
L.A. Care Medi-Cal
2017
™
Provider Manual
LA1722 01/17
Toll Free: 1.888.839.9909 | TTY: 711 lacare.org
Contents
1.0 Welcome to L.A. Care Health Plan ...6
General Introduction ........................ 6
Medi-Cal and e Two Plan Model ............. 6
Responsibility of Participating Providers .......... 6
L.A. Care’s Commitment to
Provide Excellent Services ..................... 6
Traditional and Safety Net Providers ............ 6
Website Information Available to Providers ....... 6
Notice to Providers .......................... 7
L.A. Care Departmental Contact List ............ 8
2.0 Membership and
Membership Services ................ 12
Responsibility of Participating Providers ......... 12
Program Eligibility ......................... 12
Member Enrollment,
Assignment and Disenrollment ............... 12
Member Identification Card .................. 14
Eligibility Verification ....................... 14
Evidence of Coverage ....................... 14
Co-Payments ............................. 14
Member’s Rights And Responsibilities .......... 15
Notice to Members Regarding
Change in Covered Services .................. 16
Member Grievances and Appeals .............. 16
3.0 Access to Care .................... 19
Responsibility Of Participating Providers ........19
Access to Care Requirements (Primary Care
and Specialty Care Physicians, Behavioral
Health And Ancillary Providers) ............... 19
Primary Care Provider (PCP)
Appointment Standards ..................... 19
Specialty Care Provider (SCP)
Appointment Standards ..................... 20
Ancillary Care Appointment Standards ......... 20
Behavioral Health Care Appointment Standards ....20
After Hours Care Accessibility Standards ........ 21
Practitioner Telephone Responsiveness .......... 21
Monitoring .............................. 21
4.0 Scope of Benets ................. 22
Principal Benefits and Coverages .............. 22
Principal Exclusions and Limitations ........... 22
Excluded (Carve-Out) Services ............... 22
Exceptions for Services Not Covered by
L.A. Care Health Plan or Regular Medi-Cal ...... 23
Nurse Advice Line (NAL) ................... 23
Non-Emergency Medical Transportation ........ 23
5.0 Utilization Management .......... 24
Goal and Objectives ........................ 24
Scope of Service ........................... 25
Delegation of Utilization Management .......... 26
Utilization Management Delegation
Monitoring and Oversight ................... 27
Benefits ................................. 33
Continuity of Care (COC) .................. 33
New Medical Technology .................... 37
Responsibility of Participating Providers ........ 37
After Hours Authorization ................... 37
UM Referral Management Review Processes ..... 38
Services Exempt From (Not Requiring)
Prior Authorization (Pre-Service Review) ........ 39
Services Requiring Prior Authorization .......... 39
Utilization Management Services
Not Delegated to PPGS ..................... 39
Medical Necessity Definitions ................ 42
PPG UM Criteria ......................... 44
Criteria for Use in L.A. Care Review of Appeals
and Other Requested Clinical Reviews .......... 44
Second Opinion Process ..................... 50
Standing Referral Process .................... 50
Coordination of Medically
Necessary Services ......................... 51
Tuberculosis Treatment Services
Provided by Primary Care Provider ............. 54
Cervical Cancer Screening ................... 54
Health Risk Assessment (HRA) ............... 55
Care Management (CM) .................... 56
Hospice Care Services. . . . . . . . . . . . . . . . . . . . . . . 58
L.A. Care Appeals Process ................... 59
Independent Medical Review (IMR) ........... 61
Initial and Periodic Health Assessments ......... 61
Missed or Broken Appointments .............. 64
Children With Special
Health Care Needs (CSHCN) ................ 65
Disease Management ....................... 65
Behavioral Health Services ................... 65
Vision Services ............................ 67
Matrix for Linked and Carve Out
Services By Product Line .................... 68
Care Coordination with Medi-Cal
Linked and Carved-Out Services .............. 68
Description and Responsibilities for the
Linked and Carved Out Programs
California Children Services (CCS) ............ 69
Maternal and Child Health – Comprehehsive
Prenatal Services Program (CPSP) ............. 71
School Linked Child Health And Disabilities
Prevention (CHDP) – Medi-Cal .............. 72
Tuberculosis/Direct Observation
erapy - Medi-Cal ........................ 73
Women, Infants And Children (WIC)
Nutritional Supplement Program .............. 74
Developmental Disabilities Services (DDS) ...... 75
Early Intervention/Early Start-Medi-Cal ........ 76
Specialty Mental Health ..................... 78
Alcohol and Drug Treatment Programs ......... 78
Local Education Agency (LEA) – Medi-Cal ...... 79
Dental Services for Medi-Cal Members ......... 79
Targeted Case Management Services ........... 81
EPSDT Supplemental Services For Members
Under the Age of 21 Years – Medi-Cal .......... 83
Excluded Services Requiring Member
Disenrollment – Medi-Cal ................... 86
Child Health and Disabilities
Prevention Program (CHDP) ................. 86
Attachment A: L.A. Care Timeliness Standards ... 87
Attachment B: Vision, Dental,
and Behavioral Health Benefit Grid ........... 102
6.0 Quality Improvement
(QI) Program ........................104
Annual Quality Improvement
Program Evaluation ....................... 104
Annual Quality Improvement Work Plan ....... 104
Committee Structure ...................... 104
Clinical Care Measures ..................... 105
Service Measures ......................... 105
Preventive Health Care Guidelines ............ 106
Disease Management Programs .............. 106
Patient Safety ............................ 106
Disease Reporting Statement ................ 106
PPG and Other Contracted Provider
and Vendor Reporting Responsibilities ......... 106
Categories of Critical Incidents .............. 106
Referrals to Local Agencies .................. 108
7.0 Credentialing ....................109
Overview ............................... 109
Delegation of Credentialing ................. 109
PPG Responsibilities ...................... 109
Provisional Credentialing ................... 113
Confidentiality and Practitioner Rights ........ 113
Requirements ............................ 114
Recredentialing .......................... 116
Credentialing Committee ................... 116
Meetings and Reporting .................... 116
Committee Decisions ...................... 116
Participation of Medical Director
or Other Designated Practitioner ............. 116
Committee Functions ..................... 116
Credentials Committee File Review ........... 117
Appeal and Fair Hearing .................... 117
Required Reporting ....................... 118
Expired License .......................... 118
8.0 Provider Network
Management (PNM) .................119
Provider Training And Education ............. 119
Provider Directories ....................... 120
Primary Care and Mid-Level
Medical Practitioner Capacity ............... 120
Provider Relations Contact Information ........ 120
Provider Appeals and Grievances ............. 121
9.0 Health Education ................122
Health Education Services .................. 122
L.A. Care Family Resource Centers ........... 123
Nurse Advice Line ........................ 123
Health Education Programs ................. 123
Provider Education ........................ 123
10.0 Cultural & Linguistic Services ...124
Assessing Bilingual Language Proficiency ....... 124
Inerpretating Services ...................... 124
Translation Services and Alternative Formats ......126
Cultural and Linguistic Tools and Resources ......127
Reporting Requirements .................... 128
11.0 Finance ........................130
Capitation Payments ...................... 130
Capitation Statement Report ................ 130
Insurance ............................... 130
Minimum Financial Solvency Standards ........ 131
Reimbursement Services and Reports .......... 131
Records, Reports, and Inspection ............. 132
12.0 Claims and Payment ............133
Responsibility of Participating Providers ........ 133
Claims Submission ........................ 133
Claims Adjudication ....................... 133
Provider Portal Claims Verification ............ 134
Coordination of Benefits ................... 134
Balance Billing ........................... 134
Provider Disputes ......................... 134
Payment ................................ 135
Reporting: Quarterly Filing of AB1455 ........ 136
13.0 Encounter Data ................. 137
Requirements ............................ 137
14.0 Marketing ...................... 138
Regulatory Approval ....................... 138
Marketing Activities and Standards ........... 138
Approval Process ......................... 139
Prohibited Activities ....................... 140
15.0 Compliance ....................141
Goal and Objectives ....................... 141
Authority and Responsibility ................ 141
Delegation of Compliance and Audit Program ... 141
Audit and Oversight Activities ............... 141
Provider Compliance Responsibilities .......... 142
L.A. Care’s Program Integrity Plan ............ 144
Enforcement of Disciplinary Standards ........ 146
e Federal and California False Claims Acts .... 146
Health Insurance Portability
and Accountability Act (HIPAA) ............. 146
Privacy and Information Security
Related Resources and Websites .............. 147
16. 0 Pharmacy ......................148
Overview ............................... 148
Pharmacy Quality and
Oversight Committee (PQOC) .............. 148
How to Use the Formulary .................. 148
Generic Substitution ...................... 148
Non-Formulary Agents .................... 148
Restrictions on Drug Coverage ............... 148
Prescription Drug Prior
Authorization Request Process ............... 149
Appeals and Grievances .................... 149
Diabetes Testing Supplies ................... 149
Over-the-Counter Medication Coverage ....... 150
Devices & Vaccines ....................... 150
General Benefit Exclusions (Not Covered) ...... 150
Pharmacy Network ........................ 150
Mail Order Prescriptions ................... 150
Specialty Pharmacy ........................ 150
Pain Medication for the Terminally Ill ......... 151
erapeutic Interchange .................... 151
Opioid Utilization Monitoring ............... 151
E-Prescribing/Electronic Health Records ....... 151
Role of Navitus Health Solutions ............. 151
Contact Us .............................. 151
17.0 Managed Long Term
Services and Support ...............152
Managed Long Term Services and
Supports: A Resource for Providers ............ 152
In-Home Supportive Services ................ 152
Community Based Adult Services ............. 153
Multipurpose Senior Services Program ......... 153
Care Plan Options ........................ 153
Long Term Care .......................... 154
6
1.0 Welcome To
L.A. Care Health Plan
1.1 General Introduction
ank you for participating in L.A. Care Health Plan’s
(L.A. Care) provider network and helping fulfill its
mission to provide high quality health care services to
L.A. Care’s members in Los Angeles County.
We would like to welcome you to L.A. Care. As part
of L.A. Care’s Medi-Cal Direct (MCLA) network
of providers; you play a very important role in the
delivery of health care services to our members.
e purpose of this L.A. Care Medi-Cal Provider
Manual (Provider Manual) is to furnish all Providers,
including Participating Physician Groups (PPGs) and
their affiliated Provider networks, specialty health
plans, physicians or physician groups, hospitals, safety
net providers, California Community-Based Adult
Services (CBAS) centers, and other ancillary providers,
with information on the important processes related
to L.A. Care’s Medi-Cal product. e Provider
Manual is organized by substantive sections and
provides information about applicable requirements
for the Medi-Cal program, L.A. Care policies, general
reference information, including minimum standards
of care, and other responsibilities. Please read each
section in this Provider Manual carefully in order to
determine your contracted provider responsibilities.
1.1.1 Medi-Cal and the Two Plan Model
Medi-Cal is California’s Medicaid program. It is a
public health insurance program administered by
the California Department of Health Care Services
(DHCS). e Medi-Cal program was established
in 1965 to provide the necessary health services for
low-income individuals or people with disabilities. In
California, the Medi-Cal program is governed by the
California Welfare and Institutions Code and provisions
of Title 22 of the California Code of Regulations. Since
1998, significant portions of the Medi-Cal population
have been enrolled into managed care organizations
on a mandatory basis. In 2014, as a result of the
implementation of Affordable Care Act, Medi-Cal
managed care enrollment expanded. In Los Angeles
County, Medi-Cal is operated through a Two-Plan
Model consisting of a “local initiative” health plan
and a commercial plan. L.A. Care is the local initiative
managed care plan in Los Angeles County. Currently,
Health Net is the commercial plan.
1.1.2 Responsibility of
Participating Providers
L.A. Care requires that its contracted Providers
(including but not limited to medical groups, hospitals,
Providers, PPGs, specialized health plans, physicians
or physician groups, hospitals, community-based
adult services (CBAS) centers, and other ancillary
Providers) meet specific requirements. Many sections
of this Provider Manual include a section entitled
“Responsibility of Participating Providers.” is section
is provided to assist the contracted Provider with
understanding which functions are the responsibility of
L.A. Care, PPGs, hospitals, ancillary Providers, and/or
other participating Providers, respectively.
1.1.3 L.A. Care’s Commitment
to Prvide Excellent Services
L.A. Care’s overall goal is to develop policies,
procedures, and guidelines for effective
implementation of Provider services in its product
lines. To accomplish this goal, L.A. Care will work
cooperatively with network Providers to ensure
that they have timely access to information and the
appropriate resources to meet service requirements.
1.1.4 Traditional and Safety
Net Providers
L.A. Care considers the following provider types as
some examples, but not all inclusive examples of
Traditional or Safety Net Providers: Child Health
and Disability Prevention (CHDP) Providers,
Federally Qualified Health Centers (FQHCs),
licensed community clinics, and Disproportionate
Share Hospitals.
1.2 Website Information
Available to Providers
e L.A. Care website has useful information for
Providers. Please visit our website at www.lacare.org
for information about the following:
• Provider Portal Sign In
°
Check Patient Eligibility
°
PCP Registration
• Provider Resources
°
Cal MediConnect Tools
°
Provider Manuals
°
Provider Forms
Utilization Management Forms
− Pre-Authorization Request Form
7
− Hospital Authorization and Billing Reference
Guide
Care Management Forms
− Care Management Referral Form
Claims Forms
− PM-160 Form
− CMS 1500 Claim Form
− Provider Dispute Resolution Request Form
Managed Long Term Services and Supports
− Long Term Care and CBAS Referral Request
Form
− LTSS Referral Form
Prescription Drug Prior Authorization Request
Form
− Medicare (Cal MediConnect) Coverage
Determination Form
− Prior Authorization Request Forms
Reference Guide
− Coding Reference Guide for Acute Respiratory
Conditions
− Provider Authorization and Billing Reference
Guide
− SNF Authorization and Billing Guidance
Provider Portal Resources
− Provider Portal Reference Guide
Additional Referral Forms
− CA Pediatric WIC Referral Form
°
Provider Policies
°
Provider Toolkits
°
Staying Healthy Forms
°
Clinical Guidelines
°
Skilled Nursing Resources
• Behavioral Health
°
Behavioral Health Services
°
Forms and Toolkits
°
Specialty Mental Health
°
Substance Use Disorder
• Pharmacy Services
°
Medication Adherence
°
Prior Authorizations
°
List of Covered Drugs
• HEDIS Resources
• Health Education Tools
• Social Services Directory
• Quality Improvement Program
• Provider FAQs
• Provider News
°
Health Advisories
°
Progress Notes
°
e PULSE
°
Newsletter Sign Up
• Claims and ICD-10
°
Submitting a Claim
°
ICD-10
• Provider Training
°
Classes & Seminars
°
Physician Leadership Program
If you would like paper copies of any of the information
available on the website, please contact us at
1.866.LA.CARE6 (1.866.522.2736) and submit
your request.
1.3 Notice to Providers
From time to time, L.A. Care amends Provider
contracts and updates the Provider Manual and/
or its Policies and Procedures. Updates are done
to ensure Providers have necessary information on
the most up-to-date laws, regulations, and revisions
to provide the highest quality services to L.A. Care
Members and ensure regulatory compliance. L.A. Care
works to promptly notify all Providers of material
changes in requirements. L.A. Care utilizes multiple
communication avenues to advise providers of changes
e.g. newsletters, e-mails, letters, and announcements
on our website. For more information, please refer to
the L.A. Care’s website located at www.lacare.org.
8
1.4 L.A. Care Departmental Contact List
L.A. Care Health Plan
1055 W. 7th Street
Los Angeles, CA 90017
1.213.694.1250
Department Contact Information
Capitation 1.213.694.1250, x 4377
Care Management 1.844.200.0104
Claims 1.866.522.2736
Mail L.A. Care claims questions to:
L.A. Care Health Plan
Attn: Claims Dept.
P.O. Box 811580
Los Angeles, CA 90081
Cultural and Linguistic Services 1.213.694.1250, x 4523
Eligibility Verification,
Provider Service Line
Register for the Provider Portal to verify member eligibility at:
lacare.org and click on Provider Sign in.
1.866.522.2736 or 1.866.LACARE6
Encounter Data Provider Service Line;
1.866.LA.CARE6 or 1.866.522.2736
Health Education;
Health in Motion
1.855.856.6943
Managed Long Term
Services and Supports (MLTSS)
Provider Inquiry Line:
1.855.427.1223
Fax: 1.213.438-4866
Marketing/Sales 1.213.694.1250, x 5712
Member Services General Information Line
Medi-Cal – 888.839.9909
CMC – 1.888.522.1298
Pharmacy 1.877.795.2227
Prior Authorizations and
Hospital Admissions
L.A. Care UM Department must be notified within 24 hours
or the next business day following inpatient admission.
To submit an Authorization request:
Call Toll-Free: 1.877.431.2273
Fax: 1.213.623.8669
Written Requests:
L.A. Care Health Plan
1055 W. 7
th
Street, 10
th
Floor
Los Angeles, CA 90017
Attn.: Utilization Management/Authorizations

9
Department Contact Information
Provider Credentialing, Performance,
and Certification
1.844.530.7596
Provider Information/Data Issues Provider Inquiry Line
1.866.LA.CARE6 or 1.866.522.2736
Provider Network
Management
1.213.694.1250, extension 4719
Provider Inquiries Providers may communicate questions or concerns to
their contracted PPG or to L.A. Care directly.
Telephone:
L.A. Care’s Provider Services Unit:
1.866.LACARE6,
(1.866.522.2736)
In writing:
L.A. Care Health Plan
Attn: Provider Relations
1055 W. 7
th
Street, 10
th
Floor
Los Angeles, CA. 90017
E-mail:
LACarePSU@lacare.org
(Five to seven business-day turn-around response)
Your assigned Provider Relations Representative
Quality Improvement, Senior Director 1.213.694.1250, x 5744
Quality Improvement, Medical Director 1.213.694.1250, x 5315
Quality Improvement,
Disease Management
1.213.694.1250, x 4768
Quality Management, Director 1.213.694.1250, x 5203
Regulatory Affairs and Compliance 1.213.694.1250, x 4292
Utilization Management, Director 1.213.694.1250, x 5181

10
Glossary of Terms
Acronym or Word(s) Denition
AAP American Academy of Pediatrics
AIM Access for Infants and Mothers Program
Ancillary Service
e following services are considered ancillary: ambulance transportation;
durable medical equipment (DME) including but not limited to apnea monitor,
artificial limbs, and hearing aids; home health care; prosthetic and orthodontic
devices; and skilled nursing facilities.
BOG Board of Governors
CAP Corrective Action Plans
CBAS Community Based Adult Services
CCS
California Children’s Services – is program provides health care services to
children with certain physical limitations and diseases whose families cannot
afford all or part of the care.
CHDP Child Health & Disability Prevention
CPSP Comprehensive Perinatal Services Programs
DDS Developmental Disability Services
DHCS Department of Health Care Services
DOFR Division of Financial Responsibility
FSR Facility Site Review
HEDIS Healthcare Effectiveness Data and Information Set
IBNR Incurred But Not Reported
PASC-SEIU Home Care Workers Union

11
Acronym or Word(s) Denition
IPA
Independent Practice Association – In the L.A. Care Provider Manual, IPA will
be referred to Participating Physician Groups (PPGs)
L.A. Care L.A. Care Health Plan (Local Initiative Health Authority for Los Angeles County)
LTC Long Term Care
LTSS
Long Term Services and Supports
(a.k.a. Managed Long Term Supports and Services)
MOU Memorandum of Understanding
MLTSS
Managed Long Term Services and Supports
(a.k.a. Long Term Services and Supports)
MRMIB Managed Risk Medical Insurance Board
MSSP Multipurpose Senior Services Program
NCQA National Committee for Quality Assurance
NAL Nurse Advice Line
PCP Primary Care Provider
PNM Provider Network Management
QIP Quality Improvement Plan
SED Severely Emotionally Disturbed
SNF Skilled Nursing Facility
WIC Program Women, Infant & Children’s Nutritional Supplemental Program
12
2.0 Membership and
Membership Services
is section covers L.A. Care Medi-Cal membership
and Member Services. Topics include eligibility,
enrollment and disenrollment, Primary Care Physician
(PCP) assignment, complaint resolution, and member
rights and responsibilities.
2.1 Responsibility of
Participating Providers
L.A. Care Medi-Cal participating Providers are
responsible for adhering to the Member Services
provisions and guidelines specified in this section.
2.2 Program Eligibility
Individuals who wish to enroll in L.A. Care must have
been determined eligible for the Medi-Cal program
through a County, Department of Health Care
Services (DHCS) state office, or the Social Security
Administration.
DHCS basic Medi-Cal eligibility criteria include the
following categories:
• Children under 21 years old
• Adults over 65 years old
• Low-income adults
• Families with children
• Individuals with disabilities
• Foster youth up to age 26
• Pregnant women
In addition, Medi-Cal applicants must meet income
and asset levels, as established by the Medi-Cal program.
All beneficiaries who are determined eligible for the
Medi-Cal program may enroll into L.A. Care’s Medi-Cal
product line. For further information, go to the DHCS’
site at http://www.dhcs.ca.gov/ or Covered California’s
site at http://www.coveredca.com/medi-cal/.
2.2.1 Conditions of Enrollment
At the time of enrollment, L.A. Care provides new
enrollees with a Summary of Benefits, a Provider
Directory, a Pharmacy Directory, a copy of the
Pharmacy Formulary, and an enrollment date.
Member materials as well as other helpful resources are
available on the L.A. Care website at www.lacare.org.
2.2.2 Disenrollment
Members who do not meet the Medi-Cal eligibility
requirements may be disenrolled from L.A. Care
by DHCS.
2.3 Member Enrollment, Assignment,
and Disenrollment
L.A. Care informs Members about their enrollment
rights, responsibilities, plan benefits and rules.
L.A. Care uses multiple methods to meet the
cultural and linguistic needs of Members as well as
to communicate with them in their own language,
including, but not limited to, the following:
• Translation of Member materials into threshold
languages
• Referral to physicians who can provide services in
the Member’s preferred language
• Use of qualified bilingual staff contracts for
telephonic and face-to-face interpreting services,
including American Sign Language (ASL) at medical
and non-medical points of contact
• Hearing or speech impaired members can
contact L.A. Care through the California
Telecommunications Relay Services at TTY 711
L.A. Care publishes access information for People
with Disabilities for each contracted Provider in the
L.A. Care Provider Directories, which is updated
monthly. Updated Provider Directories are sent to new
Members upon enrollment with the “New Member
Welcome Kit” and then annually thereafter, based on
Member eligibility.
Providers should notify L.A. Care immediately of changes
to their language capabilities and access information.
2.3.1 Medi-Cal Guidelines
ere are two types of Medi-Cal programs in Los Angeles
County, i.e. “fee-for-service” and “managed care.” Most
Medi-Cal beneficiaries in Los Angeles County are
enrolled in “managed care.” L.A. Care is a managed care
health plan.
Medi-Cal beneficiaries, who are part of the “fee-for-
service” program, are not enrolled in a managed care
health plan and must find doctors and other providers
who will accept payment directly from Medi-Cal.
2.3.2 Medi-Cal Expansion
Under the Affordable Care Act, Medi-Cal has been
expanded to include low-income adults without
13
children. Coverage under the expansion began
January 1, 2014.
Medi-Cal currently provides health coverage for low-
income individuals including families with children,
Seniors and People with Disabilities (SPD), foster care
youth, pregnant women, and low income people with
specific diseases such as tuberculosis, breast cancer, or
HIV/AIDS. e Medi-Cal program now covers low-
income adults up to 138% of the federal poverty level.
2.3.3 Mandatory Medi-Cal Managed Care Members
DHCS is in charge of administering the Medi-Cal
Program. DHCS states that in Los Angeles County,
most Medi-Cal members must enroll in a health plan
and be in managed care. Members who must enroll
in a health plan are commonly known as “mandatory
members.” A mandatory member may disenroll from
Medi-Cal managed care only if the member:
1. Has a complex medical condition (such as HIV/
AIDS or cancer)
2. Has been in Medi-Cal managed care less than
90 days, and
3. Is being treated by a physician who does not work
with any Medi-Cal managed care health plan.
Otherwise, the mandatory member must choose a
managed care health plan, like L.A. Care.
2.3.4 Voluntary Medi-Cal Managed Care Members
In Los Angeles County, people with Medi-Cal may
choose to enroll in a health plan. Members who
choose to enroll in a health plan are called “voluntary
members.” A voluntary member can choose to leave
his or her health plan and return to fee-for-service
Medi-Cal at any time. Voluntary members include:
• American Indians; who are eligible to get services
from an Indian Health Center or Native American
Health Clinic
• Children in foster care or in the Adoption
Assistance Program
• Members with an HIV/AIDS diagnosis
• Some individuals with disabilities or elderly persons
receiving Supplemental Security Income (SSI)
• ose 65 years or older
2.3.6 Member Enrollment
2.3.6.1 Enrollment into Medi-Cal is administered by
DHCS using the State-contracted enrollment vendor,
Health Care Options (HCO). Eligible Prospective
Enrollees complete a CMS/DHCS approved
enrollment form that is processed through HCO.
2.3.6.2 Dual members are eligible beneficiaries under
the Medicare and Medi-Cal programs. All Dual-
Eligibles have a Medicare Special Election Period,
which allows them to enroll in and disenroll from a
Medicare-Advantage plan on a monthly basis. Dual-
Eligibles may join a Medicare-Advantage plan outside
of their Initial Election Period and Medicare’s Annual
Election Period.
2.3.6.3 All Dual-Eligibles who do not enroll in a
managed care plan are required to enroll in a managed
care Medi-Cal plan for their Medi-Cal benefits, with
some exceptions.
2.3.7 Selection, Assignment, and Change of Primary
Care Provider (PCP) and/or Participating Provider
Group (PPG)
2.3.7.1 Selection and Assignment
2.3.7.1.1 At the time of enrollment, eligible Medi-Cal
enrollees should select a PCP and PPG. Enrollees may
choose to keep their current doctors or clinics as long
as the doctors or clinics participate with L.A. Care.
Enrollees may choose a new doctor or clinic from
Providers in L.A. Care’s Provider Directory, which
lists all contracted L.A. Care PPGs, PCPs, specialists,
and hospitals. e Provider Directory also has helpful
information about each doctor and clinic. Enrollees
may choose a specialist as a PCP as long as the specialist
is listed as a PCP in the provider directory.
2.3.7.1.2 Enrollees who do not choose a PCP and
PPG will be assigned to a PCP and PPG by L.A. Care.
2.3.7.1.3 Health Care Options (HCO) will send a
confirmation enrollment letter. L.A. Care will send
a Welcome Packet that includes a welcome letter,
Provider Directory, Evidence of Coverage/Member
Handbook, and an identification card to an enrollee
no later than ten (10) calendar days from receipt of
confirmation of enrollment or by the last day of the
month prior to the effective date, whichever is later.
e selected or assigned PCP and PPG will be stated
on the Member’s identification card.
2.3.7.1.4 e PCP is responsible for coordinating,
supervising, and providing primary health care services,
including but not limited to, initiating specialty care
referrals and maintaining continued care. Specialists who
also meet the requirements for PCP participation and are
willing to assume the responsibilities of a PCP may also
request designation as a PCP in L.A. Care’s network.
14
2.3.7.2 Change of PCP and/or PPG
2.4.2.2.1 Members may change their PCP and/or
PPG on a monthly basis by calling L.A. Care Member
Services at 1.888.839.9909 (CRS TTY: 711). e
change will occur on the first of the following month,
provided the request is received by L.A. Care Member
Services by the 20
th
of the month.
2.4.2.2.2 Changes in the L.A. Care provider
network may also result in changes to the members’
PCP and/or PPG. L.A. Care will notify the members
of the change, the effective date of the change, and
the members’ right to request a different
PPG and/or PCP assignment.
2.3.7.3 Disenrollment
2.3.7.3.1 Disenrollment refers to the termination
of a member’s enrollment with Medi-Cal L.A. Care.
Disenrollment does not refer to a member transferring
from one PCP and/or PPG to another.
2.4.2.3.2 Voluntary disenrollment refers to a member
initiated termination from enrollment in L.A. Care.
A member may disenroll from L.A. Care by calling
Health Care Options (HCO) at 1.800.430.4263.
HCO enrolls or disenrolls Medi-Cal beneficiaries in
or out of a Medi-Cal managed care health plan. HCO
will send the member a disenrollment form via mail.
Membership will end on the last day of the month
in which HCO approves the member’s request for
disenrollment. Disenrollment takes from 15 to 45
business-days. e member must continue to receive
services through L.A. Care until the member is
disenrolled from L.A. Care.
2.4.2.3.3 Involuntary disenrollment means the
Medi-Cal member will lose managed care coverage
with L.A. Care, but not necessarily their Medi-Cal
benefits, if any of the following happens with a member:
• Member moves out of Los Angeles County
permanently
• Member requires medical health care services not
provided by L.A. Care (for example, some major
organ transplants)
• Member has other non-government or government-
sponsored health coverage
• Member is in prison or jail
2.4.2.3.3.1 A member may be involuntarily disenrolled
from L.A. Care if there is a loss of Medi-Cal eligibility.
is may occur under multiple circumstances including
lack of eligibility renewal.
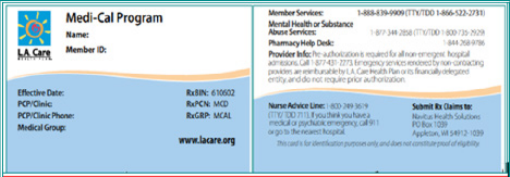
2.4 Member Identication Card
Members who are enrolled in L.A. Care Medi-Cal will
be issued an identification card like the example below.
is card contains their Health Plan (or PPG) number
and their PCP’s name and telephone number. e
card also provides other telephone numbers to assist
Members as they access services including pharmacy
and Nurse Advice Line information.
2.5 Eligibility Verication
2.5.1 A Member’s possession of an L.A. Care
membership identification card does not guarantee
current membership with L.A. Care, PPG or PCP
identified by the card. Verification of an individual’s
membership and eligibility status is necessary to assure
payment to the PPG or Provider for healthcare services
rendered to the member.
2.5.2 To verify member eligibility, providers can log
into the L.A. Care Provider Portal through L.A. Care
site at www.lacare.org, under the “For Providers”
tab, Provider Sign In/Check Patient Eligibility or call
L.A. Care’s Provider Services Line at 1.866.LA.CARE6
(1.866.522.2736).
2.6 Evidence of Coverage
An L.A. Care Evidence of Coverage/Member Handbook
(EOC) is sent to members upon enrollment and
annually thereafter. e EOC provides members with
a description of the scope of covered services and
information about how to access such services under
L.A. Care’s Medi-Cal plan. e Medi-Cal EOC is
available electronically online at www.lacare.org,
under the “For Members” tab, and Member Materials
section or in hard-copy by calling L.A. Care’s Provider
Information Line at 1.866.LA.CARE (1.866.522.2736).
2.7 Co-payments
No co-payments will be charged when receiving
services covered by the Medi-Cal program.
15
2.8 Member’s Rights and Responsibilities
2.8.1 L.A. Care Medi-Cal Members have specific rights
and responsibilities that are fundamental to the provision
and receipt of quality healthcare services, as follows:
• Respectful and courteous treatment. Members have
the right to be treated with respect, dignity and
courtesy by their provider and staff. Members have
the right to be free from retaliation or force of any
kind when making decisions about their care.
• Privacy and confidentiality. Members have the right to
have their medical records kept confidential. Provider
offices must implement and maintain procedures
that protect against disclosure of confidential patient
information to unauthorized persons. Members
also have the right to receive a copy of and request
corrections to their medical records.
• Providers must abide by California minor consent
laws. Members have the right to be counseled on
their rights to confidentiality, and members’ consent
is required prior to the release of confidential
information unless such consent is not required.
• Choice and involvement in their care. Members have
the right to receive information about their health
plan, services, and providers. Members have the
right to choose their PCP from L.A. Care’s provider
directory. Members also have the right to obtain
appointments within access standards. Members
have the right to talk with their provider about any
care provided or recommended. Members have the
right to discuss all treatment options, and participate
in making decisions about their care. Members
have the right to a second opinion. Members have
the right to speak candidly to their provider about
appropriate or medically necessary treatment options
for their condition. Members have the right to
decline treatment. Members have the right to decide
in advance how they want to be cared for in case
of a life-threatening illness or injury. Members also
have the right to assist with the formulation of their
advanced directives.
• Voice concerns. Members have the right to file a
complaint about L.A. Care and/or its affiliated
providers. ey also have the right to receive care
without fear of losing their benefits. L.A. Care
will help members with the grievance process. If
members don’t agree with a complaint resolution,
they have the right to appeal. Members have the
right to disenroll from L.A. Care whenever they
want. As a Medi-Cal member, members have the
right to request a State Hearing.
• Service outside of L.A. Care’s provider network.
Members have the right to receive emergency
or urgent services as well as family planning and
sexually transmitted disease services outside of their
health plan’s network.
• Members may also have access to Federally Qualified
Health Centers and members that meet certain
criteria may access Indian Health Services Facilities.
• Service and information. Members have the right
to request an interpreter at no charge and not use a
family member or a friend to translate for them.
• Members have the right to access the Member
Handbook and other information in another
language or format, including braille, large size
print, and audio format upon request.
• Know their rights. Members have the right to receive
information about their rights and responsibilities.
Members have the right to make recommendations
about their rights and responsibilities. Members
have the right to receive information on available
treatment options and alternatives, presented in a
manner appropriate to the member’s condition and
ability to understand.
2.8.2 L.A. Care informs Members of their
responsibilities, which are to:
• Act courteously and respectfully. Members are
responsible for treating providers and staff with
courtesy and respect. Members are responsible
for being on time for their visits or calling your
office at least 24 hours before the visit to cancel or
reschedule.
• Give up-to-date, accurate and complete information.
Members are responsible for giving correct
information and relevant information to all of their
providers. L.A. Care. Members are responsible for
getting regular check-ups and telling their provider
about health problems before they become serious.
• Members should follow their provider’s advice and
participate in their care. Members are responsible
for talking about their health care needs with their
provider, developing and agreeing on goals, doing
their best to understand their health problems, and
following the treatment plans and instructions they
both agree on.
• Use the Emergency Room only in an emergency.
Members are responsible for using the emergency room
in case of an emergency or as directed by their provider.
• Report wrong doing. Members are responsible for
reporting health care fraud or wrong doing to
L.A. Care. Members can do this anonymously by
calling the L.A. Care Fraud and Abuse Hotline toll-
free at 1.800.400.4889.
16
2.9 Notice to Members Regarding
Change in Covered Services
Members must be informed about any change in
provision of services. L.A. Care must send written
notification of any change to the member no less than
sixty (60) calendar days, or as soon as possible prior
to the date of actual change. In case of an emergency,
the notification period will be within fourteen (14)
calendar days prior to changes, or as soon as possible.
In some circumstances, when the change includes
termination of a provider’s contract, L.A. Care makes
arrangements for members affected by the termination
to continue care with their provider until their
treatment is completed. In order for L.A. Care to
make these arrangements, the medical conditions must
meet specific criteria; the provider must be willing to
continue seeing the member and must be willing to
accept L.A. Care’s rate of reimbursement.
2.10 Member Grievances and Appeals
L.A. Care Members have the right to file a grievance
and/or appeal through a formal process. Members may
elect a personal representative or a provider to file the
grievance or appeal on their behalf (See Section on
Acting as an Appointed Representative).
2.10.1 Member Grievances
A Grievance is defined as any complaint or dispute,
expressing dissatisfaction with the manner in which
L.A. Care or delegated entities provide health care
services, regardless of whether any remedial action can
be taken. A Grievance may include concerns about
the operations of L.A. Care or its Providers such as:
wait time, the demeanor of health care personnel,
the adequacy of facilities, and the lack of courteous
service. Grievance issues may also include complaints
that a covered health service procedure or item during
a course of treatment did not meet accepted standards
for delivery of health care.
2.10.2 Participating Physician Group Responsibility
L.A. Care does not delegate the grievance or appeal
process to Participating Physician Groups (PPGs)
or any of its contracted providers. erefore, any
expression of dissatisfaction by the member and
or any denial that has been protested must be
forwarded to the L.A. Care Appeals and Grievances
Department within 24 hours of receipt by telephone
at: 1.888.839.9909 by Fax at: 1.213.438.5748 or by
mail at:
L.A. Care
Appeals & Grievances Department
1055 W. 7th Street, 10th Floor
Los Angeles, CA 90017
Electronic grievances or appeals may be filed online
at www.lacare.org, under the “For Members” tab,
“Member Rights/File a Complaint” section.
L.A. Care maintains a comprehensive grievance
resolution system, which includes tracking grievances
by
category, PPG, delegate and by Provider. PPGs are
required to respond to requests for information related
to a grievance within five business days. If a PPG fails
to provide such medical records within five (5) business
days, L.A. Care will be provided access to copy the
appropriate medical records at the expense of the PPG.
e PPG is expected to cooperate with all requests
from the L.A. Care Appeals and Grievances
Department. e PPG should provide a contact
person for communication with the Appeals and
Grievances Department.
PPGs that wish to obtain information on the details
of this process are encouraged to contact L.A. Care’s
Director of Appeals and Grievances.
2.10.2.1 Acting as an Appointed Representative
A member may have any individual, including a
provider, act as his or her representative as long as the
designated representative has not been disqualified
or suspended from acting as a representative in
proceedings before Center for Medicare and Medicaid
Services (CMS), or is otherwise prohibited by law.
e member and representative must complete the
Appointment of Representative Form, in order to
act as a representative. A provider that has furnished
services or items to a member may represent that
member on the appeal; however, the provider may not
charge the member a fee for representation.
Providers may contact the Provider Service Line to request
an Appointment of Representative Form via mail.
2.10.3 L.A. Care’s resolution process for Standard
and Expedited Grievances includes the following
basic steps:
2.10.3.1 Standard Grievance
L.A. Care accepts any information or evidence
concerning a member grievance pertaining to the
Medi-Cal program, orally or in writing, for up to
60 calendar days after the precipitating event.
17
L.A. Care acknowledges, thoroughly investigates,
and resolves standard member grievances within
30 calendar days of the oral or written request.
However, if information is missing or if it is in the
best interest of the member, L.A. Care may extend
the timeframe by an additional 14 calendar days.
2.10.3.2 Expedited Grievance
L.A. Care provides expedited review of grievances
involving an imminent and serious threat to the
health of the enrollee, including, but not limited to,
severe pain, potential loss of life, limb or major bodily
function (“urgent grievances”).
A member or a member’s representative may request
an expedited grievance.
L.A. Care responds to expedited grievances within
72 hours of receipt of the oral or written request.
2.10.4 Member Appeals
A member may file an appeal when he or she does
not agree with L. A. Care’s decision to: stop, suspend,
reduce, deny a service, or deny payment for services
provided. e member must submit the appeal to
L.A. Care. Upon review of the appeal, L.A. Care
will make a determination and notify the member in
writing of the decision.
2.10.4.1 Member Appeal Procedure – Medi-Cal
A member has the right to appeal directly to L.A. Care
for all decisions to modify or deny a request for Medi-Cal
services. A provider, acting as the member’s representative,
may also appeal a decision on behalf of the member.
If a delegated PPG’s appeal process results in a
denial, deferral, and/or modification with which the
member is still dissatisfied, the member or Authorized
Representative, may request a formal appeal to L.A. Care
for a higher-level review.
Members and providers, on behalf of members, may
also appeal L.A. Care’s decision to modify or deny a
service request. e appeal request is reviewed by a
physician or physician reviewer not involved in the prior
determination. (is does not apply to the retrospective
claims review/provider dispute resolution process.)
Member requested appeals may be initiated orally or
in writing.
Members, and providers on behalf of members,
have the right to appeal an adverse utilization review
determination.
If the physician reviewer determines he/she is not
qualified, he/she will consult with another qualified
professional prior to making a determination.
A determination will be made within the established
timeframe from receipt of the appeal and necessary
information.
Written appeal acknowledgment and a determination
notification will be sent to the member and provider
via mail, within 72 hours after the receipt of the
reasonably necessary information and requested by
L.A. Care to make the appeal determination.
e notification will include:
• e final determination
• A statement setting forth the specific medical and
scientific reasons for the determination, and a
description of alternative treatments, supplies, and/
or services as appropriate
• Reasons other than medical necessity (e.g., non-
covered benefits etc.) will include the statement of
benefit structure
• Instructions for appealing further to the Department
of Managed Health Care (DMHC), to include
DMHC’s address and toll free phone number, as
applicable
• e phone number and extension of the L.A. Care
physician reviewer
Determinations that cannot be completed within the
30 calendar days for standard appeals, or within
72 hours for expedited appeals, must be forwarded to
DMHC for final resolution.
2.10.5 State Fair Hearings
Additional requirements specific to the management
of Medi-Cal Member Appeals.
Medi-Cal Members and their representative may
contact the California Department of Social Services to
request a State Fair Hearing or an Expedited State Fair
Hearing at any time during the appeal process, up to 90
days from receipt of the denial/modification letter.
Medi-Cal Members also may contact the Medi-Cal
Managed Care Office of the Ombudsman to request
assistance with an appeal.
Contact information for the Medi-Cal Managed Care
Ombudsman is as follows:
Medi-Cal Managed Care Ombudsman
1.888.452.8609 (many languages)
18
To submit the request in writing, a member may send
a letter to the following address:
California Department of Social Services
State Fair Hearing Division
P.O. Box 944243, MS 19-37
Sacramento, CA 94244-2430
To access the online site go to:
http://www.dhcs.ca.gov/services/medi-cal
2.10.6 Independent Medical Review
A member may request an Independent Medical
Review (IMR) through the Department of Managed
Health Care (DMHC) to obtain an impartial review
of a denial decision concerning the following:
• e medical necessity of a proposed treatment
• Experimental or investigational therapies for a life-
threatening or seriously debilitating disease
or condition
• Claims for out-of-plan emergency or urgent
medical services
e application and process for requesting an IMR is
always included with the L.A. Care’s appeal response
notification letter resulting from upholding a denial or
modification of a request for service.
For assistance regarding an IMR, the DMHC has a
toll-free telephone number (1.888.466.2219) and
a TDD line (1.877.688.9891) for the hearing and
speech impaired.
e DMHC Internet Website has IMR application
forms and instructions online.
To access the online site go to the DMHC,
Independent Medical Review page:
https://www.dmhc.ca.gov/FileaComplaint/
SubmitanIndependentMedicalReviewComplaint.aspx
2.10.7 Member Appeal Procedure –
Overlapping Benefits
For benefits covered by both Medicare and Medi-Cal,
the Member retains the right to a State Fair Hearing,
regardless of the designated pathway.
Medi-Cal issues follow the Medi-Cal Appeals
procedure. e final available determination possible is
that made in a State Fair Hearing.
Medicare issues follow the Medicare Appeals
procedure. Members, or their authorized
representative, who want to appeal the outcome of the
appeal decision may contact the DHCS, to request a
State Fair Hearing or an Expedited State Fair Hearing.

19
3.0 Access to Care
is section summarizes the access to care requirements for L.A. Care’s Providers in the participating provider
network, including Participating Physician Groups (PPGs) and their affiliated provider networks.
3.1 Responsibility of Participating Providers
All Providers are responsible for fulfilling the access to care standards outlined in this section. L.A. Care monitors
the ability of its Members to access each service type (left column) according to the specified L.A. Care Access
Standard (right column).
3.2 Access to Care Requirements (Primary Care and Specialty Care Physicians,
Behavioral Health and Ancillary Providers)
Primary Care Provider (PCP) Appointment Standards:
Type of Service Standard
Routine Primary Care
Appointment (Non-Urgent)
Services for a symptomatic patient who
does not require immediate diagnosis and/
or treatment.
≤ 10 business days of request
Urgent Care
Services for a non-life threatening
condition that could lead to a potentially
harmful outcome if not treated in a
timely manner.
≤ 48 hours of request if no authorization is required
Emergency Care
Services for a potentially life threatening
condition requiring immediate medical
intervention to avoid disability or serious
detriment to health.
Immediate, 24 hours a day, 7 days per week
Preventative health
examination (Routine)
≤ 10 business days of request
First Prenatal Visit
A health evaluation for a pregnant
member with no acute medical problems
≤ 14 calendar days of request
Staying Healthy Assessment
Initial Health Assessment and Individual
Health Assessment and Individual
Health Education Behavioral Health
Assessment (IHEBA)
Members >18 months of age: ≤ 120 calendar days from when
the member becomes eligible.
Members <18 months of age: ≤60 calendar days of enrollment
or within periodicity timelines as established by the American
Academy of Pediatrics (AAP) for ages two and under, whichever
is less.
20
Primary Care Provider (PCP) Appointment Standards:
Type of Service Standard
In-Office Waiting Room Time
e time after a scheduled medical
appointment a patient is waiting to be taken
to an exam room to be seen by
the practitioner.
Within 30 minutes
Specialty Care Provider (SCP) Appointment Standards:
Routine Specialty Care
Physician Appointment
≤ 15 Business days of request
Urgent Care
Services for a non-life threatening
condition that could lead to a potentially
harmful outcome if not treated in a
timely manner.
≤ 48 hours of request if no authorization is required
≤ 96 hours if prior authorization is required
Ancillary Care Appointment Standards:
Non-Urgent Ancillary Appointment ≤ 15 business days of request
Behavioral Health Care Appointment Standards:
Routine Appointment
(includes non-physician
behavioral health providers)
< 15 Business days of request (Physicians)
≤ 10 business days of request (Non-Physicians)
Urgent Care
Services for a non-life threatening
condition that could lead to a potentially
harmful outcome if not treated in a
timely manner.
≤ 48 hours of request
Life reatening Emergency
Services for a life-threatening condition
where the member is at immediate risk of
self- harm or harm to others
Immediately
Non-Life reatening Emergency
Services for a non-life threatening
condition where the risk of self-harm
or harm to others is not imminent but
requires a safe environment
≤ 6 hours of request

21
Primary Care Provider (PCP) Appointment Standards:
Type of Service Standard
Emergency Services Immediate, 24 hours a day, 7 days per week
After Hours Care Accessibility Standards:
After Hours Care
Physicians (PCP, Behavioral Health Provider
and Specialists, or covering physician) are
required to provide 24 hours a day, 7 days
per week coverage to members.
Physicians, or his/her on-call coverage
or triage/screening clinician must return
urgent calls to member, upon request
within 30 minutes.
*Clinical advice can only be provided by
appropriately qualified staff, e.g., physician,
physician assistant, nurse practitioner or RN.
• Automated systems must provide emergency 911 instructions
• Automated system or live party (office or professional exchange
service) answering the phone must offer a reasonable process
to connect the caller to the PCP, Behavioral Health Provider,
Specialist or covering practitioner, or offer a call-back from
the PCP, Behavioral Health Provider, Specialist, covering
practitioner or triage/screening clinician within 30 minutes
• If process does not enable the caller to contact the PCP,
Behavioral Health Provider, Specialist or covering practitioner
directly, the “live” party must have access to a practitioner or
triage/screening clinician for both urgent and non-urgent calls.
Practitioner Telephone Responsiveness:
Speed of Telephone Answer
(Practitioner’s Office)
e maximum length of time for
practitioner office staff to answer the phone.
Not to Exceed (NTE) 30 seconds
Call Return Time (Practitioner’s Office)
e maximum length of time for PCP,
Behavioral Health Provider, Specialist offices,
covering practitioner or triage/screening
clinician to return a Member call.
*Clinical advice can only be provided by
appropriately qualified staff, e.g., physician,
physician assistant, nurse practitioner or RN.
< 30 minutes
3.3 Monitoring
L.A. Care regularly monitors and audits the appointment and access standards identified in this Section, and others
per applicable rules, regulations, contracts, and guidance. e PPG and/or Provider, as applicable, are responsible
for responding to any appointment and/or access deficiencies identified by L.A. Care Health Plan review methods,
including the following:
• Access to care studies
• Facility Site Review (FSR)
• Exception reports generated from Member grievances
• Medical records review
• Random Member surveys
• Feedback from PCP regarding other network services (i.e., pharmacies, vision care, hospitals, laboratories, etc.)
• Provider office surveys or visits
22
4.0 Scope of Benets
Principal Benets and Coverages
e below listed benefits and services are available
for prevention, diagnosis, and treatment of illness
or injury (including ancillary services). Please refer
to the Prior Authorization section of this Provider
Manual for authorization requirements to understand
benefits and service coverage according to the contract
and service area or contact the L.A. Care Provider
Services line at 1.866.522.2736.
• Provider/Practitioner Services
• Preventive Health Services
• Family Planning
• Maternity Care
• Hospital Services
• Outpatient Mental Health Services
• Substance Use Disorder Preventive Services/
Screening, Brief Intervention and Referral to
Treatment (SBIRT)
• Behavioral Health Treatment for Autism Spectrum
Disorder
• Prescription Drugs and Medications
• Vision Services
• Laboratory X-ray, and Prescribed Services
• Cancer Clinical Trials
• Durable Medical Equipment
• erapeutic Formulas
• Enteral Nutrition Products
• Diabetic Equipment and Supplies
• Long Term Services and Supports (LTSS)
• Home Health Care
Hospice Care
• Emergency Care
• Medical Transportation
In Los Angeles County, L.A. Care Health Plan
is responsible for Long Term Care (LTC) coverage.
Additional information can be found in the
LTSS section.
For custodial authorization or outpatient services
needed while in custodial level of care, please fax all
requests to the Prior Authorization Department at
1.213.438.5777
Principal Exclusions and Limitations
Services that are not covered by L.A. Care
Health Plan or Medi-Cal
ese services will not be provided by L.A. Care or
Regular Medi-Cal (fee-for-service program) and are
excluded from coverage:
• Experimental or investigational drug, device, or
procedures (unless approved)
• Over-the-counter (OTC) drugs (unless approved)
• Cosmetic surgery, except when required to repair
trauma or disease-related disfigurement
• Personal comfort or convenience items
• Private duty nurses (except when medically necessary)
• Elective circumcisions
• Audiology Services not performed/prescribed by a
provider in a provider office
• Speech erapy Services
• Podiatry Services
• Services outside the United States, except Emergency
services requiring hospitalization in Canada and Mexico
Excluded (Carve-Out) Services
Medi-Cal beneficiaries enrolled in a managed care plan
obtain most of their benefits from their health plan.
Medi-Cal services not covered by a health plan are
referred to as “excluded” or as “carve-out.”
Excluded services can only be rendered by a Medi-Cal
enrolled Provider/Practitioner and must be billed
through the Medi-Cal Fee-for-Service (FFS) system.
In most cases, beneficiaries remain enrolled in their
health plan while receiving these excluded services.
Coordination of carved out services is part of the role
of the primary care provider. Below is a list of excluded
services that may be obtained while a beneficiary
remains enrolled in a managed care plan:
• California Children’s Services (CCS)
• Mental Health
°
L.A. Care does not cover hospital care and
specialty mental health care. Medi-Cal FFS or the
County Department of Mental Health (DMH)
provides these services.
• Alcohol and Drug Treatment
• Dental Services
• Directly Observed erapy for Tuberculosis (TB)
• Women, Infants, and Children Supplemental Food
Program (WIC)
• Local Education Agency Services
• End of Life Services
°
Contact the Medi-Cal Member and Provider
Helpline at 1.800.541.5555 (outside of
California, please call 1.916.636.1980 to learn
about these services.
23
Exceptions for Services Not Covered by
L.A. Care Health Plan or Regular Medi-Cal
Assembly Bill X3 5 (Evans, Chapter 20, Statutes of
2009) added Section 14131.10 of the Welfare and
Institutions Code (W&I Code) to exclude several
optional benefits from coverage under the Medi-Cal
Program for members 21 years and older, effective
July 1, 2009. Please refer to the Medi-Cal Provider
Manual on the Department of Health Care Services
website (http://files.medi-cal.ca.gov/pubsdoco/
manuals_menu.asp) for a description of optional
benefit exclusions and exemption criteria.
Nurse Advice Line (NAL)
L.A. Care provides a Nurse Advice Line (NAL) free of
charge. Members can call 1.800.249.3619 (TTY 711)
24 hours a day, 7 days a week. Providers are
encouraged to share this number with L.A. Care
members. e NAL is intended to provide members
with general health advice and information,
understand health concerns, understand prescriptions,
health test results, and seek the appropriate level
of care. e line is staffed with RNs who follow
medical doctor reviewed algorithms when triaging
symptomatic calls. An audio library of more than
1,000 easy to follow health topics is provided through
this service. Members can also chat live with a nurse
by logging into their L.A. Care Connect online
member account.
Other Important Numbers
Hearing or speech impaired members can contact
L.A. Care NAL through the California
Telecommunications Relay Service at TTY 711.
Medi-Cal Members with one of our Plan Partners can
call the Nurse Advice Line at:
• Anthem Blue Cross: 1.800.224.0336 or
TTY/TDD 1.800.368.4424
• Care 1
st
Health Plan: 1.800.609.4166 or
TTY/TDD 1.800.735.2929
• Kaiser Permanente: 1.888.576.6225
Non-Emergency Medical Transportation
L.A. Care Medi-Cal members can access Non-
Emergency Medical Transportation (NEMT) when
they cannot get to their medical appointment by car,
bus, train, or taxi, and the plan pays for your medical
or physical condition.
NEMT is an ambulance, litter van or wheelchair
van. NEMT is not a car, bus, or taxi. L.A. Care
Health Plan allows the lowest cost NEMT for the
member’s medical needs when they need a ride to
their appointment. at means, for example, if a
wheelchair van is able to transport the member,
L.A. Care Health Plan will not pay for an ambulance.
NEMT can be used when:
• Medically needed;
• e member can’t use a bus, taxi, car or van to get to
their appointment;
• Requested by a L.A. Care Health Plan provider; and
• Approved in advance by L.A. Care Health Plan.
Scheduling NEMT
To request NEMT, please call L.A. Care Health
Plan Member Services 1.888.839.9909 (TTY 711) at
or LogistiCare at 1.866.529.2141 at least
five (5) business days (Monday-Friday) before the
appointment. Or call as soon as you can when you
have an urgent appointment. Please instruct the
member to have their member ID card ready when
you or they call.
Services can be requested directly by calling LogistiCare
at 1.866.529.2141 at least five (5) business days
(Monday-Friday) before the appointment and
selecting one of the following transportation options:
Press 1 for Ambulatory/Wheelchair Reservations
Press 2 for Ambulatory/Wheelchair “Where is my
ride?” (Scheduling a Return Ride)
Press 3 for Gurney/Ambulance
Press 8 for Information in Spanish or dial
1.866.529.2142
Limits of NEMT
ere are no limits if you meet the terms above.
What Doesn’t Qualify for NEMT?
Getting to your medical appointment by car, bus,
taxi, or plane. Transportation will not be provided if
the service is not covered by the health plan. A list of
covered services is in this member handbook (or also
called an EOC).
Cost to Member
ere is no cost when transportation is authorized by
L.A. Care Health Plan.
24
5.0 Utilization
Management
is section summarizes L.A. Care’s Medical
Management Utilization Management (UM) processes
for its direct contract Provider network, including
direct contract Participating Physician Groups (PPGs),
direct contract physicians, hospitals and ancillary
providers, as applicable.
L.A. Care UM functions and activities vary depending
on specific contractual agreements with each contracted
PPG, provider, and hospital. Please review your Medi-Cal
Program contract with L.A. Care which outlines the
Division of Financial Responsibility (DOFR). You may
contact L.A. Care’s Provider Services Unit (PSU) line at
1.866.522-2736 to connect you with the appropriate
department to respond to your UM questions. You may
also contact the Medical Management/UM Department
at 1.877.431.2273.
L.A. Care performs UM activities which are
consistent with Federal and State regulations, state
contracts, and other L.A. Care policies, procedures,
and performance standards as set forth in L.A. Care’s
UM Program Document.
Regarding performance standards, L.A. Care adopts
evidence-based clinical practice guidelines from
recognized sources for selected conditions relevant to
our membership for the provision of non-preventive
health services for acute, and chronic medical
conditions, as well as for preventive and non-preventive
behavioral health services. Clinical Practice Guidelines
are presented for review and approval to L.A. Care’s
Physician Quality Committee (PQC) at least every
two years, and updated as needed. Clinical practice
guidelines are disseminated to practitioners via the
L.A. Care website and on a regular basis via L.A. Care
Physician Quality Improvement Liaison Nurse (PQIL)
site visits. Practitioners are also informed through a
practitioner newsletter when clinical practice guidelines
or updates are available. Guidelines compliance is
measured by several departments, including Quality
Improvement (QI), UM, Facility Site Review (FSR)
and Health Education. Annually, the QI Department
measures compliance with utilization of clinical
practice guidelines. Performance is measured by
Healthcare Effectiveness Data and Information Set
(HEDIS) rates and a medical record review.
L.A. Care UM department is staffed with professional
registered nurses and paraprofessionals who are available
to provide support to PPGs and Providers with UM
activities including but not limited to the following:
• Benefit interpretation
• Outpatient and inpatient referral management
• Coordination of care and services for linked
programs (California Children’s Services,
Department of Developmental Services, Early Start,
Local Education Agency, etc.)
• Coordination of benefits
• Targeted case management (comprehensive
and catastrophic)
• Complex case management
• Education of PPG and/or contracted providers on
policies, procedures and legislative updates
5.1 Goal And Objectives
Goal
e goal of L.A. Care’s UM Program is to ensure
and facilitate the provision of appropriate medical
and behavioral health care and services to L.A. Care
Members. e program is designed to monitor,
evaluate and support activities that continually
improve access to and the quality of member medical
care provided to L.A. Care Members.
Objectives
e UM Program’s objectives are designed to provide
mechanisms that assure the delivery of quality health
care services and to optimize opportunities for process
improvement through the following:
• Managing, evaluating, and monitoring the provision
of healthcare services rendered to L.A. Care
Members to enhance access to, and provision of,
appropriate services.
• Facilitating communication and developing
partnerships between PPGs, Providers, Practitioners,
Members and L.A. Care.
• Developing and implementing programs to
encourage preventive health behaviors that can
improve quality outcomes.
• Assisting PPGs, Providers, and Practitioners in
providing ongoing medical care for Members with
chronic or catastrophic illness.
• Developing and maintaining effective relationships
with linked and carved-out service Providers available
to L.A. Care Members through county, state, federal,
and other community-based programs to ensure
optimal care coordination and service delivery.
• Facilitating and ensuring Continuity of Care (COC)
for L.A. Care Members within and outside of
L.A. Care’s network.
25
• Integration with Quality Improvement
°
e UM Program has multiple quality operations
processes to ensure that quality of care service-
oriented interventions are initiated and carried
out. Linkage between the UM Program and the
QI Program is supported through committee
representation by UM Program management and
by presenting executive level summary of pertinent
UM documents to the L.A. Care Quality of Care
(QOC) Committee.
°
Additionally, UM integration with quality
operations supports activities to capture utilization
trends or patterns and is measured by, but not
limited to the following:
Inter-Rater Reliability (IRR)
Member and Provider Satisfaction with the
UM Experience
Referral of identified potential quality issues
for review to the QI Department for follow-
up in accordance with established procedures
(including sentinel or adverse event reporting)
• Ensuring a process for UM that is effective and
coordinated through committees, work groups and
task forces with the involvement and cooperation
of experts in all fields of medicine, management,
patient advocacy and other relevant fields.
• Providing leadership to PPGs, Providers, and
Practitioners by developing and recommending
changes and improvements in programs and
processes resulting from collection and analysis of
utilization data.
• Ensuring that UM decisions are made independent
of financial incentives or obligations. L.A. Care’s
Policy Prohibiting Financial Incentives for
Utilization Management Decision-makers states that
Utilization Management decisions are based only on
appropriateness of care and service and the existence
of coverage. ere are no rewards or incentives for
practitioners or other individuals for issuing denials
of coverage, service, or care. ere are no financial
incentives for Utilization Management decision-
makers to encourage decisions that would result in
underutilization.
• Monitoring the provision of health assessments and
basic medical case management to all Members,
PPGs, Providers, and Practitioners.
5.2 Scope of Service
e scope of L.A. Care’s Medi-Cal UM Program
includes all aspects of health care services delivered
at all levels of care to L.A. Care Medi-Cal members.
L.A. Care offers a comprehensive health care delivery
system along the continuum of care, including urgent
and emergency services, ambulatory care, preventive
services, hospital care, ancillary services, behavioral
health (mental health and addiction medicine), home
health care, hospice, rehabilitation services, skilled
nursing services, and care delivered through selected
waiver programs, and through linked and carved
out services.
L.A. Care administers the delivery of health care
services to its members through different contractual
agreements. L.A. Care’s services are administered
through different contractual arrangements with
PPGs which may include delegation of some or all
UM functions. L.A. Care and L.A. Care’s PPGs shall
provide or arrange for all medically necessary covered
services for members.
If medically necessary services are not available within
L.A. Care’s contracted networks, contracts with non-
participating provider are initiated on an individual
basis to ensure availability of medically necessary care
and services in accordance with benefit agreements.
At a minimum the UM Program includes the
following:
• Delivers medically necessary services at the
appropriate level of care, including inpatient and
ambulatory settings
• Provides services consistent with the benefits
provided by the Plan’s Medi-Cal Program
• Provides a comprehensive analysis of care by
identifying under and overutilization patterns by
network contracted PPGs, hospitals and ancillary
providers
• Reviews care and identifies trends that positively
and negatively impact the quality of care provided
to the members
• Defines, monitors, and trends medical practice
patterns impacting members’ care
• Ensures that appropriate medical review guidelines
are available and used by UM personnel
• Identifies, develops, revises, and implements
appropriate policies, procedures, processes, and
mechanisms for UM that can be used to evaluate
medical necessity for requested services on a timely
and regular basis
• Defines, adopts and distributes evidence based
criteria utilized in the utilization management
process as well as instruct contracted institutions,
physicians, and other health care clinicians regarding
26
the criteria and methods utilized in the approval and
review processes
• Provides the health plan network with information
related to effective mandated information
system and communications for the monitoring,
management, and planning of medical services
• Ensures the provision of health care services by
network institutions, physicians, and other health
care clinicians unless otherwise mandated by
regulatory standards
• Ensures coordination and COC for members
receiving linked and carved out services/programs
including, but not limited, California Children’s
Services (CCS), Regional Centers, Genetically
Handicapped Persons Program (GHPP) or Mental
Health Services
• Ensures that guidelines, standards, and criteria set
by governmental and other regulatory agencies are
adhered to as appropriate
• Facilitates consistent practice patterns among
institutions, physicians, and other health care
clinicians
• L. A. Care Health Plan by offering feedback to
the PPGs and providers to assist in optimizing
appropriate medical practice patterns
• Provides case management services to ensure cost
effective ongoing care at the appropriate level
• Utilizes information in member and physician
satisfaction surveys to develop quality improvement
activities as appropriate
• Conducts inter-rater reliability of physician and
non-physician reviewers to assess determinations
made as part of the UM process
5.2.1 Policy Prohibiting Financial Incentives for
Utilization Management Decision-makers
UM decisions are based only on appropriateness of
care and service and the existence of coverage. ere
are no rewards or incentives for practitioners or other
individuals for issuing denials of coverage, service,
or care. ere are no financial incentives for UM
decision-makers to encourage decisions that would
result in underutilization.
5.2.2 Required Reporting from UM
L.A. Care contracted PPGs’ UM departments shall
monitor, report, and address the following services to
L.A. Care and its appropriate committee structures.
e services include, but at not limited to:
• Potentially fraudulent or abusive practices
• Potential under and overutilization
• Coordination of care for results or facilitation
• Opportunities for improvement
• Breaches of adherence to confidentiality and Health
Insurance Portability and Accountability Act
(HIPAA) policies (these are referred to L.A. Care’s
Compliance, Privacy Officer)
• Potential quality issues identified through UM
activities
• Identified barriers to accessibility and availability
of services
5.3 Delegation of Utilization
Management
L.A. Care has a formal process by which specific
Utilization Management functions are delegated to
other organizations including PPGs/Specialty. [See
PPGs Service Agreement — Delegation of UM
Functions by National Committee for Quality
Assurance (NCQA) UM Standards].
L.A. Care’s Clinical Assurance Department evaluates all
proposed delegates using a formal process that assesses
the organization’s systems, processes and capabilities
according to defined criteria. Utilization Management
is not delegated until L.A. Care determines, in its sole
judgment, that the delegate is capable of performing
the delegated functions in a manner acceptable to
L.A. Care. L.A. Care’s UM delegation standards and
oversight monitoring activities are described more fully
in Delegation Agreement.
e scope of delegation for each delegate is defined
in a written delegation agreement. UM delegation is
defined in terms of:
• Standard delegation
• Extended delegation
Standard delegation is defined as delegation to perform
UM activities defined in the delegation agreement and
noted in the PPG Division of Financial Responsibility
(DOFR) as “PPG Risk.” Extended delegation is
defined as delegation to perform activities defined in
the delegation agreement and noted in the PPG DOFR
as “PPG Risk” and “Hospital Shared Risk Pool”.
e agreement also defines the oversight process and
delegate reporting requirements. Delegates are not
permitted to sub-delegate any functions without
L.A. Care’s consent. e ability for an organization
to maintain its status as a delegate depends solely on
27
the organization’s capacity, in L.A. Care’s judgment,
to continue to perform in a manner consistent
with the defined criteria. Oversight of delegation
includes periodic assessments throughout the year by
designated staff based, in part, on review of required
reports submitted by the delegate.
All delegates are formally reevaluated annually.
e scope of the reevaluation may depend on the
organization’s Knox-Keene License or other regulatory
status and NCQA accreditation or certification status
and includes conducting oversight activities, reporting
results, developing Corrective Action Plans (CAPs) and
monitoring progress in implementation of the CAPs.
L.A. Care’s Clinical Assurance Department is
responsible for making sure that the delegated
activities are performed in a manner consistent
with the delegation agreement, L.A. Care criteria,
applicable regulatory requirements and accreditation
standards. L.A. Care provides ongoing assistance,
guidance, and oversight in furtherance of this goal.
Should L.A. Care determine that an organization is
not performing any portion of the delegated functions
in a manner consistent with the delegation agreement,
L.A. Care criteria, applicable regulatory requirements,
or applicable accreditation standards L.A. Care may
institute corrective action or revoke the delegation in
whole or in part.
Non-compliance issues will be brought to the
attention of the Compliance Officer for recommended
actions. Non-compliance issues directly impacting
member care will be brought to the attention of the
Chief Medical Officer for recommendations which
could include suspension of membership, up to, and
including immediate contract termination.
If L.A. Care withholds or withdraws delegated status
for Utilization Management from a PPG/Specialty
Provider, L.A. Care’s UM Department shall assume
the level of UM activity appropriate to the new non-
delegated PPG/Specialty Provider. L.A. Care reserves
the right to continue to delegate UM to the PPGs/
Specialty Providers if they meet L.A. Care’s standards
for delegation. L.A. Care’s Clinical Assurance
Department will provide consultation to the PPG/
Specialty Provider and may actively participate with
the PPG/Specialty Provider to assist the PPG/Specialty
Provider to come into compliance with a UM
delegated function prior to L.A. Care’s revocation of a
UM delegated status.
5.4 Utilization Management
Delegation Status
PPG/Specialty Provider audited for UM delegation
will be designated a delegation status after the
due diligence review, annually and as a result of a
supplemental or focused audit findings. Delegation
status includes standard and extended delegation.
Standard is defined as delegation to perform UM
activities defined in the delegation agreement and noted
in the PPG DOFR as “PPG Risk”. Extended delegation
is defined as delegation to perform activities defined in
the delegation agreement and noted in the PPG DOFR
as “PPG Risk” and “Hospital Shared Risk Pool”.
PPG delegation status may be impacted by PPGs
contractual relationship with L.A. Care. All PPGs
will be audited for compliance with the UM related
regulatory requirements. Non-compliance may
result in supplemental audits or focused audits to
ensure compliance.
5.4.1 Delegates with NCQA accreditation
If the delegate or delegate’s sub-delegates are NCQA
Accredited or NCQA Certified or NCQA-Recognized,
the delegate is eligible for automatic credit if it meets
all other automatic credit criteria for the those areas
specific to NCQA. is does not apply to, or relieve
the delegates from, L.A. Care’s oversight process.
5.5 Utilization Management Delegation
Monitoring and Oversight
L.A. Care’s Clinical Assurance Department is
responsible for evaluating the PPGs/Specialty Providers
ability to perform the delegated activities including an
initial review to assure that the PPG/Specialty Provider
has the administrative capacity, task experience, and
budgetary resources to fulfill its responsibilities.
L.A. Care will monitor and oversee the delegated
UM activities of the PPGs/Specialty Providers and
their networks to ensure ongoing compliance with
State, Federal, NCQA and L.A. Care requirements.
UM data submitted to L.A. Care by PPGs/Specialty
Providers will be analyzed and areas for improvement
identified and managed through the CAP process with
the PPGs/Specialty Providers or through the Quality
Improvement process, as appropriate, in accordance
with L.A. Care’s organizational sanction policies.
L.A. Care will perform different types of audits and
oversight activities of PPGs/Specialty Providers as
appropriate. e UM data and oversight activities will
include, but not be limited to the following:

28
5.6 Utilization Management and Case
Management Reports
PPGs will submit UM and Case Management (CM)
reports as defined in the delegation agreements, via
the Clinical Assurance Secure File Transfer Protocol
(SFTP) site, and email a screen shot of uploaded
reports to clinicalassurance@lacare.org. Specialty
Providers will submit reports as defined in the delegation
agreements, via the Provider Vendor Management SFTP
site, and email a screen shot of uploaded reports to
clinicalassurance@lacare.org.
L.A. Care will utilize encounter data, summary reports,
and supplemental reports provided by PPGs/Specialty
Providers to track, trend, and report UM activities as
required by regulatory entities, contracted requirements,
and accreditation standards. ese reports, combined
with information obtained via site visits and audits,
will be used to accomplish UM delegated oversight
functions. Additional oversight reporting may be
required to be sent to the Delegation Oversight Unit
for ongoing monitoring. L.A. Care reviews PPGs/
Specialty Providers UM decision-making by auditing
denial determinations on a periodic basis. Modification
and Denial Notice of action letters and medical records
utilized in the modification or denial determination
must be sent to L.A. Care’s Clinical Assurance
Department upon request via the SFTP site, with a
screen shot of the uploaded letters to clinicalassurance@
lacare.org.
L.A. Care will analyze the reports and present the
results to the PPGs/Specialty Providers via quarterly
feedback provided by L.A. Care’s Clinical Assurance
Performance Monitoring Nurse Specialists. e
goal of performing plan and group specific analysis
is to monitor utilization activities, member access
to care, and to validate and compare to community
norms/benchmarks. Any variance(s) or trends will be
reviewed and discussed at the Utilization Management
committee/sub-committee meetings, and periodically
at the QOC and Internal Compliance Committee for
recommendations.
A list of the reporting requirements can be found in
each PPGs/Specialty Providers Delegation Agreement.
e following table shows a complete description of
required reports, due dates, and required format. PPGs
with Medi-Cal L.A Care (MCLA) line of business are
required to submit the following reports (*Certain
Specialty Providers with MCLA line of business are
required to submit reports with asterisk):
Report Due Date Submit To
Required
Format
Applicable to All Lines
of Business (LOB)
*UM Program Description
e UM Program describes UM, CM, Care
Coordination Programs and Processes, and the medical
and behavioral health aspects of the Program.
Annually
Feb 15
Report Previous
Year
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Narrative
Applicable to All LOB
*UM WorkPlan
Work Plan goals and
planned activities.
Annually
Feb 15
Report Current
Year
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Quarterly ICE
Reporting
template
provided by
L.A. Care
Applicable to All LOB
*UM Program Evaluation
Report that provides a detailed description of
utilization activities, delegated activities, and strategic
initiatives accomplished during the past year. is
report is incorporated into the Q4 UM ICE Report,
no need to submit a separate report.
Annually
Feb 15
Report Previous
Year
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Quarterly ICE
Reporting
template
provided by
L.A. Care

29
Report Due Date Submit To
Required
Format
Applicable to All LOB
*UM ICE Quarterly Report
Report that provides a detailed description of utilization
activities, delegated activities, and strategic initiatives
accomplished during the quarter
Quarterly
1
st
Qtr – May 15
2
nd
Qtr – Aug 15
3
rd
Qtr – Nov 15
4
th
Qtr – Feb 15
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Quarterly ICE
Reporting
template
provided by
L.A. Care
Applicable to All LOB
*QI Continuity & Coordination
of Care Report (COC-TOC)
Number of terminated primary care and specialty care
providers; number of members requesting assistance for
COC (COC) with terminated providers
COC (NCQA NET 5 Element A & B)
Tracking log of members requesting COC due to
provider termination:
• Total # of termed Primary Care Physicians (PCP)/
SCP
• Total # of members requesting assistance for COC
with termed PCP/SCP
• Total # of members allowed to continue access to
termed PCP/SCP
Tracking log of members requesting COC when
benefits end: (NCQA QI 8 Element D)
• Total # of members whose benefit coverage ended while
still needing care
• Total # of members assisted in transition to other care
when benefit coverage ended.
Quarterly
1
st
Qtr – April 15
2
nd
Qtr – July 15
3
rd
Qtr – Oct 15
4
th
Qtr – Jan 15
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Reporting
template
provided by
L.A. Care

30
Report Due Date Submit To
Required
Format
Applicable to All LOB
*UM Monthly Activity
Report and Logs
*UM Monthly Activity Report: Delegates are required
to complete our UM Monthly Activity Report
*UM Monthly Activity Logs:
1. *Referral/Authorization Approval Log: Delegates have
the option of using our template or adding the fields
found in our template (if missing) to their own reporting
log. Submitted log must contain fields found in our
template, as these fields will be needed for NCQA.
2. *Denial/Modification/Termination Log: Delegates have
the option of using our template or adding the fields
found in our template (if missing) to their own reporting
log. Submitted log must contain fields found in our
template, as these fields will be needed for NCQA.
3. Bed Days Report- Acute Inpatient Log, includes
LTAC: Delegates may use their own template, as long
as they report member information.
4. Bed Days Report- Inpatient Admissions Greater than
10 days LOS: Delegates have the option of using our
template or adding the fields found in our template
(if missing) to their own reporting log. Submitted log
must contain fields found in our template.
5. Bed Days Report-Sub-Acute SNF Log: Delegates
may use their own template, as long as they report
member information.
6. ESRD/Dialysis Log: Delegates may use their own
template, as long as they report member information.
7. HIV/AIDS Encounters Log: Delegates may use
their own template, as long as they report member
information.
8. Major Organ Transplant Requests Log: Delegates
may use their own template, as long as they report
member information.
9. Case Management/Care Coordination Log:
Delegates need to use our template, do not make any
modifications to our template.
Service Logs to be maintained, but to be submitted
only upon request:
• Sterilization Log • Hospice Referral
• TB (New Diagnosis) Log • Standing Referrals
• CPSP (Pregnancy) Log • Specialty Referrals
• Drug-Alcohol Referral
Linked Services Logs to be maintained, but to be
submitted only upon request:
• CCS**
• New TB Referrals to Direct Observed erapy (DOT)**
• Non-CCI SNF admissions, Custodial (Long Term) Care
Log**
• AIDS In-Home & Community Based Waivers**
• Medi-Cal Waivers**
**Not applicable with CMC Line of Business
Monthly
Every 15th of the
month
Previous month’s
data
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Reporting
template
provided by
L.A. Care
Logs need to
be submitted
in excel
format,
L.A. Care
needs to be
able to filter
and sort
through fields

31
Report Due Date Submit To
Required
Format
MCLA LOB ONLY
COC with FFS Provider for Transitional SPDs
Report
(COC-SPD):
COC requests related to members transitioning from
MediCal Fee for Service (FFS) to MediCal Managed
Care. Aid codes: 10, 14, 16, 20, 24, 26, 36, 60, 64, 66,
1E, 1H, 2E, 2H, 6A, 6C, 6E, 6G, 6H, 6J, 6N, 6P, 6V
Quarterly
1
st
Qtr – April 15
2
nd
Qtr – July 15
3
rd
Qtr – Oct 15
4
th
Qtr – Jan 15
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Reporting
template
provided by
L.A. Care
MCLA LOB ONLY
Dental General Anesthesia Services Report (DGAS):
Dental general anesthesia services provided by a
physician in conjunction with dental services for
managed care beneficiaries in hospitals, ambulatory
medical surgical settings, or dental offices.
Quarterly
1
st
Qtr – April 15
2
nd
Qtr – July 15
3
rd
Qtr – Oct 15
4
th
Qtr – Jan 15
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Reporting
template
provided by
L.A. Care
MCLA LOB ONLY
COC for Optional Targeted Low Income Children
Report (COC-OTLIC):
COC for members requesting FFS providers through
plan. Aid codes:
2P, 2R, 2S, 2T, 2U, 5C, 5D, E2, E5, E6, E7, H1, H2,
H3, H4, H5, M5, T0, T1, T2, T3, T4, T5, T6, T7, T8,
T9
Quarterly
1
st
Qtr – April 15
2
nd
Qtr – July 15
3
rd
Qtr – Oct 15
4
th
Qtr – Jan 15
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Reporting
template
provided by
L.A. Care
MCLA LOB ONLY
COC for Medical Exemption Requests Report
(COC-MER):
COC requests for returning member in the middle of
care with a non-participating provider
Quarterly
1
st
Qtr – April 15
2
nd
Qtr – July 15
3
rd
Qtr – Oct 15
4
th
Qtr – Jan 15
via Clinical
Assurance SFTP Site
Email screen shot of
uploaded reports to
clinicalassurance@
lacare.org
Reporting
template
provided by
L.A. Care
On monthly and quarterly basis, Clinical Assurance Performance Monitoring Coordinators will email report
reminders, and attach the required reporting templates. For required reporting templates, please contact your
assigned Performance Monitoring Coordinator or send request to clinicalassurance@lacare.org. If your
organization requires additional training or assistance with a particular report, please contact your assigned
Performance Monitoring Coordinator to set-up a training.
32
5.7 Utilization Management Delegation
Oversight Audits
Oversight for L.A. Care’s directly contracted PPGs/
Specialty Providers are performed as prescribed in
the UM Delegation Oversight Plan as approved by
the UM Committee. Wherever possible these audits
may be done in conjunction with other L.A. Care
departments to improve efficiencies and decrease
duplication. e primary objective of the oversight
audit is to ensure compliance with L.A. Care’s policies
and procedures, standards of care, local, State, and
Federal regulatory requirements, accreditation
standards, and provisions of the purchaser contracts
(e.g. Department of Health Care Services (DHCS),
Centers for Medicare & Medicaid (CMS)). e
oversight audit consists of document review and
staff interviews to verify that policies/procedures/
processes have been implemented, applied, and are in
compliance.
is may include, but not be limited to, audits of case files
and medical records. e oversight audits are conducted
to ensure compliance with the following requirements:
• Annual approved Utilization Management Program,
Work Plan, and Evaluation
• UM Policies/Procedures/Processes
• UM Administrative capacity, staffing resources
• UM Over/Under Utilization
• UM referral management
• UM Criteria and consistency of application of criteria
• Emergency Services and After Hours Authorizations
• UM sub-delegation activities
• UM Case Management, for Members identified by the
HRA or CM program as “low” or “moderate” risk
• UM Care Coordination for in and out of network
referrals/hospitals
• UM Care Coordination for Linked and Carved
Out Services
As part of L.A. Care’s oversight process, L.A. Care
performs due-diligence reviews prior to Provider
contracting as well as an annual on-site audit of
delegated Provider groups to ensure compliance with
federal, state and NCQA requirements related to the
delivery of quality healthcare services. Specifically,
administrative and clinical oversight responsibilities
are assigned to multidisciplinary group of health plan
professionals representing the following administrative
and clinical areas:
• Credentialing
• Financial Compliance
• Pharmacy
• Regulatory Affairs & Compliance
• Medical Management (UM)
• Quality Management
• Provider Network Management
e scope of L.A. Care’s administrative and clinical
audits is comprehensive and based on Federal, State,
accreditation and contractual requirements. L.A. Care
uses an audit tool for each specific audit area that is
designed to assess compliance and delegation capacity.
e audit tools are updated annually to capture new
regulatory and contractual requirements. e audit
tools for each specific audit area capture, in part, audit
elements for audit area.
5.8 Supplemental Audits
Focused supplemental audit topics may be identified
by the Utilization Management Committee, Chief
Medical Officer or Medical Director. Focused
supplemental audit topics may also be identified by a
mid-year assessment, new legislative implementation
requirements or indicated as a consequence of findings
from internal (e.g., performed by L.A. Care) or external
(e.g. State or Federal) oversight/audit activity. e
purpose of a supplemental audit is to capture more
specific detailed information that may not be captured
through encounter data, supplemental reports or the
annual oversight audit. e goal of the supplemental
audit is to ensure compliance with L.A. Care’s
department’s policies and procedures, standards of care,
regulatory requirements, and provisions of contracts
with a specific issue. e supplemental audit may
consist of document review, file review and/or medical
record review and staff interviews; in addition to follow-
up on identified deficiencies or areas of concern.
A sampling methodology used to select member
records ensures a representative sample from the
PPG/Specialty Provider for the supplemental audit.
Supplemental audit tools are scored according to
the methodology approved by the UM Committee.
e supplemental audit may address any UM and
coordination of care category as identified by L.A. Care
UM Program.
5.9 Continuous Monitoring Activities
Continuous monitoring activities are used to
further supplement the basic oversight activities.
ese activities include annual/focused audits and
supplemental report submission review in order to
provide more comprehensive and timely oversight
33
in selected areas where episodic audits/reviews have
not been adequate in ensuring compliance with
regulations. A sampling methodology appropriate
to each continuous monitoring activity is defined to
ensure representative sampling, and approved by the
UM Committee. Examples of continuous monitoring
may include, but are not limited to:
• Referral Management – Timeliness, Clinical
Decisions, Member/Provider Notification, benefits,
and medical necessity determinations
• Case Coordination Review for in and out of network
referrals and hospitals
• Care Coordination for Linked and Carved Out
Services Delegation Oversight Review
• Care Coordination for HRAs and care management
services for low and moderate risk acuity levels
5.10 Continuous Monitoring of
Un-appealed Denials
e L.A. Care Clinical Assurance Department reviews
denials issued and submitted by the PPGs/Specialty
Providers. Delegated PPGs/Specialty Providers
are required to submit all denial letters with any
supporting documentation current to the denial
upon request or on schedule defined in L.A Care’s
Delegation Oversight Monitoring Policy upon request.
Plan Partner and PPG denial letters are evaluated for
compliance in the following areas:
• Appropriate template
• Timeliness of the decision-making and
notification process
• Physician involvement in the decision making
• Clear and concise denial reason
• Appropriate information available for decision-making
• Documentation of criteria for medical necessity
denials or benefit reference
• Appeal rights and process
If deficiencies are found in the initial review, the Plan or
delegated PPG is notified of the areas of deficiencies for
immediate correction. Continued non-compliance issues
are reported to the Utilization Management Committee
(UMC), Quality of Care (QOC), and/or Internal
Compliance Committee (ICC) for recommendations
in corrective action planning or disciplinary action.
Delegated PPGs/Specialty Providers letters are also
audited during the annual oversight audits. Corrective
Action Plans (CAPs) are required for those PPGs/
Specialty Providers with less than 90% compliance.
PPGs/Specialty Providers with deficiencies or CAPs will
be monitored according to L.A. Care policy. If a PPG/
Specialty Provider remains non-compliant, the findings
will be reported to the Delegation Oversight Group for a
decision regarding continued delegation.
e Plan will provide delegated PPGs/Specialty
Providers with the approved CMS, DHCS, or L.A. Care
letter templates that need to be utilized as the member
communication during the utilization management
process. Documents will be shared at least once every
year or more often as the need arises. e utilization on
the approved templates ensures that the PPG/Specialty
Provider is using approved standard regulatory language
to explain member’s rights.
5.11 Benets
e DHCS mandates benefits for Medi-Cal Members.
Member Handbooks for the Medi-Cal MCLA LOB
are maintained by Product Management and are
provided annually to each member. e Benefits
Section of the handbook describe in detail the covered
and non-covered services, procedures, and medical
equipment for the line of business.
5.12 Continuity of Care (COC)
COC provisions related to any member who is:
• New member transitioning into L.A. Care and who
is in the middle of care
• Members assigned to a contracted provider who is
terminated from the network
• New Medi-Cal enrollees transitioning into Medi-Cal
Managed Care
• Dually eligible beneficiaries (beneficiaries eligible for
Medi-Cal and Medicare) in the Cal MediConnect
program
• New Enrollees Transitioned to Managed Care After
Requesting a Medical Exemption
L.A. Care and it Delegates must provide COC with an
out-of-network provider when:
1. L.A. Care is able to determine that the beneficiary
has an ongoing relationship with the provider
(self-attestation is not sufficient to provide proof
of a relationship with a provider);
2. e provider is willing to accept the higher of
the L.A. Care or it’s Delegates contract rates or
Medi-Cal FFS rates; and
3. e provider meets applicable professional standards
and has no disqualifying quality of care issues.
Beneficiaries, their authorized representatives on file
with Medi-Cal, or their provider, may make a direct
request for COC. When this occurs, the L.A. Care and
it Delegates must:
34
• begin to process the request within five working days
after receipt of the request.
• the request must be completed in three calendar
days if there is a risk of harm to the beneficiary. For
the purposes of this APL, “risk of harm” is defined
as an imminent and serious threat to the health of
the beneficiary.
e COC process begins when L.A. Care and it
Delegates starts the process to determine if the
beneficiary has a pre-existing relationship with the
provider. L.A. Care and it Delegates shall accept
requests for COC over the telephone, according to the
requester’s preference, and shall not require that the
requester complete and submit a paper or computer
form if the requester prefers to make the request by
telephone. To complete a telephone request, L.A. Care
and it Delegates may take any necessary information
from the requester over the telephone.
L.A. Care and it Delegates shall accept and approve
retroactive requests for COC that meet all COC
requirements noted above, and in 1-3 below. e
services that are the subject of the request must have
occurred after the beneficiary’s enrollment into the
L.A. Care, and L.A. Care and it Delegates must have
the ability to demonstrate that there was an existing
relationship between the beneficiary and provider prior
to the beneficiary’s enrollment into L.A. Care. L.A. Care
and it Delegates shall only approve retroactive requests
that meet the following requirements:
1. Have dates of services that occur after the effective
date of this APL;
2. Have dates of services within 30 calendar days
of the first date of service for which the provider
is requesting, or has previously requested, COC
retroactive reimbursement; and
3. Are submitted within 30 calendar days of the first
service for which retroactive COC is being requested.
L.A. Care and it Delegates should determine if a
relationship exists through use of data provided by
DHCS to L.A. Care, such as Medi-Cal FFS utilization
data. A beneficiary or his or her provider may also
provide information to L.A. Care or it Delegates which
demonstrates a pre-existing relationship with a provider.
A beneficiary may not attest to a pre-existing relationship
(instead, actual documentation must be provided) unless
the L.A. Care or it Delegates makes this option available to
him or her.
Following identification of a pre-existing relationship,
L.A. Care or it Delegates must determine if the
provider is an in-network provider. If the provider is
not an in-network provider, L.A. Care and it Delegates
must contact the provider and make a good faith effort
to enter into a contract, letter of agreement, single-case
agreement, or other form of relationship to establish a
COC relationship for the beneficiary.
5.12.1 COC Request Completion Timeline
Each COC request must be completed within the
following timeline:
• irty calendar days from the date of the received
the request;
• Fifteen calendar days if the beneficiary’s medical
condition requires more immediate attention, such
as upcoming appointments or other pressing care
needs; or,
• ree calendar days if there is risk of harm to the
beneficiary.
A COC request is considered completed when:
• e beneficiary is informed of his or her right of
continued access;
• L.A. Care or it Delegates and the out-of-network
FFS or prior managed care health plan provider are
unable to agree to a rate;
• L.A. Care or it Delegates has documented quality of
care issues; or
• L.A. Care or it Delegates makes a good faith effort
to contact the provider and the provider is non-
responsive for 30 calendar days.
5.12.2 Requirements after the
COC Request Process is Completed
If L.A. Care or it Delegates and the out-of-network
FFS provider are unable to reach an agreement
because they cannot agree to a rate or L.A. Care or
it Delegates has documented quality of care issues
with the provider, L.A. Care or it Delegates will
offer the beneficiary an in-network alternative. If the
beneficiary does not make a choice, the beneficiary
will be referred or assigned to an in-network provider.
If the beneficiary disagrees with the result of the COC
process, the beneficiary maintains the right to pursue a
grievance and/or appeal.
If a provider meets all of the necessary requirements
including agreeing to a letter of
agreement or contract with L.A. Care or it Delegates,
the L.A. Care or it Delegates must allow the
beneficiary to have access to that provider for the
length of the COC period unless the provider is
35
only willing to work with L.A. Care or it Delegates
for a shorter timeframe. In this case, L.A. Care or it
Delegates must allow the beneficiary to have access to
that provider for the shorter period of time. At any
time, beneficiaries may change their provider to an in-
network provider regardless of whether or not a COC
relationship has been established.
When the COC agreement has been established,
L.A. Care or it Delegates must work with the provider
to establish a care plan for the beneficiary. Upon
approval of a COC request, L.A. Care or it Delegates
must notify the beneficiary of the following within
seven calendar days:
• e request approval;
• e duration of the COC arrangement;
• e process that will occur to transition the
beneficiary’s care at the end of the COC period; and
• e beneficiary’s right to choose a different provider
from L.A. Care or it Delegates provider network.
L.A. Care or it Delegates shall also notify the
beneficiary 30 calendar days before the end of the
COC period about the process that will occur to
transition the beneficiary’s care at the end of the COC
period. is process shall include engaging with the
beneficiary and provider before the end of the COC
period to ensure continuity of services through the
transition to a new provider.
5.12.3 Extended COC Option
L.A. Care or it Delegates may choose to work with
the beneficiary’s out-of-network provider past the
12-month COC period, but L.A. Care or it Delegates
is not required to do so to fulfill its obligations under
the regulatory guidance.
An approved out-of-network provider must work with
L.A. Care or it Delegates and its contracted network
and cannot refer the beneficiary to another out-of-
network provider without authorization from L.A. Care
or it Delegates. In such cases, L.A. Care or it Delegates
will make the referral, if medically necessary and if
L.A. Care or it Delegates does not have an appropriate
provider within its network.
5.12.4 Covered California to Medi-Cal Transition
is section specifies requirements for populations
that undergo a mandatory transition from Covered
California to Medi-Cal managed care coverage due
to the Covered California yearly coverage renewal
determination. ese requirements are limited to these
transitioning beneficiaries.
As part of the process to ensure that COC and
coordination of care requirements are met, L.A. Care
or it Delegates shall ask the beneficiary if there are
upcoming health care appointments or treatments
scheduled and assist the beneficiary to initiate the COC
process at that time, if the beneficiary chooses to do so,
according to the provider and service continuity rights
described below or other applicable continuity of care
rights. When a new beneficiary enrolls in Medi-Cal,
L.A. Care or it Delegates shall contact the beneficiary
by telephone call, letter, or other resources no later
than 15 days after enrollment. e requirements noted
above in this paragraph shall be included in this initial
beneficiary contact process. L.A. Care or it Delegates
shall make a good faith effort to learn from and obtain
information from the beneficiary that will assist
L.A. Care or it Delegates to honor active Prior
Treatment Authorizations and/or establish out-of-
network provider COC as described below.
L.A. Care or its delegated provider networkshall honor
any active Prior Treatment Authorizations for up to
60 days or until a new assessment is completed by
L.A. Care or it Delegates. A new assessment has been
completed by L.A. Care and its delegated provider
network if the member has been seen by a L.A. Care-
contracted provider and this provider has completed
a new treatment plan that includes assessment of
the services specified by the pre-transition active
Prior Treatment Authorization. e Prior Treatment
Authorizations must be honored without a request by
the beneficiary or the provider.
L.A. Care or its delegated provider network shall, at
the beneficiary’s or provider’s request, offer up to
12 months of COC with out-of-network providers,
in accordance with the DHCS policy requirements
for other transitioning populations regarding out-of-
network COC.
5.12.5 Senior and Persons with Disabilities Fee
For Service Treatment Authorization Request
Continuity Upon Enrollment with L.A. Care
For a newly enrolled Seniors and Persons with
Disabilities (SPDs), L.A. Care or it Delegates must
honor any active FFS Treatment Authorization
Requests (TARs) for up to 60 days or until a new
assessment is completed by L.A. Care or it Delegates.
A new assessment has been completed by L.A. Care
or it Delegates if the member has been seen by a
L.A. Care-contracted provider and this provider
has completed a new treatment plan that includes
assessment of the services specified by the pre-
36
transition active Prior Treatment Authorization. e
FFS TAR must be honored as outlined above without
a request by the beneficiary or the provider.
5.12.6 Behavioral Health Treatment Coverage For
Children For Children Diagnosed with Autism
Spectrum Disorder
L.A. Care or it Delegates are responsible for providing
Early and Periodic Screening, Diagnosis, and
Treatment services for beneficiaries ages 0 to 21.
Effective September 15, 2014, the services include
medically necessary Behavioral Health Treatment
(BHT) Services such as Applied Behavioral Analysis
and other evidence-based behavioral intervention
services that develop or restore, to the maximum
extent practicable, the functioning of the beneficiaries
diagnosed with Autism Spectrum Disorder (ASD).
In accordance with the requirements listed in this
APL and APL 14-011, L.A. Care or it Delegates shall
provide continued access to out-of-network BHT
providers for up to 12 months beginning September
15, 2014. e beneficiary must have an existing
relationship with the BHT provider. An existing
relationship means a beneficiary has seen the out-
of-network BHT provider at least twice during the
12 months prior to September 15, 2014, or the date
of his or her initial enrollment in the L.A. Care if
enrollment occurred on or after September 15, 2014.
Retroactive requests for BHT services are limited to
services that were provided after September 15, 2014
or the date of the beneficiary’s enrollment into L.A. Care
or it Delegates if the enrollment date occurred after
September 15, 2014.
L.A. Care or it Delegates must continue ongoing BHT
services until L.A. Care or it Delegates have conducted
a comprehensive diagnostic evaluation and assessment,
and established a treatment plan. L.A. Care or it
Delegates may refer to the COC section of APL
14-011 for additional requirements and information
regarding COC for BHT services for beneficiaries
diagnosed with ASD.
5.12.7 Existing COC Provisions under California
State Law
In addition to the protections set forth above, L.A. Care
beneficiaries also have rights to protections set forth in
current State law pertaining to COC. In accordance
with W&I Code §14185(b), L.A. Care or it Delegates
must allow beneficiaries to continue use of any (single-
source) drugs that are part of a prescribed therapy (by
a contracting or non-contracting provider) in effect
for the beneficiary immediately prior to the date of
enrollment, whether or not the drug is covered by
L.A. Care, until the prescribed therapy is no longer
prescribed by the L.A. Care-contracting provider.
Additional requirements pertaining to COC are set
forth in Health and Safety (H&S) Code § 1373.96
and require all health plans in California to, at the
request of a beneficiary, provide for the completion of
covered services by a terminated or nonparticipating
health plan provider. Under §1373.96, health plans
are required to complete services for the following
conditions: acute, serious chronic, pregnancy, terminal
illness, the care of a newborn child between birth and
age 36 months, and surgeries or other procedures that
were previously authorized as a part of a documented
course of treatment. L.A. Care’s continues obligation
to fully comply with the requirements of §1373.96. In
addition to the requirements, L.A. Care or it Delegates
must allow for completion of covered services as
required by §1373.96, to the extent that doing so
would allow a beneficiary a longer period of treatment
by an out-of-network provider than would otherwise
be required under the terms of this this APL. L.A. Care
or it Delegates must allow for the completion of these
services for certain timeframes which are specific to each
condition and defined under H&S Code § 1373.96.
5.12.8 Medical Exemption Requests
A Medical Exemption Request (MER) is a request for
temporary exemption from enrollment into L.A. Care
only until the Medi-Cal beneficiary’s medical
condition has stabilized to a level that would enable
the beneficiary to transfer to a L.A. Care provider
of the same specialty without deleterious medical
effects. A MER is a temporary exemption from Medi-
Cal Managed Care enrollment that only applies to
beneficiaries transitioning from Medi-Cal FFS to an
Medi-Cal Managed Care Plan. A MER should only be
used to preserve COC with a Medi-Cal FFS provider
under the circumstances described above in this
paragraph. L.A. Care or it Delegates are required to
consider MERs that have been denied as an automatic
COC request to allow the beneficiary to complete a
course of treatment with a Medi-Cal FFS provider.
5.12.9 PPG Responsibility for COC Coordination
Delegates are responsible for the initial assessment and
care coordination for COC determinations. L.A. Care
will provide reporting instructions, templates and
documentation requirements for the various regulatory
reporting needs. Delegates are also responsible for
37
ensure the necessary financial arrangements are made
with providers who agree to the provision on continued
services to our members. Delegates must ensure:
• e request for COC is managed within the defined
timelines.
• e appropriate documentation of the request is
maintained as defined by regulatory requirements
• Written communication explaining the provision of
the services within timeframes of the provision of
services is provided to the Member, the Requested
Provider, the assigned Primary Care Physician and
the PPG.
• e Member is assigned to a care coordination program
to assist in care coordination while the member is
receiving care with a non-participating provider
• A care transition plan is developed to ensure
communication to the member and providers on
understanding the COC services and the plan for
transitioning back into the network provider.
If the COC is not approved or the non-participating
provider does not accept the conditions of the COC
process, L.A. Care would support transitioning the
member in-network when there is:
• Documentation to ensure an in-network physician
has spoken with the treating physician, agreed to
accept the member and agreed that the services
needed can be provided within the assigned network
• ere is an acceptable transition plan notifying
the member of where to receive services, contact
information and a scheduled appointment
• ere is a written Notification of Action letter,
containing their appeal rights, to the member
regarding the denial of services
• e member is assigned to a PPG care
coordination program
5.12.10 Transition to Other Care When Benefits End
L.A. Care assists with, and/or ensures that
practitioners assist with a member’s transition to other
care, if necessary, when benefits end.
5.13 New Medical Technology
L.A. Care evaluates the inclusion of new technologies
and new applications of existing technologies in
the benefit plans. e Utilization Management
and Pharmacy and erapeutics Committee are
responsible for evaluating and recommending coverage
status for new technology to the UM Committee
and to the Quality Oversight Committee. is
includes evaluation of medical and behavioral health
procedures, pharmaceuticals, and devices.
Members and providers may ask L.A. Care to review
new technology. To request a new technology review
or new use of an existing technology, the PPG
may contact L.A. Care’s UM administrative staff at
1.877.431.2273.
5.14 Responsibility of Participating
PPGS and Contracted Providers –
Coordination of Health Care Services
PPGs are responsible for assisting participating
providers with the provision and coordination of health
care services, referral management and payment of
services for which the PPG has financial responsibility
for members enrolled with their primary care
physicians. PPGs are also responsible for primary (basic)
medical case management and care coordination.
e PPG agrees and is required to:
• Provide health care services as defined by L.A. Care
policy, regulatory requirements, clinical practice
guidelines or associated medical professional guidance.
• Provide supportive care management/care
coordination activities for the PCPs
• Make available to L.A. Care any requested data,
documents and reports
• Allow site visits, periodic attendance at UM meetings,
evaluation and audits by L.A. Care or other agencies
authorized by L.A. Care to conduct evaluations
• Have representation and involvement in L.A. Care’s
UM committee meetings and other activities
scheduled to enhance and/or improve the quality of
health care services provided to L.A. Care’s members
A full description of these services are defined in the
PPG contract, the contract Division of Financial
Responsibility (DOFR) and a delegation agreement.
5.14.1 After Hours Authorization
PPGs must have a system in place for members to
contact their Primary Care Physician, or a physician
delegated to provide medical advice, after hours (24
hours, 7 days a week). is includes contacting the
delegated UM Staff or physician covering for the PCP
or PPG for hospital notifications.
PPGs are required to have 24 hours/7 days per week
telephone access to UM professionals to:
• Review and provide
• Instructions for Medical Necessary post-stabilization
care and coordinate the transfer of stabilized
members in an emergency department, if necessary

