Non-Institutionalized Individuals Age 0–18 by Primary Source of Health Coverage, 2021, MEPS Data
Characteristics
Primary coverage source at time of most recent interview
1
Total Private
2
Medicaid or
CHIP
3
Uninsured
4
Total (percent distribution across coverage sources)
5
100.0% 56.2% 36.7% 5.1%
Child has special health care needs 14.1 13.3 15.8 9.8*
Contact with health care professionals (past 12 months)
Number of oce-based visits to a doctor or other health professional, excluding dental visits and inpatient hospital stays
None 27.3* 20.3* 35.1 44.4
At least 1 72.7* 79.7* 64.9 55.6
1 21.4* 20.1* 24.0 17.7*
2–3 23.4 25.2* 21.3 19.5
4 or more 27.9* 34.4* 19.6 18.3
Had at least 1 dental care visit
6
50.6* 58.7* 41.8 24.7*
Received care at home 1.3* 0.8* 2.1 †
Receipt of appropriate care (past 12 months)
Had more than 15 oce-based or hospital outpatient visits 5.4 6.1 4.6 †
Annual total number of days received visits from paid/unpaid home health care providers
None 98.7 99.2* 97.9 97.8
1 † † † †
2–30 0.9 † 1.4 †
31–90 † † † †
91–200 † † † †
More than 200 † † † †
Number of emergency room visits
None 91.4* 93.6* 88.1 93.3*
At least 1 8.6* 6.4* 11.9 6.7*
1 7.2* 5.6* 9.5 †
2–3 1.4* 0.7* 2.3 †
4 or more † † † †
Had at least 1 overnight hospital stay 1.4 1.0* 2.0 †

December 2023
118
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
Characteristics
Primary coverage source at time of most recent interview
1
Total Private
2
Medicaid or
CHIP
3
Uninsured
4
Count of all prescribed medications purchased during the year, including initial purchases and rells
None 69.1% 68.2% 68.4% 81.0%*
1 10.9 11.8 10.3 †
2 5.5 5.9 5.2 †
3–5 6.6 6.8 6.5 †
6–2 4.5 4.5 5.2 †
13–24 2.1 1.6* 2.7 †
More than 24 1.3 1.1 1.6 †
Notes: MEPS is the Medical Expenditure Panel Survey. Percentage calculations for each item in the exhibit exclude individuals with missing and unknown values.
Standard errors are available in the Excel version of this exhibit at https://www.macpac.gov/publication/use-of-care-among-non-institutionalized-individuals-age-0-18-
by-primary-source-of-health-coverage-data-from-medical-expenditures-panel-survey/. Due to dierences in methodology (such as the wording of questions, length
of recall periods, and prompts or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example, the National Health
Interview Survey (NHIS) is known to produce higher estimates of service use than the MEPS. For purposes of comparing groups of individuals, the NHIS provides
the most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be appropriate to consult
estimates from MEPS or another source.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
1
Total includes all non-institutionalized children under age 19, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals with
multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those covered
by Medicare (generally children with end-stage renal disease), any type of military health plan, or other federal government-sponsored programs. Coverage source
is dened as of the time of the most recent survey interview. Because an individual may have multiple coverage sources or changes over time, responses to survey
questions may reect characteristics or experiences associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health plan,
or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or only a private plan that paid for one type of service, such
as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare (which is rare for children) or private coverage. Components do not sum to 100 percent
because not all coverage sources are shown.
6
This measure should not be compared to other dental measures included in databooks before 2019. Dental visit is dened as a visit to any person for dental care,
including general dentists, dental hygienists, dental technicians, dental surgeons, orthodontists, endodontists, and periodontists. Additional dental variables included in
previous years (general dentist, orthodontist, dental check-up) are no longer available.
Source: MACPAC, 2023, analysis of MEPS data.
EXHIBIT 41. (continued)

MACStats: Medicaid and CHIP Data Book
119
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 42. Measures of Access to Care among Non-Institutionalized Individuals Age 0–18 by Primary Source of Health Coverage, 2022,
NHIS Data
Characteristics
Primary coverage source at time of interview
1
Total Private
2
Medicaid or CHIP
3
Uninsured
4
Total (percent distribution across coverage sources)
5
100.0% 54.6% 36.8% 4.2%
Connection to the health care system (past 12 months)
Has a usual source of care
6
96.8 98.3* 96.5 78.6*
Kind of usual place for medical care
Doctor's oce or health center 95.8 96.5 95.7 87.9*
Urgent care/ walk-in clinic 3.7 3.3 3.7 8.1*
Other 0.5 † † †
Timeliness of care (past 12 months)
Delayed medical care because of costs 1.2 0.7 0.9 10.6*
Delayed getting dental care 4.4 3.0 3.7 26.6*
Delayed lling prescription to save money 1.7 1.9 † †
Unmet need for selected types of care due to cost
Medical care 0.9 0.4 0.7 8.5*
Mental health care or counseling
7
1.0 0.9 0.6 †
Dental care
8
3.1 1.9* 3.2 17.0*
Prescription drugs 0.9 0.9 0.8 †
Problems paying or unable to pay medical bills, past 12 months 11.9* 9.1* 15.4 16.9
Notes: NHIS is National Health Interview Survey. Percentage calculations for each item in the table exclude individuals with missing and unknown values. The
individual components listed under the subcategories are not always mutually exclusive and may not sum to 100 percent. Standard errors are available in the
Excel version of this exhibit at https://www.macpac.gov/publication/measures-of-access-to-care-for-non-institutionalized-children-by-source-of-health-coverage/.
Due to dierences in methodology (such as the wording of questions, length of recall periods, and prompts or probes used to elicit responses), estimates obtained
from dierent survey data sources will vary. For example, the NHIS is known to produce higher estimates of service use than the Medical Expenditure Panel
Survey (MEPS). For purposes of comparing groups of individuals (as in this exhibit), the NHIS provides the most recent information available. For other purposes,
such as measuring levels of use relative to a particular benchmark or goal, it may be appropriate to consult estimates from MEPS or another source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.

December 2023
120
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 42. (continued)
1
Total includes all non-institutionalized children under age 19, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by Medicare (generally children with end-stage renal disease), any type of military health plan, or other federal government-sponsored programs.
Coverage source is dened as of the time of the survey interview. Because an individual may have multiple coverage sources or changes over time, responses to
survey questions may reect characteristics or experiences associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare (which is rare for children) or private coverage. Components do not sum to 100 percent
because not all coverage sources are shown.
6
Excludes emergency room.
7
Survey information is limited to children age two or older.
8
Survey information is limited to children age one or older.
Source: MACPAC, 2023, analysis of NHIS data.

MACStats: Medicaid and CHIP Data Book
121
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 43. Access to and Experience of Care among Non-Institutionalized Individuals Age 0–18 by Primary Source of Health Coverage, 2021,
MEPS Data
Characteristics
Primary coverage source at time of most recent interview
1
Total Private
2
Medicaid or
CHIP
3
Uninsured
4
Total (percent distribution across coverage sources)
5
100.0% 56.2% 36.7% 5.1%
Access to Care
Has usual place for medical care 86.1 88.3 86.3 63.8*
Travel time to usual source of care
Less than 15 minutes 63.4 63.2 63.4 62.2
15–30 minutes 28.6 29.2 27.8 30.9
31–60 minutes 7.2 6.8 7.8 †
More than an hour 0.9 † † †
Diculty reaching usual medical provider by phone during business hours
Very dicult 2.9 2.4 3.6 †
Somewhat dicult 12.0 9.5* 14.6 †
Not too dicult 27.7 30.0* 24.6 22.5
Not at all dicult 57.5 58.0 57.2 50.9
Diculty reaching usual medical provider after hours for urgent medical needs
Very dicult 16.6* 11.6* 22.4 37.0
Somewhat dicult 18.2 18.6 18.7 †
Not too dicult 29.8* 33.8* 23.5 29.2
Not at all dicult 35.3 36.1 35.5 25.8
Usual medical provider has night or weekend availability 47.6 51.1* 44.0 36.2
Usual medical provider speaks preferred language or provides
translator, among those with limited English abilities in family
88.8 100.0 83.7 100.0
Usual medical provider asks person to help decide between choice of treatments
Never 5.5* 3.2* 9.0 †
Sometimes 10.6 9.0* 12.5 †
Usually 16.5 18.0 14.4 11.4
Always 67.3 69.8* 64.1 69.0
Usual medical provider presents and explains all options 97.7 98.2 96.7 99.4*
December 2023
122
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 43. (continued)
Notes: MEPS is the Medical Expenditure Panel Survey. Access to care variables are elded for only a subset of MEPS respondents (to be eligible to receive the
access to care section questions, individuals had to be current, non-institutionalized members of the responding unit in round two for panel members in relative
year one and round four for panel members in relative year two). Percentage calculations for each item in the exhibit exclude individuals with missing and unknown
values. Standard errors are available in the Excel version of this exhibit at https://www.macpac.gov/publication/exhibit-43-access-to-and-experience-of-care-
among-non-institutionalized-individuals-age-0-18-by-primary-source-of-health-coverage-meps-data/. Due to dierences in methodology (such as the wording of
questions, length of recall periods, and prompts or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example,
the National Health Interview Survey (NHIS) is known to produce higher estimates of service use than the MEPS. For purposes of comparing groups of individuals,
the NHIS provides the most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be
appropriate to consult estimates from MEPS or another source.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
¹ Total includes all non-institutionalized individuals age 0–18, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by any type of military health plan or other federal government-sponsored programs. Coverage source is dened as of the time of the most recent
survey interview. Because an individual may have multiple coverage sources or changes over time, responses to survey questions may reect characteristics or
experiences associated with a coverage source other than the one assigned in this exhibit.
² Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
³ Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
⁴ Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
⁵ Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare (which is rare for children) or private coverage. Components do not sum to 100 percent
because not all coverage sources are shown.
Source: MACPAC, 2023, analysis of MEPS data.

