
Family Planning and Medicaid Managed Care:
Improving Access and Quality Through
Integraon
Phase One Report
Sara Rosenbaum, JD
Peter Shin, PhD, MPH
Maria Casoni, MPH
Morgan Handley, JD
Rebecca Morris, MPP
Caitlin Murphy, MPA-PNP
Jessica Sharac, PhD, MSc, MPH
Akosua Tuoffer, JD
Devon Minnick, JD
In collaboration with Health Management Associates
June 2021

The George Washington University Milken Instute School of Public Health
2
Acknowledgements
We are very grateful for the time we received from the state Medicaid agency leaders who
participated in this study, and the expertise and insights provided by our advisory committee,
whose members are listed in the Appendix. We deeply appreciate our colleagues at Health
Management Associates (Donna Checkett, Rebecca Kellenberg, and Carrie Rosensweig), who
collaborated with us throughout this study and continue to advise the project.
We are also so grateful to FAIR Health for providing us with healthcare claims data from the
private insurance market, which we used to analyze current practices among private insurers.
We are, of course, especially grateful to Arnold Ventures for its ongoing support.

The George Washington University Milken Instute School of Public Health
3
State agencies, managed care plans, and public
health experts are increasingly focused on how
Medicaid managed care — a foundational part
of most state Medicaid programs — can
address whole-person health needs. Given its
documented impact on patient and population
health, high-quality family planning is essential
to a comprehensive managed care strategy.
For a half-century, family planning has been a
mandatory Medicaid service. Furthermore,
family planning has been deemed so essential
that since 1981, federal law has contained a
family planning out-of-network safeguard. This
safeguard guarantees that members of
Medicaid plans can continue to receive family
planning services from their Medicaid-qualified
provider of choice regardless of whether their
provider is part of their plan’s network.
At the same time, however, integration of family
planning and managed care is a desirable aim.
Good managed care practice means that
members should be able to look to their health
plans for comprehensive preventive care
delivered by a high-performing provider
network. Furthermore, family planning visits
uncover previously undisclosed physical and
mental health conditions requiring follow-up
care from other providers. This type of
integrated care approach presumably works
best when all providers and care managers
involved are members of the patient’s network.
This study was undertaken to understand the
current status of family planning and managed
care integration 40 years after enactment of the
“freedom of choice” safeguard, when managed
care now enrolls nearly 70 percent of the
Medicaid population. The study’s goal is to
identify practical, actionable opportunities for
greater integration and how managed care
purchasing might be used to strengthen family
planning while preserving the “freedom of
choice” safeguard.
This report shares findings from the first phase
of the study, which consisted of a review of
state purchasing documents related to
comprehensive managed care, and in-depth
interviews with senior Medicaid officials in 10
states. During Phase Two, we will conduct
similar in-depth interviews with managed care
plans and family planning providers.
Key findings include:
All states using comprehensive managed
care treat family planning as a fundamental
system feature. State officials emphasized
their expectations that contractors will fully
meet members’ family planning needs.
State purchasing documents codify the
“freedom of choice” safeguard to some
degree, but relatively few explicitly require
contractors to inform members regarding
the existence of their access safeguard.
No state viewed the “freedom of choice”
safeguard as imposing any real policy or
operational burden; indeed, nearly all
agreements address their obligation through
provisions requiring contractors to cover
and pay for family planning services
regardless of a provider’s network status.
States can do more to promote family
planning and managed care integration.
Areas of priority focus include: clarifying the
scope of family planning services to which
the “freedom of choice” safeguard should
apply, more detailed specifications
regarding contraceptive coverage, emphasis
on building strong family planning provider
networks to minimize reliance on out-of-
Execuve Summary

The George Washington University Milken Instute School of Public Health
4
network care when possible, policies that
encourage contractor use of evidence-based
family planning practice guidelines to guide
network performance and value-based
payments that attract and reward strong
network providers, and ongoing work to
develop patient and population performance
measures.
More comprehensive federal guidance
regarding managed care and family planning
integration is of enormous importance, in
particular, guidance regarding the scope of
family planning services that should be
covered by “freedom of choice” safeguard —
including sexually transmitted infection (STI)
diagnostic and treatment services, HIV
assessment and counseling, and
immunizations to reduce cancer risk.
Classifying these services as part of the family
planning bundle for freedom of choice
purposes would promote greater consistency
between Medicaid and commercial sector
practices, where it is common and standard
for providers that offer basic family planning
services to provide, bill, and receive payment
for services such as STI treatment and testing.
Such a change in Medicaid managed care
practice would also help promote access to
treatment for STIs, which have reached public
health crisis proportions.
In addition to clarifying the scope of the
“freedom of choice” safeguard, the Centers
for Medicare and Medicaid Services (CMS)
could spearhead efforts to develop best
practice approaches for family planning and
managed care integration, including service
coverage, network design, access
e n h a n c e m e nt , t e a m - b as e d c a r e
m a n a g e m e n t , a n d pe r f o r m a n c e
measurement and improvement. These
efforts can build on landmark Centers for
Disease Control (CDC) and HHS Office of
Population Affairs (OPA) family planning
standards of care by translating these
standards into managed care operational
terms. This comprehensive effort could be
carried out in collaboration with state
agencies, experts in managed care
performance and financing, clinical and
family planning practice experts, and experts
in public health and population-based health
improvement. Of great value would be the
inclusion of experts from the CDC and OPA,
who led the development of the family
planning practice standards. Such an effort
would come at a crucial time, as federal
agencies simultaneously move to restore the
nationwide Title X family planning network,
and whose providers play such a crucial
access role for the Medicaid population.

The George Washington University Milken Instute School of Public Health
5
Introducon
This report presents initial findings and
recommendations from a two-phase study of
family planning and Medicaid managed care. The
purpose of the study is to identify strategies and
options for strengthening access to high-quality,
comprehensive family planning services as a core
Medicaid managed care service while at the same
time preserving key family planning direct access
safeguards that are a longstanding hallmark of
federal Medicaid policy.
Over the past 40 years, Medicaid managed care
has grown in scope and sophistication, and
enrollment in comprehensive managed care plans
now accounts for nearly 70 percent of all Medicaid
beneficiaries.
1
In the modern managed care era,
state purchasers, managed care plans, public
health and health management experts, providers,
and consumers are increasingly focused on putting
purchasing strategies to work to address the whole
-person health needs of plan members. Given the
profound relationship between overall physical
and mental health on one hand and reproductive
health on the other, family planning emerges as an
essential part of such a strategy.
Furthermore, in the U.S. — which has the highest
infant and maternal morality rates among wealthy
nations, and in which nearly half of all pregnancies
are unintended
2
— planned pregnancies become a
vital tool for ensuring that women enter and go
through pregnancy and the postpartum period in
optimal health. The argument for a greater focus
on high-quality family planning as an explicit,
integrated feature of Medicaid managed care is
also supported by research showing the large
proportion of patients in publicly funded family
planning settings — a patient group
disproportionately enrolled in Medicaid — whose
exams reveal previously unidentified physical and
mental health conditions requiring referral and
follow-up care.
3
For historic reasons explored further below, the
term “family planning” as used in Medicaid is a
broad one that has evolved over time to
encompass not only routine counseling, exams,
contraceptive services, and related follow-up care,
but also certain diagnostic and treatment
procedures aimed at preventing and treating
health conditions that can affect reproductive and
overall health. As a result, this report uses the
term “family planning” to encompass the full scope
of services as this scope has evolved under federal
law in response to public health and health care
expert recommendations.
4
Three major findings emerge from this initial study
phase.
First, states treat family planning as a
fundamental element of Medicaid managed
care and expect their health plans to fully meet
their members’ needs in this regard. In doing
so, states have absorbed Medicaid’s special
family planning “freedom of choice” access
safeguard into basic managed care operations
as a core feature of their purchasing systems.
Second, despite this embrace of family
planning as a basic feature of Medicaid
managed care, significant ambiguities emerge
in how states define and operationalize family
planning services in a managed care context.
These ambiguities begin with a lack of clarity
about what is covered by the “freedom of
choice” safeguard. Ambiguities also exist
concerning other key aspects of integrating
family planning into Medicaid managed care,
including strong network and access standards,
expectations regarding the level and quality of
family planning practice, quality improvement
and performance measurement, strategies for
follow-up care for family planning patients
with additional physical and mental health
conditions, and the use of value-based
payments to encourage a high-performing
network that can reduce reliance on out-of-
network care.