38
• Response to these requests is required within 30
minutes or the service is deemed approved in
accordance with State regulations
• Coordination of professional services for hospital
admissions or transfers
• Review and provide instructions for non-urgent care
following an exam in the emergency room
• Response to these requests are required within
30 minutes or the service is deemed approved in
accordance with DHCS contractual regulations
• Respond to expedited UM requests for;
°
Referrals due within a 72 hour (from the time of
the receipt) period
• Assistance in the resolution for appeals of
denied services
• Assistance in the resolution of clinical grievances
• Assistance in the resolution of requests for
information from regulatory agencies
5.14.2 How to Communicate with UM Staff and
Instructions for Triaging Inbound Calls Specific to
utilization management Cases/Issues:
L.A. Care and PPGs must provide members and
practitioners access to UM staff when they are seeking
information regarding the Utilization Management
process and the authorization of care as defined in L.A.
Care policies.
• L.A. Care contact information:
• UM Staff members are available at least eight hours
a day during normal business hours for inbound
collect or toll-free calls regarding UM issues
• e toll free UM number at L.A. Care is (877)
431.2273
• Staff can receive inbound communication regarding
UM issues after normal business hours
• Staff members identify themselves by name, title and
organization name when initiating or returning calls
regarding UM issues
• For telephone calls from Members and Providers
regarding UM issues:
°
For Members: L.A. Care will accept collect calls
from members and also provides the following toll
free numbers (L.A. Care product specific member
800 toll free numbers)
TDD/TTY services for members who need them
Language assistance for members to discuss
UM issues
°
For Practitioners: L.A. Care provides a Toll-
free telephone number/L.A. Care’s UM toll free
provider “800” authorization line: 1.877.431.2273
Additional instructions on how to obtain authorizations
and communicate with UM staff are listed below.
5.14.3 UM Referral Management Review Processes
PPG contract status impacts how the PPG will
coordinate UM referral activities with L.A. Care.
Currently, L.A. Care contract models include:
• Fee For Service (FFS)
• Shared Risk (SR)
• Dual Risk (DR)
• Full Risk (FR)
• Capitated
PPGs with FFS contracts are capitated for primary
care services. Non-primary care related request for
services (referrals) that are not considered exemptions
from prior authorization or auto-authorization must
be referred to L.A. Care UM Department for UM
decision making.
PPGs with SR contracts are capitated for primary care
and some diagnostic procedures. PPG may make medical
necessity decisions on outpatient services noted as
“hospital shared risk” when services are provided at a
L.A. Care contracted facility. PPG must notify L.A. Care
at the time of the decision via the standard L.A. Care
Referral request form of the decision and the facility
utilized. PPG is responsible for notification to the
Member, the requesting provider, the rendering provider
and the PCP. PPG must refer all inpatient, acute or sub-
acute, settings to L.A. Care.
PPGs with DR contracts maintain a hospital and PPG
risk arrangement. L.A. Care delegates UM activities to
the PPG. e PPG and the hospital have arrangements
defining responsible parties for UM activities. PPG is
responsible for maintaining UM referral management
activities and ensuring communication and notifications
to the Member, the requesting provider, the rendering
provider and the PCP.
PPGs with FR contracts have Knox Keene or limited
Knox Keene licensure and maintain a hospital and PPG
risk arrangement; L.A. Care delegates UM activities to
the PPG. e PPG and the hospital have arrangements
defining responsible parties for UM activities. PPG is
responsible for maintaining UM referral management
activities and ensuring communication and notifications
to the Member, the Requesting Provider, the Rendering
Provider and the PCP.
Capitated contracts are usually specialty health
plans or services providers and are fully at risk for
contracted services; L.A. Care delegates UM activities
39
to the provider. e provider may be responsible
for maintaining UM referral management activities
and ensuring communication and notifications to
the Member, the Requesting Provider, the Rendering
Provider and the PCP based on the terms of the
delegation agreement.
5.14.4 Services Exempt from (Not Requiring)
Prior Authorization (Pre-service Review)
PPGs must provide, arrange for, or otherwise facilitate
the following services, including appropriate coverage
of costs without prior authorization as described in
corresponding policies and procedures:
• Emergency services (medical screening and
stabilization) where a prudent layperson, acting
reasonably, would have believed that an emergency
medical condition existed and when an authorized
representative acting for L.A. Care has authorized
the provision of emergency services
• Preventive health services for all ages
including immunizations
• Family Planning Services including outpatient
abortions through any family planning provider
• Basic in-network prenatal care, including OB/GYN
in-network referrals and consults
• Sensitive and confidential services and treatment,
including but not limited to, services relating to
sexual assault, pregnancy and pregnancy related
services, family planning, abortion/pregnancy
termination, sexually transmitted diseases, drug
and alcohol abuse, HIV testing and treatment, and
outpatient mental health counseling and treatment.
Please note: If you do not provide abortion/
pregnancy termination
• services, you must refer the member to L.A. Care
Member Services line.
• Sexually Transmitted Disease (STD) treatment
services both in and out of network including
follow-up care
• Confidential HIV counseling and testing services
both in network and through out-of-network local
health departments and family planning providers
5.14.5 Services Requiring Prior Authorization
e delegation of certain UM activities affords
flexibility for the PPG to establish internal prior
authorization requirements. ese requirements must
be reviewed and approved by L.A. Care through the
delegation process.
ere are services for which the PPG must submit a
request/referral to L.A. Care for prior authorization, or
notification concurrently with or retrospective of the
services for authorization by L.A. Care.
Unless defined in the most recent L.A. Care PPG Auto
Approval Listing, the services listed below, and any future
updates dependent on delegation and DOFR, must first
be authorized by L.A. Care’s UM department:
• Certain pharmaceuticals (the pharmacy prior-
authorization process can be found in the Pharmacy
section of this manual)
• Durable Medical Equipment (DME)
• Home Health Services
• Hospice
• Non-Emergent/Non-Urgent Hospital or Skilled
Nursing Facility (SNF) admissions (see DOFR)
• Medical Supplies (not provided in physicians’ offices)
• Most elective surgical and invasive diagnostic
procedures (inpatient or outpatient facility
component) (see DOFR)
• Orthotics & Prosthetics
• Physical/Occupational & Speech therapies (see DOFR)
• Rehabilitation Services
• Transplant Evaluation
5.14.6 Utilization Management Services Not
Delegated To PPGS:
Referrals for:
• Power Wheelchairs (shared risk only)
• Coagulation Factors (see Pharmacy section)
• Early Periodic Screening Diagnosis and Treatment
(EPSDT) Supplemental Services – In Home Shift
Nursing Care/Private Duty Nursing (See Section:
EPSDT Supplemental Services)
• Managed Long Term Services and Supports
(MLTSS)
• Clinical Trials
• Experimental/Investigational
• Non-emergency Transportation
• Behavioral Health
• Chemical Dependency
• Transgender Health Services
5.14.7 Referral Management Processes:
Types of referrals:
• Pre-Service Review (also called prior authorization,
pre-certification)
• Concurrent Review (A request for coverage of medical
care or services made while a member is in the process
of receiving the requested medical care or services,
even if the organization did not previously approve
the earlier care)
40
• Post Service Review (service provided but no claim
has been submitted)
• Retrospective Claim Review
• Second Opinion Review
• Reconsideration Review (Peer review between
physicians for a second review within 24 hours of
the initial decision); NOT the CMS definition of a
UM appeal.
• Independent Medical Review
5.14.7.1 Classification of Referral Management
Requests
L.A. Care uses the definitions below to classify
UM cases:
5.14.7.1.1 Expedited (Urgent) request. A request for
medical care or services where application of the time
frame for making routine or non-life threatening care
determinations:
• Could seriously jeopardize the life or health of the
member or the member’s ability to regain maximum
function, based on a prudent layperson’s judgment,
OR
• In the opinion of a practitioner with knowledge of
the members medical condition, would subject the
member to severe pain that cannot be adequately
managed without the care or treatment that is the
subject of the request.
5.14.7.1.2 Routine (Non-urgent) request: A request
for medical care or services for which application of the
time periods for making a decision does not jeopardize
the life or health of the member or the member’s ability
to regain maximum function and would not subject the
member to severe pain.
5.14.7.1.3 Timelines for UM determinations
All authorization requests submitted to L.A. Care will be
responded to within the defined timeframes as follows:
• Expedited – 72 hours from the receipt of the request
for service
• Routine – 5 working days from receipt of the
information necessary to make the decision, not to
exceed 14 calendar days from receipt of the request
• Urgent concurrent- 24 hours of receipt of the request
°
e request to approve additional days for urgent
concurrent care is related to care not previously
approved. e organization must document that it
made at least one attempt to obtain the necessary
information within 24 hours of the request, but
was unable to. e organization has up to 72
hours to make a decision
• Post-service or Retrospective - 30 calendar days of
the request
• Extending timeframes – see Attachment A, for
the most recent version of L.A. Care’s Timeliness
Standards for the appropriate documentation
requirements and timelines for extensions
NOTE: Referral requests submitted as expedited/
urgent must meet the regulatory definition for urgent
care (see above). Referrals submitted as such will
be reviewed by clinical staff to ensure the service
requested meets this definition. Referrals that DO
NOT meet the definition will be modified to the
appropriate determination status, e.g. routine, and
processed accordingly. e modification will be
referred to a Medical Director to ensure the Member’s
condition is not such that the Member faces an
imminent and serious threat to his or her health,
including, but not limited to, the potential loss of life,
limb, or other major bodily function, or the normal
timeframe for the decision-making process and would
be detrimental to the Member’s life or health or could
jeopardize the Member’s ability to regain maximum
function. e requestor will receive notification of the
modification and given an opportunity to submit a
reconsideration of the determination.
5.14.7.1.4 UM determinations are made in
accordance with the standard regulatory requirements
for referral management
and include:
• Approved
• Modified
• Denial
• Deferred/Pended/Delayed
Occasionally referral requests are submitted with
clerical or eligibility errors or the requesting provider
has made a decision to withdraw the request.
Additional determinations may be utilized to identify
the scenario, such as withdrawn or void. In either case,
the identified issue must be documented in the case to
identify why the determination was made.
5.14.7.2 Pre-service Review (Prior Authorization)
Pre-service Review or Prior Authorization is the formal
process requiring a health care provider to obtain
advance approval for coverage of specific services
or procedures, allows for benefit determination,
determination of medical necessity and clinical
appropriateness, level of care assessment, assignment of
the length of stay for inpatient admissions, appropriate
facility placement prior to the delivery of service, and
41
identification of the intensity of case management that
may be needed for optimal patient outcomes.
5.14.7.3 24 hour Access to Pre-service Review
(Prior Authorization) A Physician with an active
unrestricted California license is available 24 hours a
day to review requests for post-stabilization care and
to coordinate the transfer of stabilized Members in an
emergency department, if necessary.
5.14.7.4 Services Requiring Pre-service Review
(Prior Authorization) L.A. Care develops, reviews, and
approves at least annually, lists of auto pay and auto
authorization. Any procedure, treatment, or service not
on these lists requires prior authorization. L.A. Care
communicates to all contracted health care practitioners
the procedures, treatments, and services that require
prior authorization and the procedures and timeframes
necessary to obtain such prior authorization.
NOTE: Service types identified by the PPG
Staff as Pre-Service Urgent may be reviewed for
appropriateness by the L.A. Care UM Medical
Director. PPG will be contacted if a request is
determined by the Medical Director not to meet the
definition of urgent, and advised that the requested
service will be revised to reflect a routine request.
Providers who disagree with the revision may contact
L.A. Care at 1.877.431.2273.
5.14.7.5 Concurrent review of authorization is an
authorization for treatment regimen already in place,
reviewed within five working days or less, and is consistent
with urgency of the member’s medical condition
NOTE: is does not include inpatient concurrent
review; pre-service inpatient concurrent review of
service must be responded to within 24 hours of
the request
5.14.8 Member Eligibility Verification
Member eligibility and covered benefits should be
verified prior to UM decisions
5.14.8.1 Authorizations and Member Eligibility
L.A. Care and its delegates authorize services for
extended time periods (up to 12 months) when
the member’s condition is not likely to change
and the service is expected to be required into the
future. Examples of such authorizations are standing
referrals, specialty referrals, wheelchairs, incontinence
supplies, CBAS services and Long Term Care services.
ese extended authorizations offer convenience
and operational efficiency to the Provider because
it eliminates the need for monthly submission of
authorization requests. However, every authorization
is issued with the expectation that members will
continue coverage under L.A. Care and the process
requires Provider to verify eligibility.
5.14.8.1.1 Provider Responsibility for
Authorizations and Member Eligibility
Notwithstanding the authorization, the provider is
required to verify the member’s eligibility prior to
providing the services authorized. Failure to confirm
eligibility prior to providing the services may result in
nonpayment of your claim. L.A. Care recommends
that member eligibility be verified on the date services
are to be rendered. Daily eligibility may be checked
through L.A. Care’s IVR system. If you have any
questions regarding a member’s eligibility, please
contact L.A. Care’s Provider Information Line at
1.866.522.2736.
5.14.8.1.2 Delegate Responsibility
Delegates are required to provide the disclaimer
language in notices of authorization to facilities,
practitioners, and other providers. Delegates are
responsible to inform individual providers or practitioners
of the requirement to verify member eligibility prior to
providing services.
5.14.8.1.3 Claim Denied for Lack of
Member Eligibility
If a claim is denied for lack of member eligibility, and
rendering provider believes the member’s eligibility was
verified and the service was provided in good faith, the
provider may submit a Provider Dispute Request Form.
Provider is to include all documentation relative to
verification of eligibility in the provider dispute request.
Providers may access a form at http://www.lacare.org/
providers/provider-resources/provider-forms.
5.14.8.2 Requests for Authorization (Referrals) to
L.A. Care’s UM Department
Requests for Authorization (Referrals) may be
submitted on paper, by phone, or electronically. All
requests must be submitted on a L.A. Care Referral
Form and include the following information:
• Requesting provider
• Patient’s name, date of birth, address, phone number,
and social security number
• Confirmation of current L.A. Care eligibility
• Patient’s diagnosis and medical history supportive to
the service requested
• Supportive medical records needed to make
a determination
42
• Appropriate coding (using current CPT-4, ICD-9
procedure, and/or HCPCS codes), and identification
of services requested
• Identification of requested provider of service,
including name, type of provider, location and
provider’s phone number
5.14.8.2.1 Minimum Clinical Information for
Review of UM Requests for Authorization
Requests for services are reviewed in accordance
with approved UM criteria and the member’s
benefit structure. When making a determination of
coverage based on medical necessity, relevant clinical
information is obtained and consultation with the
treating practitioner occurs as necessary. Clinical
information for making determinations of coverage
includes that which is reasonably necessary to apply
relevant UM Criteria, and may include, but is not
limited to, the following:
• Office and hospital records
• A history of the presenting problem
• A clinical exam
• Diagnostic testing results
• Treatment plans and progress notes
• Patient psychosocial history
• Information on consultations with the treating
practitioner
• Evaluations from other health care practitioners
and providers
• Photographs
• Operative and pathological reports
• Rehabilitation evaluations
• A printed copy of criteria related to the request
• Information regarding benefits for services or procedures
• Information regarding the local delivery system
• Patient characteristics and information
• Information from responsible family members
Referrals submitted to L.A. Care UM Department for
a clinical determination must contain the information
to assess for medical necessity of the service. Missing
information provided by PPGs or PCPs delay the services
and may result in referrals returned to the requestor
5.14.8.2.2 Timeliness Standards
Timeliness standards for decisions and notification of
UM decisions are described for each line of business in
the most current UM policies and procedures. Please
contact L.A. Care for the most recent version of the
policies and matrix.
For operational purposes, L.A. Care’s timeliness
standards for the initial start date of a referral are:
• Routine requests
°
Day of receipt of the request as “Day 0”
°
Day following receipt of the request as “Day 1”
• Expedited or Urgent requests
(within 72 hours)
°
24 hours is equivalent to one calendar day
°
72 hours is considered as 3 calendar days.
5.15 Medical Necessity Denitions
Medically Necessary or Medical Necessity means
those reasonable and necessary services, procedures,
treatments, supplies, devices, equipment, facilities, or
drugs that a medical practitioner, exercising prudent
clinical judgment, would provide to a member for
the purpose of preventing, evaluating, diagnosing, or
treating an illness, injury, or disease or its symptoms to
protect life, to prevent significant illness or significant
disability, or to alleviate severe pain that is consistent
with nationally accepted standards of medical practice:
• “Generally accepted standards of medical practice”
means standards that are based on credible scientific
evidence published in peer-reviewed medical
literature generally recognized by the relevant
medical community, national physician specialty
society recommendations, and the views of medical
practitioners practicing in relevant clinical areas and
any other relevant factors.
• For drugs, this also includes relevant finding
of government agencies, medical associations,
national commissions, peer reviewed journals
and authoritative compendia consulted in
pharmaceutical determinations.
• For purposes of covered services for Medi-Cal
members, the term “medically necessary” will
include all Covered Services that are reasonable and
necessary to protect life, prevent significant illness
or significant disability, or to alleviate severe pain
through the diagnosis or treatment of disease, illness,
or injury and
• When determining the medical necessity of Covered
Services for a Medi-Cal beneficiary under the age
of 21, “medical necessity” is expanded to include
the requirements applicable to Early and Periodic
Screening, Diagnosis, and Treatment (EPSDT)
Services and EPSDT Supplemental Services and
EPSDT Supplemental Services as defined in Title 22,
51340 and 51340.1.
5.15.1 Clinical Criteria For Decision Making
Decision Support Tools
e appropriate use of criteria and guidelines require
43
strong clinical assessment skills, sound professional
medical judgment, and application of individual case
information and local geographical practice patterns.
Licensed nursing review staff apply professional
judgment during all phases of decision-making
regarding L.A. Care members.
“Decision Support Tools” are intended for use by
qualified licensed nursing review staff as references,
resources, screening criteria, and guidelines with
respect to the decisions regarding medical necessity
of health care services, and not as a substitute
for important professional judgment. e
Medical Director evaluates cases that do not meet
review criteria/guidelines, and is responsible for
authorization/denial determinations.
UM staff clearly document the Review Criteria/
Guidelines utilized to assist with authorization
decisions. In the event that a provider questions a
medical necessity/appropriateness determination,
any criteria, standards, or guidelines applied to the
individual case supporting the determination is
provided to the provider for reference.
e following describes the approved Department
“Decision Support Tools” that have been implemented,
and are evaluated and updated at least annually.
5.15.1.1 UM Review Criteria, Guidelines
and Standards
L.A. Care, Plan Partners, PPGs, and Vendors delegated
for UM functions must utilize evidenced based nationally
recognized criteria for UM decision making. UM criteria
are used to determine medical necessity in the referral
management Authorization Request review process.
Standards, criteria and guidelines are the foundation
of an effective UM Program. e tools are utilized
to assist during evaluation of individual cases to
determine the following:
• Services are medically necessary
• Services are rendered at the appropriate level of care
• Quality of care meets professionally-recognized
industry standards
• UM decision-making is consistent
e following standards, criteria, and guidelines
are utilized by UM staff and Medical Directors as
resources during the decision making process:
• UM Medical necessity review criteria and guidelines
• Length of stay criteria and guidelines
• Clinical Practice Guidelines
• Referral Guidelines
• Policies and Procedures
5.15.1.2 Application of UM Criteria
L.A. Care requires that UM criteria be applied in a
consistent and appropriate manner by physician and
non-physician UM staff based on available medical
information and the needs of individual Members.
For use in determining the appropriateness of UM
determinations at the L.A. Care Plan level for the
MCLA direct requests for authorization, L.A. Care
adopts and maintains approved criteria with current
versions of the following UMC approved UM Criteria
Auto Authorization UM Criteria as approved by the
UM Committee in the following hierarchy:
• UM Auto Authorization Criteria as approved by the
UM Committee
• Other Utilization Management Committee
Approved Criteria
• Pharmacy erapeutics Committee Approved
Criteria
• DHCS and CMS UM Criteria -- to be determined
by Primary Payer for the request
°
DHCS Medi-Cal UM Criteria is available and
updated on Department of Health Care Services
(DHCS) Web Site
°
CMS Medicare UM Criteria as available and
updated on CMS Web Site
• When none of the above criteria are applicable,
consider the following and two (2) or more of the
following criteria are applicable, then MCG Health
care guidelines criteria are to be used as the first
choice.
°
MCG Health Guidelines
°
Apollo® Managed Care Criteria
°
Uptodate® (uptodate.com)
• Hayes, Inc.
• Definition of Medical Necessity (Product Line
specific when the above criteria does not apply to a
specific request for a UM decision)
• Other resources
Due to the dynamic state of medical/health care
practices, each medical decision must be case specific,
and based on current medical knowledge and practice,
regardless of available practice guidelines. Listed
criteria in fields other than primary care, such as
OB/GYN, surgery, etc., are primarily appended for
guidance concerning medical care of the condition, or
the need for a referral.
5.15.1.3 Inter-rater Reliability Requirements (IRR)
At least annually, PPGs are required to ensure that
consistency and appropriateness with which health
care professionals involved in utilization review apply
44
criteria in decision making is evaluated and reported.
e assessment of Inter-rater Reliability (IRRs) applies
only to determinations made as part of a UM process.
A primary care practitioner’s referral of a member to
a specialist, when the referral does not require prior
authorization, is not considered a UM determination.
Opportunities to improve consistency in the
application of criteria are acted upon as appropriate.
Required IRR Methodologies use Statistically Valid
Samples (see most recent copy of L.A. Care policy):
• 5 percent or 50 of its UM determination files,
whichever is less; or
• NCQA “8/30 methodology” or a valid sampling of
hypothetical cases
L.A. Care reserves the right to review the PPGs IRR
on an annual basis to ensure that PPGs are using
required IRR Methodology with statistically valid
samples.
5.15.1.4 Criteria Based on Individual Need
Because nationally developed procedures for applying
criteria, particularly those for lengths of hospital
stay, are often designed for “uncomplicated” patients
and for a complete delivery system, they may not
be appropriate for patients with complications or
for a delivery system with insufficient alternatives
to inpatient care. erefore, L.A. Care considers at
least the following when applying criteria to a given
individual:
• age
• comorbidities
• complications
• progress of treatment
• psychosocial needs
• home environment, when applicable
L.A. Care also considers characteristics of the local
delivery system available for specific members, such as,
but not limited to:
• availability of contracted hospitals within the
network and other hospitals out of network
• availability of contracted specialists and specialty centers
• availability of non-contracted specialists and
specialty centers which may be contracted through
a one-time MOU for a specific member for unusual
specialty services
• availability of skilled nursing facilities, sub-acute care
facilities or home care in the service area to support
the patient after hospital discharge
• coverage of benefits for skilled nursing facilities, sub-
acute care facilities or home care where needed
• local hospital’s ability to provide all recommended
services within the estimated length of stay
If none of the approved UM Criteria meet the
member’s medically necessary service needs, even when
considering the member’s individual needs, and/or the
characteristics of the local delivery system, then the
physician reviewer considers other alternatives, such as:
• approving higher levels of care within the local area
• making arrangements to send the member out-of-
the local network or out-of-Plan for the needed
services
• arranging for case discussion with a local
physician consultant or a physician consultant
from the contracted vendor assembling a panel
of independent experts to identify other possible
alternatives
• Ultimately the physician reviewer makes a UM
decision in a timely manner that will meet the
member’s individual medically necessary needs. In
these instances, the physician reviewer makes the
determination in a manner which is consistent with
L.A. Care’s Utilization Management Principles.
5.16 PPG UM Criteria
PPGs may choose to review or adopt specific evidence
based UM criteria to be used for decision making.
L.A. Care reserves the right to review the PPGs criteria
on an annual basis to ensure that PPGs are using
evidence based criteria and the most current available
versions of the evidence based criteria.
5.17 Criteria for Use in L.A. Care Review
of Appeals and Other Requested Clinical
Reviews (e.g. Clinical Grievance Review,
PQIs, etc.
• MCG Criteria is used by L.A. Care as the first choice
in review of appeals and other requested clinical
reviews (e.g. Clinical Grievance Review, Potential
Quality Incidents, etc.).
• Assessment of consistency of UM decisions
• PPGs are required to ensure that UM criteria be
applied in a consistent and appropriate manner
by physician and non-physician UM staff based
on available medical information and the needs of
individual Members.
45
5.18 Access to and Disclosure of UM
Criteria and UM Policies/Procedures and
Processes
UM criteria and UM procedures and processes
are available to L.A. Care practitioners, providers,
members and their representatives, and the public
upon request. To obtain a copy of any L.A. Care
UM criteria, UM policies/procedure or UM
processes; practitioners, providers, members,
their representatives, and the public may contact
the L.A. Care Member Services Department at
1.888.839.9909, or the L.A. Care UM Department
at 1.877.431.2273 and ask to speak with the UM
Director or UM Manager to make the request.
PPGs shall make information available so that
practitioners, providers, members, member
representatives, and the public know how to request the
PPG’s UM criteria, UM policies/procedures and UM
processes. e PPG shall maintain a log for requests of
UM Criteria and report the number and types of UM
Criteria requests annually to their UM Committees.
5.19 Use of Board Certied Consultant
to assist in making UM Decisions based
on Medical Necessity and covered
Medical Benets
L.A. Care provides a description of guidelines for the
use of Board Certified Consultants to assist in making
UM decisions based on medical necessity, covered
medical benefits as defined in the member’s Evidence
of Coverage (EOC), and care or services that could be
considered either covered or non-covered, depending
on the circumstances. L.A. Care has access to a broad
range of contracted medical, pharmaceutical, and
behavioral health practitioners in various specialties
and subspecialties in Los Angeles County available for
verbal and written consultation.
L.A. Care also maintains a contract with an outside
vendor for various services, including use of Board
Certified Consultants, who are available for review
upon request. If the Board Certified Consultant is
from the contracted vendor that L.A. Care uses to
obtain the services of a Board Certified Consultants
(i.e. non-L.A. Care physician/peer reviewer), the
consultant shall provide advice that the UM Medical
Director/peer reviewer considers in making his/her
UM decision. Non-L.A. Care consultants cannot
make a denial decision.
5.20 Notication Process for UM
Decisions (See Attachment A, L.A. Care
UM Timeliness Standards)
Notifications of UM decisions are made in accordance
with all current regulatory requirements as described
for each line of business in the most current UM
Policies and Procedures. For PPGs delegated to
perform UM functions, the PPG is responsible for
member and provider notifications.
PPGs are required to notify members and providers of
UM determinations related to approvals, modifications,
deferrals (pended) or denials. Providers should be
notified of determinations by phone within 24 hours
of the determination. e written determination must
be mailed to the Member and Provider within two (2)
business days of the determination.
For services that are the financially responsibility of the
PPG hospital shared risk pool is managed by L.A. Care:
• PPGS with standard delegation
°
PPG managing an outpatient referral and
using a contracted L.A. Care facility; PPG UM
Department is responsible for notifying the
member, the requesting provider, the rendering
provider and the PCP.
°
When PPG must utilize a non-L.A. Care facility,
PPG will hold the determination and route
the request to L.A. Care’s UM Department for
review/determination. NOTE: Decision-making
timeframe is within the 5 business days of
receipt of the information necessary to make the
information:
Upon final determination, L.A. Care will notify
the PPG UM Department, of the determination
and
PPG UM Department is responsible for
notifying the member, the requesting provider,
the rendering provider and the PCP.
°
For requests with insufficient information to make
the determination AND additional information is
necessary to make an appropriate determination,
the PPG will issue a deferral notification. e
deferral must be communicated, completed before
the 5th calendar day of receipt of the request
and approved by the Member and Provider; the
notification must include the reason for the delay
and a date the request will be completed (must be
within the 14 calendar days of the request), the
L.A. Care UM Department will notify the PPG
UM Department and the member.
46
• PPGs with Extended Delegation
°
PPG is responsible for processing the request,
notifying the appropriate providers and
documentation of notification to the providers and
members as defined in attachment A, L.A. Care
UM Timeliness standards matrix
°
PPG will notify L.A. Care as defined in the PPG
contract agreements (i.e. electronic file exchange or
Excel file logs).
5.21 L.A. Care’s CAPitation Deduction
Process for PPGs:
Should a Standard delegated PPG authorize a service
that is L.A. Care’s financial responsibility according
to the DOFR, L.A. Care will honor the authorization
request and pay the claim, but as defined in the PPG
Service Agreement, services are subject to capitation
deduction from the PPG monthly capitation (See PPG
contract Section 1.22 E). L.A. Care will notify the
PPG and L.A. Care’s Provider Network Management
Department when a determination is made that a
service is eligible for capitation deduction, commonly
known as CAP deduct.
5.22 Rescission or Modication of an
Authorization after a Service has been
provided is not allowed
PPG shall not rescind or modify an authorization after
the provider renders the health care service in good
faith for any reason, including, but not limited to,
subsequent rescissions, cancellations or modification of
the member’s contract, or when the PPG did not make
an accurate determination of the member’s eligibility.
5.23 Delay, Denial, Modication, and
Termination Determinations/Notice of
Action Letters
PPGs are required to utilize the most recent version
of the UM Notice of Action Letters (NOA’s) specific
to the Medi-Cal. Copies of the template letters
are provided to the PPG or may be obtained by
contacting the L.A. Care UM Department.
5.24 Reference to Basis of UM
Determination
e following are included in a UM Notice of
Action Letter:
• Clear documentation and communication of the
reasons for the determination so that Members and
Providers receive sufficient information in easily
understandable language to be able to understand the
decision and decide whether to appeal the decision
• A reference to the UM criteria, citation (when
applicable), or benefit provision on which the
decision is based
• Information about how the member, upon request,
can obtain a copy of the actual UM criteria or
benefit provision on which the decision was based.
5.25 Contacting the Peer Reviewer
(Reconsideration)
All UM Notice of Action correspondences sent to
the requesting PCP or specialist shall include a name
and phone number for contacting the Peer Reviewer
in order to allow the requesting practitioner the
opportunity to discuss issues or concerns regarding
the decision. A requesting practitioner may call
L.A. Care to discuss a denial, deferral, modification,
or termination decision with the physician (or
peer) reviewer, or may write to supply additional
information for the physician (or peer) reviewer.
To file a reconsideration of a UM determination,
the reconsideration must be filed by the requesting
practitioner within 24 hours of the notice of action.
If a requesting practitioner would like to discuss
L.A. Care denials/modifications decisions with the
physician (or peer) reviewer, please call L.A. Care’s
UM Department at 1.877.431.2273.
L.A. Care’s UM Department responds to
reconsideration requests within one (1) business day of
the receipt of the requesting practitioner telephone call
or written request. If the physician (or peer) reviewer
reverses the original UM determination based on the
discussion with, or additional information provided
by the requesting practitioner, the case will be closed.
If reconsideration does not resolve a difference of
opinion, and the previous UM determination remains
or a modification results, or the requesting practitioner
does not request reconsideration, the requesting
practitioner may submit a request for review through
the appropriate practitioner dispute processes or may
appeal on behalf of the member, if appropriate.
5.25 Practitioner Appeal Processes – How
to Dispute an Adverse Determination
Process for Filing a Formal Appeal
If a requesting practitioner believes that a
determination is not correct, he/she has the right to
appeal the decision on behalf of the member by filing
47
a grievance with L.A. Care. e requesting practitioner
should submit a copy of the member’s denial notice
and a brief explanation of his/her concern with any
other relevant information to the address below:
L.A. Care Health Plan
Attn: Appeals and Grievance Unit
P.O. Box 811610
Los Angeles, CA 90081
1.888.839.9909
FAX 1.213.438.5748
5.26 Inpatient Concurrent Review
Inpatient concurrent review is usually a coordinated
effort between L.A. Care and the PPG. Once notified,
L.A. Care’s UM staff or its delegate’s will perform
telephone reviews with the hospital staff. Hospital
inpatient care may be pre-planned/pre-authorized
(elective), urgent or an emergency admission. e PCP
is responsible for obtaining required pre-authorizations
for elective inpatient care from the PPG. e PCP
must notify the PPG of an emergency admission.
Concurrent Review is the assessment used to
determine medical necessity or clinical appropriateness
of services as the services are being rendered.
Concurrent review is used for the assessment of the
need for continued inpatient or ongoing ambulatory
care. Concurrent review is generally conducted
telephonically, but may also occur on site. Generally:
• Inpatient concurrent review will begin within one
(1) day of notification of the admission and include
an assessment of the appropriateness of the level of
acute care by using accepted criteria.
• Concurrent review will be conducted periodically
on or before the dates assigned at the end of the
initial review and each subsequent review. For the
applicable timeframes, see the most recent version of
the UM Timeliness Standards matrix; see attachment
A of this Section.
• Concurrent review includes an evaluation of the
following:
°
Appropriateness of acute admission
°
Plan of treatment
°
Level of care
°
Intensity of services/treatment
°
Severity of illness
°
Quality of care
°
Discharge planning
Concurrent Review is the assessment used to
determine medical necessity or clinical appropriateness
of services as the services are being rendered.
Concurrent review is used for the assessment of the
need for continued inpatient or ongoing ambulatory
care. Concurrent review is generally conducted
telephonically, but may also occur on site. Concurrent
review includes, but is not limited to:
• Verifying medical necessity
• Determining approximate length of stay
• Determining appropriate level or intensity of service
and setting of care
• Ensuring access to ancillary care
• Determining and/or changing the level of case
management, when appropriate
• Initiating timely discharge planning activities
ese reviews will be conducted utilizing accepted
guidelines for acute levels of care, such as intensity of
service and severity of illness criteria, MCG Health,
Interqual® or other care guidelines and criteria
developed and/or approved by L.A. Care. PPGs may
perform the management of hospital admissions by
way of a hospitalist program, or retain the services
of a hospitalist. At all times, the hospitalist will
facilitate care with L.A. Care UM staff or its delegate.
Concurrent quality issues (Provider Preventable
Conditions or Serious Reportable Adverse Events)
noted during utilization review will be documented
and reported to the PPG, L.A. Care’s UM Medical
Director and Quality Improvement department.
When appropriate, quality issues will be discussed
with the attending physician by the UM medical
staff for appropriate intervention. Depending on the
urgency or gravity of the situation, discussion of the
issues may also be necessary with L.A. Care’s Senior
Executive Administration.
Utilization review concurrent focus will be proactive,
and UM/Case Management levels of focus will be
employed as appropriate. L.A. Care will coordinate
continued monitoring and management of concurrent
reviews. Whenever possible, L.A. Care will transfer
members admitted to non-contracted hospitals or
hospitals where the PPG does not have hospital
services, to an in-network hospital. Admissions to
non-contracted hospitals – hospitals are reimbursed
based on the most recent DHCS contract
methodology. At this time, L.A. Care utilizes the APR-
DRG Methodology to reimburse non-participating
hospitals with Medi-Cal contracts, which requires
determination of member stability from transition to
an in-network hospital.
48
Concurrent Review/In-patient Hospital Care
Unless defined in the L.A. Care/PPG delegation
agreement, the PPGs is not delegated to perform
concurrent review.
NOTE: Unless delegated for admissions and
concurrent review, the PPG must notify L.A. Care of
all inpatient admissions.
While a member is hospitalized, the PCP must:
• Coordinate, with the assistance of UM staff,
care for members admitted to out of network
facilities for emergency care, or other reasons.
After determination of the appropriateness of an
emergency admission and a transfer assessment
is made, the member will either be transferred
to a network facility or care will be continuously
monitored at the initial facility of admission until
discharge, or a transfer is appropriate.
• Respond to the concurrent review process, including
level of care, length of stay, and medical necessary
elements, when he/she acts as the attending
physician or works in conjunction with the
attending physician for a hospital stay.
• Assist with discharge planning by ordering and
requesting authorization for appropriate elements
of discharge.
ADMISSIONS TO NONCONTRACTED
HOSPITALS MEDICAL ONLY
• Members admitted to non-contracted hospitals
will be managed under the APR DRG, effective
7/1/2013. Admissions to non-contracted hospital
will be assessed for the continued length of stay and
the ability to provide the most appropriate care for
the member.
• If services can be provided in the facility with a
discharge within a total of five (5) days from the
admission date, the member should be maintained
in the same facility
• If the facility is requesting a transfer and the member
will not be discharged within five (5) days from the
admission, or the services needed to care for the
member cannot be met in the current facility, L.A. Care
and it’s delegates will transfer to an in-network provider
or the most appropriate facility to manage the care
California Children’s Service (CCS)
L.A. Care will ensure timely referrals are made to and
for CCS specialists, hospitals and specialty centers
for Members under the age of 21 years who have
conditions eligible for services through CCS.
°
Providers must follow the most recent CCS
Numbered Letter instructions on referral to CCS
paneled hospitals using CCS paneled physicians.
Providers are referred to the DHCS website for
full instructions: http://www.dhcs.ca.gov/Services/
CCS/Pages/default.aspx
• For members admitted to non-CCS paneled facility,
L.A. Care and its delegates will ensure timely
referrals are made to CCS and CCS staff informed of
the member’s stability for transfer as needed. Once
stable, L.A. Care or its delegates will obtain approval
to transfer to an appropriate CCS-paneled center.
• L.A. Care and its delegates will ensure, the cases where
CCS is pending a determination, L.A. Care
will approve medically necessary services as needed.
Authorization documentation will evidence
appropriate decision-making pending the final CCS
decisions; decisions will not be held pending CCS
final decisions. Once the CCS decision is made,
the authorization/referral will be updated in the
appropriate information system to reflect the decision
and the CCS Service Authorization Referral (SAR)
Discharge Planning
• L.A. Care’s UM staff will begin discharge planning
within 24 hours of notification of admission and
will facilitate the involvement of a multidisciplinary
team of physicians, nursing, social work, and others,
as appropriate.
• Patient and family intervention will occur, as
appropriate, throughout the stay to assure discharge
plans are in place and appropriate for each member.
Discharge plans will consider the disease process,
treatment requirements, the family situation,
available benefits and community resources.
• Average length-of-stay guidelines will be used for
discharge planning purposes. Discharge screens,
lower level of care guidelines, or clinical decision
made by the physician are to be used for the final
discharge date plan.
• Questionable continued stay plans are to be
discussed with the attending physician and then
reviewed by L.A. Care’s physician reviewer for
further discussion with the attending physician.
NOTE: For SPD members, PPGs delegated for
concurrent review must maintain a provision for
discharge planning when a SPD member is admitted
to a hospital or institution and continuing into the
post discharge period. Discharge planning shall
include ensuring that necessary care, services, and
supports are in place in the community for the SPD
49
member once they are discharged from a hospital
or institution, including scheduling an outpatient
appointment and/or conducting follow-up with the
patient and/or caregiver. Minimum criteria for a
discharge planning checklist must include:
• Documentation of pre-admission status, including
living arrangements, physical and mental function,
social support, durable medical equipment and other
services received
• Documentation of pre-discharge factors, including
an understanding of medical condition by the
member or a member representative of the SPD
member as applicable, physical and mental function,
financial resources, and social supports
• Services needed after discharge, type of placement
preferred by the SPD member/representative of
the member/representative, specific agency/home
recommended by the hospital, specific agency/home
agreed to by the SPD member/representative and
pre-discharge counseling recommended
• Summary of the nature and outcome of the
SPD member/representative involvement in the
discharge planning process, anticipated problems
in implementing post-discharge plans, and further
action contemplated by the hospital/institution.
Transition of Care (TOC) – PPGs delegated for
concurrent review must maintain a discharge planning
process or transition to the next level of care that
includes a workflow and supportive documentation for
communication to the primary care provider, SNF
or specialist.
TOC Programs
Successful transition programs include:
• A standardized TOC program elements to reduce
variability in processes and outcome
• Use of an readmission risk stratification tool
designed for this population is essential
°
Perform early in the admission (within 1 business day)
°
Must assess for social determinates
°
Ability to focus intense resources where they are
most needed
• Medication reconciliation at discharge is essential
• For highest risk, form a TOC team to closely follow
the member until care is fully transitioned to the
receiving provider
°
At a minimum, include hospitalist, case manager
and PCP or receiving physician in TOC team
TOC documentation should ensure:
• Documentation of status of admission, planned
or unplanned
• Date reflecting the notification of the admission
• Name of staff member assigned to manage the
transition
• Date TOC record (care plan) is shared to next care
setting or usual care practitioner
• Date of notification sent to the PCP or usual
practitioner
• Date Member or Member’s family notified of the
transition
• Diagnosis
• Follow up apt with usual practitioner (should be
within 10 days of admission, but no later than 30 day)
• If member readmitted, date of last admission
• Length of stay in the most recent hospital (related to
the reported admission)
• Date of notification to L.A. Care of the admission
Emergency Admission Notification
PPGs that are not Dual Risk, Full Risk or do not
have extended delegation must report all elective and
emergency inpatient admissions to L.A. Care’s UM
department within 24 hours of the admission. ese
notifications may occur by calling in or faxing the
patient’s admission face sheet to the following:
1.877.452.CARE (1.877.452.2273)
Fax: 1.213.438.5777
Maternity Length of Stay
L.A. Care and/or PPGs shall have procedures in
place that require members who deliver vaginally,
or by caesarean section, to be provided appropriate
maternity benefits as required by the Newborn and
Mother Health Act of 1997. Prior authorization is not
required for these benefits as follows:
• Postpartum stay of 48 hours following normal
vaginal delivery
• Postpartum stay of 96 hours following caesarean
section delivery
NOTE: For PPGs managing the concurrent review,
L.A. Care’s Auto Authorization policy allows for up
to 48 hours pre-delivery inpatient services while the
member is in active labor. If more than 48 hours pre-
delivery have occurred, services should be reviewed
based on medical necessity.
Decisions to discharge mothers/newborns earlier than
48 or 96 hours post-delivery are to be made by the
treating physician in consultation with the mother and
must include appropriate documentation for follow-up
plans in the member’s medical record.
50
When the mother/newborn are discharged prior to
48 hours for vaginal delivery/96 hours for cesarean
section delivery, L.A. Care and/or PPGs shall cover a
post discharge follow-up visit, when agreed to by the
mother and ordered by the treating physician. A post
discharge follow up visit must occur within 48 hours
of discharge or 96 hours post cesarean section, when
prescribed by the treating physician.
e treating physician, in consultation with the mother,
shall determine whether the visit will occur at home
by a home health nurse or whether the member shall
see the physician in the physician’s office. e visit
shall be provided by a licensed health care provider
whose scope of practice includes postpartum care and
newborn care. e visit shall include parent education,
assistance and training in breast or bottle-feeding, and
the performance of any necessary maternal or neonatal
physician assessments. L.A. Care’s PCPs and OB/GYN
providers are expected to provide written notification
of these maternity benefits to members during prenatal
care. L.A. Care shall provide written notification of
these maternity benefits to members through the EOC.
Maternity Kick Payment Reporting (Medi-Cal)
PPGs and providers are required to report live births
to ensure accuracy of reporting and reconciliation of
maternity kick payments.
POST SERVICE
Post Service (Retrospective Review) is the assessment
of the appropriateness of medical services after the
services have been provided. Post Service Review is
conducted when there has been no notification or
request for review prior to services being rendered.
Decisions are based on medical necessity and
appropriateness of care using UM Criteria and the
member’s benefit structure.
Post Service Review includes, but is not limited to:
• Reviewing for medical necessity and clinical
appropriateness of services in those instances where
authorization was not obtained. ese services are
usually related to the urgency of the care provided.
• Reviewing for eligibility and benefit coverage.
RETROSPECTIVE CLAIM REVIEW
Retrospective Claim Review is the assessment of
the appropriateness of medical services related to
a provider/facility claim. Retrospective Review
is conducted in collaboration with the Claims
Department and subject to the review timelines
associated with the Claims Department. Decisions are
based on medical necessity and appropriateness of care
using UM Criteria and the member’s benefit structure.
Retrospective Claim Review includes, but is not
limited to:
• Reviewing for medical necessity and clinical
appropriateness of services in those instances where
authorization was not obtained.
• Reviewing for eligibility and benefit coverage at the
time of service.
Retrospective Claim reviews determination is
made within 30 calendar days of the request or the
regulatory requirement for claims processing.
SECOND OPINION PROCESS
e second opinion program provides members
and providers with the ability to validate the need
for specific procedures. e use of screening criteria
will be employed in addition to securing a second
physician consult, when necessary. Second opinions
will be rendered by an appropriately qualified health
care professional identified as a primary care physician
or a specialist who is acting within his or her scope
of practice, and who possesses clinical background,
including training and expertise related to the particular
illness, disease, condition or conditions associated with
the request for a second opinion. Second opinions shall
be provided to L.A. Care Medi-Cal members at no cost.
PPGs shall maintain policies to ensure second opinion
request will be processed in accordance with the State
regulatory requirements. PPGs requiring assistance in
locating a specialist for assistance in processing requests
for second opinions may contact the L.A. Care
UM Department.
STANDING REFERRAL PROCESS
PPGs must maintain a process for a Member with a
condition or disease that requires specialized medical
care over a prolonged period of time and is life-
threatening, degenerative, or disabling to receive a
referral to a specialist or specialty care center that
has expertise in treating the condition or disease for
the purpose of having the specialist coordinating the
Member’s health care.
A standing referral is a referral made by the PCP for
more than one (1) visit to a specialist or specialty care
center as indicated in an approved treatment plan
for a particular diagnosis. A member may request a
standing referral to a specialist through his/her PCP
51
or through a participating specialist. e standing
referral request will be made in collaboration with the
PCP, the treating specialist, and the L.A. Care Medical
Director or the delegate.
If a treatment plan is necessary in the course of care
and is approved by L.A. Care, in consultation with
the PCP, specialist and member, a referral shall be
made in accordance with the recommended treatment
plan. A treatment plan may be deemed unnecessary
if L.A. Care approves a current standing referral to a
specialist. e treatment plan may limit the number
of visits to the specialist, limit the period of time that
the visits are authorized, or require that the specialist
provide the PCP with regular reports on the health
care provided to the member.
Standing referrals do not require L.A. Care, or it’s
delegates, to refer to a specialist who, or to a specialty
care center that, is not employed under contract
with L.A. Care or the delegate to provide health care
services to members unless there is not a specialist
within the network that is appropriate to provide
treatment to members as determined by the PCP and in
collaboration with the L.A. Care Medical Director, or
their designee, as documented in the treatment plan.
L.A. Care maintains a referral management process
and may delegate the referral management process to
delegated entities. PPGs shall maintain policies and
procedures for referral management that include review
of standing referrals for members who require specialty
care or treatment for a medical condition or disease that
is life threatening, degenerative, or disabling.
Authorization determinations for specialty referral/
services shall be processed in accordance with
L.A. Care and/or its delegated entity policies and
procedures for referral management within required
time frames for standing referrals, as described in this
procedure. Services shall be authorized as medically
necessary for proposed treatment identified as part of
the member’s care treatment plan utilizing established
criteria and consistent with benefit coverage. Once
a determination is made, the referral shall be made
to the Specialist within four (4) business days of the
date the proposed treatment plan, if any, is submitted
to the physician reviewer. e duration of a standing
referral authorization shall not exceed one year at a
time, but may be renewed for periods of up to one
year, if medically appropriate.
Credentialing Requirements
e specialty provider/special care center shall be
credentialed by and contracted with L.A. Care or
its delegated entities’ network to provide the needed
services. If standing referrals are made to providers
who are not contracted with L.A. Care or its delegated
entity network, L.A. Care and/or its delegated entities
shall make arrangements with that provider for
credentialing prior to services rendered, appropriate
care coordination, and timely and appropriate
reimbursement.
In approving a standing referral, in-network or out-of-
network, L.A. Care and PPGs delegated for UM will
take into account the ability of the member to travel
to the provider. PPGs can request assistance from
L.A. Care for locating a specialist (See Specialty Care
Liaison Program Procedure).
HIV/AIDS Referrals
When authorizing a standing referral to a specialist
for the purpose of the diagnosis or treatment of
a condition requiring care by a physician with a
specialized knowledge of HIV medicine, PPGs
shall refer the member to an HIV/AIDS specialist.
When authorizing a standing referral to a specialist
for purposes of having that specialist coordinate the
member’s health care, who is infected with HIV/
AIDS, PPG shall refer the member to an HIV/AIDS
specialist. e HIV/AIDS specialist may utilize the
services of a nurse practitioner or physician if:
• the nurse practitioner or physician assistant is under
the supervision of an HIV/AIDS specialist; and
• the nurse practitioner or physician meets the
qualifications specified in the state regulations; and
• the nurse practitioner or physician assistant and the
provider’s supervising HIV/AIDS specialist have the
capacity to see an additional patient
Care Coordination
e PCP shall retain responsibility for basic case
management/coordination of care unless a specific
arrangement is made to transfer care to the specialist
for a specified period of time, in accordance with the
PPG contract with L.A. Care. NOTE: Requests for
standing referrals will be processed in accordance with
state regulatory requirements.
COORDINATION OF MEDICALLY
NECESSARY SERVICES
e PCP is responsible for providing members with
routine medical care and serves as the medical case
52
manager within each managed care system. Referrals
are made when services are medically necessary,
outside the PCP’s scope of practice, or when members
are unresponsive to treatments, develop complications,
or specialty services are needed. e PCP is responsible
for making referrals and coordinating all medically
necessary services required by the member. Pertinent
summaries of the member’s record should be
transferred to the specialist by the PCP. Authorization
flow charts are provided at the end of this section.
OUTPATIENT REFERRALS AND SPECIALTY
REFERRAL TRACKING
Prior Authorization Specialty Referral Tracking
Systems PPGs are required to maintain a system
to track and monitor specialty referrals requiring
prior authorization. e system tracks the decision
(authorization, denial, deferral, modification, and
termination) and the timeliness of the decision.
L.A. Care ensures that all contracting health care
practitioners are aware of the referral processes and
tracking procedures.
If the PCP determines that a member requires
specialty services or examinations outside of the
standard primary care, the provider must request
for these services to be performed by appropriate
contracted providers. e provider must ensure the
following steps in coordinating such referrals:
• Submit a referral request to the PPG or the
designated hospital physician to obtain authorization
for those services
• e PPG will process the request or contact the
L.A. Care UM department to obtain authorization
for the facility component of services needed, as
appropriate
• After obtaining the authorization(s):
°
PCP/PPG is responsible for notifying and referring
the member to the appropriate specialist or facility
°
e PCP, office staff, or member may arrange the
referral appointment
°
Note the referral in the member’s medical record
and attach any authorization paperwork
°
Discuss the case with the member and the
referral provider
°
Receive reports and feedback from the referral
provider regarding the consultation and treatment.
NOTE: A written report must be sent to the PCP
by the referral provider, or facility the member was
referred to.
°
Discuss the results of the referral, any plan for
further treatment, and care coordination with the
member, if needed
Referrals should be tracked by the PCP’s office and
authorizing PPG for follow-up through a tickler file,
log or computerized tracking system. e log or
tracking mechanism should note, at a minimum, the
following for each referral:
• Member name and identification number
• Diagnosis
• Date of authorization request
• Date of authorization
• Date of appointment
• Date consult report received
Receipt of Specialist’s Report
e PCP must ensure timely receipt of the specialist’s
report (e.g. use of tickler file). Reports for specialty
consultations or procedures should be in the member’s
chart within a given timeframe, usually two (2) weeks.
If the PCP has not received the specialist’s report within
the determined timeframe, the PCP should contact the
specialist to obtain the report. For urgent and emergent
cases, the specialist should initiate a telephone report to
the PCP as soon as possible, and a written report should
be received within two (2) weeks.
SPECIALIZED DURABLE MEDICAL
EQUIPMENT WHEELCHAIRS
Medi-Cal covers a wheelchair if it is needed to:
• Prevent significant illness or disability
• Ease severe pain
• Maintain bodily functions needed to perform
daily activities
Medi-Cal does not cover a wheelchair if a
household or furniture item could otherwise serve
the member’s needs.
Providers are required to obtain prior authorization
from L.A. Care for:
• e purchase or a rental of standard and custom
wheelchair
• e repair of a standard or custom wheelchair that
exceeds $250
To ensure member safety and the appropriate
equipment is provided, L.A. Care requires an
evaluation by a physiatrist or physical therapist and an
in-home assessment be submitted at the time of the
referral request.
e following description outlines how providers
should request authorization for purchase or rental of a
53
standard or custom wheelchair, as well as for the repair
of a wheelchair.
HOW TO REQUEST AUTHORIZATION OF A
STANDARD WHEELCHAIR
PPGs Dual or Full Risk
PPG is responsible for the decision making, care
coordination and financial reimbursement for the
wheelchair. PPG will approve, modify or deny the
request for a standard wheelchair in accordance with
L.A. Care Policies.
PPGs – Shared Risk with Standard Delegation:
PPG should submit the Authorization Request Form
to the L.A. Care’s UM Department. L.A. Care will
approve, modify or deny the request for a standard
wheelchair in accordance with L.A. Care Policies.
PPGs – Shared Risk with Extended Delegation:
PPG process the request using a L.A. Care contracted
ancillary provider in accordance with L.A. Care Policies.
For Member in need of a standard wheelchair, the
member’s PCP or specialist should complete an
Authorization Request Form. In completing the form,
please be sure to supply the following information:
• Member’s name, date of birth, phone number,
address and Medi-Cal identification number
• Full name, address, telephone number and signature
of the prescribing provider
• Date of request
• Diagnosis codes
• Specific item(s) requested, including Healthcare
Common Procedure Coding System (HCPCS)
codes
• Identify rental (short term usage – less than 8
months) versus purchase (long term usage – more
than 8 months)
• Copy of physiatrist or physical therapist evaluation
HOW TO REQUEST AUTHORIZATION OF A
CUSTOM WHEELCHAIR
L.A. Care does not delegate the UM decision making
for customized wheelchairs to PPGs with standard
delegation; PPGs with Extended Delegation, contact
L.A. Care’s UM Department for information on the
contracted vendor for in-home assessments
PPGs should complete an Authorization Referral
form, Customized Wheelchair Evaluation
Request (CWER) form and Wheelchair Clinical
Questionnaire. Contact L.A. Care UM Department
to obtain copies of these forms: Custom Wheelchair
Evaluation Request (CWER) and Wheelchair
Clinical Questionnaire.
In completing the form, please be sure to supply the
following information:
• Member’s name, date of birth, phone number,
address and Medi-Cal identification number
• Full name, address, telephone number and signature
of the prescribing provider
• Date of request
• Diagnosis codes
• Specific item(s) requested, including Healthcare
Common Procedure Coding System (HCPCS) codes
• Copy of physiatrist or physical therapist evaluation
• Member’s medical condition or diagnosis
necessitating the custom wheelchair, including
functional limitations and a description of how the
custom wheelchair would improve the member’s
medical status or functional ability
PPG should fax the CWER and Clinical Questionnaire
to L.A. Care’s UM Department at 1.213.438.5777. All
requests for custom wheelchairs must obtain an in-
home assessment or have received an evaluation for in-
home and out of home evaluation through a recognized
wheelchair seating clinic. L.A. Care will approve,
modify or deny the request for a standard wheelchair in
accordance with L.A. Care Policies. For referral
request submitted without adequate information,
L.A. Care UM Department staff will notify the member
and provider of the need to defer the decision allowing
time for an in-home assessment; the referral will be
completed within the 14 days of the submitted request.
Request for a customized wheelchair evaluation will
be accompanied by an evaluation by a contracted
Evaluation Service Provider to arrange for an
assessment of the member. e Evaluation Service
Provider will assess the member and the medical
necessity of a customized wheelchair based upon
criteria, based upon the member’s medical needs and
living environment. e Evaluation Service Provider
will submit a letter of recommendation based upon
its initial assessment of the member to L.A. Care UM
Staff. If the Evaluation Service Provider’s letter of
recommendation varies from the provider’s original
request, it will be reviewed by L.A. Care’s Medical
Director for the final determination. If L.A. Care
approves a customized wheelchair, L.A. Care will make
arrangements with a selected wheelchair provider.
e wheelchair provider will arrange for a fitting
54
appointment with the member. For more information,
please see Custom Wheelchair Request and Approval
Process - Provider Fact Sheet. To obtain a copy of
this attachment, Custom Wheelchair Request and
Approval Process - Provider Fact Sheet, contact
L.A. Care’s UM Department at 1.877.431.2273.
HOW TO REQUEST AUTHORIZATION OF A
WHEELCHAIR REPAIR
PPGs Dual or Full Risk
PPG is responsible for the decision making, care
coordination and financial reimbursement for the
wheelchair. PPG will approve, modify or deny the
request for the wheelchair repair in accordance with
L.A. Care Policies.
PPGs – Shared Risk with Standard Delegation:
PPG should submit the Authorization Request Form
to the L.A. Care’s Utilization Management (UM)
Department. L.A. Care will approve, modify or deny
the request for a standard wheelchair in accordance
with L.A. Care Policies.
PPGs – Shared Risk with Extended Delegation:
PPG processes the request using an L.A. Care
contracted ancillary provider.
Wheelchair repair requests with a cumulative cost
less than $250 that do not utilize miscellaneous or
“by report” codes, and that do not exceed frequency
limitations, do not require prior authorization.
If a member requires a wheelchair repair costing more
than $250 that does not utilize miscellaneous or “by
report” codes, PPG should complete an authorization
request form. If a wheelchair repair costing more
than $250 that does not utilize miscellaneous or “by
report” codes, the PPG should complete a Wheelchair
Repairs Authorization Request Form. Contact L.A.
Care’s UM Department to obtain a copy of this form:
Wheelchair Repairs Authorization Request.
In completing the form, please be sure to supply the
following information:
• Member’s name, date of birth, phone number, address
and Medi-Cal identification number
• Full name, address, telephone number and signature
of the prescribing provider
• Date of request
• Diagnosis codes
• Specific item(s) requested, including Healthcare
Common Procedure Coding System (HCPCS) codes
• Description of the repair or maintenance required
PPG should fax the Wheelchair Repairs Authorization
Request Form to L.A. Care’s UM Department at
1.213.438.5777. L.A. Care UM staff review the
request for benefit coverage, frequency limits and
medical necessity. L.A. Care U.M. Department will
approve, modify or deny the request for wheelchair
repair in accordance with L.A. Care Policies.
TUBERCULOSIS TREATMENT SERVICES
PROVIDED BY PRIMARY CARE PROVIDER
PPG shall have established programs for ensuring that
basic care for tuberculosis is provided to members
at the primary care provider level through basic case
management services. PPG shall ensure that primary
care providers provide TB care and treatment in
compliance with the guidelines recommended by
American oracic Society and the Centers for Disease
Control and Prevention to include, but not limited to:
• TB screening
• TB diagnosis
• TB treatment
• TB follow-up
PPG shall ensure that primary care providers
coordinate with Local Health Department in the
referral of members requiring Tuberculosis Direct
Observed erapy, a linked and carved out service
available through the Local Health Department (See
L.A. Care UM Procedure 17046 Tuberculosis, Directly
Observed erapy (DOT).
CERVICAL CANCER SCREENING
PPGs shall have procedures to provide for Cervical
Cancer Screening, a covered preventive health benefit
for L.A. Care members. e coverage for an annual
Cervical Cancer Screening test shall include the
conventional Pap test, a human papillomavirus (HPV)
screening test that is approved by the federal Food and
Drug Administration, and the option of any Cervical
Cancer Screening test approved by the federal Food
and Drug Administration. e referral is made by
the Member’s health care provider (PCP or treating
physician, a nurse, practitioner, or certified nurse
midwife, providing care to the member and operating
within the scope of practice otherwise permitted for
the licensee).
PPGs shall ensure that routine referral processes
are followed when the member requests a human
papillomavirus (HPV) screening test, in addition to
the conventional Pap test, that is approved by the
Federal Food and Drug Administration, and the

55
option of any Cervical Cancer Screening test approved
by the Federal Food and Drug Administration.
HEALTH RISK ASSESSMENT HRA
e Health Risk Assessment (HRA) is a standardized
screening tool to collect L.A. Care members’ self-
reported information about their health and well-
being. e HRA information is used as an initial
determination of a care management risk level and as
a starting point to guide further assessment questions
which lead to the formation of an Individualized Care
Plan. e HRA is generally conducted telephonically
with the assistance non-clinical support staff or by
mail if the member is unable to be reached by phone
or by member preference.
A Health Risk Assessment is conducted for:
• Seniors and Persons with Disabilities (SPD)
members within the first 45 days (high risk) or 105
days (low risk) of enrollment and reassessments
at least annually, Reassessments of member risk
level is performed by L.A. Care through a monthly
predictive modeling report, designed to identify
members with complex needs.
HRAs reports are accessible through the L.A. Care
Portal for Provider Groups and by request. e report
is used to identify members who have completed the
HRA. e HRA responses are contained in L.A.
Care’s vendor system (C3). Access to C3 is granted
to all PPGs and Providers after submitting the request
through the Provider Network Liaison contact.
Responses to the HRAs result in a generic care plan.
Staff responsible for the care management will utilize
the generic care plan, additional care management
assessments and member responses to develop the
formal individualized care plan (ICP).
L.A. Care’s Care Management staff is responsible
to review High Risk HRA results, complete the
ICP and convene an Interdisciplinary Care Team
(ICT meeting) per regulatory guidance. e PPG
Care Management staff is responsible to review the
Moderate and Low Risk HRA results and develop
an ICP according to the member’s needs. e HRA
results and developed ICPs are shared with the PCP.
DEVELOPING INDIVIDUALIZED
CARE PLAN GOALS
Prioritized goals consider the member/caregiver
goals, preferences and desired level of involvement
in the ICP. Goals should be “SMART” - Specific,
Measureable, Actionable, Realistic, Time-bound.
Care Plans must document the identification and
management of barriers to member goals:
• Understanding the member’s condition and
treatment
• Desire to participate in the case management plan
• Belief that their participating will improve their
health
• Financial or transportation limitation that may
hinder participating in care
• Mental and physical capacity
ICPs must also contain an assessment of goals and
progress (documented as ongoing process). In addition
to the member’s self-reported outcomes and health
data to assess if member goals are being met. is
includes but is not limited to:
• Utilization data
• Preventive health outcomes
• Pharmacy data
e ICP is updated as often as necessary, reflecting if
goals are met ,not met or revised.
Timing of the ICP
e ICP will be reviewed and revised by the
designated Care Manager (at a minimum):
• At least annually
• Upon notification of change in member status
scheduled follow-up
For High Risk members, the ICP is reviewed during
ICT meetings and in accordance with scheduled
follow-up on member goals. e ICP should be
developed within 30 days of HRA completion.
Individualized Care Team
e member’s ICT should be comprised of appropriate
staff to meet the needs identified during the care
plan discussions. Composition of ICT based on
identified needs (e.g., PCP, Specialist, PPG CM, and
Social Worker). Member or Members designated
representative should be invited to participate in the ICT
as feasible. ICT lead team members are responsible for
documenting the operation detail and communication
(meeting dates-phone call and follow up).
e outcome of the ICT meeting is shared with
the members (dissemination of ICT reports to all
stakeholders).
At a minimum the ICT meeting minutes require:
• the date of meeting
• names and roles of attendees