MACStats: Medicaid and CHIP Data Book
123
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
MACStats
EXHIBIT 44. Coverage, Demographic, and Health Characteristics of Non-Institutionalized Individuals Age 19–64 by Primary Source of Health
Coverage, 2022
Characteristic
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Total (percent distribution across coverage
sources)
5
100.0% 4.2% 66.8% 13.1% 12.6%
Coverage
Length of time with any coverage during year
Full year 84.2* 97.9* 95.5* 93.5 –
Part year 7.1 2.1* 4.5* 6.5 25.8*
No coverage during year 8.7* – – – 74.2*
Demographics
Age
19–25 14.8* 3.9* 13.7* 21.4 17.1*
26–44 42.8* 16.7* 41.9* 47.6 52.1*
45–54 20.7* 21.6* 22.4* 14.5 17.8*
55–64 21.7* 57.8* 22.1* 16.6 13.0*
Gender
Male 49.5* 50.0* 50.3* 37.1 57.3*
Female 50.5* 50.0* 49.7* 62.9 42.7*
Sexual orientation
Heterosexual 94.5* 94.7 94.6* 92.7 95.8*
Lesbian/gay 2.3 2.3 2.6 2.4 1.2*
Bisexual 3.2* 2.9* 2.8* 4.9 3.0*
Race
Hispanic 19.4* 12.1* 14.4* 24.4 44.0*
White, non-Hispanic 58.6* 64.2* 65.4* 43.4 35.4*
Black, non-Hispanic 12.6* 16.7 10.4* 20.1 13.6*
American Indian, non-Hispanic 0.8 † 0.4 † 1.4
Asian, non-Hispanic 6.4 3.9* 7.2 6.6 3.5*
Other single and multiple races, non-Hispanic 2.3 2.3 2.1* 3.1
2.0

December 2023
124
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
Characteristic
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Marital status
Married 51.2%* 41.4%* 58.5%* 28.4% 37.7%*
Widowed 1.7* 6.1* 1.2* 2.5 1.7*
Divorced or separated 9.0* 19.0* 7.6* 12.3 9.1*
Living with partner 10.9* 7.0* 9.3* 14.6 18.3*
Never married 27.3* 26.6* 23.5* 42.3 33.2*
Family income
Less than 138 percent FPL 17.0* 40.5* 5.9* 51.7 33.3*
Has income in ranges below
Less than 100 percent FPL 10.1* 24.4* 3.1* 32.9 19.5*
100–199 percent FPL 16.9* 33.5 9.2* 37.2 31.2*
200–399 percent FPL 28.3* 25.3 28.3* 22.7 33.6*
400 percent FPL or higher 44.7* 16.8* 59.4* 7.2 15.7*
Education
Less than high school 9.5* 19.4 4.1* 20.1 25.1*
High school diploma/GED 26.4* 39.6 21.3* 37.7 38.3
Some college 29.9 28.1 30.1 31.9 24.7*
College or graduate degree 34.2* 12.9 44.5* 10.3 11.9
Other demographic characteristics
Citizen of United States 90.4 95.9* 94.1* 89.5 67.7*
Born outside U.S. 19.8 13.1* 16.7* 21.3 40.0*
Number of years spent in the U.S. (among those born
outside U.S.)
Less than 5 years 8.9 † 7.0* 11.4 13.4
5–9 years 15.0 † 13.0 16.4 19.9
10 years or more 76.1 95.2* 80.1* 72.2 66.7
EXHIBIT 44.
(continued)

MACStats: Medicaid and CHIP Data Book
125
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
Characteristic
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Parent of a dependent child 34.0%* 12.4%* 33.3%* 42.7% 36.1%*
Currently working 76.9* 16.4* 86.5* 53.7 72.3*
Working full time (usually works 35 hours or more
per week)
87.9* 91.4* 89.9* 80.7 84.8*
Working part time (less than 35 hours per week) 11.9* 8.4* 10.0* 19.1 14.7*
Veteran 5.2* 6.9* 4.1* 1.8 2.9*
Lives in a family that receives
SSI or SSDI 8.8* 70.9* 3.6* 20.1 5.2*
SSI 3.8* 23.7* 1.6* 11.2 2.5*
SSDI 6.0* 59.8* 2.4* 11.0 3.1*
WIC 6.5* 8.1* 3.0* 19.2 11.6*
SNAP 14.1* 35.2* 5.1* 52.0 18.1*
Public assistance 4.0* 10.2* 1.6* 14.5 4.4*
Any school-aged child in family received free or
reduced-cost meals at school in past 12 months
56.7* 72.6 46.5* 82.0 71.5*
Health
Current health status
Excellent or very good 59.3* 17.8* 65.9* 42.7 56.2*
Good 28.6* 29.6* 26.9* 34.1 30.5*
Fair or poor 12.1* 52.7* 7.2* 23.2 13.3*
BMI
Healthy weight (BMI less than 25) 32.4 23.5* 33.5 32.4 29.8
Overweight (BMI 25–29) 33.2* 30.9 33.8* 29.4 35.0*
Obese (BMI 30 or higher) 34.4* 45.6* 32.8* 38.1 35.2
Smoking status
Current smoker 12.7* 25.0 9.0* 21.7 19.7
Former smoker 19.1* 25.8* 19.7*
16.5 15.7
EXHIBIT 44. (continued)

December 2023
126
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 44. (continued)
Characteristic
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Never smoked 68.2%* 49.2%* 71.4%* 61.7% 64.6%
Current e-cigarette user 7.4* 4.6* 6.6* 11.3 8.7*
Former e-cigarette user 16.4* 18.3 15.5* 19.4 16.6*
Never used e-cigarettes 76.1* 77.2* 77.8* 69.3 74.7*
Limitations and health conditions
Has basic action diculty or complex activity limitation
Any basic action diculty
6
10.6* 50.2* 6.3* 21.9 8.4*
Any complex activity limitation
7
17.7* 82.0* 10.9* 33.3 14.0*
Either one 20.7* 82.8* 13.6* 38.4 17.1*
Washington Group on Disability Statistics indicator for
adults 18 and older
8
6.6* 38.7* 3.4* 14.3 4.6*
Has diculty walking 100 yards without equipment 3.1* 26.3* 1.0* 8.0 1.6*
Has mobility or hearing problem that requires special
equipment
4.4* 29.7* 2.6* 7.1 2.3*
Unable to work now due to health problem 6.7* 63.1* 1.5* 17.9 3.5*
Limited in amount or kind of work due to health 16.1* 75.0* 10.1* 29.4 12.4*
Needs assistance with dressing and bathing 0.7* 5.5* 0.2* 1.9 †
Work loss days due to illness or injury in past 12 months
0 days 50.8 55.2 48.9 51.7 60.6*
1 day 6.2 † 6.6 5.1 4.3
2–5 days 24.3 19.3 25.8* 21.9 18.0*
6–10 days 9.1 † 9.5 8.6 7.7
11–20 days 5.1 † 4.9 5.8 5.1
More than 20 days 4.6* 12.4 4.2* 6.9 4.3*
Health conditions
Currently pregnant
9
2.7 – 2.7 3.6 †

MACStats: Medicaid and CHIP Data Book
127
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 44. (continued)
Characteristic
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Ever been told he or she has selected conditions
Hypertension 23.9* 55.3* 22.5* 26.8 17.1*
Coronary heart disease 2.1* 10.1* 1.6* 2.8 1.2*
Heart attack 1.5%* 8.5%* 1.0%* 2.2% 0.8%*
Stroke 1.4* 8.8* 0.7* 3.4 1.2*
Cancer 5.1* 12.2* 5.4* 3.6 1.8*
Diabetes 6.7* 24.8* 5.7* 8.9 4.1*
Arthritis 14.4* 47.0* 12.7* 17.8 7.0*
Asthma 15.2* 22.6 14.4* 20.9 11.6*
Chronic bronchitis, COPD, or emphysema 3.1* 17.2* 1.8* 6.7 1.8*
Dementia 0.2* † † † †
High cholesterol 20.2* 46.7* 20.2 18.4 12.5*
Anxiety disorder 19.3* 40.4* 17.1* 28.7 11.4*
Depression 18.8* 45.3* 16.0* 29.5 11.8*
Notes: FPL is federal poverty level. GED is general educational development test. SSI is Supplemental Security Income. SSDI is Social Security Disability
Insurance. WIC is Supplemental Nutrition Program for Women, Infants, and Children. SNAP is Supplemental Nutrition Assistance Program, formerly referred
to as food stamps. BMI is body mass index. COPD is chronic obstructive pulmonary disease. Percentage calculations for each item in the exhibit exclude
individuals with missing and unknown values. The individual components listed under the subcategories are not always mutually exclusive and may not add to
100 percent. Standard errors are available in the Excel version of this exhibit at https://www.macpac.gov/publication/exhibit-44-coverage-demographic-and-health-
characteristics-of-non-institutionalized-individuals-age-19-64-by-primary-source-of-health-coverage/. Due to dierences in methodology (such as the wording of
questions, length of recall periods, and prompts or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example,
the National Health Interview Survey (NHIS) is known to produce higher estimates of service use than the Medical Expenditures Panel Survey (MEPS). For
purposes of comparing groups of individuals (as in this exhibit), the NHIS provides the most recent information available. For other purposes, such as measuring
levels of use relative to a particular benchmark or goal, it may be appropriate to consult estimates from MEPS or another source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
– Dash indicates zero.

December 2023
128
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 44. (continued)
1
Total includes all non-institutionalized individuals age 19–64, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by any type of military health plan or other federal government-sponsored programs. Coverage source is dened as of the time of the survey interview.
Because an individual may have multiple coverage sources or changes over time, responses to survey questions may reect characteristics or experiences
associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare or private coverage. Components do not sum to 100 percent because not all coverage
sources are shown.
6
Captures limitations or diculties in movement (walking, reaching overhead, and using the hands and ngers) and limitations or diculties in sensory (seeing
or hearing), emotional (serious psychological distress), and cognitive diculties. Because composite measures of mental health are available on a rotating basis
starting in 2019, this measure may not be directly comparable to prior MACStats exhibits.
7
Reects a limitation in the tasks and organized activities that, when executed, make up numerous social roles, such as working, attending school, or maintaining
a household. Adults are dened as having a complex activity limitation if they have one or more of the following types of limitations: self-care limitation, social
limitation, or work limitation. Due to availability of elds in 2019 following redesign, this denition no longer includes "diculty relaxing at home without special
equipment" or "help with routine needs."
8
Washington Group on Disability Statistics questions focus on several domains of functioning that identify individuals who are at greater risk than the general
population of experiencing restrictions in participation because of diculties performing certain universal, basic actions, which include trouble with vision,
trouble with hearing, diculty walking or climbing steps, diculty communicating in usual language, diculty washing or dressing, or diculty remembering or
concentrating.
9
Information is limited to women age 19–44.
Source: MACPAC, 2023, analysis of NHIS data.