The George Washington University Milken Instute School of Public Health
6
Third, the federal government similarly has a
critical opportunity to clarify and strengthen
the policy framework that guides the
integration of family planning, Medicaid
managed care, and states’ and plans’ efforts to
improve quality and accessibility. Of particular
importance is the need for greater clarity
regarding which family planning services
should be classified as family planning for
purposes of Medicaid’s special “freedom of
choice” safeguard, and guidance on strategies
to strengthen managed care performance
where family planning is concerned. An
initiative to strengthen the bonds between
managed care and family planning would
come at a crucial time, as the administration
works to restore the Title X family planning
program and the provider network on which
so many Medicaid beneficiaries depend.
A full study methodology, including all of the
tables that present the information presented in
this report in detailed form, can be found in the
Appendix, along with a list of advisors and the
states we interviewed.
Overview: Medicaid Managed Care
and Family Planning
The starting point for this initial project phase —
an in-depth examination of Medicaid managed
care purchasing agreements — reflects the
evolution of both Medicaid managed care and
family planning policy over the decades, virtually
from Medicaid’s enactment.
Medicaid managed care
The origins of what we know today as Medicaid
managed care date to the original 1965 law, which
authorized state agencies to purchase private
health insurance as a form of medical assistance
benefit.
5
Widespread adoption of managed care
began in earnest in the early 1980s with the
passage of the Omnibus Budget Reconciliation Act
of 1981 (OBRA-81).
6
Over the ensuing decades, managed care became
the Medicaid program’s operational norm,
particularly for children and adults whose eligibility
is tied to low income alone. Enrollment grew
significantly in the 1990s as a result of a series of
federal Medicaid demonstrations carried out by
the Clinton administration under Section 1115 of
the Social Security Act. The Clinton
demonstrations initially coupled expanded
eligibility for low-income working-age adults (a
precursor to the 2010 ACA Medicaid expansion)
with compulsory enrollment into managed care
plans.
7
The Balanced Budget Act of 1997 codified
mandatory Medicaid managed care as a state
option that eliminated the need for special
demonstration authority, with enrollment required
as a condition of eligibility for most beneficiaries.
8
Because of who enrolls in Medicaid — and
therefore, who is enrolled in Medicaid managed
care — any discussion of Medicaid managed care
policy also automatically becomes a discussion of
Medicaid and reproductive health policy. Seventy-
seven percent of women who are of reproductive
age and entitled to comprehensive Medicaid
coverage are also enrolled in Medicaid managed
care. This group includes women eligible under a
traditional eligibility category (very low-income
parents or caretakers of minor children, people
with disabilities, children and adolescents, and
women whose eligibility is tied to pregnancy). It
also includes women eligible as low-income adults
under the ACA Medicaid expansion.
9
(As discussed
below, certain Medicaid beneficiaries are entitled
only to limited family planning benefits and
services and generally are not enrolled in Medicaid
managed care).
The relevance of Medicaid managed care to
reproductive health is not limited to women, of
course. Millions of sexually active males — teens,
young adults, and, especially in Medicaid
expansion states, working-age men who are
fathers and sexual partners — depend on
Medicaid managed care for a full range of health
needs.
In many design and operational aspects, Medicaid
managed care parallels private health plans that
tie coverage to care through participating provider
networks. At the same time, Medicaid managed
care is distinct in the degree to which coverage is

The George Washington University Milken Instute School of Public Health
7
restricted to in-network care. In a typical private
insurance plan, an insurer incentivizes in-network
care through lower patient cost-sharing and
protections against balance billing; members can, if
they choose, seek out-of-network care, with
coverage at a higher cost-sharing rate. But cost-
sharing financial incentives of any magnitude
cannot work for impoverished populations whose
access to care is so sensitive to more than nominal
cost-sharing.
10
For this reason, Medicaid managed
care systems utilize closed provider networks
subject to strict cost controls.
At the same time, federal law recognizes three
exceptions to Medicaid’s tightly controlled network
and coverage model:
Emergency care.
Like the Affordable Care Act
protections that govern the private insurance
and health plan markets,
11
federal Medicaid law
allows an exception for hospital emergency
care using a “prudent layperson standard.”
12
Services exempted from a state’s managed care
contract
. Most states either partially or wholly
exempt certain services from their managed
care purchasing agreements, especially benefits
related to high cost, high-need health care and
care furnished in settings that may not easily fit
within a managed care model, such as
homeless shelters or schools. Managed care
plans may, in some cases, help manage access
to these services and perform third-party
claims administration functions. However,
provider network restrictions would not apply,
and members would continue to have access to
any qualified Medicaid provider without regard
to network status. By law, managed care
organizations must inform members about
services covered under the state plan but are
not included in the service agreement.
12
“Freedom of choice” for family planning
services and supplies
. As part of OBRA-81,
Congress included a special family planning
exemption to normal managed care network
and access rules. The family planning
exemption covers “family planning services and
supplies” and guarantees that plan members
can continue to receive these services from
their Medicaid-qualified provider of choice,
regardless of network status. This special
exemption, required by federal law, reflects
both a Congressional desire to promote access
to care and to accommodate managed care
participation by religiously-affiliated health
plans whose contracts might limit or exclude
covered family planning services. The OBRA-81
“freedom of choice” guarantee, a key focus of
this study, is distinct from a separate protection
added to Medicaid in 1997, which guarantees
direct access to
in-network
women’s health
care providers without the need for a referral
from their primary care provider. This later
protection (discussed further below) would
subsequently be extended to insurance plans
more generally.
Medicaid family planning benets
Family planning has been a mandatory Medicaid
service for 50 years. In the context of this study,
two aspects of the benefit are notable.
First, under federal Medicaid law, the definition of
what constitutes “family planning services and
supplies” is quite broad. Under longstanding law
dating to the original 1972 family planning
amendments,
14
certain family planning services
(examinations and related tests, contraceptives,
and counseling) qualify for enhanced federal
funding at a 90 percent federal payment rate. But
the Affordable Care Act extended and broadened
the definition of family planning also to encompass
“medical diagnosis and treatment services that are
provided pursuant to a family planning service in a
family planning setting.”
15
In implementing this expanded definition of family
planning, the Centers for Medicare and Medicaid
Services (CMS) has elected to divide the benefit
into two clusters: family planning services and
“family planning-related services.” Under CMS
guidelines, “family planning services” qualify for 90
percent federal funding, while “related” services are
paid at the regular federal medical assistance rate
(between 50 percent and 77 percent in 2021). Both
types of benefits can be covered for people

The George Washington University Milken Instute School of Public Health
8
entitled to limited Medicaid benefits for family
planning under the ACA’s special Medicaid family
planning eligibility option. As of 2021, 26 states
provide coverage for this limited benefit group.
16
Second, in the case of beneficiaries entitled to full
Medicaid benefits, the definition of family planning
benefits also can vary. For the traditional
population entitled to Medicaid prior to the ACA,
the required scope of family planning benefits
includes contraceptives whose scope would be
governed by Medicaid’s basic test of coverage
reasonableness.
17
For the ACA adult expansion
group, however, contraceptive coverage explicitly
includes all FDA-approved contraceptive
methods.
18
Furthermore, the ACA Medicaid
expansion group is entitled to “essential health
benefits” under “alternative benefit plans.” The
essential health benefit standard also explicitly
includes a bundle of services classified as “women’s
preventive health services” that includes both
benefits considered to be family planning services
and supplies as well as other benefits such as
screening for interpersonal and domestic violence,
preventive exams, and diabetes screening, as
shown in Figure 1 below.
Figure 2 shows the three basic Medicaid eligibility
pathways and how family planning benefits can
vary by pathway depending on how states
implement the family planning coverage
requirement.
Regardless of the basis of eligibility, however, it is
important to stress that the federal definition of
family planning is potentially very broad. CMS
provides guidance on which family planning
benefits qualify for 90 percent federal funding and
which are “related” and qualify for federal
payments at the regular FMAP rate and are
potentially available to the limited family planning
eligibility group. But the guidance is silent on
which family planning benefits are covered by
Medicaid’s “freedom of choice” safeguard. The
assumption appears that the safeguard extends to
those benefits recognized as such in 1981
(counseling, contraceptives, exams). The guidance
does not consider the interaction between the
“freedom of choice” safeguard and the subsequent
2010 amendment that fundamentally altered the
Figure 1. Women’s Preventive Health Services
Source: Health Resources and Services Administration (HRSA)
Screening for anxiety
Breastfeeding services and supplies
Cervical cancer screening
Screening for cervical cancer
Contraception care including counseling, initiation of contraceptive use,
counseling (all FDA-approved contraceptive methods)
Screening for diabetes both during and after pregnancy
Screening for HIV
Screening for interpersonal and domestic violence
Counseling for sexually transmitted infections
Well women preventive visits
Screening for urinary incontinence