56
• fact that Member or member representative was invited
• topics discussed
• any revision to the ICP
CARE MANAGEMENT: CARE AND
CASE MANAGEMENT MAY BE USED
INTERCHANGEABLY
Case Management relates to the coordination of
care and services provided to members to facilitate
appropriate delivery of care and services (NCQA).
Care Management (CM) is a collaborative process
that assesses, develops, implements, coordinates,
monitors, and evaluates care plans designed to
optimize members’ health care across the care
continuum. It includes empowering members
to exercise their options and access the services
appropriate to meet their individual health needs,
using communication, education and available
resources to promote quality outcomes and optimize
health care benefits.
L.A. Care’s Care Management Program includes
five levels:
• Basic Care Management
• Care Coordination
• High Risk Care Management
• Complex Care Management
• Targeted Care Management
All Care Management programs are free and providers
are encouraged to refer their members according to the
identified need.
Basic Care Management
e Primary Care Physician (PCP) is responsible for
Basic Care Management for his/her assigned members.
e PCP is responsible for ensuring that members
receive an initial screening and health assessment,
which initiates Basic Medical Care Management.
e PCP conducts the initial health assessment (IHA)
upon enrollment, and through periodic assessments
provides age-appropriate periodic preventive
health care according to established preventive
care guidelines. e PCP also makes referrals to
specialists, ancillary services, and linked and carved
out services, as needed, based on the member’s
individual treatment plan. e PPG supports the
member and PCP through the referral management
process. Members whose care management needs do
not exceed basic case management are considered low
risk and care management activities such as follow
up on Health Risk Assessment results (as applicable).
PPGs are responsible for developing, updating the
Individualized Care Plan (ICP) and organizing an
Interdisciplinary Care Team (ICT) as warranted.
Care Coordination
L.A. Care’s Care Management Program is a member
advocacy program designed and administered to assure
that the member’s healthcare services are coordinated with
a focus on continuity, quality and efficiency in order to
produce optimal outcomes. Members who are Low and
Moderate Risk level primarily receive care coordination
and care management services through the PPG CM
staff. ese activities include review of the HRA results
(SPD), completing and updating an Individualized Care
Plan(ICP) as well as organizing an Interdisciplinary Care
Team(ICT) meeting as warranted.
Care coordination by Care Managers or designated
staff is provided for members needing assistance
in coordinating their health care services. is
service includes members who may have opted out
of complex care management but have continuing
coordination of health care needs. ese include, but
are not limited to, members assigned to or receiving:
• Out of Area/Network services
• Hospital discharge follow up calls
• Assistance with navigating the managed care system
• Health promotion (e.g. screening tests)
High Risk Care Management (High Risk Level):
High Risk Care Management is provided for members
who have extensive utilization of medical services, have
chronic or immediate medical needs requiring more
management. ese members do not meet criteria for
Complex Case Management (CCM) or have declined
to consent to participate in Complex Case Management
(CCM). e High Risk population is managed by
L.A. Care’s CM staff. Members are managed intensively
at the High Risk level for 30-45 days and then re-
evaluated for possible lower level of CM.
Complex Care Management
L.A. Care retains the responsibility for case
management and does not delegate complex case
management to the PPGs.
e goal of complex case management is to help
members regain optimum health or improved
functional capability, in the right setting and in a
cost-effective manner. It involves comprehensive
assessment of the member’s condition; determination
of available benefits and resources; and development
and implementation of a case management plan with
performance goals, monitoring and follow-up.
57
e program incorporates the dynamic processes
of individualized screening, assessment, problem
identification, care planning, intervention, monitoring
and evaluation. e Care Management Program
uses an interdisciplinary collaborative team (ICT)
approach comprised of patient care management and
education through experienced licensed professionals in
collaboration with the Primary Care Physician and other
disciplines according to the members’ individualized
needs. e ICT may be comprised of the member,
PCP, Specialists, Medical Directors, RN Care Managers,
Clinical Pharmacists, Social Workers and non-clinical
support staff Coordinators, Primary or Specialty Care
Providers and Behavioral Health Specialists.
e team works closely with contracted practitioners
and agencies in the identification, assessment
and implementation of appropriate health care
management interventions for eligible children and
adults with special health care needs, including the
provision of care coordination for specialty and state
waiver programs.
Complex Care Management is provided for members
with extensive utilization of medical services or those
having chronic or immediate medical needs requiring
more management than is normally provided through the
Basic Care Management. Complex Care Management
is a collaborative process between the member, Primary
Care Provider, an RN Care Manager and Interdisciplinary
Care Team (ICT) who provides assistance in planning,
coordinating, and monitoring options and services to
meet the Member’s health care needs.
L.A. Care’s Care Management team is responsible
for working collaboratively with all members of
the health care team including the PCP, hospital
discharge planners, specialty practitioners, ancillary
providers, community and state resource staff. e
Care Managers, in concert with the health care team,
focus on coordinating care and services for members
whose needs include preventive services, ongoing
medical care, rehabilitation services, home health and
hospice care, and/or require extensive coordination of
services related to linked and carved out services or the
coordination and/or transfer of care when “carved-out”
services are denied.
Care Managers assist in assessing, coordinating,
monitoring, and evaluating the options and services
available to meet the individual needs of these
members across the continuum. e essential
functions of the Care Manager include:
• Assessment
• Care Planning
• Interventions
• Coordination and Implementation
• Monitoring/Evaluation
• Facilitation
• Advocacy
L.A. Care’s Care Managers provide the care
management activities for the complex and High
Risk members which includes reviewing HRA results,
completing the ICP with the member and ICT and
organizing and leading the ICT. Communication with
the PPG and PCP is an important component in the
collaborative process and interdisciplinary approach.
Referrals to L.A. Care for Complex
Case Management:
Members may be referred for complex case
management by:
• Disease Management (DM) program referrals
• Referrals are received from the DM program
upon identification of complex needs according to
specified CCM program criteria.
• Discharge planner referrals
• Referrals to the CCM program may be made during
the discharge planning process when real or potential
complex needs are identified. ese referrals may
be made by hospital discharge planners or Social
Workers involved in the discharge planning process.
• L.A. Care UM (UM Staff) referrals
• Referrals to CCM are made by UM staff when
complex needs are identified. Identification may
occur during multidisciplinary conferences or during
the concurrent review process.
• Member or caregiver referral
• Members or caregivers are provided with materials
(Member Handbook) containing instructions
on how to self-refer and/or access Complex Case
Management
• Practitioner referrals
°
Contracted Practitioners are provided information
on how to refer for Complex Care Management.
Referrals for case management or care coordination
may be faxed to 1.213.438.5077. A copy of the
referral form may be found at L.A. Care’s website
through http://www.lacare.org/providers/
provider-resources/provider-forms.
• Other referrals including, but not limited to:
• L.A. Care Medical Director Referrals
• PPG Medical Director(s) referrals
• External Service Partners referrals
58
Identifying Members for Care Management:
Multiple sources are used to identify members
who may be a higher risk for adverse outcomes or
transitions from their usual environment to needing
a higher level of care. L.A. Care uses multiple data
sources to identify members that are eligible for the
program but no yet referred.
ese data sources include, but are not limited to:
• Claims and Encounter Data
• Pharmacy Data
• Laboratory Data, when available
• Behavioral Health Joint Operations Report
• PPG Supplemental Reports
• Catastrophic Medical Condition (e.g. Genetic
conditions, Neoplasms, organ/tissue transplants,
multiple trauma)
• Chronic Illness (e.g. Asthma, Diabetes, Chronic
Kidney Disease, HIV/AIDS)
• Data provided by purchasers
• Hospital Utilization
• Hospital discharge data
• Hospital Length of Stay (LOS) exceeding 10 days
• Readmission Reports
• Skilled Nursing facility (SNF), rehabilitation admissions
• Acute Rehabilitation admissions
• Ambulatory Care Utilization Reports
• Emergency Room utilization
• Nurse Advice Line (NAL) Reports/ER Referrals
• Referral Management Reports
• Precertification Data
• Prior Authorization Data
• High-technology home care requiring greater than
two weeks duration of home care
• Long Term Care (LTC) referrals and monitoring logs
• Non-adherence with treatment plan
How to Refer for Complex or High Risk
Care Management:
For more information about L.A. complex case
management or high risk care management programs
or to make a referral, call the L.A. Care CM
Department directly at 1.844.200.0104 and ask
to speak with a Case Manager or complete a CM
Referral Form located on L.A. Care’s website provider
internet page : http://www.lacare.org/sites/default/
files/la1348_061215.pdf or by faxing a request to
1.213.438.5077.
Targeted Care Management
Targeted Care Management (TCM) assists Members
within specific target groups to gain access to needed
medical, social, educational and other services. In
prescribed circumstances, Targeted Care Management
is available as a carve-out Medi-Cal benefit through
the State of California, Los Angeles County Public
Health Department and their contractors as specified
in Title 22, Section 51351. e Care Managers are
responsible for identifying members that may be
eligible for TCM services and must refer members,
as appropriate, for the provision of TCM services.
TCM services are integrated into the overall care
plan, as a barometer for measuring disease progression
and cost of care. State and county TCM services
may include, but is not limited to, Pediatric and
adult partial hospitalization programs (i.e. adult day
health care centers, pediatric day care centers, MSSP,
AIDS Wavier Programs, community based in-home
operation services).
L.A. Care is responsible for co-management of
the member’s health care needs with the TCM
providers, providing preventive health services and
for determining the medical necessity of diagnostic
and treatment services. e TCM services will serve
to supplement care where needed to keep the member
safe within their community based setting.
Targeted Case Management services and how to
refer patients
For more information about targeted case
management, or to make a referral, call the L.A. Care
CM Department at 1.844.200.0104 and ask to speak
with a Case Manager or complete a
MAJOR ORGAN TRANSPLANTS
Medi-Cal – Major Organ Transplants are a carved out
health benefit (See Medi-Cal Linked and Carved out
Services Section)
HOSPICE CARE SERVICES
Hospice Care Services are available to all L.A. Care
members. Members and their families shall be fully
informed of the availability of hospice care as a covered
service and the methods by which they may elect to
receive these services. For individuals who have elected
hospice care, continuity of medical care shall be
arranged, including maintaining established patient-
provider relationships to the greatest extent possible.
L.A. Care and the PPGs shall cover the cost of all
hospice care provided as defined by the DOFR. PPGs
are also responsible for all medical care not related to
the terminal conditions.
59
Members with a terminal condition covered by CCS
must be clearly informed that election of hospice will
terminate the child’s eligibility for CCS services.
Outpatient Hospice Services
MediCal members are eligible for hospice services
without prior authorization. L.A. Care may not
require prior authorization for routine home care,
continuous home care and respite care or hospice
physician services. Hospices shall notify L.A. Care
or it Delegates of general inpatient care placement
that occurs after normal business hours on the
next business day. L.A. Care or it Delegates may
require documentation following the provision of
general inpatient and continuous care for reasons of
justification. If the documentation does not support
these levels of care, or if the documentation included is
inadequate, reimbursement may be reduced to the rate
for routine home care.
Inpatient Hospice Services
Medi-Cal members may be eligible for additional
inpatient hospices services (acute) as described in
MMCD All Plan Letter 05003 Hospice Service and
Medi-Cal Managed Care.
Of the four levels of hospice care as described in
Title 22, CCR, Section 51349 only general inpatient
care is subject to prior authorization. Documents to be
submitted for authorization include:
1. Certification of physician orders for general
inpatient care.
2. Justification for this level of care.
For assistance in accessing this inpatient hospice benefit,
PPGs may contact the L.A. Care UM Department.
Hospice in a SNF setting
Medi-Cal members are eligible for additional hospice
services in a sub-acute setting. Hospice services are
covered cervices and are not LTC services regardless
of the Member’s expected or actual length of stay in a
nursing facility. Hospice and Room and board services
provided in a sub-acute setting are paid by the hospice
provider; L.A. Care will reimburse the hospice provider
as defined in MMCD All Plan Letter 05003 Hospice
Service and Medi-Cal Managed Care.
L.A. Care maintains a network of hospice providers.
Members are not required to utilize a contracted
hospice. In situations where a member or member’s
family elects to utilize a non-contracted hospice
provider or is on services with a non-contracted
provider at the time of enrollment, PPG should contact
L.A. Care’s UM Department for contracting assistance.
L.A. CARE APPEALS PROCESS
L.A. Care does not delegate the appeal process to
PPGs. e PPG must ensure that a timely appeal
process is operational and ensure the submission of
appeals to L.A. Care. Requests for appeals received by
the PPG must be routed to the L.A. Care Member
Services Grievance and Appeals Unit within 24 hours
of receipt at:
L.A. Care Health Plan
Attn: Appeals and Grievance Unit
P.O. Box 811610
Los Angeles, CA 90081
1.888.839.9909
FAX 1.213.438.5748
A member has the right to appeal directly to L.A. Care
for all decisions to modify or deny a request for services.
A physician, acting as the member’s representative, may
also appeal a decision on behalf of the member.
• If the group’s reconsideration process results in a
denial, deferral, and/or modification with which the
provider is still dissatisfied, the provider may request a
formal appeal to L.A. Care for a higher level review.
• Members and providers may also appeal L.A. Care’s
decision to modify or deny a service request (this
does not apply to the retrospective claims review/
provider dispute resolution process). e appeal
request is reviewed by a physician or physician
consultant not involved in the prior determination.
• Member requested appeals may be initiated orally or
in writing.
• Members (and Providers on behalf of Members)
have the right to appeal an adverse
• utilization review determination.
• Members have the right to be represented by
anyone they choose when they appeal an adverse
determination, including an attorney, and have that
representative act on their behalf at all levels of the
appeal. ey can name a relative, friend, advocate,
doctor, or someone else to act for them. Others may
also be authorized under State law to act for them.
• L.A. Care has a full and fair process for resolving
member disputes and responding to member
requests to reconsider a decision they find
unacceptable regarding their care and service. e
process for filing an appeal is made available to the
member in writing through the member handbook
(evidence of coverage), the L.A. Care Web site, and
to the provider through the Provider Manual, the
L.A. Care Web Site, and policies and procedures.
60
• Appeal Procedures provide for:
°
Allowance of at least 90 days for Medi-Cal
members after notification of the denial for the
member to file an appeal.
°
Acknowledgement of the receipt of the appeal
within five (5) calendar days (Acknowledgement
upon receipt by phone, if expedited).
°
Documentation of the substance of the appeal and
any actions taken.
°
Full investigation of the substance of the appeal,
including any aspects of clinical care involved.
°
e opportunity for the member to submit written
comments, documents or other information
relating to the appeal.
°
An authorized representative to act on behalf of
the member.
°
e appointment of a new person to review
the appeal, who was not involved in the initial
determination and who is not the subordinate of
any person involved in the initial determination.
°
e appointment of at least one person to review
the appeal, who is a practitioner in the same or
similar specialty that typically treats the medical
condition, performs the procedure, or provides the
treatment.
°
Notification of the decision of the appeal to the
member within 30 calendar days of receipt of the
request, or 72 hours if expedited.
°
Providing to the member upon request, access
to and copies of all documents relevant to the
member’s appeal.
°
Notification to the member about further appeal
rights.
°
Members who have disagreement with the appeal
decision, and wish to appeal further, have the right
to contact and file a grievance with DMHC, or to
request an Independent Medical Review (IMR).
Standard Review
• Upon receipt of a standard appeal, the UM Specialist
will immediately investigate and inform the Chief
Medical Officer/physician designee.
• An acknowledgment letter will be sent to the
member or provider acting on behalf of the member
within five (5) business days. e letter will include
information regarding the appeals process.
• e physician reviewer will review the standard
appeal and determine if he/she is qualified to make a
determination on the clinical issues presented in
the case.
• If the physician reviewer determines he/she is qualified,
he/she will make a resolution/disposition determination.
• If the physician reviewer determines he/she is not
qualified, he/she will consult with another qualified
professional prior to making a determination.
• e physician reviewer may also contact the provider
requesting services to further discuss the member’s
clinical condition.
• A determination will be made within thirty (30)
calendar days from receipt of the appeal and
information necessary to make a determination.
• Written notification of determination will be sent
within two (2) business days of the determination.
e notification will include:
°
Final determination
°
A statement setting forth the specific medical
and scientific reasons for the determination, and
a description of alternative treatments, supplies,
and/or services as appropriate
°
Reasons other than medical necessity (e.g., non-
covered benefits, etc.) will include the statement of
benefit structure
°
Instructions for appealing further to DMHC will
include DMHC’s address and toll-free telephone
number, as applicable
°
e phone number and extension of L.A. Care’s
physician reviewer
Expedited Review
A member or provider may request an expedited
reconsideration of any decision to deny or modify a
requested service if waiting thirty (30) calendar days for
a standard appeal determination may be detrimental to
the enrollee’s life or health, including but not limited
to, severe pain, potential loss of life, limb or major
bodily function. In the case of an expedited appeal,
the decision to approve, modify, or deny requests by
a provider prior to, or concurrent with, the provision
of healthcare services to members, will be made in a
timely manner that is appropriate for the nature of the
member’s condition and not to exceed 72 hours after
the plan’s receipt of the information.
Upon receipt of an expedited request, the UM specialist
will immediately investigate and inform the physician
reviewer. e physician reviewer will review the expedited
appeal request and determine if he/she is qualified to
make a determination on the clinical issues of the case. If
the physician reviewer determines he/she is not qualified,
he/she will consult with another qualified professional
prior to making a determination. A determination will
be made within the established timeframe from receipt of
the appeal and necessary information.
61
Written appeal acknowledgement/determination
notification will be sent to the member and provider
within 72 hours after the plan’s receipt of the
information reasonably necessary and requested by
the plan to make the appeal determination. e
notification will include:
• e final determination
• A statement setting forth the specific medical and
scientific reasons for the determination, and a
description of alternative treatments, supplies, and/
or services as appropriate
• Reasons other than medical necessity (e.g., non-
covered benefits etc.) will include the statement of
benefit structure
• Instructions for appealing further to DMHC, to
include DMHC’s address and toll free telephone
number, as applicable
• e phone number and extension of the L.A. Care
physician reviewer
Determinations that cannot be completed within
the thirty (30) calendar days for standard appeals,
or within 72 hours for expedited appeals, must be
forwarded to DMHC for final resolution.
State Hearings - Additional Requirements Specific to
the Management of Medi-Cal Member Appeals
Medi-Cal Members or their representative may contact
the State Department of Social Services to request a
State Fair Hearing or an Expedited State Fair Hearing
at any time during the appeal process up to ninety (90)
days from receipt of the denial/modification letter.
Medi-Cal Members also may contact the Office of the
Ombudsman to request assistance with their appeal.
INDEPENDENT MEDICAL REVIEW IMR
A member may request an Independent Medical
Review (IMR) through DMHC to obtain an impartial
review of a denial decision concerning:
• e medical necessity of a proposed treatment.
• Experimental or investigational therapies for a
life-threatening or seriously debilitating disease
or condition.
• Claims for out-of-plan emergency or urgent
medical services.
e application and process for seeking an IMR is
always included with the appeal response notification
letter resulting from upholding a denial or
modification of a request for service.
INITIAL AND PERIODIC HEALTH
ASSESSMENTS FOR ADULTS
PPGs are responsible for maintaining and
disseminating to its Provider Network, protocols
and High Risk Categories by adult age groupings
based on the latest edition of the Guide to Clinical
Preventive Services published by the U.S. Preventive
Services Task Force (USPSTF) for use in determining
the provision of clinical preventive services to
asymptomatic, health adult Members (age 21 and
older). High risk individuals are defined as individuals
whose family history and/or life style indicates a high
tendency towards disease, or who belong to a group
(socioeconomic, cultural, or otherwise) which exhibits
a higher tendency toward a disease.
L.A. Care shall provide lists of new member enrollees
to the PPGs on a monthly basis.
PPGs shall have processes in place to ensure the
provision of an IHA (complete history and physical
examination) to each new adult member (over age 21)
within 120 calendar days that:
• Includes a health education behavioral assessment using
an age appropriate DHS approved assessment tool.
• Makes arrangements for any needed follow-up
services that reflect the findings or risk factors
discovered during the IHA and health education
behavioral assessment.
• Documents the member’s completed IHA and
health education behavioral assessment tool in the
members’ medical record and makes available during
subsequent preventive health visits.
• PPGs shall make reasonable attempts to contact a
member and schedule an IHA. All attempts shall be
documented.
• Documented attempts that demonstrate
unsuccessful efforts to contact a member and
schedule an IHA shall be considered evidence in
meeting this requirement.
• For follow-up on missed and broken appointment
documentation requirements see Section:
Coordination of Medically Necessary Services.
When New Member’s Health does not indicate any
Urgency for an IHA (based on previous medical
records if available):
• If the PCP has access to a new L.A. Care member’s
medical records from a previous Plan or other PCP,
and those records indicate that the member has
had an IHA within the previous 12 months, and
the examination provides evidence that there is no
62
urgency for an IHA, then the visit can be waived
until the next periodic visit is due.
For members whose health status does not indicate
urgency, and if conducting the assessment as part of
the first visit is not feasible, the PCP must contact
the member within 90 days after the member’s first
medical visit to schedule a initial health assessment
appointment.
• PPGs shall ensure that the performance of the initial
complete history and physician exam for adults
includes, but is not limited to:
°
Blood pressure.
°
Height and weight.
°
Total serum cholesterol measurement for men ages
35 and over and women ages 45 and over.
°
Clinical breast examination for women over 40.
°
Mammogram for women age 50 and over.
°
Pap smear (or arrangements made for
performance) on all women determined to be
sexually active.
°
Chlamydia screen for all sexually active females
aged 21 and older who are determined to be at
high-risk for Chlamydia infection using the most
current CDC guidelines. ese guidelines include
the screening of all sexually active females aged 21
through 25 years of age,
°
Screening for TB risk factors, including a Mantoux
skin test on all persons determined to be at high risk.
°
Health education behavioral risk assessment.
Adult Preventive Services
PPGs shall cover and ensure the delivery of all
preventive services and medically necessary diagnostic
and treatment services for adult members. PPGs
shall ensure that the latest edition of the Guide to
Clinical Preventive Services published by the U.S.
Preventive Services Task Force (USPSTF) is used to
determine the provision of clinical preventive services
to asymptomatic, healthy adult Members (age 21 and
older). As a result of the IHA or other examinations,
discovery of risk factors or disease conditions will
determine the need for further follow-up, diagnostic,
and/or treatment services.
In the absence of the need for immediate follow-
up, the core preventive services identified in the
requirements for the adult IHA described above shall
be provided in the frequency required by the USPSTF
Guide to Clinical Preventive Services. PPGs shall cover
and ensure the provision of all medically necessary
diagnostic, treatment, and follow-up services which
are necessary given the finding or risk factors identified
in the IHA or during visits for routine, urgent, or
emergent health care situations. PPGs shall ensure
that these services are initiated as soon as possible, but
no later than 60 days following discovery of a problem
requiring follow up.
Immunizations for Adults
PPGs are responsible for ensuring all adults are
fully immunized and shall cover and ensure the
timely provision of vaccines in accordance with
the most current California Adult Immunization
recommendations and L.A. Care Preventive Health
Guidelines (see L.A. Care Website/Provider Resources/
Clinical Practice Guidelines). In addition, PPGs
shall cover and ensure the provision of age and risk
appropriate immunizations in accordance with the
finding of the IHA, other preventive screenings and/
or the presence of risk factors identified in the health
education behavioral assessment.
Children
L.A. Care shall provide lists of new member enrollees
to the PPGs on a monthly basis.
PPGs shall have processes in place to ensure the
provision of an IHA (complete history and physical
examination and an individualized behavioral health
assessment) to each new member under age 21 in
required timeframes as follows:
• For members under the age of 18 months, PPGs
are responsible to cover and ensure the provision
of an IHA within 120 days following the date of
enrollment.
• For members 18 months of age and older upon
enrollment, PPGs are responsible to ensure an IHA
is performed with 120 days of enrollment.
• PPGs shall cover and ensure the provision of an IHA
(complete history and physical examination and an
individualized behavioral health assessment) to each
new member under age 21 as follows:
°
Performance of the California CHDP program’s
age appropriate assessment due for each child at
the time of enrollment is accomplished at the
IHA.
°
e initial assessment must include, or arrange for
provision of, all immunizations necessary to ensure
that the child is up-to-date for age.
°
Includes a health education behavioral assessment
using an age appropriate DHS approved
assessment tool.
°
Arrangements are made for any needed follow-
up services that reflect the findings or risk factors
63
discovered during the IHA and health education
behavioral assessment.
°
Document the members’ completed IHA and
health education behavioral assessment tool in the
members’ medical record and to be made available
during subsequent preventive health visits.
°
PPGs shall make reasonable attempts to contact a
member and schedule an IHA. All attempts shall
be documented.
°
Documented attempts that demonstrate PPGs
unsuccessful efforts to contact a member and
schedule an IHA shall be considered evidence in
meeting this requirement.
Children’s Preventive Services
PPGs shall provide preventive health visits for all
members less than twenty-one (21) years of age at times
specified by the most recent AAP periodicity schedule.
is schedule requires more frequent visits than does
the periodicity schedule of the CHDP program. PPGs
shall provide, as part of the periodic preventive visit,
all age specific assessments and services required by the
CHDP program and the age specific health education
behavioral assessment, as necessary.
Where the AAP periodicity exam schedule is more
frequent than the CHDP periodicity examination
schedule, PPGs shall ensure that the AAP scheduled
assessment includes all assessment components
required by the CHDP for the lower age nearest to
the current age of the child. Where a request is made
for children’s preventive services by the member, the
member’s parent(s) or guardian, or through a referral
from the local CHDP program, an appointment shall
be made for the member to be examined within two
weeks of the request.
At each non-emergency Primary Care encounter with
members under the age of twenty-one (21) years, the
member (if an emancipated minor) or the parent(s)
or guardian of the member shall be advised of the
children’s preventive services due and available from
PPGs, if the member has not received children’s
preventive services in accordance with CHDP
preventive standards for children of the member’s
age. Documentation shall be entered in the member’s
medical record which shall indicate the receipt of
children’s preventive services in accordance with the
CHDP standards, or proof of voluntary refusal of
these services in the form of a signed statement by the
member (if an emancipated minor) or the parent(s)
or guardian of the member. If the responsible party
refuses to sign this statement, the refusal shall be noted
in the member’s medical record.
e Confidential Screening/Billing Report form,
PM 160-PHP, shall be used to report all children’s
preventive services encounters to DHS and the local
children’s preventive services program within thirty
(30) calendar days of the end of each month for all
encounters during that month.
• Original – Goes to L.A. Care
• Yellow – Copy to the Local CHDP office
• White – Goes in the Medical Chart
• Pink – Goes to the parents
Immunizations
PPGs shall ensure that all children receive necessary
immunizations at the time of any health care visit.
PPGs shall cover and ensure the timely provision of
vaccines in accordance with the most recent childhood
immunization schedule and recommendations
published by the Advisory Committee on
Immunization Practices (ACIP) Documented attempts
that demonstrate L.A. Care’s unsuccessful efforts
to provide the immunization shall be considered
sufficient in meeting this requirement.
If immunizations cannot be given at the time of the
visit, the member must be instructed as to how to
obtain necessary immunizations or a scheduled and
documented appointment must be made.
Appropriate documentation shall be entered in the
member’s medical record that indicates all attempts to
provide immunizations. A receipt of vaccines or proof
of prior immunizations; or proof of voluntary refusal
of vaccines in the form of a signed statement by the
member (if an emancipated minor) or the parent(s),
or guardian of the member, shall be entered in the
member’s medical record. If the responsible party
refuses to sign this statement, the refusal shall be noted
in the member’s medical record.
Upon federal Food and Drug Administration (FDA)
approval of any vaccine for childhood immunization
purposes, PPGs shall develop policies and procedures
for the provision and administration of the vaccine.
Such policies and procedures shall be developed within
60 calendar days of the vaccine’s approval date. PPGs
shall cover and ensure the provision of the vaccine
from the date of its approval regardless of whether
or not the vaccine has been incorporated into the
Vaccines for Children (VFC) Program. Policies and
procedures must be in accordance with any Medi-Cal
Fee-For-Service guidelines issued prior to the final
ACIP recommendations.
PPGs shall provide information to all network
providers regarding the VFC Program.
64
Blood Lead Screens
PPGs shall cover and ensure the provision of a blood
lead screening test to members at ages one (1) and two
(2) in accordance with Title 17, Division 1, Chapter 9,
Articles 1 and 2, commencing with Section 37000.
PPGs shall document and appropriately follow up
on blood lead screening test results. PPGs shall make
reasonable attempts to ensure the blood lead screen
test is provided and shall document attempts to
provide test.
If the blood lead screen test is refused by the member,
proof of voluntary refusal of the test in the form of a
signed statement by the member (if an emancipated
minor), or the parent(s) or guardian of the member,
shall be documented in the member’s medical record.
If the responsible party refuses to sign this statement,
the refusal shall be noted in the member’s medical
record. Documented attempts that demonstrate a
PPG’s unsuccessful efforts to provide the blood lead
screen test shall be considered sufficient in meeting
this requirement.
Screening for Chlamydia
PPGs shall screen all females less than 21 years of
age, who have been determined to be sexually active,
for Chlamydia. Follow up of positive results must
be documented in the member’s medical record.
PPGs shall make reasonable attempts to contact
appropriately identified members and provide
screening for Chlamydia. All attempts shall be
documented. Documented attempts that demonstrate
PPGs unsuccessful efforts to contact a member and
screen for Chlamydia shall be considered sufficient in
meeting this requirement.
If the member refuses the screening, proof of voluntary
refusal of the test in the form of a signed statement by
the member (if an emancipated minor) or parent(s),
or guardian of the member ,shall be documented in
the member’s medical record. If the responsible party
refuses to sign this statement, the refusal shall be noted
in the member’s medical record.
Human Papillomavirus (HPV) vaccinations are
covered benefits and should be provided based on the
recommended USPSTF guidelines. Please see the
most recent versions at L.A. Care’s website for Clinical
Guidelines at: http://www.lacare.org/clinical-
practice-guidelines
MISSED OR BROKEN APPOINTMENTS
Appointments may be missed due to member
cancellation or no show. Providers are required to
attempt to contact the member a minimum of three
times when an appointment is missed or broken.
Attempts to contact members must include:
• First Attempt – Phone call to member (or written
letter if no telephone). If member does not
respond, then;
• Second Attempt – Phone call to member (or written
letter if no telephone). If member does not respond
then;
• ird Attempt – Written letter.
Pregnant member with two or more missed/broken
appointments must be referred to the L.A. Care
UM Care Manager for follow-up after the broken
appointment procedure is completed without response
from the member. Documentation must be noted in
the member’s medical record regarding any missed or
broken appointments, reschedule dates, and attempts
to contact.
Missed and Broken Procedure or Laboratory Test
Appointments for procedures or tests may be missed
or broken. e provider must contact the member by
phone or letter to reschedule. Documentation must
be noted in the medical record regarding any missed
or broken procedure or tests, reschedule dates, and any
attempts to contact the member.
Unusual Specialty Services
L.A. Care and its PPGs/PCP must arrange for the
provision of seldom used or unusual specialty services
from specialists outside the network if unavailable
within network, when determined Medically Necessary.
Services Received in an Alternative Care Setting
e PCP should receive a report with findings,
recommended treatment and results of the treatment
for services performed outside of the PCP’s office.
e provider must also receive emergency department
reports and hospital discharge summaries and other
information documenting services provided.
Home health care agencies submit treatment plans to
the PCP after an authorized evaluation visit and every
30 days afterward for review of continued home care
and authorization. e PCP should also receive reports
regarding diagnostic or imaging services with abnormal
findings or evaluations and subsequent action.
65
CHILDREN WITH SPECIAL HEALTH CARE
NEEDS CSHCN
PPGs must maintain a program for Children with
Special Health Care Needs, which includes, but is not
limited to, the following:
• L.A. Care performs a New Member Outreach call
to all newly enrolled members that includes a health
risk assessment to identify Children with Special
Health Care Needs within 60 days of enrollment.
• e outcomes of the health risk assessment are
routed to the assigned PCP and delegated PPG to
coordinate medically necessary care.
• Members identified as CSHCN are referred to the
Care Management Program for assistance in care
coordination
• e PPGs/PCPs are responsible for ensuring and
monitoring timely access to pediatric specialists,
sub-specialists, ancillary therapists, and specialized
equipment and supplies; these may include
assignment to a specialist as PCP, standing referrals,
or other methods as defined by regulatory and
L.A. Care policy requirements.
• L.A. Care’s PPGs/PCPs are responsible for ensuring
that each Child with Special Health Care Needs,
receives a comprehensive assessment of health and
related needs and that all medically necessary follow-
up services are documented in the medical record,
including needed referrals. e comprehensive
assessment should be completed at the time of the
Initial Health Assessment and periodically thereafter.
• L.A. Care has an established case management/ care
coordination Care Management Program for Children
with Special Health Care Needs that includes the
coordination with other agencies, which provide
services for children with special health care need (e.g.
mental health, substance abuse, Regional Center, CCS,
local education agency, child welfare agency)
• L.A. Care monitors and identifies opportunities for
improving the quality and appropriateness of care
for children with special health care needs through
established quality processes:
°
Healthcare Effectiveness Data and Information Set
(HEDIS) results
°
Utilization Reports (e.g. IHA, Hospitalizations,
ER, Ambulatory Care)
°
Potential Quality of Care Issues (PQIs)
°
Grievance and Appeals
°
Member and Provider Satisfaction Surveys
DISEASE MANAGEMENT
L.A. Care does not delegate Disease Management
to PPGs/PCPs.
e Centers for Medicare and Medicaid Services
defines Disease Management as a “system of
coordinated health care interventions and
communication for populations with conditions
in which patient self-care is substantial”. Disease
Management supports the provider-member
relationship and treatment plan while emphasizing
prevention and self-management.
L.A. Care offers a variety of Disease Management
programs which focus on the development,
implementation and evaluation of a system
of coordinated health care interventions and
communication for members with chronic conditions
and caregivers/individuals that care for them. Using a
multi-disciplinary approach, members are identified,
stratified, assessed and care plans are developed to
assist members and their caregivers with navigating
the managed care system and managing their chronic
conditions. Programs may include:
• Self-management support
• Education and materials
• Community referrals
• Care coordination
Providers or members may contact L.A. Care Member
Services to inquire about the available programs.
BEHAVIORAL HEALTH SERVICES
(Described in further detail in Attachment B
following this Section 5.0)
Mental Health Services
L.A. Care is responsible for outpatient mental
health services to members with mild to moderate
impairment(s) resulting from a Mental Disorder. A
“Mental Disorder” is a mental health condition that
results in clinically significant distress or impairment
of mental, emotional, or behavioral functioning,
according the latest addition of the Diagnostic and
Statistical Manual.. We do not cover services for
conditions that the DSM identifies as something
other than a “mental disorder.” For example, the DSM
identifies relational problems as something other
than a “mental disorder,” so we do not cover services
(such as couples counseling or family counseling) for
relational problems.
We cover the following Services when provided
by participating physicians or other participating
66
providers who are licensed health care professionals
acting within the scope of their license:
• Individual and group mental health evaluation a
nd treatment
• Psychological testing when clinical indicated to
evaluate a mental health condition
• Psychiatric consultation
• Outpatient Services for the purpose of monitoring
medication treatment
• Outpatient laboratory, supplies and supplements
L.A. Care has contracted with Beacon Health
Strategies, to administer the delivery of behavioral
health services for L.A. Care members. While Beacon
is the contracted administrative service provider with
the Health Plan, College Health IPA will render all
utilization management determinations.
Beacon Health Strategies performs medical review on
all referrals for outpatient mental health services and
will coordinate the requested services as necessary.
For referring your patients to receive outpatient mental
health services, you may directly call 1.877.344.2858,
Option 6 to speak with a Beacon representative, 24/7.
For Crisis Intervention, please call 1.877.344.2858,
Option 1, to speak with a Beacon representative, 24/7.
Members may directly access mental health services by
calling the numbers above.
Specialty Mental Health Services, including inpatient
psychiatric hospitalization, is the responsibility of the
Los Angeles County Department of Mental Health
(LAC DMH). For members who meet the criteria for
Specialty Mental Health Services, L.A. Care behavioral
health vendor will coordinate and ensure COC.
Behavioral Health Treatment for Autism
Spectrum Disorder
Behavioral Health Treatment for members with
Autism Spectrum Disorder (inclusive of Aspergers
Disorder, Autism Disorder and Pervasive
Developmental Disorders) is covered when prescribed
by a Physician or licensed psychologist. Behavioral
Health Treatment must be prior authorized and
obtained from Participating Providers. is provider
network is contracted directly with L.A. Care and can
be reached at 1.888.347.2264.
Behavioral Health Treatment used for the purposes
of providing respite, day care, or educational services,
or to reimburse a parent for participation in the
treatment is not covered.
“Behavioral Health Treatment” is defined as follows:
Professional services and treatment programs,
including applied behavior analysis and evidence-based
intervention programs that develop or restore, to the
maximum extent practicable, the functioning of an
individual with autism spectrum disorder.
Exclusions and Limitations
• Alternative erapies,
• Biofeedback, unless the treatment is Medically
Necessary and prescribed by a licensed physician,
surgeon or licensed psychologist.
• Non-skilled care that can be performed safely and
effectively by family members (whether or not
such family members are available to provide such
services) or persons without licensure certification or
the presence of a supervising licensed nurse.
SUBSTANCE USE DISORDERS SERVICES
Inpatient Detoxification
L.A. Care will ensure appropriate medical
inpatient detoxification is provided under the
following circumstances:
• Life-threatening withdrawal from sedatives,
barbiturates, hypnotics, or medically complicated
alcohol and other drug withdrawal.
• Where it is medically necessary to monitor the
Member for life-threatening complications. In
such instances, two or more of the following must
be present: tachycardia, hypertension, diaphoresis,
significant increase or decrease in psychomotor activity,
tremor, significant disturbed sleep pattern, nausea and
vomiting, and/or threatened delirium tremens.
• When the Member is medically stabilized, the PCP/
L.A. Care shall provide a referral/linkage to a Substance
Abuse Treatment Program since Medi-Cal Substance
Use Disorder treatment is a carved out benefit.
Outpatient Substance Use Disorders Services
For Medi-Cal members 18 and older identified with
risky or hazardous alcohol use or a potential alcohol
misuse problem, a PCP can provide up to three 15
minutes Brief Interventions every year. L.A. Care will
maintain processes to ensure that substance use disorders
treatment services are available to Medi-Cal members
by providing timely linkage to these carved out benefits
through the Office of Substance Abuse, Prevention and
Control (SAPC), a program of L.A. County Department
of Public Health (LAC DPH).
e following services are provided by SAPC:
• Outpatient Methadone Maintenance
• Outpatient Drug Free Treatment Services

67
• Perinatal Residential Services
• Day Care Habilitative Services
• Naltrexone Treatment Services (Opiate Addiction)
• Outpatient Heroin Detoxification Services
L.A. Care and its contracted PPGs will ensure PCP
screening of L.A. Care Members for substance use
disorders during the IHA and in all subsequent
visits as appropriate. When a substance use disorder
is recognized as a potential condition, the PCP will
refer the Member to a treatment facility serving the
same geographic area. Referral is done by calling
the Community Assessment Services Center toll free
number 1.800.564.6600.
Members can access substance use disorder treatment
services by self-referral, by a family referral, or referral
from the PCP or other appropriate provider. During
treatment for substance use disorder, all medical
services will continue to be provided by the PCP or
other appropriate medical provider. e PCP will
make relevant medical records available to SAPC and its
providers with appropriate consent and release of medical
record information following federal and state guidelines.
VISION SERVICES
MediCal Members should be advised to contact
L.A. Care’s contracted Vision Vendor for covered
vision services. e vendor will coordinate services
and ensure the provision of eye examinations and
prescriptions for corrective lenses as appropriate for all
Members according to the member’s current Medi-Cal
benefits for eye examinations and lenses. Additional
services and lenses are provided based on medical
necessity for examinations and new prescriptions.
Members are eligible for eye examination with
refractive services, but the dispensing of prescription
lenses at least every two years is dependent on whether
the member has the benefit as described below.
L.A. Care MEDI-CAL Adults (age 21 and over):
On July 15, 2010, the State of California reinstated
adult Optometry services retrospective to July 1,
2009 (See MMCD All Plan Policy Letter#10-010
“Reinstatement of Optometry Services”). To date,
this reinstatement does not include lenses for adults
(services provided by fabricating optical laboratories).
For Medi-Cal Members – Children up to Age 21:
Medi-Cal Eye exams are covered by L.A. Care and
children are limited to one pair of eyeglasses every two
years unless:
• Prescription has changed at a minimum of .50 diopters
• Replacement lenses are needed because the member’s
previous lenses have been lost, stolen, broken, or
marred and damaged beyond the member’s control
to a degree significantly interfering with vision or eye
safety (a certificate or statement is required)
• Frame needs replacement because a different size or
shape is necessary.
• is includes lenses and covered frames for eyeglasses
when authorized.
For eyeglasses for eligible members, L.A. Care’s
contracted vision vendor will coordinate services with
the PIA and DHCS is responsible for reimbursing
the PIA for the fabrication of the optical lenses in
accordance with the contract between DHCS and PIA.
CCS Referrals for Certain Eye Conditions
Eye conditions leading to a loss of vision, strabismus
requiring surgery, infections such as keratitis,
choroiditis; and chronic diseases such as glaucoma,
cataract, retinal detachment, ptosis, optic atrophy
or retrolental fibroplasis may be covered by CCS.
Contact the L.A. Care UM Department or CCS
for assistance. Ordinary refractive errors, chronic
chalazion, anisometropia, amblyopia, strabismus when
periodic refraction, glasses or when patching is needed
are not covered by CCS.
DENTAL SERVICES
Dental Services for Medi-Cal Are Carved Out To
Denti-Cal (See Medi-Cal Carved Out Section)

68
Medi-Cal Linked and Carve Out Services
Linked and Carve Out Program Medi-Cal
California Children Services (Ccs)
X
School Linked Child Health
Disability Prevention (Chdp) Services
X
Tb/Dot X
WIC, Nutritional Program X
Developmental Disabilities Services
(Dds)
X
Early Intervention/Early Start
X
Specialty Mental Health
X
Substance Use Disorder Treatment
X
Local Education Agency
X
HIV/ Aids Home And Community
Based Waiver Programs
X
Dental Services X
Vision X
Targeted Case Management
X
Early Periodic Screening, Diagnosis
And Treatment
X
Early Periodic Screening, Diagnosis
And Treatment – Supplemental Srvcs
X
CARE COORDINATION WITH LINKED AND
CARVED OUT SERVICES
Care Managers are available to assist members, who may
need or who are receiving services from out of plan
providers and/or programs, in order to ensure coordinated
service delivery and efficient and effective joint case
management. However, the coordination of care and
services remains the responsibility of each member’s PCP.
PPG’s and the member’s PCP will monitor the following:
• Member referral to and/or utilization of special
programs and services
• Member referral to and/or utilization of specialty care,
including ensuring consultative notes and summaries
are maintained in the medical home records
• Routine medical care, including providing the
necessary preventive medical care and services
• Provision of Initial Health Assessments and
completion of the age-specific Individual Health
Education and Behavioral Assessment (IHEBA)
PPGs and PCPs are encouraged to make referrals to
local health departments, mental health programs and
regional centers.
Out-of-Plan Case Management and Coordination
of Care for Linked and Carved out Services
L.A. Care shall implement procedures to identify
individuals, who may need or who are receiving
services from out of plan providers and/or programs,
in order to ensure coordinated service delivery and
efficient and effective joint case management.
L.A. Care maintains Memorandum of Understanding
(MOU) agreements defined by the DHCS contract to
promote continuity and coordination of care for
Medi-Cal members between the health plan and local
public health programs (Linked and Carved-Out
Programs). e agencies meet regularly with L.A. Care
staff to monitor the effectiveness of the MOU. An
MOU is a document defining services to be provided,
when reimbursement is not made by L.A. Care, but the
L.A. Care and/or its PPGs is responsible for
coordinating the services. Also see subcontract
definition below.
e Managed Medi-Cal Program requires L.A. Care
to establish and maintain MOUs for the following
carved-out services:
• California Children Services (CCS)
• Maternal and Child Health (MCH)
• Child Health and Disability Prevention
(CHDP) Program
• Tuberculosis Direct Observed erapy (DOT)
• Women, Infants, and Children Supplemental
Nutrition Program (WIC)
• Regional Centers for Services for Persons with
Developmental Disabilities
• Specialty Mental Health Services
• Public Health Department
A Subcontract is a written agreement entered into
by L.A. Care with a provider of health care services
who agrees to furnish Covered Services to members
or with any other organization or person(s) who
agree(s) to perform any administrative function or
service for L.A. Care specifically related to fulfilling
L.A. Care’s obligation to DHS under the terms of
the DHS Contract. Subcontracts must specify scope
and responsibilities of both parties in the provision of
services to members as follows:
• Billing and reimbursements
• Reporting responsibilities
69
• How services are to be coordinated between the
agency and L.A. Care and/or its PPGs, including
exchange of medical information as necessary
• Subcontracts include, but are not limited to, the
following linked services:
°
Family Planning Services
°
Sexually Transmitted Disease (STD) Services
°
HIV Testing and Counseling Services
°
Immunizations
°
School Based Child Health and Disability
Prevention (CHDP) Services (with Covina Valley
USD, Long Beach USD, and Los Angeles USD)
Linked agencies have defined roles and responsibilities
to ensure coordination of care for members. In most
instances, the agency, not L.A. Care, is financially
responsible for the linked services.
DESCRIPTION AND RESPONSIBILITIES
FOR THE LINKED AND CARVED OUT
PROGRAMS: CALIFORNIA CHILDREN
SERVICES CCS
CCS services are carved out of and excluded from
L.A. Care’s responsibilities under the Medi-Cal contract
with DHS, and will be provided by the L.A. County
CCS in accordance with the current MOU between
L.A. Care and CCS. Services provided by the CCS
program are not covered under the DHS State contract.
Upon adequate diagnostic evidence that a Medi-
Cal Member under 21 years of age may have a
CCS eligible condition, L.A. Care and/or its PPGs
shall refer the member to the local CCS office for
determination of eligibility.
L.A. Care and/or its PPGs shall develop and implement
written policies and procedures for identifying and
referring children with CCS-eligible conditions to the
local CCS program. e policies and procedures shall
include, but not be limited to those which:
• Ensure that L.A. Care and/or its PPGs’ providers
perform appropriate baseline health assessments and
diagnostic evaluations which provide the sufficient
clinical detail to establish, or raise a reasonable suspicion,
that a member has a CCS-eligible medical condition;
• Assure that contracting providers understand that
CCS reimburses only CCS-paneled providers and
CCS-approved hospitals within L.A. Care and/or its
PPGs’ network; and only from the date of referral;
• Enable initial referrals of members with CCS-eligible
conditions to be made to the local CCS program by
telephone, same-day mail or FAX, if available. e
initial referral shall be followed by submission of
supporting medical documentation sufficient to allow
for eligibility determination by the local CCS program;
• Ensure that L.A. Care and/or its PPGs continue to
provide all Medically Necessary Covered Services to
the member until CCS eligibility is confirmed;
• Ensure that, once eligibility for the CCS program is
established for a member, L.A. Care and/or its PPGs
shall continue to provide all Medically Necessary
Covered Services that are not authorized by CCS,
and shall ensure the coordination of services and
joint case management between its Primary Care
Providers, the CCS specialty providers, and the local
CCS program.
If the local CCS program does not approve eligibility,
L.A. Care and/or its PPGs remain responsible for the
provision of all Medically Necessary Covered Services
to the member. If the local CCS program denies
authorization for any service, L.A. Care and/or its
PPGs remain responsible for obtaining the service, if
it is medically necessary and paying for the service if it
has been provided.
Identification
Identify and track current and new enrollees with
potential and/or eligible CCS conditions.
Eligibility
L.A. Care shall be responsible for generating and
distributing, to its PPGs and the member’s PCP, lists
received from CCS of L.A. Care members identified as
being eligible or authorized to receive CCS services.
L.A. Care will send these lists to its PPGs and to the
member’s PCP on a monthly basis. L.A. Care and/or its
PPGs will notify the member’s PCP, and will work with
the local CCS office to ensure the member is receiving
appropriate medical care and that coordination of care is
documented in the member’s medical records. L.A. Care
and/or its PPGs will undertake regular activities, such as
review of encounter data necessary to identify members
with potential CCS conditions and assure appropriate
referrals to CCS.
Referral
Members (parent/guardian) may self-refer to CCS.
L.A. Care will make available to its PPGs, a list of
CCS paneled providers and facilities as received from
the local and/or State CCS program office. PCP or
specialist may refer to CCS paneled provider or CCS
local program using the L.A. Care, and/or its delegated
provider’s, referral process or refer the member directly
to CCS. L.A. Care and/or its PPGs are required
70
to provide to PCPs, information on CCS paneled
providers and facilities including mechanism for
accessing specific provider facility contact information
for referral.
e CCS program authorizes Medi-Cal payments
to L.A. Care and/or its delegated provider’s network
physicians who currently are members of the CCS panel,
and to other providers who provided CCS-covered
services to the member during the CCS-eligibility
determination period who are determined to meet
the CCS standards for paneling in accordance with
subparagraph D below. L.A. Care and/or its PPGs shall
inform providers, except as noted above, that CCS
reimburses only CCS paneled providers. L.A. Care
and/or its PPGs shall submit information to the CCS
program on all providers who have provided services to a
member thought to have a CCS eligible condition.
Authorization for payment shall be retroactive to
the date the CCS program was informed about the
member through an initial referral by L.A. Care and/or
its PPGs, or a L.A. Care and/or its delegated provider’s
network physician, via telephone, FAX, or mail. In
an emergency admission, L.A. Care and/or its PPGs,
or L.A. Care and/or its PPGs’ network physician
shall be allowed until the next business day to inform
the CCS program about the member. Authorization
shall be issued upon confirmation of panel status or
completion of the process described above. L.A. Care
will ensure that the member and provider manuals
document the CCS referral options and processes.
Coordination of Care:
L.A. Care and/or its PPGs shall:
• Designate a CCS coordinator (liaison) to interface
with a designated L.A. Care CCS Coordinator,
the CCS office, CCS panel provider, the member’s
family or guardian.
• Implement procedures to ensure confidential
transfer of medical documentation between the PCP
and CCS paneled providers in compliance with all
federal and state regulations.
• Ensure that the PCP provides basic case
management for the member and assures appropriate
referrals for members with potential and/or eligible
CCS conditions.
• Make available CCS Program referral forms to all
member families/guardians and PCP offices.
• Continue to provide case management of all services
(primary and specialty care) until eligibility has been
established with the CCS program.
• CCS program case management is responsible for
the CCS eligible condition and authorizes medically
necessary care.
• L.A. Care and/or its PPGs must continue to provide
primary care case management, coordination of
services, and health care service other than those
required for the CCS condition and keep active
CCS case logs.
• For inpatient admissions CCS referrals,
authorization for inpatient hospital stays is limited
to the time of eligibility for the CCS program. It is
recommended that the L.A. Care and/or its PPGs
or designated CCS coordinator continue to track
the hospitalization in collaboration with the CCS
Case Manager.
• L.A. Care’s PPGs are capitated to provide
services not unrelated to the treatment of the
CCS eligible condition.
Referral/Care Coordination of Members to the
Genetically Handicapped Persons Program (GHPP)
L.A. Care and/or its PPGs shall have mechanisms in
place to refer members who may be eligible for services
provided by the Genetically Handicapped Persons to
assure appropriate care coordination of members who
will no longer be eligible for CCS at age of 21, but will
still need services.
Dispute Resolution
L.A. Care and/or its PPGs need to have a mechanism
in place to resolve disputes between the PCP or
Specialist and the CCS program office. In the absence
of a resolution, L.A. Care and/or its PPGs Liaison
will notify L.A. Care UM of all unresolved disputes
regarding CCS services. All dispute resolutions must be
resolved within 30 calendar days. L.A. Care and/or its
PPGs are required to provide any medically necessary
special services during the time of dispute resolution.
L.A. Care will facilitate any unresolved disputes.
Disagreements with regards to CCS program
eligibility, payments for the treatment of services of the
CCS eligible condition and associated or complicated
conditions must be resolved cooperatively between
L.A. Care and the county CCS program.
If the dispute is not resolved at the local level, L.A. Care
must notify the Medi-Cal Managed Care contract
manager, and the county CCS program must notify
the State CCS Regional Office. e State Children’s
Medical Services (CMS) program and the Medical
Managed Care Division will ultimately render a joint
decision if the problem is not resolved at the lower level.
71
Training and Education
L.A. Care and/or its PPGs will coordinate with the local
CCS, to develop and implement training programs
for L.A. Care and/or its PPGs, PCPs, and L.A. Care
Staff. L.A. Care will ensure that provider manuals and
the member enrollment materials outline information
describing CCS benefits and eligibility.
MATERNAL AND CHILD HEALTH
COMPREHEHSIVE PRENATAL SERVICES
PROGRAM CPSP
L.A. Care and it’s PPGs must complete a comprehensive
risk assessment tool for all pregnant female Members
that is comparable to the American College of Obstetrics
and Gynecology standard and Comprehensive Perinatal
Services Program (CPSP) standards.
e results of this assessment shall be maintained
as part of the obstetrical records and shall include
medical/obstetrical, nutritional, psychosocial, and
health education needs risk assessment components.
e risk assessment tools shall be administered at the
initial prenatal visit, once each trimester thereafter
and at the postpartum visit. Risks identified shall be
followed up on by appropriate interventions, which
must be documented in the medical record.
Standard Obstetrical Record Elements
Standard Obstetrical record elements shall be
included in the obstetric, nutritional, psychosocial
and educational examination of pregnant members
in compliance with DHS and the most current
guidelines of the American College of Obstetrics and
Gynecology (ACOG), CPSP, and Title 22. Obstetrical
records include the CPSP Patient Records - CPSP
Documentation Forms and/or any obstetric record that
applies with the CPSP standards for documentation.
Referral to Specialists
L.A. Care and its PPGs are responsible for ensuring that
appropriate hospitals are available within the provider
network to provide necessary high-risk pregnancy
services. Pregnant women that are at high risk of a
poor pregnancy outcome are referred to appropriate
specialists including perinatologists and have access to
genetic screening with appropriate referrals.
Specialists may include, but are not limited to:
• Cardiologists
• Psychiatrists
• Internists
• Infectious Disease
• Geneticists
• Specialty High-Risk Obstetricians
• Oncologists
• Endocrinologists
Examples of these referral types and protocols may
include, but are not limited to:
• Diabetes
• Hypertension
• Hepatitis
• HIV+
• Genetic Problems
• Epilepsy or Neurological Disorder
• Renal Disease
• Alcohol or Drug Abuse
• Maternal Cardiac Disorders
• yroid or Other Endocrine Disorders
• Epilepsy or Neurological Disorder
Common Pregnancy Conditions/Issues Requiring
Multidisciplinary Management
Pregnant members exhibiting any of the following
representative conditions/ issues will have
interventions and referrals developed utilizing the
Nutrition (N), Psychosocial (PS), or Health Education
(HE) protocols:
• Unintended or unwanted pregnancy (PS)
• Teenage pregnancy (PS)
• Fear of physicians, hospitals, and medical
personnel (HE)
• Language barriers (HE)
• Lack of basic reproductive awareness (HE)
• Housing and transportation problems (PS)
• Domestic violence (PS)
• No previous contact with health care systems (HE)
• Multiple gestation (HE), (PS), (N)
• Need for bed rest during pregnancy (PS), (HE)
• Previous receipt of unfriendly health care services (HE)
• Personal and religious beliefs at odds with optimal
prenatal care (HE)
Common Postpartum Conditions/Issues Requiring
Multidisciplinary Management:
• Postpartum blues, postpartum depression (PS)
• Housing, food, transportation problems (PS)
• Lack of basic parenting skills and role models (HE)
• Breastfeeding difficulties (HE)
• Sexual pain/difficulties (HE)
• Severe anemia (N)
Comprehensive Perinatal Services Personnel
e primary component of quality multidisciplinary
management of comprehensive perinatal care is
72
personnel. Participating obstetrical providers must
ensure that health education, nutrition, psychosocial
assessment, re-assessment and intervention are
administered by qualified personnel. Training of
Comprehensive Perinatal Services personnel will be
provided by L.A. Care with technical assistance from
the County of Los Angeles Comprehensive Perinatal
Service Program.
Comprehensive Perinatal practitioners may include
any of the following:
• General Practice physician
• Family Practice physician
• Pediatrician
• Obstetrician-Gynecologist
• Certified Nurse Mid-Wife
• Registered Nurse
• Nurse Practitioner
• Physician’s Assistant
• Social Worker
• Health Educator
• Childbirth Educator
• Registered Dietitian
• Comprehensive Perinatal Health Worker
Ancillary Services/staff who may provide services
within specific components of Comprehensive
Perinatal services or services available within Linked/
Carved out Services include, but are not limited to:
• Geneticists
• Other medical specialists
• Public Health Services
• Family Planning Services
• Substance Abuse Prevention Service
• Community-Based Organizations
• Community Outreach Services
• Agencies providing transportation
• Domestic Violence Units
• Child Protective Services
• Local Diabetes and Pregnancy Programs
• Dental Services
• Specialty Mental Health Services
• Translation Services
• Women’s Center
• Respite Care Services
Other Referrals include, but are not limited to:
• Supplemental Nutrition Program for Women,
Infants, and Children (WIC)
L.A. Care and its PPGs shall ensure that all pregnant,
breastfeeding and postpartum women, and infants
and children who are eligible for WIC services will be
assessed, and if appropriate, referred to the Los Angeles
County Public Health Services WIC Program. Family
planning referral protocols may include assistance
with birth control issues, STD information or control,
procedure or counseling. A referral may be done, but
is not required for this service, as members can self-
refer to Family Planning Services. For instance,
Social Work referrals due to:
• Family Abuse/Domestic Violence
• Financial Problems
• Other identified social needs
SCHOOL LINKED CHILD HEALTH AND
DISABILITIES PREVENTION PROGRAM
CHDP MEDICAL ONLY
L.A. Care has a mutually agreed upon arrangement
with the local School Districts that provide EPSDT/
CHDP services. at arrangement describes eligibility
requirements, scope of services, client services ,
outreach, tracking follow-up, health education, data
collection, quality assurance mechanisms, dispute
resolution and billing/ reimbursement mechanisms
governing the relationship between and among
L.A. Care and the participating school districts.
L.A. Care will directly reimburse schools for the
provision of some or all of the CHDP services,
including guidelines for sharing of critical medical
information. L.A. Care will provide guidelines
specifying coordination of services reporting
requirements, quality standards, processes to ensure
services are not duplicated and process for notification
to member/student/parent on where to receive initial
and follow-up services.
PPGs are required to maintain a “medical home”
and ensure the overall coordination of care and case
management of members who obtain CHDP services
through the local school districts or school sites.
PCP will provide basic case management for the
member and coordinate the provision of any referrals
or additional services necessary to diagnose and/or
treat conditions identified during the school EPSDT/
CHDP assessment.
PCP will also provide ongoing preventive and primary
services, as required. EPSDT/CHDP services are
provided to members for school entry only while
maintaining the “medical home” with the PCP
for ongoing health care management. e PCP,
as the medical home, is responsible for ongoing
comprehensive health care delivery.
73
Reimbursement to Schools for the Provision of
School Based EPSDT/CHDP Services
L.A. Care shall be responsible to pay school district
claims directly for EPSDT/CHDP services provided
in accordance with the agreement as determined by
the total amount of claims. L.A. Care will generate
a PPG Claims Paid reconciliation report to identify
claims paid on behalf of the PPG by L.A. Care for that
capitation period.
Provider Training
L.A. Care will collaborate with the PPGs and the
Los Angeles area CHDP programs to ensure provider
training regarding school linked EPSDT/CHDP services.
TUBERCULOSIS/DIRECT OBSERVATION
THERAPY MEDICAL
L.A. Care and its PPGs must provide screening for all
members at risk for TB to determine risk factors for and
diagnosis of Tuberculosis. Mantoux skin tests will be
performed on all persons at increased risk of developing
TB. Children will be screened for TB risk factors and
will follow recommended guidelines for the provision
of Mantoux skin testing. In collaboration with the
Local Health Departments TB Control, L.A. Care will
provide education and access to training upon request.
L.A. Care and its PPGs must have systems in place to:
• Coordinate services provided to members
diagnosed with active TB through the Local Health
Department TB Control Department and DOT.
• Each confirmed TB case or suspected case must
be reported within one business day to the local
Health Department.
• Maintain evidence that members with a suspected
or confirmed TB diagnosis are reported to the Local
Health Department within one business day.
• All individuals at increased risk for TB will be
offered TB testing and managed, according to
CDC guidelines for the management of individuals
identified at high risk for TB, unless they have
documentation of prior positive test results, TB
disease and/or treatment.
e Primary Care Physicians (PCP), as required by the
current California TB guidelines, understand that a
tuberculin reaction of 5mm of induration or greater is
classified as positive in the following groups:
• Persons known to have or at risk for HIV infection
• Close recent contact with a person who has
infectious TB
• Persons who have a chest x-ray consistent
with tuberculosis
• Persons who are immunosuppressed
• Other groups as identified in the current
California TB Guidelines.
A tuberculin reaction of 10mm of induration or
greater is classified as positive in all other persons.
e PCP will evaluate all members with a positive
skin test, even if asymptomatic.
To report positive results, the PCP’s must document
the appropriate action as follows:
• Positive tests in children under the age of three (3)
are reported to the Local Health Department and
L.A. Care Management Program.
• All members with a new positive skin test must
be evaluated for active TB which may include a
chest x-ray.
• When active TB is suspected, an appropriate culture
must be obtained from sputum or other body fluid/
tissue, as appropriate.
When TB is suspected, treatment will be initiated
prior to bacteriological confirmation. e PCP
must refer appropriate members to the Local Health
Department TB Control
Program to provide members with active TB, the
services of Directly Observed erapy (DOT).
All active cases determined to be at risk for non-
compliance will be referred to the TB Control
Program for evaluation of DOT services.
Directly Observed erapy (DOT) for TB is offered
by local health departments (LHDs) and is a linked
and carved out service. L.A. Care and/or its PPGs
shall assess the risk of non-compliance with drug
therapy for each member who requires placement on
anti-tuberculosis drug therapy. e following groups
of individuals are at risk for non-compliance for the
treatment of TB:
• Members with demonstrated multiple drug
resistance (defined as resistance to Isoniazid
and Rifampin);
• Members whose treatment has failed or who have
relapsed after completing a prior regimen;
• Children, adolescents and individuals who have
demonstrated noncompliance (those who failed to
keep office appointments).
L.A. Care and/or its PPGs shall refer members with
active TB and who have any of these risks to the TB
Control Officer of the LHD for DOT.
74
L.A. Care and/or its PPGs shall assess the following
groups of members for potential noncompliance and
for consideration for DOT:
• Substance abusers
• Persons with mental illness
• e elderly
• Persons with unmet housing needs
• Persons with language and/or cultural barriers
If, in the opinion of L.A. Care and/or its delegated
entities’ providers, a member with one or more of
these risk factors is at risk for noncompliance, the
member shall be referred to the LHD for DOT.
L.A. Care and/or its delegated entities shall provide
all Medically Necessary covered Services to the
member with TB on DOT, and shall ensure joint case
management and coordination of care with the LHD
TB Control Officer. L.A. Care, in conjunction with
its delegated entities, will work in close collaboration
with the Public Health Departments of the County of
Los Angeles and the cities of Pasadena and Long Beach
to ensure compliance with guidelines for TB treatment
and control.
WOMEN, INFANTS, AND CHILDREN
NUTRITIONAL SUPPLEMENT
PROGRAM WIC MEDICAL
WIC services are defined as a carve out service and are
provided as a benefit to eligible Women, Infants, and
Children through referral to the Carved Out Service,
the WIC Program.
L.A. Care and its PPGs must have systems to identify
and refer eligible members needing WIC services are
referred to appropriate WIC sites/services.
IDENTIFICATION
Eligibility Verification
Eligibility for WIC services is determined by the WIC
centers based on residency and other factors.
PCP and other Physicians or Primary Care
Providers WIC Referrals
PCPs, Other Physicians or other Primary Care
Providers WIC referral process as part of its Initial
Health Assessment of members, or as part of the initial
evaluation of newly pregnant women, shall refer and
document the referral of pregnant, breastfeeding or
postpartum women or a parent/ guardian of a child
under the age of five to the WIC program as mandated
by Title 42, CFR 431.635 (c).
As part of the referral process, PCPs, Other Physicians
or other Primary Care Providers referring to the WIC
program must include:
• A current hemoglobin or hematocrit laboratory value
• Present height and weight
• Confirmation of the pregnancy date
• Birth weight and length for infants
• For small or pre-term infants, documentation of the
gestational age
PCPs, Other Physicians or other Primary Care
Providers must document these laboratory values and
the referral in the member’s medical record.
Members Self-Referral to WIC
Members may self-refer to WIC.
Basic Case Management
e PCP maintains the role of the overall case
manager for the member, which includes assuring
appropriate referrals for members needing WIC
services and providing routine preventive and other
necessary care.
Transfer of Information between Providers and WIC
L.A. Care and its PPGs/PCPs must implement HIPAA
compliant procedures to ensure confidential transfer of
medical documentation including CPSP assessment,
and WIC program dietary assessment forms, to and
from the PCP to WIC Centers in compliance with all
federal and state regulations.
DEVELOPMENTAL DISABILITIES
SERVICES DDS MEDICAL
L.A. Care and its PPGs must maintain policies,
procedure, and processes in place to address the
following: identification, diagnosis, referral, and
tracking of members with potential and eligible
DDS conditions for the provision of all screening,
preventive, medically necessary, and therapeutic
services. L.A. Care and its PPGs will utilize network
providers for diagnosis and treatment of members
with developmental disabilities. Members may access
the Regional Centers if services are needed and not
available within the L.A. Care network. L.A. Care
and its PPGs will refer members with developmental
disabilities to the Regional Centers for those non-
medical services such as respite, out of home
placement, supportive living, etc.
Identification
L.A. Care will:
For existing Medi-Cal members, L.A. Care obtains
75
a list of eligible members currently enrolled in a
Regional Center. is list is distributed to the assigned
PCPs and PPGs to ensure care coordination. On
a monthly basis, L.A. Care provides PPGs and PCPs
with a list of members receiving services through the
community Regional Centers. is information serves as
notification to providers and allows them to coordinate
any services requested by L.A. Care or the Regional
Center. For a listing of current approved ICD-9 codes of
potential eligible DDS conditions, you may contact the
UM Department or visit www.dds.cahwnet.gov for
additional information about DDS.
PPGs will:
Maintain mechanisms to support the identification of
members with eligible and potential DDS conditions
and use the list of members with potential and eligible
DDS conditions generated by L.A. Care and any
additional information generated by the L.A. Care
to facilitate the provision of basic case management
and coordination of care by the PCP. Be responsible
to track the identified potential and eligible DDS
members and the services provided to them to assure
coordination and COC. Notify PCPs of potential and
eligible DDS members and work with the PCPs and
the local Regional Centers to ensure these members
continue to receive preventive and medically necessary
care and that coordination of care is documented in
member medical records.
PCPs will:
Be responsible for basic case management and
coordination of care for members with potential and
eligible DDS conditions.
Eligibility
L.A. Care will verify member eligibility and send the
list of members to the PPGs by facsimile, encrypted
email or via a secure PPG FTP sites.
Referral
Members (parent/guardian) may self refer to the
Regional Centers for confirmation of Regional
Center eligibility criteria. A current listing of the local
Regional Centers is available at www.lacare.org or
www.dds.cahwnet.gov.
Members must submit a signed consent form for
“Release of Medical Information” to facilitate data
exchange.
e PCP or specialist should refer potential and
eligible members directly to the Regional Center
and are encouraged to include the specific member
information in the referral matching Regional Center
eligibility criteria.
PPGs must:
Implement procedures to ensure confidential transfer
of medical documentation to and from the PCP to
Regional Centers in compliance with all federal and
state regulations.
Establish procedures to support the identification and
management of problems with the PCP, Regional
Centers, and L.A. Care.
Ensure that the PCP maintains the role of the overall
case manager for the member and assure appropriate
referrals for members with potential and or eligible
DDS conditions.
PCPs must:
Maintain the role of the overall case manager for the
member and assure appropriate referrals for members
with potential and or eligible DDS conditions.
HOME AND COMMUNITY BASED
WAIVER PROGRAMS
L.A. Care maintains processes and mechanisms for the
identification of candidates for the Medi-Cal Home
and Community-Based Waiver Programs. rough
its care management programs, L.A. Care identifies
members who may need services or placement in a
Medi-Cal HCBS Waiver Program and works with the
PCP in order to ensure coordinated service delivery
and efficient and effective case management for
services needed by the Member.
When L.A. Cares identifies Members who may benefit
from the Home and Community-Based Services
(HCBS) Waiver programs, L.A. Care refers them to
the specific Agency – needed for assessment:
• Assisted Living Waiver (ALW)
• Nursing Facility/Acute Hospital (NF/AH Waiver)
• Home and Community-Based Services Waiver for
Persons with Developmental Disabilities (HCBS-DD)
• HIV/AIDS Medi-Cal Waiver Program (MCWP)
If the agency administering the waiver program
concurs with L.A. Care’s assessment of the Member
and there is available placement in the waiver
program, L.A. Care is responsible for continuing
to cover and ensure that all medically necessary
care unrelated to the Home and Community Based
Services Waiver Program is provided when a member
has been referred to and been accepted or has directly
accessed the Home and Community Based Services
Waiver Program.