MACStats: Medicaid and CHIP Data Book
129
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 45. Use of Care among Non-Institutionalized Individuals Age 19–64 by Primary Source of Health Coverage, 2022, NHIS Data
Characteristics
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or CHIP
3
Uninsured
4
Total (percent distribution across
coverage sources)
5
100.0% 4.2% 66.8% 13.1% 12.6%
Contact with health care professionals (past 12 months)
Saw selected health professionals in past year
Saw doctor or other health care professional
6
79.8* 92.0* 83.1 83.0 52.4*
Received counseling/therapy from mental health
professional
14.5* 27.4* 13.6* 20.1 6.6*
Now sees a counselor, psychiatrist,
psychologist, or social worker regularly
(among those who have received counseling)
63.9 76.7 61.4* 68.6 51.4*
Had at least 1 overnight hospital stay 7.0* 17.6* 5.3* 13.8 4.3*
Received care at home 1.8* 11.9* 1.2* 3.1 †
Used prescription medication 61.8* 89.8* 64.4 64.7 34.4*
Had a medical appointment by video or phone 30.1* 46.2* 31.6 33.7 11.2*
Dental exam 62.7* 49.1 70.8* 49.2 36.7*
Eye exam 45.7* 50.6* 50.4* 39.3 24.2*
Receipt of appropriate care (past 12 months)
Had u shot
All individuals 40.7* 51.9* 45.5* 33.7 17.5*
Individuals age 50–64 50.3* 56.5* 53.4* 44.8 22.9*
Interval since last wellness visit
Within the past year 73.5* 88.2* 76.5 78.1 45.2*
More than 1 year ago but less than 2 years 11.9 4.5* 11.7 10.6 17.5*
2–5 years 9.5* 4.1* 8.4 7.8 19.4*
5–10 years 2.5 † 1.7 1.9 7.9*
More than 10 years ago 2.2* † 1.5 1.4 7.9*
Never 0.5 † 0.3 † 2.0*

December 2023
130
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
Characteristics
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or CHIP
3
Uninsured
4
Number of emergency room visits
None 81.1%* 66.0% 85.1%* 66.4% 81.8%*
At least 1 18.9* 34.0 14.9* 33.6 18.2*
1 12.2* 19.6 10.5* 18.5 11.7*
2–3 5.2* 9.3 3.7* 11.1 5.3*
4 or more 1.4* 5.1 0.7* 4.0 1.2*
Number of urgent care visits
None 65.8 70.8* 63.2 64.6 78.1*
At least 1 34.2 29.2* 36.8 35.4 21.9*
1 18.1* 12.4 20.1* 14.8 12.5
2–3 12.4* 11.3* 12.9* 15.7 7.7*
4 or more 3.7* 5.4 3.8 4.8 1.8*
Notes: NHIS is the National Health Interview Survey. Percentage calculations for each item in the exhibit exclude individuals with missing and unknown values.
The individual components listed under the subcategories are not always mutually exclusive and may not sum to 100 percent. Standard errors are available in the
Excel version of this exhibit at https://www.macpac.gov/publication/use-of-care-among-non-institutionalized-individuals-age-19-64-by-primary-source-of-health-
coverage-data-from-national-health-interview-survey/. Due to dierences in methodology (such as the wording of questions, length of recall periods, and prompts
or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example, the NHIS is known to produce higher estimates
of service use than the Medical Expenditure Panel Survey (MEPS). For purposes of comparing groups of individuals (as in this exhibit), the NHIS provides the
most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be appropriate to consult
estimates from MEPS or another source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
1
Total includes all non-institutionalized individuals age 19–64, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by any type of military health plan or other federal government-sponsored programs. Coverage source is dened as of the time of the survey interview.
Since an individual may have multiple coverage sources or changes over time, responses to survey questions may reect characteristics or experiences
associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
EXHIBIT 45. (continued)

MACStats: Medicaid and CHIP Data Book
131
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 45. (continued)
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare or private coverage. Components do not sum to 100 percent because not all coverage
sources are shown.
6
Any health professional includes general doctor, nurse practitioner, physician assistant, midwife, obstetrician-gynecologist, medical specialist, eye doctor, mental
health professional, therapist, chiropractor, or podiatrist.
Source: MACPAC, 2023, analysis of NHIS data.

December 2023
132
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
EXHIBIT 46. Use of Care among Non-Institutionalized Individuals Age 19–64 by Primary Source of Health Coverage, 2021, MEPS Data
Characteristics
Primary coverage source at time of most recent interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Total (percent distribution across coverage sources)
5
100.0% 3.8% 68.7% 12.7% 12.6%
Contact with health care professionals (past 12 months)
Number of oce-based visits to a doctor or other health professional, excluding dental visits and inpatient hospital stays
None 25.9* 11.4* 20.8* 30.0 55.6*
At least 1 74.1* 88.6* 79.2* 70.0 44.4*
1 13.5 8.7* 13.4 14.0 14.2
2–3 19.6 15.2 20.9* 17.4 14.8
4 or more 41.0 64.7* 44.9* 38.5 15.4*
Had at least 1 dental care visit
6
38.8* 31.3* 46.5* 22.6 15.9*
Received care at home 1.6* 13.6* 0.8* 3.2 †
Receipt of appropriate care
Had more than 15 oce-based or hospital outpatient visits 12.7* 29.4* 13.0 14.9 2.9*
Annual total of days received visits from paid/unpaid home health care providers
None 98.4* 86.4* 99.2* 96.8* 99.4*
1 0.3 † † † †
2–30 0.6 4.0* 0.5 0.9 †
31–90 0.2* 2.1* † † †
91–200 0.1 † † † †
More than 200 0.3* 4.8* † 0.9 †
Number of emergency room visits
None 89.0* 75.2 91.1* 79.1 92.8*
At least 1 11.0* 24.8 8.9* 20.9 7.2*
1 8.4* 17.1 7.1* 14.8 5.7*
2–3 2.2* 6.4 1.7* 4.6 1.4*
4 or more 0.4*
† 0.2* 1.4 †
Had at least 1 overnight hospital stay 4.9* 12.4 4.1* 9.5 2.3*

MACStats: Medicaid and CHIP Data Book
133
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 46. (continued)
Characteristics
Primary coverage source at time of most recent interview
1
Total Medicare Private
2
Medicaid or
CHIP
3
Uninsured
4
Count of all prescribed medications purchased during the year, including initial purchases and rells
None 44.4%* 10.2%* 43.0%* 39.2% 69.6%*
1 7.9 2.0* 8.3 8.0 7.1
2 5.3 2.5* 5.6 5.6 3.6*
3–5 10.2* 9.9 11.2* 8.6 6.8
6–12 13.4 12.7 14.8* 12.1 6.3*
13–24 9.4 18.0* 10.0 8.6 4.1*
More than 24 9.4* 44.6* 7.0* 17.9 2.5*
Notes: MEPS is the Medical Expenditure Panel Survey. Percentage calculations for each item in the exhibit exclude individuals with missing and unknown values.
Standard errors are available in the Excel version of this exhibit at https://www.macpac.gov/publication/use-of-care-among-non-institutionalized-individuals-age-
19-64-by-primary-source-of-health-coverage-data-from-medical-expenditures-panel-survey/. Due to dierences in methodology (such as the wording of questions,
length of recall periods, and prompts or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example, the
National Health Interview Survey (NHIS) is known to produce higher estimates of service use than the MEPS. For purposes of comparing groups of individuals,
the NHIS provides the most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be
appropriate to consult estimates from MEPS or another source.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
1
Total includes all non-institutionalized individuals age 19–64, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by any type of military health plan or other federal government-sponsored programs. Coverage source is dened as of the time of the most recent
survey interview. Because an individual may have multiple coverage sources or changes over time, responses to survey questions may reect characteristics or
experiences associated with a coverage source other than the one assigned in this exhibit.
2
Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
3
Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
4
Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
5
Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare or private coverage. Components do not sum to 100 percent because not all coverage
sources are shown.

December 2023
134
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
⁶ This measure should not be compared to other dental measures included in databooks before 2019. Dental visit is dened as a visit to any person for dental
care, including general dentists, dental hygienists, dental technicians, dental surgeons, orthodontists, endodontists, and periodontists. Additional dental variables
included in previous years (general dentist, orthodontist, dental check-up) are no longer available.
Source: MACPAC, 2023, analysis of MEPS data.
EXHIBIT 46. (continued)

MACStats: Medicaid and CHIP Data Book
135
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 47. Measures of Access to Care among Non-Institutionalized Individuals Age 19–64 by Primary Source of Health Coverage, 2022,
NHIS Data
Characteristics
Primary coverage source at time of interview
1
Total Medicare Private
2
Medicaid or CHIP
3
Uninsured
4
Total (percent distribution across
coverage sources)
5
100.0% 4.2% 66.8% 13.1% 12.6%
Connection to the health care system (past 12 months)
Has a usual source of care
6
85.1 93.0* 89.2* 86.5 56.9*
Kind of usual place for medical care
Doctor's oce or health center 87.8 93.5* 89.8 88.3 77.5*
Urgent care/ walk-in clinic 9.9 3.7* 9.3 11.0 19.1*
Veterans Aairs facility 1.5* 2.5* 0.4 † †
Other 0.8 † 0.6 † 3.1*
Timeliness of care (past 12 months)
Delayed because of costs 8.4 9.9* 5.7* 7.3 25.0*
Delayed getting dental care 20.8* 29.5 14.5* 26.9 45.8*
Delayed lling prescription to save money 6.6 9.9 5.2* 7.7 17.4*
Unmet need for selected types of care due to cost
Medical care 7.5 9.6 4.8* 7.8 22.1*
Mental health care or counseling 6.2 6.8 5.4* 7.1 9.5*
Dental care 16.8* 28.1 11.2* 25.3 35.1*
Prescription drugs 5.9 12.8* 4.5* 6.9 10.9*
Problems paying or unable to pay medical
bills, past 12 months
11.6 23.1* 9.5* 12.1 19.4*
Other barriers to care in the past 12 months
Lack of transportation kept you from medical
appointments, meetings, work, other needs
for daily living
6.1* 13.0 3.8* 14.5 7.8*
Notes: NHIS is National Health Interview Survey. Percentage calculations for each item in the table exclude individuals with missing and unknown values. The
individual components listed under the subcategories are not mutually exclusive and may not sum to 100 percent. Standard errors are available in the Excel
version of this exhibit at https://www.macpac.gov/publication/measures-of-access-to-care-for-non-institutionalized-individuals-age-19-64-by-source-of-health-
coverage/. Due to dierences in methodology (such as the wording of questions, length of recall periods, and prompts or probes used to elicit responses),
estimates obtained from dierent survey data sources will vary. For example, the NHIS is known to produce higher estimates of service use than the Medical

December 2023
136
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
Expenditure Panel Survey (MEPS). For purposes of comparing groups of individuals (as in this exhibit), the NHIS provides the most recent information available.
For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be appropriate to consult estimates from MEPS or another
source.
The NHIS underwent a substantial redesign in 2019, and users should be cautious about making any comparisons to prior years. More information about the
redesign is available at https://www.cdc.gov/nchs/nhis/2019_quest_redesign.htm/.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
¹ Total includes all non-institutionalized individuals age 19–64, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by any type of military health plan or other federal government-sponsored programs. Coverage source is dened as of the time of the survey interview.
Because an individual may have multiple coverage sources or changes over time, responses to survey questions may reect characteristics or experiences
associated with a coverage source other than the one assigned in this exhibit.
² Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
³ Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
⁴ Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
⁵ Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare or private coverage. Components do not sum to 100 percent because not all coverage
sources are shown.
⁶ Excludes emergency room.
Source: MACPAC, 2023, analysis of NHIS data.
EXHIBIT 47. (continued)

