New York State Department of Health AIDS Institute – Updated December 2023 Page 1 of 28
HIV Testing, Reporting and Confidentiality in New York State
2023 Update: Fact Sheet and Frequently Asked Questions
New York State Department of Health AIDS Institute
New York State Public Health Law (PHL) related to HIV testing has evolved over the years to keep pace
with changes in the epidemic and clinical practice. Key provisions were enacted in 2010, 2014, 2015 and
2016 and comprehensive updated HIV/AIDS Testing, Reporting and Confidentiality of HIV-Related
Information regulations were finalized and published in the New York State Register on May 17, 2017.
The following changes were adopted and posted in the New York State Register on March 22, 2023:
1. Reducing the timeframe for reporting of new HIV diagnoses from 14 days to 7 days;
2. Requiring the reporting of every case of acute HIV within 24 hours of diagnosis;
3. Requiring the reporting of the results of HIV testing done for purposes of insurance underwriting
decisions by the clinician under whose medical license the HIV-testing was ordered.
This document includes all developments since 2010 and represents the current regulatory landscape.
Note: 2023 updates are highlighted by being placed in boxes in this document.
How to use this document:
This PDF document allows the user to easily navigate the document to the desired information.
By clicking on a topic in the Table of Contents, you will be taken directly to that section.
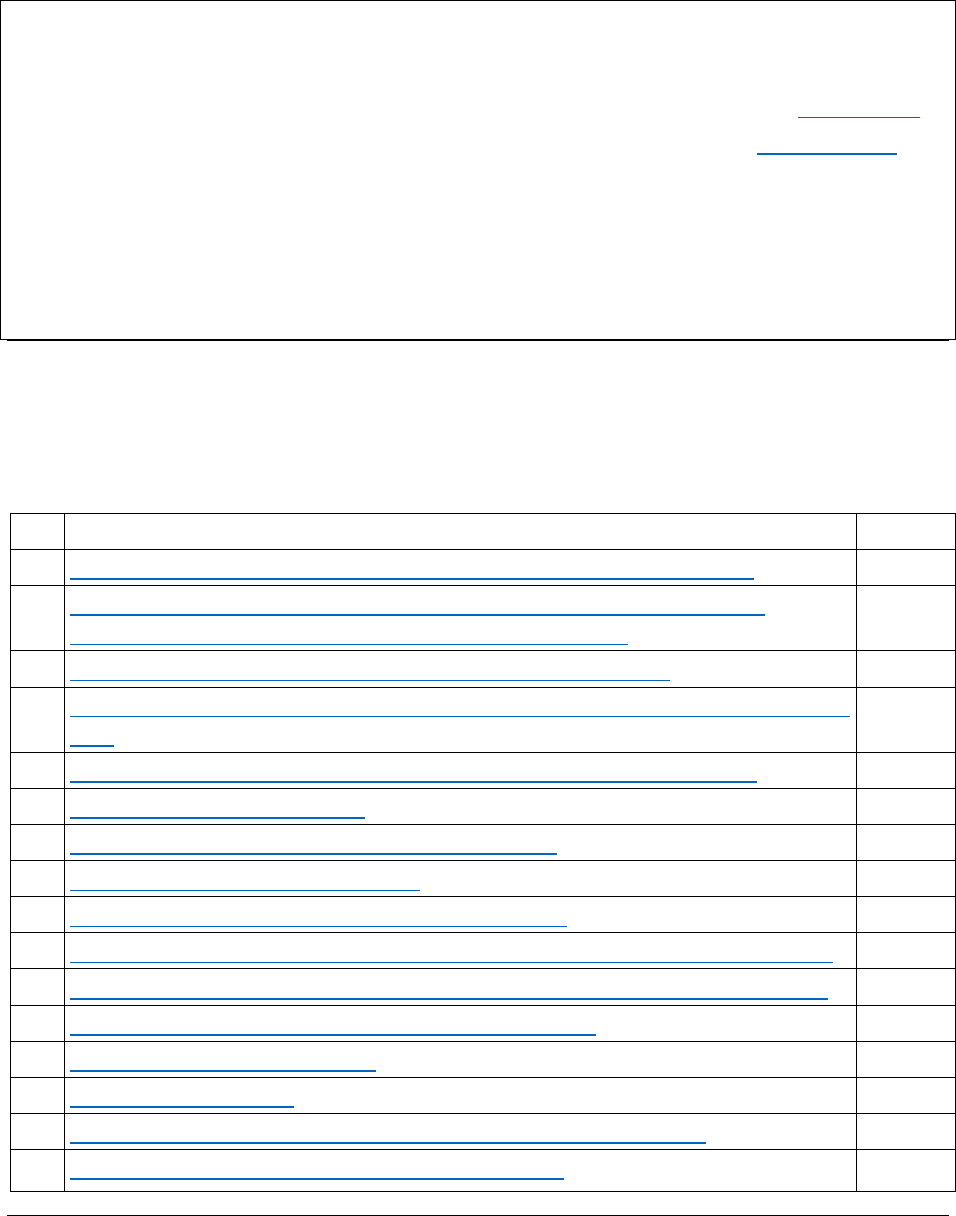
Table of Contents
Topic
Pages
1
The Requirement to Offer HIV Testing as a Routine Part of Health Care
2-4
2
Removal of Requirement for Written or Oral Patient Informed Consent,
Including Prenatal and Maternity Settings, to HIV Testing
4-6
3
Information to Be Provided to the Patient Prior to an HIV Test
6-7
4
Post-test Counseling and Requirements to Link Newly Diagnosed Patients to HIV
Care
7-10
5
Expansion of Minor Consent to HIV Treatment and Preventive Services
10-11
6
Documentation Requirements
12
7
Health Care Provider HIV Reporting Requirements
12-14
8
Laboratory Reporting Requirements
15-16
9
Partner Notification and Partner Services Programs
16-18
10
Confidentiality of HIV-Related Information in Medical / Social Services Records
18-19
11
Sharing of Patient-Specific Information to Promote Linkage/ Retention in Care
19-24
12
Health Department Assistance with Patient Follow-Up
24-25
13
Reimbursement for HIV Testing
25-26
14
Occupational Exposure
27
15
NYSDOH Expectations for Compliance and Enforcement Activities
27
16
Access to HIV Information for Medical Researchers
27-28

New York State Department of Health AIDS Institute – Updated December 2023 Page 2 of 28
1. The Requirement to Offer HIV Testing as a Routine Part of Health Care
HIV testing must be offered at least once as a routine part of health care to all patients age 13
or older receiving primary care services at an outpatient clinic or primary care services from a
physician, physician assistant, nurse practitioner or midwife.
In order to identify cases of HIV infection among people who are not engaged in regular
primary care services, the law also requires that hospitals offer HIV testing to all inpatients and
persons seeking services in emergency departments with the following exceptions:
• When the individual is being treated for a life threatening emergency;
• When the individual has previously been offered or has previously been tested for HIV
(unless otherwise indicated due to risk factors);
• When the individual is comatose or determined by the attending provider to lack mental
capacity to consent.
IMPORTANT POINTS:
• NYS Public Health Law mandates the offer of HIV testing to all patients age 13 or older.
• The 2016 amendments to the NYS Public Health Law removed the previous upper age
limit of 64.
• The offer of HIV testing is most effective when it is presented as a clinical
recommendation of the health care provider.
• The offer of HIV testing must be documented in the patient medical record.
HIV Testing Toolkit: Resources to Support Routine HIV Testing for Adults and Teens
The New York State Department of Health (NYSDOH) developed a toolkit for primary care
providers that contains all of the resources needed to meet New York State clinical guidelines
and legal requirements for offering voluntary, routine HIV testing as a part of health care to all
patients aged 13 and older. Please click to access the HIV Testing Clinician’s Toolkit.
Updated HIV Diagnostic Testing Algorithm
The HIV Diagnostic Testing Algorithm is a multi-test algorithm, incorporating tests that detect
HIV antigens, antibodies and RNA. The final interpretation is based on a combination of test
results. All preliminary positive HIV rapid test results must be confirmed through additional
testing performed at a clinical laboratory. More information can be found at:
https://www.hivguidelines.org/hiv-testing-acute-infection/hiv-testing/#tab_3
FAQ 1: How often does the offer of HIV testing need to be repeated?
In addition to offering HIV testing once in the course of routine care, testing should be offered
annually to patients whose behavior indicates elevated risk. In order to promote early
identification, HIV testing may be offered as frequently as every three months to patients with
identified risk behaviors. Since many people choose not to disclose their risk behaviors,