76
Members Meeting Criteria for a HCBS
Waiver Program
Although Services provided under the Home and
Community-Based Services (HCBS) Waiver Programs
are a Linked/Carved-Out Service and not covered
under L.A. Care , members meeting criteria for
placement and when placement is available, these
members are not disenrolled from L.A. Care and
receive the carved out waiver services while remaining
enrolled in L.A. Care.
• L.A. Care maintains systems to identify members
with conditions that may meet the requirements for
participation in this waiver and refers these members
to the appropriate HCBS Waiver program
• If the agency concurs with the L.A. Care’s assessment
of the member and there is available placement in
the waiver program, the member will receive waiver
services and L.A. Care shall continue to provide
all other medically necessary covered services to
members while in the HCBS Waiver Program.
Members Not Meeting Criteria for a Waiver
Program or Placement Not Available for Members
Who Do Meet Criteria for a Waiver Program
• If the HCBS Agency determines that the member
does not meet the criteria for a waiver program or if
placement is not available, L.A. Care continues to be
responsible for the member’s care.
• If the member is denied placement because of the
limited number available for the waiver program,
L.A. Care UM shall:
°
Maintain contact with the appropriate agency
to assure the member is reconsidered when space
is available
°
Continue comprehensive case management and
shall continue to cover all Medically Necessary
Covered Services to the Member.
(HIV/AIDS) Home And Community Based
Services Waiver Program Services
L.A. Care members, who are subsequently diagnosed
with HIV/AIDS as defined by the most recently
published Mortality and Morbidity Report from the
Centers of Disease Control and Prevention, may
participate in the HIV/AIDS Home and Community
Based Services Waiver Program without having to
disenroll from L.A. Care. Services provided under
the HIV/AIDS Home and Community Based Services
Waiver are provided through a carved out program.
Members must meet the eligibility requirements of the
program and enrollment is dependent on available space.
L.A. Care and its PPGs/PCPs should refer any
member that may meet the qualifications of the waiver
program to the L.A. Care Management Program.
EARLY INTERVENTION/EARLY START
L.A. Care and its PPGs are responsible for assuring
identified eligible members under the age of three
3 years with or at risk for developmental disabilities
are referred to Early Start/Early Intervention
Services (including CHDP). e Early Start
Program is administered through the Department of
Developmental Services (DDS). DDS is responsible
for coordinating a wide array of services for:
• California residents with developmental disabilities
• Infants at high risk for developmental disabilities
• Individuals at high risk for parenting a child with
a disability
• Conducting oversight activities to monitor the need
for EPSDT Early Start/Early Intervention Services
• Services are evaluated during the IHA ( Initial
Health Assessment) within the required timeframes
as described below of Plan membership and during
preventive health visits thereafter:
• When medically indicated, the provision of
medically necessary Early Start/Early Intervention
Services within Plan and
• When medically indicated, the provision and/
or coordination of Early Start/Early Intervention
Services if these services are delivered out-of-Plan.
• Coordinating with the Plan Partners and local programs
to develop and implement programs for PCPs.
PPGs must:
Have systems in place to address the identification,
diagnosing, referral, case management, tracking, and
reporting of members who are eligible for Early Start/
Early Intervention Services. Additionally, the systems
must identify children who may be eligible to receive
services from the Early Start program and refer them
to the local Early Start program. ese children would
include those:
• With a condition known to lead to developmental
delay in either cognitive, communication, social
or emotional, adaptive, or physical and motor
development including vision and hearing.
• In whom a significant developmental delay is suspected.
• Whose early health history places them at risk for delay.
• Collaborate with the local Regional Center or local
Early Start program in determining the Medically
Necessary diagnostic and preventive services and
treatment plans for members participating in the
Early Start program.
77
Provide case management and care coordination to
the Member to ensure the provision of all Medically
Necessary covered diagnostic, preventive and treatment
service identified in the individual family service plan
developed by the Early Star/Early Intervention Program,
with Primary Care Provider participation.
Identification
L.A. Care and its PPGs must:
• Identify current and new enrollees needing Early
Start/Early Intervention services.
• Track the identified persons and the services
provided to them to assure coordination and COC.
• Ensure members receive an Initial Health
Assessment (IHA), through the member’s PCP.
For members under the age of 18 months, PPGs/PCPs
are responsible to cover and ensure the provision of an
IHA within 60 days following the date of enrollment
or within periodicity timelines established by the
American Academy of Pediatrics (AAP) for ages
two and younger whichever is less. For members 18
months of age and older upon enrollment, PPGs/
PCPs are responsible to ensure an IHA is performed
with 120 days of enrollment and that the IHA will
be consistent with the AAP and EPSDT Periodicity
Schedule of assessment requirements.
Eligibility
L.A. Care and its PPGs are required to review encounter
data to determine members’ eligible for Early Start/
Early Intervention Services. e following conditions
are among those which potentially place infants and
children at risk of developmental disabilities:
• HIV/AIDS
• Cancer
• Blindness, hearing impaired
• Retardation
• Heart conditions
• Epilepsy
• Juvenile diabetes
• Cleft palate
• Lung disorders, asthma, cystic fibrosis
• Downs syndrome
• Physically handicapped due to extensive orthopedic
problems
• Neurologically impaired, spinal cord injuries
• Sickle cell anemia.
Referral
L.A. Care works with the local Regional Centers for
assistance in locating programs which are available
for infants and children who are eligible for early
intervention services through local education agencies
and family resource centers. L.A. Care works closely
with the local Early Start Programs and Regional
Centers to ensure that medical and health assessment
information is provided/processed in a timely manner
as follows:
• Children must be referred to an Early Start Program
within two (2) working days of identifying that child
as potentially requiring developmental interventions
services.
• Federal Regulation requires that the Early Start
programs and Regional Centers complete the
individual family service plan, eligibility assessments
and eligibility determination within forty five (45)
days from the receipt of the referral.
• Parents or guardians may refer children directly to
Early Start/Early Intervention Services.
PCPs or specialists may refer to Early Start/Early
Intervention programs for children who meet the
eligibility criteria using the L.A. Care and/or its delegated
entities’ referral process, or refer the member directly
to Early Start/Early Intervention programs. Once it is
determined that a referral is needed, L.A. Care and/or its
delegated entities’ liaison/coordinator will contact PCP to
make referrals to an Early Start Program. L.A. Care and/
or its delegated entities will notify PCPs and can work
with the local regional centers for assistance in locating
programs which are available for infants and children who
are eligible for early intervention services through local
education agencies and family resource centers.
Coordination of Care
PPGs shall:
• Designate a Case Manager to interface with a
designated L.A. Care Liaison, Early Start/Early
Intervention programs, Regional Centers, L.A. City
Special Education Programs (SELPA), PCP, and the
member’s family or guardian as necessary.
• Implement procedures to ensure confidential
transfer of medical documentation to and from the
PCP to Early Start/Early Intervention programs in
compliance with all Federal and State regulations.
• Establish procedures for identification and
management of problems with the PCP, Early Start/
Early Intervention programs, SELPAS’ Regional
Centers, and L.A. Care.
• Ensure that the PCP maintains the role of the overall
case manager for the member and assure appropriate
referrals for members assessed as needing Early Start/
Early Intervention programs.
78
• Provide comprehensive case management as necessary.
• Maintain logs of active EI/ES cases.
• Ensure that members continue to receive medically
necessary care and that coordination of care is
documented in members’ medical records.
• Continue to provide medically necessary covered
services while the member receives waiver services as
long as the member is enrolled in L.A. Care.
PCP Responsibilities
When eligible members for early intervention
services are referred to an Early Start Program, the
PCP shall assure:
• Participation/cooperation in the development of the
member’s Regional Center individual service plan
• Provision of available medical reports, as requested,
to the early intervention team, keeping in mind
the 45-day time lines required by state and federal
statute for the completion of the initial Individual
Family Service Plan (IFSP)
• Follow up and coordination of treatment
plans between the PCP, specialists and Early
Start Programs. Consultations and ongoing
responsibilities for preventive care and all medically
necessary services are specified by the specialty care,
diagnostic and treatment services, therapies and
durable medical equipment.
Problem Resolutions
L.A. Care is available to review and attempt to resolve
any disagreements over diagnosis and/or treatment
authorizations with providers, local Regional Centers
and the Local Education Agencies. Any unresolved
issues should be forwarded to the L.A. Care UM
Liaison for assistant.
SPECIALTY MENTAL HEALTH
All inpatient mental health and outpatient specialty
mental health services are carved out of and excluded
from L.A. Care’s responsibilities under the Medi-
Cal contract with DHS, and will be provided by the
L.A. County Department of Mental Health (LAC/
DMH) in accordance with the current MOU between
L.A. Care and LAC/DMH. L.A. Care will ensure
contracted PPG network and Primary Care Physicians
(PCP) provide basic outpatient mental health services,
within the scope of the PCP’s practice and training,
and shall ensure appropriate referral of members
to and coordination of care with LAC/DMH for
assessment and treatment of mental health conditions,
outside the scope of their practice and training.
L.A. Care’s UM Liaison will act as a resource to the
PPGs/PCP’s to ensure understanding of the referral
process and to define services that are part of the
PPGs’ and PCPs’ responsibility. e resolution of
disputes is a shared responsibility between L.A. Care
and LAC/DMH and will be processed as defined in
the fully executed MOU, L.A. Care policies and the
established state laws and regulations.
ALCOHOL AND DRUG
TREATMENT PROGRAMS
Substance use disorder treatment services are defined
in the Scope of Benefits section - Members and
Providers may directly refer to L.A. Care’s behavioral
health Provider, Beacon Health Strategies, by calling:
1.877.344.2858 (TTY/TDD 1.800.735.2929).
Referrals are not required from the PPG/PCP or
L.A. Care for Members seeking substance abuse
treatment. Members have additional benefits available
to all Medi-Cal members through the Los Angeles
County Department of Mental Health (DMH)
subject to DMH eligibility criteria.
Inpatient Detoxification
L.A. Care will ensure appropriate medical
inpatient detoxification is provided under the
following circumstances:
• Life-threatening withdrawal from sedatives,
barbiturates, hypnotics or medically complicated
alcohol and other drug withdrawal.
• Where it is medically necessary to monitor the
Member for life-threatening complications. In
such instances, two or more of the following must
be present: tachycardia, hypertension, diaphoresis,
significant increase or decrease in psychomotor activity,
tremor, significant disturbed sleep pattern, nausea and
vomiting, and/or threatened delirium tremens.
• When the member is medically stabilized, the
PCP/L.A. Care shall provide a referral and follow-up
to a Substance Abuse Treatment Program
• For members 18 and older identified with risky or
hazardous alcohol use or a potential alcohol misuse
problem, a PCP can provide up to four 15-minute
Brief Interventions every year.
Outpatient
L.A. Care will maintain processes to ensure that
Alcohol and Drug Abuse Treatment Services be
available to members and are provided as a linked and
carved out benefit through the Office of Alcohol and
Drug Programs of L.A. County.
79
e following services are provided by the Alcohol and
Drug Programs of L.A. County:
• Outpatient Methadone Maintenance
• Outpatient Drug Free Treatment Services
• Perinatal Residential Services
• Day Care Rehabilitative Services
• Naltrexone Treatment Services (Opiate Addiction)
• Outpatient Heroin Detoxification Services
L.A. Care and its contracted PPGs will ensure
Primary Care Physician (PCP) screening of L.A. Care
members for substance abuse during the Initial Health
Assessment and in all subsequent visits as appropriate.
When substance abuse is recognized as a potential
condition, PCPs will refer to a treatment facility
serving the geographic area. Referral is done by using
the substance abuse referral form or by referral to
the Community Assessment Services Center toll free
number 1.800.564.6600.
Members can access substance abuse treatment services
by self-referral, by a family referral or referral from the
PCP or other appropriate provider.
During treatment for substance abuse, all medical
services will continue to be provided by the PCP
or other appropriate medical provider. e PCP
will make relevant medical records available to the
Substance Abuse Treatment Program with appropriate
consent and release of medical record information
following federal and state guidelines.
Pregnant Members
All pregnant members identified as substance abusers
will be recommended for a toxicology screen. If the
member refuses this test, the PCP will explain the
potential negative health outcomes of drugs and
alcohol on the mother and unborn fetus. Treatment
will be recommend and a list of treatment programs
and the toll free number to access a treatment program
will be given to the member. L.A. Care will assist with
care coordination for members, as requested. e
member will be asked to sign a release of information
and confidentiality statement, allowing the treatment
program and the PCP or appropriate medical provider,
to coordinate and communicate about the member’s
treatment progress.
It is the responsibility of the PCP, or appropriate
medical provider, to notify the inpatient facility where
the pregnant woman is likely to deliver, of the existence
of a positive toxicology screen or that substance abuse
or use is suspected. It is the responsibility of the hospital
after the birth, to determine if the fetus has been drug
or alcohol exposed. e hospital will perform the
necessary diagnostic tests and inform Department
of Children and Family Services if drug and alcohol
exposure is suspected.
LOCAL EDUCATION AGENCY LEA MEDICAL
L.A. Care and its PPGs will maintain systems to
refer members to the carve out program and services
through the Local Education Agency Services (LEA).
L.A. Care and its PPGs are responsible for:
• Providing all of the medically necessary covered
services and
• Ensuring the member’s PCP cooperates and
collaborates in the development of the Individual
Education Plan (IEP), Individualized Health and
Support Plan (IHSP) or the Individual Family
Service Plan (IFSP).
L.A. Care is responsible for:
• Providing a Primary Care Physician and all medically
necessary covered services for the members, and shall
ensure that the member’s Primary Care physician
cooperates and collaborates in the development
of the Individual Education Plan (IEP) or the
Individual Family Service Plan.
• Providing basic or complex/comprehensive case
management and care coordination to the member
as necessary to ensure the provision of all medically
necessary covered diagnostic, preventive and
treatment services identified in the Individual
Education Plan developed by the Local Education
Agency with Primary Care Provider participation.
PPGs/PCPs are responsible for:
• Providing all medically necessary covered diagnostic,
preventive, and treatment services identified in the
IEP development.
• Referring the members to the L.A. Care Utilization
Management Care Management Program.
DENTAL SERVICES FOR MEDICAL MEMBERS
Dental Care Treatment Services are a carved out
benefit to Medi-Cal members through the Medi-Cal
Denti-Cal Program. Dental Services for adults ages 21
and over will no longer be payable under the Dentil-
Cal program with a few exceptions. Exemptions to the
eliminated adult dental services include:
• Medical and surgical services provided by a doctor
of dental medicine or dental surgery would be
considered physician services and which service
may be provided by the either a California licensed
physician or a dentist
80
• Pregnancy-related services and services for the
treatment of other conditions that might complicate
the pregnancy and 60 days post-partum
• Members under the Early and Periodic Screening,
Diagnosis and Treatment program
• Members who are under 21 years of age and whose
course of treatment is scheduled to ,continue after
he/she turns 21 years of ages (continuing services for
EPSDT member)
L.A. Care and its PPGs are responsible for Dental
Screening and Referral of Members to the Carved out
Medi-Cal Denti-Cal Program for Dental Treatment
when treatment needs are identified and continuing
benefit coverage exists. Primary Care Providers should
perform dental screenings as part of the IHA, periodic,
and other preventive health care visits and provide
referrals to Medi-Cal Denti-Cal Program for treatment
in accordance with the most current:
• CHDP/AAP guidelines for Member age 21
and younger.
• Guide to Clinical Preventive Services published by
the U.S. Preventive Services Task Force (USPSTF)
for adult members {age twenty-one (21) and older.
Dental Screening Requirements
L.A. Care’s recommended dental screening for all
members is included as part of the initial and periodic
health assessments:
• For members under twenty-one (21) years of age,
a dental screening/oral health assessment shall be
performed as part of every periodic assessment, with
annual dental referrals made commencing at age
three (3) years or earlier if conditions warrant.
• For members under 6 years of age, fluoride varnish
shall be provided up to 3 times in a 12 month
period as indicated in MMCK APL Letter 07-
008. Furthermore PPG agrees to train providers on
fluoride varnish including:
°
How to obtain fluoride varnish supplies
°
Providing fluoride varnish applications, periodic
dental assessments and parental anticipatory
guidance on scheduling visits.
°
Referring children to a dentist for dental
examinations and care at 1 year of age per CHDP
guidelines.
°
Coordinating member care with dental
professionals and
°
Documenting dental assessments and
documenting fluoride varnish (using HCPCS
Code D1203) in the member medical record and
on encounter date provided to the PPG.
Covered Medical Services not provided by Dentist or
Dental Anesthetists:
L.A. Care and its PPGs shall cover and ensure the
provision of covered medical services that are not
provided by dentists or dental anesthetists. Covered
medical services include:
• Contractually covered prescription drugs
• Laboratory service
• Pre-admission physical examinations required for
admission to an out-patient surgical service center
or an in-patient hospitalization required for a dental
procedure (including facility fee
and anesthesia services for both inpatient and
outpatient services).
Financial Responsibility for General Anesthesia
including Conscious Sedation for Dental Services
and Associated Facility Office Charges
L.A. Care and its PPGs are responsible for covering
general anesthesia and associated facility/office charges
for dental procedures rendered in a hospital, surgery
center, or office setting when the clinical status or
underlying medical condition of the patient requires
dental procedures that ordinarily would not require
general anesthesia to be rendered in a hospital, surgery
center, or office setting (as defined by the applicable
DOFR). A prior authorization of general anesthesia and
associated charges required for dental care procedures is
required in the same manner that prior authorization is
required for other covered diseases or conditions.
General anesthesia and associated facility charges are
covered only for the following members, and only if
the members meet one of the criteria as follows:
• Members who are under seven (7) years of age.
• Members who are developmentally disabled,
regardless of age.
• Members whose health is compromised and for
whom general anesthesia Is medically necessary,
regardless of age.
e professional fee of the dentist and any charges of
the dental procedures itself is not covered. Coverage
for anesthesia and associated facility charges may be
covered and are subject to the terms and conditions of
the plan benefits as described in the DOFR.
Referral to Medi-Cal Dental Providers through
Carved Out Medi-Cal Dental Program
L.A. Care and its PPGs must refer members to the
appropriate Medi-Cal dental providers for treatment
of dental care needs. Updated lists of Medi-Cal dental
providers are made available to network providers.
81
CCS Referrals
Dental services for child with complex congenital
heart disease, cystic fibrosis, cerebral palsy, juvenile
rheumatoid arthritis, nephrosis, or when the nature
or severity of the disease makes care of the teeth
complicated may be covered by CCS. Contact the
L.A. Care UM Department or CCS for assistance.
Orthodontia care when a child has a handicapping
malocclusion may be covered by CCS. Contact the
L.A. Care UM Department or CCS for assistance.
Routine dental care and orthodontics are not covered
by CCS.
Targeted Case Management Services
MEMBERS ELIGIBLE FOR AND/OR WHO
ARE RECEIVING TARGETED CASE
MANAGEMENT SERVICES CARVED OUT
SERVICES MEDICAL
Identification and Referral: L.A. Care and/or its
PPGs are responsible for determining whether a
member requires Targeted Case Management services,
and must refer members who are eligible for Targeted
Case Management services to a Regional Center or
local governmental health program as appropriate for
the provision of Targeted Case Management services.
Persons who are eligible to receive targeted case
management services shall consist of the following
Medi-Cal beneficiary groups:
• Persons who have language or other
comprehension barriers.
• Are unable to access or appropriately utilize
services themselves.
• Have demonstrated noncompliance with their
medical regimen.
• Are unable to understand medical directions because
of language or other comprehension barriers.
• Have no community support system to assist in
follow-up care at home.
• Persons who are 18 years of age and older and
who Are on probation and have a medical and/or
mental condition.
• Have exhibited an inability to handle personal,
medical, or other affairs; or are under public
conservatorship of person and/or estate; or have a
representative payee.
• Are in frail health and in need of assistance to access
services in order to prevent institutionalization.
• “High-risk persons” means those persons who
have failed to take advantage of necessary health
care services, or do not comply with their medical
regimen or who need coordination of multiple
medical, social and other services due to the
existence of an unstable medical condition in need
of stabilization, substance abuse or because they are
victims of abuse, neglect, or violence, including, but
not limited to, the following individuals:
°
Women, infants, children and young adults to age
21 pregnant women.
°
Persons with Human Immunodeficiency Virus/
Acquired Immune Deficiency Syndrome.
°
Persons with reportable communicable disease.
°
Persons who are technology dependent. Solely for
the purposes of the Targeted Case Management
Services program, “technology dependent
persons” means those persons who use a medical
technology, embodied in a medical device, that
compensates for the loss of normal use of a vital
body function and require skilled nursing care to
avert death or further disability.
• Persons with multiple diagnoses who require services
from multiple health/social service providers.
• Persons who are medically fragile. Solely for the
purposes of the Targeted Case Management Services
program, “medically fragile persons” means those
persons who require ongoing or intermittent medical
supervision without which their health status would
deteriorate to an acute episode.
Member Receiving Targeted Case
Management Services
For Members who are receiving Targeted Case
Management services specified in Title 22, CCR,
Section 51351, L.A. Care and/or its PPGs shall be
responsible for coordinating the member’s health care
with the Targeted Case Management provider and
for determining the Medical Necessity of diagnostic
and treatment services recommended by the Targeted
Case Management provider that are Medi-Cal
Covered Services.
Targeted Case Management Services means carved-
out Medi-Cal services as specified in Title 22, CCR,
Section 51351 as follows:
Targeted case management services shall include at
least one of the following service components:
• A documented assessment identifying the
beneficiary’s needs. e assessment shall support the
selection of services and assistance necessary to meet
the assessed needs and shall include the following, as
relevant to each beneficiary:
• Medical/mental condition
• Physical needs, such as food and clothing
82
• Social/emotional status
• Housing/physical environment
• Familial/social support system
• Training needs for community living
• Educational/vocational needs
• Development of a comprehensive, written,
individual service plan, based upon the assessment
specified in subsection (a)(1) above. e plan shall
be developed in consultation with the beneficiary
and/or developed in consultation with the
beneficiary’s family or other social support system.
e plan shall be in writing and, as relevant to each
beneficiary, document the following:
°
e nature, frequency, and duration of the services
and assistance required to meet identified needs.
°
e programs, persons and/or agencies to which
the beneficiary will be referred
°
Specific strategies to achieve specific
beneficiary outcomes.
°
Case manager’s supervisor’s signature.
Implementation of the service plan includes linkage
and consultation with and referral to providers of
service. e case manager shall follow-up with the
beneficiary and/or provider of service to determine
whether services were received and whether the
services met the needs of the beneficiary. e follow-
up shall occur as quickly as indicated by the assessed
need, but shall not exceed thirty days(30)from the
scheduled service.
Assistance with accessing the services identified in the
service plan includes the following:
• Arranging appointments and/or transportation to
medical, social, educational and other services.
• Arranging translation services to facilitate
communication between the beneficiary and the case
manager, or the beneficiary and other agencies or
providers of service.
• Crisis assistance planning to coordinate and arrange
immediate service or treatment needed in those
situations that appear to be emergent in nature or
which require immediate attention or resolution in
order to avoid, eliminate or reduce a crisis situation
for a specific beneficiary.
For the target populations defined above at the
beginning of Section
• 5.37 Targeted Case Management -“Members
Eligible For and/or Who are Receiving Targeted
Case Management Services (Carved Out Services),”
crisis assistance planning shall be restricted to
nonmedical situations.
• Periodic review of the beneficiary’s progress toward
achieving the service outcomes identified in the
service plan to determine whether current services
should be continued, modified or discontinued. e
review or reinvestigation shall be:
°
Completed at least every six months,
°
Conducted by the case manager in consultation
with the beneficiary and/or in consultation with
the beneficiary’s family or social support system,
and approved by the case manager’s supervisor.
°
Any modifications to the plan of service shall be
made in writing and become an addendum to the
plan of service.
When Members Under the of Age 21 Are Not
Accepted For Targeted Case Management Services,
Care Coordination/ Case Management Services are
required to be provided In-Plan
If members under age twenty-one (21) have been
referred by L.A. Care and/or its PPGs to a Regional
Center or local governmental health program but who
have not been accepted for Targeted Case Management
Services, L.A. Care and/or its PPGs shall ensure the
members access to services in-Plan that are comparable
to EPSDT Targeted Case Management services.
L.A. Care and/or PPG Responsibilities for EPSDT
Targeted Case Management Services:
Financial Responsibility: L.A. Care and/or its PPGs are
not responsible for payment for services provided under:
• CCS
• Specialty Mental Health
• Targeted Case Management services provided by a
State-contracted referral provider such as a Regional
Center or other governmental agency
L.A. Care and/or its PPGs do have financial
responsibility for and shall provide the following (but
not limited to) EPSDT Supplemental Services in-
network to members when medically necessary for the
purpose of assuring care coordination for:
• Targeted Case Management services
provided in-network.
• EPSDT supplemental services include those targeted
case management services designed to assist children
in gaining access to necessary medical, social,
educational and other services.
• Also See L.A. Care UM Procedure 17033 EDSDT
Supplemental Services for a full list of EPSDT
Supplemental Services.
83
EPSDT SUPPLEMENTAL SERVICES
FOR MEMBERS UNDER THE AGE OF
21 YEARS MEDICAL
For members under the age of twenty-one (21) who are
receiving medically necessary ESPDT Supplemental
Services and Targeted Case Management Services
through the Regional Centers or local governmental
health programs as appropriate, L.A. Care and its
contracted PPGs are responsible for providing ongoing
care coordination/case management services.
L.A. Care and its contracted PPGs are not financially
responsible for the payment of services provided under:
• CCS
• Specialty Mental Health
• Targeted Case Management Services provided by the
Regional Centers or local governmental health programs
For members under the age of twenty-one (21) who are
not receiving medically necessary EPSDT Supplemental
Services and Targeted Case Management Services
through the Regional Centers or local governmental
health programs as appropriate, L.A. Care and its
contracted PPGs are responsible for providing access
to in-network services that are comparable to EPSDT
Targeted Case Management Services
EPSDT Supplemental Services include those targeted
case management services designed to assist children in
gaining access to necessary medical, social, educational
and other services.
L.A. Care is responsible for:
• Assuring members under the age of 21 years are referred
to EPSDT (Screening (including CHDP services
provided by the PCP) and Supplemental services.
• Conducting oversight activities to monitor
the need for EPSDT Screening and EPSDT
supplemental services are evaluated during the
IHA within the initial 120 days of Plan enrollment
membership and during preventive health visits;
when medically indicated.
• e provision of medically necessary EPSDT
supplemental services within Plan and the
provision and coordination of EPSDT
supplemental services if these services are delivered
out-of-plan; when medically indicated.
• Coordinating with the local EPSDT programs to
develop and implement educational programs for PCPs.
L.A. Care and/or PPG Responsibilities/
Financial Responsibility
L.A. Care and/or its PPGs shall provide or arrange
and pay for EPSDT supplemental services or members
under the age of 21 years, including case management
and supplemental nursing services except when
EPSDT supplemental services are provided as CCS
services, or as mental health services. L.A. Care and/or
its PPGs are responsible to have implemented Policies
and Procedures to ensure the identification, diagnosis,
referral, and tracking of eligible members for referral
to EPSDT screening services and determining the
Medical Necessity of EPSDT supplemental services
using criteria established in Title 22, CCR, Section
51240 and 51340.1.
L.A. Care and/or its PPGs shall provide the following
(but not limited to) EPSDT supplemental services to
members when medically necessary for the purpose of
assuring care coordination:
• Targeted Case Management services
• EPSDT supplemental services include those targeted
case management services designed to assist children
in gaining access to necessary medical, social,
educational and other services.
• Cochlear implants
• Supplemental nursing services
• Psychology
• Occupational therapy
• Audiology
• Orthodontics
• DME
• Incontinence medical supplies (including diapers) at
home or in board and care facilities
For young children when their developmental deficits
are such that bowel and/or bladder control cannot
be achieved
Where the incontinence is due to a chronic physical
or mental condition, including cerebral palsy and
developmental delay, and at an age when the child
would normally be expected to achieve continence
• Hearing aids
• Dental and Psychotropic drugs
• Medical nutrition services assessment and therapy
• Pharmacy
• Physical therapy evolution and services
• Pulse oximeters
• Speech therapy
Members are identified for EPSDT Supplemental
Services in the following ways:
L.A. Care and/or its PPGs, provider network PCPs/
specialists identify the need for and make the
appropriate referral for EPSDT supplemental services
84
at the time of the Initial Health Assessment or at
any subsequent health assessment visit. e member,
the member’s parents, legal guardian, and/or other
family members may identify the need for EPSDT
supplemental services. e local CHDP program may
identify the member’s need for EPSDT supplemental
services prior to the member’s enrollment in Medi-Cal
Managed Care.
Any health professional, in or out-of-Plan, or school
professional may identify the member’s need for
EPSDT supplemental services when an encounter
results in one or more of the following:
• e determination of the existence of a suspected
illness or condition.
• A change or complication(s) in the condition.
• A determination that a pre-existing condition may
now be amenable to specific therapeutic intervention.
Prior Authorization
L.A. Care and/or its PPGs may apply their referral
authorization processes to EPSDT supplemental
services based upon medical necessity criteria using
the criteria established in Title 22, CCR, Sections
51340 and 51340.1 subject to the Medi-Cal and
other regulatory grievance and appeal procedures. e
requirements for documentation of authorizations,
denials and appeals shall be in accordance with
applicable contractual and regulatory requirements.
Upon identification of the need for EPSDT
supplemental services, including EPSDT supplemental
services that are not covered services under the terms
of their contract (i.e., CCS and MH) L.A. Care and/or
its delegated entities must provide the member with a
referral to an appropriate provider or organization.
EPSDT Supplemental Services Will Meet the
Following Criteria:
• e services requested are to correct, or ameliorate a
defect, physical or mental illness, discovered during
any health assessment.
• e supplies, items and/or equipment requested are
medical in nature.
• e services requested are not solely for the
convenience of the member, the family, the
physician or any other provider of service.
• e services requested are not primarily cosmetic
in nature or designed to primarily improve the
member’s appearance.
• e services requested are safe and are not
experimental and are recognized as an accepted
modality of medical practice.
• e services requested are the most cost effective
when compared with alternatively acceptable and
available modes of treatment.
• e services requested are within the authorized
scope of practice of the provider and are an
appropriate mode of treatment for the medical
condition of the member.
• e service requested improves the overall
health outcome as much as, or more than, the
established alternatives.
• e predicted beneficial outcome outweighs the
potential harmful effects.
Care Coordination and Liaison Process for EPSDT
Supplemental Services
L.A. Care and/or its PPGs will:
• Ensure that the PCP provides basic case
management for the member and assures appropriate
referrals for members with potential and/or eligible
EPSDT supplemental services needs.
• Implement procedures to ensure confidential
transfer of medical documentation between the
PCP and EPSDT supplemental services providers in
compliance with all federal and state regulations.
• Provide liaison/case management staff to coordinate
EPSDT supplemental services including but not
limited to:
• Developing and implementing written plans for
communicating issues of EPSDT supplemental
services eligibility, available services, arranging
consultation with regional supple-mental service
providers, and providing coordination of care of
services with network providers.
• Facilitating bi-directional communication between
regional EPSDT supplemental service providers and
the member’s PCP, whether or not the referral is for
a covered service.
• Coordinating and providing the member with
appropriate out-of-Plan referrals when necessary for
EPSDT supplemental services not covered by the Plan.
• Maintaining an ESPDT supplemental services
referral log(s) which includes the services provided
and the treatment outcomes.
EPSDT supplemental services – In Home Shift
Nursing/Private Duty Nursing (PDN)
EPSDT services are provided to full-scope Medi-Cal
beneficiaries who are under the age of 21. Services
may be authorized once medical necessity criteria
have been met.
85
L.A. Care is responsible for providing PDN services;
L.A. Care does not delegate this responsibility to
PPGs. PPGs must submit prior authorization
requests to L.A. Care UM Department.
Authorized services must meet either the regular Medi-
Cal definition of medical necessity or the Institutional
Level of Care definition for medical necessity services,
which is outlined in CCR, Title 22, Division 3,
Section 51124.6, 51335, 51343.1 and 51343.2
Authorized services must be cost-effective to the
Medi-Cal program. is means that the individual
cost of providing EPSDT private duty nursing services
in home settings must be less than the total cost
incurred by the Medi-Cal program for providing the
care in a licensed health care facility. When necessary,
a home health assessment will be arranged to validate
the necessity of the requested services and to ensure
that the home is an appropriate environment for the
provision of the requested services.
EPSDT services are subject to prior authorization. When
medical necessity criteria have been met, such requests
will be approved. Cases in which medical necessity
criteria have not been met will be denied or modified as
appropriate to meet the needs of the member.
How to Refer a Member for EPSDT PDN
If a provider has a member who requires EPSDT
PDN services, the provider should complete an
Authorization Request Form and submit it to
L.A. Care’s UM Department.
Authorization requests must be accompanied
by medical documentation sufficient to support
the medical necessity of the services. Required
documentation includes the following:
• Completed prior authorization request form
(clearly mark requested service as –“FOR EPSDT
SUPPLEMENTAL SERVICES – PRIVATE
DUTY NURSE”)
• Plan of Treatment (POT) signed by a physician
(within 30 days);
• Nursing Assessment, signed by a physician (within
30 days);
• Medical information supporting the nursing
services requested, i.e. medication record, discharge
summary notes, and treatment notes.
Medical necessity for Private Duty Nurse (PDN) will
be assessed utilizing the information provided by the
requesting physician and criteria defined in Title 22
Title 22, Division 3, Section 51124.6 (Pediatric Sub-
Acute Care):
• Tracheostomy with dependence on mechanical
ventilation for a minimum of 6 hours per day.
• Dependence on tracheostomy care requiring
suctioning at least every 6 hours, and room air mist
or oxygen as needed, and dependence on one of the
six treatment procedures listed below :
°
intermittent suctioning at least every 8 hours and
room air mist and oxygen as needed
°
continuous IV therapy, including administration of
a therapeutic agent necessary for hydration or of IV
pharmaceuticals, or IV pharmaceutical administration
of more than one agent, via peripheral or central
line, without continuous infusion
°
peritoneal dialysis treatments requiring at least 4
exchanges every 24 hours
°
tube feeding by means of a nasogastric or
gastrostomy tube
°
other medical technologies required continuously,
which require the services of a professional nurse
°
biphasic positive airway pressure at least 6 hours
a day, including assessment or intervention every
3 hours and lacking either cognitive or physical
ability to protect his or her airway
• Dependence on total parenteral nutrition or other
IV nutritional support, and dependence on one of
the treatment procedures specified above.
• Dependence on skilled nursing care in the
administration of any 3 of the 6 treatment
procedures listed above
• Dependence on biphasic positive airway pressure or
continuous positive airway pressure at least 6 hours
a day, including assessment or intervention every 3
hours and lacking either cognitive or physical ability
to protect his or her airway and dependence on one
of the 5 treatment procedures specified in procedures
1-5 listed above.
PDN hours will be approved based on the services to
be provided and the willingness of family participation
in care. Authorizations will be given for up to 90
calendar days at a time, pending continued eligibility.
All services will be coordinated by L.A. Care staff.
EPSDT, PDN, and CCS
e CCS program may authorize EPSDT
supplemental service requests for skilled nursing
services, PDN, also known as shift nursing, from
a Registered Nurse (RN) or a Licensed Vocational
Nurse (LVN) and/or Pediatric Day Health Care
(PDHC) services under the EPSDT benefit. Under
Medi-Cal, the day program is less than
24 hours, individualized, and family-centered,
86
with developmentally appropriate activities of play,
learning, and social integration designed to optimize
the individual’s medical status and developmental
functioning, so that he or she can remain with the
family. ese services do not include respite care (See
California Code of Regulations [CCR], Title 22,
Section 51184[k] [1] [B].)
L.A. Care will coordinate services with local CCS agency.
EXCLUDED SERVICES REQUIRING MEMBER
DISENROLLMENT MEDICAL
Major Organ Transplants
Except for kidney transplants, major organ transplant
procedures that are covered by Medi-Cal Fee-for-
Service are not covered by L.A. Care. When a member
is identified as a potential major organ transplant
candidate, L.A. Care must refer the member to a
Medi-Cal approved transplant center. If the transplant
center Physician considers the member to be a
suitable candidate, L.A. Care will submit a Treatment
Authorization Request (TAR) to either the San
Francisco Medi-Cal Field Office (for adults) or the CCS
Program (for children) for approval. L.A. Care’s Care
Manager will notify the Member Services Department
to initiate disenrollment of the member when all of the
following has occurred:
• Referral of the member to the organ transplant facility
• Facility’s evaluation has concurred that the member is
a candidate for major organ transplant
• Major organ transplant is authorized by either DHCS
Medi-Cal Field Office or the CCS Program
L.A. Care and its PPGs are responsible for providing all
medically necessary covered services until the member has
been disenrolled from L.A. Care. Upon disenrollment,
L.A. Care will ensure COC by transferring all for the
member’s medical documentation to the transplant
physician. e effective dates may be retroactive to
the beginning of the month in which the member
was approved so Care Managers will follow all services
provided through the completion of the disenrollment.
LONG TERM CARE LTC
Effective April 1, 2014 California’s Coordinated Care
Initiative (CCI) began transitioning LTC services
to managed care for a sub-set of beneficiaries. is
includes skilled level of care and sub-acute level of
care for adults. As the CCI benefit transition is tied to
dual eligibility or beneficiaries’ month of birth, PPGs
are encouraged to contact L.A. Care for assistance in
understanding member’s eligibility for LTC services.
For members not eligible for CCI, L.A. Care’s Two
Plan Model Contract language defining long term care
as the month of admission plus the following month
continues. For members admitted to Nursing Facilities
where there is no plan to return to the community
setting, member should be submitted to DHCS/HCO
for disenrollment to Medi-Cal Fee for Service.
CHILD HEALTH AND DISABILITIES
PREVENTION PROGRAM CHDP
L.A. Care has a mutually agreed upon arrangement
with the local School Districts that provide EPSDT/
CHDP services. at arrangement describes:
• Eligibility requirements, scope of services, client
services and outreach, tracking and follow-
up, health education, data collection, quality
assurance mechanisms, dispute resolution and
billing/ reimbursement mechanisms governing the
relationship between and among L.A. Care and the
participating school districts.
• How L.A. Care will directly reimburse schools
for the provision of some or all of the CHDP
services, including guidelines for sharing of critical
medical information.
• Guidelines specifying coordination of services
reporting requirements, quality standards, processes
to ensure services are not duplicated, and process for
notification to member/student/parent on where to
receive initial and follow-up services.
• PPGs are required to maintain a “medical home”
and ensure the overall coordination of care and case
management of members who obtain CHDP services
through the local school districts or school sites.
• PCP will provide basic case management for the
member and coordinate the provision of any
referrals or additional services necessary to diagnose
and/or treat conditions identified during the school
EPSDT/CHDP assessment.
• PCP will also provide ongoing preventive and
primary services, as required.
• EPSDT/CHDP services are provided to members for
school entry only while maintaining the “medical home”
with the PCP for ongoing health care management.
• e PCP, as the medical home, is responsible for
ongoing comprehensive health care delivery.
Reimbursement to Schools for the Provision of
School Based EPSDT/CHDP Services
L.A. Care shall be responsible for paying school district
claims directly for EPSDT/CHDP services provided in
accordance with the agreement as determined by the

87
total amount of claims. L.A. Care will generate a PPG
Claims Paid reconciliation report to identify claims paid
on behalf of the PPG by L.A. Care for that capitation
period. L.A. Care Claims Department is responsible
for routing the PM160 forms to the appropriate PCP
for identified care coordination within 30 days of
claims payment.
Provider Training
L.A. Care will collaborate with the PPGs and the
Los Angeles area CHDP programs to ensure provider
training regarding school linked EPSDT/CHDP services.
Attachment A
L.A. Care UM Timeliness Standards
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Emergency Care No prior authorization
required; follow the
reasonable lay person
standard to determine that
the presenting complaint
might be an emergency.
N/A N/A
Post-Stabilization
Following Medical
Screening in the
Emergency Room
Decision Timeframe:
Within 30 minutes of
request or the requested
service is deemed approved
Practitioner:
For approvals:
Verbal notification
within 30 minutes of
request, (if after hours
a tracking number is
provided authorizing
the requested service
and follow-up the
next business day
with an authorization
number.)
For denials/
modifications:
verbal notification
within 30 minutes of
requests and fax (with
confirmation) or
electronic notification
to the requesting
practitioner the same
day of the denial
decision
Practitioner and Member
For denials/modifications:
written notification to requesting
practitioner and member
deposited with the United States
Postal Service in time for pick-up
same day

88
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Pre-Service Urgent
Expedited Request.
An Expedited
Request means any
request for medical
care or treatment
with respect to which
the application of
the time periods for
making non urgent
care determinations:
Could seriously
jeopardize the life or
health of the member
or the member’s
ability to regain
maximum function,
based on a prudent
layperson’s judgment,
or In the opinion of
a practitioner with
knowledge of the
member’s medical
condition, would
subject the member
to server pain that
cannot be adequately
managed without
the care or treatment
that is the subject of
the request.
Decision Timeframe:
e decision must be made
within a timely fashion
appropriate to the member’s
condition not to exceed
72 hours after receipt of
the initial request.in cases
where the enrollee faces
imminent and serious threat
to health, including but
not limited to the potential
loss of life, limb, or other
major bodily function, or
the normal timeframe for
the decision-making process
as set forth in sentence one
of this paragraph, would be
detrimental to the enrollee’s
life or health, or could
jeopardize the enrollee’s
ability to regain maximum
function.
Practitioner and
Member:
Initial Notification
of Decision:
Verbal notification
to requesting
practitioner and
member as soon as the
decision is made not
to exceed 72 hours
after receipt of the
original request.
Practitioner and Member:
Written Notification
For Approvals:
Approval Template
for denials/modifications,
provide an expedited written
notification to requesting
practitioner and member as
the member’s health condition
requires and no later than72 hours
(3 calendar days) after receipt of
the request deposited with the
United States Postal Service in
time for pick-up by 72 hours (or 3
calendar days) from the receipt of
the original request.
Downgrade an
Expedited Request
to Routine – this is a
modify decision that
must be made by a
physician reviewer
Decision Timeframe:
In a timely fashion
appropriate to the member’s
condition not to exceed 72
hours after receipt of the
initial request
Practitioner:
Initial Notification
of Decision:
Verbal notification
to requesting
practitioner
as soon as the decision
is made not to exceed
72 hours after receipt
of the original request
Practitioner and Member:
Written Notification to the
requesting practitioner and
member same day as the
downgrade decision using the
MISSING
COPY?

89
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Delay of
Pre-Service Urgent
Delay of Expedited
Request
A delay to ask
for additional
information is not a
requirement:
Decision Timeframe:
e time limit for a decision
of an expedited request may
be extended past the original
72 hours by an additional
48 hours up to 5 calendar
days if the member requests
an extension.
If more information
is needed, notify the
requesting practitioner or
member by phone within 24
hours of receipt of the initial
request. Allow at least 48
hours for the practitioner
or member to provide the
additional information.
Make the decision within
48 hours of a) receiving a
response from the member
or practitioner or b) the
expiration of the 48 hours
allowed for the additional
information to be supplied,
whichever is sooner.
Practitioner:
Verbal or fax
notification
to requesting
practitioner same day
as delay decision
Practitioner and Member:
Written Notification to the
requesting practitioner and
member same day as delay
decision
NOA TEMPLATE:
Delay

90
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Pre-Service Routine
Non-urgent Request
Decision Timeframe for
Medi-Cal & MCLA
Decisions to approve,
modify, deny, or terminate
requests by providers prior to
the provision of health care
services to enrollees that do
not meet the requirements
for the 72-hour review shall
be made in a timely fashion
appropriate for the nature of
the enrollee’s condition, not
to exceed five (5) working
days from the receipt of
the information reasonably
necessary to render a decision
(these are requests for
specialty service, cost control
purposes, out-of-network not
otherwise exempt from prior
authorization) in accordance
with Health and Safety
Code, Section 1367.01,
or any future amendments
thereto, but, no longer than
14 calendar days from the
receipt of the request.
Decision Timeframe
for L.A. Care Covered, and
PASC-SEIU
Decisions to approve,
modify, deny, or terminate
requests by providers prior to
the provision of health care
services to enrollees that do
not meet the requirements
for the 72-hour review shall
be made in a timely fashion
appropriate for the nature of
the enrollee’s condition, not
to exceed five (5) working
days from date of receipt
of request
Practitioner:
Initial Notification:
All decisions:
Within 24 hours of
the decision with
confirmation
(Notification May
Be Oral and/or
Electronic)
Practitioner and Member:
Denial/Modification
Within 2 working days of denial/
modification decision
Deposited with the United States
Postal Service in time for pick-up
no later than the third working
day after the decision is made not
to exceed 14 calendar days from
receipt of the original request.
NOA TEMPLATE:
Denial or Modify
Approvals:
Written notification
mailed to member

91
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Delay of Pre-Service
Routine
Non-urgent Request
- Extension Needed
A delay to ask
for additional
information is not a
requirement:
e delay extension
is 14 days for Medi-Cal
and L.A. Care
Covered & 30 days
for PASC-SEIU
Medi-Cal and
L.A. Care Covered
Members can request
an additional 14
days to total 28
days; (And the
additional 14 days
is granted only if the
member or provider
makes the request
or L.A. Care can
provide justification
upon request by
the State for the
need for additional
information and how
it is in the Member’s
interest.
Decision Timeframe
Medi-Cal, L.A. Care
Covered, & PASC-SEIU
Within 5 working days of
receipt of request
Any decision delayed
beyond the time limits is
considered a denial and
must be immediately
processed as such.
Practitioner:
All decisions:
Within 24 hours of
the decision with
confirmation
(Notification May
Be Oral and/or
Electronic)
Practitioner and Member:
NOA TEMPLATE: Delay
Important NCQA Note:
Since the delay extension is only
14 days for making the decision
for Medi-Cal and L.A. Care
Covered & 30 days for PASC-
SEIU, NCQA would expect the
member be given the full 14 days-
or 30 days respectively to respond.
Although allowing the full time
of 14 or 30 days for the member/
provider to respond provides very
little time for the UM decision
following the delay period,
according to NCQA, it is more
important to provide as much
time as possible to the member/
provider within mandated
timeframes to provide the
requested information.

92
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Requests To
Continue Routine
Current Service/
Treatment Other
an Acute Hospital
(Such as PT, Home
Health, Long Term
Care, etc.)
For Medi-Cal
10 day advance
notice required
for termination
of services ( i.e.
stopping services)
Decision Timeframe:
If a request to extend
a course of treatment
beyond the period of time
or number of treatments
previously approved does
not meet the definition of
“urgent care,” the request
may be handled as a new
request and decided within
the time frame appropriate
for the type of decision (i.e.
preservice (within 5 working
days of receipt of request
or post-service within 30
calendar days of receipt of
request).
However, it is important
to assess whether it is
reasonable to handle
the request as urgent if
application of a non-urgent
time frame could involve
an unnecessary interruption
in the member’s treatment
that may jeopardize the
member’s health or ability to
recover.
Timeframes specifically for
Home Health Requests
1. Home Health Discharge
Orders = URGENT
(Same Day), otherwise,
patient may end up staying
in-house for another day
2. Home Health Extension =
Pre-service Urgent (24-72
hours),
Practitioner:
All decisions:
Within 24 hours
of the decision
with confirmation
(Notification May
Be Oral and/or
Electronic)
Member:
Approvals:
Within 24 hours
(Written Notification)
Practitioner and Member:
Written Notification:
For denials/modifications: the
notice must be mailed at least 10
days before the date of action,
except as permitted by the
exceptions described in column
“Type of Request”
NOA Template: Terminate
Exceptions from the advance
notice required in this section:
e notice may be mailed no later
than the date of action if:
1. ere is factual information
confirming the death of a member;
2. ere is receipt of a clear written
statement signed by a member
that:
A. Member no longer wishes
services; or
B. Information is given that
requires termination or
reduction of services and
indicates that the member
understands that this must
be the result of supplying that
information;
3. e member has been admitted
to an institution where the
member is ineligible under the
plan for further services;
4. e member’s whereabouts are
unknown and the post office
5. returns agency mail directed to
him indicating no forwarding
address
6. e fact is established that the
member has been accepted for
Medicaid services by another
local jurisdiction, State,
territory, or commonwealth;
7. ere is a change in the level of
medical care is prescribed by the
Member’s physician;
8. e notice involves an adverse
determination made with regard
to the preadmission screening
requirements
9. e date of action will occur in
less than 10 days- long term care
exceptions to the 30 days notice

93
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Urgent Concurrent
Review (acute
hospital inpatient)
Urgent Concurrent
reviews are those
reviews associated
with inpatient care.
A new request for
inpatient care is
considered urgent
concurrent review
and ongoing
hospitalization
requests are
considered urgent
concurrent review
unless determined
otherwise.
Upon receipt of a
new request for
urgent concurrent
review from a
hospital, a review
must be requested.
If the request for
authorization is made
while a member is in
process of receiving
care, the request is
an urgent concurrent
request if medical care
requested meets the
definition of urgent,
even if L.A. Care did
not approve the earlier
care.
For example, if
L.A. Care finds out
on day 2 that a
member is in an
inpatient facility,
and the member’s
practitioner requests
authorization for
additional inpatient
days, L.A. Care
handles the request as
an urgent concurrent
request.
Decision Timeframe:
Within 24 hours of receipt of
the request for authorization.
If the request for
authorization is made while
a member is in process of
receiving care, the request is
an urgent concurrent request
if medical care requested
meets the definition of
urgent, even if L.A. Care did
not approve the earlier care.
For example, if L.A. Care
finds out on day 2 that a
member is in an inpatient
facility, and the member’s
practitioner requests
authorization for additional
inpatient days, L.A. Care
handles the request as an
urgent concurrent request.
Upon receipt of a request for
urgent concurrent review,
L.A. Care UM immediately
requests necessary
information. For operational
purposes 24 hours is
considered equivalent to 1
calendar day.
Hospital Inpatient Stay
Requests
Hospital Inpatient Stay
Requests are considered
Concurrent Urgent and the
Urgent Concurrent decision
timeframe applies unless:
Necessary information is not
received within 24 hours
of receipt of the request for
authorization and at least
one call has been made
to conduct the review
or request the necessary
information. e timeframe
for decision making changes
from Concurrent Urgent to
Pre-Service Urgent (see Pre-
Service Urgent above).
Practitioner:
Initial Notification
of Decision:
All Decisions:
Verbal, fax (with
confirmation), or
electronic notification
to the requesting
practitioner within 24
hours of the receipt of
the request
Practitioner and Member:
Written Notification:
For denials/modifications:
written notification to requesting
hospital within 24 hours of the
receipt of the request.
NOA Template:
Provider Terminate

94
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
If L.A. Care receives
a request for coverage
of an acute inpatient
stay after the
member’s discharge,
L.A. Care handles
the request as a post-
service issue.
When the hospital inpatient
care has already been
received, L.A. Care can
decide to review the request
for the already-rendered
care as part of the Urgent
Concurrent request, or
change the timeframe to
Post-Service request (see
Post-Service below).
If the request for
authorization for an acute
hospital stay is received after
the member’s discharge, the
request is considered a Post-
Service request (see Post-
Service below).
Course of
Treatments Requests
If the request for
authorization is to extend a
course of treatment beyond
the period of time or number
of treatments previously
approved by L.A. Care does
not meet the definition of
Urgent Care, the request is
handled as a new request
and decided within the
timeframe appropriate for
the type of decision (i.e., Pre-
Service or Post-Service).
Request to Continue
Concurrent Review
(Acute Hospital
Inpatient)
A concurrent
review decision
is any review for
an extension of a
previously approved
ongoing course
already in place
Decision Timeframe:
If the request for
authorization is to extend
a course of treatment
beyond the period of time
or number of treatments
previously approved does
not meet the definition of
Urgent Care, the request is
handled as a new request
and decided within the
timeframe appropriate for
the type of decision (i.e.,
Pre-Service or Post-Service).
Practitioner:
All Decisions:
Within 24 hours of
receipt of the request
Practitioner and Member:
Written Notification:
Within 24 hours of receipt
of the request
If oral notification is given within
24 hours of request, then written/
electronic notification must be
given no later than 3 calendar days
after the oral notification.
NOA Template: to Hospital
Terminate
Post-Service /
Retrospective
Review
Decision Timeframe:
Within 30 calendar days
from receipt or request
N/A Practitioner and Member:
Within 30 calendar days of receipt
of the request.
NOA Template: Denial or Modify

95
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Hospice - Inpatient
Care
Decision Timeframe:
Within 24 hours of
receipt of request
Practitioner:
Initial Notification:
Within 24 hours of
making the decision
Member:
None Specified
Practitioner and Member:
Written Notification
Within 2 working days of making
the decision
NOA Template: Terminate
Pharmaceuticals
Including
Injectables, Routine
Within one business day of
receipt of the request.
For denials,
verbal notification
to member
and requesting
practitioner within
the same time frame
as the decision.
For denials, written notification
to the member and requesting
practitioner by confirmed
facsimile transmission or
deposited with the United States
Postal Service in time for pick-up
within one business day after the
decision.
Pharmaceuticals
Including
Injectables, Urgent
Concurrent And
Urgent Preservice
Within one calendar day of
receipt of the request.
For denials,
verbal notification
to member
and requesting
practitioner within
the same time frame
as the decision.
For denials, written notification
to the member and requesting
practitioner by confirmed facsimile
transmission or deposited with
the United States Postal Service
in time for pick-up within one
business day after the decision.
Emergency Care No prior authorization
required; follow the
reasonable lay person
standard to determine that
the presenting complaint
might be an emergency.
N/A N/A
Post-stabilization
following Medical
Screening in the
Emergency Room
Decision Timeframe:
Within 30 minutes of
request or the requested
service is deemed approved
Practitioner:
For approvals: within
30 minutes of request,
(if after hours, a
tracking number is
provided authorizing
the requested service
and follow-up the
next business day
with an authorization
number.)
For denials/
modifications:
verbal notification
within 30 minutes of
requests and fax (with
confirmation) or
electronic notification
to the requesting
practitioner the same
day of the denial
decision
Practitioner:
Written Notification:
For approvals: If no response
within the required 30 minutes,
the requested service is deemed
approved. (If after hours, a
tracking number is provided
authorizing the requested service
and follow-up the next business day
with an authorization number.)
Practitioner and Member -
For denials/modifications:
written notification to requesting
practitioner and member
deposited with the United States
Postal Service in time for pick-up
within 3 calendar days from the
receipt of the original request.

96
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Delay of
Pre-Service Urgent
Delay of Expedited
Request
Decision Timeframe:
e time limit for a decision
of an expedited request may
be extended past the original
72 hours by an additional
48 hours up to 5 calendar
days if the member requests
an extension.
If more information
is needed, notify the
requesting practitioner or
member by phone within 24
hours of receipt of the initial
request. Allow at least 48
hours for the practitioner
or member to provide the
additional information.
Make the decision within
48 hours of a) receiving a
response from the member
or practitioner or b) the
expiration of the 48 hours
allowed for the additional
information to be supplied,
whichever is sooner.
Practitioner:
Verbal notification
to requesting
practitioner and
member as soon as the
decision is made not
to exceed 5 calendar
days if the member
requests an extension,
or within 48 hours of
receiving additional
requested information
or expiration of
the extension
without receipt of
additional requested
information.
Practitioner and Member:
For denials/modifications,
written notification to requesting
practitioner and member
deposited with the United
States Postal Service in time for
pick-up by 5 calendar days or
within 48 hours of receiving
additional requested information
or expiration of the extension
without receipt of additional
requested information not to
exceed 5 calendar days.
NOA Template: Delay
Pre-Service Routine
Non-urgent Request
Decision Timeframe
Within 5 working days of
receipt of request
Practitioner:
Initial Notification:
All decisions:
Within 24 hours
of the decision
with confirmation
(Notification May
Be Oral and/or
Electronic)
Member:
Approvals:
Practitioner and Member:
Within 2 working days of denial/
modification decision
NOA Template: Denial or Modify

97
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Delay of
Pre-Service Routine
Non-urgent
Request - Extension
Needed
Decision Timeframe:
Medi-Cal-Within 5
working days of receipt of
information not to exceed
14 calendar days from date
of receipt of request
Practitioner:
All decisions:
Within 24 hours
of the decision
with confirmation
(Notification May
Be Oral and/or
Electronic)
NOA TEMPLATE: Delay
Medi-CalPractitioner and
Member: Within 2 working days
of decision to delay; however:
14 days allowed for delay; Member
can request an additional 14
days to total 28 days; (And the
additional 14 days is granted only
if the member or proider makes
the request or the Plan/PPG can
provide justification upon request
by the State for the need for
additional information and how
it is in the Member’s interest. Any
decision delayed beyond the time
limits is considered a denial and
must be immediately processed
as such. is means the decision
making & notification processing,
must not exceed the last day of the
delay time limit (for Medi-Cal
- 14 or 28 days, and also when
requested information has not been
received, not before the last day of
the delay time limit (for Medi-Cal
14 or 28 days
Important NCQA Note:
Since the State allows only 14
days for making the decision for
Medi-Cal. Although we realize
this provides very little time
for your organization to make
a decision, NCQA believes it
is more important to provide
the member with as much time
as possible within the state's
mandated requirement, to provide
the information. Please also
understand that delaying to ask
for additional information is not a
requirement: e organization may
make a decision within the routine
5 business day timeframe on the
information received initially with
the request without requesting any
additional information.