MACStats: Medicaid and CHIP Data Book
137
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
EXHIBIT 48. Access to and Experience of Care among Non-Institutionalized Individuals Age 19–64 by Primary Source of Health Coverage, 2021,
MEPS Data
Characteristics
Primary coverage source at time of most recent interview
1
Total Medicare Private
2
Medicaid or CHIP
3
Uninsured
4
Total (percent distribution across
coverage sources)
5
100.0% 3.8% 68.7% 12.7% 12.6%
Access to Care
Has usual place for medical care 66.4 86.0* 69.7 68.4 37.6*
Travel time to usual source of care
Less than 15 minutes 58.4 53.3 59.1 58.4 59.6
15–30 minutes 32.7 32.6 32.8 33.0 30.3
31–60 minutes 7.4 10.7* 6.8 6.8 8.5
More than an hour 1.5 3.5 1.2 1.8 †
Diculty reaching usual medical provider by phone during business hours
Very dicult 4.6 6.4 4.1 5.6 6.3
Somewhat dicult 13.6 12.2 12.9 16.3 14.9
Not too dicult 31.5 29.7 31.8 31.3 32.6
Not at all dicult 50.3 51.7 51.2 46.7 46.2
Diculty reaching usual medical provider after hours for urgent medical needs
Very dicult 24.8* 24.7* 22.3* 32.2 32.4
Somewhat dicult 20.6 15.1* 21.0 21.6 20.7
Not too dicult 25.4* 22.8 26.7* 21.1 23.7
Not at all dicult 29.2 37.4* 30.0* 25.1 23.3
Usual medical provider has night or weekend
availability
32.3 24.1* 33.8 30.7 29.9
Usual medical provider speaks preferred
language or provides translator, among those
with limited English abilities in family
93.2 99.2* 93.4 89.4 95.6

December 2023
138
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 5
Characteristics
Primary coverage source at time of most recent interview
1
Total Medicare Private
2
Medicaid or CHIP
3
Uninsured
4
Usual medical provider asks person to help decide between choice of treatments
Never 7.4%* 13.0% 5.8%* 12.6% 9.3%
Sometimes 13.7* 15.7 12.0* 19.0 21.3
Usually 21.9* 22.8 22.7* 17.6 19.2
Always 57.1* 48.5 59.4* 50.7 50.2
Usual medical provider presents and explains
all options
96.5* 94.4 97.0* 94.0 97.2*
Experience with care
How often providers give easy-to-understand information
Always 69.6* 57.1 71.9* 62.2 66.9
Most of the time or usually 25.4 35.7* 24.7 27.0 22.3
Some of the time or sometimes 4.1* 6.8 3.0* 8.7 6.5
None of the time or never 0.9 † 0.5* † †
Doctor gave instructions, past 12 months 71.2 82.8* 71.1 69.7 61.8*
Notes: MEPS is the Medical Expenditure Panel Survey. Access to care variables are elded for only a subset of MEPS respondents (to be eligible to receive the
access to care section questions, individuals had to be current, non-institutionalized members of the responding unit in round two for panel members in relative
year one and round four for panel members in relative year two). Percentage calculations for each item in the exhibit exclude individuals with missing and unknown
values. Standard errors are available in the Excel version of this exhibit at https://www.macpac.gov/publication/exhibit-48-access-to-and-experience-of-care-
among-non-institutionalized-individuals-age-19-64-by-primary-source-of-health-coverage-meps-data/. Due to dierences in methodology (such as the wording of
questions, length of recall periods, and prompts or probes used to elicit responses), estimates obtained from dierent survey data sources will vary. For example,
the National Health Interview Survey (NHIS) is known to produce higher estimates of service use than the MEPS. For purposes of comparing groups of individuals,
the NHIS provides the most recent information available. For other purposes, such as measuring levels of use relative to a particular benchmark or goal, it may be
appropriate to consult estimates from MEPS or another source.
* Dierence from Medicaid or CHIP is statistically signicant at the 0.05 level.
† Estimate is unreliable because it has a relative standard error greater than or equal to 30 percent.
¹ Total includes all non-institutionalized individuals age 19–64, regardless of coverage source. In this exhibit, the following hierarchy was used to assign individuals
with multiple coverage sources to a primary source: Medicare, private, Medicaid or CHIP, other, or uninsured. Not separately shown are the estimates for those
covered by any type of military health plan or other federal government-sponsored programs. Coverage source is dened as of the time of the most recent
survey interview. Because an individual may have multiple coverage sources or changes over time, responses to survey questions may reect characteristics or
experiences associated with a coverage source other than the one assigned in this exhibit.
EXHIBIT 48. (continued)

MACStats: Medicaid and CHIP Data Book
139
Section 5: Beneciary Health, Service Use, and Access to Care
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 5
² Private health insurance coverage excludes plans that paid for only one type of service, such as accidents or dental care.
³ Medicaid or CHIP also includes persons covered by other state-sponsored health plans.
⁴ Individuals were dened as uninsured if they did not have any private health insurance, Medicaid, CHIP, Medicare, state- or other government-sponsored health
plan, or military plan. Individuals were also dened as uninsured if they had only Indian Health Service coverage or had only a private plan that paid for one type of
service, such as accidents or dental care.
⁵ Because a hierarchy was used in this exhibit to assign individuals with multiple coverage sources to a primary source (see note 1), the Medicaid or CHIP
percentages shown in this row exclude individuals who also have Medicare or private coverage. Components do not sum to 100 percent because not all coverage
sources are shown.
Source: MACPAC, 2023, analysis of MEPS data.
EXHIBIT 48. (continued)


SECTION 6:
Technical Guide
to MACStats


MACStats: Medicaid and CHIP Data Book
143
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
Section 6: Technical Guide to MACStats
This technical guide provides supplementary
information to help readers interpret the exhibits in this
data book as well as understand the data sources and
methods used. In addition, we explain why MACPAC’s
statistics, particularly those on enrollment and
spending, may dier from each other or from those
published elsewhere.
1
Interpreting Medicaid
and CHIP Enrollment and
Spending Numbers
Published numbers for enrollment in Medicaid and the
State Children’s Health Insurance Program (CHIP) can
vary substantially depending on the source of data,
the enrollment period examined, and the individuals
included in the data.
Data sources
Medicaid and CHIP enrollment and spending numbers
are available from data compiled by states and the
federal government in the course of administering
these programs. Program data are updated on
dierent schedules, so the latest year of available
data may dier depending on the source. MACPAC
commonly uses the following types of administrative
data, which are submitted by the states to the Centers
for Medicare & Medicaid Services (CMS):
•
Form CMS-64 data for state-level Medicaid
spending and enrollment;
•
Transformed Medicaid Statistical Information
System (T-MSIS) data for person-level detail;
•
CMS performance indicator enrollment data;
•
Medicaid managed care enrollment reports; and
•
Statistical Enrollment Data System (SEDS) data
for CHIP enrollment.
CMS began reporting two administrative data sources
on enrollment in 2014, referred to here as performance
indicator enrollment data and CMS-64 enrollment
data.
2
These sources dier in the timing of the reports
and the enrollees covered. Performance indicator
enrollment data are published monthly by CMS and
include only full-benet Medicaid and CHIP enrollees.
CMS-64 enrollment data are published quarterly and
include Medicaid enrollees with limited benets but
exclude CHIP enrollees.
Additionally, CMS-64 enrollment data include detailed
information about the new adult group made eligible
under Section 1902(a)(10)(A)(i)(VIII) of the Social
Security Act (the Act) by the Patient Protection and
Aordable Care Act (ACA, P.L. 111-148, as amended).
MACPAC uses the spending and enrollment data
submitted on the CMS-64 to produce an exhibit on
spending and enrollment from the most recent year for
all Medicaid enrollees and those adults newly eligible
for Medicaid under the ACA (Exhibit 23).
T-MSIS. Over the past several years, CMS has been
working with states to implement the updated version
of the Medicaid Statistical Information System (MSIS).
T-MSIS builds on the person-level and claims-level
data previously available under MSIS to improve
timeliness, reliability, and completeness of national
Medicaid and CHIP data. Additionally, T-MSIS is
designed to capture considerably more data and
information. It includes additional variables and
expands reporting options for many existing variables.
All states are now submitting T-MSIS data.
CMS takes each state’s raw T-MSIS data and
standardizes them into a research-ready data set
known as the T-MSIS Analytic Files (TAF). The TAF is
further rened to remove certain personally identiable
information and proprietary information on managed
care payment amounts to providers before the data
are publicly released as the TAF research identiable
le (RIF). In addition, CMS has released updated
versions of earlier TAF RIF les as states have
addressed certain data quality issues.
CMS has developed resources to help users
understand how to use the TAF data and identify
potential concerns in validity and reliability. In
conjunction with the TAF data releases, CMS
publishes an interactive, web-based Data Quality Atlas
that contains information for all years of TAF data that
have been released.
3
These resources provide insight

December 2023
144
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
on the quality and usability of the TAF and include
summary statistics on a number of priority elds (e.g.,
eligibility group, dually eligible status, type of service).
These statistics include information on le usability,
the percentage of values missing, benchmark
comparisons to other data sources (e.g., performance
indicator enrollment), and data anomalies that may
require special consideration.
One consequence of the extended transition from
MSIS to T-MSIS is that not all states transitioned at
the same time, and data for 2014 and 2015 are split
between MSIS and T-MSIS data.
4
Additionally, CMS
has been working closely with states to improve the
quality and completeness of the data.
5
These quality
improvement eorts have focused on more recent
data, and not all states have gone back to prior
periods to make these improvements and resubmit
the data. The CMS data quality resources have shown
the quality and completeness of data are better for
more recent periods.
Because of the mix of data sources for 2014 and 2015
and the improvements in data quality over time, scal
year (FY) 2018 was the rst year of T-MSIS data that
was used for MACStats. In this data book, we used
the most recently available T-MSIS data that had more
than 12 months of claims run-out.
Survey data. MACStats also uses nationally
representative surveys based on interviews of
individuals, including the National Health Interview
Survey (NHIS) and the Medical Expenditure Panel
Survey (MEPS). The NHIS was redesigned in
2019, so users should be cautious about making
comparisons to prior years. Additionally, certain
measures in previous editions of MACStats are no
longer available.
Estimates of Medicaid and CHIP enrollment from
survey data tend to be lower than estimates
generated from administrative data, in part because
survey respondents tend to underreport Medicaid and
CHIP coverage. However, survey data provide many
more details on individual and family circumstances
(e.g., health status, ease in accessing services, and
reasons for delaying care) and can therefore provide
a richer picture of the individuals enrolled in Medicaid
and CHIP.
Enrollment period examined
Characterizations of the size of the Medicaid and
CHIP populations may vary based on the enrollment
period examined. The number of individuals enrolled
at a particular point during the year will be lower
than the total number enrolled at any point during an
entire year. Point-in-time numbers are sometimes
referred to as average, full-year equivalent, or person-
year enrollment. These statistics are often used for
budget analyses (such as those by the CMS Oce
of the Actuary) and when comparing enrollment and
expenditure numbers. Per enrollee spending levels
based on full-year equivalents ensure that amounts
are not biased by individuals’ transitions in and out of
Medicaid coverage during the year.
Enrollees versus beneciaries
Depending on the source and the year in question, data
may reect dierent ways of characterizing individuals
in Medicaid. Certain terms commonly used to refer
to people with Medicaid have specic denitions in
administrative data sources provided by CMS:
6
•
Enrollees (less commonly referred to as eligibles)
are individuals who are eligible for and enrolled
in Medicaid or CHIP. Before FY 1990, CMS
did not track the number of Medicaid enrollees
but tracked only beneciaries (see below). In
some cases, CMS has estimated the number of
enrollees before 1990.
•
Beneciaries, or persons served (less commonly
referred to as recipients), are enrollees who
receive covered services or for whom Medicaid
or CHIP payments are made. Before FY 1998,
individuals were not counted as beneciaries if
managed care payments were the only Medicaid
payments made on their behalf. Beginning
in FY 1998, however, Medicaid managed
care enrollees with no fee-for-service (FFS)
spending were also counted as beneciaries,
which increased the number of individuals
reported in enrollment statistics. Generally,
the number of beneciaries will approach
the number of enrollees as more of these
individuals use Medicaid-covered services or