New York State Department of Health AIDS Institute – Updated December 2023 Page 3 of 28
providers should consider adopting a low threshold for recommending HIV testing.
FAQ 2: Which health care facilities and health care providers are impacted by the requirement
to offer HIV testing?
HIV testing must be offered in the following health care settings:
• Primary care services in diagnostic and treatment centers (including school-based clinics
and family planning sites)
• Primary care services in outpatient departments of hospitals
• Inpatient departments of hospitals
• Emergency departments
HIV testing must be offered by physicians, physician assistants, nurse practitioners or midwives
who provide primary care, or their representatives, regardless of setting. Primary Care means
the medical fields of:
• Family medicine
• General pediatrics
• Primary care
• Internal medicine
• Primary care obstetrics/gynecology
FAQ 3: Does the offer of HIV testing apply to nursing homes, college health services, retail
clinics, urgent care centers, employee health services or STD clinics that provide primary care?
Yes. Even though these facilities are not specifically mentioned in the law, if primary care is
being provided by a physician, physician assistant, nurse practitioner, or midwife, they are
required to make the offer regardless of board certification of the practitioner or setting where
primary care is provided.
FAQ 4: If I am unsure, how can I determine if my facility is covered by the law?
The important thing is to consider what your facility does rather than what your facility is
called. For instance, an urgent care center that offers many or all of the services available at a
family physician’s office would be considered a primary care provider. However, there are
diagnostic and treatment centers that are restricted to ambulatory surgery, and these would
not be covered by the mandated testing offer provision since they do not offer primary care.
FAQ 5: How do the latest changes in regulations pertaining to HIV testing impact HIV testing
practices in prenatal and maternity settings?
New York’s regulatory framework for preventing perinatal transmission of HIV has proven
highly effective and remains unchanged. The 2016 updates to HIV testing do remove the
requirement to obtain consent for HIV testing in writing or orally (see Section 2). All pregnant
people must be offered HIV testing as a clinical recommendation as early as possible during
pregnancy. Third trimester testing is recommended for all pregnant people in NYS who tested
negative for HIV earlier in their pregnancy. When being offered HIV testing, the individual

New York State Department of Health AIDS Institute – Updated December 2023 Page 4 of 28
should be provided the key points of information and informed of their right to decline the test
(see Section 3). Pregnant people who are diagnosed as living with HIV should be linked to
treatment as soon as possible to protect their health and prevent transmission of HIV to the
newborn. Pregnant people who present to the labor/delivery setting with no history of HIV
testing during their current pregnancy should be counseled with the recommendation for HIV
testing. If the birthing parent declines testing in labor/delivery, they should be informed that
the newborn will be tested immediately at birth without their consent. All newborns, including
those tested at birth, are routinely tested for HIV through the New York State Newborn
Screening Program. Documentation of the individual’s prenatal HIV testing should be forwarded
to the delivering hospital and a copy of the HIV test history results should be placed in the
newborn’s medical record to ensure administration of medications during labor/delivery and
initiation of medication to the infant for the first four-six weeks of life or until the infant is
definitively excluded from HIV infection. To access the latest regulations visit:
https://regs.health.ny.gov/content/section-69-13-responsibilities-chief-executive-officer or
https://regs.health.ny.gov/content/section-40521-perinatal-services
FAQ 6: As a patient, what do I do if I am not offered an HIV test?
If you are not offered an HIV test by a health care provider covered by the law or their
representative, you should bring it to the attention of that provider and ask for a test or an
explanation for why the offer was not made. If you believe your health care provider is not
complying with the law, email your name and contact information, the name of the provider,
and whatever details you think would be helpful to [email protected] and the situation
will be reviewed. Or, you can complete the patient complaint form found at
http://www.health.ny.gov/forms/doh-4299.pdf and submit it to the address indicated on the
form.
2. Removal of Requirement for Written or Oral Patient Informed Consent to HIV Testing
Effective November 28, 2016, amendments to the New York State Public Health Law removed
the requirement for written or oral informed consent prior to ordering an HIV-related test,
including elimination of written consent for HIV testing in New York State correctional facilities,
and removing references to consent forms. The objective of the update is to eliminate barriers
to HIV testing and make HIV testing comparable to the manner in which other important
laboratory tests are conducted. HIV testing remains voluntary and patients have the right to
refuse an HIV test, but obtaining written or oral consent for testing is no longer required in any
setting. At a minimum, patients must be advised orally that an HIV test is going to be performed.
If the patient objects to the HIV test, this must be noted in the patient’s medical record. HIV
test requisition forms submitted to laboratories do not require provider certification of
informed consent.

New York State Department of Health AIDS Institute – Updated December 2023 Page 5 of 28
IMPORTANT POINTS:
• As part of the HIV testing process, patients must be provided information about HIV as
defined by Public Health Law. See Section 3 for details. Information may be provided
orally, in writing, through office signage or in any other patient-friendly audio-visual
format.
• If the patient declines the offer of an HIV test, this must be noted in the patient’s
medical record.
• For patients diagnosed as living with HIV, the health care provider administering testing
must arrange, with the consent of the patient, an appointment for HIV medical care.
Simply providing the name of a care provider is not sufficient. A specific appointment
with a provider who offers HIV care must be provided (see Section 4 for details).
2023 Update: Obtaining Written Informed Consent for HIV Testing Performed for
Insurance Underwriting Purposes and Reporting of Such Results
The 2023 update to HIV testing regulations mandates that tests performed for insurance
underwriting purposes be reported when they indicate a diagnosis of HIV or AIDS.
1. It is important to note that regulations regarding the conduct of HIV testing for insurance
purposes are outlined in New York Insurance Law Sec. 2611, not Public Health Law.
2. The 2023 update does not change the informed consent procedure for these tests.
3. The 2016 updates to public health law that removed the requirement for written informed
consent apply to HIV testing as part of routine health care, but do not apply to HIV testing for
purposes of insurance underwriting decisions.
4. Health care providers conducting HIV testing for insurance purposes must obtain patient written
informed consent before conducting an HIV test.
FAQ 7: The goal of the NYSDOH is to streamline the process of HIV testing and make it similar
to how other important laboratory tests are conducted. What are some approaches that
health care facilities may implement to simplify the process of HIV testing and increase the
number of people aware of their HIV status?
While consent no longer has to be obtained orally or in writing, it is standard practice that
health care facilities provide services in accordance with patient consent. At a minimum,
patients must be orally informed that HIV testing is going to be conducted and have the right to
decline an HIV test. Below are two different ways that health care facilities can operationalize
HIV testing in a manner that meets or exceeds the minimum requirement of the law:
1. A member of the care team orally informs the patient that HIV testing will be
conducted. Key points of information, including informing the patient that they may
decline an HIV test, may be provided orally, in writing, electronically, through office
signage or in any other patient-friendly audio-visual method. If the patient objects, the
HIV test would not be conducted and the patient objection must be noted in the
patient’s medical record.

New York State Department of Health AIDS Institute – Updated December 2023 Page 6 of 28
2. The health care facility may include an explanation that HIV testing is routinely
conducted in the general medical consent statement that is signed to authorize
treatment during the visit. If the patient signs a general medical consent that includes
informing the patient about HIV testing, they have effectively been informed of the test
and provided consent. This would exceed the minimum requirement of the law (i.e. that
a patient be advised orally than an HIV test is going to be performed) but may serve as
an efficient manner to operationalize HIV testing in some health care facilities. Key
points of information, including informing the patient that they may decline an HIV test,
may be provided orally, in writing, electronically, through office signage or any other
patient-friendly audio-visual method. If the patient objects, the HIV test would not be
conducted and the patient objection must be noted in the patient’s medical record.
In cases where the patient declines HIV testing, it would be good practice for the health care
provider to inquire about the reason and take the opportunity to address these concerns and
explain the clinical benefits of every person knowing their HIV status. Health care facilities
should have policies and procedures in place to ensure that if a patient objects to the test, that
HIV testing is not conducted.
FAQ 8: Do the consent procedures in the law apply to tests used for monitoring HIV disease
progression or treatment such as viral load, CD4 count, or HIV resistance tests?
No. The law applies specifically to testing that is being performed for the initial diagnosis of HIV
infection. The law does not apply to tests used for monitoring HIV disease progression or to
assess treatment effectiveness.
FAQ 9: New York State Public Health Law has, since early in the epidemic, allowed minors to
consent to their own HIV test, without parental involvement. How does the removal of the
requirement of written or oral consent for HIV testing impact HIV testing of minors?
The intent of recent amendments to the Public Health Law is to facilitate routine HIV testing for
all persons age 13 and older. Minors have the ability to consent to the HIV test without
parental/guardian involvement and must be provided the required information about HIV and
afforded the right to object to an HIV test. Amendments to the NYSDOH regulations in 2017
allow minors to consent to HIV treatment as well as preventive services. For more information,
see Section 5.
3. Information to Be Provided to the Patient Prior to an HIV Test
Prior to conducting diagnostic HIV testing, information about HIV must be provided orally, in
writing, through signage or in any other patient-friendly audio-visual format. Placing the
NYSDOH HIV testing clinic poster in a visible location or providing patients with the NYSDOH
patient brochure on HIV testing are simple ways of conveying this information to patients. The
key points of information that must be provided are:

New York State Department of Health AIDS Institute – Updated December 2023 Page 7 of 28
• HIV testing is voluntary and all HIV test results are confidential (private);
• HIV can be transmitted through unprotected sex, sharing needles, childbirth or
breastfeeding;
• Treatment for HIV is very effective, has few or no side effects and may involve taking
just one pill once a day;
• Partners can keep each other safe by knowing their HIV status and getting HIV
treatment or taking HIV pre-exposure prophylaxis (PrEP). Not sharing needles and
practicing safer sex will help protect against HIV, hepatitis C and other STDs.
• It is illegal to discriminate against a person because of their HIV status and services are
available to help address discrimination;
• Anonymous HIV testing (without giving your name) is available at certain public testing
sites;
• HIV testing is a routine part of health care but you have the right to decline an HIV test.
Testing will not be performed if you object. If you wish to decline HIV testing, inform
the health care provider.
FAQ 10: How are the key points of information provided to patients who may be unconscious
or comatose?
In cases where the patient is unconscious or comatose, the Family Health Care Decisions Act
(FHCDA) has provisions which allow a surrogate to make treatment decisions. Clinicians should
follow their facility’s policies and procedures regarding the FHCDA. The surrogate would have
authority to make decisions about HIV testing and should be provided points of information
about HIV, including that testing will not be performed over the surrogate’s objection.
4. Post-Test Counseling and Requirements to Link Newly Diagnosed Patients to HIV Care
When testing indicates a diagnosis of HIV infection, the person ordering HIV testing or their
representative must provide the patient the final interpretation of diagnostic testing, and, with
the patient’s consent, schedule an appointment for follow-up HIV medical care.
IMPORTANT NOTE: A person with laboratory evidence of acute or early HIV infection (i.e.
detectable HIV antigen and virus, but no evidence of HIV antibodies) has a high likelihood of
passing the virus to sexual or needle sharing partners and should be counseled about how to
avoid passing the virus to others. The Medical Provider HIV/AIDS and Partner/Contact Report
Form (PRF) (DOH-4189), must be submitted within 24 hours of diagnosis of acute HIV. See
section 7 for more information.
Patient education should be provided that addresses:
• That the diagnosis means the person is living with HIV, a lifelong health condition;
• That people can live a healthy life with HIV. HIV treatment is effective, has few or no
side effects and may involve taking just one pill once a day;

New York State Department of Health AIDS Institute – Updated December 2023 Page 8 of 28
• That financial assistance is available, if needed, for HIV medical care and HIV
medications;
• That the patient can pass HIV to sexual or needle sharing partners and strategies for
avoiding transmission; including information about mother to child transmission;
• The importance of notifying sexual or needle sharing partners to prevent further
transmission and to promote access of exposed persons to HIV testing, health care and
prevention services;
• The range of partner notification options and available partner services programs;
• That names and other information about the patient is not shared during the partner
notification process;
• That all cases of HIV infection are reported to the NYSDOH;
• That known contacts, including a known spouse, are reported to the NYSDOH;
• The risk of domestic violence and performance of domestic violence screening using the
NYSDOH-approved domestic violence screening protocol;
• That HIV-related information is confidential; information may be shared with medical
providers to provide needed care but may not be shared with others without patient
authorization to release confidential HIV-related information;
• That a minor who has been diagnosed with HIV may consent to their own HIV treatment
(if applicable);
• That patient authorization to release confidential HIV-related information may be
revoked at any time;
• That discrimination against persons with HIV in the areas of employment, housing,
public accommodations, health care and social services is prohibited by law;
• That if a person with HIV appears to be out of care, they may be contacted by the
medical provider or health department staff to address barriers to entry into care and
promote engagement in care.
IMPORTANT INFORMATION: Undetectable equals Untransmittable (U=U): There are many
important reasons to start HIV treatment as soon as possible. In addition to getting treatment
to support their own health, a person living with HIV who is on HIV treatment and virally
suppressed for 6 months or longer has effectively no risk of passing HIV to a partner through
sex.
A person who tests negative for HIV infection must be informed of the result and provided
information concerning the risk of acquiring HIV through sexual and needle sharing activities.
Pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) should be discussed as
prevention options. This information may be in the form of written materials such as the
NYSDOH document titled Information for Patients with a Negative HIV Test Result available in
English or Spanish. The negative test result and required information do not need to be
provided in person. Other mechanisms such as email, mail, and phone may be used as long as
there is an established protocol. Alternative methods of delivering results must be discussed

New York State Department of Health AIDS Institute – Updated December 2023 Page 9 of 28
with the patient. It is not appropriate to tell patients that if they are not contacted, they may
assume their test was negative.
Patients with potential recent exposure to HIV present diagnostic challenges due to the
"window period," or the length of time after infection that it takes for antibodies or the virus to
be detected by HIV diagnostic tests. More information about the window period for various
types of tests can be found at https://www.hivguidelines.org/hiv-testing-acute-infection/hiv-
testing/#tab_2. Clinicians should be familiar with the testing process used by the laboratory
conducting testing for their patients because recommendations for retesting patients with
recent exposure will vary depending on the test used.
A person with inconclusive or incomplete HIV diagnostic testing results (i.e. when the HIV
Diagnostic Testing Algorithm did not produce an overall valid or conclusive result) must be
informed that the test result was inconclusive or incomplete and have an additional specimen
collected as soon as possible. In these cases, the entire algorithm should be repeated. More
information is available at https://www.hivguidelines.org/hiv-testing-acute-infection/hiv-
testing/#tab_3
The NYSDOH may be able to assist if you have difficulty locating a patient in need of additional
testing to resolve inconclusive HIV diagnostic testing. See Section 9 of this document for more
information, including how to contact partner services programs throughout NYS. For
additional information visit: www.health.ny.gov/diseases/communicable/std/partner_services
FAQ 11: To meet the requirement to arrange follow-up care for a patient newly diagnosed
with HIV, is it sufficient to simply provide the name of a local HIV care provider?
No, the law specifies that the health care provider who ordered testing is responsible for
providing or arranging for an appointment for follow-up HIV care. This means that an actual
appointment date and time scheduled as soon as possible should be provided. It is considered
the gold standard for a newly diagnosed person to begin HIV treatment on the same day. While
that may not always be possible, it is ideal for people to begin treatment within three days and
in no case should it take longer than thirty days to begin treatment. A best practice is for HIV
testing providers to have formal or informal agreements with HIV clinical providers to promote
a “warm handoff” of patients to HIV clinical care in a timely fashion. Every reasonable effort
should be made to link persons who are newly diagnosed with HIV to health care, prevention,
supportive services and partner services. If you are having difficulty making an appointment for
a patient, contact Charles Gonzalez, MD at [email protected].
Q 12: Does the appointment need to be with an Infectious Disease Provider or HIV Specialist?
The law does not specify the clinician specialty. The NYSDOH website includes contact
information for Designated AIDS Centers and other resources to help identify providers and
health care facilities offering HIV care. Visit the AIDS Institute’s Provider Directory.