98
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Medi-Cal Only-
Requests to
Continue Routine
Current Service/
Treatment (such
as PT, LTC, etc.)
Exceptions from
the advance notice
required in this section:
e notice may be
mailed not later than
the date of action if:
(a) ere is factual
information
confirming
the death of a
member;
(b) ere is receipt
of a clear written
statement signed
by a member that–
(1) Member no
longer wishes
services; or
(2) Information
is given that
requires
termination
or reduction
of services and
indicates that
the member
understands
that this must
be the result of
supplying that
information;
(c) e member has
been admitted
to an institution
where the member
is ineligible under
the plan for
further services;
(d) e member’s
whereabouts are
unknown and
the post office
returns agency
mail directed to
him indicating no
forwarding address
Decision Timeframe:
within 5 working days of
receipt of request
Practitioner:
All decisions:
Within 24 hours
of the decision
with confirmation
(Notification May
Be Oral and/or
Electronic)
Member:
Approvals:
Within 24 hours
(Written Notification)
Practitioner and Member:
Written Notification:
For denials/modifications:
the notice must be mailed at
least 10 days before the date of
action, except as permitted by the
exceptions described in column
“Type of Request”
NOA Template: Terminate

99
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
(e) e fact is
established that
the member has
been accepted for
Medicaid services
by another local
jurisdiction,
State, territory, or
commonwealth;
(f) ere is a change
in the level of
medical care
prescribed by
the Member’s
physician;
(g) e notice
involves an adverse
determination
made with
regard to the
preadmission
screening
requirements
(h) e date of action
will occur in less
than 10 days- LTC
exceptions to the
30 days’ notice
Urgent Concurrent
Review (Acute
Hospital Inpatient)
Urgent Concurrent
reviews are those
reviews associated
with inpatient care.
A new request for
inpatient care is
considered urgent
concurrent review
and ongoing
hospitalization
requests are
considered urgent
concurrent review
unless determined
otherwise.
Upon receipt of a new
request for urgent
concurrent review
from a hospital,
a review must be
requested.
Decision Timeframe:
Within 24 hours of
receipt of the request for
authorization. If the request
for authorization is made
while a member is in process
of receiving care, the request
is an urgent concurrent
request if medical care
requested meets the
definition of urgent, even if
L.A. Care did not approve
the earlier care.
For example, if L.A. Care
finds out on day 2 that a
member is in an inpatient
facility, and the member’s
practitioner requests
authorization for additional
inpatient days, L.A. Care
handles the request as an
urgent concurrent request.
Practitioner:
Initial Notification
of Decision:
All Decisions:
Verbal, fax (with
confirmation), or
electronic notification
to the requesting
practitioner within
24 hours of the receipt
of the request
Member:
Approvals:
Within 24 hours of
receipt of the request
Practitioner and Member:
Written Notification:
For denials/ modifications: written
notification to member and
requesting practitioner within
24 hours of the receipt of the
request.
NOA Template: Terminate

100
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
If the request for
authorization is made
while a member is in
process of receiving
care, the request is
an urgent concurrent
request if medical
care requested meets
the definition of urgent,
even if L.A. Care
did not approve the
earlier care.
For example, if
L.A. Care finds
out on day 2 that
a member is in an
inpatient facility,
and the member’s
practitioner requests
authorization for
additional inpatient
days, L.A. Care
handles the request as
an urgent concurrent
request.
If L.A. Care receives
a request for coverage
of an acute inpatient
stay after the
member’s discharge,
L.A. Care handles
the request as a post-
service issue.
For example, if L.A. Care
finds out on day 2 that a
member is in an inpatient
facility, and the member’s
practitioner requests
authorization for additional
inpatient days, L.A. Care
handles the request as an
urgent concurrent request.
Upon receipt of a request for
urgent concurrent review,
L.A. Care UM immediately
requests necessary information.
For operational purposes 24
hours is considered equivalent
to 1 calendar day.
Hospital Inpatient
Stay Requests
Hospital Inpatient Stay
Requests are considered
Concurrent Urgent and the
Urgent Concurrent decision
timeframe applies unless:
Necessary information is not
received within 24 hours
of receipt of the request for
authorization and at least
one call has been made
to conduct the review
or request the necessary
information. e timeframe
for decision making changes
from Concurrent Urgent to
Pre-Service Urgent (see Pre-
Service Urgent above).
When the hospital inpatient
care has already been
received, L.A. Care can
decide to review the request
for the already-rendered
care as part of the Urgent
Concurrent request, or
change the timeframe to
Post-Service request (see
Post-Service below).
If the request for
authorization for an acute
hospital stay is received after
the member’s discharge, the
request is considered a Post-
Service request (see Post-
Service below).

101
Notication Timeframe
Type of Request Decision Initial Notication Written Notication
Course of Treatments
Requests
If the request for
authorization is to extend a
course of treatment beyond
the period of time or number
of treatments previously
approved by L.A. Care does
not meet the definition of
Urgent Care, the request is
handled as a new request and
decided within the timeframe
appropriate for the type of
decision (i.e., Pre-Service or
Post-Service).
Request to
Continue
Concurrent review
(Acute Hospital
Inpatient)
A concurrent review
decision is any review
for an extension of a
previously approved
ongoing course
already in place
Decision Timeframe:
If the request for
authorization is to extend
a course of treatment
beyond the period of time
or number of treatments
previously approved does
not meet the definition of
Urgent Care, the request is
handled as a new request
and decided within the
timeframe appropriate for
the type of decision (i.e.,
Pre-Service or Post-Service).
Practitioner:
All Decisions:
Within 24 hours of
receipt of the request
Member:
Approvals:
Within 24 hours of
receipt of the request
Post-Service /
Retrospective
Review
Decision Timeframe:
within 30 calendar days
from receipt or request
Practitioner and
Member:
None specified
Hospice - Inpatient
Care
Decision Timeframe:
Within 24 hours of receipt
of request
Practitioner:
Initial Notification:
Within 24 hours of
making the decision
Member:
None Specified

102
Attachment B
L.A. Care Health Plan
Vision, Dental, and Behavioral Health Benet Grid
Medi-Cal
Vision
Benefits
Medi-Cal Vision care services are covered and are the responsibility of and provided by L.A. Care.
• L.A. Care has contracted with Vision Vendor - VSP - to coordinate L.A. Care’s Medi-Cal
members’ vision care and lenses services.
• All referrals for Vision care services should be referred to VSP.
• To access Medi-Cal vision care and lenses benefits, Medi-Cal members should be directed to call
VSP at the toll free number 1.800.877.7195.
• To find out more about Medi-Cal eye exams or vision care coverage, Medi-Cal members can also
call L.A. Care Member Services at the toll free number1.888.839.9909
For Medi-Cal Members up to Age 21, and certain adults as defined by DHCS, Medi-Cal Eye
exams are covered by L.A. Care and carved out to the Prison Industry Labs. Lenses are limited to
one pair of eyeglasses every two years unless:
• Prescription has changed at a minimum of .50 diopters
• replacement lenses are needed because the member’s previous lenses have been lost, stolen, broken,
or marred and damaged beyond the member’s control to a degree significantly interfering with
vision or eye safety (a certificate or statement is required)
• Frame needs replacement because a different size or shape is necessary.
• is includes lenses and covered frames for eyeglasses when authorized.
L.A. Care Medi-Cal Adults (age 21 and over):
According to MMCD All Plan Policy Letter #10-010 “Reinstatement of Optometry Services”,
on July 15, 2010 the State of California reinstated Optometry services for Medi-Cal Adults
retrospective to July 1, 2009
To date, reinstatement of Optometry Services for Medi-Cal Adults does not include lenses for adults.
Dental
Benefits
Medi-Cal dental benefits are not covered under L.A. Care, but are carved out to the Medi-Cal
Denti-Cal Program.
Effective July 1, 2009 the State of California excluded Adult dental services from the Medi-Cal
Denti-Cal Program
L.A. Care is responsible for ensuring that Medi-Cal members up to age 21 are referred to
appropriate Medi-Cal dental providers through the Medi-Cal Denti-Cal Program.
To find a Denti-Cal dentist, Medi-Cal members up through age 21 should call Denti-Cal at the toll
free number 1.800.322.6384.
Denti-Cal can also be contacted on the internet at http://www.denti-cal.ca.gov/

103
Medi-Cal
Behavioral
Health
Benefits
L.A. Care covers Medi-Cal outpatient mental health services for members with mild to moderate
mental health conditions.
L.A. Care covers Inpatient Detoxification Alcohol/Drug Treatment:
L.A. Care is responsible for and covers appropriate medical inpatient detoxification provided under
the following circumstances: Life threatening withdrawal from sedatives, barbiturate, hypnotics or
medically complicated alcohol and other drug withdrawal. is Inpatient detoxification is covered in
the rare cases where it is medically necessary to monitor the member for life threatening complications;
two or more of the following must be present, tachycardia, hypertension, diaphoresis, significant
increase or decrease in psychomotor activity, tremor, significant disturbed sleep pattern, nausea and
vomiting, threatened delirium tremens. When the member is medically stabilized, the PCP/L.A. Care
shall provide a referral and follow-up to a Substance Abuse Treatment Program.
Medi-Cal Specialty Mental Health Services are carved out from L.A. Care:
Medi-Cal members may receive Specialty Mental Health Services (treatment for serious mental
illness and serious emotional disturbance) from the Los Angeles County Department of Mental
Health (LACDMH) with or without a referral from their PCP.
LACDMH may be reached toll free at 1.800.854.7771
Medi-Cal Alcohol/Drug Treatment Carved Out Services:
Medi-Cal members may receive substance use disorders services from the Los Angeles County
Department of Public Health Substance Abuse Prevention and Control (DPH SAPC) with or
without a referral from their PCP. e following services are the responsibility of and provided by
DPH SAPC:
• Outpatient Methadone Maintenance
• Outpatient Drug Free Treatment Services
• Perinatal Residential Services
• Day Care Rehabilitative Services
• Naltrexone Treatment Services (Opiate Addiction)
• Outpatient Heroin Detoxification Services
DPH SAPC can be reached by calling the Community Assessment Services Center toll free number
1.800.564.6600.
104
6.0 Quality
Improvement Program
L.A. Care annually prepares a comprehensive Quality
Improvement Program that defines L.A. Care’s
Quality Improvement (QI) structures and processes
for all L.A. Care products. e QI Program is
designed to improve the quality and safety of clinical
care and services for L.A. Care’s membership. A copy
of L.A. Care’s QI Program is available upon request
by calling 1.213.694.1250, extension 5772.
e L.A. Care QI Program is responsible for the
following activities:
• Define, oversee, continuously evaluate, and improve
the quality and efficiency of health care delivered
through organizational commitment to L.A. Care’s
goals and principles
• Ensure that medically necessary covered services
are available and accessible to Members, taking
into consideration the Member’s cultural and
linguistic needs
• Ensure L.A. Care’s contracted network of Providers
cooperates with L.A. Care quality initiatives
• Ensure that timely, safe, medically necessary, and
appropriate care is available
• Consistently meet quality standards as required
by contract, regulatory agencies, recognized care
guidelines, the industry, and the community
• Promote health education and disease prevention
designed to promote life-long wellness by
encouraging and empowering each Member to adopt
and maintain optimal health behaviors
• Maintain a well-credentialed network of
Providers based on recognized and mandated
credentialing standards
• Safeguard Members’ protected health
information (PHI)
6.1 Annual Quality Improvement
Program Evaluation
Annually, L.A. Care reviews data reports and other
performance measures regarding program activities
to assess the effectiveness of its QI Program. is
evaluation includes the following:
• Review of completed and continuing program
activities and audit results
• Trending of performance data
• Analysis of the results of QI initiatives including
barriers, successes and challenges
• Assessment of the effectiveness of monitoring
activities and identifying and acting upon quality of
care and service issues
• Evaluation of the overall effectiveness of the QI
program including progress toward influencing
network-wide safe clinical practices as well as the
goals and plans for the next year
6.2 Annual Quality
Improvement Work Plan
e annual QI Work Plan is developed in
collaboration with an interdepartmental team and is
based, in part, upon the results of the prior year’s QI
Program evaluation. Each of the elements identified
on the Work Plan has activities defined, responsibility
assigned, and the date by which completion is
expected. Quarterly updates to the Work Plan are
documented and reported to the Quality Oversight
Committee (QOC) and the Compliance and Quality
Committee of the Board.
6.3 Committee Structure
L.A. Care’s quality committees oversee various
functions of the QI program. e committees serve
as the major mechanism for intradepartmental
collaboration for the QI program.
e Quality Oversight Committee (QOC), a
cross-functional staff committee of L.A. Care,
is the cornerstone for communication within
the organization. It is responsible for aligning
organization-wide QI goals and efforts prior to
program implementation and monitoring the overall
performance of L.A. Care’s QI infrastructure. e
QOC conducts the following activities:
• Reviews current strategic projects and performance
improvement activities to ensure appropriate
collaboration and to minimize duplication of efforts
• Reviews quantitative and qualitative analysis of
performance data of subcommittees through formal
reports as needed
• Identifies opportunities for improvement based
on analysis of performance data and prioritizes
these opportunities
• Tracks and trends quality measures though quarterly
updates of the QI work plan
• Reviews and makes recommendations regarding
quality delegated oversight activities such as
reporting requirements on a quarterly basis
• Reviews, modifies, and approves policies
and procedures
105
• Reviews and approves the QI and UM program
descriptions, QI and UM work plans, quarterly QI
work plan reports and evaluations of the QI and
UM programs.
Network physicians participate in many of L.A. Care’s
QI Committees. For example, the Joint Performance
Improvement Collaborative Committee and Physician
Quality Committee (Joint PICC/PQC) reviews and
approves the updated Clinical Practice Guidelines so that
the QOC members know that the guidelines have been
approved. Upon approval, the updated information is
posted on the L.A. Care website at lacare.org. Providers
are notified of the updates in the next newsletter, which
includes a link to the updated guidelines.
e Joint PICC/PQC’s primary objective is to ensure
practitioner participation in the QI program through
planning, design, and review of programs, quality
improvement activities, and interventions designed to
improve performance. e Joint PICC/PQC provides
an opportunity for L.A. Care to collaborate with the
Provider community and gather feedback on clinical
and service initiatives. e Joint PICC/PQC reports
to the QOC through the QI Medical Director (or
designee). e Joint PICC/PQC serves as an advisory
group to L.A. Care’s QI infrastructure for the delivery of
health services to the CFAD population. Participation
in the Joint PICC/PQC, including committee
membership, is open to network practitioners
representing a broad spectrum of appropriate primary
care specialties serving L.A. Care Members including,
but not limited to, practitioners who provide health
care services to dually-eligible Members or who have
expertise in managing chronic conditions (e.g., asthma,
diabetes, congestive heart failure).
6.4 Clinical Care Measures
L.A. Care measures clinical performance through
Healthcare Effectiveness Data and Information Set
(HEDIS). L.A. Care expects that the network assist
the health plan in continuously improving its HEDIS
rates. e network is also expected by contract to
cooperate with the annual HEDIS data collection
efforts and keep encounter data current and accurate.
6.5 Service Measures
L.A. Care monitors services and Member satisfaction
by collecting, analyzing, and acting on numerous
sources of data, focusing on areas such as Member
satisfaction, complaints and appeals, access to and
availability of practitioners and Provider satisfaction.
e following measures will be collected annually:
• Healthcare Effectiveness Data and Information
Set (HEDIS)
• Consumer Assessment of Healthcare Providers and
Systems (CAHPS)
• Health Outcomes Survey (HOS)
6.5.1 Continuity and Coordination of Medical Care
L.A. Care encourages PPGs and their affiliated
Provider network to assess and improve how well they
coordinate care through the following:
• If referring to a specialist, contact the specialist
before the Member’s appointment.
• Have staff set up a quick phone appointment and
fax over the Member’s medical history.
• Request that the specialist also contact the PCP once
the evaluation and/or treatment is finished.
• Keep track of specialty referrals that require prior
authorization.
• Talk to the PPG about getting timely hospital
discharge reports that will help follow up and
coordinate care after a hospitalization or emergency
room visit.
6.5.2 Continuity and Coordination of
Medical and Behavioral Health Care
L.A. Care provides mental health services and substance
use disorder services through PCPs and Behavioral
Health Specialists from Beacon Health Services. Beacon
Behavioral Services may be reached at 1.877.344.2858.
Specialty Mental Health Services are provided through
the Los Angeles County Department of Mental Health
(LACDMH). ere is no need for an L.A. Care referral
to obtain services from LACDMH. LACDMH may
be reached toll-free at 1.800.854.7771.
L.A. Care will coordinate non-specialty behavioral
health services and cover laboratory, radiological,
and radioisotope services needed for the diagnosis,
treatment, and monitoring of a behavioral health
condition. L.A. Care covers mental health drugs listed
on the formulary and prescribed by the PCP or by a
licensed mental health provider authorized to prescribe
drugs. If medically necessary, L.A. Care may cover a
mental health drug not on the formulary.
For a directory of L.A. Care’s behavioral health
Providers, please refer to the electronic Provider
and hospital directory on L.A. Care’s website, at
http://www.lacare.org/members/member-tools/
find-doctor-or-hospital, which will link to the Find a
Doctor or Hospital tool.
106
6.6 Preventive Health Care Guidelines
More information about Preventive Services is
provided at the following L.A. Care website address:
http://www.lacare.org/providers/provider-
resources/clinical-practice-guidelines
Clinical Practice Guidelines for Acute and Chronic
Medical Care – See the L.A. Care website at http://
www.lacare.org/providers/provider-resources/
clinical-practice-guidelines for current and updated
guidelines for acute and chronic medical care,
including guidelines for asthma and diabetes.
Clinical Practice Guidelines for Behavioral
Health Care – See the L.A. Care website at http://
www.lacare.org/providers/provider-resources/
clinical-practice-guidelines for current guidelines
for behavioral health care, including guidelines for
depression and ADHD.
6.7 Disease Management Programs
L.A. Care’s Chronic Care Improvement Programs
(CCIPs) use a system of coordinated healthcare
interventions and communications in an effort to
improve the health status of those eligible Members
with chronic conditions and those for whom self-
care efforts are significant. e CCIPs achieve this
objective by educating Members and by enhancing
their ability to self-manage their condition or illness.
CCIPs are developed from evidenced-based clinical
practice guidelines and support the practitioner/
patient relationship and plan of care. e current
CCIPs address asthma (L.A. Cares About Asthma),
cardiovascular disease (L.A. Care About Your Heart),
and diabetes (L.A. Cares About Diabetes). To enroll
a Member, contact L.A. Care at 1.866.LA.CARE6
(1.866.522.2736).
Population of Focus: Serving Seniors and
Persons with Disabilities and Health Disparities
L.A. Care seeks to improve the health and overall well-
being of all its members, including seniors and people
with disabilities, as well as focusing on health disparities.
L.A. Care specifically develops programs that target and
accommodate members who are at higher risk for health
disparities, including those related to race and ethnicity,
language, disabilities, and chronic conditions.
6.8 Patient Safety
L.A. Care is committed to improving patient safety
and promoting a supportive environment for network
Providers to improve patient safety in their practices.
Many of the ongoing QI Program measurement
activities include safety components, including measures
for accessibility, availability, adherence to clinical
practice guidelines and medical record documentation.
6.9 Disease Reporting Statement
L.A. Care complies with disease reporting standards as
cited by Section 2500 of Title 17 of the California Code
of Regulations, which requires public health professionals,
medical Providers, and others to report approximately
85 diseases or conditions to their local health department.
e primary objective of disease reporting and surveillance
is to protect the health of the public, determine the extent
of morbidity within the community, evaluate risk of
transmission, and intervene rapidly when appropriate.
Forms to report the required diseases or conditions are
available at http://www.dhcs.ca.gov.
6.10 PPG and Other Contracted Provider
and Vendor Reporting Responsibilities
L.A. Care requires PPGs/their affiliated Provider
networks and contracted vendors to have a mechanism
in place to address the following issues regarding
Critical Incidents:
• Collecting and tracking Critical Incidents by a
Member
• Reporting all Critical Incidents to L.A. Care’s QI
Department every quarter
• Training their staff on protocol for Critical Incidents
A “Critical Incident” is an incident in which a
Member is exposed to one or more of the following:
• Abuse; neglect or exploitation
• Serious, life-threatening, medical event that requires
immediate emergency evaluation by medical
professional(s)
• Disappearance
• Suicide attempt
• Death
• Restraint or seclusion
6.11 Categories of Critical Incidents
6.11.1 Abuse is characterized by any one of
the following:
• Willful use of offensive, abusive, or demeaning
language by a caretaker that causes mental anguish
of any Member
• Knowing, reckless, or intentional acts or failures to
act which cause injury or death or which place a
Member at risk of injury or death
• Rape or sexual assault
107
• Corporal punishment or striking
• Unauthorized use or the use of excessive force in the
placement of bodily restraints
• Use of bodily or chemical restraints, which is not
in compliance with federal laws, state laws or
administrative regulations
6.11.2 Exploitation is characterized
by the following:
An act committed by a caretaker, a relative of a
Member, or any person in a fiduciary relationship with
a Member that entails any one of the following:
• e taking or misuse of property or resources by
means of undue influence, breach of fiduciary
relationship, deception, harassment, criminal
coercion, theft, or other unlawful or improper means
• e use of health services without just compensation
• e use of a Member for the entertainment or sexual
gratification of others under circumstances that
cause degradation, humiliation, or mental anguish
6.11.3 Neglect is characterized by any
one of the following:
• Inability of a Member to secure food, shelter,
clothing, health care, or services necessary to
maintain his/her mental and physical health
• Failure by any caretaker to meet, either by
commission or omission, any statutory obligation,
court order, administrative rule or regulation, policy,
procedure, or minimally accepted standard for care
• Negligent act or omission by any caretaker which
causes injury or death or which places a Member at
risk of injury or death
• Failure by any caretaker, who is required by law
or administrative rule, to establish or carry out an
appropriate individual program or treatment plan
• Failure by any caretaker to provide adequate
nutrition, clothing, or healthcare
• Failure by any caretaker to provide a safe
environment
• Failure by any caretaker to provide adequate
numbers of appropriately trained staff in its
provision of care and services
6.11.4 Disappearance/Missing Member is
characterized by the following:
Whenever there is police contact regarding a missing
Member, regardless of the amount of time the
Member was missing.
6.11.5 Death is characterized by the following:
Whenever the death of a Member is reported
regardless of the cause or setting in which it occurred.
6.11.6 A Serious Life reatening, Medical Event
that Requires Immediate Emergency Evaluation by a
Medical Professional is characterized by the following:
Admission of a Member to a hospital or psychiatric
facility for emergency medical services (treatment by
EMS) that results in medical care that is unanticipated
and/or unscheduled for the Member and which would
not routinely be provided by a physician.
6.11.7 Restraints or Seclusion falls under
one of the following types:
• Personal – the application of pressure, except
physical guidance or prompting of brief duration
that restricts the free movement of part or all of a
Member’s body.
• Mechanical – the use of a device that restricts the
free movement of part or all of a Member’s body.
Such devices include anklets, wristlets, camisoles,
helmets with fasteners, muffs with fasteners, mitts
with fasteners, Posey gait belts, waist straps, head
straps, and restraining sheets. Such devices do
not include those used to provide support for
functional body position or proper balance, such as
a wheelchair belt or one used for medical treatment,
such as a helmet used to prevent injury during a
seizure. It also means to render unusable a device for
free movement, such as locking a wheelchair or not
allowing an individual access to technology.
• Chemical – the use of a chemical (including a
pharmaceutical) through topical application, oral
administration, injection, or other means to control a
Member’s activity and which is not a standard treatment
for a Member’s medical or psychiatric condition.
• Seclusion – involuntary confinement in a room such
that a Member is physically prevented from leaving.
• Isolation – forced separation or failure to include a
Member in the social surroundings of the setting
or community.
6.11.8 Suicide Attempt is characterized
by the following:
e intentional attempt to take one’s own life. A
suicide attempt is limited to the actual occurrence of
an act and does not include verbal suicidal threats by a
Member receiving services.

108
6.12 Referrals to Local Agencies
PPGs, PCPs, and their affiliated Provider networks
and/or vendors must refer identified Critical Incidents
to local Adult Protective Services (APS) agencies or law
enforcement, when appropriate, as required by state
and/or federal regulations.
Suspected Abuse,
Exploitation and Neglect
Adult Protective Services (APS) County Contact Information.
Los Angeles County
http://www.cdss.ca.gov/agedblinddisabled/PG1298.htm
Community & Senior Services
3333 Wilshire Blvd. Suite 400
Los Angeles, CA 90010
1.888.202.4248
24 Hour Abuse Hotline:
1.877.477.3646
http://www.dss.cahwnet.gov/cdssweb/entres/forms/English/SOC341.pdf
Seclusion and
Restraint
Report as Abuse Incident (see above)
Adult Protective Services (APS) County Contact Information.
Los Angeles County
http://www.cdss.ca.gov/agedblinddisabled/PG1298.htm
Community & Senior Services
3333 Wilshire Blvd. Suite 400
Los Angeles, CA 90010
1.888.202.4248
24 Hour Abuse Hotline:
1.877.477.3646
http://www.dss.cahwnet.gov/cdssweb/entres/forms/English/SOC341.pdf
Suicide Attempt For immediate threats: Call 911
For non-immediate threats: e 24-Hour Suicide Prevention Crisis Line
at 1.877.727.4747
Serious Life reatening
Medical Event that Requires
Immediate Emergency
Evaluation by a Medical
Professional
Call 911
L.A. Care, PPGs, PCPs, and their affiliated networks must follow company procedure.
Missing Persons Adult Missing Person Unit: 1.213.996.1800
Note: Contrary to popular belief, law enforcement agencies in California do not require
a person to wait a specific period of time before reporting a missing person.
Death Report notification of death to immediate supervisor for further reporting
direction. In addition, call L.A. Care Member Services: 1.888.839.9909
6.12.1 Critical Incident Reporting Agency/Authority
PPGs and their affiliated provider networks must
report any identified Critical Incident(s) to the
appropriate authorities as required. Critical Incidents
must also be reported to L.A. Care by secure e-mail to
[email protected] on a quarterly basis to L.A. Care’s QI
department via L.A. Care’s Critical Incident Tracking
Report Tool.
109
7.0 Credentialing
7.1 Overview
7.1.1 Criteria and Standards
L.A. Care contracted providers are required to
be credentialed in accordance with L.A. Care’s
credentialing criteria and the standards of the
Department of Health Care Services (DHCS), National
Committee on Quality Assurance (NCQA), and
Centers for Medicare & Medicaid Services (CMS).
7.1.2 Licenses and Qualifications
L.A. Care requires that all providers who are
performing services for L.A. Care members have a
current license at all times to provide patient care
to members and abide by state and federal laws
and regulations. All providers must be qualified to
participate in the Medi-Cal and CMS programs in
order to participate in all L.A. Care lines of business.
Failure to meet Medi-Cal, NCQA and CMS
requirements may be cause for removal from
L.A. Care’s network.
7.2 Delegation of Credentialing
Delegation is a formal process by which an
organization gives another entity the authority to
perform certain functions on its behalf. Although
the organization can delegate the authority to
perform such a function, it cannot delegate the
responsibility for assuring that those functions are
performed appropriately.
7.2.1 Monitoring Credentialing Activities
L.A. Care is responsible for monitoring all contracted
PPGs’, credentialing, and recredentialing activities.
A PPG must pass the L.A. Care Credentialing
Department’s due diligence (pre-delegation)
credentialing audit in order to be delegated the
credentialing responsibility. Otherwise, L.A. Care’s
Credentialing Department is responsible for a
PPG’s credentialing activities. Regardless of a PPG’s
credentialing delegation status, when L.A. Care
has determined, based on L.A. Care’s reasonable
assessment of its provider network, that L.A. Care
already has adequate access to the types of services
provided by the Licentiate, L.A. Care retains the
right to approve new providers and sites, as well as to
terminate or suspend individual providers, based on
credentialing issues at all times.
7.2.2 PPG Accountability
e PPG that has been delegated the credentialing
responsibility is accountable for credentialing and
recredentialing its providers, even if it delegates all
or part of these activities. If the PPG delegates any
credentialing and recredentialing activities, there must
be evidence of oversight of the delegated activity.
ere must be annual evidence of a mutually agreed
upon delegation agreement between the PPG and the
delegate, i.e., NCQA certified Credential Verification
Organizations (CVOs), non-certified CVOs, etc.
e delegation agreement must meet all elements
of NCQA’s standards. As a note, CMS does not
recognize NCQA certified CVOs. As such, all files are
subject to full file review.
7.2.3 When delegates have access to the PPG’s
Member’s protected health information (PHI) or
create PHI in the course of their work, the mutually
agreed-upon document between the PPG and the
delegate must ensure that the information will
remain protected. is is not applicable if there
is no delegation arrangement, or if the delegation
arrangement does not involve the use, creation or
disclosure of PHI.
7.2.4 If the delegation arrangement does not include
the use of PHI in any form, an affirmative statement
to that fact in the delegation agreement is sufficient,
but is not required; the PPG may document the lack
of PHI in a delegation arrangement in other manners.
7.2.5 Prior to delegation, L.A. Care’s Credentialing
Department audits the PPG (the potential delegated
entity) to determine whether the PPG meets
L.A. Care’s criteria for delegation. e Credentialing
Department evaluates the potential delegated entity’s
ability to perform the delegated activities, which
will include all activities related to credentialing and
recredentialing in accordance with the standards
required by L.A. Care, NCQA, DHCS and CMS.
Using a modified version of the Standardized Audit
Tool in accordance with L.A. Care, NCQA, DHCS
and CMS standards, the Credentialing Department
will evaluate delegated entity’s performance.
7.2.6 Types of Delegation Status
7.2.6.1 Upon completion of the pre-delegation
audit, the audit tool is scored and recommendations
regarding delegation are presented to L.A. Care
Credentialing Committee as follows:
7.2.6.1.1 Full Delegation – PPG scores 100%.
No CAP Required.
110
7.2.6.1.2 Full delegation – PPG scores 80% to
99.9% CAP Required.
7.2.6.1.3 Denial of Delegation – PPG Scores 70%
to 79.9%. CAP Required. – Opportunity to cure
deficiencies. A follow up audit will be conducted
within six months. A corrective action must be
successfully completed.
7.2.6.1.4 Denial of Delegation – PPG chooses not
to pursue delegation of credentialing, or receives less
than a 70% on the pre-delegation credentialing audit.
PPG has a Non-Delegated credentialing status for a
minimum of one year. e credentialing of PPG’s
providers is performed by L.A. Care’s Credentialing
department. Denial of delegation letters will be sent to
the PPG.
7.2.6.2 Following recommendations by the
Credentialing Committee, delegation letters will be sent
to the PPG’s scoring 80% or above, and Delegation
Agreements for credentialing will be executed.
7.2.6.3 L.A. Care retains the right to determine in
its sole discretion whether to delegate credentialing
functions regardless of the results of an audit.
7.2.7 Delegation Status
7.2.7.1 All credentialing activities have been delegated
to either the PPG or a combination of a hospital and
PPG. e Delegation Agreement will identify in detail
exactly what functions have been delegated to the PPG.
7.2.8 Delegation Oversight
7.2.8.1 e PPG agrees, upon delegation, to
make available to L.A. Care the credentialing and
recredentialing status on the PPG’s participating
providers, including credentialing data elements as well
as documents and quarterly reports, as appropriate,
using the standardized Industry Collaboration Effort
(ICE) form or another approved L.A. Care format.
7.2.8.2 On an annual basis, L.A. Care will audit
the credentialing and recredentialing activities of the
PPG. e PPG’s credentialing and recredentialing files
will be reviewed according to the following file pull
methodology: A roster of providers which includes
Autism providers credentialed and recredentialed within
the audit period and a list of the PPG’s Utilization
Management providers who make medical decisions
will be requested. In addition, a full roster of the PPG’s
network will also be requested. L.A. Care will also
review the PPG’s quarterly reports for comparison
and file selection. NCQA’s 8/30 methodology will be
used in evaluating files. e minimum files reviewed
will be eight (8) initial files and eight (8) recredential
files. If any credentialing element are deficient
during the review of the 8/30 Rule, then the deficient
element(s) will be reviewed for the remaining files,
up to a maximum of 30 initial credentialing and 30
recredentialing files.
7.2.8.3 L.A. Care’s oversight audit will include
a review of the PPG’s credentialing policies and
procedures, Committee meeting minutes, practitioner
credentialing and recredentialing files which includes
Autism providers, Utilization Management providers
who make medical decisions, a list of contracted health
delivery organizations (HDOs), ongoing monitoring
reports, oversight audits and any sub-delegations
agreements, if applicable.
7.2.8.4 Results of L.A. Care’s oversight audit will be
reported to the PPG, including the corrective action
plan if deficiencies are noted. L.A. Care’s Credentialing
Department works collaboratively with the PPG when
deficiencies have been identified through the oversight
process. e delegate is given a Corrective Action Plan
(CAP) and asked to respond within 30 calendar days.
If no response is received within 30 Calendar days, or
the CAP is not acceptable or complete as submitted,
the Regulatory Affairs and Compliance (RA&C)
Department sends a revised CAP letter requesting a
response within 14 calendar days and advising that
failure to respond may be cause for revocation of the
delegation agreement. e PPG will implement such
CAP within the time period stated and will permit a
re-audit by L.A Care or its agent, if requested.
7.2.8.5 If a delegate has not cured the identified
deficiencies by the next annual audit and when
L.A. Care determines the deficiencies are reoccurring
the delegate will be subject to additional point
deduction if their process does not match their policies
and L.A. Care will conduct a focus review of the
delegate’s credentialing activities within six months of
the previous audit, if applicable.
If the delegate continues to demonstrate noncompliance
with the standards, L.A. Care will recommend de-
delegation of the delegate’s credentialing activities
within six months of the previous audit, if applicable.
7.2.8.6 At L.A. Care’s discretion, or in the event that
L.A. Care determines that significant deficiencies are
occurring related to performance by the delegate and
are without remedy and fails to complete the CAP
process and has gone through the exigent process
111
which results in de-delegation, the PPG cannot appeal
and must wait one year to reapply for a pre-delegation
audit. If the pre-delegation audit reveals deficiencies
identified are the same as those from previous
audits, delegation will be at the sole discretion of the
Credentialing Committee, regardless of the score.
7.2.8.7 A PPG that receives a rating of “excellent”,
“commendable”, “accredited”, or “certified”,
from NCQA, will be deemed to meet L.A. Care’s
requirements for credentialing. ese PPGs may be
exempt from the L.A. Care audit of credentialing in
elements for which they are accredited or certified.
As a note, CMS does not recognize NCQA certified
CVOs. In such cases, all files may be subject to full
file review. If a PPG sub-delegates to an NCQA
CVO for primary source activities, the PPG must still
perform annual oversight of these activities for the
Medicare line of business, if applicable.
7.2.8.8 If the PPG is NCQA accredited, and
L.A. Care chooses to use the NCQA accreditation
in lieu of a pre-delegation or annual audit, the PPG
will be required to demonstrate compliance with the
credentialing and recredentialing of UM Medical
Director(s) annually. is will be accomplished
through a signed Attestation submitted by the
Medical Director(s) attesting to compliance with this
requirement. If the PPG is not compliant with this
process, the PPG will be subject to sanctions according
to the PPGSA, Sections 1.36 and 1.37.
7.2.8.9 L.A. Care retains overall responsibility for
ensuring that credentialing requirements are met;
as such, L.A. Care will require documentation from
PPG to establish proof of NCQA accreditation status.
Elements not listed in the NCQA accreditation
documentation will require further validation through
due diligence or annual audits. L.A. Care retains the
right to perform oversight audits as necessary.
7.2.8.10 L.A. Care retains the right to approve new
participating providers/providers and sites (delegated
or sub-delegated), and to terminate, suspend, and/
or limit participation of PPG’s providers who do not
meet L.A. Care’s credentialing requirements.
7.2.9 PPG Responsibilities
7.2.9.1 PPG must have policies and procedures to
address credentialing of providers, non-practitioner
health care professionals, licensed independent
providers, Autism providers, UM providers making
medical decisions, attending physicians within a
teaching facility, if applicable, and HDOs that fall
within in its scope of credentialing. PPG must state
in policy that they do not make credentialing and
recredentialing decisions based on an applicant’s race,
ethnic/national identity, gender, age, sexual orientation
or the types of procedures (e.g., abortions) or patients
(e.g., Medicaid) in which the practitioner specializes.
A statement that the PPG does not discriminate
does not meet the intent of the requirement. e
policy must explicitly describe how it both monitors
and prevents discriminatory practices to ensure that
credentialing and recredentialing are conducted in
a nondiscriminatory manner; taking proactive steps
to protect against discrimination occurring in the
credentialing/recredentialing process these practices
may include but are not limited to periodic audits of
credentialing files and practitioner complaints, and
maintaining a heterogeneous credentialing committee
decisions to sign a statement affirming that they do
not discriminate.
7.2.9.2 PPG will establish standards, requirements
and process for the practitioner/HDOs that are
performing services for L.A. Care Members to ensure
that these providers and HDOs are qualified to
perform the services, and are licensed and/or certified
consistent with L.A. Care, NCQA, DHCS, and
CMS requirements. ese standards, requirements
and processes are applicable regardless whether or
not credentialing and recredentialing activities are
delegated. For CBAS facilities, L.A. Care annually
verifies license and credentialing status.
7.2.9.3 PPG’s policies must explicitly define the
process used to ensure that the information submitted
to L.A. Care is consistent with the information obtained
during the credentialing process which is included
in member materials and practitioner directories.
Specifically, any practitioner information regarding
qualifications given to members must match the
information regarding practitioner’s education, training,
certification and designated specialty gathered during
the credentialing process. “Specialty” refers to an area of
practice, including primary care disciplines.
7.2.9.4 PPG will establish a peer review process by
designating a Credentialing Committee that includes
representation from a range of participating providers.
e credentialing process can encompass separate
review bodies for each specialty (e.g., practitioner,
dentist, and psychologist) or a multidisciplinary
committee with representation from various types of
providers and specialties.
112
7.2.9.5 PPG must notify the practitioner, in writing,
of any adverse actions to the practitioner and notify
L.A. Care of PPG’s action taken as soon as the PPG has
knowledge of the adverse action. e PPG must require
the provider to notify the PPG of any adverse action
taken against the provider within 14 days of knowledge.
7.2.9.6 PPG must document the review of adverse
events, actions taken, the monitoring and follow
through of the process including timeframes and
closure of each adverse events.
7.2.9.7 PPG must notify L.A. Care in writing, if
any contracted practitioner has any adverse action
or criminal action taken against them promptly and
no later than fourteen (14) calendar days from the
occurrence of any adverse event, criminal action,
changes in privileges, accusation, probation, or
other disciplinary action of providers. Failure to
do so may result in the removal of the practitioner
from L.A. Care’s network. is is referenced in
the California Participating Physician Application
Information Release Acknowledgements.
Providers must not have limitations or restrictions
on hospital privileges. L.A. Care’s Credentialing
Committee will make decisions based on review of any
limitations or restrictions that have been imposed. If
a facility should require a proprietary release form to
release information on a practitioner’s hospital status,
the prospective participating practitioner will be
required to complete the required proprietary form.
Failure to do so will be considered non-compliance
with the credentialing/recredentialing process.
7.2.9.8 PPGs that are delegated for credentialing
and recredentialing are required to review, investigate
and take appropriate action for any adverse events
or criminal actions taken against a contracted
provider including, but not limited to fair hearing
and reporting to appropriate authorities as delegated.
L.A. Care retains the right to approve, close panel
to new membership, and/or terminate contracted
providers at all times.
7.2.9.9 Pursuant to PPGSA, L.A. Care reserves the
right to coordinate, consolidate, and participate in any
PPG participating practitioner disciplinary hearing,
conducted in accordance with L.A. Care Policy and
Procedures, and California Business and Professions
Code Section 805.
7.2.9.10 PPG will advise L.A. Care of any changes
to its credentialing and recredentialing policies and
procedures, processes, delegation or sub-delegation,
and criteria within thirty (30) days of the change. If
L.A. Care deems the changed items not in compliance
with L.A. Care, NCQA, DHCS, and/or CMS
requirements, L.A. Care shall notify PPG immediately.
PPG will have 30 days to attain compliance, and,
if not in compliance, L.A. Care may de-delegate
credentialing and assume responsibility for all or part
of the credentialing functions.
7.2.9.11 PPG will provide quarterly reports to
L.A. Care following the end of each report month
(May 15th, August 15th, November 15th, February
15th) with accurate and complete PPG practitioner
data. PPG must provide Board certification status and
Board expiration date, if applicable, when adding a
practitioner to L.A. Care’s network and any updates.
7.2.9.11.1 Using the standardized ICE format and
Excel grid will include the following:
• Number of adds/deletes of PCPS (i.e. MDs, DOs, etc.)
• Number of adds/deletes of SCPS (i.e. MDs, and
DOs, etc.)
• Numbers of adds/deletes of independent providers
(i.e. DCs, DPMs, etc.)
• Any new or revised policies and procedures,
additions of a computer system, CVO
• Providers termed for quality issues
7.2.9.12 PPG will submit a profile of the PCP,
SCP, Mid-Levels and Autism providers credentialing
information to L.A. Care. Along with the profile,
the following documents must be attached; first
and last page of the contract, W-9, all addenda to
the California Participating Physician Application
(CPPA), and appropriate hospital coverage letter, if
applicable, must be attached.
7.2.9.13 PPG profiles must meet L.A. Care’s
requirements as follows: Providers who do not
have hospital privileges with a L.A. Care contracted
hospital, may use the PPGs admitting panel or
have a direct agreement with a practitioner who
has admitting privileges within the same specialty
at a L.A. Care contracted hospital. is agreement
must capture responsibility for the provisions and
coordination of care, when members are discharged
from the hospital, referral of members back to PCP
with a hospital discharge summary, and coordinate
a seven day week, 24-hour call coverage utilizing the
providers that are contracted with the PPG.
113
7.2.9.14 e PPG is responsible to ensure that
members have access to their assigned PCP twenty-four
(24) hours per day, seven (7) days per week. PPG will
notify L.A. Care thirty (30) days prior to any changes
in the status of any of the PPG’s participating providers,
including, but not limited to, termination, resignation
or any leave. PPGs must ensure that physicians on leave
of any duration are covered by a practitioner with a like
specialty (e.g. Pediatrician covered by a Pediatrician) or
a provider who is otherwise experienced and qualified to
provide appropriate coverage.
Failure to ensure that physicians on extended leave
are covered by a credentialed practitioner with a like
specialty or a provider who is otherwise experienced
and qualified to provide appropriate coverage shall be
considered a material breach and may result in sanctions
as outlined in section 1.36 of the Participating Provider
Group Service Agreement (PPGSA).
7.2.9.15 PPGs will ensure that providers and all of
their contracted sites are reviewed in accordance with
the requirements of L.A. Care, NCQA, DHCS and
CMS requirements. All Providers must have a current
and valid (i.e., within 3 years of the date of initial
credentialing/recredentialing) full scope site review at the
time of initial credentialing/recredentialing. Providers
who are only contracted for the Medicare program are
required to undergo a medical record review.
7.2.9.16 PPG’s Board of Governors (Board), or the
group or committee to whom the Board has formally
delegated the credentialing function, reviews and
approves the credentialing policies and procedures on
an annual basis.
7.3 Provisional Credentialing
7.3.1 Provisional Credentialing Criteria
e PPG may conduct provisional credentialing (in
compliance with L.A. Care, NCQA, DHCS, and
CMS requirements) of providers who completed
residency or fellowship requirements for their
particular specialty area within the 12 months before
the credentialing decision.
7.4 Condentiality and
Practitioner Rights
7.4.1 Confidential Information
PPG’s credentialing policies and procedures must
clearly state the confidential nature of information
obtained in the credentialing process. e PPG must
also describe the mechanisms in effect to ensure
confidentiality of information collected in this process.
e PPG must ensure that information obtained
in the credentialing process is kept confidential
and, ensure that providers can access their own
credentialing information, as outlined in Right to
review information, below.
7.4.2 Confidential Files
During the credentialing process, all information that
is obtained is considered confidential. All Committee
meeting minutes and practitioner files are to be securely
stored and can only be seen by an appropriate Medical
Director or his/her equally qualified designee, and the
Credentialing Committee members. Documents in
these files may not be reproduced or distributed, except
for confidential peer review and credentialing purposes
consistent with Section 1157 of the State of California
Evidence Code and Section 1370 of the Health and
Safety Code of the State of California.
7.4.3 Right to Review Information
PPG’s policies and procedures must state that providers
are notified of their right to review information
obtained by the PPG to evaluate their credentialing
application. e evaluation includes information
obtained from any outside source (malpractice
insurance carriers, state licensing boards, etc.).
7.4.4 Written Policies and Procedures
PPG must have written policies and procedures
for notifying a practitioner in the event that
credentialing information obtained from other
sources varies substantially from that provided by the
practitioner. e policies and procedures must clearly
identify timeframes, methods, documentation and
responsibility for notification.
7.4.5 Sources of Information
PPG is not required to reveal the source of information
if the information is not obtained to meet PPG
credentialing verification requirements or if disclosure is
prohibited by law.
7.4.6 Right to Correct Erroneous Information
Policies and procedures must also state the practitioner’s
right to correct erroneous information submitted by
another source. e policy must clearly state:
7.4.6.1 Timeframe for changes
7.4.6.2 Format for submitting corrections
7.4.6.3 e person to whom corrections must
be submitted
114
7.4.6.4 Receipt of documented corrections
7.4.6.5 How providers are notified of their right to
correct erroneous information as outlined in this manual.
7.4.7 Right to Application Status Information
PPG’s credentialing policies and procedures must state
that providers have a right to be informed of the status of
their applications upon request, and must also describe
the process for responding to such requests, including
what information that the PPG may share with providers.
is element does not require the PPG to allow a
practitioner to review references, recommendations or
other peer-review protected information
7.5 Requirements
7.5.1 Qualifications
All providers/providers must be qualified to participate
in the Medi-Cal and CMS programs in order to
participate in all L.A. Care lines of business. Providers/
providers must not be excluded, suspended or
ineligible or opted out for participation in the Medi-
Cal or Medicare programs. Failure to meet Medi-Cal
and/or CMS requirements may be cause for removal
from L.A. Care’s network.
7.5.2 Notification of Sanctions or Reports
e PPG or vendor is required to notify the Plan
immediately when providers are identified on any
sanctions reports for removal from network.
7.5.3 ese requirements include verification of the
following circumstances:
7.5.3.1 Excluded Providers
7.5.3.1.1 Confirmation that providers/providers or
other health care providers/entities are not “excluded
providers” on the Office of the Inspector General
(OIG) sanction list that identifies those individuals
found guilty of fraudulent billing, misrepresentation
of credentials, etc. Organizations employing or
contracting with providers have the responsibility to
check the sanction list with each new issuance of the
list, as they are prohibited from hiring, continuing to
employ, or contracting with individuals named on that
list. All contracted PPGs and vendors are required to
review OIG reports publication on a monthly basis
and are required to ensure they are reviewing the most
current iteration and take action as required by contract.
Lists of the excluded providers are available at:
https://exclusions.oig.hhs.gov/Default.aspx
7.5.3.2 Medi-Cal Suspended and Ineligible Providers
7.5.3.2.1 Medi-Cal law (Welfare and Institutions Code,
Section 14123) mandates that the Department of
Health Care Services (DHCS) suspends a Medi-Cal
provider when he/she has been (a) convicted of a crime
involving fraud or abuse of the Medi-Cal program, or
(b) suspended from the federal Medicare program for
any reason.
7.5.3.2.2 Suspension is automatic when either of
the above events occurs, and suspended Medi-Cal
providers will not be entitled to a hearing under the
California Administrative Procedures Act.
7.5.3.2.3 All contracted PPGs and vendors, i.e.,
carved out contacts, are required to review sanctions
Med-Cal publication on a monthly basis and are
required to ensure they are reviewing the most current
iteration and take action as required by contract.
List of suspended providers are available at:
http://files.medi-cal.ca.gov/pubsdoco/man-
ual/man_query.asp?wSearch=%28%23file-
name+%2A%5F%2Az03%2A%2E%2A%29&w-
FLogo=Suspended+and+Ineligible+Provider+List&w-
FLogoH=32&wFLogoW=418&wAlt=Suspend-
ed+and+Ineligible+Provider+List&wPath=pubsdoco%2F-
publications%2Fmasters%2DMTP%2FzOnlineOn-
ly%2Fsusp100%2D49%5Fz03%2F&prevP=search
7.5.3.3 Opt-Out Providers
7.5.3.3.1 If a practitioner/provider opts out of
Medicare, that practitioner/ providers may not accept
Federal reimbursement for a period of 2 years. e
only exception to that rule is for emergency and
urgently needed services. Payment must be made for
emergency or urgently needed services furnished by
an “opt-out” practitioner to a member, but payment
should not otherwise be made to opt-out providers.
Information on providers who opt-out of Medicare
may be obtained from the local Medicare Part B
carrier. is list must be checked on a regular basis.
7.5.3.3.2 All contracted PPGs and vendors are
required to review Opt-Out publication on a
monthly basis and are required to ensure they are
reviewing the most current iteration and take action
as required by contract.
List of Opt-Out providers are available at:
https://data.cms.gov/dataset/Medicare-Individual-
Provider-List/u8u9-2upx
115
7.5.3.4 National Provider Identifier (NPI) Number
7.5.3.4.1 All providers of Covered Services, including
PCP and specialists, must have a valid National
Provider Identifier (NPI) Number.
7.5.3.4.2 All contracted PPGs and vendors are
required to verify that their contracted providers have
a valid NPI number.
7.5.3.5 Clinical Laboratory Identifier
Amendments (CLIA) Certification
7.5.3.5.1 CMS regulates all laboratory testing (except
research) performed on humans in the U.S through
the Clinical Laboratory Improvement Amendments
(CLIA). CLIA requires all facilities to meet certain
federal requirements if they perform even one test,
including waived tests, on materials derived from
human body for the purpose of providing information
for the assessment of health, diagnosis, prevention,
or treatment of any disease or impairment of, or the
assessment of health of, human beings to meet certain
Federal requirements. If a facility performs tests for
these purposes, it is considered a laboratory under
CLIA and must apply and obtain a certificate from the
CLIA program that corresponds to the complexity of
the tests performed.
7.5.3.5.2 All contracted PPGs and vendors shall ensure
that all contracted laboratory testing sites have either a
current and valid CLIA certificate or waiver of a certificate
of registration along with a CLIA identification number.
If a vendor is used to perform laboratory testing, the
vendor is required to have a CLIA certificate and there
must be a contract between both parties.
7.5.3.6 Drug Enforcement Administration (DEA) or
Controlled Dangerous Substances (CDS) Certificate,
as applicable
7.5.3.6.1 e PPG must have a documented process
for allowing a provider with a valid DEA certificate
and participates within L.A. Care’s network, to write
all prescriptions for a provider who has a pending
DEA certificate, or require an explanation from
a qualified practitioner who does not prescribe
medications and provide arrangements for the
provider’s members who need prescriptions for
medications. e PPG will maintain a current DEA
or CDS certificate on all contracted providers.
7.5.3.7 Medicare Number
7.5.3.7.1 All PPGs must ensure that their contracted
facilities and contracted providers that serve Medicare
members must have a Medicare number.
7.5.3.8 Ongoing Monitoring of Sanctions,
Complaints, and Quality Issues
7.5.3.8.1 PPG must implement a process for
monitoring practitioner sanctions, complaints and the
occurrence of adverse events between recredentialing
cycles. e PPG must conduct ongoing monitoring of
all providers who fall within the scope of credentialing.
e PPG must be fully compliant with L.A. Care,
NCQA, DHCS, and CMS and use the approved
current sources of sanction information.
7.5.3.8.2 PPG must develop and implement policies
and procedures for ongoing monitoring of practitioner
sanctions, complaints and quality issues between
recredentialing cycles, and must take appropriate action
against providers when it identifies occurrences of poor
quality. PPG identifies and, when appropriate, acts on
important quality and safety issues in a timely manner
during the interval between formal credentialing.
7.5.3.8.3 PPG must show how they monitor all
adverse events and demonstrate this process has
been reviewed by the Credentialing Committee
at least every six months. e PPG’s Credentials
committee may vote to flag a practitioner for ongoing
monitoring. e PPG must fully demonstrate in
the PPG’s Credentialing Committee which types of
monitoring they impose, the timeframe used, the
intervention, and the outcome.
7.5.3.8.4 PPG must provide proof of any practitioner
identified on the OIG, Medi-Cal Suspended &
Ineligible List, Medicare Opt-Out, etc. e PPG
must demonstrate that they have taken action to
terminate the contracted practitioner. If a practitioner
has been identified on any of the lists above, they are
to be terminated for all lines of business for L.A. Care.
7.5.3.8.5 PPG must notify L.A. Care promptly
and no later than fourteen (14) calendar days of any
adverse event or criminal action, changes in privileges,
accusation, probation, other disciplinary action against a
practitioner, or non-compliance with L.A. Care’s policies
and procedures. Failure to do so may result in the
removal of the practitioner from L.A. Care’s network.
7.5.3.8.6 L.A. Care retains the right, based on quality,
facility site review, adverse events, criminal actions, or
changes in privileges, accusations, and/or probation
to close providers to new member assignment until
such time the L.A. Care’s Credentialing Committee
determines otherwise.
116
7.5.3.8.7 PPG who fails to comply with any
requested information within the specific timeframe is
subject to sanctions as described in L.A. Care’s policies
and procedures and PPGSA, section 1.36 and 1.37.
In the event that the PPG fails to respond as required,
L.A. Care will perform the oversight functions of
the Adverse Event and will be subject to L.A. Care’s
policies and procedures and Credentials committee’s
outcome of the adverse events.
7.6 Recredentialing
7.6.1 Participating providers must satisfy
recredentialing standards required for continued
participation in the network. Recredentialing is
completed three years from the month of initial
credentialing and every three (3) years thereafter.
7.6.2 A facility site review does not need to be
repeated as part of the recredentialing process if the
site has a current passing score (this applies to PCPs). A
passing site review survey will be considered “current”
if it is dated within the last three (3) years (with use of
new tool) of the recredentialing date, and does not need
to be repeated until the due date of the next scheduled
facilitysite review survey or when determined necessary
through monitoring activities by the Plan
7.6.3 If a practitioner/provider is contracted for the
Medi-Cal and Medicare programs, they are subject
to both a facility site review and medical record
review. However, if the practitioner/provider is only
contracted for the Medicare program, a medical record
review is all that is required. However, Facility Site
Review or other L. A. Care staff may visit a provider’s
office at any time without prior notification.
7.7 Credentialing Committee
7.7.1 e Credentialing Committee will consist of
not less than three (3) participating providers in good
standings with state and federal agencies in order to
ensure accurate representation of medical specialties.
7.7.2 Administrative support staff may attend at the
request of the Chair but are not entitled to vote.
7.7.3 A quorum should consist of three (3)
practitioner committee members. Any action taken
upon the vote of a majority of committee members
present at a duly held meeting at which a quorum is
present shall be an act of the committee.
7.8 Meetings and Reporting
7.8.1 e Credentialing Committee shall meet at least
quarterly but as frequently necessary to demonstrate
follow-up on all findings and required action. e
Credentialing Committee shall maintain a permanent
record of its proceedings and actions. e activities,
findings, recommendations, and actions of the
committee must be reported to the governing body or
designee in writing on a scheduled basis.
7.8.2 Additional meetings of the Credentialing
Committee may be called by the Committee
Chairperson on an as-needed basis.
7.9 Committee Decisions
7.9.1 L.A. Care considers the decision made by the
Credentialing Committee to be final.
7.9.2 e PPG’s credentialing policies and procedures
must include a time frame for notifying applicants
of credentialing decisions, not to exceed sixty (60)
calendar days from the Committee’s decision.
7.10 Participation of Medical Director
or other Designated Practitioner
7.10.1 PPG must have a practitioner (medical
director or equally qualified designated practitioner)
who has overall responsibility for the credentialing
process. PPG’s credentialing policies and procedures
must clearly indicate the Medical Director is directly
responsible for the credentialing program and must
include a description of his/her participation.
7.11 Committee Functions
7.11.1 Review and evaluate the qualifications of each
practitioner applying for initial credentialing, and
recredentialing.
7.11.2 Investigate, review and report on matters
referred by the Medical Director or his/her designee
or the Board regarding the qualifications, conduct,
professional character or competence of any applicant
or practitioner.
7.11.3 Review of periodic reports of activities, i.e.,
ongoing monitoring reports, credentialing activity
reports, etc.
7.11.4 Review annually policies and procedures
relevant to the credentialing process, and make revisions
as necessary to comply with L.A. Care, NCQA, DHCS,
and CMS requirements, regulations and practices.
117
7.11.5 PPG’s Credentialing Committee must
review practitioner credentials and give thoughtful
consideration to the credentialing elements before
making recommendations about a practitioner’s ability
to deliver care. At a minimum, the Credentialing
Committee must receive and review the credentials of
providers who do not meet the PPG’s established criteria.
7.11.6 PPG’s Credentialing Committee must clearly
document detailed discussion that reflects thoughtful
consideration of credentials reviewed during its meeting
in the minutes. Discussion that demonstrates approval/
denial does not meet the intent of detailed discussion.
7.11.7 When the credentialing function is not
delegated to the PPG, L.A. Care’s Credentialing
Department will be responsible for credentialing and
recredentialing activities in-house.
7.11.8 L.A. Care’s Credentialing Committee may
terminate, suspend or modify participation of
those providers who fail to meet eligibility criteria.
e decisions to terminate, suspend, or modify
participation of a contracted practitioner as a result of
a reportable quality of care issue shall be subject to an
appeals process by the practitioner.
7.12 Credentials Committee File Review
7.12.1 PPG’s policies and procedures must describe
the process used to determine and approve clean
files. ey must identify the Medical Director as the
individual with the authority to determine that a file
is “clean” and to sign off on it as complete, clean and
approved. With regard to clean files, the practitioner
may not provide care to members until the final
decision of the Credentialing Committee or the Medical
Director or his or her equally qualified designee.
7.12.2 PPG’s credentialing and recredentialing
policies must explicitly define the process used to reach
a credentialing decision.
7.13 Appeal and Fair Hearing
7.13.1 Delegated PPG, or if not delegated, L.A. Care
must have a mechanism for fair hearing and appeal
process for addressing adverse decisions that could
result in limitation of a practitioner’s participation
based on issues of quality of care and/or service, in
accordance with all applicable statutes. e process
should include notification to practitioner within an
established time frame and established time frame for
practitioner to request a hearing, scheduling of hearing
requests, followed by the procedures hearings, the
composition of the hearing committee and the agenda
for the hearing.
7.13.2 Licentiate is not entitled to a hearing under
LS-005: When L.A. Care has determined, based
on L.A. Care’s reasonable assessment of its provider
network that L.A. Care already has adequate access to
the types of services provided by the Licentiate.
7.13.3 PPG must have an appeal process for instances
in which it chooses to alter the conditions of a
practitioner’s participation based upon issues of quality
of care and/or service. Except as otherwise specified
in this Provider Manual, any one or more of the
following actions or recommended actions taken for a
medical disciplinary cause or reason shall be deemed
actual or potential adverse action and constitute
grounds for a hearing:
7.13.3.1 Denial of initial panel appointment
7.13.3.2 Denial of reappointment to panel
7.13.3.3 Suspension of panel appointment
(except as described below)
7.13.3.4 Revocation of panel appointment
7.13.3.5 Other adverse restrictions on panel
appointment (except as described below)
7.13.4 e following actions entitle the practitioner
the opportunity to appear before a Credentialing
Committee to present rebuttal evidence before a final
determination is made. e practitioner shall have
the right to be represented by an attorney during
this process. e following actions also entitle the
practitioner the opportunity for a hearing before a
hearing panel in the event that the final determination of
a Credentialing Committee is adverse to the practitioner,
unless the right to a hearing has been forfeited.
7.13.5 Peer Review Committee has the right
to recommend closing panels to new members/
specific age range or gender of a practitioner’s panel
appointment while an investigation is being conducted
to determine the need for committee action, without
the practitioner having a right to the rebuttal and/or
fair hearing process set forth below.
7.13.6 e Credentialing Committee has the right
to recommend immediate suspension or restriction
of a practitioner’s membership if the committee
reasonably believes that the health of any individual
would be jeopardized by the continued participation
of the practitioner. In the case of such an immediate
suspension or limitation on privileges (summary
118
action), the practitioner has the right to receive notice,
an opportunity to present rebuttal information and
a fair hearing, in accordance with the procedure
described in L.A. Care’s Policy LS-005, but those
rights apply subsequent to the summary action, rather
than prior to it.
7.14 Required Reporting
7.14.1 PPG must file a Section 805 report with the
Medical Board of California and a report with the
National Practitioner Data Bank/Healthcare Integrity
Protection Data Bank within thirty (30) calendar
days after the effective date of the action, if any of the
following events occur:
7.14.2 e practitioner’s application for participation
status (credentialing) is denied or rejected for a
medical disciplinary cause or reason.
7.14.3 e practitioner’s participation status is
terminated or revoked for a medical disciplinary cause
or reason.
7.14.4 Restrictions are imposed or voluntarily
accepted for a cumulative total of thirty (30) days
or more for any 12-month period, for a medical
disciplinary cause or reason.
7.14.5 e practitioner resigns or takes a leave of
absence from participation status following notice of
any impending investigation based on information
indicating medical disciplinary cause or reason or for
any of the following:
7.14.5.1 Resigns, retires, or takes a leave of absence.
7.14.5.2 Withdraws or abandons the application.
7.14.5.3 Withdraws or abandons his or her request
for renewal.
7.15 Expired License
7.15.1 L.A. Care requires that all providers who
are performing services for L.A. Care members have
a current California license at all times to provide
patient care to members and abide by State and
Federal laws and regulations.
7.15.2 Failure to Renew
7.15.2.1 Providers contracted with L.A. Care shall
be licensed or certified by their respective board or
agency, where licensure or certification is required by
law. e license to practice medicine in California must
be renewed upon expiration (every two (2) years).
7.15.2.2 If any practitioner fails to renew their license
by the expiration date, the following steps will be
initiated by L.A. Care.
7.15.2.3 If the identified practitioner(s) has
member enrollment:
7.15.2.3.1 Close provider’s panel to new members
upon license expiration.
7.15.2.3.2 Notify PPG of expiration and possible
reassignment of members
7.15.2.3.3 Remove assigned members from
unlicensed practitioner/practitioner five (5) business
days following license expiration, if not renewed
7.15.2.3.4 Reassign members to a qualified licensed
credentialed practitioner and
7.15.2.3.5 Remove unlicensed practitioner from network
7.15.2.4 If the identified practitioner(s) has no
member enrollment:
7.15.2.4.1 Close practitioner’s panel to new members
7.15.2.4.2 If practitioner has not renewed by the
fifth (5
th
) business day following the expiration date,
the unlicensed practitioner will be removed from
L.A. Care’s network
Note: Credentialing and recredentialing standards
are the same for all L.A. Care product lines. Some
product lines may not be required to adhere to some
standards and that is clearly identified in the policies
and procedures.
In addition L.A. Care retains the right to close the
practitioner’s panel without notice.
119
8.0 Provider Network
Management (PNM)
8.1 Provider Training and Education
Provider training and education (goals, objectives,
curricula and implementation guidelines) are
established by L.A. Care based on regulatory
requirements. L.A. Care provides additional annual
and ongoing training and education, as requested by
its network and regulatory agencies.
e goal of provider training and education is to
improve the delivery of services to L.A. Care members
by providing appropriate forums for providers to:
• be better informed about products offered by
L.A. Care, its systems, and processes;
• understand the needs of L.A. Care members;
• improve clinical/patient interaction; and
• comply with regulatory requirements.
Distribution of L.A. Care’s Provider Manuals
Physician Participating Groups (PPG) must make a
L.A. Care provider manual available to its contracted
providers/network within 10 business-days of becoming
active with L.A. Care’s provider network. Educating a
new provider on how to locate the L.A. Care provider
manual on the L.A. Care website will meet the provider
manual distribution regulatory requirement. e
Provider Manual can be located at L.A. Care’s website
at lacare.org or http://www.lacare.org/providers/
provider-resources/provider-manuals.
Communication with Contracted Providers
On-site visits are an integral component of provider
education because all contracted providers must receive
ongoing education. On-site visits consist of, but are
not limited to Joint Operational Meetings (JOMs)
and in-service educational opportunities. ese visits
will focus on policy and program updates as required
by the Department of Health Care Services, (DHCS),
Department of Managed Health Care (DMHC), and
other regulatory agencies. ese meetings are generally
announced, but some visits may be unannounced
if L.A. Care deems them necessary. L.A. Care
understands that, in some instances, on-site educational
opportunities may be limited due to time constraints
resulting from provider offices working diligently to
serve our members. erefore, updated information
may also be shared in written documents, online via
the Provider Portal or Webinars for the convenience of
L.A. Care’s PPGs and their contracted providers.
PPG Responsibility for Contracted
Provider Education
PPGs are responsible for ensuring that all contracted
Primary Care Physicians (PCPs), specialists, and
ancillary providers receive on-going comprehensive
training and education as stipulated in the Participating
Provider Service Agreement (PPGSA) and required
by applicable regulatory bodies. L.A. Care also
requires its contracted network to meet the training
requirements of the National Committee for Quality
Assurance (NCQA).
PPG Publication of Provider Bulletins,
Newsletters and General Meetings
PPGs should publish and distribute provider
newsletters and/or bulletins at least semi-annually.
e newsletters should provide relevant and timely
information concerning applicable standards, services
available to members, quality improvement activities,
updates, and other pertinent issues related to the
delivery of health services to L.A. Care members.
Semi-annual general meetings that provide updates
on health care delivery issues, hosted by PPGs or its
affiliated contracted providers will meet the requirement
to publish semi-annual newsletters/bulletins.
MONITORING AND OVERSIGHT
In order to ensure that PPGs are conducting new
provider orientations and on-going provider education
and training that are compliant with contractual
requirements and regulatory guidelines, L.A. Care will
require PPGs to submit monthly reports. ese reports
must be submitted monthly. L.A. Care may also
conduct quarterly and annual audits of PPG records
including training reports, signed attendance sheets;
and, may sample provider records. L.A. Care will
perform additional oversight of education and training
as appropriate.
Management of Provider Network Panels
L.A. Care Direct Lines of Business and Plan Partners:
Panel Status and Closure Requests:
e requirements for updates to provider panels and
requests for panel closure are as follows:
Physicians:
A physician may request age/gender modifications
to panels provided that the change initiated is
effective for all lines of business, affiliated PPGs, and
contracted health plans.
A physician may request Medi-Cal panel closure
provided that it is applicable to all health plans
affiliated with the contracted PPG.