MACStats: Medicaid and CHIP Data Book
145
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
are enrolled in managed care.
7
(In common
usage outside of CMS statistical publications, the
term beneciaries is typically synonymous with
enrollees.)
Institutionalized and limited-benet
enrollees
Administrative Medicaid data include enrollees who
are in institutions, such as nursing facilities, as well
as individuals who receive only limited benets (e.g.,
coverage for emergency services only). Survey
data tend to exclude such individuals from counts
of coverage. In percentage terms, the dierence
between estimates from administrative data and
estimates from survey data tends to be largest among
older beneciaries, who are more likely to be living
in institutions (in which case they are excluded from
most surveys) and more likely to be receiving limited
Medicaid benets that pay only for their Medicare
premiums and cost sharing (which may not be counted
as Medicaid coverage in some surveys).
CHIP enrollees
Medicaid-expansion CHIP enrollees are children
who are entitled to the covered services of a state’s
Medicaid program but whose Medicaid coverage is
generally funded with CHIP dollars. Depending on
the data source, Medicaid enrollment and spending
gures may include both Medicaid enrollees funded
with Medicaid dollars and Medicaid-expansion CHIP
enrollees funded with CHIP dollars. For MACStats, we
generally exclude Medicaid-expansion CHIP enrollees
from Medicaid analyses, but some data sources do not
allow these children to be broken out separately.
Understanding Data
on Health and Other
Characteristics of Medicaid
and CHIP Populations
MACStats uses data from the federal NHIS and the
MEPS to describe Medicaid and CHIP enrollees
in terms of their self-reported demographic,
socioeconomic, and health characteristics as well as
their use of care. Background information on these
surveys is provided here.
NHIS and MEPS data
The NHIS is an annual face-to-face household survey
of civilian non-institutionalized persons designed to
monitor the health of the U.S. population through the
collection of information on a broad range of health
topics.
8
A subsample of households that participated
in the previous year’s NHIS undergo further interviews
for the household component of the MEPS, which
collects more detailed information on use of health
care services and expenditures.
9
Although other surveys are available, the NHIS is
the main survey data source used in MACStats
because it provides relatively timely estimates and
because its sample size is large enough to produce
reliable estimates by coverage source and to detect
meaningful dierences between them. In addition, it is
generally considered to be one of the best surveys for
health insurance coverage estimates, and it captures
detailed information on individuals’ health status.
10
However, the NHIS is known to produce higher
estimates of service use than the MEPS.
11
As a result,
MACStats includes estimates of service use from
both sources. For purposes of comparing groups of
individuals, the NHIS has the advantage of providing
the most recent information available; for other
purposes, such as measuring levels of service use
relative to a particular benchmark or goal, consulting

December 2023
146
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
estimates from the MEPS or another source might be
more appropriate.
The NHIS has some limitations. As in most surveys,
respondents in the NHIS do not always accurately
report information about participation in programs such
as Medicaid, CHIP, Medicare, Supplemental Security
Income, and Social Security Disability Insurance.
As a result, survey data may not match estimates of
program participation computed from the programs’
own administrative data. In addition, although the
NHIS asks about participation in Medicaid and CHIP
in two dierent questions, program participation
estimates from the survey are not reported separately.
One reason for this is that many states’ CHIP
and Medicaid programs use the same name, so
respondents may not necessarily know which program
funds their children’s coverage. Even when the
programs have dierent names, it may be dicult for
respondents and interviewers to correctly categorize
the coverage. As a result, separate survey questions
regarding participation in Medicaid and CHIP are
generally used to minimize the undercounting of
Medicaid and CHIP enrollees, not to produce valid
estimates separately for each program. Thus, survey
data analyses typically combine Medicaid and CHIP
into a single category.
In previous editions of MACStats, NHIS data allowed
MACPAC to use responses to several questions to
identify children and youth with special health care
needs (CYSHCN). Based on an approach developed
by the Child and Adolescent Health Measurement
Initiative, children were identied as meeting CYSHCN
criteria if they had at least one diagnosed or parent-
reported ongoing health condition and elevated
service use. Following the 2019 redesign, a number
of variables used to identify specic health conditions,
as well as some of the variables related to elevated
service use, are no longer available. As such, we are
no longer able to identify CYSHCN using the NHIS,
although the measure remains in the MEPS.
Beginning with the 2022 edition of MACStats, NHIS
data are reported using the Washington Group on
Disability Statistics measures. The measures describe
the functional status of individuals across domains of
seeing; hearing; mobility; communication; cognition;
self-care; anxiety; depression; dexterity; playing;
learning; relationships; and kicking, biting, or hitting
others. The questions ask about the level of diculty
in basic domains of functioning and, when used with
other questions on the survey, can evaluate if adults
and children with functional limitations are able to
participate in everyday activities at levels similar to
their peers without functional limitations.
12
Methodology for T-MSIS
Analysis
As noted above, MACStats uses T-MSIS data to
create exhibits on Medicaid enrollment and spending
by eligibility group. Although we used the raw T-MSIS
data instead of the TAF, our process of identifying
nal action records is similar and should produce
similar results as the TAF. We relied on the nal
action indicator CMS appends to claims as part of its
TAF development process. Additionally, claims are
organized by service date (ending date of service)
to assign a claim to a particular time period, which is
similar to the TAF.
13
Our tabulations of the raw T-MSIS
data produced similar totals to the TAF; however, there
were some dierences due to a dierence in how
many months of claims run-out were included.
Our process of assigning enrollee characteristics is
similar to prior years, relying on the most recent valid
value for a particular characteristic. T-MSIS includes a
new eligibility group variable that expands the number
of groups reported and is more specic than the basis-
of-eligibility variable reported in MSIS. As such, we
developed a new algorithm to aggregate these more
granular eligibility codes into our larger groupings of
child, adult, disabled, and aged. In addition, we further
split adults into the new adult group and other adults.
14
Furthermore, the new T-MSIS eligibility groups do not
specically separate individuals who qualify on the
basis of a disability from the aged and do not separate
children from adults in many categories. We included
age as another identier to assign enrollees to our
larger groupings. The assignment of beneciaries is
shown in Exhibit 49.
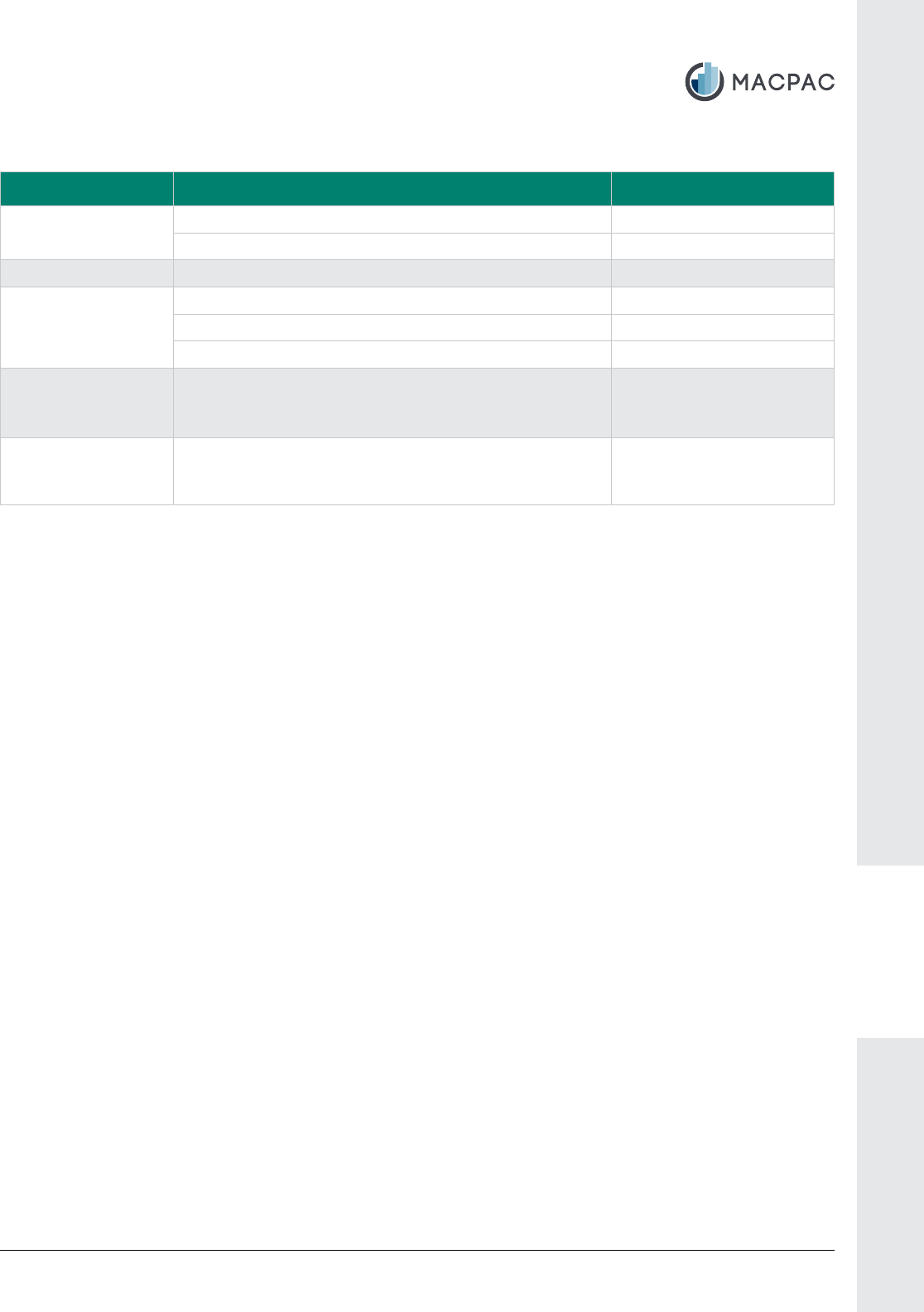
MACStats: Medicaid and CHIP Data Book
147
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
EXHIBIT 49. MACPAC Assignment of T-MSIS Eligibility Groups
MACPAC group T-MSIS eligibility code Age
Child 06, 07, 08, 28, 29, 30, 31, 54, 55 Any age
01, 02, 03, 04, 14, 27, 32, 33, 35, 36, 56, 69, 70, 71, 76 Age under 19 years
New adult group
1, 2
72, 73, 74, 75 Any age
Other adult
3
05, 09 Any age
01, 02, 03, 04, 27, 33, 35, 36, 56, 70, 76 Age 19 and older
32, 69, 71 Age 19–64
Disabled 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25,
26, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50,
51, 52, 59, 60
Age under 65 years (age
19–64 for code 14)
Aged 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25,
26, 32, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49,
50, 51, 52, 59, 60, 69, 71, 76
Age 65 and older
Note: T-MSIS is Transformed Medicaid Statistical Information System. Excludes individuals enrolled in CHIP-nanced
Medicaid coverage (e.g., Medicaid-expansion CHIP) when the CHIP code indicates separate or Medicaid-expansion CHIP
(values of 2 or 3) or the T-MSIS eligibility code is 61–68.
¹ Includes both newly eligible and not newly eligible adults who are eligible under Section 1902(a)(10)(A)(i)(VIII) of the Social
Security Act (the Act). Newly eligible adults include those who were not eligible for Medicaid under the rules that a state had
in place on December 1, 2009. Not newly eligible adults include those who would have previously been eligible for Medicaid
under the rules that a state had in place on December 1, 2009; this includes states that had already expanded to adults
with incomes greater than 100 percent of the federal poverty level as of March 23, 2010, and receive the expansion state
transitional matching rate.
² Because Idaho and Virginia appear to classify their new adult group under eligibility code 71, we assign eligibility code 71 to
the new adult group for Idaho and Virginia.
³ Includes adults under age 65 who qualify through a pathway other than disability or Section 1902(a)(10)(A)(i)(VIII) of the Act
(e.g., parents and caretakers, pregnancy).
Source: MACPAC, 2023, analysis of T-MSIS data.
We also assigned Medicaid enrollees a unique
national identication (ID) number using an algorithm
that incorporates state-specic ID numbers and
beneciary characteristics, such as date of birth and
gender. The national enrollment counts are then
unduplicated using this national ID, which results in
slightly lower enrollment counts than the sum of state-
level enrollment.
T-MSIS includes spending amounts on a claim at both
the header and line levels. To calculate spending,
we used the Medicaid paid amounts reported on
the header.
15
We included payment amounts from
FFS, capitation, service tracking, and supplemental
payment claim types that were linked to an individual
enrollee. We did not include any lump sum payments,
such as supplemental payments, that could not be
linked to a specic enrollee. Additionally, we did not
include paid amounts from encounter records because
that spending is already represented in the amount the
state made in capitation payments.
To classify claims into our broad service categories, we
primarily relied on the type-of-service variable (Exhibit
51). Because type of service is reported at the line
level, it is possible for a single claim to include multiple
types of service. To assign a single type of service to
a claim, we applied the type of service associated with
the greatest proportion of line-level spending. We did
additional checks to assess the reasonableness of the
type of service assignment. For facility-based services
(e.g., hospital, nursing facility), we checked to see if
the claim had a bill type that corresponded to a facility
service or a valid revenue code. For professional
December 2023
148
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
services, we checked for place of service. In cases in
which a nal type of service was still undetermined,
we defaulted to the claim le in which the claim was
reported. Claims in the inpatient le were assigned
to the hospital category, claims in the long-term
care le were assigned to the institutional long-term
services and supports (LTSS) category, claims in
the prescription drug le were assigned to the drug
category, and claims in the other services le were
assigned to the non-hospital acute care category.
We used additional variables to categorize managed
care and non-institutional LTSS claims. We assigned
any claim classied as a capitation payment (claim
type 2) as managed care regardless of the type of
service assigned to the claim. We classied a claim as
non-institutional LTSS if any of the following variables
so indicated: type of service, program type, or Title
XIX service category (i.e., CMS-64 service category)
(Exhibit 51).
Readers should note that due to changes in both
methods and data, T-MSIS gures shown in this year’s
data book may not be directly comparable to gures
from earlier editions that were based on MSIS data.
Key dierences between the current and previous
methodologies include the following:
•
We assigned a time period to T-MSIS claims
using the service date. This corresponds to how
CMS classies the time period in the TAF. In
our previous work with MSIS, we used the le
submission date (which generally corresponds
to a paid date) when assigning a claim to a
particular time period.
•
The new eligibility groups in T-MSIS means that
some enrollees may be classied dierently
than under MSIS, depending on how states
map individuals between the two systems. In
particular, the new T-MSIS eligibility categories do
not separate individuals who qualify on the basis
of a disability from the aged and do not separate
children from adults in many categories. We
included age as another identier to categorize
beneciaries into our larger groupings. Although
we had previously taken those age 65 and older
in the disabled category and classied them
as aged, this is the rst time we specically
incorporated age into the classication of
children and adults. Furthermore, the separate
identication of the new adult group may make
it dicult to compare adults to prior years. The
other adult category generally corresponds to
the adult category used in previous MACStats
publications based on MSIS data, but in states
that expanded coverage to adults before the
ACA, the expansion adults that would have
appeared in the adult category in prior years are
now included in the new adult group category.
•
The expanded type-of-service categories in
T-MSIS means that some spending may be
classied dierently than under MSIS, depending
on how states mapped services between the
two systems. This is particularly true for non-
institutional LTSS. Previously in MSIS, we
relied on program type, because home- and
community-based services (HCBS) was not a
separate type of service. We still use program
type, but we can now also capture claims with
an HCBS type of service or a Title XIX service
category. This expansion of the algorithm may
result in our capturing more claims as non-
institutional LTSS.
•
State practices for classifying enrollees and
services in T-MSIS may change over time as
states become more familiar with the T-MSIS
reporting structure and requirements. Future
changes in enrollment and spending, particularly
across eligibility groups or service categories,
may reect changes in reporting in addition
to changes in policy. Finally, enrollment and
spending amounts for a particular year could
change over time if states correct reporting errors
and anomalies for past years.
Methodology for Adjusting
Benet Spending Data
The Medicaid benet spending amounts presented in
this data book were calculated based on T-MSIS data
that have been adjusted to match total benet spending
reported by states in CMS-64 data.
16
Although the CMS-