New York State Department of Health AIDS Institute – Updated December 2023 Page 10 of 28
FAQ 13: Is the health care provider who conducted the test responsible for confirming that the
patient attended the appointment for follow-up HIV care?
The law requires that the patient’s medical record must document the name of the
provider/facility with whom the appointment was made but does not require that the HIV
testing provider document that the appointment was kept. However, best practice, in support
of ending the epidemic, would be to establish a protocol that includes confirmation of the
individual’s attendance at the initial appointment.
5. Expansion of Minor Consent for HIV Treatment and Preventive Services
2017 amendments to the NYSDOH’s regulations allow minors to consent to their own HIV
treatment and HIV preventive services such as pre-exposure prophylaxis (PrEP) and post-
exposure prophylaxis (PEP) without parental/guardian involvement (10 NYCRR Part 23). Part 23
has long established the legal capacity of minors to consent to treatment and preventive
services for sexually transmitted diseases (STDs). Provisions in Part 23 require that the
Commissioner of Health promulgate a list of STDs. The 2017 amendments to 10 NYCRR Part 23
added HIV to the list of STDs, thereby bringing minor capacity to consent to HIV treatment and
preventive services on par with other STDs. In addition, under Part 23, medical or billing records
may not be released or made available to the parent or guardian without the minor patient’s
permission.
After being diagnosed, young people currently face barriers that can prevent or delay access to
care, including denial and fear of their HIV status, misinformation, HIV-related stigma, low self-
esteem, lack of insurance, homelessness, substance use, mental health issues, and lack of
adequate support systems. Because of these factors, many young people need the ability to
consent to their HIV treatment. Updates to the regulation help ensure that more young people
have optimal health outcomes and prevent transmission of HIV to others. In addition, minors
will now have the ability to consent to HIV-related preventive services, including PrEP and PEP
just as they can consent for other reproductive or sexual health-related services.
FAQ 14: Does the change in the NYSDOH Regulations mean that clinical providers must not
seek to engage the parents or guardians of a minor in the minor’s HIV health care or HIV
prevention decisions?
The change in regulations means that minors have the ability to consent to their own HIV
treatment and prevention services, without the involvement of a parent or guardian. Clinical
providers may, over time, discuss with their minor patients opportunities for parental or
guardian involvement in these decisions, including exploring with the young person the
potential benefits of parental or guardian involvement. However, decisions about the
involvement of a young person’s parent or guardian must be left to the young person. Clinical
providers should maintain a high level of sensitivity to the concerns of the young person
regarding potential negative consequences of involvement of a parent or guardian. Discussions

New York State Department of Health AIDS Institute – Updated December 2023 Page 11 of 28
about whether to involve a parent or guardian should never result in a delay in starting HIV
treatment or prevention services.
FAQ 15: If a young person does not want their parent(s) or guardian(s) to be informed that
they are taking PrEP or PEP, what can be done to stop the explanation of benefits form (EOB)
from being sent to the parent’s address?
Minors may contact the health care plan and request that an alternative address be used when
issuing an EOB for services provided to the adolescent patient. The minor, with assistance from
a health or support services provider when possible, should contact the health plan to
determine what procedures or forms are required to request an address change. Furthermore,
minors should make this request before seeking billable health care services in order to allow
enough time for the health plan to make the necessary changes to their information system. In
some situations, the minor may list the health care provider’s address as the alternative
address for EOB notifications. Minors should be advised that Insurance Law §3234(c) allows the
primary policyholder to demand an EOB even if one is not required. Adult children who are
covered by their parents’ insurance plan as well as other adults who are concerned about, or at
risk of, retaliation from their partner or spouse may also wish to redirect EOBs. Insurance Law
§2612(h)(2)(A) and 11 NYCRR 244.3 provide protections for the redirection of communications
from health plans for victims of domestic violence.
FAQ 16: What can providers communicate to minors who consent to PrEP or PEP about their
ability to access financial assistance to pay for PrEP and PEP?
Regardless of age, many people benefit from assistance with navigating payment for PrEP or
PEP. This is especially true for minors. Health and support services providers working with a
minor interested in PrEP should seek to connect the patient to a PrEP specialist in the
community whenever possible. Providers working with minors around PrEP may direct these
young people to a local sexual health Clinic or STD Clinic that offers PrEP. Minor patients of
these clinics have the right to request that their insurance plans not be billed for services and
may have access to services on a sliding fee scale. Medicaid will cover the cost of PrEP but prior
approval may be required. Minors who are covered by private insurance may need assistance
determining how their plan covers the various expenses of PrEP.
Minors who follow the directions outlined in FAQ 15 (see above) can take steps to avoid having
EOBs sent to their parents. Minors have access to assistance from the New York State PrEP
Assistance Program (PrEP-AP) which covers the cost of health care appointments and lab work
when these services are accessed through a provider registered with PrEP-AP. The Gilead Co-
Pay Coupon and Medication Assistance Program are not available to minors but other patient
assistance programs may be available to minors. For a complete review of resources related to
paying for PrEP, please review the NYSDOH Payment Options for PrEP. To be effective, PEP
must be initiated as soon as possible. Initiation of PEP should not be delayed in order to make
arrangements for payment. Minors who are victims of sexual assault should be directed to the

New York State Department of Health AIDS Institute – Updated December 2023 Page 12 of 28
emergency room and are eligible for assistance from the NYS Office of Victim Services. For a
complete description of payment options, please review the NYSDOH Payment Options for PEP
Following Non-Occupational Exposures Including Sexual Assault.
6. Documentation Requirements
According to the Public Health Law, the following elements pertaining to HIV testing must be
documented in the patient medical record:
• The patient was advised that HIV testing is being done;
• If the patient declines the HIV test;
• For patients with confirmed HIV infection, the name of the provider/facility with whom
the follow-up appointment was made.
FAQ 17: Is it acceptable to use drop-down boxes or checklists in electronic health records to
meet the documentation requirements for advising the patient that HIV testing is being done?
Yes. Drop down boxes or checklists are acceptable. HIV testing documentation requirements
are not intended to create undue burden on health care providers or facilities. Similarly, brief
statements such as “Patient advised that HIV testing will be conducted” or “Patient declined
HIV testing” are sufficient to meet documentation requirements.
FAQ 18: Does the inclusion of the HIV test result in the medical record meet the requirement
of advising the patient that HIV testing is being done?
No. Having the test result in the record does not indicate that the patient was advised of the
HIV test. Including the test result in the medical record is considered standard practice,
separate from the requirement of documenting that the patient was advised of the test.
7. Health Care Provider HIV Reporting Requirements
2023 Update to HIV Reporting Requirements
The Medical Provider HIV/AIDS and Partner/Contact Report Form (PRF) (DOH-4189), must
be submitted:
• within 24 hours of diagnosis of acute HIV, including primary HIV infection, acute
retroviral syndrome, and early HIV infection.
• within 7 days of all other initial diagnosis of HIV, HIV illness, or AIDS diagnoses.
• HIV-testing conducted in the context of insurance institution underwriting decisions is
required to be reported to NYSDOH by clinicians under whose medical license the
HIV-testing is ordered.
Details are provided below.

New York State Department of Health AIDS Institute – Updated December 2023 Page 13 of 28
New York State Public Health Law Article 21 requires the reporting of persons with HIV and
AIDS to the NYSDOH. The law also requires that reports contain the names of sexual or needle-
sharing partners known to the medical provider or whom the patient wishes to have notified.
Under the federal HIPAA Privacy Rule, public health authorities have the right to collect or
receive information “for the purpose of preventing or controlling disease” and in the
“conduct of public health surveillance…” without further authorization. This provision of
HIPAA regulations authorizes medical providers to report HIV/AIDS cases to the NYSDOH or
the New York City Department of Health and Mental Hygiene (NYCDOHMH) without obtaining
patient permission.
The Medical Provider HIV/AIDS and Partner/Contact Report Form (PRF) (DOH-4189), must be
submitted within 7 days of diagnosis for persons with the following diagnoses or with known
sex or needle-sharing partners:
• Initial/New HIV diagnosis - First report of testing documenting HIV diagnosis; acute
cases of HIV must be reported within 24 hours.
• Previously diagnosed HIV (non-AIDS) - Applies to a medical provider who is seeing the
patient for the first time.
• Initial/New diagnosis of AIDS - Including <200 CD4 cells/mm
3
or an opportunistic
infection (AIDS-defining illness).
• Previously diagnosed AIDS - Applies to a medical provider who is seeing the patient for
the first time.
• Known sex or needle-sharing partners of persons with diagnosed HIV infection.
Clinicians seeing for the first time a patient previously diagnosed with HIV or AIDS should report
to the NYSDOH using the PRF. The rationale is that this is often the only indication the NYSDOH
receives of a patient new to New York, but not newly diagnosed, and perhaps not in need of
extensive Health Department Partner Services. Additionally, particularly for the well suppressed
patient who moves into NYS, the report by the clinician can be the only indication that the
person is in fact HIV positive.
Information regarding electronic reporting via the HIV/AIDS Provider Portal (see below) or
paper forms is available from the NYSDOH at 518-474-4284; clinicians located in NYC, call 212-
442-3388. In order to protect patient confidentiality, faxing of reports is not permitted.
HIV/AIDS Provider Portal
The HIV/AIDS Provider Portal is an electronic system which enables clinicians to:
1. meet their reporting requirements electronically;
2. provide a mechanism for clinicians statewide to notify the NYSDOH that a patient needs
linkage to Health Department Partner Services; and,
3. submit inquiries for patients with diagnosed HIV infection who are thought to be in
need of assistance with linkage to or retention in HIV medical care.