120
PPGs:
A PPG may request modifications to provider panels
with the stipulation that a minimum of fifteen percent
(15%) of their network will continue to be active and
available for assignment of adult members, and twenty
percent (20%) for children aged 0-21.
L.A. Care Direct Lines of Business and Plan
Partners: Provider Panel Availability
L.A. Care and the Plan Partners must also maintain a
minimum of fifteen percent (15%) panel availability
for the assignment of adult membership and twenty
percent (20%) for children aged 0-21. Additionally,
Plan Partners’ provider networks must provide
healthcare services in all L.A. Care approved zip codes.
L.A. Care retains the authority to close panels as
deemed appropriate or necessary.
Non-compliance with Panel Availability Requirements
If a request for panel modification causes non-compliance
with availability requirements, the provider’s affiliated
PPGs will be informed of this. Corrective Action
Plans to address non-compliance may be requested or
required of the PPG and/or Plan Partner. Failure to
comply will result in panel closure.
8.2 Provider Directories
L.A. Care’s Medi-Cal Provider Directory (Directory) is
updated regularly. Data for the Directory is compiled
by L.A. Care from PPG provider information. PPGs
must submit accurate and timely provider data
through the appropriate established process in order
to ensure complete and updated in-network provider
information is available to members and prospective
beneficiaries. e provider directory includes a listing
of PPGs, PCPs, hospitals, pharmacies and other
network providers. Updated provider directories
are located on the L.A. Care website at lacare.org.
Directories are also available to providers in hardcopy
upon request.
8.3 Primary Care and Mid-Level Medical
Practitioner Capacity
PCPs, including practitioners of general medicine,
family practice, internal medicine, obstetrics and
gynecology (OB/GYN) and pediatrics, are allowed a
maximum membership capacity of 2,000 members
when there is no non-physician practitioner (mid-level
extender) support. A single non-physician practitioner
can potentially increase the supervising PCP’s total
membership capacity by 1,000 members. However, the
PCP cannot be assigned more than 5,000 L.A. Care
members, including membership assigned across any
product line, Plan Partner, or PPG contract within
L.A. Care’s network. Please note that physician panels
are closed at 95% of capacity.
Number
of PCP
Number of
Mid-Level
Extenders
Maximum
Membership
Capacity
1 PCP No Extenders 2,000
1 PCP 1 Extender 3,000
1 PCP 2 Extenders 4,000
1 PCP 3 Extenders 5,000
1 PCP 4 Extenders 5,000
A Scope of Practice Agreement that is signed by
the non-physician practitioner and the supervising
physician, as well as standardized procedures, must
be filed and maintained at the medical practice site.
e Scope of Practice Agreement must address the
following elements:
• Delegated responsibilities
• Disciplinary policies
• Method and frequency of physician supervision
• Monitoring and evaluation of the
non-physician practitioner
• Chart review requirements
• Term of the agreement/contract
8.4 PNM Provider Relations
Contact Information
Please call L.A. Care’s Provider Services line at
1.866.522.2736 or your assigned Provider Relations
Account representative if you have any questions
or concerns. PCPs, specialists and ancillary
providers contracted with L.A. Care’s PPGs should
communicate their questions directly to their
contracted PPG. Providers directly contracted with
L.A. Care may communicate with L.A. Care by
telephone, in writing, or by e-mail.
Telephone: 1.866.522.2736
In Writing: L.A. Care Health Plan
Attention: Provider Relations
1055 W. 7
th
Street, 10
th
Floor
Los Angeles, CA. 90017
E-mail: ProviderRelations@lacare.org or e-mail
your Provider Relations representative
121
8.5 Provider Appeals and Grievances
Provider clinical grievances will be handled
through L.A. Care’s Utilization Management process.
Provider administrative grievances will be handled as
specified below.
Providers Contracted with PPGs:
• Providers must communicate their grievances
directly to their contracted PPG. is
communication must be in writing.
• e PPG will be responsible for resolving the grievance
within 30 calendar days and communicating to the
provider the resolution/disposition.
°
PPG representative will give the provider detailed
instructions for filing a grievance.
°
PPG representative will record the grievance
on the provider grievance log. Regardless of the
method of filing of the provider’s grievance, PPG
will send an acknowledgment letter to the provider
within 5 business days
• If a provider contacted the PPG regarding a
grievance and challenge the resolution provided by
the PPG, then the provider may contact L.A. Care
directly and submit a grievance against the PPG, to
the contacts listed above.
°
e provider must submit a detailed written
grievance, including the desired resolution and all
supporting documentation and correspondence to
Provider Relations. L.A. Care will respond with an
acknowledgement letter within five (5) business days.
°
Provider Relations will inform the PPG of the
grievance to provide response to L.A. Care within
5 business days.
°
Provider Relations will be responsible for
informing the provider of the resolution/
disposition in this case.
L.A. Care Directly Contracted Providers:
• Providers directly contracted with L.A. Care must
communicate their administrative grievance with
L.A. Care by telephone or in writing, to the contacts
listed above.
• Provider Network Management will be coordinate
grievance resolution within 30 calendar days. e
provider will receive the resolution/disposition
in writing.
°
e provider grievance will be recorded on the
provider grievance log; regardless of the method of
filing of the provider’s grievance
°
Acknowledgement of receipt of grievance will be
issued within five (5) business days
122
9.0 Health Education
9.1 Health Education Services
L.A. Care’s Health Education Unit supports network
providers in point-of-service patient education by
offering Health Education services, resources, and
programs at no cost to L.A. Care network providers or
Direct Line of Business members.
9.1.1 Health Education Services – e Health In
Motion™ Program
L.A. Care’s Health In Motion™ program offers an
array of skills-based, interactive wellness workshops
and group appointments in various locations
throughout Los Angeles County. To access a calendar
of upcoming events, visit: www.lacare.org/healthy-
living/health-resources/workshops-and-classes.
L.A. Care’s Registered Dietitians and Certified Health
Coaches assist Members unable to attend in-person
workshop in managing their conditions and health
status via telephonic consultations. Topics of expertise
include the following:
• Medical Nutrition erapy
• Diabetes Self-Management Education
• Weight management
• Support for managing chronic conditions, including
hypertension and asthma
• Smoking cessation
• Senior health topics such as fall prevention and
osteoporosis, among others.
To refer a patient for Health Education services,
complete and fax the referral form located on
L.A. Care’s website at: www.lacare.org/providers/
provider-resources/health-education-tools.
L.A. Care members may also access wellness tools and
resources 24/7 in the comfort of their own home by
visiting L.A. Care’s on-line wellness site: My Health
In Motion™. To access the site, members may go to
www.lacare.org, and register into the member portal.
To initiate registration, click on “Member Sign-In.”
Once the member is registered and has logged into
the member portal, the member may click on the “My
Health In Motion” tab.
9.1.2 Health Education Resources – Free Materials
for Your Patients
L.A. Care makes available free hard copy health
education materials in multiple topics and languages
for L.A. Care providers. Health education topics
include: asthma, breastfeeding, dental, diabetes, exercise,
family planning, HIV/STD prevention, hypertension,
immunizations, injury prevention, nutrition, parenting,
perinatal/pregnancy, substance abuse, tobacco
prevention/cessation, and weight management and more.
Providers may order hard-copy L.A. Care health
education materials at no cost to them through the
online health education material order form located
at: www.lacare.org/providers/provider-resources/
health-education-tools. Written Health Education
materials provided by L.A. Care comply with the
guidelines set forth by DHCS.
9.1.3 Staying Healthy Assessments
PCPs are responsible for ensuring the use of the
Individual Health Education Behavioral Assessment
(also called “IHEBA” or “Staying Healthy.”) e
assessment tool sponsored and approved by DHCS is
called the Staying Healthy Assessment (SHA).
PCPs must administer the SHA to all new L.A. Care
members within 120 days of enrollment as part of
the Initial Health Assessment. Current members who
have not completed an updated SHA must complete
it during the next preventive care office visit (e.g.
well-baby, well-child, well-woman exam). Pediatric
Members 0–17 years of age must complete the SHA
during the first scheduled preventive care office visit
upon reaching a new SHA age group.
e SHA must be re-administered to adults
and seniors every three to five years. Annual
administration is encouraged for 12-17 years and
seniors due to rapidly changing risk factors.
e SHA must be reviewed annually for all age groups
in the interval years between administrations.
L.A. Care offers training on completing Staying Healthy
Assessment via an on-line recorded presentation on
the L.A. Care website at: www.lacare.org/providers/
provider-resources/staying-healthy-forms
PCPs may download Staying Healthy forms in
writable PDF at: www.lacare.org/providers/provider-
resources/staying-healthy-forms or order hard
copies by accessing the Health Education Materials
order form at: www.lacare.org/providers/provider-
resources/health-education-tools. Additional tools
and resources such as health education materials in
multiple languages are also available to order online.
Please contact [email protected] with any
questions related to completing the SHA.
123
9.2 L.A. Care Family Resource Centers
L.A. Care operates four Family Resource Centers
(FRC’s) located throughout Los Angeles County:
Lynwood, Inglewood, Boyle Heights and Pacoima. e
FRC’s partner with community based organizations in
offering free health education and fitness classes open to
all community members. New Member Orientations,
health screenings, and application and enrollment
assistance are also available. For more information about
the Family Resource Centers please visit our website at
www.lacare.org/frc.
9.3 Nurse Advice Line
L.A. Care offers a nurse advice line 24/7, including
holidays. Members can call 1.800.249.3619
(TTY 711) to get answers to their common health care
related questions.
9.4 Health Education Programs
L.A. Care’s Health Education Programs are a combination
of coordinated and systematic health education services,
resources, and Member outreach designed to target a
specific health problem or population. Eligible Members
are identified for participation in these programs based
on specific inclusion criteria for each program. e
programs are available at no cost to Members:.
• “Healthy Mom” Program – L.A. Care identifies
new mothers via hospital discharge and
authorization data. We conduct phone outreach to
educate them on the importance of the postpartum
visit and assist with scheduling an appointment with
their obstetrician. L.A. Care offers interpreting and
transportation services and provides Members with a
gift card upon confirmation of visit attendance.
• “Smoke Free” Program – Adult L.A. Care Health Plan
Members who have filled prescriptions for smoking
cessation medication (nicotine gum, patch, lozenge,
Buproprion, Varenicline) receive health education
materials promoting available smoking cessation
resources, including “You Can Quit Smoking–Support
and Advice from L.A. Care Health Plan” and a
listing of free local smoking cessation resources.
• “Fight the Flu” Program – L.A. Care uses a
coordinated series of communication methods to
encourage Members to obtain a flu shot. Outreach
efforts include: self-mailing educational postcards
with promotional items, automated phone calls with
messages targeted to the audience, and thank-you
cards with an incentive, which also helps Members
remember they received a flu shot.
9.5 Provider Education
e content of Provider education includes, but is not
limited to, the following:
• Communication to providers of both applicable
regulatory agencies’ and L.A. Care Health Plan’s
health education requirements;
• e availability of health education services
and resources;
• e availability of health education materials and the
process for obtaining materials;
• e inclusion of health education material
requirements; including qualified health educator
oversight, reading level, field testing (if applicable),
medical accuracy, availability of materials in
alternative formats, and cultural/linguistic
appropriateness; and
• Establishing a Staying Healthy Assessment
(SHA) requirement.
L.A. Care’s PPGs are responsible for educating their
network providers on health education requirements
and available L.A. Care health education services
as listed above. Methods may include, but are
not limited to: provider mailings and newsletters;
meetings, seminars or other trainings; onsite visits;
blast-faxes; informing network providers of the
content of this Provider Manual; informing network
providers of the content of applicable policies and
procedures; and website postings.
124
10.0 Cultural and
Linguistic Services
e relationship among culture, language, and health
is complex and inextricably linked to the health status
of individuals and, subsequently, their communities.
Cultural competence and linguistic competence are
widely recognized as fundamental aspects of equity
and quality in health care and mental health care—
particularly for diverse patient populations—and
as essential strategies for reducing disparities by
improving access, utilization and quality of care.
e goals of the L.A. Care Cultural and Linguistic
(C&L) program are the following:
• Ensure that limited English proficient (LEP)
Members receive the same scope and quality of
health care services that other members receive
• Ensure the availability and accessibility of cultural
and linguistic services including quality interpreting
services and written materials in the Members’
preferred languages and in a manner and format that
is easily understood
• Improve health outcomes and decrease disparities
• Continually evaluate and improve C&L programs
and services
C&L services include the following:
• Language proficiency assessment of bilingual
Providers and staff
• Language assistance services that include the
following:
°
Interpreting services
°
Translation services
°
Alternative format conversion
• Cultural and linguistic trainings for Providers and staff
10.1 Assessing Bilingual
Language Prociency
10.1.1 All L.A. Care Providers (PPGs, Network
Providers, Specialty Plans, Vendors, Hospitals,
LTSS providers):
L.A. Care Providers and staff who communicate
directly with L.A. Care Members in a language
other than English at medical and non-medical
points of contact must be assessed and qualified for
their language capabilities (Refer to Sections 10.2
Interpreting Services and 10.3 Translation Services
and Alternative Formats for definitions of qualified
interpreters and translators).
L.A. Care bilingual Providers and staff, who are not
formally assessed and qualified, should use qualified
interpreting services to better serve Members as well as to
minimize the risk of liability and malpractice lawsuits.
At a minimum, assessing the language proficiency of
L.A. Care contracted bilingual Providers and staff must
be completed by using the Industry Collaboration
Effort (ICE) Employee Language Skills Assessment
Tool. However, more robust assessment by a professional
language assessment vendor is strongly encouraged.
e evidence of the language proficiency assessment of
L.A. Care contracted bilingual Providers and staff must
be kept on file, including the following information:
• Name
• Title/Position
• Department
• Spoken and written language
• Proficiency level for spoken and written language (ICE
Employee Language Skills Assessment Tool results or
any other language proficiency assessment results)
AND one or more of the following (if any):
• Number of years of employment the individual has
as an interpreter (e.g., resume)
• Certification of medical interpreters (e.g., National
Board of Certification for Medical Interpreters,
Certification Commission for Healthcare
Interpreters)
• Documentation of successful completion of
education and training in interpreting ethics,
conduct and confidentiality that are promulgated by
the California Healthcare Interpreters Association or
the National Council on Interpreting in Healthcare
• Other reasonable alternative documentation of
interpreter capability
is information must be updated annually for
L.A. Care contracted Providers and staff.
10.2 Interpreting Services
L.A. Care Members must be provided with qualified
interpreting services, including American Sign
Language (ASL), at no cost to them. Interpreting
services must be available 24/7 at medical and non-
medical points of contact. Languages for interpreting
services should not be limited to the threshold
languages. Effective communication through qualified
interpreters improves quality of care, increases
Member satisfaction, and minimizes the risk of
liability and malpractice lawsuits.
125
Qualified interpreters must have:
• Documentation of demonstrated spoken language
proficiency in both English and the other language
• A fundamental knowledge in both languages of
health care terminology and concepts relevant to
health care delivery systems
• Documentation of successful completion of
education and training in interpreting ethics,
conduct and confidentiality that align with the
California Healthcare Interpreters Association or the
National Council on Interpreting in Healthcare or
its equivalent
AND one or more of the following:
• Documentation of the number of years of
employment the individual has as an interpreter
(e.g., resume)
• Certification of medical interpreters (e.g., National
Board of Certification for Medical Interpreters,
Certification Commission for Healthcare Interpreters)
• Other reasonable alternative documentation of
interpreter capability
10.2.1 All L.A. Care Providers (PPGs, Network
Providers, Specialty Plans, Vendors, Hospitals,
LTSS providers):
All L.A. Care network Providers must:
• Offer no-cost qualified interpreting services
to Members.
• Not require, suggest to, or imply to Members that
they provide their own interpreter.
• Strongly discourage use of friends and family
members, especially minors, as interpreters except
in extraordinary circumstances such as medical
emergencies. A Member may choose to use a family
Member or friend as an interpreter only after
they are informed of the right to no-cost qualified
interpreting services.
• Document a Member’s preferred language in the
medical chart.
• Document a Member’s request or refusal of no-cost
qualified interpreting services and request to use
a family member or friend as an interpreter in the
medical chart.
• Post translated signage at key points of contact
regarding the availability of no-cost language services
and how to access the services.
10.2.2 Face-to-Face Interpreting Services for
L.A. Care Members
Face-to-face interpreting services should be used for
L.A. Care Members medical encounters or to discuss
complex matters because it is the most effective and
preferred mode of interpreting services.
10.2.2.1 L.A. Care PPGs and Network Providers:
L.A. Care offers no-cost face-to-face interpreting
services to contracted PPGs and Network Providers.
To request a face-to-face medical interpreter (including
ASL), call L.A. Care’s Member Services Department at
1.888.839.9909 at least 10 business days prior to the
L.A. Care member medical appointment.
Both L.A. Care Members and Network Providers can
request face-to-face interpreting services for confirmed
Members medical appointments.
e following information is needed:
• Member Information
°
Name
°
L.A. Care ID number
°
Date of birth
°
Language being requested
°
Requested preferred gender of interpreter
• Appointment Information
• Provider’s name
• Provider’s specialty
• Requestor’s name and phone number
• Contact person’s name at appointment site and
phone number (if different from requestor)
• Date and time of appointment
• Duration of appointment
• Address of appointment (including facility name
and suite number)
°
Purpose of appointment
°
Other special instructions, as applicable
If the appointment date, time or location is changed,
call L.A. Care’s Member Services Department at
1.888.839.9909 immediately.
10.2.2.2 L.A. Care Specialty Plans, Vendors,
Hospitals, and LTSS providers:
L.A. Care delegates interpreting services to Specialty
Plans, Vendors, Hospitals, and LTSS providers. Please
contact the appropriate personnel at your organization
or facility to learn more information on how to
access face-to-face interpreting services through these
delegated entities.
126
10.2.3 Telephonic Interpreting Services
Telephonic interpreting services should be used to set
up appointments or communicate simple matters, or
as a backup to face-to-face interpreting services.
10.2.3.1 L.A. Care PPGs and Network Providers:
L.A. Care offers no-cost telephonic interpreting
services to contracted PPGs and Network Providers.
To access L.A. Care’s telephonic interpreting services,
call one of the following numbers:
PPGs may contact L.A. Care’s vendor, Language Select
at: 1.888.718.4366
Network Providers may contact L.A. Care’s vendor,
Language Select at: 1.888.930.3031
e following information is needed:
• Name of PPG or Medical Board License Number
(Network Providers only)
• Member’s L.A. Care ID number
• Language being requested
10.2.3.2 L.A. Care Specialty Plans, Vendors,
Hospitals, and LTSS providers:
L.A. Care delegates interpreting services to Specialty
Plans, Vendors, Hospitals, and LTSS providers. Please
contact the appropriate personnel at your organization
or facility to learn more information on how to
access telephonic interpreting services through these
delegated entities.
10.2.4 California Relay Service – 711
California Relay Service (CRS) can be used to
communicate with deaf and hard of hearing Members.
CRS is a no-cost, 24/7 relay service which helps a
person using a TTY/TDD to communicate by phone
with a person who does not use a TTY/TDD. CRS
can also help a non-TTY/TDD user call a TTY/TDD
user. Trained relay operators are online to relay the
conversation as it takes place.
10.2.4.1 All L.A. Care Providers (PPGs, Network
Providers, Specialty Plans, Vendors, Hospitals,
LTSS providers):
To communicate with deaf or hard of hearing
L.A. Care Members over the phone, call CRS at 711.
e following information is needed:
• Member’s name
• Member’s phone number
10.3 Translation Services and
Alternative Formats
According to regulatory timelines, L.A. Care Members
should receive written “Member Informing Materials”
in a Member’s preferred threshold language on a
routine basis and in a preferred alternative format
(e.g., large print, audio) upon request.
Translation can be completed by a translation services
vendor or qualified internal bilingual staff as long as
the following requirements are met:
• Translations must meet the following specifications:
°
A complete accurate meaning-for-meaning
rendition of the source text (English) in the target
language(s)
°
At the 6th grade reading level (calculated by
Readability software, including but not limited to
SMOG, Fry Graph, FOG, Flesch Reading Ease,
and Dale-Chall)
°
Culturally appropriate and relevant to L.A. Care’s
Member population
• Translation process must include the following at
a minimum:
°
ree-step process including translation, editing,
and proofreading
°
Completion of this three-step process by at least
two separate qualified translators
• Qualified translators must meet the following criteria:
°
Documentation of demonstrated written language
proficiency in both English and the other language
°
Formal education in the target language
°
Ability to read, write and understand the
target language
°
Ability to read and understand the source language
°
Knowledge and experience with culture(s) of the
intended audience
°
A fundamental knowledge of health care terminology
and concepts relevant to health care delivery systems
in both the source and target languages
• Written Member Informing Materials must be
available in all Los Angeles County reshold
Languages. Following are the 11 threshold
languages for:
°
English
°
Spanish
°
Arabic
°
Armenian
°
Chinese
°
Farsi
°
Khmer
°
Korean
°
Russian
°
Tagalog
°
Vietnamese
127
e documents that must be kept on file for translated
Member Informing Materials include the following:
• e source document (English).
• e translated document.
• A signed attestation for each translated document in
each translated language from the translation services
vendor or bilingual staff who performed translation.
It should attest to the accuracy and completeness
of the translation using the three-step process by at
least two separate qualified translators.
Member Informing Materials that are sent in English
or are not fully translated (e.g., if member-specific
information in Notice of Action letters remains in
English) must include a translated written notice
informing members of the availability of no-cost
translation and interpreting services and how to access
these services. is notice should be available in all
threshold languages.
10.3.1 L.A. Care PPGs:
L.A. Care PPGs are delegated to translate the Member
Informing Materials (e.g., appointment reminders,
flyers and consent forms) that they have developed.
PPGs are responsible for translating these materials
into threshold languages and distributing them to
Members in the appropriate threshold languages on a
routine basis and in alternative formats upon request.
L.A. Care provides PPGs with translated Notice
of Action (NOA) letter templates in all threshold
languages. PPGs are responsible for sending NOA
letters to Members. However, PPGs are responsible for
translating the member-specific information within
these NOA letter templates.
10.3.2 L.A. Care Network Providers:
Please contact the appropriate personnel at your PPG
to learn more information on how to access materials
in threshold languages and alternative formats.
10.3.3 L.A. Care Specialty Plans, Vendors,
Hospitals, and LTSS providers:
L.A. Care delegates translation services and
alternative formats to Specialty Plans, Vendors,
Hospitals, and LTSS. Please contact the appropriate
personnel at your organization or facility to learn
more information on how to materials in threshold
languages and alternative formats.
10.4 Cultural and Linguistic
Service Trainings
Training on C&L requirements, cultural competency,
and disability sensitivity is required for all network
Providers. Training must be delivered to staff and
Providers serving Members at both medical and non-
medical key points of contact. ese trainings must be
completed initially and on an annual basis.
10.4.1 L.A. Care PPGs and Network Providers:
L.A. Care offers the following trainings to PPGs and
Network Providers. e trainings are available at no
cost either as instructor–led classroom trainings or via
an online learning system:
• Cultural Competency (including C&L requirements)
• Disability Awareness
• Communicating rough Healthcare Interpreters
(CME – available only for Network Physicians)
To schedule classroom training sessions or access the
online CME course, e-mail CLStrainings@lacare.org.
PPGs are delegated to inform its staff and Network
Providers of the availability of the L.A. Care’s C&L
trainings, services, and resources, as well as how to access
the trainings. PPGs can distribute this information via
multiple methods, such as the following:
• For Staff: Staff orientations, in-service trainings,
meetings, staff newsletters and e-mail
• For Network Providers: Provider orientations, in-
service trainings, meetings, Provider newsletters,
faxes and mailings
10.4.2 L.A. Care Specialty Plans, Vendors,
Hospitals, and LTSS providers:
L.A. Care delegates the provision of C&L education
and training to Specialty Plans, Vendors, Hospitals,
and LTSS providers. Contracted Providers and staff
must be trained on the following content:
• Legal obligations under state and federal laws
regarding language access services
• Resources and services available to help comply with
those obligations
• C&L Requirements, including the following:
°
Posting of the interpreter poster at Provider
office sites
°
Availability of no-cost qualified interpreting
services, including ASL, at all points of contact
24/7, including after-hours services and how to
access the services
128
°
Discouraging the use of family and friends,
especially minors, as interpreters.
°
Documenting a Member’s preferred language
°
Documenting a Member’s request and refusal of
interpreting services
°
Identifying, assessing and tracking the linguistic
capability of bilingual clinical and non-clinical staff
°
Processes for filing a grievance if a Member’s
cultural or language needs are not met
°
Working effectively with Members who use in-
person and telephonic interpreters
°
Availability of written Member Informing
Materials in threshold languages and alternative
formats and how to access the services
°
Availability and use of TTY/TDD
• Cultural competency, including the following:
°
Unbiased attitude and respect for cultural diversity
°
Respect for the multifaceted nature and
individuality of people
°
Awareness that culture and cultural beliefs may
influence health and health care delivery
°
Knowledge about diverse attitudes, beliefs,
behaviors, practices, and methods regarding
preventive health, illnesses, diseases, traditional
home remedies, and interaction with Providers and
health care system.
°
Skills to communicate effectively with
diverse populations
°
Language and literacy needs
• Disability sensitivity
Documentation of all provided trainings must be kept
on file including, but not limited to, sign-in sheets and
training evaluation.
10.5 Cultural and Linguistic
Tools and Resources
Tools and resources are available to assist all Providers
in delivering culturally and linguistically appropriate care.
10.5.1 L.A. Care PPGs and Network Providers:
L.A. Care offers the following C&L tools and
resources to assist PPGs and Network Providers in
delivering culturally and linguistically appropriate care.
10.5.1.1 Provider Toolkit for Serving
Diverse Populations
e Provider toolkit is a comprehensive guide to
culturally and linguistically appropriate services. It is
organized in five sections, which contain helpful C&L
information and tools.
To order the toolkits, go to https://external.lacare.org/
HealtheForm/.
To download the toolkits (PDF), go to www.lacare.
org/Providers/Provider-resources/Provider-tool-kits.
10.5.1.2 Language Skills Assessment Tool
e ICE Employee Language Skills Assessment Tool
can be used to document language proficiency of
bilingual Providers and staff.
To download the assessment tool (PDF), go to
http://www.lacare.org/Providers/Provider-
resources/Provider-forms.
10.5.1.3 Interpreting Services Poster
e poster is translated into 14 languages. It informs
the availability of no-cost interpreting services and
how to access the services from L.A. Care. It should be
posted at all key points of contact such as front office
and exam rooms.
To order the posters, go to
https://external.lacare.org/HealtheForm/.
10.5.1.4 Telephonic Interpreting Card
e card has the number for L.A. Care’s no-cost
telephonic interpreting services and information
needed to place interpreted calls.
To order the telephonic cards, go to
https://external.lacare.org/HealtheForm/.
10.5.1.5 Culturally and Linguistically
Appropriate Referrals
PPGs and Network Providers can refer Members to
culturally and linguistically appropriate community
services by using the online community directory,
Healthy City or L.A. Care’s referral form.
To access the online resource directory, go to
http://www.healthycity.org/.
To download the referral forms, go to www.lacare.org/
Providers/Provider-resources/health-education-tools.
10.5.1.6 Patient Interpreter Services Labels
e labels can be used to document a Member’s
spoken and written languages as well as request and
refusal of interpreting services.
To download the labels (Word), go to www.lacare.org/
Providers/Provider-resources/Provider-forms.