MACStats: Medicaid and CHIP Data Book
149
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
64 provides a more complete accounting of spending
than T-MSIS and is preferred when examining state or
federal spending totals, it cannot be used for analysis of
benet spending by eligibility group and other enrollee
characteristics. Thus, we adjust T-MSIS amounts for
several reasons:
•
CMS-64 data provide an ocial accounting of
state spending on Medicaid for purposes of
receiving federal matching dollars; in contrast,
T-MSIS data are used primarily for statistical
purposes.
•
T-MSIS generally understates total Medicaid
benet spending because it excludes
disproportionate share hospital (DSH) payments
and additional types of supplemental payments
made to hospitals and other providers, Medicare
premium payments, and certain other amounts.
17
Although states may report DSH and other
supplemental payments through T-MSIS, most
states are not reporting these data at this time.
•
T-MSIS generally overstates net spending on
prescribed drugs because it excludes rebates
from drug manufacturers. Although T-MSIS does
allow states to report drug rebate collections,
most states are not reporting these data at this
time.
•
The extent to which spending in T-MSIS diers
from that reported on the CMS-64 varies by
state, meaning that a cross-state comparison
of unadjusted T-MSIS amounts may not reect
true dierences in benet spending. (See Exhibit
50 for unadjusted benet spending amounts in
T-MSIS as a percentage of benet spending in
the CMS-64.)
The methodology MACPAC uses for adjusting T-MSIS
benet spending data involves the following steps:
•
We aggregate the service types into broad
categories that are comparable between the two
sources. (See Exhibit 51 for additional detail on
these categories.) This is necessary because
there is not a one-to-one correspondence of
service types in T-MSIS and CMS-64 data.
Even service types with identical names may
be reported dierently in the two sources due
to dierences in the instructions given to states.
Although T-MSIS includes a new variable that
corresponds to the service categories reported
on the CMS-64, many states are not currently
submitting complete information under this
variable. The submission of complete and
accurate information for this variable would allow
us to make more direct comparisons between
T-MSIS and the CMS-64 in the future.
•
We calculate state-specic adjustment factors for
each of the service categories by dividing CMS-
64 benet spending by T-MSIS benet spending.
•
We then multiply T-MSIS dollar amounts in each
service category by the state-specic factors to
obtain adjusted T-MSIS spending. For example,
in a state with an FFS hospital factor of 1.2,
each Medicaid enrollee with hospital spending in
T-MSIS would have that spending multiplied by
1.2; doing so makes the sum of adjusted hospital
spending amounts among individual Medicaid
enrollees in T-MSIS total the aggregate hospital
spending reported by states in the CMS-64 (as
noted later, MACPAC excludes some amounts
from the CMS-64 hospital total).
18
These adjustments to T-MSIS data are meant to provide
more complete estimates of Medicaid benet spending
across states that can be analyzed by eligibility group
and other enrollee characteristics. Other organizations,
including the CMS Oce of the Actuary, KFF, and the
Urban Institute, use similar methodologies, although
these may dier in some ways—for example, by using
the proportion of spending across eligibility groups in
T-MSIS to allocate CMS-64 spending to these groups.
Even so, data anomalies in T-MSIS may create large
discrepancies between the results obtained by our
methodology and results obtained by methodologies
used by other organizations. We expect to see these
discrepancies wane as states get used to T-MSIS
reporting and the accuracy and consistency of their
T-MSIS data improves.

December 2023
150
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
EXHIBIT 50. Medicaid Benet Spending in T-MSIS and CMS-64 Data by State, FY 2021 (millions)
State
Benet spending totals included in analysis
Amounts excluded from CMS-64
benet spending totals
Unadjusted
T-MSIS CMS-64
1
T-MSIS as a
percentage
of CMS-64 DSH
Incentive and
uncompensated
care pool waivers
Total $669,408 $699,301 95.7% $16,961 $10,935
Alabama 5,440 6,257 86.9 409 –
Alaska 2,315 2,146 107.9 25 –
Arizona 16,430 17,403 94.4 124 61
Arkansas 6,544 7,162 91.4 9 –
California
2
98,822 105,889 93.3 510 3,157
Colorado 9,324 10,568 88.2 219 –
Connecticut 9,377 9,180 102.1 170 –
Delaware 2,757 2,422 113.8 – –
District of Columbia 3,325 3,254 102.2 104 –
Florida 26,384 26,723 98.7 342 1,067
Georgia 11,882 11,850 100.3 433 –
Hawaii
3
2,821 2,823 99.9 10 –
Idaho 3,017 2,876 104.9 26 –
Illinois 19,142 26,392 72.5 528 –
Indiana 15,776 15,506 101.7 139 –
Iowa 6,066 5,934 102.2 65 –
Kansas 4,127 3,934 104.9 76 81
Kentucky 13,386 14,238 94.0 266 –
Louisiana 13,055 12,489 104.5 911 –
Maine 3,127 3,398 92.0 58 –
Maryland 13,237 13,278 99.7 189 –
Massachusetts 18,426 19,038 96.8 – 1,044
Michigan 17,204 20,635 83.4 218 –
Minnesota 15,087 14,912 101.2 54 –
Mississippi 5,457 5,523 98.8 235 –
Missouri 10,105 10,607 95.3 908 –
Montana 1,944 2,183 89.1 0 –
Nebraska 2,977 3,035 98.1 30 –
Nevada 4,549 4,666 97.5 95 –
New Hampshire 2,106 2,152 97.8 242 0
New Jersey 18,042 17,990 100.3 1,148 –
New Mexico 6,569 6,844 96.0 34 12
New York 71,901 71,252 100.9 4,162 –