New York State Department of Health AIDS Institute – Updated December 2023 Page 14 of 28
A NYSDOH Health Commerce System (HCS) Medical Professionals account is required. After
logging into the HCS at https://commerce.health.ny.gov/, select “Refresh My Applications List”
on the left side and then under “My Applications” select HIV/AIDS Provider Portal. Follow the
prompts to set up an account. For detailed directions on how to set up an account on the
HIV/AIDS Provider Portal, click here.
FAQ 19: The 2023 update specifies that cases of acute HIV infection be reported within 24
hours. What is the rationale for this change?
It is a public health priority that persons with diagnosed acute or early HIV infection are offered
timely partner services to ensure the individual is linked to HIV treatment, and their sexual or
needle-sharing contacts are tested/treated for HIV to prevent transmissions and outbreaks.
Initiation of antiretroviral therapy (ART) during the early stage of HIV infection can benefit
individuals and reduce HIV transmission. Treatment of acute and early HIV infection with
combination ART improves laboratory markers of disease progression. Data also suggest that
treatment of acute HIV infection might decrease the severity of acute disease, lower the viral
set point, slow disease progression rates in the event therapy is stopped, reduce the size of the
viral reservoir, and decrease the rate of viral mutation by suppressing viral replication and
preserving immune function. Because very high levels of virus in blood and genital secretions
increase infectiousness during and immediately after acute HIV infection, initiating treatment
during acute infection can also reduce the risk of HIV transmission substantially.
Acute HIV infection is the earliest stage of HIV disease, and it precedes the development of
detectable antibodies to HIV resulting from the viral infection. A report of acute HIV infection
must include the basis for the determination or diagnosis, which is: (i) laboratory testing results
demonstrating the presence of p24 antigen and HIV virus (RNA or DNA), in the absence of HIV
antibodies; and/or (ii) clinical evidence of documented negative testing history which includes
previous negative or indeterminate test results within 180 days before the first confirmed
positive HIV test result of any type.
For information about laboratory diagnosis and clinical management of cases of acute HIV,
please visit https://www.hivguidelines.org/hiv-testing-acute-infection/acute-hiv/#tab_0.
FAQ 20: What guidance is available for notifying partners of people newly diagnosed as living
with HIV?
New York State Public Health Law requires that medical providers talk with HIV-diagnosed
individuals about their options for informing their sexual and needle-sharing partners that they
may have been exposed to HIV. The HIV Testing Toolkit: Resources to Support Routine HIV
Testing for Adults and Teens contains guidance and resources about talking to your patients
about HIV testing. Additionally, the NYSDOH Partner Services program or NYC Health
Department Contact Notification Assistance Program provides assistance to people living with
HIV and medical providers who would like help notifying partners. See Section 9 of this
document for more information, including how to contact partner services programs
throughout NYS.

New York State Department of Health AIDS Institute – Updated December 2023 Page 15 of 28
FAQ 21: How has the 2016 update impacted reporting by blood and tissue banks?
As in the past, blood and tissue banks are required to report confirmed positive HIV antibody
test results. The 2016 update includes the requirement to report reactive nucleic acid tests.
8. Laboratory Reporting Requirements
Laboratory reporting of suspected or confirmed positive findings or markers of HIV infection is
mandated under New York State Public Health Law. Guidance has been prepared in an effort to
assist permitted clinical laboratories and blood banks in meeting their obligations to report HIV-
related laboratory test results, as well as other communicable disease markers. The guidance is
available on the Wadsworth Laboratory website.
HIV laboratory reporting is an essential source of information for New York’s HIV surveillance
efforts and maintaining high quality, complete data is critical to tracking progress toward
National HIV/AIDS Strategy retention and care measures and NY’s effort to end the epidemic.
To keep pace with advances in HIV care, testing technologies and disease monitoring, there
have been some important changes to HIV laboratory reporting requirements. Laboratories and
blood/tissue banks performing tests for screening, diagnosis or monitoring of HIV infection for
NYS residents and/or NYS health care providers (regardless of patient residence) must report
the following laboratory tests or series of tests used in the diagnosis of HIV infection:
• All reactive/repeatedly reactive initial HIV immunoassay results AND all positive,
negative or indeterminate results from all supplemental HIV immunoassays performed
under the second or third step in the diagnostic testing algorithm, including HIV-1/2
antibody differentiation assay, HIV-1 Western blot, HIV-2 Western blot or HIV-1
Immunofluorescent assay;
• All HIV nucleic acid (RNA or DNA) detection tests (qualitative and quantitative), including
tests on individual specimens for confirmation of nucleic acid-based testing (NAT)
screening results;
• All CD4 lymphocyte counts and percentages, unless known to be ordered for a condition
other than HIV;
• HIV genotypic resistance testing via the electronic submission of the protease, reverse
transcriptase and integrase nucleotide sequence;
• Positive HIV detection tests (culture, P24 antigen).
All HIV-related laboratory reporting, including by NYC providers and for NYC residents, must be
made directly to the NYSDOH, submitted electronically via the NYSDOH Electronic Clinical
Laboratory Reporting System (ECLRS).
To improve the quality of data, and in keeping with changes that allow for enhanced use of
surveillance data to improve linkage and retention in care, laboratories are required to report

New York State Department of Health AIDS Institute – Updated December 2023 Page 16 of 28
results using patient identifying, demographic and locating information, as well as the
requesting provider and facility ordering the lab test. The 2016 update requires that when labs
report HIV-related test results, the following information must be included:
• Patient name, date of birth, and other identifying information;
• Patient demographic information (e.g., sex at birth, race/ethnicity, etc.);
• Patient address and telephone number;
• Provider ordering the test and facility name;
• Complete provider and facility address and telephone number;
• Provider and facility National Provider Identification.
For a complete list of this information and instructions on how to report required data
FAQ 22: NYS has required specific statements regarding disclosure of HIV-related information
on the laboratory report. Are these statements still required?
A statement regarding re-disclosure of HIV-related information under 10 NYCRR Section 63.5 is
no longer required on reports of test results because the lab report is necessary to provide
appropriate care or treatment.
FAQ 23: Do the updates to law change any of the existing requirements for reporting
preliminary positive HIV testing results?
Yes. As stated above, clinical laboratories or blood/tissue bank are required to report results
from tests approved for use within the diagnostic testing algorithm, including
reactive/repeatedly reactive initial HIV immunoassay results AND all positive, negative or
indeterminate results from all supplemental HIV immunoassays (HIV-1/2 antibody
differentiation assay, HIV-1 Western blot, HIV-2 Western blot or HIV-1 Immunofluorescent
assay). For additional information, please visit the following website
https://www.wadsworth.org/sites/default/files/WebDoc/CDRG%20NYState%202020_101920%202.pdf
or contact [email protected] for additional information.
FAQ 24: Can HIV lab results be posted on an electronic medical record?
Yes. Facilities may post such information but are responsible for the protection of confidential
information.
9. Partner Services and the Role of Partner Services Programs
Medical providers or their designee must explain to all newly diagnosed patients the
importance of notifying any sexual or needle-sharing partners that they may have been
exposed to HIV. Partner services is a cornerstone of HIV prevention efforts that provides an
opportunity for sexual or needle sharing contacts of a person living with HIV to be offered
testing in a timely manner, and if diagnosed with HIV infection, be linked into care. Every