The George Washington University Milken Instute School of Public Health
9
definition of family planning services.
Medicaid care and family planning
integraon
The breadth of family planning services and
supplies are foundational to preventive care and
can act as a key entry point into health care more
generally. This underscores the value and
desirability of integrating family planning into
comprehensive managed care systems as part of a
“whole person” health strategy improvement
strategy. A strong orientation toward integration
would emphasize a wide choice of family planning
network providers and a comprehensive range of
family planning services to encourage early
detection of conditions affecting overall
reproductive health. Inclusiveness also would
emphasize performance standards that include
special accessibility efforts reaching all qualified
providers in medically underserved communities,
Figure 2. Principal Medicaid Eligibility Pathways and Family Planning Coverage Variaon
Eligibility Pathways Family Planning Coverage
“Traditional” beneficiaries:
Low-income children
Very poor parents and caretaker
relatives
Children and adults with disabilities
Pregnant/postpartum women
Family planning services and supplies. Federal guidelines that
identify which services qualify for 90 percent federal funding
define the term as consisting of counseling services and
patient education; examination and treatment; laboratory
examinations and tests; medically approved methods,
procedures, and devices to prevent conception; and certain
infertility services. Medically necessary diagnosis and
treatment services for conditions found in a family planning
visit typically would be covered under the state plan rather
than as a family planning service.
ACA expansion beneficiaries:
Low-income, non-elderly adults with
household incomes up to 138% FPL
All essential health benefits, including all FDA-approved
contraceptive methods, as well as a broad package of
women’s preventive health services — which may extend be-
yond the Medicaid definition of family planning and related
services both in scope and the range of services furnished in a
family planning setting (e.g., screening for anxiety and
depression).
Beneficiaries eligible for family
planning and family planning-related
coverage:
Incomes between 138% FPL and
states’ upper-income limit for
pregnant women
Family planning services and supplies — defined as including
not only contraceptives, tests, and counseling, but medically
necessary diagnosis and treatment for conditions disclosed
during a family planning visit and furnished in a family
planning setting.

The George Washington University Milken Instute School of Public Health
10
especially those that offer special programs for
hard-to-reach populations such as immigrants,
adolescents, or patients with disabilities or
underlying behavioral health conditions. In other
words, effectively integrating family planning into
Medicaid managed care raises a host of important
considerations when designing effective systems
for a diverse and vulnerable population that go
beyond simply covering and paying for family
planning services but orienting managed care
systems to reach members with complex needs,
and to focus special attention on issues such as
confidentiality and patient supports. Integration
also means incorporating evidence-based practice
standards as a network expectation, adopting value
-based payment strategies to attract and retain a
high-performing network, and developing
performance measures that can capture certain
outcomes, as well as evidence of basic procedures
such as cervical cancer screening for adults
19
and
chlamydia screening for adolescent women ages
16-20.
20
Models of managed care/family planning
integration.
The complexity of integration means
that managed care and family planning integration
can be thought of as happening along a spectrum,
from limited integration to comprehensive
integration and prioritization. Under limited
integration that mainly relies on the “freedom of
choice” safeguard to promote access to care,
family planning might be covered. Still, only a
modest focus would be given to aspects of
managed care such as networks, access,
performance standards, payment incentives, links
between family planning network providers and
social services, and quality measurement and
performance improvement. Plans essentially would
emphasize their role as claims managers, and
members would seek care from their provider of
choice. Family planning would exist as a covered
Limited Comprehensive
Family planning benefits are covered but
broadly defined
Services covered by the “freedom of choice”
exemptions are not defined
Contract does not specify family planning-
focused access or network specifications
Contract does not specify specific expectations
regarding referrals between out-of-network
family planning providers and in-network care
Contract does not incorporate social
determinants expectations specifically into
family planning services
Contract does not specify family planning-
related performance expectations or quality
improvement goals
Family planning is specified in detail with
coverage spanning the full range of federally-
permissible services
Services covered by the “freedom of choice”
exemption are defined
Contract specifies detailed access and network
expectations
Contract specifies referral arrangements for
follow-up care
Contract specifies a focus on family planning
patients with social determinants needs
Contract specifies family planning performance
expectations and quality improvement goals
Figure 3. Models of Family Planning/Managed Care Integraon

The George Washington University Milken Instute School of Public Health
11
benefit but not one subject to robust coverage,
access, or performance specifications.
In a more robust integration model, the contract
would lay out more detailed specifications
governing coverage and performance to elevate
the importance of family planning access, quality,
and performance as a major focus of managed
care patient and population health improvement.
The contract would be more specific regarding
networks, coverage, performance expectation,
referral systems, linkages between family planning
and social services, and other matters. Payment
incentives would be in place for plans and provider
networks that achieve high performance as defined
by evidence-based practice standards, such as
providing same-day walk-in care, the “quick start”
family planning method, and other strategies
designed to make family planning simple and easy
to access.
The basic features of what might be thought of as
two distinct models for approaching managed care
and family planning are shown above in Figure 3.
Study Aims and Assumpons
This two-phase study has been designed to better
understand the issues in family planning and
Medicaid managed care integration and how states
currently approach these issues. The first study
phase, whose results are presented here, offers a
baseline assessment of issues and state
approaches through an in-depth review of
managed care purchasing agreements coupled
with in-depth discussions with state Medicaid
leaders.
As with our previous work in the field of managed
care policy and practice, we assume that there is
no correct answer to the question of “how much”
or “to what extent” to integrate managed care and
family planning — and how robustly and with what
level of focus. On-the-ground health care
conditions, public health, and policy priorities,
consumer preferences, other considerations
strongly influence how states shape and design
their managed care systems and the priorities they
choose.
At the same time, we also believe that much is to
be gained from a focus on greater managed care
and family planning integration in terms of quality,
efficiency, and the promotion of reproductive and
overall patient and population health.
Furthermore, because real-world considerations
play such an important role in Medicaid managed
care design and operationalization, the 1981
“freedom of choice” exemption remains as
important today as it was when it was originally
enacted, since the exemption assures that states
and health plans can adjust their activities and
areas of emphasis without compromising access to
this essential benefit.
Finally, we assume that because an understanding
of, and experience with, both family planning
practice and the field of Medicaid managed care
has changed dramatically over the past four
decades; we believe that a deep dive into the
family planning/managed care integration
question will add value to health care practice and
policy.
Study Overview
This study phase presents findings from our
baseline study, which involved a detailed analysis
of state Medicaid managed care purchasing
agreements coupled with discussions with senior
Medicaid officials in ten states. This baseline is
intended to help illuminate what can be thought of
as the managed care “blueprint” in all states: the
major purchasing agreements on which all
Medicaid managed care systems sit.
21
Medicaid managed care contracting is challenging
for an impoverished, high-need population
because the act of purchasing goes far beyond the
concerns involved in purchasing typical private
health plans. In light of the concentration of
Medicaid beneficiaries with complex needs in poor
rural and urban communities with extensive
medical underservice problems, network
sufficiency and capability considerations rise to the
forefront, as do access concerns. Coverage must be
well-defined to capture the full range of covered
services included in the contract. Utilization
management approaches must be tailored to a

The George Washington University Milken Instute School of Public Health
12
member population with elevated health and social
needs. Relationships with social service and other
providers must be in place. Quality improvement
priorities must be tailored to a member population
with complex needs. Federal managed care
requirements must be satisfied along with state
laws governing large-scale procurements.
Thus, managed care can vary enormously from
state to state depending on population need, on-
the-ground health care conditions, legal
considerations, policy priorities among state
lawmakers, advocates, and health professionals,
procurement laws, and the customs and practices
of the managed care industry itself. Along with
this variation in approaches to Medicaid managed
care comes variation in state purchasing
agreements. Some states may broadly word their
agreements and supplement general agreements
with more detailed guidance documents, while
other states might take a granular approach to
their agreements, filling them with detail. Some
states may use a procurement approach that
begins with a procurement announcement and
then incorporates acceptance of plan responses to
a standard set of terms and conditions, meaning
that the contractor’s response guides the detail.
Despite these differences, federal law treats
Medicaid contracts as the foundation of state
systems, and our studies of Medicaid managed
care contracts over nearly three decades
underscore the degree to which all states use
purchasing agreements to signal areas of high-
priority interest and focus. A state’s priorities might
result from the on-the-ground public health
conditions or health care realities (particularly, the
concentration of Medicaid beneficiaries in low-
income urban and rural communities at risk for
health and social risks coupled with a shortage of
primary care services). State priorities might also
reflect gubernatorial or legislative initiatives.
Moreover, because the purchase of health care is
so complex, any managed care contract is a mix of
the specific and the general. That is, in any state,
the contract will reflect areas of high specificity
where a state desires a specific approach or a
specific result, and the other issues are left
substantially to contractor discretion in accordance
with prevailing industry practice.
In sum, despite certain limitations, Medicaid
managed care purchasing documents play a
central role in state systems and offer a means of
gaining an overall picture of states’ health system
approaches and priorities.
Appendix 2 provides a fuller explanation of our
methods. In brief, this study involved collecting
public purchasing documents from the 39 states
and the District of Columbia in which
comprehensive managed care was in use in 2020.
These documents were reviewed using an
instrument designed to capture each document’s
framework in detail through a series of six
domains, each with numerous sub-topics (shown in
Figure 4). Each domain and sub-topic are relevant
in assessing the extent to which state purchasing
agreements contain express specifications aimed at
translating family planning practice and policy for
medically underserved populations into their
managed care purchasing blueprints. In developing
these domains and sub-topics, we were guided by
comprehensive family planning guidelines
developed by the Centers for Disease Control and
Prevention (CDC) and the Office of Population
Affairs (OPA), federal Medicaid policy
considerations, and project advisors (listed in
Appendix 3) whose expertise spans Medicaid
policy, family planning policy and practice,
managed care, and primary care practice and
policy.
Once the domains and sub-topics were finalized
and converted into a review instrument, a team
trained and experienced in analyzing Medicaid
managed care purchasing documents reviewed all
state agreements and prepared the detailed
master tables found in Appendix 1. These tables
provide two levels of information: 1) an overview of
the degree to which documents do or do not
contain family planning-specific provisions
addressing a particular domain or subtopic; and 2)
the actual language contained in each state
document relevant to that domain or subtopic,
which gives users the ability to compare precisely