MACStats: Medicaid and CHIP Data Book
151
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
State
Benet spending totals included in analysis
Amounts excluded from CMS-64
benet spending totals
Unadjusted
T-MSIS CMS-64
1
T-MSIS as a
percentage
of CMS-64 DSH
Incentive and
uncompensated
care pool waivers
North Carolina $15,577 $16,436 94.8% $443 –
North Dakota
2
1,124 1,378 81.5 1 –
Ohio 27,466 26,956 101.9 688 –
Oklahoma 4,830 5,788 83.5 55 –
Oregon 8,439 11,165 75.6 86 –
Pennsylvania 26,935 36,392 74.0 996 –
Rhode Island 2,571 2,809 91.5 142 $67
South Carolina 6,624 6,726 98.5 517 –
South Dakota 1,036 1,004 103.2 1 –
Tennessee 10,611 10,671 99.4 72 417
Texas 38,850 39,271 98.9 1,801 4,854
Utah
2
3,759 3,528 106.5 30 –
Vermont 1,415 1,533 92.3 23 118
Virginia 18,796 16,008 117.4 -44 –
Washington 14,659 21,652 67.7 205 57
West Virginia 15,531 4,575 339.5 70 –
Wisconsin 9,888 10,253 96.4 138 –
Wyoming 572 598 95.5 0 –
Notes: T-MSIS is Transformed Medicaid Statistical Information System. FY is scal year. DSH is disproportionate share
hospital. Includes federal and state funds. T-MSIS and CMS-64 data reect unadjusted amounts as reported by states. Both
sources exclude spending on administration, the territories, and Medicaid-expansion CHIP enrollees; in addition, CMS-64
amounts exclude $14.7 billion in osetting collections from third-party liability, estate, and other recoveries. For greater detail
on the dierence between T-MSIS and CMS-64, please see the Methodology for Adjusting Benet Spending Data section.
DSH payments and incentive and uncompensated care pool payments made under waiver expenditure authority of Section
1115 of the Social Security Act have also been excluded from CMS-64 totals. For informational purposes, the DSH and waiver
expenditure amounts that were excluded are shown here.
– Dash indicates zero; $0 indicates an amount less than $0.5 million that rounds to zero.
¹ The total amount reported on the CMS-64 may dier slightly from the state and national totals of our adjusted T-MSIS
spending reported in other exhibits due to rounding when applying certain adjustments.
² State has a state plan amendment (SPA) that allows the state to receive the enhanced federal medical assistance
percentage (FMAP) for children enrolled in Medicaid who would have, before January 1, 2014, been enrolled in CHIP if not
for the elimination of the Medicaid asset test. These children cannot be separately identied in the T-MSIS data. Because
the state claims the spending for these children as Medicaid-expansion CHIP, we reduced child enrollment and spending in
these states based on the proportion reported in their SPAs. Correspondingly, we reduced California's T-MSIS spending by
approximately $681.9 million, North Dakota's T-MSIS spending by approximately $9.3 million, and Utah's T-MSIS spending by
approximately $33.5 million.
³ The CMS-64 total for Hawaii excludes $0.5 million in fee-for-service (FFS) drug spending because the state did not report
any FFS drug spending in T-MSIS.
Source: MACPAC, 2023, analysis of T-MSIS data as of February 2023, and CMS-64 nancial management report net
expenditure data as of June 2022.
EXHIBIT 50. (continued)

December 2023
152
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
EXHIBIT 51. Service Categories Used to Adjust FY 2021 Medicaid Benet Spending in T-MSIS to Match CMS-64
Totals
Service category T-MSIS service types
1
CMS-64 service types
Hospital
•
Inpatient hospital
•
Outpatient hospital, including
mental health other than outpatient
substance abuse treatment
•
Emergency hospital
•
Critical access hospital
•
Skilled care, exceptional care, and
non-acute care—hospital residing
•
EHR payments to provider (on
hospital claim)
•
Inpatient hospital non-DSH
•
Inpatient hospital non-DSH supplemental
payments
•
Inpatient hospital GME payments
•
Outpatient hospital non-DSH
•
Outpatient hospital non-DSH supplemental
payments
•
Emergency services for aliens
2
•
Emergency hospital services
•
Critical access hospitals
Non-hospital
acute care
•
Rural health clinic
•
Laboratory
•
Radiology
•
EPSDT
•
Family planning
•
Physician
•
Dental
•
Outpatient substance abuse treatment
•
Other practitioner
•
Home health—supplies, equipment,
and appliances
•
Private duty nursing
•
Nursing, including advanced practice,
pediatric, nurse-midwife, and nurse
practitioner
•
Respiratory care for ventilator-
dependent individuals
•
Clinic
•
Physical, occupational, speech, and
hearing therapy
•
Over-the-counter medications (not on
pharmacy claim)
•
Dentures
•
Medical equipment and prosthetics
(not on pharmacy claim)
•
Eyeglasses
•
Hearing aids
•
Diagnostic and screening services
•
Preventive services
•
Well-baby and well-child services
•
Rehabilitative services
•
Targeted case management
•
Other case management
•
Care coordination
•
Transportation
•
Enabling services
•
Sterilizations
•
Physician (including primary care physician
payment increase)
•
Physician services supplemental payments
•
Preventive services with USPSTF Grade A or
B and ACIP vaccines
•
Dental
•
Nurse-midwife
•
Nurse practitioner
•
Other practitioner
•
Other practitioner supplemental payments
•
Non-hospital clinic
•
Rural health clinic
•
Federally qualied health center
•
Laboratory and radiology
•
Sterilizations
•
Abortions
•
Hospice
•
Targeted case management
•
Statewide case management
•
Physical therapy
•
Occupational therapy
•
Services for speech, hearing, and language
•
Non-emergency transportation
•
Private duty nursing
•
Rehabilitative services (non-school based)
•
School-based services
•
EPSDT screenings
•
Diagnostic screening and preventive services
•
Prosthetic devices, dentures, eyeglasses
•
Freestanding birth center
•
Health home with chronic conditions
•
Health home for enrollees with substance use
disorder
•
Tobacco cessation for pregnant women
•
COVID-19 vaccines and administration
•
MAT treatment services for OUD
•
Care not otherwise categorized

MACStats: Medicaid and CHIP Data Book
153
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
EXHIBIT 51. (continued)
Service category T-MSIS service types
1
CMS-64 service types
Non-hospital
acute care
(continued)
•
Prenatal care and prepregnancy
family planning
•
Other pregnancy-related procedures
•
Hospice
•
Disposable medical supplies
•
Indian Health Service—family plan
•
Religious non-medical health care
institutions
•
EHR payments to provider in
outpatient setting (not on hospital
claim)
•
COVID-19 in vitro diagnostic products
or testing-related services
•
MAT and drugs for evidenced-based
treatment of OUD (not on a pharmacy
claim)
•
Residential pediatric recovery center
•
Other care
Drugs
•
Prescribed drugs
•
Over-the-counter medications (on a
pharmacy claim)
•
Medical equipment and prosthetic (on
a pharmacy claim)
•
EHR payments to pharmacy provider
•
MAT and drugs for evidence-based
treatment of OUD (on a pharmacy
claim)
•
Prescribed drugs
•
Drug rebates (national, state sidebar, ACA
oset—fee for service)
•
MAT drugs for OUD
•
MAT drug rebates (national, state sidebar, ACA
oset—fee for service)
Managed care
and premium
assistance
Claim type 2 (capitated payment) or
type of service:
•
Capitated payments to
comprehensive risk based managed
care plans (HMO, HIO, PACE)
•
Capitated payments to PHP
•
Capitated payments for PCCM
•
Premium payments for private
insurance
•
Per member, per month (PMPM)
payments for health home services;
Medicare Parts A, B, or D premiums;
Medicare Advantage dual special
needs plans
•
PMPM payments for other payments
•
MCO (i.e., comprehensive risk-based managed
care)
•
MCO drug rebates (national, state sidebar,
ACA oset—MCO)
•
MCO MAT drug rebates (national, state
sidebar, ACA oset—MCO)
•
PACE
•
PAHP
•
PIHP
•
PCCM
•
MCO, PAHP, and PIHP payments associated
with the primary care physician payment
increase, Community First Choice option,
certied community behavioral health clinic,
preventive services with USPSTF Grade A
or B, ACIP vaccines, and services subject to
electronic visit verication requirements
•
Premium assistance for private coverage

December 2023
154
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
EXHIBIT 51. (continued)
Service category T-MSIS service types
1
CMS-64 service types
LTSS non -
institutional
Type of service:
•
Home health, including nursing;
home health aide; and physical,
occupational, speech, and hearing
therapy
•
Personal care
•
Residential care
•
HCBS waiver
•
Payments to individuals for personal
assistance services under 1915(j)
Or program type:
•
HCBS waiver
•
Balancing incentive payment
•
HCBS—1915(i)
•
HCBS—1915(j)
•
HCBS—1915(k)
Or Title XIX service code is one of the
LTSS non-institutional CMS-64 service
types
•
Home health
•
Personal care
•
Personal care—1915(j)
•
HCBS waiver
•
HCBS—1915(i)
•
HCBS—1915(j)
•
HCBS—1915(k)
•
Certied community health clinic
LTSS institutional
•
Nursing facility
•
Inpatient hospital and nursing facility
services for individuals age 65 and
older in IMD
•
Intermediate care facility
•
Inpatient psychiatric or skilled nursing
facility for individuals under age 21
•
Inpatient and residential substance
abuse treatment
•
EHR payments to LTSS institutional
provider
•
Inpatient psychiatric services for
beneciaries ages 22 to 64 who
receive services in an IMD
•
Nursing facility
•
Nursing facility supplemental payments
•
ICF/ID
•
ICF/ID supplemental payments
•
Mental health facility for individuals under age
21 or age 65 and older, non-DSH
Medicare
3, 4
•
Medicare Part A and Part B premiums
•
Medicare coinsurance and deductibles for
QMBs
Notes: FY is scal year. T-MSIS is Transformed Medicaid Statistical Information System. DSH is disproportionate share
hospital. GME is graduate medical education. EHR is electronic health record. EPSDT is early and periodic screening,
diagnostic, and treatment. USPSTF is U.S. Preventive Services Task Force. ACIP is Advisory Committee on Immunization
Practices. MAT is medication-assisted treatment. OUD is opioid use disorder. ACA is the Patient Protection and Aordable
Care Act (P.L. 111-148, as amended). HMO is health maintenance organization. HIO is health insuring organization. PACE
is Program of All-Inclusive Care for the Elderly. PHP is prepaid health plan. MCO is managed care organization. PCCM is
primary care case management. PAHP is prepaid ambulatory health plan (a type of PHP). PIHP is prepaid inpatient health
plan (a type of PHP). HCBS is home- and community-based services. LTSS is long-term services and supports. IMD is
institution for mental disease. ICF/ID is intermediate care facility for persons with intellectual disabilities. QMB is qualied
Medicare beneciary. Service categories and types reect fee-for-service spending unless noted otherwise. Service types
with identical names in T-MSIS and CMS-64 data may still be reported dierently in the two sources due to dierences in
the instructions given to states; amounts for those that appear only in the CMS-64 (e.g., drug rebates) are distributed across
Medicaid enrollees with T-MSIS spending in the relevant service categories (e.g., drugs).