New York State Department of Health AIDS Institute – Updated December 2023 Page 17 of 28
physician or other person authorized to order diagnostic testing is required to report HIV and
AIDS diagnoses to the health department. This report must include identifying information
about any contacts known to the clinical provider or provided to the clinical provider by the
patient. The HIV/AIDS Provider Portal described in Section 7, may be used to report cases,
including partners and to request assistance from the health department with partner
notification. As part of post-test counseling, the following must be provided to the patient:
1. An explanation of the importance of notifying sexual or needle sharing partners to
prevent further transmission, and to promote early access of exposed persons to HIV
testing, health care, and prevention services;
2. A description of notification options and assistance available to the protected individual;
3. A discussion about the risk of domestic violence and screening for domestic violence
prior to partner notification in accordance with the NYSDOH domestic violence
screening protocol;
4. The fact that known contacts, including a known spouse, will be reported to the health
department. That protected persons will also be requested to cooperate in contact
notification efforts of known contacts and that protected persons may name additional
contacts they wish to have notified with the assistance of the provider or authorized
public health officials; and
5. An explanation that the name and other information about the person living with HIV
will be protected during the contact notification process.
The NYSDOH Partner Services Program and the NYC Health Department Contact Notification
Assistance Program (CNAP) provide a wide range of services, including: performing
notifications; assisting patients with decision making; and consulting with health care providers.
In some situations, Partner Services Specialists can meet with the patient at the same time that
the laboratory results are given to assist with post-test counseling and development of a
partner notification plan. Additional NYSDOH/NYCDOHMH services may be available such as
assistance in locating persons who test positive but who do not return for their results. For
more information about partner services and how to contact partner services programs
throughout NYS, visit: https://health.ny.gov/diseases/communicable/std/partner_services/index.htm.
IMPORTANT POINT:
In recognition of the need for ongoing partner services beyond the time of initial diagnosis of
HIV, the 2016 updates to the NYSDOH Regulations formally prioritized partner services for
people who were previously diagnosed with HIV who are at elevated risk of transmitting the
virus to others. Several factors are considered as evidence of elevated risk of transmitting the
virus to others. These factors include that the individual: 1) is not engaged in health care
services, 2) is not virally suppressed; 3) has had a recent STD; or 4) has recently moved back to
NYS from another jurisdiction.
FAQ 25: Will the NYSDOH provide outreach to previously diagnosed patients to assist with
partner notification and/or link them to care or is this only done for newly diagnosed cases?
New York State Department of Health AIDS Institute – Updated December 2023 Page 18 of 28
Yes. The 2016 updates to the NYSDOH regulations specifically add patients to the contact
notification prioritization process who were previously diagnosed with HIV and are at elevated
risk of transmitting HIV to others. Partner services staff may also be available to help link and
re-engage these persons, if they are out-of-care. Updated law and regulations allow for sharing
of patient-level information to promote linkage and retention in care. For more information see
Section 10.
10. Confidentiality of HIV-Related Information in Medical and Social Services Records
New York has a long history of affording a high level of protection for HIV-related patient-
specific information. HIV-related information is any information that shows a person:
• Had an HIV-related test (such as an HIV antibody test, CD4 test, viral load test, PCR
[polymerase chain reaction]) test, or other test;
• Has HIV-infection, HIV-related illness, or AIDS;
• Has been exposed to HIV;
• Has any of these conditions and has information on any of their sexual contacts or
needle-sharing contacts.
Note: The offer of an HIV test is not considered confidential information.
Generally, HIV-related information can only be disclosed if the person signs an approved HIV
release form. The NYSDOH Form 2557 Authorization for Release of Medical Information and
Confidential HIV Related Information, is used for this purpose. This form allows for the release
of both HIV-related information and non-HIV-related information. The NYSDOH Form 5032
titled Authorization for Release of Health Information (Including Alcohol/Drug Treatment and
Mental Health Information) and Confidential HIV/AIDS Related Information is available for use
when information to be released includes information about alcohol or substance use that is
afforded additional protection under federal regulation 42 C.F.R. Part 2.
However, HIV-related information may be shared without an HIV-specific consent form by
medical providers and other clinical entities when needed to provide appropriate medical care
or treatment. For example:
• When making a referral for HIV-related care, such as when arranging HIV care for a
newly diagnosed person;
• Medical professionals working on the treatment team with the person’s existing
provider may discuss a patient’s HIV-related information with each other or with their
supervisors, but only to give necessary care;
• Medical personnel and certain other supervisory staff may have access to HIV-related
information to provide or monitor services if the person is in jail or prison or is on
parole.

New York State Department of Health AIDS Institute – Updated December 2023 Page 19 of 28
FAQ 26: When releasing HIV-specific information to another health care provider, is it
necessary to include a statement that the information may not be re-disclosed without the
protected individual’s consent?
Updates to the law add two additional items to the current list of exceptions to the
requirement that disclosures of HIV-related information be accompanied by a re-disclosure
statement. The additional exceptions are disclosure to:
• A health care provider or health facility when knowledge of the HIV-related information
is necessary to provide appropriate care;
• Third party reimbursors or their agents to the extent necessary to reimburse health care
providers for health services; provided that, where necessary, an otherwise appropriate
authorization for such disclosure has been secured by the provider.
FAQ 27: May a medical provider share confidential HIV information from a person’s medical
record with a case manager or other staff person from a community based organization
without a signed release?
No. In order to disclose HIV-related information from a medical record to a non-medical
provider for any purpose, including linkage to care, a specific signed release is required.
11. Sharing of Patient-Specific Information to Promote Linkage/ Retention in HIV Care
Information reported to the NYS and NYC HIV/AIDS Surveillance Systems is afforded the highest
level of protection, beyond the levels of protection afforded to HIV-related information
contained in medical records. It is essential that people living with HIV trust that state and local
health departments will safeguard the privacy of information included in surveillance systems.
Amendments to the New York State Public Health Law §2135 that went into effect on
September 1, 2010 allow state and local health departments to share information from the
HIV/AIDS surveillance system with health care providers for the purpose of linkage and
retention in HIV care. Since that time, post-test information provided to people with newly
diagnosed HIV included making these individuals aware that if a person with HIV appears to be
out of care, that person may be contacted by the medical provider or health department staff
to address barriers to entry into care and promote engagement in care. The 2010 amendments
were further clarified under the 2016 regulations to also include sharing of information with
care coordination entities (see FAQ §32-33).
Information That Can be Shared with Health Care Providers and Care Coordination Entities
The NYSDOH and the NYCDOHMH are able to share surveillance information for the purpose of
promoting linkage and retention in HIV care. Information most likely to be helpful for these
purposes will include:
• General information about care status;
• Patient relocation out of state or out of region;
• Report of death and date.

New York State Department of Health AIDS Institute – Updated December 2023 Page 20 of 28
IMPORTANT POINT: Amendments to New York State Public Health Law allow for the sharing of
information for the purpose of linkage and retention in HIV care. Therefore, information shared
is limited to the points listed above.
Who May Request Information from the NYS or NYC HIV Surveillance System
Information may be requested by:
• A licensed medical practitioner with a documented or verifiable diagnostic, clinical or
public health interest in the patient* (see Note)
o The licensed medical provider may be a physician, midwife, nurse practitioner or
physician assistant;
o The health care provider may designate an individual within their practice or at
an affiliated organization to submit a request and receive the information.
Examples of affiliated organizations may include: health home entities; care
coordination entities; Regional Health Information Organizations; and/or CBOs
involved in patient linkage and retention;
• Medical Director of a managed care organization or their designee, including persons
the Medical Director may designate from an affiliated health home or care coordination
agency.
• Care coordinators may request information from the NYS or NYC HIV Surveillance
System with a written documented affiliation with the licensed medical practitioner of
the patient.
*Note: If the NYSDOH does not have a record of the association between the patient and an
affiliated health care provider, CBO laboratory testing program or care coordination entity, the
NYSDOH will request information from the provider to document the association.
Requirements for Requesting Information
Eligible providers requesting information should be prepared to provide the following patient
information to the NYSDOH:
• Patient first and last name;
• Patient date of birth;
• Patient sex assigned at birth;
• Patient last known address and telephone number;
• Patient’s date of last contact with the requesting health provider (including laboratory
test type and date);
• If known and applicable, the following should also be provided:
o Medicaid Member Client Identification Number (CIN);
o New York State Department of Corrections and Community Supervision or
Criminal Justice System identifier (NYSID, DIN)

New York State Department of Health AIDS Institute – Updated December 2023 Page 21 of 28
When seeking information about patient linkage to care status, information provided regarding
patient relocation and reports of death may help health care facilities update their active
patients list and accurately report on their facility cascade of care.
Directions for Requesting Information
The HIV/AIDS Provider Portal is an electronic system which enables clinicians to meet their
Public Health reporting requirements electronically and provides a mechanism to submit to the
NYSDOH inquiries for patients residing anywhere in the state with diagnosed HIV infection who
are thought to be in need of assistance with linkage to, or retention in, HIV care. See Section 7
for more information about the HIV/AIDS Provider Portal.
NYC HIV Care Status Report System
Eligible NYC providers with patients who are out-of-care can use the NYC Health Department’s
HIV Care Status Reports System (CSR) to obtain NYC current care and vital status. Eligible NYC
providers may also call the NYC Health Department HIV Epidemiology and Field Services
Program’s Provider Call Line (NYC PCL) at 212-442-3388 for care status queries about ≤10
patients at one time.
For Urgent Requests:
In the event of an urgent request, such as an out-of-care pregnant or breastfeeding woman
living with HIV or individuals with suspected acute HIV infection, the NYSDOH or the
NYCDOHMH can be contacted for more immediate assistance.
For Providers Located in NYS outside of New York City: Urgent requests should be called into
the Bureau of HIV/AIDS Epidemiology at 518-474-4284 from 8:00am to 4:45pm Monday-Friday.
NYC Health Department Provider Call Line: For providers located within NYC, urgent requests
should be called into the NYC Health Department’s NYC PCL at 212-442-3388 from 8:00am and
4:45pm Monday-Friday.
Timeline for Receiving Information
Urgent requests will be responded to within 1 business day. For routine requests to the NYS
Provider Portal, the turn-around time will be within 1-3 business days. Depending on the
volume of requests at any given time, the turnaround time for routine requests may be up to 2
weeks. Queries submitted to the NYC CSR system are returned within 1 day.
FAQ 28: When should an eligible provider consider submitting a request for information
about an individual to the NYS HIV/AIDS Provider Portal (NYS Portal) or the NYC Provider Call
Line (NYC PCL) or NYC HIV Care Status Reports System (NYC CSR)?
Requests for information should be placed for persons who are not engaged in care for an
extended period of time and in-house efforts to reach an individual have been exhausted. The