The George Washington University Milken Instute School of Public Health
13
Figure 4. Managed Care and Family Planning: Study Domains and Sub-Topics
Domain 1. Coverage
Identifies family planning as a covered benefit
Coverage is explicit on coverage of all FDA-approved family planning methods
Coverage of family planning services and supplies is coextensive with the coverage provided by the state Medicaid
plan
Coverage of family planning as a postpartum benefit is required
Family planning-related services are defined
Quick start contraception
1
is required as a contract service
Domain 2. Access and Provider Networks
Coverage of out-of-network family planning services regardless of network status
Coverage of family planning-related services regardless of network status and without prior authorization
Network contracts offered to all Medicaid-qualified family planning providers in the plan service area
Bars against the use of prior authorization or other utilization management methods for family planning services
Incentives for same day walk-in care
Maximum wait times for family planning visits
Maximum travel time for family planning visits
Family planning provider/patient ratios
Telehealth family planning visits
Non-emergency transportation for family planning
Domain 3. Information for Plan Members
Contractors required to inform members of free choice of family planning providers
Contractors required to inform female members of their right to direct access to in-network women’s health
specialists without prior authorization
Contractors required to inform members of any family planning services covered under the state plan but not
include in the contract
Contractors required to inform members about relevant family planning confidentiality considerations
Contractors barred from disclosing family planning visit information in members explanation of benefits
Domain 4. Payment Incentives
Requirement for payment add-on or incentives for family planning drugs and devices furnished incident to a family
planning visit
Separate payment for postpartum long-acting reversible contraceptives (LARCs; i.e., IUDs, contraceptive implants)
Value-based payments for family planning services
Domain 5. Social Determinants of Health
Family planning patients identified as a prioritized population for social risk health screening
Referral arrangements required between family planning providers and social service agencies
Domain 6. Quality Improvement and Performance Measurement
Family planning and family planning-related-specific performance measures
Family planning performance measures as part of maternity care
Specifies one or more family planning health outcome measures
Adolescent performance measures for family planning specified
1
“Quick starting” is a the term used to describe immediate initiation of a contraceptive method at the time a woman requests it, rather than waiting for
the start of the next natural menstrual period.

The George Washington University Milken Instute School of Public Health
14
how different states may address a topic. In the
context of purchasing agreements, these details
matter in framing the scope of state expectations
and the degree of discretion afforded to plan
contractors.
Findings
Our review of state Medicaid plans — the
foundation on which managed care contracts rest
— results in two key findings.
First, our review suggests that in contracting for
managed care, while all states view family planning
as a foundational service, states tend not to elevate
family planning as a major area of focus in terms of
coverage and performance specificity. Indeed,
contract documents tend to leave plans with broad
discretion to define the full scope of what
constitutes family planning coverage itself,
including the types of coverage that should be
covered by the “freedom of choice” exemption. Of
course, there are notable exceptions, but overall,
family planning is a basic expectation but not one
that merits extensive specification or emphasis as a
performance priority.
Second, while the selection of key areas of focus is
principally a matter of state leadership and choices,
the federal government’s silence on managed care
and family planning is also quite notable. For
example, the federal government has been a leader
in the development and publication of landmark
guidelines on high-quality family planning services.
CMS has launched an effort to develop more
robust measures of managed care family planning
performance. But in other critical respects, CMS
activities have been limited. For example, CMS has
never developed detailed guidance on how states
might translate the CDC/OPA guidelines into a
managed care operating environment. Nor does
CMS maintain guidelines regarding the range of
considerations that go into Medicaid managed
care and family planning integration or how to
align managed care coverage and performance
with the “freedom of choice” exemption.
Indeed, even basic CMS documents — such as the
preprinted document states use to describe their
state plan coverage — are ambiguous and unclear.
As a result, it is not possible from the preprints to
know the full scope of state coverage of family
planning, including which benefits and services
identified in federal law are classified as a family
planning benefit and which benefits are covered by
the “freedom of choice exemption.”
22
Two states
plans specify unequivocally (Ohio and New Jersey)
that as a basic state plan matter, all comprehensive
coverage beneficiaries are entitled to all FDA-
approved contraceptive methods regardless of
their basis of eligibility. Other state plans are
ambiguous, and this ambiguity carries through to
the purchasing itself.
In sum, an important consideration in most states’
decisions to elevate family planning as a focus of
managed care priority may be that except for an
effort to develop more refined quality measures,
managed care and family planning are not a focus
for CMS either.
Summary ndings from the Medicaid
managed care contract review
Figures 5 through 10 present summary findings
from our contract review of public purchasing
documents from the 39 states and the District of
Columbia utilizing comprehensive managed care in
2020. The tables referred to in each of these
figures can be found in Appendix 1.
Coverage
As Figure 5 shows, family planning is a basic
offering of all state managed care agreements. In
other words, no states, in response to the “freedom
of choice” guarantee, has elected to simply exempt
family planning services and supplies from its
managed care system. States assume (confirmed
by our discussions with state officials) that family
planning is a basic feature of their managed care
systems. Eight states explicitly include language on
coverage of all FDA-approved family planning
methods. Figure 5 also shows that 12 state
agreements specify that contractor coverage of
family planning services must be coextensive with
the state plan, presumably eliminating contractor
discretion to define coverage scope.