MACStats: Medicaid and CHIP Data Book
155
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
Understanding Managed
Care Enrollment and
Spending Data
There are four main sources of data on Medicaid
managed care available from CMS.
Medicaid Managed Care Enrollment
and Program Characteristics Report
The Medicaid Managed Care Enrollment and Program
Characteristics Report provides state-reported
aggregate enrollment statistics and other basic
information for each managed care plan within a state.
This report is the source of information on Medicaid
managed care most commonly cited by CMS as well
as by outside analysts and researchers.
T-MSIS
T-MSIS provides person-level and claims-level
information for all Medicaid enrollees. For managed
care, T-MSIS claims include records of each capitated
payment made on behalf of an enrollee to a managed
care plan (generally referred to as capitated claims)
as well as records of each service received by
the enrollee from a provider under contract with a
managed care plan (which may be referred to as
encounter or so-called dummy claims). All states
collect encounter data from their Medicaid managed
care plans, and CMS is working with states so
these data are reported into T-MSIS. Managed care
enrollees may also have FFS claims in the T-MSIS
if they used services beyond those covered by a
managed care plan’s contract with the state.
CMS-64
The CMS-64 nancial management report provides
aggregate spending information for Medicaid grouped
into major benet categories, including managed care.
The spending amounts reported by states on the CMS-
64 are used to calculate their federal matching dollars.
SEDS
The SEDS provides aggregate statistics on CHIP
enrollment and child Medicaid enrollment that include
the number of individuals covered under FFS and
managed care systems. The SEDS is currently the
primary source of information on managed care
participation among separate CHIP enrollees across
states. However, states can submit information on
separate CHIP into T-MSIS, so T-MSIS may become
another source of information on separate CHIP in
the future.
¹ Claims in T-MSIS include variables for claim type (e.g., fee for service, capitated payment), type of service (such as inpatient
hospital, physician, personal care), program type (including HCBS waiver), and Title XIX service category code (corresponds
to CMS-64 category). When classifying T-MSIS claims into service categories, we generally relied on type of service, with a
few exceptions. We classied all claims with a claim type indicating a capitated payment as managed care regardless of the
type of service associated with the claim. For non-institutional LTSS, we also included any claim with a program type indicating
HCBS or a Title XIX service category code that matched the CMS-64 service types we select for this category.
² Emergency services for non-qualied aliens are reported under individual service types throughout T-MSIS but primarily as
inpatient and outpatient hospital. As a result, we include this CMS-64 amount in the hospital category.
³ Medicare premiums are not reported in T-MSIS. We distribute CMS-64 amounts proportionately across dually eligible
enrollees identied in the T-MSIS for each state.
⁴ Medicare coinsurance and deductibles are reported under individual service types throughout T-MSIS. We distribute CMS-
64 amounts for QMBs across CMS-64 spending in the hospital, non-hospital acute, and LTSS institutional categories before
calculating state-level adjustment factors based on the distribution of Medicare cost sharing for hospital, Part B, and skilled
nursing facility services among QMBs using 2020 Medicare data. See MedPAC and MACPAC, 2023, Table 5: Fee-for-service
Medicare Part A and Part B cost sharing incurred by dual-eligible and non-dual Medicare beneciaries (dollars in billions), CY
2020, in Data book: Beneciaries dually eligible for Medicare and Medicaid, Washington, DC: MedPAC and MACPAC, https://
www.macpac.gov/wp-content/uploads/2023/02/Feb23_MedPAC_MACPAC_DualsDataBook-WEB-508.pdf.
Source: MACPAC, 2023, analysis of T-MSIS and CMS-64 nancial management report net expenditure data.
EXHIBIT 51. (continued)

December 2023
156
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4 Section 1
MACStats
Section 6
Historically, the annual Medicaid managed care
enrollment report generally contains the most
recent information available from CMS on Medicaid
managed care for all states; however, it does not
provide information on many characteristics of
enrollees in managed care (e.g., basis of eligibility and
demographics such as age, sex, race, and ethnicity).
It does provide information on whether individuals
are dually eligible for Medicare. Due to improved
timeliness, T-MSIS provides data that are as recent
as the Medicaid managed care report, and these
data can be analyzed at the beneciary level. As a
result, MACStats also includes statistics based on
T-MSIS and CMS-64 data, such as the percentage
of individuals enrolled in managed care by eligibility
group and the percentage of Medicaid benet
spending attributable to managed care.
When examining managed care statistics from various
sources, the following issues should be noted:
•
Figures in the annual Medicaid managed care
enrollment report published by CMS include
Medicaid-expansion CHIP enrollees. Although
we generally exclude these children (about 5 to 6
million) from Medicaid analyses in MACStats, it is
not possible to do so with the CMS annual Medicaid
managed care enrollment report data.
19
•
The types of managed care reported by states may
dier somewhat between the Medicaid managed
care enrollment report and T-MSIS. For example,
some states report a small number of enrollees in
comprehensive risk-based managed care in one
data source but not the other.
•
The Medicaid managed care enrollment report
provides point-in-time gures. In contrast, T-MSIS
data allow the calculation of number of enrollees
ever enrolled in managed care during a scal year
or other period of time.
Endnotes
1
For technical guides to earlier editions of MACStats,
see the MACStats archive page of the MACPAC website,
https://www.macpac.gov/publication/macstats-archive/. For
MACStats before December 2015, the technical guide is
included in each year’s June report.
2
CMS has been collecting Medicaid and CHIP performance
indicator data on key processes related to eligibility and
enrollment since late 2013. In part because the Medicaid
and CHIP performance indicator enrollment data do not
identify newly eligible individuals for whom there is a higher
federal matching rate, CMS is using a separate process to
collect monthly Medicaid enrollment by eligibility category
when states submit their CMS-64 quarterly expenditures.
Specically, a CMS-64 enrollment form has been created
to accompany the current expenditure forms. Although
enrollment is submitted at the same time as expenditures,
there is not a direct link between the amount of federal
expenditures claimed by states and the number of enrollees
reported. Instead, CMS uses CMS-64 enrollment data for
monitoring and oversight purposes.
3
The Data Quality Atlas can be found at https://www.
medicaid.gov/dq-atlas/welcome.
4
The timing of each state’s transition from MSIS to T-MSIS
can be found at https://www.medicaid.gov/medicaid/data-
and-systems/downloads/macbis/taf-rif-availability-chart.pdf.
5
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2018. Letter
from Tim Hill to state health ocials regarding “Transformed-
Medicaid Statistical Information System (T-MSIS).” August
10, 2018. https://www.medicaid.gov/federal-policy-guidance/
downloads/sho18008.pdf.
⁶ See, for example, Centers for Medicare & Medicaid
Services (CMS), 2010, Brief summaries and glossary
(2010 edition), in Medicare & Medicaid statistical
supplement, Baltimore, MD: CMS. https://www.cms.
gov/Research-Statistics-Data-and-Systems/Statistics-
Trends-and-Reports/MedicareMedicaidStatSupp/
Downloads/2010SummariesGlossary.zip.
⁷ States make capitated payments for all individuals enrolled
in managed care plans even if no health care services are
used. Therefore, all managed care enrollees currently are
counted as beneciaries or persons served, regardless of
whether they have used any health services.

MACStats: Medicaid and CHIP Data Book
157
Section 6: Technical Guide to MACStats
MACStats
Section 6 Section 3Section 5 Section 2Section 4
Section 1
MACStats
Section 6
⁸ Centers for Disease Control and Prevention (CDC), U.S.
Department of Health and Human Services, 2022, About the
National Health Interview Survey. http://www.cdc.gov/nchs/
nhis/about_nhis.htm.
⁹ Agency for Health Care Research and Quality (AHRQ),
U.S. Department of Health and Human Services, 2019,
Medical Expenditures Panel Survey: Survey background.
http://meps.ahrq.gov/mepsweb/about_meps/survey_back.
jsp.
10
Kenney, G., and V. Lynch, 2010, Monitoring children’s
health insurance coverage under CHIPRA using federal
surveys, in Databases for estimating health insurance
coverage for children: A workshop summary, Plewes, T.J.,
ed., Washington, DC: National Academies Press. http://
www.nap.edu/catalog/13024.html.
11
Rhoades, J.A., J.W. Cohen, and S.R. Machlin, 2010,
Methodological comparison of estimates of ambulatory
health care use from the Medical Expenditure Panel Survey
and other data sources (pp. 2828–2837, health policy
statistics section), in JSM Proceedings, Alexandria, VA:
American Statistical Association. http://www.asasrms.org/
Proceedings/y2010/Files/307444_58577.pdf
.
12
IPUMS Health Surveys. 2019. User note: Washington
Group on Disability Statistics Measures. https://nhis.ipums.
org/nhis/userNotes_washingtongroup.shtml
.
13
In Kansas, several claims were missing service dates. We
used paid dates to assign these claims to a time period.
14
The new adult group includes those enrollees who are
eligible under Section 1902(a)(10)(A)(i)(VIII) of the Act. We
include both newly eligible adults and not newly eligible
adults eligible under this pathway. Newly eligible adults
include those enrollees who were not eligible for Medicaid
under the rules that a state had in place on December 1,
2009, and received a federal matching rate of 100 percent
in 2014 through 2016, phasing down to 90 percent in 2020
and subsequent years. Adults considered not newly eligible
include those enrollees who would have previously been
eligible for Medicaid under the rules that a state had in
place on December 1, 2009; this includes states that had
already expanded to adults with incomes greater than 100
percent of the federal poverty level as of March 23, 2010,
and receive the expansion state transitional matching
rate. Other adults include adults under age 65 who qualify
through a pathway other than disability or Section 1902(a)
(10)(A)(i)(VIII) of the Act (e.g., parents and caretakers,
pregnancy).
15
Until December 2017, Georgia did not report header-level
spending for capitation payments. If the header amount was
zero or missing, we used the aggregate line-level spending
for capitated payments in Georgia.
16
Medicaid benet spending reported here excludes
amounts for Medicaid-expansion CHIP enrollees, the
territories, administrative activities, the Vaccines for Children
program (which is authorized by the Medicaid statute but
operates as a separate program), and osetting collections
from third-party liability, estate, and other recoveries.
17
Some of these amounts, including certain supplemental
payments to hospitals and drug rebates, are lump sums that
are not paid on a claim-by-claim basis for individual Medicaid
enrollees. Nonetheless, we refer to these CMS-64 amounts
as benet spending, and the adjustment methodology
described here distributes them across Medicaid enrollees
with T-MSIS spending in the relevant service categories.
18
The sum of adjusted T-MSIS benet spending for all
service categories is equal to CMS-64 benet spending,
exclusive of osetting collections from third-party liability,
estate, and other recoveries. These collections are not
reported by type of service in the CMS-64 and are not
reported at all in the T-MSIS.
19
We generally exclude children enrolled in Medicaid-
expansion CHIP from Medicaid analyses because their
funding stream (Title XXI of the Act) diers from that of
other Medicaid enrollees (Title XIX of the Act). In addition,
spending (and often enrollment) for the Medicaid-expansion
CHIP population is reported by CMS in CHIP statistics along
with information on separate CHIP enrollees.