New York State Department of Health AIDS Institute – Updated December 2023 Page 22 of 28
following are examples of vulnerable patients, situations and timeframes where submitting a
request for information to the various systems would be warranted:
• Pregnant or breastfeeding people living with HIV who are not on ART or are not known to
be engaged in care (NYS Portal, NYC PCL);
• Persons diagnosed with acute HIV infection who have not attended an appointment for 30
days and in-house efforts to reach the person were unsuccessful (NYS Portal, NYC PCL);
• Persons with a detectable viral load who have not attended an appointment for more than
120 days and in-house efforts to reach the person were unsuccessful (NYS Portal);
• Any person living with HIV with no evidence of HIV care, CD4 monitoring or viral load testing
for more than 6 months (NYS Portal, NYC PCL, NYC CSR).
Requests should not be placed for individuals who have consistently accessed care, are virally
suppressed and/or have an isolated instance of a missed appointment.
Additional information about the NYC CSR and NYC PCL for urgent requests can be found at
https://www1.nyc.gov/site/doh/health/health-topics/aids-hiv-care-status-reports-system.page.
Additional information about the NYS HIV/AIDS Provider Portal can be found in Section 7.
FAQ 29: How can a medical provider grant access to the HIV/AIDS Provider Portal or NYC Care
Status Reports System to others, and what tasks can those persons perform in the system?
A licensed medical provider can delegate HIV/AIDS Provider Portal access to a limited number
of users to carry out clearly defined tasks in the system. All users are able to submit electronic
reports of the Confidential Medical Provider HIV/AIDS and Partner/Contact Report Form (DOH-
4189). Only the licensed medical provider or a user with the appropriate role within the portal
may submit inquiries for patients who are thought to be in need of assistance with linkage to,
or retention in, HIV medical care. A licensed medical provider can name a designee to access
the NYC CSR for care status queries.
FAQ 30: When a medical provider grants access to the HIV/AIDS Provider Portal what
protections are in place to ensure confidential information remains protected?
Medical providers who designate access to the HIV/AIDS Provider Portal should convey to their
delegates the importance of protecting information related to HIV case reporting and out of
care follow-up as highly confidential and should ensure that designees have appropriate
training in HIPAA and New York State Public Health Law Article 27-F. The clinician and their
agents must not disclose information obtained from the HIV/AIDS Provider Portal to any other
person unless that person is legally authorized and has official reasons to obtain the
information.
FAQ 31: Can a health care provider who obtains information from the NYSDOH or the
NYCDOHMH share that information with other medical providers and/or with community-
based organizations?
Yes. Information provided by the NYSDOH or the NYCDOHMH to a health care provider or their
designee should be treated as other HIV-related information already contained within the

New York State Department of Health AIDS Institute – Updated December 2023 Page 23 of 28
patient record and so can be shared according to existing rules governing the sharing of HIV
medical information with other providers. Information must be handled and stored
confidentially and shared in accordance with HIPAA, New York State Public Health Law Article
27-F, and other applicable laws for sharing of HIV-related information.
FAQ 32: What is the process by which a health home or care coordination agency would be
able to request data from the surveillance system to assist with linkage and retention in care?
Licensed medical providers, including those who are part of Health Home networks, may
request data from the surveillance system for their current or past patients. The health care
provider may also designate an individual at an affiliated organization, such as a health home
entity or care coordination entity. Managed Care Plans may appoint organizations within a
Health Home network (Health Home lead agencies, care coordination agencies) to submit
requests to the surveillance system. Care coordinators may request information from the NYS
or NYC HIV Surveillance System with a written documented affiliation with the licensed medical
practitioner of the patient.
FAQ 33: How should care coordination entities and licensed medical providers manage the
process of designating multiple care coordinators from different entities?
Care coordination entities may request information from the NYS or NYC HIV Surveillance
System with written documented affiliation with the licensed medical practitioner of the
patient. It is strongly recommended that a single point of contact within a care coordination
entity is designated by a licensed medical provider to operate on their behalf. This single point
of contact should be a senior level staff member who accepts responsibility for protecting
privileged, confidential and/or protected health information (PHI) according to HIPAA, NYS
Public Health Law Article 27-F, and other federal and state privacy laws related to sharing and
storing HIV-related information.
FAQ 34: If a health care provider has a patient who did not keep their last appointment and is
unable to contact the individual, can the NYSDOH or the NYCDOHMH be of assistance?
Yes, they may be able to help in two ways: 1) The NYSDOH may be able to share information
with a health care provider on the current status of care or notification that the patient has
relocated out of state or region; 2) The NYSDOH staff may be able to assist with locating the
individual when an urgent need to return the individual to care can be established.
Information That Can be Shared with Health Care Providers and Care Coordination Entities
The NYSDOH and the NYCDOHMH are able to share surveillance information for the purpose of
promoting linkage and retention in HIV care. Information most likely to be helpful for these
purposes will include:
• General information about care status;
• Patient relocation out of state or out of region;
• Report of death and date.
FAQ 35: If a health care provider is having trouble getting prior medical records on a new

New York State Department of Health AIDS Institute – Updated December 2023 Page 24 of 28
patient, can the NYSDOH provide that patient’s past CD4 and viral load values?
No. The law authorizes sharing of surveillance data with a licensed medical practitioner with a
documented or verifiable diagnostic, clinical or public health interest in the patient for purposes
of linkage and retention in HIV care.
FAQ 36: Can information be requested for medical-legal documentation to confirm HIV status
in my medical records?
No. A clinician needing to establish medical-legal documentation of HIV status should order the
appropriate screening and confirmatory HIV testing. The intent of sharing data from the HIV
surveillance system is to promote linkage to HIV care, not to share HIV-related information with
a health care provider who is not aware of a patient’s HIV status. Information regarding HIV
diagnostic testing, including confirmation of an existing diagnosis, can be found at:
https://www.hivguidelines.org/hiv-testing-acute-infection/
FAQ 37: Given the growing importance of Regional Health Information Organizations (RHIOs),
what role can RHIOs play in promoting linkage/retention in care and to what extent is
information shared between the surveillance systems and the RHIOs?
In their role facilitating electronic sharing of health-related information between health care
providers, community-based organizations, and other types of entities, RHIOs can play an
important role providing access to patient-specific care status information, to the extent that
the patient has consented to such data sharing and the patient is receiving care from a health
care facility participating in the RHIO. For the purpose of expanded data sharing in supporting
patient linkage and retention in care, a RHIO is considered a care coordination entity.
Providers who are eligible to request information from the surveillance system may also be
affiliated with a RHIO. Such providers can request information directly from the surveillance
system rather than through their RHIO. In many cases, the RHIO may contain more complete
and readily accessible information such as exact viral load lab values, other diagnoses (such as
hepatitis C), and lists of recent providers. These data may be useful to care coordination. The
NYSDOH is conducting special projects to explore how to best align RHIOs and other public
health systems, such as conducting data matches between one RHIO and the surveillance
registry, under project-specific legal agreements. It should be noted that the amendments to
NYS Public Health Law §2135 that went into effect on April 1, 2014 do not currently allow for
data transfer from the surveillance system to a RHIO specifically. Any such data transfer would
have to be established under a project-specific legal agreement. The NYS and NYC Health
Department will continue dialogue with RHIOs and will explore promising practices while
recognizing the individuality of each RHIO. Additional information regarding RHIOs is available
at https://www.nyehealth.org/shin-ny/what-is-the-shin-ny/.
12. Health Department Assistance with Patient No-Show Follow-Up