The George Washington University Milken Instute School of Public Health
15
Nine states specify family planning as a pregnancy-
related postpartum service. No states specify what
is meant by coverage of family planning-related
services. No states specify coverage of quick-start
contraception, which permits coverage in the
absence of an initial exam.
Access to coverage and provider networks
Figure 6A shows that 18 states specify that
contractors must pay for all family planning
services when furnished by a qualified Medicaid
provider, regardless of the provider’s network
status. Twenty-six states bar use of prior
authorization or other utilization management
techniques in the case of family planning services.
Figure 6A also shows that although states do not
specify what constitutes family planning-related
services in a coverage context, four states specify
that contractors must pay for family planning-
related services when furnished by a Medicaid
provider, regardless of network status and without
prior authorization. Six states specify that
contractors must offer network contracts to all
qualified Medicaid providers in their plan service
area.
Figure 6B reports on family planning-specific
versions of general access measures such as travel
times, wait times, and provider/patient ratios. With
respect to rapid access, six states require or specify
incentives to create same-day walk-in access. Six
states reference maximum wait times for in-
network family planning services, 19 reference
travel times, four reference provider/patient ratios,
six specify the use of telehealth services, and 31
states specify non-emergency transportation for
family planning visits.
Information for plan members
As seen in Figure 7, 11 states specify that
contractors must inform members of their right to
family planning services from the qualified provider
of their choice and without regard to network
status or prior authorization. Fifteen states
expressly require that contractors inform members
of their right to directly access any in-network
women’s health specialist for routine preventive
care, a specific information guarantee under
federal law.
Fourteen states require plans to inform members
regarding the full scope of family planning
coverage under the state plan (which may differ
from what the contractor offers) and where and
how to obtain services not covered under the
contract. Among these 14 states, five states
specifically stipulate that enrollees must be
informed about how to access covered services
that the contractor has objected to on moral or
religious grounds. However, no contract appeared
to require contractors to identify religiously
affiliated providers within their network.
No states specifies that contractors are required to
inform members about their rights regarding
family planning and provider-patient
confidentiality. One state bars contractors from
including identifiable information about a family
planning visit in the explanation of benefits (EOB)
sent to members.
Payment and payment incentives
As Figure 8 shows, one state specifies additional
payment to providers for drugs and devices
furnished during an office-based family planning
visit. In contrast, two states require contractors to
make separate payments for hospital-inserted
LARCs. Five states encourage the use of value-
based payment models for either office-based or
hospital-based family planning services.
Social determinants of health
Figure 9 reports that no state identifies family
planning patients as a specific priority population
for social and health risk screening, while one state
requires contractors to maintain referral
relationships between their in-network providers
and social service agencies.
Quality improvement and performance
measurement
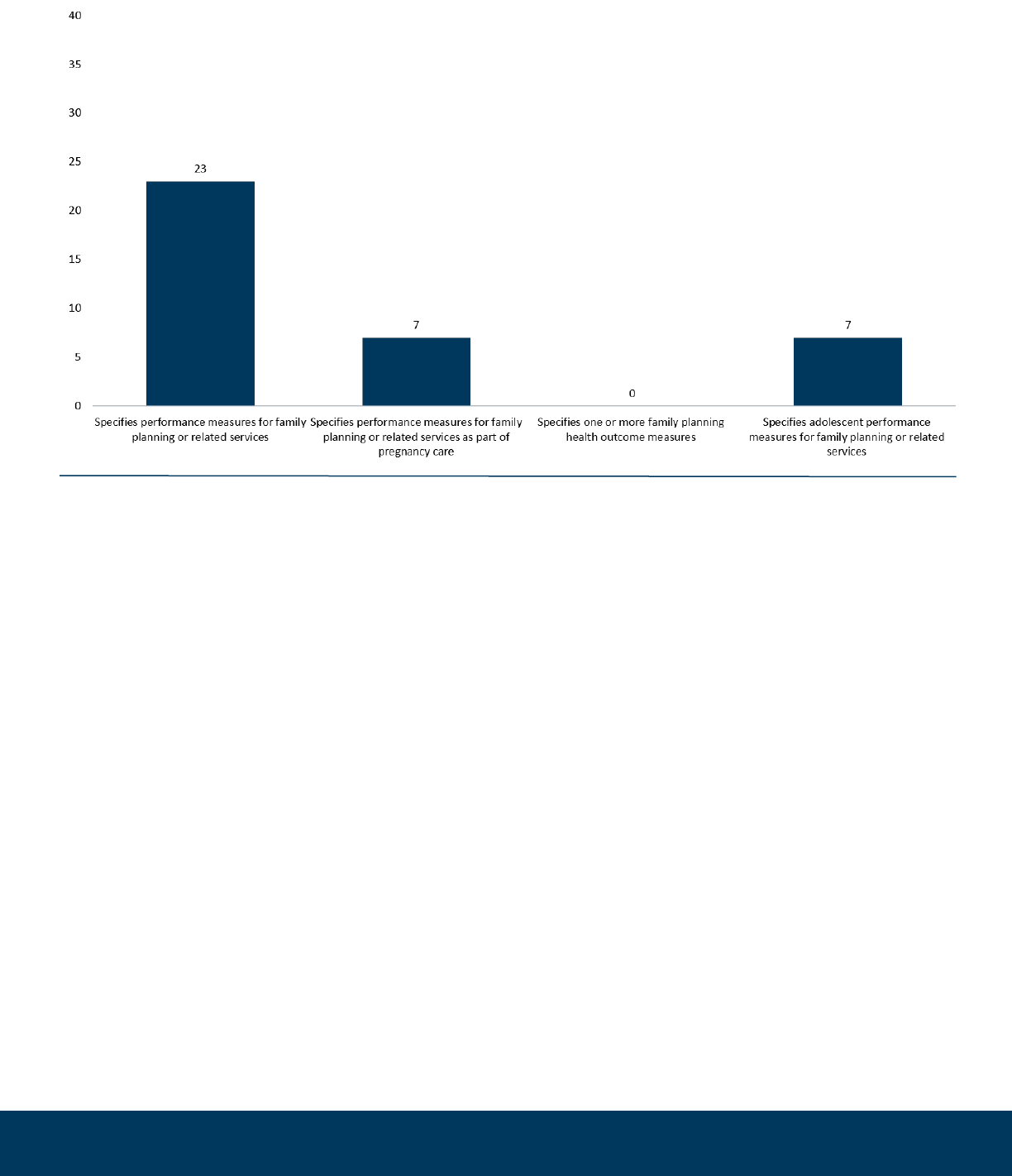
Last, Figure 10 shows that 23 states specify
performance measures for family planning or
family planning-related services. In many cases,
state measures focus on family planning-related
services, such as cervical cancer screening or
chlamydia screening. Seven states specify family

The George Washington University Milken Instute School of Public Health
16
planning as a pregnancy-related performance
measure, and seven states specify family planning
performance as a measure of adolescent health.
No states specifies a family planning health
outcome measure.
State variaon in contract terms: a closer
look
These summary findings provide a high-level
overview of the extent to which state purchasing
documents, as a group, contain coverage, access,
network, quality, payment, and performance
provisions specific to family planning. But within
these high-level patterns, important differences
can be seen in the precise approach that any two
or more states might take to the same topic or
focus area. As we have noted in our previous
Medicaid managed care research,
23
empirical
evidence does not exist that would suggest that
one approach to drafting achieves better
outcomes; contracts that vest plans with discretion
as to whether to cover and furnish certain services
and, if so, to what extent, may achieve results that
do not differ from contracting approaches that are
more directive.
But for standard setting and accountability
reasons, states and plans typically agree to specific
performance expectations regarding coverage,
care, payment, quality improvement, consumer
safeguards, and other matters. Indeed, one of the
most important decisions states and plans make is
how to balance deference against clarity. Many
considerations may enter into this equation, such
as whether on-the-ground conditions make the
realization of the standard feasible, and
considerations of cost and efficiency. For this
reason, this variation in coverage and deference is
a signature characteristic of state contracting
practices around any particular topic. For example,
a specification that defines contractor coverage
obligations as “appropriate family planning
services” would signal to contractors the flexibility
to set parameters on coverage that may differ from
all FDA-approved contraceptive methods or even
the level of coverage afforded by the underlying
state Medicaid plan.
Silence on a particular matter signals a policy
judgment in its own right. For example, a contract
may be silent on the use of telehealth services. This
does not mean that telehealth services might not
be available under plans’ operating standards, but
instead that whether to use telehealth services and
under which conditions is left to contractor
discretion.
Drawing from the tables in Appendix 1, we offer
several comparisons to illustrate this basic point
about how contracts are drafted.
I. Coverage of Family Planning Services
As discussed, federal law gives states considerable
discretion to define the term “family planning
services and supplies.” A state’s definition would
be relevant not only as an expression of the state’s
policy regarding what a high-quality family
planning service should encompass but also
because the definition would play a key role in
defining the scope of the state’s “freedom of
choice guarantee.”
Nevada uses a succinct definition:
Vendor Covered Services … At a minimum, the
Vendor must provide directly, or by subcontract, all
covered medically necessary services, which shall
include, but may not be limited to, the following:
4.2.2.13 Family Planning Services.
South Carolina uses a more extensive definition:
4.2.12. Family Planning Services—Family Planning
Services include traditional contraceptive drugs,
supplies, and preventive contraceptive methods.
These include, but are not limited to the following:
(1) examinations, (2) assessments, (3) diagnostic
procedures, and (4) health education, prevention
and counseling services related to alternative birth
control and prevention as prescribed and rendered
by various Providers.
Under both state definitions, contractors
presumably would have the latitude to determine
when certain services are furnished in a family
planning setting and pursuant to a family planning
visit (such as the HPV vaccine or diagnosis).

The George Washington University Milken Instute School of Public Health
17
Figure 5. Summary Findings from Table 1: Coverage
Figure 6A. Summary Findings from Table 2: Access to Coverage and Provider Networks

The George Washington University Milken Instute School of Public Health
18
Figure 6B. Summary Findings: Access to Coverage and Provider Networks
Figure 7. Summary Findings from Table 3: Informaon for Plan Members

The George Washington University Milken Instute School of Public Health
19
Figure 8. Summary Findings from Table 4: Payment Incenves
Figure 9. Summary Findings from Table 5: Social Determinants of Health
The George Washington University Milken Instute School of Public Health
20
Arizona’s contract defines the postpartum family
planning duty as follows:
The Contractor must monitor rates and implement
interventions to improve or sustain rates for low/
very low birth weight deliveries, utilization of long
acting reversible contraceptives (LARC), prenatal
and postpartum visit.
Louisiana defines the postpartum coverage
obligation as follows:
The MCO shall provide pregnancy-related services
that are necessary for the health of the pregnant
woman and fetus, or that have become necessary
as a result of being pregnant and includes but is
not limited to prenatal care, delivery, postpartum
care, and family planning services for pregnant
women.
Arizona’s contract is drafted in a way that
approaches postpartum family planning as an
intervention that arises out of patient monitoring
post-delivery, with the intervention seemingly
required if monitoring suggests the need for such
an intervention. Louisiana, by contrast, specifies
family planning as part of the pregnancy bundle,
not conditioned on the results of member or
patient monitoring. Arizona’s drafting would
support contractor accountability in terms of
provision of the intervention in the wake of
evidence, as defined by the contractor, that is
gained from monitoring. Louisiana sets a
performance expectation of family planning as a
basic element of postpartum coverage.
II. Access to Family Planning-Related Services
from Out-of-Network Providers
Although the contracts lack specific coverage
terms regarding what must be covered out-of-
network, four states set standards in terms of
access. California addresses the issue of out-of-
network coverage in some depth, while
Pennsylvania offers a general minimum and thus
would rely on contractor discretion.
California’s contract providers as follows:
Out of network family planning services. Members
of childbearing age may access the following
services from out-of-network family planning
providers to temporarily or permanently delay
pregnancy: (a) health education and counseling. . . ;
Figure 10: Summary Findings from Table 6: Quality Improvement & Performance