129
10.5.2 L.A. Care Specialty Plans, Vendors,
Hospitals, and LTSS providers:
Please contact the appropriate personnel at your
organization or facility to learn more information
about available C&L tools and resources and how to
access them.
10.6 Reporting Requirements
As part of L.A. Care’s monitoring process, regular
reports must be submitted via e-mail to CLReports@
lacare.org. Reports must be provided using either
L.A. Care’s reporting templates or L.A. Care’s format
requirements. For the most up-to-date reporting
templates or format information, please e-mail
CLStrainings@lacare.org.
10.6.1 L.A. Care PPGs:
PPGs must submit the following reports according to
the following schedule:
Annual Report
Due
Date
Quarterly Report
Dates of Service
Due
Date
January
31
Qtr. 1
January
–
March
May 15
Qtr. 2
April
–
June
August 15
Qtr. 3
July
–
September
November 15
Qtr. 4
October
–
December
February 15
1. Annual Bilingual Staff List
2. Quarterly Translated Document Report for the
reporting period
3. Quarterly Face-to-Face Interpreting Utilization
Report* for the reporting period
4. Quarterly Telephonic Interpreting Utilization
Report* for the reporting period.
*Face-to-Face and Telephonic Interpreting Utilization
Reports are required only if a PPG uses its own interpreting
services instead of the services offered by L.A. Care.
10.6.2 L.A. Care Specialty Plans and Vendors:
Specialty Plans and Vendors must submit the following
reports according to the schedule listed below:
Annual Report
Due
Date
Quarterly Report
Dates of Service
Due
Date
January
31
Qtr. 1
January
–
March
May 15
Qtr. 2
April
–
June
August 15
Qtr. 3
July
–
September
November 15
Qtr. 4
October
–
December
February 15
1. Annual Bilingual Staff List
2. Quarterly Translated Document Report for the
reporting period
3. Quarterly Face-to-face Interpreting Utilization
Report for the reporting period
4. Quarterly Telephonic Interpreting Utilization
Report for the reporting period
5. Quarterly C&L Referral Report for the reporting
period (Behavioral health plans only)
130
11.0 Finance
11.1 Capitation Payments
L.A. Care, under contractual agreement, pays PPGs a
pre-determined capitation each month for the provision
of health services to L.A. Care Medi-Cal Members.
is section covers guidelines for financial reports and
requirements, capitation, and other related issues.
11.1.1 100% of capitation payments will be remitted
to a PPG no later than the 10th calendar day of
a month (except as defined in “Financial Security
Requirements,” and “Assumption of Financial Risk”).
e payments will constitute payment in full for health
care and administration services rendered under the
PPG’s L.A. Care PPG Services Agreement (PPGSA).
11.1.2 For further information regarding PPG
compensation, please refer to the Capitation Schedule
of the L.A. Care Physician Capitated Services Agreement.
11.2 Capitation Statement Report
11.2.1 A Capitation Statement Report will be placed in
a protected PPG website on or before the 10th business
day of every month. e Capitation Statement Report
will provide a summary of the capitation payment for
each enrolled Member assigned to each PPG, and will
include the following information:
• Number of current active enrollees (initial eligibles)
• Number of retroactive disenrollments (decaps) –
representing the number of retroactive disenrollment
months processed
• Capitation amount
• Capitation total
11.2.2 e Capitation Statement Report is also
used to create the Group Capitation Payment
Summary Report.
11.3 Insurance
Each PPG is responsible for the total costs, except as
described here, of care rendered to Members enrolled
with that PPG under the terms of its L.A. Care
PPGSA. Each PPG must maintain adequate insurance
as follows:
11.3.1 Professional Liability Insurance
A PPG must have and maintain, at its expense
throughout the term of its PPGSA, Professional
Liability Insurance for each employed physician.
Limits must not be less than $1,000,000.00 per
occurrence and $3,000,000.00 in the aggregate for
the year of coverage, or another amount acceptable
and permitted by L.A. Care in writing. PPGs must
provide copies of insurance policies within 5 business
days of a written request by L.A. Care.
11.3.2 Federal Tort Claims Act Alternative
In lieu of providing Professional Liability Insurance
described above, a PPG may provide L.A. Care with
evidence of liability protection under the Federal Tort
Claims Act by the Bureau of Primary Health Care in
accordance with Section 224(h) of the Public Health
Service Act, 42 U.S.C. 233(h), as amended (“FTCA
Coverage”). However, a PPG must ensure that only
those Providers covered under the Professional Liability
Insurance described above or under FTCA Coverage
may provide Provider services to L.A. Care Members.
11.3.3 Reinsurance/Stop-Loss Insurance
A PPG must maintain adequate stop-loss insurance to
cover its catastrophic cases in an amount reasonably
acceptable to L.A. Care, but in no event less than
$30,000.00 plus 50% of any medically necessary
billed charges. e cost of a PPG’s reinsurance/stop-
loss coverage is the PPG’s sole financial responsibility.
11.3.4 General Liability Insurance
A PPG must maintain general liability insurance in at
least the minimum amounts acceptable to L.A. Care
to cover any property loss that is not covered under
any lease agreement with the landlord or contract
agreement with the management company. e limits
of liability must not be less than $100,000.00 for
each claim and $300,000.00 in aggregate under each
insurance policy period.
11.3.5 Errors and Omissions
A PPG must maintain Errors and Omissions (E&O)
Insurance that covers the claims made against managed
care activities. e insurance policy must be written
on a claim made basis. e limits of liability must not
be less than $100,000 for each claim and $100,000 in
aggregate for each insurance policy period.
11.3.6 Directors and Officers
A PPG must maintain Directors and Officers (D&O)
Insurance that covers claims made against directors and
officers of the company. e insurance policy must be
written on a claim made basis. e limits of liability
must not be less than $100,000 for each claim and
$100,000 in aggregate for each insurance policy period.
131
11.3.7 Independent Certified Public Accounting
Firm Liability Insurance
A PPG must ensure that all independent certified
public accounting firms conducting audits on the
PPG’s financial statements maintain at its expense
throughout the term of its PPGSA, liability insurance
with limits of not less than $250,000.00 in aggregate
for the year of coverage or another amount acceptable
to and permitted by L.A. Care in writing.
A PPG must provide copies of these insurance policies
within 5 business days of a written request by L.A. Care.
11.4 Minimum Financial
Solvency Standards
11.4.1 Each PPG must maintain adequate financial
resources to meet its obligations as they become due.
PPGs contracted with L.A. Care must be solvent at
all times, and must maintain the following minimum
financial solvency standards:
11.4.1.1 Prepare quarterly financial statements in
accordance with Generally Accepted Accounting
Principles (GAAP). ese financial statements must
include, but are not limited to, a Balance Sheet, a
Statement of Income, and a Statement of Cash Flow.
ese financial statements must be submitted to the
Financial Compliance Department of L.A. Care no
later than 45 calendar days after the close of each
quarter of the fiscal year.
11.4.1.2 Reimburse, contest, or deny at least ninety
percent (90%) of all claims within thirty (30) calendar
days, ninety-five percent (95%) within forty-five
(45) working days, and ninety-nine percent (99%)
of all clean claims within ninety (90) calendar days
or in accordance with applicable law, regulation and
contractual timeliness requirements.
11.4.1.3 Estimate and document, on a monthly
basis, the PPG’s liability for incurred but not reported
(IBNR) claims using a lag study, an actuarial estimate,
or other reasonable method as stipulated by Title 28,
California Code of Regulations, Section 1300.77.2.
11.4.1.4 Maintain, at all times, a positive working
capital (current assets net of related party receivables
less current liabilities).
11.4.1.5 Maintain, at all times, a positive Tangible
Net Equity (TNE) as defined in Title 28, California
Code of Regulations, Section 1300.76(e).
11.4.1.6 Maintain, at all times, the current minimum
“cash to claims ratio” of .75.
A cash to claims ratio is cash, readily available
marketable securities and receivables (excluding all
risk pool, risk-sharing, incentive payment program,
and pay-for-performance receivables reasonably
anticipated to be collected within 60 days) divided
by the organization’s unpaid claims (claims payable
and IBNR claims) liability (as listed per SB 260 and
Title 28, California Code of Regulations, Section
1300.75.4.2).
11.4.1.7 On an annual basis, submit financial
statements, including but not limited to a Balance
Sheet, a Statement of Income, and a Statement of
Cash Flow audited by an independent Certified Public
Accounting Firm within 150 calendar days after
the close of the fiscal year to L.A. Care’s Financial
Compliance Department.
11.4.2 Each PPG must actively monitor its affiliated
network of Providers to measure their financial
stability. Copies of all reports, including findings,
recommendations, corrective action plans, and other
information regarding these reviews must be provided
to L.A. Care upon request.
11.4.3 On a discretionary basis, L.A. Care’s Financial
Compliance Department has the right to periodically
schedule audits to ensure compliance with any
of the following: the above requirements, CMS
requirements, and all regulations per SB 260 Title 28
and the California Code of Regulations. Since the
financial solvency standards apply to the PPG entity
as a whole, these audits will be conducted for all of the
PPG’s books of business, not just for those contracted
with L.A. Care. PPG Representatives must facilitate
access to the records necessary to complete the audit.
11.5 Reimbursement Services and Reports
11.5.1 In accordance with the provisions of PPG’s
subcontracts, the PPG will provide all normal
reimbursement services, including those relating to
the payment of capitation, processing and payment of
any claims on a fee-for-service basis, administration
of any stop-loss and risk-sharing programs, and any
other payment mechanisms. Claims processing may
be delegated to PPGs (and is stated as such in the
PPGSA) in cases where UM is delegated.
132
11.5.1.1 PPGs that are delegated for the claims
processing function must submit a monthly claims
timeliness report (in an ICE approved Medicare
template) and a respective supporting claims data file
to L.A. Care by the 15
th
calendar day of each month
following the month being reported.
11.5.2 Upon request, the PPG must provide to
L.A. Care a copy of payment records, summaries, and
reconciliations with respect to L.A. Care Members.
e PPG must also provide any other payment
compensation reports that it customarily provides to
its Providers.
11.6 Records, Reports, and Inspection
11.6.1 Records
Each PPG will maintain all books, records, and other
pertinent information that may be necessary to ensure
the PPG’s compliance with its L.A. Care Services
Agreement, and the requirements of regulatory
agencies which included the DMHC, for a period of
five (5) years from the end of the fiscal period in which
its Services Agreement with L.A. Care terminates.
ese books, records, and other information must
be maintained in accordance with generally accepted
accounting principles, applicable state law and
regulations, DHCS and DMHC requirements.
ese books and records will include, without
limitation, all physical records originated or prepared
under the performance of a PPG contract including,
but not limited to:
• Working papers
• All reports submitted to DMHC
• Financial records
• All books of account
• Encounter data
• All medical records
• Hospital discharge summaries
• Medical charts and prescription files
• Any other documentation pertaining to medical and
non-medical services rendered to Members
• Records of Emergency Services and other
information as reasonably requested by L.A. Care
and DMHC to disclose the quality, appropriateness,
and/or timeliness of health care services provided
to Members under the PPG’s Physician Capitated
Services Agreement
• PPG subcontracts
• Reports from other contracted and
non-contracted Providers
11.6.2 Any reports deemed necessary by L.A. Care,
DHCS, and DMHC to ensure compliance by L.A. Care
with the regulatory requirements must also be maintained.
11.6.3 Each PPG must maintain all books and
records necessary to disclose how the PPG is fulfilling
and discharging its obligations under its PPGSA, and
the PPG’s responsibilities as defined by DHCS and
DMHC. ese books and records will be maintained
to disclose all the following:
• Quantity of covered services provided
• Quality of those services
• Method and amount of payment made for
those services
• Persons eligible to receive covered services
• Method in which the PPG administered its
daily business
• Cost of administering its daily business
11.6.4 Inspection of Records
At any time during normal business hours, PPGs
must allow L.A. Care, DMHC, DHCS, and any other
authorized federal and state agencies (as well as their
designees) to collect, inspect, evaluate, and audit any
and all books, records, and facilities maintained by a
PPG and its affiliated network of Providers pertaining
to services rendered under the PPG’s Physician
Capitated Services Agreement. Access is subject to
the confidentiality restrictions discussed in the PPG’s
Physician Capitated Services Agreement.
11.6.5 Records Retention Term
e PPG’s books and records must be maintained for
a minimum of five (5) years from the end of the fiscal
year in which the PPG’s contract with L.A. Care expires
or is terminated. However, in the event the PPG has
been duly notified that DMHC or other applicable
regulatory agency has initiated an audit or investigation
of L.A. Care, the PPG, or the Physician Capitated
Services Agreement, the PPG will retain these records
the greater of the above timeframe or until the matter
under audit or investigation has been resolved.
11.6.6 Financial Statements
As required by Section 11.4 above, each PPG must
provide L.A. Care with a copy of its Quarterly
Financial Statements and Annual Audited Financial
Statements. If requested, these financial documents,
as well as any other reports required by CMS and
DMHC, must be made available to DMHC, CMS,
and any other regulatory agencies.
133
12.0 Claims
and Payment
is section covers guidelines for reimbursement
for services rendered or claims processing and other
claims-related areas for L.A. Care’s Medi-Cal Direct
Line of Business (LOB), MCLA.
12.1 Responsibility of
Participating Providers
L.A. Care has entered into agreements with Plan
Partners, Contracted Providers, PPG/IPA’s and
Hospitals (Participating Providers) to divide the
financial responsibility of adjudicating claims. Within
the terms of the Participating Provider’s agreement
with L.A. Care, each Participating Provider must stay
within compliance with Title 28 of the California
Code of Regulations (CCR), Section 1300.71
Claims Settlement Practices (and with 42 U.S.C.
Section 1396a (a)(37)(A) and title 22 of the CCR,
Section 51008 for the Medi-Cal Program), and other
applicable federal and state regulations.
12.2 Claims Submission
Timely Filing Deadline
Timely filing of a claim to L.A. Care is as soon as
possible but not later than within 180 days of the
date of service unless a L.A. Care contract specifies
otherwise. Contracted Providers please refer to your
contract with L.A. Care for timely filing criteria.
Billing and Electronic Data Interchange Submissions
Providers must use good faith effort to bill with the
most current coding available.
LA Care encourages Electronic Data Interchange
(EDI) claims submissions.
Providers may register with:
• Office Ally at https://cms.officeally.com; L.A. Care’s
payer Identification is “LACAR.” Providers may reach
Office Ally customer support at 1.866.575.4120
• Change Healthcare at www.changehealthcare.com.
For assistance with submitting claims electronically,
please contact your Practice Management System
Vendor or Change Healthcare Customer Support
1.877.363.3666
Any paper claims that must be submitted should be on
CMS 1500 forms for professional services and on UB-
04 forms for facility services.
PROFESSIONAL AND SUPPLIER CLAIMS
Providers sending paper professional and supplier
claims to L.A. Care must use a valid version of Form
CMS 1500. is form is maintained by the National
Uniform Claim Committee (NUCC), an industry
organization in which CMS participates.
Cal MediConnect Claims
Once a Cal MediConnect claim is submitted for the
Medicare portion, L.A. Care Health Plan will create a new
claim for the Medi-Cal portion for secondary processing.
Providers should follow the standard processes (e.g.,
corrected claims, re-submissions, etc.) for these claims.
Incomplete Claims
Claims submitted with incomplete or invalid
information may be returned to the submitter as an
unclean claim. Examples include the following:
Unclean Claims
Unclean claims include those with incomplete or
missing, required information. Claims that contain
complete and necessary but invalid information are
also unclean. Valid information may be required for all
claims or may be required on a conditional basis.
Incomplete Information
ese claims include those with missing required
or conditional information (e.g., no Unique
Physician Identification Number (UPIN) / Provider
Identification Number (PIN) or National Provider
Identifier (NPI) when effective).
Invalid Information
ese claims include those with required or conditional
information on a claim that is illogical, or incorrect
(e.g., incorrect UPIN/PIN or NPI when effective) or
that is no longer in effect (e.g., an expired number).
Paper Claims Submission
Initial and Resubmitted Paper Claims may be
submitted hard copy to:
L.A. Care Health Plan
Attention: Claims Department
P.O. Box 811580
Los Angeles, CA 90081
L.A. Care encourages electronic submission of claims,
as stated above.
12.3 Claims Adjudication
Every claim is subject to a comprehensive series of
quality “edits” and “audits.” ese quality checks verify
and validate all claim information to determine if the
claim should be paid, denied or suspended for Manual
134
review. Edit and audit checks include but are not
limited to the verification of the following:
• Data validity
• Procedure and diagnosis compatibility
• Provider eligibility on date of service
• Recipient eligibility on date of service
• Medicare or other insurance coverage
• Claim duplication
• Authorization requirements
12.4 Provider Portal Claims Verication
e L.A. Care Provider Portal is the preferred method
for contracted Providers to check claims status. Go
to the following link to register at http://www.lacare.
org/providers/provider-sign-in/provider-registration.
Providers may obtain claim status by calling
1.866.522.2736 or e-mailing LACarePSU@lacare.org.
Non-contracted providers may register with Change
Healthcare (formerly Emdeon) to submit claims
electronically, check member eligibility, and obtain
claims status for a fee. For assistance, contact Change
Healthcare Customer Support 1.877.363.3666.
12.5 Coordination of Benets
In accordance with requirements of the Balanced
Budget Act of 1997, L.A. Care, as a secondary payer,
will pay deductibles, co-insurance and co-payments
for Medi-Cal covered services up to the lower of our fee
schedule or the Medicare/other insurance-allowed amount.
California law limits Medi-Cal’s reimbursements for
a crossover claim to an amount that, when combined
with the Medicare payment, does not exceed Medi-
Cal’s maximum allowed for similar services (Welfare and
Institutions Code, Section 14109.5). When a Member
has other health insurance (including Medicare, a
Medicare Health Maintenance Organization (HMO)
or a commercial carrier), L.A. Care will coordinate
payment of benefits. ese other insurers are considered
the primary payer, and L.A. Care is the secondary payer.
12.6 Balance Billing
Federal law prohibits balance billing of beneficiaries
eligible for Medi-Cal and Medicare, including
L.A. Care CMC members.
Balance billing is the practice of billing a Member
for the difference between what is reimbursed for
a covered service and what a Provider feels should
have been paid. It includes asking a beneficiary to
enter into a private payment agreement or waive their
balance billing protection and charging deductibles,
coinsurance, co-pays or other administrative fees.
For information on a L.A. Care members’ Medi-Cal
eligibility, please call L.A. Care at 1.888.839.9909.
12.7 Provider Disputes
L.A. Care makes available to all Providers a fast, fair and
cost-effective dispute resolution mechanism for disputes
regarding invoices, billing determinations or other
contract, non-contracted issues to the Providers. e
dispute resolution mechanism is handled in accordance
with applicable law and the Provider’s Agreement.
Disputes
A Provider has a right to file a dispute in writing to
L.A. Care within 365 days from the date of service or
the most recent action date, if there are multiple actions.
A Provider dispute is a written notice to L.A. Care
challenging or appealing or requesting consideration
of a claim such as the following:
• Payment of a claim
• Denial of a claim
• Adjusted
• Contested
• Seeking resolution of a billing determination
• Seeking resolution of other contract dispute
• Disputing a request for reimbursement of an
overpayment to a claim
Second Level Disputes
A Provider who is unable to resolve a billing and
payment issues can follow a second level dispute process
within 365 days of the initial action in question.
Submitting Payment Disputes
A Provider must submit a written notice to L.A. Care by
U.S. Mail or other physical delivery for a dispute relating
to the adjudication of a claim or a billing determination.
Disputes must be sent to the following address:
L.A. Care Health Plan
Attention: Provider Disputes
P.O. Box 811610
Los Angeles, CA 90081
Required Information for Provider
Payment Dispute Notices
A Provider Dispute Notice must contain at least
the information listed below, as applicable. If the
Provider Dispute Notice does not contain all of the
applicable information listed below, L.A. Care may
return the Provider Dispute Notice, with written
identification of the missing information necessary to
consider the dispute.
135
A Provider may submit an amended Provider
Payment Dispute Notice (including the missing
information) within 30 business days after the date
the Provider Payment Dispute Notice was received
back from L.A. Care. Amended Provider Payment
Dispute Notices can be sent to:
L.A. Care Health Plan
Attention: Provider Disputes
P.O. Box 811610
Los Angeles, CA 90081
e following information is required for a Provider
Payment Dispute Notice:
• Provider name, the tax identification number under
which services were billed and contact information.
• If the payment dispute concerns a claim or a request
for reimbursement of an overpayment of a claim,
a clear identification of the disputed item, using
L.A. Care’s original claim number, the date of
service, and a clear explanation of the basis upon
which the payment amount, request for additional
information, request for reimbursement for the
overpayment of a claim, contest, denial, adjustment
or other action is disputed.
• If the payment dispute is not about a claim, a clear
explanation of the issue and the Provider’s position
on the issue.
• If the payment dispute involves a Member or a
group of Members, the name(s) and Member ID
number(s), of CINs of the Member(s).
• Second Level Disputes must state “Second Level
Dispute” and include a copy of the first level dispute
filing and determination.
Acknowledgment of Receipt of Dispute
L.A. Care will acknowledge receipt of a dispute by
mail within 15 calendar days of the date of receipt by
L.A. Care.
Dispute Determinations
L.A. Care will issue a written determination stating
the outcome decision for its determination within 45
calendar days after the receipt of a clean dispute.
12.8 Payment
L.A. Care encourages providers to register for Electronic
Funds Transfer (EFT) to receive electronic payment.
L.A. Care contracts with PaySpan® to process EFT.
Benefits of Electronic Claims Payment:
• Expedited Payment via EFT
• Expedited remittance advices via the 835 Electronic
Remittance Advice (ERA) that can be used to auto-
post into your accounts receivable without manual
intervention (Your software management system
must contain this feature)
• No lost/missing checks or paper remittance advices
• Reduced administrative expenses (labor for posting
payments, courier fees)
• Streamlined payment reconciliation process
• Receive all payments electronically (including
capitation and incentive payments, where applicable)
How to Register with PaySpan® Health:
First Time Registration: You can begin the quick
and easy enrollment process online at https://www.
payspanhealth.com/ProviderPortal/Registration.
Detailed registration instructions can be found at
http://www.lacare.org/sites/default/files/universal/
how-to-register-for-payspan.pdf.
*User must check box: “Assign new or additional
Payers to this receiving account” in the Account
Setup Section to complete the enrollment process.
Existing Users: If you are already registered with
PaySpan® Health, you may add L.A. Care as a new
payer by following these simple steps:
*User must check box: “Assign new or additional
Payers to this receiving account” in the Account
Setup Section
1. Request a new registration code at
https://www.payspanhealth.com/RequestRegCode/
2. PaySpan® Health will send an automated email
indicating that a registration code will be sent to you
3. Upon receiving the registration code, go to
www.payspanhealth.com
4. Log into your account
5. Click Your Payments
6. On the right, select Add New Reg. Code
• Start Registration. You may refer to the registration
instructions found on page 3 at http://www.lacare.
org/sites/default/files/universal/how-to-register-
for-payspan.pdf
Need Assistance?
PaySpan® Health Provider Service Specialists are
available to provide assistance at 1.877.331.7154.
136
12. 9 Reporting: Quarterly Filing
of AB1455
PPGs shall submit a self-reported Claims Timeliness
Report to L.A. Care within 30 calendar days
following the end of each quarter in accordance with
AB1455 regulations (Title 28, Sections 1300.71 and
1300.71.38, Claims Settlement Practices and Dispute
Resolution Mechanism). Delegated payer’s Principal
Officer(s) must sign or personally transmit those
reports to L.A. Care. e reports include a statement
attesting to the accuracy of the information.
If the aggregate results for the quarter do not meet or
exceed the 90% on-time standard within 30-calendar
days or 95% on-time standard within 45 working days,
Days Receipts on Hand (DROH), must be reported
and a Corrective Action Plan (CAP) must be attached.
PPGs shall submit these reports electronically to
137
13.0 Encounter Data
Contracted PPGs, Specialty Plans, Vendors, Hospitals
and LTSS Providers are responsible for gathering,
processing, and submitting Encounter Data for the
services provided to all L.A. Care Members. Encounter
Data is the primary source of information about the
delivery of services provided by healthcare or atypical
providers to L.A. Care Members. Encounter Data is
utilized by the State to validate services provided and will
be used by the state to determine future reimbursements
to providers. erefore, not reporting accurate Encounter
Data may result in decreased rates paid by the State.
L.A. Care staff will track the utilized services and
analyze the validity of capitation rates when contracted
PPGs submit Encounter Data that is timely, accurate,
and complete. Capitation is a payment arrangement
for health care service providers for a set amount for
each enrolled person assigned to them, per period of
time, whether or not that person seeks care.
Encounter Data is a very important source of
information for determining needed changes and
improvements in health related programs administered
at L.A. Care. L.A. Care will also use Encounter Data
for monitoring and oversight functions including
HEDIS reporting, Capitation Rate development, and
for meeting various regulatory requirements.
L.A. Care has contracted with TransUnion Healthcare,
a data clearinghouse company, to assist PPGs with the
proper formatting timely and accurate submission of
Encounter Data.
13.1 Requirements
PPGs, Specialty Plans, Vendors, Hospitals and
LTSS providers are required to submit all requested
Encounter Data, including data for services provided
under the capitated arrangement for L.A. Care
Members. Encounter Data is required to be submitted
within sixty (60) calendar days after the end date of
service in which the encounter occurred. Encounter
Data must be submitted at minimum, on a monthly
basis. Services must be coded accurately and comply
with national standards.
Entities that are required to submit encounters to
L.A Care directly must submit electronically using
the national standard transaction format and in
accordance with specifications established in the
Implementation Guides
©
(subscription required) and
L.A. Care’s supplied Companion Guides.
PPG and Hospital Encounter Data must be
submitted in an electronic format in accordance with
the Encounter Data specifications established by
TransUnion Healthcare. PPGs must submit Encounter
Data directly to TransUnion Healthcare. When a PPG
uses TransUnion Healthcare to process its Encounter
Data, TransUnion Healthcare will convert the PPG’s
Encounter Data into the appropriate format to meet
L.A. Care’s specifications.
PPGs and Hospitals must use TransUnion Healthcare’s
services under the below mentioned terms and
conditions free of charge. L.A. Care will reimburse
TransUnion Healthcare for services rendered to
all contracted PPGs. Listed below is TransUnion
Healthcare’s contact information.
Doris Bermejo
Major Account Executive
TransUnion Healthcare
200 Corporate Point, Suite 350
Culver City, CA 90230
1.310.337.8530 voice
Email: [email protected]
Website: www.transunion.com/payers
To use TransUnion Healthcare services, PPGs and
Hospitals are required to:
• Submit Encounter Data to TransUnion
Healthcare within the parameters required
by TransUnion Healthcare.
• Submit Encounter Data to TransUnion Healthcare
sixty (60) calendar days after the end date of service in
which the encounter occurred to ensure routine and
timely submission of Encounter Data to L.A. Care.
138
14.0 Marketing
14.1 Regulatory Approval
L.A. Care’s RA&C Department ensures all marketing
materials are submitted to the appropriate regulatory
agencies for approval. Once approved, L.A. Care uses
these marketing materials to inform Members of their
benefits, rights, and processes to navigate through the
healthcare delivery system.
e purpose of the regulatory submission process
section is to ensure that all marketing and or other
Member materials used by L.A. Care and L.A. Care’s
Providers have been approved by DHCS, DMHC and
other regulatory agencies.
14.2 Marketing Activities and Standards
L.A. Care’s marketing standards for Providers’
MCLA marketing and promotional activities are in
accordance with DHCS and other relevant regulatory
marketing guidance.
L.A. Care may impose sanctions on a Provider,
according to this Manual or the Provider’s contractual
agreement, for any violation of these standards, in
accordance with DHCS marketing guidelines.
Nothing here affects a Provider’s obligation to
communicate with L.A. Care or a Member pursuant
to contractual, statutory, regulatory, or L.A. Care
policy requirements.
Permitted Activities
• Providers may enter into discussions with
their Members when the Member is asking for
information or advice from the Provider regarding
their options, as long as the Provider gives the
Member objective information, in accordance with
marketing guidelines from DHCS and other relevant
regulatory marketing guidance.
• Providers may distribute L.A. Care materials or
make them available in their office, provided that
materials are distributed or made available for all
plans with which the Provider contracts.
• Providers may display posters or other materials
announcing their L.A. Care contractual
arrangements, provided they do so for all plans with
which the Provider contracts.
• Providers may provide objective information on all
L.A. Care sponsors’ specific plan formularies, based
on a particular Member’s medications and health
care needs.
• Providers may provide objective information regarding
all plan sponsors’ specific plans being offered, such as
covered benefits, cost sharing and UM tools.
• Providers may refer their Members to other sources
of information, such as the following:
°
State Medi-Cal office
°
L.A. Care’s Health Plan Field Representatives
• Providers may print out and share information with
Members from the CMS and/or DHCS website.
• Providers may distribute printed information provided
by a plan that compares the benefits of all the different
plans with which they contract. Plan benefit comparison
materials must adhere to all of the following:
°
Do not highlight or rank order any specific plan.
°
Include only objective information.
°
Have the concurrence of all plans listed in
the materials.
°
Be approved by DHCS. (ese materials are
not subject to File and Use provisions that states
materials will only need to be submitted and do
not have to wait for approval prior to use.)
• Providers may provide a link on their website to the
DHCS Online Enrollment Center.
L.A. Care considers health education material and
wellness promotion materials as Marketing Materials if
such material is any of the following:
• Used in any way to promote L.A. Careor a Provider
• Used to explain benefits
• Contains any commercial message or Member
notification information
L.A. Care shall consider any communication via
the Internet as both Marketing Materials and as
Promotional Activities.
• Communication via the Internet consists of,
but may not be limited to, electronic transfer,
transmittal, dissemination, and distribution through
the Provider’s or partner organization’s website.
• Providers must follow the approval procedures
provided in this section for all Marketing Materials and
Promotional Activities conducted through the Internet.
Marketing Standards
All Marketing Materials and Marketing Activities must
follow all DHCs marketing guidelines, which pertain
to, but are not limited to, all of the following:
• Advertising and pre-enrollment materials
• Post-enrollment materials
• Outreach to Members
• Promotional activities/events
• Other marketing activities
139
Marketing Materials must not contain false, misleading,
or ambiguous information. L.A. Care and its contracted
Providers must ensure all Marketing Materials are
at a reading level no greater than 6
th
grade and they
must be both culturally and linguistically appropriate
(See Section 10 of this Manual, Cultural and
Linguistic Services).
All Marketing materials must clearly be labeled
with the following:
• e year they were last updated
• e source of any representations, endorsements, or
awards referred to in the Marketing Materials
• e entity responsible for producing the
Marketing Materials
L.A. Care Logo
L.A. Care reserves the right to review and ensure correct
usage of the L.A. Care logo, including the contents of
the material that contains the L.A. Care logo.
L.A. Care must review and approve the use of the
L.A. Care logo prior to publishing.
14.3 Approval Process
14.3.1 A Provider must submit all Marketing
Materials and Promotional Activities to L.A. Care
through the Provider Network Management
Department for review and approval at least
45 calendar days prior to using the Marketing
Materials or engaging in the Promotional Activities.
Mail or fax to:
L.A. Care Health Plan
Attn: Provider Network Management Department
1055 West 7
th
Street, 10
th
Floor
Los Angeles, CA 90017
Fax: 1.213.438.5732
Providers must submit documentation of proposed
Marketing Materials and Promotional Activities to
L.A. Care. is documentation must include all of
the following:
• An English draft in final layout of the proposed
Marketing Materials or description of the
proposed Activities
• A brief description of the use of the material
• A draft of translated versions of the proposed
Marketing Materials with a letter attesting that the
translated material conveys the same information
and level of detail as the English material
(translation to only occur after the English version
has been approved)
• e total cost of the proposed Marketing Materials
or Promotional Activities
If, upon review, L.A. Care does not object to a
Provider’s Marketing Materials and Promotional
Activities and associated documentation, L.A. Care
will send a written notice to the Provider within
ten 10 business days stating L.A. Care’s review and
intent to submit the proposed Marketing Materials
and Promotional Activities to DHCS and relevant
regulatory agency.
If, upon review, L.A. Care objects to a Provider’s
Marketing Materials or Promotional Activities,
L.A. Care will send a written notice to the
Provider within 10 business days after receipt of all
documentation that describes its objections in detail.
In this situation, the following process applies:
• e Provider may resubmit revisions of the Marketing
Materials or Promotional Activities and all applicable
documentation to L.A. Care within 5 business days
after receipt of L.A. Care’s notice of objection.
• L.A. Care will review the resubmitted, revised
documentation and will notify the Provider within
5 business days after receipt if the Marketing
Material is approved.
• If approved, L.A. Care will submit the proposed
Marketing Materials or Promotional Activities to
DHCS and relevant regulatory agency.
• If a Provider fails to resubmit revisions of Marketing
Materials or Promotional Activities within 5
working days after receipt of L.A. Care’s review, then
the Provider must submit such materials as new
Marketing Materials or Promotional Activities.
14.3.2 A Provider must NOT use Marketing
Materials or engage in Promotional Activities prior to
receipt of L.A. Care’s written notice of approval.
14.3.3 L.A. Care must notify the Physician Group
or Provider that proposed Marketing Materials or
Promotional Activities have been approved within
5 working days after receipt of regulatory approval.
14.3.4 L.A. Care will consider Marketing Materials
and Promotional Activities approved if DHCS or
relevant regulatory agency fail to respond to
L.A. Care’s request to approve Marketing Materials
or Promotional Activities within 45 working days.
140
14.4 Prohibited Activities
Prohibited activities include the following:
• Engaging in prohibited activities in accordance with
DHCS marketing guidelines
• Use of Marketing Materials or engaging in
Promotional Activities without prior written
approval from L.A. Care
• Use of logos or other identifying information used
by a government or public agency, including
L.A. Care, without prior authorization
e rules regarding prohibited activities include, but
are not limited, to the following:
• Directing, urging, or attempting to persuade
potential enrollees to enroll in a specific plan based
on financial or other interests
• Mailing marketing materials on behalf of L.A. Care,
without prior approval
• Offering anything of value to induce L.A. Care
Members to select them as their Provider
• Offering inducements to persuade potential enrollees
to enroll in L.A. Care
• Accepting any compensation directly or indirectly
from a L.A. Care Field Representative or contracted
Agents for enrollment activities
• Giving any Member names, addresses, or phone
numbers for the solicitation of enrollment to the
L.A. Care Health Plan Field Representatives or
contracted Agents
Failure to Comply
L.A. Care may impose sanctions on a Provider for any
violation of the terms and conditions of this section,
in accordance with marketing guidelines from DHCS,
and other relevant regulatory guidance, which include
but are not limited to the following:
• Financial penalties
• Immediate suspension of use of all Marketing
Materials and Promotional Activities for a period
not to exceed 6 months
• Imposition of an enrollment cap or Membership cap
and Provider Contract termination
141
15.0 Compliance
15.1 Goals And Objectives
e goal of L.A. Care’s Compliance Program is to ensure
that all L.A. Care members receive appropriate and quality
health care services through the provider network in
compliance with all applicable California and federal rules
and regulations including CMS requirements as well
as L.A. Care contractual requirements.
L.A. Care’s Compliance Program:
Provides oversight and ongoing monitoring of delegated
responsibilities of L.A. Care’s provider network.
Requires the implementation of corrective actions
by the Provider to address deficiencies concerning
provision of health care services or L.A. Care
performance standards.
Establishes policies and procedures to identify,
investigate, and resolve potential or actual fraud,
waste, and abuse (FWA) activities.
Establishes education/training opportunities and other
available resources to assist Provider in becoming
compliant with the Health Insurance Portability
and Accountability Act (HIPAA) requirements and
member rights concerning privacy and confidentiality.
Establishes education/training opportunities and
other available resources to assist Providers in
achieving and maintaining compliance with CMS
MA-PD requirements.
Establishes education/training opportunities to
assist Providers with compliance concerns and issues
regarding fraud, waste, and abuse.
Provides L.A. Care’s latest code of conduct online
training program at: lachp.org/compliance/
coc_2010_ppg.nsf/coc_login
Note: is link will be changing and you will be
notified of this change.
(When taking the online training, please log-in with
your name, as well as the name of the organization
before beginning).
15.2 Authority and Responsibility
L.A. Care’s Compliance Program strives to ensure
compliance with federal and California State rules and
regulations affecting the administration of the Medi-Cal
program. is includes, but is not limited to, the
following requirements as applicable to each Provider’s
contract with L.A. Care:
Requirements set forth by DHCS and DMHC as
described in state and federal regulations and other
guidance or communications.
Rules and regulations promulgated by and for the
DMHC and the DHCS.
All applicable federal rules and regulations that apply
to the provision of health care services.
Federal and California State governing law and
legal rulings.
Terms and conditions as set forth in L.A. Care’s
contracts with CMS and DHCS.
Requirements established by L.A. Care and
implemented with the provider as stated in the
Provider’s contract with L.A. Care.
15.3 Delegation of Compliance and
Audit Program
L.A. Care does not delegate its Compliance Program
responsibilities to a Provider. However, the provider
is required to comply with all state and federal
Compliance Program requirements. L.A. Care staff
works with provider staff to administer compliance
activities and implement corrective actions to rectify
deficiencies. Provider staff are encouraged to work
with L.A. Care compliance staff to ensure compliance
with all L.A. Care performance standards.
15.4 Audit and Oversight Activities
To ensure that all L.A. Care members receive
appropriate health care services, L.A. Care staff performs
an annual audit of contract responsibilities and services
delegated by L.A. Care to provider. L.A. Care’s audit
program for delegated Providers includes, but is not
limited to, the following activities:
Annual on-site visit and/or desk-top audit to delegated
Providers to ensure that all delegated responsibilities
and services are in compliance with Medi-Cal
program requirements. e annual evaluation will be a
comprehensive assessment of the delegate’s performance,
including both compliance with applicable standards
and the extent to which the delegate’s activities promote
L.A. Care’s overall goals and objectives for the delegated
function. If any problems or deficiencies are identified,
the evaluation will specify any necessary corrective
action and include procedures for assuring that the
corrective action is implemented.
Ad-hoc on-site visits to review provider activities to
ensure compliance with program requirements.
142
Ongoing monitoring through review of periodic reports
and data required as outlined in the delegation agreement.
Review of all provider books and records and
information as may be necessary to demonstrate
provider compliance with federal, California State,
and L.A. Care contractual requirements. Records
include, but are not limited to, financial records and
books of accounts, all medical records, medical charts
and prescription files, and any other documentation
pertaining to medical and non-medical services
rendered to members, and such other information as
reasonably requested by L.A. Care.
15.5 Provider Compliance Responsibilities
15.5.1 General
Provider agrees to comply with Medi-Cal laws, state
and federal regulations, and DHCS and DMHC
instructions; provider also agrees to audits and
inspection by DHCS and DMHC and/or their
designees and to cooperate, assist, and provide
information as requested, and maintain records
(including records of education, training, and
supporting documentation) for a minimum of 10 years.
Provider shall ensure all their related entities,
contractors, or subcontractors, and downstream
entities involved in transactions related to L.A. Care’s
Medi-Cal line of business maintain and provide
access to all pertinent contracts, books, documents,
papers, and records (including records of education,
training, and supporting documentation) necessary for
compliance with state and federal requirements.
Provider shall require all related entities, contractors,
subcontractors, and downstream entities to agree
to comply with Medi-Cal laws, state and federal
regulations, and DHCS and DMHC instructions
and agree to audits and inspection by DHCS and
DMHC and/or their designees and to cooperate, assist,
and provide information as requested, and maintain
records (including records of education, training and
supporting documentation) for a minimum of 10 years.
Provider shall conduct annual general and specialized
compliance training for their employees. Provider
must submit documentation of that general and
specialized compliance training to L.A. Care’s
Compliance Officer annually.
15.5.2 Policies and Procedures and Standards
of Conduct
Provider shall have written policies, procedures, and
standards of conduct (code of conduct) that are detailed
and specific, describing the operation of the Provider’s
compliance program. e policies, procedures, and
standards of conduct shall ensure the following:
1. Articulate the Provider’s commitment to comply
with all applicable federal and state standards
2. Describe compliance expectations as embodied in
the standards of conduct
3. Implement the operation of the compliance program
4. Provide guidance to employees and others on
dealing with suspected, detected, or reported
compliance issues
5. Identify how to communicate compliance issues to
appropriate compliance personnel
6. Describe how suspected, detected, or reported
compliance issues are investigated and resolved by
the provider
7. Include a policy of non-intimidation and non-
retaliation for good faith participation in the
compliance program including, but not limited
to, reporting potential issues, investigating issues,
conducting self-evaluations, audits and remedial
actions, and reporting to appropriate officials.
8. Describe the Provider’s expectations that all
employees, downstream, and related entities
conduct themselves in an ethical manner; that
issues of noncompliance and potential FWA are
reported through appropriate mechanisms; and that
reported issues will be addressed and corrected.
Provider’s compliance policies, procedures, and standards
of conduct shall be distributed to Provider’s employees
who support the Provider’s Medi-Cal business at the
following times: within 90 days of hire, when there are
updates to the policies, and annually thereafter.
Provider shall ensure that policies, procedures, and
standards of conduct are distributed to downstream
and related entities’ employees who support the
Provider’s Medicare, Medi-Cal business at the
following times: within 90 days of hire, when there are
updates to the policies, and annually thereafter.
15.5.3 Compliance Officer or Designee
Provider shall designate a compliance officer, or
designee, and a compliance committee who report
directly and are accountable to the Provider’s chief
executive or other senior management.
15.5.4 Training and Education
Provider shall establish, implement, and provide
effective compliance training and education for its
employees (including the CEO, senior administrators
or managers, and governing body members) and for
143
downstream and related entities. Provider’s training
and education shall include the following:
1. Annual training and education for Provider’s
employees (including the CEO, senior
administrators or managers, and governing body
members) and for downstream and related entities;
2. Provider’s employees (including temporary workers,
volunteers, the CEO, senior administrators or
managers, and governing body members) and
downstream and related entities receive general
compliance and FWA training within 90 days of
hire/contracting and annually thereafter;
15.5.5 Effective Lines of Communication
Provider ensures that general compliance information
is communicated to downstream and related entities’
employees; and
Provider reviews and updates, if necessary, the general
compliance training whenever there are material
changes in regulations, policy, or guidance, and at least
once annually.
Provider shall establish and implement effective lines
of communication, ensuring confidentiality between
the Provider’s compliance officer, members of the
Provider’s compliance committee, the Provider’s
employees, managers, and governing body, and the
Provider’s downstream and related entities. Such lines
of communication must be accessible to all and allow
compliance issues to be reported including a method
for anonymous and confidential good faith reporting
of potential compliance issues as they are identified.
Provider’s lines of communication shall include the
following in order to be considered effective:
Provider has an effective way to communicate information
from the Provider’s compliance officer to others;
Provider’s written standards of conduct and/or policies
and procedures must require all employees, members
of the governing body, and downstream and related
entities to report compliance concerns and suspected
or actual violations related to the Medi-Cal program
to L.A. Care and the provider;
Provider must have a system in place to receive, record,
respond to, and track compliance questions or reports
of suspected or detected noncompliance or potential
FWA from employees, members of the governing
body, enrollees, and downstream and related entities
and their employees;
Provider adopts, widely publicizes, and enforces a no-
tolerance policy for retaliation or retribution against
any employee or downstream and related entities who
in good faith reports suspected FWA;
e methods available for reporting compliance or
FWA concerns and the non-retaliation policy are
publicized throughout the PPG’s facilities; and
Provider makes the reporting mechanisms user
friendly, easy to access and navigate, and available
twenty-four hours a day, seven days a week for
employees, members of the governing body, and
downstream and related entities.
15.5.6 Well-Publicized Disciplinary Standards
Provider shall have well-publicized disciplinary
standards through the implementation of procedures
which encourage good faith participation in the
compliance program by all affected individuals.
15.5.7 Routine Auditing and Monitoring
Provider shall establish and implement an effective
system for routine monitoring and identification of
compliance risks. e system should include internal
monitoring and audits and, as appropriate, external
audits, to evaluate the Provider’s compliance with
Medi-Cal requirements and the overall effectiveness
of the compliance program; the Provider’s compliance
includes compliance by the Provider’s downstream and
related entities. Provider’s system for routine monitoring
and identification of compliance risks shall include the
following in order to be considered effective:
Provider shall develop a monitoring and auditing work
plan that addresses the risks associated with the
Medi-Cal benefits. e compliance officer and
compliance committee are key participants in this process;
Provider shall establish and implement policies and
procedures to conduct a formal baseline assessment of
the Provider’s major compliance and FWA risk areas,
such as through a risk assessment;
Provider shall have a monitoring and auditing work plan
that is based upon the results of the risk assessment;
Provider shall have a work plan that includes a
schedule that lists all of the monitoring and auditing
activities for the calendar year;
Provider’s compliance officer and compliance
committee shall ensure the implementation of an
audit function to conduct oversight of the Provider’s
operation and compliance program appropriate to the
Provider’s size, scope, and structure;
144
Provider shall develop a strategy to monitor and audit
its downstream and related entities to ensure that
they are in compliance with all applicable laws and
regulations; and
Provider shall track and document compliance efforts.
15.5.8 OIG/GSA and Other Exclusions
Provider shall review the DHHS OIG List of
Excluded Individuals and Entities (LEIE list) and
the GSA Excluded Parties Lists System (EPLS) prior
to the hiring or contracting of any new employee,
temporary employee, volunteer, consultant, governing
body member, or downstream and related entities,
and monthly thereafter, to ensure that none of these
persons or entities are excluded or become excluded
from participation in state and federal programs.
15.5.9 System for Promptly Responding to
Compliance Issues
Provider shall establish and implement procedures
and a system for promptly responding to compliance
issues as they are raised, investigating potential
compliance problems as identified in the course of
self-evaluations and audits, correcting such problems
promptly and thoroughly to reduce the potential for
recurrence, and ensuring ongoing compliance with
state and federal requirements.
Provider’s system for promptly responding to
compliance issues shall include the following:
1. Provider conducts a timely and well-documented
reasonable inquiry into any compliance incident or
issue involving potential Medi-Cal, state and/or
federal program noncompliance or potential FWA;
2. Provider undertakes appropriate corrective
actions in response to potential noncompliance or
potential FWA;
e provider ensures that provider and downstream
and related entities have corrected their deficiencies;
e elements of the corrective action that address
noncompliance or FWA committed by the Provider’s
employee(s) or downstream and related entities are
documented, and include ramifications should the
PPG’s employee(s) or its downstream and related
entities fail to satisfactorily implement the corrective
action. e provider enforces effective correction
through disciplinary measures, including employment
or contract termination, if warranted; and
Provider self-reports potential FWA discovered at
the provider level, and potential fraud and abuse by
downstream and related entities, as well as significant
waste and significant incidents of Medi-Cal, state and/
or federal program noncompliance to L.A. Care.
15.6 L.A. Care’s Program Integrity Plan
L.A. Care (“L.A. Care”) recognizes the importance
of preventing, detecting and investigating Fraud,
Waste and Abuse (FWA). L.A. Care is committed to
protecting and preserving the integrity and availability
of health care resources for our members, stakeholders,
and business partners by maintaining a comprehensive
program integrity plan, i.e., Compliance Program.
ese responsibilities are delegated to the Program
Integrity Unit – a subdivision of RA&C which includes
the Special Investigation Unit (SIU), whose mission is
to maintain adherence to the Program Integrity Plan to
ensure the integrity of publicly funded programs.
e Role of the SIU in Program Integrity
e SIU is a team of L.A. Care personnel charged with
investigating allegations of FWA, and facilitating all anti-
fraud efforts at L.A. Care. e team consists of clinicians
and subject matter experts who represent the following
areas within the organization including, but not limited
to, Legal Services, Regulatory Affairs and Compliance,
Health Services, Finance, Claims, Member Services,
Pharmacy and Formulary, and Credentialing.
e goal of the SIU is to protect and preserve the
integrity and availability of health care resources
for L.A. Care members, stakeholders, and business
partners by maintaining a comprehensive program
integrity plan. Anti-fraud activities will be coordinated
between L.A. Care and its Providers and the FDRs of
its Providers. e term “Provider” includes all health
care practitioners and institutions or organizations that
provide health care services or supplies.
Fraud, Waste and Abuse Defined
Fraud is defined as an intentional deception or
misrepresentation made by a person with the
knowledge that the deception could result in some
unauthorized benefit to himself or herself or some
other person. It includes any act that constitutes fraud
under applicable federal or state law.
Waste is defined as an overutilization of services or
careless practices that result in unnecessary costs.
Waste is generally not considered a criminally
negligent action, but rather the misuse of resources.
Abuse is defined as actions that may directly or
indirectly result in unnecessary costs to the Medicaid
and Medicare programs or any other health care
145
programs funded in whole or in part by the state,
federal, and/or local governments; improper payment;
payment for services that fail to meet professionally
recognized standards of care; or services that are
medically unnecessary. Abuse involves payment for
items or services where there is no legal entitlement to
that payment and the one receiving the payment has
not knowingly and/or intentionally misrepresented
facts to obtain payment.
Reporting Potentially Fraudulent Activities to L.A. Care
Under the terms of the contract between L.A. Care
and the Provider, the Provider or its FDRs is required
to report suspected cases of FWA.
ere are four (4) ways in which Providers and FDRs can
do this:
1. rough the Compliance Helpline
Call 1.800.400.4889 or file a report online at –
www.lacare.ethicspoint.com. e Compliance
Helpline is available 24 hours a day, seven days a
week and can be used by L.A. Care Board members,
employees, contractors, Providers, members and
other interested persons to report all violations or
suspected violations of law and/or the compliance
program and/or questionable or unethical conduct or
practices including, without limitation, the following:
• Incidents of FWA
• Criminal activity (fraud, kickback, embezzlement,
theft, etc.)
• Conflict of interest issues
• Code of conduct violations
2. rough the SIU (Compliance Officer)
e SIU is set up to receive and handle reports of
all types of potentially fraudulent activities. You
can access this by calling L.A. Care’s Compliance
Officer directly at 1.213.694.1250, ext. 4292.
3. In Writing
You can mail a written letter regarding potentially
fraudulent activities to L.A. Care at:
L.A. Care Health Plan
Attn: Compliance Officer
Regulatory Affairs & Compliance
c/o Special Investigation Unit (SIU)
1055 West 7th Street, 10th Floor
Los Angeles, CA 90017
4. Call the Provider Inquiry Line:
If, for whatever reason, you are not able to report
a potential FWA case by calling these phone
numbers, please call L.A. Care’s Provider Inquiry
Line at 1.866.522.2736.
Referral Requirements
Regardless of what method is used to report FWA to
L.A. Care, the following should be included:
• Name of Person Reporting Fraud or Abuse
(Optional, but highly recommended)
• Name, Address, License or Insurance ID of suspect
(if known)
• Nature of Complaint
• Date of Incident(s)
• Supporting Documentation (Optional)
If FWA is found, the fraudulent incident or
activity is reported to the appropriate outside
law enforcement and/or regulatory agency. To
learn more about FWA or how to report it to the
government, please go to: www.stopmedi-calfraud.
DHCS.ca.gov or call the Medi-Cal Fraud
Hotline at 1.800.822.6222. You can also visit
www.stopmedicare.fraud.gov.
Non-Retaliation
Neither L.A. Care nor any of its contracted
entities, including PPGs, shall retaliate against any
employee, temporary employee, contractor, or agent
who, in good faith, reports suspected FWA or code
of conduct violations to L.A. Care, the contracted
entity, or to a regulatory agency. Additionally,
L.A. Care’s contracted entities shall require that its
subcontractors abide by this non-retaliation policy.
Communication of L.A. Care’s FWA Detection Efforts
L.A. Care uses various means to educate its provider
network and membership about its FWA detection
efforts. Information about L.A. Care’s FWA detection
activities is communicated in some of the following
ways: provider bulletins; provider mailings; provider
trainings; member newsletters; new member handbook
and other sources which may include L.A. Care’s
Regional Community Advisory Committee meetings.
Annual Fraud Waste and Abuse
and General Compliance Training
All L.A. Care contracted Providers must ensure
that all employees and contracted downstream
and related entities participate and complete the
Medicare Parts C and D Fraud, Waste, and Abuse
and General Compliance Training within 90 days of
hire/contracting and annually thereafter. Effective
January 1, 2016 all Medicare Providers must use the
training materials provided by CMS; the materials can
146
be accessible through the CMS Medicare Learning
Network at:
http://www.cms.gov/Outreach-and-Education/
Medicare-Learning-Network-MLN/MLNProducts/
ProviderCompliance.html
Providers that have met FWA certification standards
through enrollment as a Medicare provider are
deemed to have met FWA training and educational
requirements, but still must fulfill the general
compliance training requirements.
All Providers are required to submit an executed FWA and
General Compliance Awareness Attestation confirming
their organization’s compliance with this requirement.
15.7 Enforcement of
Disciplinary Standards
It is L.A. Care’s expectation that Providers and their
FDRs immediately report to L.A. Care any suspected
compliance issues, such as noncompliant, unethical,
or illegal behavior. Such behavior may include, but is
not limited to, falsifying diagnoses, claims, or other
documents; refusal to cooperate with state or federal
audits or investigations; and other behavior. Such reports
can be made directly to L.A. Care’s Compliance Officer
at 1.213.694.1250, x4292. Anonymous complaints of
noncompliant, unethical, or illegal conduct may also
be reported by calling L.A. Care’s Compliance Helpline
at 1.800.400.4889 or via the internet at www.lacare.
ethicspoint.com. e Compliance Helpline is available
twenty-four hours a day, seven days a week. e provider
or FDR shall also assist in the resolution of reported
compliance issues.
L.A. Care will timely, consistently, and effectively act
when noncompliant or unethical behavior is found and
reported to L.A. Care. Such action will be appropriate
to the seriousness of the violation and may include
de-delegation of a function, restriction of enrollment
or assignment of members, withholding capitation,
instituting monetary sanctions, or terminating a
contract. Refer to the PPGSA or other Provider
Agreement for further details on these measures. PPG
shall ensure that it has established, implemented, and
enforced disciplinary standards that are publicized to
those entities with which it contracts. It is L.A. Care’s
expectation that the provider will cooperate with
L.A. Care’s efforts to monitor compliance.
15.8 The Federal and California False
Claims Acts
e federal and California False Claims Acts are
the government’s primary weapon in the fight against
health care fraud. e majority of funds recovered
come from False Claims Acts suits or settlements. e
False Claims Acts permit a person who learns of Fraud
against the government to file a lawsuit on behalf of
the government against the person or business that
committed the Fraud. If the action is successful, the
person filing the lawsuit or “plaintiff” is rewarded with
a percentage of the recovery. ese persons are often
referred to as whistleblowers.
For full details on the False Claims Acts and the
protections available to whistleblowers, please see
L.A. Care Policy RAC-013, “Federal and California
False Claims Acts.”
15.9 Health Insurance Portability and
Accountability Act (HIPAA)
If a provider receives a misdirected communication
from L.A. Care, the provider must immediately notify
L.A. Care’s Privacy Office by calling 1.213.694.1250,
x4186 or e-mailing PrivacyOfficer@lacare.org.
Providers should securely destroy, return to L.A. Care,
or safely safeguard the misdirected communication.
As covered entities, L.A. Care expects all Providers
to comply with applicable privacy and security
requirements outlined by federal and state regulation
and guidelines, including those set forth under the
HIPAA Rules. A brief overview of some of these
requirements is provided below, however Providers
should review the actual HIPAA Rules or consult
with their legal counsel to understand all applicable
regulations and requirements.
Security Rule
e Security Rule requires covered entities to ensure
the confidentiality, integrity, and availability of all
electronic protected health information (“ePHI”)
it creates, receives, maintains, or transmits. It also
requires entities to protect against any reasonably
anticipated threats or hazards to the security or
integrity of ePHI, protect against any reasonably
anticipated uses or disclosures of such information
that are not permitted or required by the Privacy Rule,
and ensure compliance by their workforce. Required
safeguards include application of appropriate policies
and procedures, safeguarding physical access to ePHI,
and ensuring that technical security measures are
147
in place to protect networks, computers, and other
electronic devices.
e Security Rule is intended to be scalable; in other
words, it does not require specific technologies to
be used. Covered entities may elect solutions that
are appropriate to their operations, as long as the
selected solutions are supported by a thorough security
assessment and risk analysis.
Privacy Rule
e Privacy Rule is intended to protect the privacy of
all individually identifiable health information in the
hands of covered entities, regardless of whether the
information is transmitted or maintained on paper,
electronically, or verbally. e Privacy Rule also gives
members a number of rights under HIPAA, including:
• e right to access their PHI;
• e right to request a restriction on certain uses and
disclosures of their PHI;
• e right to request changes to their PHI; and
• e right to receive a list (or accounting) of when
the covered entity disclosed PHI, with some
exceptions (such as for treatment, payment, and
health care operations).
In addition to these rights, the Privacy Rule includes
requirements to formally notify members of the
covered entity’s privacy practices, obtain a patient’s
permission before using or disclosing their PHI
with limited exceptions, as well as other requirements
that address their proper use and disclosure of
patient information.
15.9.3 Breach Notification Rule
If an impermissible acquisition, access, use, or
disclosure that compromises the security or privacy
of PHI occurs, HIPAA’s Breach Notification
Rule outlines the requirements for assessment
and notification. While there are specific federal
requirements that outline how to assess, who to notify,
and the notification timelines, there may be other state
and contractual standards that also apply. Providers are
strongly encouraged to familiarize themselves with all
applicable requirements and guidance.
15.9.4 Transaction and Code Sets Standards
According to CMS, electronic transactions are
activities involving the transfer of healthcare
information for specific purposes. e HIPAA
regulations have identified certain standard
transactions for Electronic Data Interchange (“EDI”)
for the transmission of health care data. ese
transactions are:
• Claims and encounter information
• Payment and remittance advice
• Claims status
• Eligibility
• Enrollment and disenrollment
• Referrals and authorizations
• Coordination of benefits
• Premium payment
If a provider engages in one of the identified
transactions electronically, they must comply with the
standard for that transaction. See https://www.cms.
gov/Medicare/Billing/ElectronicBillingEDITrans/
index.html.
15.10 Privacy and Information Security
Related Resources and Websites
U.S. Department of Health & Human Services-
Office of Civil Rights
http://www.hhs.gov/ocr/hipaa/
Centers for Medicare & Medicaid Services (CMS)
https://www.cms.gov/Research-Statistics-Data-and-
Systems/Computer-Data-and-Systems/Privacy/
Privacy_Office.html
California Department of Justice, Office of the
Attorney General
www.privacy.ca.gov
California Department of Health Care Services
http://www.dhcs.ca.gov/formsandpubs/laws/priv/
Pages/default.aspx
National Committee on Vital and Health Statistics
http://www.ncvhs.hhs.gov/
National Institutes of Health
http://privacyruleandresearch.nih.gov/
National Institute of Standards and Technology
http://www.nist.gov
Centers for Medicare and Medicaid Services
Regulations & Guidance
http://www.cms.gov/home/regsguidance.asp
148
16.0 Pharmacy
16.1 Overview
L.A. Care’s prescription drug formulary is a preferred
list of covered drugs, approved by the L.A. Care
Health Plan Pharmacy Quality Oversight Committee
(PQOC). is formulary applies only to outpatient
drugs and self-administered drugs. It does not apply
to drugs administered in the inpatient or medical
office setting, unless otherwise specified.
e formulary is a continually reviewed and revised
list of preferred drugs based on safety, clinical
efficacy, and cost-effectiveness. Prescribing healthcare
providers are requested to prescribe medications
included on the formulary.
16.2 Pharmacy Quality and Oversight
Committee (PQOC)
e PQOC Committee oversees the Pharmacy and
erapeutics Committee administered by the contracted
Pharmacy Benefit Manager (PBM). e PQOC’s role
is to ensure formulary development and maintenance
that is evidence-based and tailored to the unique needs of
L.A. Care’s membership.
Additionally, the PQOC provides a peer review forum
for discussion regarding L.A. Care’s clinical policies,
provider communication/education opportunities,
pharmacy clinical programs/outcomes, and specialty
drug management strategy. e PQOC convenes
quarterly to review the clinical direction of the
pharmacy benefit to support and enhance health care
outcomes for L. A. Care members.
16.3 How to Use the Formulary
e formulary is updated monthly. To view the most
updated formulary, please visit our website at lacare.
org/members/member-services/pharmacy-services.
Drugs available in generic formulations are listed by
their generic names in lower case letters and the most
common proprietary (branded) name is capitalized next
to the generic name in parenthesis. Drugs that are only
available in branded formulations are listed by their
proprietary name in ALL CAPITAL letters.
e formulary can be searched by using the “Ctrl + F”
function or the index. Drugs can be searched by generic
name, proprietary name, or therapeutic drug category.
e formulary is a tool to promote cost-effective
prescription drug use. L.A. Care has made every
attempt to create a formulary that meets all
therapeutic needs; however, the art of medicine
makes this a formidable task. L.A. Care welcomes the
participation of physicians, pharmacists, and ancillary
medical providers, in this dynamic process.
Physicians are highly encourage to direct any
suggestions or comments to L.A. Care through the
L.A. Care Health Plan Formulary Drug Review
Request Form.
is form is found on the L.A. Care website or by
clicking on this link: http://www.lacare.org/sites/
default/files/universal/formulary_review_request.pdf.
16.4 Generic Substitution
L.A. Care’s Medi-Cal Plan coves generic and branded
drug products. However, when available, FDA
approved generic drugs are to be used, regardless of
the availability of a branded product unless otherwise
specified. Generic drugs generally cost less than
branded products. All drugs that are or become
available generically are subject to review by L.A. Care’s
Pharmacy Quality Oversight Committee (PQOC).
A prescriber may request a branded product in lieu
of an approved generic product, if the prescriber
determines that there is a documented medical need
for the branded equivalent. is type of request for
coverage may be made using the ‘Prescription Drug
Prior Authorization Request’ process described in the
section 16.7.
16.5 Non-Formulary Agents
Any drug name not found in the formulary listing
shall be considered a non-formulary drug. A prescriber
may request an exception to coverage for a non-formulary
drug if the prescriber determines that there is a
documented medical need. is type of request for
coverage may be made using the ‘Prescription Prior
Authorization Request’ process described in section 16.7.
16.6 Restrictions On Drug Coverage
Formulary Agents:
A. Prior Authorization (PA): ese drugs require
approval prior to being dispensed at a network
pharmacy. Requests are reviewed with specific
prior authorization guidelines. Each request will be
reviewed on individual patient need. If the request
does not the meet guidelines established by the
149
P&T Committee/PQOC, the request will not
be approved and alternative treatment may
be recommended.
Prescribers may access specific prior authorization
criteria and forms online at www.navitus.com
under the “Prescribers” section. Prescribers will
need their NPI to access this portal.
B. Quantity Limits (QL): ese drugs have
quantity limits. If quantities exceeding the limit
are necessary, an exception to coverage may be
requested by the prescriber. Each request will be
reviewed on individual patient need. Approval
will be given if a documented medical need exists
without compromising safety.
C. Step erapy (ST): ese drugs require one or
more first step drugs to be tried before progressing
to the second step drug. If there is a medical need
to use a second step drug without trying a first step
drug, an exception to coverage may be requested
by the prescriber. Each request will be reviewed on
an individual patient need. Approval will be given
if a documented medical need exists.
Non-Formulary Agents:
A. Any drug not found on this list is considered non-
formulary. Coverage for non-formulary agents may
be requested by the prescriber. Each request will be
reviewed on individual patient need. Approval will
be given if a documented medical need exists.
B. e ‘Medication Request Process’ is generally not
available for drugs that are specifically excluded by
benefit design. For benefit exclusions refer to the
‘General Exclusions’ section below.
Please refer to the formulary introductory pages for
the full list of coverage restrictions.
16.7 Prescription Drug Prior
Authorization Request Process
Prior authorization request forms can be found on the
L.A. Care website at www.lacare.org.Click on “For
Providers” and under “Pharmacy Services” click on
“Prior Authorizations”.
e PBM reviews pharmacy prior authorizations for
L.A. Care.
A response from the PBM regarding prior
authorization requests may include a notice of action
letter in the form of an approval, denial or request for
additional information to make a determination of
medical necessity. Decisions will be made within one
business day unless there is mutual agreement between
the clinical reviewer and the prescribing provider
indicating that it is clinically appropriate for the review
time to be extended.
Expedited prior authorization requests may be made
by the prescribing provider when there is a serious risk
to life, limb, and/or rehabilitation.
Prior authorization questions or information regarding
the process may be obtained through the following:
• Telephone: Navitus Customer Care at
1.844.268.9786 for Medi-Cal.
• Fax: Providers may fax fully completed and signed
Prior Authorization Form to Navitus Health
Solutions 24 hours a day, 7 days a week, including
holidays at 1.855.878.9209 for Medi-Cal.
Non-approved requests may be appealed. e
prescriber must provide information to support the
appeal on the basis of medical necessity. Please refer to
section 16.8 for additional information.
16.8 Appeals and Grievances
If you would like to discuss a decision for a prior
authorization denial with a clinical reviewer,
prescribing providers may call Navitus Health
Solutions at 1.844.268.9786.
You have the right to appeal the decision for a non-
approved request on behalf of the member by filing an
appeal with L.A. Care. For additional information on
appeals on behalf of a member, please call L.A. Care
at 1.866.522.2736. You may also submit a copy of the
denial notice and a brief explanation of your concern
with any other relevant information to the address
below or fax it to L.A. Care at 1.213.438.5748.
L.A. Care Health Plan
Attn: Appeals and Grievances Department
1055 West 7
th
Street, 10th Floor
Los Angeles, CA 90017
16.9 Diabetes Testing Supplies
L.A. Care provides coverage for the following products
through the pharmacy benefit for the monitoring of
diabetes:
• blood glucose monitors (Abbott Products preferred;
Freestyle/Freestyle Lite),
• blood glucose test strips (Abbott Products preferred;
Freestyle/Freestyle Lite),
150
• ketone urine test strips,
• lancets and lancet puncture devices,
• injectable medications (including insulin),
• disposable needles and syringes, and
• glucagon.
16.10 Over-the-Counter
Medication Coverage
Select over-the-counter (OTC) products are available
as a covered benefit, and may be prescribed as an
alternative to prescription drugs.
OTC medications are covered with a written prescription.
ey include, but are not limited to the following:
• Analgesics
• Antacids
• Anti-diarrheal medication
• Anti-histamines
• Anti-inflammatories
• Benzoyl peroxide
• Calcium replacement
• Contraceptives
• Hydrocortisone
• Laxative/stool softeners
• Prenatal vitamins
• Select vitamins
• Smoking cessation products
• Topical anti-fungal products
• Topical antibiotics
• Topical anti-parasites
• Vaginal anti-fungal preparations
16.11 Devices & Vaccines
L.A. Care provides coverage for the following devices
through the pharmacy benefit for Medi-Cal members:
• spacers;
• peak flow meters; and
• immunizations.
Please refer to the formulary for a comprehensive list
of covered devices & vaccines.
16.12 General Benet Exclusions
(Not Covered)
A. Investigational/Experimental drug products, or
any drug product used in an investigational/
experimental manner, unless certain requirements
are met.
B. Infertility agents,
C. Drugs used for cosmetic purposes,
D. Non self-administered injectable drug products
are not covered unless otherwise specified in the
formulary listing,
E. Drugs used for erectile dysfunction
F. Foreign drugs or drugs not approved by the
United States Food & Drug Administration.
Please note that this list is subject to change.
16.13 Pharmacy Network
A large number of pharmacies are available to
members across Los Angeles County. e pharmacy
network includes most major chain pharmacies
and community pharmacies. Members should fill
prescriptions at network pharmacies. To find a
network pharmacy near you or a member, please
click on the following link: http://www.lacare.org/
members/member-tools/find-pharmacy.
16.14 Mail Order Prescriptions
L.A. Care offers members the option of getting up to
a 90-day supply of select maintenance medications
mailed to their home or alternate address through our
prescription mail order program. Please remember to
write a 30-day supply, as well as a 90-day supply plus
refills on the prescription for maintenance medication.
e mail order service is provided by WellDyneRx.
Additional information may be found at https://www.
lacare.org/providers/provider-resources/provider-
forms and under ‘Pharmacy & Formulary Forms’.
WellDyneRx accepts new prescriptions from prescribers
by phone or fax 24 hours a day, 7 days a week.
• WellDyneRx Phone: 1.866.490.3326
• WellDyneRx Fax: 1.888.830.3608
16.15 Specialty Pharmacy
L.A. Care has specific policies for use of specialty
drugs. Specialty drugs are often high cost
pharmaceuticals which may require special handling
by the manufacturer and/or the FDA, and their
effectiveness is driven by coordinated clinical support
for the member. Most of these therapies require Prior
Authorization, and most of these therapies must be
dispensed by L.A. Care’s preferred specialty pharmacy.
is is to ensure the patient achieves the optimal
clinical benefit from the prescribed therapy.
To learn more about specialty drug access and
coverage determination for these drugs and therapies
prescribing providers and pharmacies may call Navitus
Customer Care at 1.844.268.9786.
151
16.16 Pain Medication for the Terminally Ill
L.A. Care’s PBM will follow the standard coverage
determination time requirements of 24 hours or one
business day for patients identified as terminally ill
by their provider. is applies when responding to
any request by the provider for pain medication. If a
decision is not made within 72 hours, the requested
treatment shall be deemed authorized.
e provider shall contact the L.A. Care Pharmacy
Department at 1.866.522.2736 within one business
day of proceeding with the deemed authorized
treatment and provide the following information so
treatment can begin:
• confirm the 72 hour timeframe has expired
• provide member identification
• notify L.A. Care of the prescribing provider or
providers performing the treatment
• notify L.A. Care of the facility or location where the
treatment was or is to be is rendered
Prescribing providers may also call Navitus Customer
Care for additional information on the PA process at
1.844.268.9786 for Medi-Cal.
16.17 Therapeutic Interchange
L.A. Care may utilize therapeutic interchange
protocols to promote compliance, safe medication
use, improve clinical outcomes, and reduce cost when
appropriate. erapeutic interchange protocols are
never automatic. erapeutic interchanges will not
occur without the knowledge and authorization of the
prescribing provider.
16.18 Opioid Utilization Monitoring
Opioid utilization is monitored by L.A. Care and
Navitus to reduce potentially inappropriate and unsafe
use of opioids. Patient specific reports are generated
when pre-established overutilization criteria are met
during a defined time period, and the reports are
supplied to the appropriate providers.
e information is shared with providers to increase
awareness and facilitate next steps to address opioid
overutilization. e program also improved Drug
Utilization Review (DUR) controls at the point-of-
sale, formulary management, case management, and
overall utilization reviews.
Please remember to refer to the Controlled Substance
Utilization Review and Evaluation System (CURES)
before prescribing opioids.
16.19 E-Prescribing/Electronic
Health Records
L.A. Care strongly encourages all prescribing
practitioners to adopt e-prescribing and electronic
health records.
Please refer to L.A. Care’s HITEC-LA website at www.
hitecla.org for information to assist you with adopting
E-Prescribing/EHRs.
16.20 Role of Navitus Health Solutions
L.A. Care contracts with Navitus Health Solutions,
a pharmacy benefit manager, to partner in the
administration of pharmacy benefits for our members.
16.21 Contact Us
Physicians and pharmacists are highly encouraged
to direct any questions or comments related to
the pharmacy benefit to L.A. Care via e-mail to
[email protected] or by mail to the
following address:
L.A. Care Health Plan
Attn: Pharmacy & Formulary
1055 W. 7th Street, 10th Floor
Los Angeles, CA 90017
152
17.0 Managed Long
Term Services
and Supports
Managed Long Term Services and Supports (MLTSS)
provides services that support members living
independently in the community. is includes In-
Home Supportive Services (IHSS), Community-Based
Adult Services (CBAS), Multipurpose Senior Services
Program (MSSP), Care Plan Options (CPO), and
Long Term Care (LTC) provided in nursing facilities.
L.A. Care is responsible for coordinating, paying
for, and overseeing MLTSS services for members.
L.A. Care MLTSS uses a member-centered care
model designed to help members to find the right
combination of services to reside safely in the
community or in a long term care nursing facility.
MLTSS also assists with referrals to community-based
services. For example, programs such as Independent
Living Centers, Regional Centers, and Los Angeles
Area Agencies on Aging.
L.A. Care MLTSS contact information is:
E-mail MLTSS@lacare.org
Call 1.855.427.1223, or
Fax 1.213.438.4866
17.1 Managed Long Term Services and
Supports: A Resource for Providers
L.A. Care MLTSS can be an important resource for
members and providers. Providers should contact
L.A. Care MLTSS when they identify a member who:
• Qualifies for nursing home placement, but wants to
stay home.
• Has a condition that indicates a possible need for
MLTSS in the future.
• Needs social services or caregiver support.
• Needs assistance with Activities of Daily Living (ADLs)
such as bathing, dressing, toileting, and eating.
• Requires help with Instrumental Activities of Daily
Living (IADLs) such as cooking, driving, using the
phone or computer, shopping, keeping track of
finances, and managing medication.
• Receives MLTSS services, but has unmet needs.
(Unmet needs may refer to gaps in services or
the need for coordination of MLTSS services i.e.
member receiving IHSS, but may also benefit from
attending a CBAS center for physical therapy or
occupational therapy and socialization; member
attending CBAS center; but needs transportation for
medical appointments).
• Experiences difficulty with a particular MLTSS program.
• Is preparing to transition into a long term care
nursing facility or is returning to community living
from a long term care nursing facility.
L.A. Care’s MLTSS staff provides support and
expertise to providers by:
• Assisting members to find the right combination of
services through assessment and service coordination.
• Enhancing access to services, including L.A. Care
benefits, MLTSS programs, and community
resources.
• Providing oversight of MLTSS providers and
working to implement system improvements.
• Serving as MLTSS subject matter experts on
interdisciplinary care teams.
• Facilitating MLTSS provider and physician
participation on interdisciplinary care teams.
17.2 In-Home Supportive Services
In-Home Supportive Services (IHSS) pays for
homecare services that enable seniors and individuals
with disabilities (including children) to remain safely
in their own homes. Members who qualify, hire their
own IHSS - provider to assist with: personal care
services such as bathing, grooming, dressing, and
feeding; domestic services such as cooking, house
cleaning, and laundry; protective supervision for
individuals with mental impairment; paramedical
services such as assistance with medications,
bowel and bladder care; and other services such as
accompaniment to medical appointments.
To qualify for IHSS, a member must be: a legal
resident of California; living in his/her own home;
receiving (or eligible to receive) Supplemental Security
Income/State Supplemental Payment (SSI/SSP) or
Medi-Cal benefits; and be 65 years of age or older,
legally blind, or disabled by Social Security standards.
A Health Care Certification Form signed by a licensed
health care professional indicating that the individual
needs assistance to stay living at home is required.
is form will be provided to the member when they
begin the application process.
Accessing IHSS
IHSS program eligibility and service authorizations are
determined by the Los Angeles County Department
of Public Social Services (DPSS). Once approved for
153
services, members are responsible for hiring, training,
and supervising their own IHSS provider. L.A. Care
can assist members by coordinating and navigating
the IHSS assessment and re-assessment process,
connecting the member to resources that can assist
with locating a - IHSS provider, resolving IHSS-
related issues, navigating the DPSS grievance and
appeals processes, and coordinating IHSS benefits with
other health plan benefits.
Providers may refer L.A. Care members to the
MLTSS IHSS team at 1.855.427.1223 for
application assistance. e provider may also assist
with completion of required IHSS forms, and
provide members with other documentation to
support their need for IHSS services. Members who
have questions about their IHSS may be referred to
L.A. Care MLTSS for assistance.
17.3 Community Based Adult Services
Community Based Adult Services (CBAS) is a facility-
based program that members can attend during the
day for assistance with daily needs. CBAS centers
provide nursing services, medication management,
social services, physical and occupational therapy,
speech therapy, personal care, and family/caregiver
training and support. CBAS centers also provide
mental health services, nutritional counseling, meals,
and transportation to and from a member’s residence.
To qualify for CBAS, members must be over 18 years
of age and meet nursing home level of care criteria or
have other disabilities or health conditions, such as
traumatic brain injury, mild cognitive impairment,
dementia, or a developmental disability.
Accessing CBAS Services
Accessing CBAS involves a multi-step enrollment
process. A completed L.A. Care Managed Long Term
Services and Supports Authorization Request Form
must be submitted with a physician’s order. CBAS
must be ordered by the member’s physician. e
request form is accessible via the Provider Portal at
www.lacare.org. Completed authorization request forms
may be submitted to L.A. Care’s Utilization Management
Department via fax at 1.213.438.5739 for review.
A Face-to-Face evaluation is conducted by a registered
nurse to determine if the member meets the program
eligibility criteria. If the member is determined to
meet eligibility criteria, a CBAS center is authorized
to conduct a three-day assessment to develop an
Individual Plan of Care (IPC). e completed IPC is
submitted to L.A. Care for review and authorization of
services. e MLTSS Nurse Specialist will support the
assigned physician with facilitation and coordination
of care needs. e MLTSS Nurse Specialist will also
conduct regular telephonic clinical review of members
receiving CBAS services.
17.4 Multipurpose Senior
Services Program
Multipurpose Senior Services Program (MSSP)
provides intensive care coordination services for
senior members who are certified for nursing home
placement, but wish to remain at home. MSSP
providers conduct an assessment to determine the
services and supports needed for the member to
maintain their independence, and connect the
member to those services. MSSP providers may
also purchase additional services for members
such as supplemental chore and personal care
services, nutrition, handyman services, respite care,
transportation, and appliance assistance.
In order to be eligible for MSSP services, a member
must be 65 years of age or older, live within an MSSP
service area, be eligible for Medi-Cal, and be certified
for nursing home placement. If the member does not
meet the eligibility requirements for MSSP, MLTSS
staff will work with the member and their care team to
identify alternative services.
Accessing MSSP Services
L.A. Care contracts with six MSSP providers located
in designated County geographic areas that are
responsible for determining Member eligibility for
MSSP. If the member is eligible, but placed on a
waiting list, MLTSS staff will work with the member,
the MSSP provider, and other community-based
providers to ensure the member receives needed
assistance during the waiting period.
Providers may refer members who can benefit from
MSSP to L.A. Care MLTSS at 1.855.427.1223.
17.5 Care Plan Options
Care Plan Options (CPO) provides additional
services that L.A. Care MLTSS may arrange to help
Cal MediConnect members stay living safely in the
community. is includes services that are outside
of the normal scope of benefits and the MLTSS
program, such as respite care, supplemental personal
care services, home modifications or maintenance, and
nutritional services.
154
Accessing CPO Services
Providers may refer members who can benefit from
CPO services to L.A. Care MLTSS at 1.855.427.1223.
Members who wish to access CPO services may also
contact L.A. Care MLTSS directly.
17.6 Long Term Care
Long Term Care (LTC) is the provision of medical,
social, and personal care services in an institution.
Most LTC services are provided in skilled nursing
facilities (SNFs). e primary purpose of LTC is
to assist the member in activities of daily living,
such as assistance with mobility, bathing, dressing,
feeding, using the toilet, preparing special diets, and
supervision of medication.
To qualify for LTC, members must be receiving Medi-
Cal, require 24-hour long or short-term medical care,
and be eligible to receive services in a SNF. Additional
criteria for LTC may be found in State regulations
under Title 22, CCR, Section 51335.
Accessing LTC Nursing Facility Services
LTC nursing facility placement must be ordered by a
physician. If the physician believes a member needs
LTC, they should complete a L.A. Care Managed
Long Term Services and Supports Authorization
Request Form and submit to L.A. Care’s Utilization
Management Department via fax at 1.213.438.4877
for review. e form is accessible via the Provider
Portal at www.lacare.org. L.A. Care will notify the
referring individual of the LTC referral outcome
within five (5) business days for routine situations and
72 hours for urgent situations.
L.A. Care MLTSS assists members residing in a LTC
nursing facility LTC by monitoring member progress,
assisting with transitions of care, and coordinating
LTC nursing facility services with other health plan
benefits. e MLTSS Nurse Specialist will support the
assigned physician with facilitation and coordination
of care needs. e MLTSS Nurse Specialist will
conduct regular telephonic clinical review of members
in LTC nursing facilities.
For additional information please refer to L.A. Care’s
Skilled Nursing Facility Resource Center located
at: https://www.lacare.org/providers/provider-
resources/skilled-nursing-facility-resource-center.

L.A. Care Medi-Cal
™
Provider Manual
2017
LA1722 01/17
Toll Free: 1.888.839.9909 | TTY: 711 lacare.org