New York State Department of Health AIDS Institute – Updated December 2023 Page 25 of 28
In instances where a patient with newly diagnosed HIV has not returned for post-test
counseling, the NYS HIV Partner Services (PS) and NYC Contact Notification Assistance Program
(CNAP) can assist the medical provider in locating the person to advise the individual to return
to the medical provider for post-test counseling. When the HIV diagnosis is verbally confirmed
by the testing provider and the provider requests such assistance, the HIV PS/CNAP Specialist
can perform post-test counseling on behalf of the provider.
If, in these cases, there are partners known to the medical provider, including spouses, and if
after repeated follow-up efforts the patient cannot be located or chooses not to return for
post-test counseling and/or domestic violence screening, the authorized public health official,
in consultation with the reporting medical provider, will determine whether notification of
known partners should proceed. This decision will primarily be based on the likelihood of the
index patient returning for post-test counseling, potential for risk of domestic violence, and the
risk to the potentially exposed spouse and/or other sexual and needle sharing partners known
to the medical provider. For partner services assistance in New York City, call 212-693-1419. In
other parts of the state, call 800-541-2437.
FAQ 38: In cases where a patient with a confirmed HIV diagnosis does not return for post-test
counseling and the health department has been called to assist with follow-up, will the health
department take responsibility for arranging for follow-up HIV care or does this remain with
the testing provider, even if the patient never returns for an appointment?
In such a case, the PS/CNAP Specialist will work with the testing provider to determine the best
course of action. PS/CNAP Specialists collaborate with testing and health care providers to
ensure patients understand their test results, discuss the importance of partner notification and
get linked to HIV care. Depending on the specific situation and the patient’s expressed
preference once located, the PS/CNAP Specialist may arrange for follow-up care or the testing
site may be responsible for this. Either way, the testing provider is responsible for reporting the
newly diagnosed case to the health department by completing the Medical Provider Report
Form. If the PS/CNAP Specialist arranges the appointment for follow-up care, the name of the
provider/ facility and date of appointment will be provided to the testing site to enable the site
to document this in the patient record, in accordance with their documentation requirements.
13. Reimbursement for HIV Testing
Reimbursement for HIV testing services is subject to a number of factors including the patient’s
health coverage, the setting offering the HIV test and other clinical considerations.
Health Coverage: The Affordable Care Act established ten essential health benefits which must
be covered by health plans. One of the essential health benefits is preventive screenings and
wellness services that have been proven cost effective by the U.S. Preventive Services Task Force
(USPSTF). Routine HIV testing is considered a preventive service. Routine HIV testing is highly

New York State Department of Health AIDS Institute – Updated December 2023 Page 26 of 28
cost effective and was awarded the highest “A” rating by the USPSTF for the following groups:
patients aged 15 to 65; younger or older patients at increased risk for HIV; and pregnant
women. Medicaid, Medicare and most insurance companies will cover the cost of HIV testing in
the primary care setting, especially for the groups noted above. Most individuals on Medicaid
are enrolled in a Medicaid Managed Care Plan and reimbursement for HIV testing is governed
by the negotiated fees between the Plan and the Provider, except in the cases of a federally
qualified health center (FQHC) (see additional information below). In most cases, in the primary
care setting, HIV testing will be covered by public and private health plans without a required
co-pay or patient cost sharing.
Setting: The Affordable Care Act does not necessarily require health plans to cover an HIV test
in every health care setting or whenever a patient accepts or is offered an HIV test. For example,
a health plan may cover HIV testing as part of a primary care visit but not during an emergency
room visit or not on an ongoing basis, absent documentation of a specific clinical indication.
Persons with private health coverage should check with their policy or insurance company to
determine in which settings HIV testing is covered and what co-pay may apply.
The HIV Primary Care Medicaid Program's HIV Testing visits were subsumed into the
Department's Ambulatory Patient Groups (APGs) Methodology effective July 1, 2011. Since that
time, only those FQHCs that are enrolled in the HIV Primary Care Medicaid Program (HPCMP)
who have opted out of APG's are able to access the HPCMP's HIV Testing codes.
Other Clinical Considerations: Reimbursement for HIV counseling or testing may be covered by
public and private health plans in a variety of settings when there is a specific clinical indication
for HIV testing, for example, when symptoms of acute infection or advanced HIV disease are
present or there is documentation of a specific risk behavior. In addition, under Medicaid, HIV
counseling that occurs in conjunction with a medical visit is a billable service when a physician
or other qualified health care professional spends time with the patient to discuss at some
length topics including, but not limited to: HIV disease; the importance of testing; and risk
factor reduction. Billing for such counseling services is through one of the Current Procedural
Terminology (CPT) codes for "Preventive Medicine, Individual Counseling" (CPT codes 99401-
99404) appropriate for the time spent with the patient and for which adequate documentation
is made in the patient's chart. HIV counseling services are distinct from evaluation and
management (E&M) services that may be reported and billed separately when performed. In
addition, the HIV test itself can be billed, as can the blood draw if a non-rapid test is performed,
in a manner appropriate to the provider setting (e.g., hospital outpatient clinic or diagnostic
and treatment center). All billing and payments are subject to, and paid in accordance with,
Medicaid regulation.
FAQ 39: Does the law require that HIV testing be provided free of charge if Medicaid,
Medicare or private insurance is not in place?

New York State Department of Health AIDS Institute – Updated December 2023 Page 27 of 28
No. The HIV testing law has not changed the way HIV testing is paid for. Reimbursement rules
for Medicaid and private insurers are subject to change. Patients who would like information
about free or anonymous testing sites may call 1-800-541-AIDS (2437).
14. Occupational Exposure
For information about HIV testing in instances of occupational exposure, please see the
document titled Occupational Exposure and HIV Testing: Fact Sheet and Frequently Asked
Questions available at
https://www.health.ny.gov/diseases/aids/providers/testing/docs/occupational_exposure.pdf
15. NYSDOH Expectations for Compliance and Enforcement Activities
The NYSDOH has worked collaboratively to assist providers in complying with HIV testing laws
since the 2010 amendments went into effect. With the adoption of the 2016 amendments and
now these 2023 updates, the department expects that all facilities and providers have
implemented the routine offer of testing and other provisions of the law, and that health care
facility policies and protocols are in full alignment with public health law governing HIV testing.
If technical assistance or training is needed, please email [email protected]. Online patient
complaints can be filed at: https://www.health.ny.gov/diseases/aids/providers/forms/informedconsent.htm.
All complaints are reviewed by the NYSDOH. Action will be taken with the provider or facility as
appropriate.
FAQ 40: Will the NYSDOH require any data be reported from health care facilities or private
practitioners with regard to activities mandated under this law?
No. There are no new reporting requirements included in the Law. Medical providers must
continue to complete and submit the NYS Medical Provider HIV/AIDS and Partner/Contact
Report Form (PRF) within 14 days to report new diagnoses of HIV or AIDS, previously diagnosed
persons who are new to clinic, and/or persons needing partner services. As has been the case,
New York City physicians are required to send their reports to the NYC Health Department. See
Section 7 for more information or call the NYSDOH at 518-474-4284 or NYC Health Department
at 212-442-3388.
16. Access to HIV Information for Medical Researchers
Effective March 28, 2017, Public Health Law §2782(1)(r) allows disclosure of confidential HIV-
related information to qualified researchers for medical research purposes upon approval of a
research protocol under applicable State or federal law. This update to the Public Health Law is
intended to improve the ability of qualified researchers to conduct high quality, Institutional

New York State Department of Health AIDS Institute – Updated December 2023 Page 28 of 28
Review Board (IRB)-approved research related to improving the medical care and treatment of
persons living with HIV. Researchers at academic medical centers, with approval from the
institution and the institution’s IRB, may access confidential HIV-related information from
medical records of patients of the academic medical center for the purposes of improving the
medical care and treatment of persons living with HIV.
FAQ 41: What are the definitions of “Qualified Researcher” and “Medical Research”?
A “Qualified Researcher” is any Principal Investigator of an IRB-approved medical research
study. “Medical Research” includes basic research, applied research or translational research
conducted to advance knowledge in the field of HIV.
IMPORTANT POINT:
Researchers at academic medical centers who access confidential HIV-related information from
medical records of patients with approval from the institution and the institution’s IRB must, in
all cases, ensure that this information is maintained and kept confidential in accordance with
HIPAA regulations.
FAQ 42: Will qualified researchers be allowed to access information from the HIV surveillance
system?
No. Researchers may not access patient-specific HIV-related information from the HIV
surveillance system. Researchers at academic medical centers, with approval from the
institution and the institution’s IRB, may access confidential HIV-related information from
medical records of patients of the academic medical center for the purposes of improving the
medical care and treatment of persons living with HIV.