The George Washington University Milken Instute School of Public Health
21
b) limited history and physical examination. . . . c)
laboratory tests if medically indicated. Contractor
shall not be required to use out of network
provider for pap smears if contractor has provided
pap smears to meet U.S. Preventive Services Task
Force guidelines . . . . d) diagnosis and treatment of
a sexually transmitted disease episode . . . . e)
screening testing and counseling of at risk
individuals for HIV and referral for treatment. . . . f)
follow-up care for complications associated with
contraceptive methods. . . . g) provision of
contraceptive pills, devices and supplies . . . . h)
tubal ligation. . . . i) vasectomies; j) pregnancy
testing and counseling.
Compare this language with an excerpt from
Pennsylvania:
The PHO-MCO may not use either the referral
process or Prior Authorization to manage the
utilization of family planning services. . . . Members
may access at a minimum, health education and
counseling. . . ., pregnancy testing and counseling,
breast cancer screening services, basic
contraceptive supplies such as oral birth control
pills, diaphragms, foams, creams, jellies, condoms
(male and female), Norplant, injectables,
intrauterine devices, and other family planning
procedures.
[Bold emphasis added.]
Whereas California presents contractors with a
defined list, Pennsylvania gives contractors the
discretion to add to the minimum list or elect to
not do so.
III. Performance Measurement
Performance measures are not without
controversy; nevertheless, the development of
more robust family planning performance
measures has been a recent focus within CMS. As
of 2018, four contraceptive measures were
available in the CMS Maternal and Perinatal Health
Measures Core Set for voluntary reporting by state
Medicaid agencies. These measures include 1)
Contraceptive Care among Postpartum Women
Ages 15 to 20, 2) Contraceptive Care among
Postpartum Women Ages 21 to 44, 3)
Contraceptive Care among All Women Ages 15 to
20, and 4) Contraceptive Care among All Women
Ages 21 to 44.
24
This set seeks to measure the
percent of women at risk of unintended pregnancy
who were provided with a “most effective or
moderately effective” FDA-approved method of
contraception, such as LARCs.
25
Seven states currently include at least one of these
CMS contraceptive core measures in their Medicaid
managed care contracts: Arizona, Florida, New
Jersey, Louisiana, New Mexico, and Oklahoma.
Louisiana, for example, has included the two CMS
Contraceptive Care among Postpartum Women
core measures — making the state one that
establishes a clear link between a specific
expectation of postpartum family planning
coverage and a specific measure of performance:
Contraceptive Care-Postpartum (ages 15-20)
Measure Description: The percentage of women
ages 15-20 who had a live birth and were provided
a most or moderately effective method of
contraception within 3 and 60 days of delivery.
Four rates are reported. Contraceptive Care-
Postpartum (ages 21-44) Measure Description: The
percentage of women ages 21-44 who had a live
birth and were provided a most or moderately
effective method of contraception within 3 and 60
days of delivery. Four rates are reported.
A few states included contraceptive measures
which were distinct from the CMS contraceptive
core set. For example, Georgia has attempted to
capture the outcomes of its Planning 4 Healthy
Babies Program, a special demonstration
embedded in its managed care system:
Planning 4 Healthy Babies Program Objectives […]
Improve access to family planning services by
extending eligibility for family planning services to
all women aged 18 – 44 years who are at or below
200% of the federal poverty level (FPL) during the
three year term of the Demonstration.
Achievement of this objective will be measured by:
Total family planning visits pre and post the
Demonstration; Use of contraceptive services/
supplies pre and post the Demonstration; Provide
access to inter-pregnancy primary care health
services for eligible women who have previously
delivered a very low birth weight infant.
Achievement of this objective will be measured by:

The George Washington University Milken Instute School of Public Health
22
Use of inter-pregnancy care services (primary care
and Resource Mothers Outreach) by women with a
very low birth weight delivery; Decrease
unintended and high-risk pregnancies among
Medicaid eligible women and increase child
spacing intervals through effective contraceptive
use to foster reduced low birth weight rates and
improved health status of women. Achievement of
this objective will be measured by: Average inter-
pregnancy intervals for women pre and post the
Demonstration; Average inter-pregnancy intervals
for women with a very low birth weight delivery
pre and post the Demonstration; Decrease in late
teen pregnancies by reducing the number of
repeat teen births among Medicaid eligible
women. Achievement of this objective will be
documented by: The number of repeat teen births
assessed annually; Decrease the number of
Medicaid-paid deliveries beginning in the second
year of the Demonstration, thereby reducing
annual pregnancy-related expenditures.
Achievement of this objective will be measured by:
The number of Medicaid paid deliveries assessed
annually; Increase consistent use of contraceptive
methods by incorporating Care Coordination and
patient-directed counseling into family planning
visits. Achievement of this objective will be
measured by: Utilization statistics for family
planning methods or Number of Deliveries to
P4HB participants.
Discussions with state Medicaid ocials
Upon completion of our contract review, we held a
series of 10 discussions with senior Medicaid
officials to learn more about their thinking
regarding the relationship between Medicaid
managed care and family planning generally and
their approaches to family planning through
managed care purchasing. See Appendix 4 for a
full list of the 10 states with whom discussions
were held. (Note: Interviews with plans and
providers will take place during Phase 2 of this
study.) From these discussions, several key themes
emerged:
Family planning is part of the “routine operation,”
“basic general care,” and “integrated care” that
managed care plans are expected to provide.
All
discussants viewed family planning as part of their
state’s core Medicaid managed care operation, not
one that stands apart. While the “freedom of
choice” provision stands as a key access safeguard,
the existence of this provision did not cause
agencies to either think about or treat family
planning as somehow separate from their overall
health care purchasing strategy. Indeed, officials in
one state view the safeguard as the basis for a
requirement that their contractors not only pay
providers for out-of-network care but have
working two-way referral arrangements with all
Medicaid participating family planning programs in
their service areas. In other words, the presence of
out-of-network coverage protection is in and of
itself the basis for an operational expectation.
In states that have prioritized family planning as a
service to receive a higher level of attention, this
prioritization can be traced to individual leadership.
All agencies recognize the importance of family
planning as a matter of both patient and
population health. The decision to elevate family
planning contractually — through greater clarity
and specificity of expectations — is the result,
officials say, of deliberate leadership decisions by
agency officials, public health officials, and other
state leaders concerned about both individual and
population health and its link to the timing and
spacing of pregnancy. In one state, this decision to
move more aggressively on family planning came
from the realization that the state’s unintended
pregnancy rates were too high. Another state
decided to make performance improvement in its
hospitals (in the case of postpartum family
planning) and community health centers a policy
and strategic planning priority and intends to use
its comprehensive health system reform
demonstration renewal as a tool for focusing on
this issue. Other states indicated that the focus on
family planning was part of a broader initiative —
for example, an effort to make well-woman’s health
care a major priority in Medicaid managed care or
to bring a family planning focus into initiatives
around pregnancy care.

The George Washington University Milken Instute School of Public Health
23
Agencies view family planning and the “freedom of
choice” exemption as an issue that has been
operationalized with relative ease
. All Medicaid
agencies, health plans, and providers face
challenges in operationalizing aspects of health
system delivery reform. The agency officials we
spoke with viewed family planning operations as
smooth and with few hiccups. Those officials who
were familiar with problems noted that they were
manageable (e.g., payment rate adjustments,
additional payment for postpartum LARC
unbundled from the hospital delivery rate, ensuring
that MCOs fully understand and embrace family
planning as a focus of state interest, limited
member take-up of certain types of long-acting
contraceptives). From the agencies’ perspective,
issues in family planning are considered readily
identifiable, and their resolution has clear answers.
Whatever problems arise are ones that can be
addressed. Although contracts may not specify
coverage of all family planning methods, no state
has heard from providers that a method is being
denied coverage.
Agencies struggle with which issues to prioritize
and when to translate priorities into clear
contractual expectations.
All agencies focused to a
greater or lesser degree on the tension between
the scope of the undertaking they face (that is,
buying health care for entire populations), when to
make a particular population or service a major
priority, and when to set clear expectations that
effectively are intended to move all contractors in
the same direction on a matter of overarching
importance. In other words, the question of when
to set general directions and allow contractors to
exercise judgment and innovation, and when to
choose a strategy or a standard and expect
uniform adaptation, is one of the most difficult
questions that agencies confront — whether in the
area of primary and preventive care or care for
complex health conditions. Indeed, as one agency
told us, the point of managed care is to get the
benefit of contractor expertise and the flexibility
that comes with capitation and allows contractors
to test approaches that are not possible in a fee-
for-service context. This uncertainty over when to
add or strengthen priorities also carries over into
decisions about updating and adding performance
expectations. Contracts are often for multi-year
terms, and states may frequently update or alter
terms and payment structures. In other words,
whether to modify expectations or requirements
for contractors does not arise only when new
contracts are established but is a continuous
matter.
Agencies are varied on the issue of networks.
The
in-network/out-of-network dichotomy appears to
play out differently for different states. Some
reported a deliberate strategy aimed at enlarging
their managed care family planning networks as a
means of bolstering the role of their health plans
as comprehensive systems of care and ensuring
network adequacy. Other states did not perceive
networks as an issue, expressing the sense that the
“freedom of choice” provision eases this concern
and effectively allows both providers and member
to make their own decisions. This view was perhaps
best expressed by one state official who indicated
the sense that “most state family planning
providers have in-network contracts with at least
one plan.” Still, for the agencies, the issue of in-
network or out-of-network did not raise concerns.
While states indicated their desire that plans make
a reasonable effort to enroll family planning
providers, it was evident in the discussions that
ensuring in-network access did not register as a
matter of urgency. Thus, there was no pressure in
their view to “dictate” network design to their
plans, as one agency official put it.
States are relatively split on their plans as claims
administrators for out-of-network providers.
Some
use plans as claims administrators for all family
planning services regardless of network status,
while others do not. Those who do not use plans as
claims administrators noted minimal problems, and
if problems did arise (e.g., confusion over the
payer), they were resolved with relative ease.
However, one state was concerned that requiring
family planning providers to bill multiple plans may
be placing too much of a burden on them.
States are split on the use of some level of
utilization management for family planning
services.
Several states prohibit pre-approval or

The George Washington University Milken Instute School of Public Health
24
other forms of utilization management, while
others do not. Those whose contracts do not bar
utilization management varied in their approaches.
One state actively supported utilization
management as an activity it hopes its contractors
do as appropriate for all services. Other officials
required that the use of utilization management for
family planning services would need to be “run by”
the state agency, indicating a process of informal
oversight of utilization control policies in this area.
Family planning-specific access requirements are
not perceived as necessary.
In keeping with
agencies’ relatively relaxed attitudes about network
composition and adequacy, officials also indicated
that they do not perceive the need for family
planning-specific access measures because they do
not perceive access to family planning services as a
problem. It is worth noting that during the period
in which these interviews were conducted, the 2019
Title X Family Planning Rule was in full effect.
Studies suggest that the rule had a notable impact
on family planning program participation.
26
To the
extent that patients and members were
experiencing access problems as capacity dropped,
this development did not appear to translate into
an area of concern for agency officials. It is
conceivable, of course, that because of the
“freedom of choice” guarantee, the need to ensure
strong provider networks is simply far less in the
view of Medicaid officials because managed care
does not act as an interrupter of care patterns of
pre-existing service accessibility. Simply put, the
“freedom of choice” guarantee acts as a braking
mechanism, alleviating the network adequacy
pressures state Medicaid programs and plans face
for other contract services that lack an out-of-
network exemption. Put another way; the out-of-
network safeguard lessens the need to “own” the
issue.
At least some agencies are focused on the rise of
religious providers that may resist family planning
as a priority activity.
Several agencies noted the
increase in religiously affiliated plans and
providers, which underscores the importance of
the “freedom of choice” guarantee. It is also an
issue that may, in some communities, complicate
comprehensive efforts to focus on elevating family
planning improvements as a managed care priority.
At least one state also noted the difficulty in
elevating these issues in legislative policy and
suggested that the most effective approach was to
incorporate family planning into larger initiatives.
Despite the absence of perceived pressing
problems, agencies recognize the importance of
family planning and express strong interest in
strategies for performance improvement.
Although
family planning emerged as an area relatively free
of pressing problems for state officials, all states
appreciated the importance of strong and effective
family planning services and appreciated the
significance and value of high-performance
systems where family planning is concerned, and
understood clearly that managed care offers a
major tool for improving family planning. Of
particular interest, generally, was overall plan
performance improvement. One state was
particularly focused on increasing the quality of
performance by key in-network providers such as
hospitals and community health centers that play
such a major role in delivering care to members
but whose family planning performance may need
strengthening. Indirectly, at least, this interest in
plan performance improvement despite the
absence of evidence of major problems
underscores that states are interested in improving
managed care not only in response to a “house-on
-fire” emergency but as a general matter. In other
words, the absence of critical problems in the
experience of state officials is a matter separate
and apart from the question of how to improve
and strengthen the quality and accessibility of a
service so fundamental to patient and population
health.
Discussion
The interim findings from this project suggest two
key areas of focus ongoing forward.
1) The need for greater federal policy clarity
regarding family planning and managed care
integration and how to align the family
planning “freedom of choice” exemption with
managed care principles and practice.

The George Washington University Milken Instute School of Public Health
25
One of the most striking aspects of this research
has to do with the confusing nature of federal
policy guidance and the uncertainty about what
falls within the definition of family planning
services and supplies. Some may posit that the
distinction of what is or is not a family planning
service carries little meaning for beneficiaries
entitled to comprehensive benefits since Medicaid
permits providers, plans, and states to report
diagnostic and treatment services under any
number of separate benefit categories (e.g., as a
physician service, a hospital outpatient service, a
federally qualified health center or rural health
clinic service, and so forth). It is only in the case of
beneficiaries whose coverage is limited to family
planning and family planning-related care that
what does or does not fall into this particular
benefit category takes on significance as a basic
matter of coverage.
However, the “freedom of choice” provision of
federal law makes this distinction enormously
important since the definition so highly influences
the issue of out-of-network payment and access.
At a time when sexually transmitted infections have
reached epidemic proportions
27
, for example,
public health considerations argue for ensuring
that the family planning “freedom of choice”
provision encompasses not only those services
funded at 90 percent federal funding but also
those that are fully fundable but at a lesser rate
under CMS guidance, such as STI treatment along
with other essential services such as HIV screening
and HPV vaccinations. Public health considerations
warrant identifying all of these services
contractually as covered by the “freedom of
choice” safeguard.
While the goal of in-network care to ensure
maximum care coordination and plan
accountability is extremely important and worthy
of a long-term effort, the problem of controlling
preventable sexually transmitted infections is so
urgent that clarifying coverage ambiguities rises to
a high level of importance to remove any potential
barrier to care or delay in care. Furthermore, this
recommendation is consistent with how private
insurers treat STI treatments. Data from Fair Health,
the largest repository of private insurance claims
data in the U.S., show that 69 percent of providers
that furnish basic family planning services also
provide, bill, and receive payment for STI testing,
while 76 percent furnish and receive payment for
STI treatment services.
28
These figures suggest that
it is standard practice for insurers to pay family
planning providers for STI treatment as well. By
including STI treatment within the bundle of family
planning services covered by the “freedom of
choice” safeguard, Medicaid programs would align
their practices with those followed in the
commercial insurance market.
We are convinced that the ambiguities and
uncertainties in state contracts regarding the
extent of family planning coverage are the result, in
large part, of the absence of clear guidance from
CMS on this matter. What we believe would help
enormously is policy guidance, developed by CMS
in consultation with experts from the Office of
Population Affairs and the CDC, that describes best
practice approaches to family planning coverage
both generally and in a managed care context,
including parity in coverage between traditional
and ACA expansion populations for all FDA-
approved contraceptives and the extent to which
“well-woman’s health services” as an essential
health benefit could be classified as family
planning benefits and covered for all women as
such. In addition, federal guidelines could clarify
state options regarding the ability to classify
certain diagnostic and treatment services as family
planning benefits, particularly STI diagnosis and
treatment, HPV vaccines, HIV testing and
counseling, because of their integral relationship
with family planning. Furthermore, these benefits
should be payable at the 90 percent rate and
available from any Medicaid qualified provider as a
family planning benefit, at state option.
2) The value of a collaborative state effort to
identify best practices and model purchasing
language related to managed care and family
planning.
As noted, as a strict matter of law and policy, the
“freedom of choice” safeguard has the effect of
lessening the direct pressure on states to ensure

The George Washington University Milken Instute School of Public Health
26
strong provider networks, effective access, and
high performance from their plans. This somewhat
lessened legal accountability pressure is reflected
in the contract documents themselves, containing
relatively few family planning-specific performance
measures or purchasing specifications. This is true
even in the case of matters in which specifications
presumably play a critical role. One such area is the
definition of what is covered as a family planning
benefit for both in and out-of-network care.
Another is the obligation of managed care plans to
fully inform members about their ability to obtain
family planning services (as defined) from their
provider of choice. A third — given the fact that
out-of-network access is a matter of federal policy
— is the need for two-way referral arrangements
between plans and all family planning providers in
their service areas, regardless of network status, to
ensure that members who need help finding a
family planning provider can get it and those
whose family planning visits reveal other serious
health conditions can be quickly and smoothly
referred back to their plans for in-network care.
Beyond making sure that plans effectuate the
federal out-of-network policy in a manner that
fosters strong performance, our findings confirm
considerable state interest in building strong in-
network family planning services as a basic feature
of high-performing health plans. Areas to target in
a state collaborative effort around family planning
and managed care would be coverage and
utilization management, the use of payment
incentives and community outreach to develop
provider networks that include all highly-valued
providers, and above all, perhaps, the development
of performance measures. This review suggests
that states are beginning to seriously address the
need for outcome measures beyond cervical cancer
screening. In the case of adolescents, the one
measure in the CMS quality measures that does
exist (chlamydia screening) appears to have gained
minimal traction, at least as a matter of formal
purchasing policy. States uniformly recognize the
challenge of attempting to upgrade managed care
performance in the absence of performance
standards. For this reason, performance standards
development emerges as a key priority across the
range of preventive, diagnostic, and treatment
services that would fall within a full and robust
definition of family planning.
States are beginning to devote time and energy to
family planning in a postpartum context. This
focus offers an excellent starting point for a more
expansive effort to achieve more robust
performance on family planning as a basic
preventive service and the role of integration to
improve overall patient and population health.
Perhaps the most important finding in this study is
the great importance that family planning appears
to play in the minds of state Medicaid programs.
Indeed, agencies do not consider family planning
to be an area where they face immediate and
urgent problems. But uniformly, the officials we
spoke with — and the contracts we reviewed —
underscored the view of family planning as a
central feature of managed care system. Despite
the existence of a “freedom of choice” policy
might—at least in theory—lead agencies to believe
that high-quality family planning is not a managed
care front-burner issue. This is not the case.
Officials’ appreciation for the foundational role of
family planning and their interest in using
managed care tools to improve access and quality
point to the value of a longer-term effort to
strengthen managed care performance. The fact
that several states have focused on family planning
access by expanding the populations covered for
this service underscores the timeliness of an
initiative to broaden this focus to include managed
care performance for full benefit populations.
Family planning represents one of the nation’s
most important and effective preventive services.
With 70 percent of Medicaid beneficiaries enrolled
in comprehensive managed care, it is time to
create robust guidance that helps states tackle
family planning as not only a basic aspect of
Medicaid managed care but as a major opportunity
to improve health and value.

The George Washington University Milken Instute School of Public Health
27
Appendices
Appendix 1: Medicaid Managed Care Contract
Review Tables
Appendix 2: Study Methods
Appendix 3: Advisory Committee
Appendix 4: Case Study States
References
1
Kaiser Family Foundation. Total Medicaid MCO
Enrollment. (Accessed April 9, 2021). https://
www.kff.org/other/state-indicator/total-medicaid-
mco-enrollment
2
Centers for Disease Control and Prevention.
Unintended Pregnancy. (Accessed March 31, 2021).
https:/ /www.cdc.gov/ repr odu cti vehe alth/
contraception/unintendedpregnancy/index.htm
3
Cheryl Robbins, Thomas Keyserling, Stephanie B.
Jilcott Pitts, John Morrow, Nadya Majette, Jessica A.
Sisneros, Ashley Ronay, Sherry L. Farr, Rachel
Peragallo Urrutia, and Patricia M. Dietz. (2013.)
Screening Low‐Income Women of Reproductive
Age for Cardiovascular Disease Risk Factors, J.
Women’s Health 22(4) 314‐321. https://
www.ncbi.nlm.nih.gov/pmc/articles/PMC4386647/
4
Centers for Disease Control and Prevention and
the U.S. Office of Population Affairs. (2014).
Providing Quality Family Planning Services. MMWR
63:4 https://www.cdc.gov/mmwr/pdf/rr/rr6304.pdf
5
Bruce Spitz. (1979). When a Solution is Not a
Solution: Medicaid and Health Maintenance
Organizations, Jour. Health Pol. Pol. & Law 3(4) 497
-518.
6
Pub. L. 97-35 (95 Stat. 483)
7
David Smith and Judith D. Moore. (2015.)
Medicaid Politics and Policy
. Taylor and Francis.
8
Pub. L. 105-33 (111 Stat. 251)
9
Usha Ranji, Yali Bair, and Alina Salganicoff. (2016).
Medicaid and Family Planning: Background and
Implications of the ACA
. Kaiser Family Foundation.
https://www.kff.org/report-section/medicaid-and-
family-planning-appendix-2-women-ages-15-to-
49-en r o l l e d-in-medicaid - m a naged- ca r e-
a r r a n g e m e n t s - by- s t a t e / v i e w / p r i n t /
#:~:text=Today%20the%20vast%20majority%20
(77,care%20arrangements%20(Figure%204).
10
Samantha Artiga, Petry Ubri , and Julia Zur.
(2017).
The Effects of Premiums and Cost Sharing
on Low-Income Populations: Updated Review of
Research Findings
. Kaiser Family Foundation.
https://www.kff.org/medicaid/issue-brief/the-
effects-of-premiums-and-cost-sharing-on-low-
income-populations-updated-review-of-research-
findings/
11
ACA § 2719A; 45 C.F.R. § 147.138(b)
12
42 U.S.C. 1396u-2 (b)(2)
13
42 U.S.C. 1396u-2 (b)
14
Social Security Amendments of 1972
15
42 U.S.C. § 1396a(a)(10)(G)(XVI)
16
Guttmacher Institute. (2021).
Medicaid Family
Planning Eligibility Expansions.
(Accessed April
2021). https://www.guttmacher.org/state-policy/
explore/medicaid-family-planning-eligibility-
expansions
17
42 U.S.C. § 440.230(b)
18
Guttmacher Institute. (2021).
Insurance Coverage
of Contraceptives.
(Accessed March 2021). https://
www.guttmacher.org/state -policy/explore/
insurance-coverage-contraceptives
19
2021 Core Set of Adult Health Quality Measures
for Medicaid (Adult Core Set). https://
www.medicaid.gov/medicaid/quality-of-care/
downloads/2021-adult-core-set.pdf
20
2021 Core Set of Children’s Health Care Quality
Measures for Medicaid and CHIP (Child Core Set).
https://www.medicaid.gov/medicaid/quality-of-
care/downloads/2021-child-core-set.pdf
21
42 C.F.R. § 438.3
22
Manatt. (2019).
Enhancing Access to Family
Planning Services in Medicaid: A Toolkit for States
.
(May 2019). https://www.manatt.com/
getattachment/4dfc897e-6f05-42dd-b82b-
a0bbc8725c52/attachment.aspx
23
Sara Rosenbaum, Maria Velasquez, et al. (2020).
How States Are Using Comprehensive Medicaid

The George Washington University Milken Instute School of Public Health
28
Managed Care to Strengthen and Improve Primary
Care.
The Commonwealth Fund. https://
www.commonwealthfund.org/publications/issue-
b r i e f s / 2 0 2 0 / j u l / h o w - s t a t e s - a r e - u s i n g -
comprehensive-medicaid-managed-care
24
2021 Core Set of Maternal and Perinatal Health
Measures for Medicaid and CHIP (Maternity Core
Set). https://www.medicaid.gov/medicaid/quality-
of-care/downloads/2021-maternity-core-set.pdf
25
Centers for Medicare & Medicaid Services.
(2019). Analytic Brief: The Maternal and Infant
Health Initiative Grant to Support Development
and Testing of Medicaid Contraceptive Care
Measures. https://www.medicaid.gov/medicaid/
quality-of-care/downloads/mihi-contraceptive-
measures.pdf
26
Kaiser Family Foundation. (2019). Data Note:
Impact of New Title X Regulations on Network
Participation. https://www.kff.org/womens-health-
policy/issue-brief/data-note-impact-of-new-title-x-
regulations-on-network-participation/
27
Centers for Disease Control and Prevention.
(2019). 2018 STD Surveillance Report. https://
www.cdc.gov/nchhstp/newsroom/2019/2018-STD-
surveillance-report.html
28
FAIR Health Inc. (2021). FH NPIC Medicaid SAF.
Data accessed 2020-05-04.
