
Maternal and Child
Health Services Title V
Block Grant
Maryland
FY 2023 Application/
FY 2021 Annual Report
Created on 8/11/2022
at 8:37 PM

Table of Contents
I. General Requirements
4
I.A. Letter of Transmittal
4
I.B. Face Sheet
5
I.C. Assurances and Certifications
5
I.D. Table of Contents
5
II. Logic Model
5
III. Components of the Application/Annual Report
6
III.A. Executive Summary
6
III.A.1. Program Overview 6
III.A.2. How Federal Title V Funds Complement State-Supported MCH Efforts 10
III.A.3. MCH Success Story 11
III.B. Overview of the State
12
III.C. Needs Assessment FY 2023 Application/FY 2021 Annual Report Update
18
III.D. Financial Narrative
23
III.D.1. Expenditures 25
III.D.2. Budget 27
III.E. Five-Year State Action Plan
29
III.E.1. Five-Year State Action Plan Table 29
III.E.2. State Action Plan Narrative Overview 30
III.E.2.a. State Title V Program Purpose and Design 30
III.E.2.b. State MCH Capacity to Advance Effective Public Health Systems 32
III.E.2.b.i. MCH Workforce Development
32
III.E.2.b.ii. Family Partnership
34
III.E.2.b.iii. MCH Data Capacity
36
III.E.2.b.iii.a. MCH Epidemiology Workforce
36
III.E.2.b.iii.b. State Systems Development Initiative (SSDI)
37
III.E.2.b.iii.c. Other MCH Data Capacity Efforts
39
III.E.2.b.iv. MCH Emergency Planning and Preparedness
42
III.E.2.b.v. Health Care Delivery System
44
III.E.2.b.v.a. Public and Private Partnerships
44
III.E.2.b.v.b. Title V MCH – Title XIX Medicaid Inter-Agency Agreement (IAA)
45
III.E.2.c State Action Plan Narrative by Domain 48
State Action Plan Introduction
48
Women/Maternal Health
49
Created on 8/11/2022 at 8:37 PM
Page 2 of 296 pages

Perinatal/Infant Health
75
Child Health
101
Adolescent Health
116
Children with Special Health Care Needs
127
Cross-Cutting/Systems Building
164
III.F. Public Input
172
III.G. Technical Assistance
173
IV. Title V-Medicaid IAA/MOU
174
V. Supporting Documents
175
VI. Organizational Chart
176
VII. Appendix
177
Form 2 MCH Budget/Expenditure Details
178
Form 3a Budget and Expenditure Details by Types of Individuals Served
184
Form 3b Budget and Expenditure Details by Types of Services
187
Form 4 Number and Percentage of Newborns and Others Screened Cases Confirmed and
Treated
190
Form 5 Count of Individuals Served by Title V & Total Percentage of Populations Served by
Title V
193
Form 6 Deliveries and Infants Served by Title V and Entitled to Benefits Under Title XIX
197
Form 7 State MCH Toll-Free Telephone Line and Other Appropriate Methods Data
199
Form 8 State MCH and CSHCN Directors Contact Information
201
Form 9 List of MCH Priority Needs
204
Form 9 State Priorities – Needs Assessment Year – Application Year 2021 206
Form 10 National Outcome Measures (NOMs)
207
Form 10 National Performance Measures (NPMs)
248
Form 10 State Performance Measures (SPMs)
262
Form 10 Evidence-Based or –Informed Strategy Measures (ESMs)
267
Form 10 State Performance Measure (SPM) Detail Sheets
278
Form 10 State Outcome Measure (SOM) Detail Sheets
283
Form 10 Evidence-Based or –Informed Strategy Measures (ESM) Detail Sheets
284
Form 11 Other State Data
294
Form 12 MCH Data Access and Linkages
295
Created on 8/11/2022 at 8:37 PM
Page 3 of 296 pages

I. General Requirements
I.A. Letter of Transmittal
Created on 8/11/2022 at 8:37 PM
Page 4 of 296 pages

I.B. Face Sheet
The Face Sheet (Form SF424) is submitted electronically in the HRSA Electronic Handbooks (EHBs).
I.C. Assurances and Certifications
The State certifies assurances and certifications, as specified in Appendix F of the 2021 Title V Application/Annual Report
Guidance, are maintained on file in the States’ MCH program central office, and will be able to provide them at HRSA’s request.
I.D. Table of Contents
This report follows the outline of the Table of Contents provided in the “Title V Maternal and Child Health Services Block Grant
To States Program Guidance and Forms,” OMB NO: 0915-0172; Expires: January 31, 2024.
II. Logic Model
Please refer to figure 4 in the “Title V Maternal and Child Health Services Block Grant To States Program Guidance and
Forms,” OMB No: 0915-0172; Expires: January31, 2024.
Created on 8/11/2022 at 8:37 PM
Page 5 of 296 pages

III. Components of the Application/Annual Report
III.A. Executive Summary
III.A.1. Program Overview
Maternal and Child Health in Maryland: Maryland Department of Health is committed to ensure lifelong health and
wellness for all Marylanders. This vision can be achieved through disease prevention, access to care, quality management,
and community engagement.
Maryland has a history of strong funding for health and social service programs including Maternal and Child Health
programs. During FY 2021, the federal Title V award was $11,872,645 and the state match was $10,999,716 meeting the
required match of $3 for every $4 federal. In FY 2021, Title V provided direct, enabling, and public health systems services to
approximately 228,412 pregnant people, infants, children, including children with special health care needs, and
adolescents.
The Role of Title V: The mission of Maryland Title V is to protect, promote, and improve the health and well-being of
women, infants, children, and adolescents, including those with special health care needs. Maryland Title V strengthens the
Maternal and Child Health (MCH) infrastructure within the state to ensure the availability, accessibility and quality of primary
and specialty care services for women, infants, children, including those with special health care needs, and adolescents.
As Maryland’s Title V Maternal and Child Health Block Grant agency, the Maryland Department of Health’s Maternal
and Child Health Bureau (MCHB) provides the leadership infrastructure to implement strategies focused on improving the
health and well-being of MCH populations across the state. MCHB staff partners across other Bureaus and Offices within
the Department and collaborates with other state agencies to fulfill Title V’s mission.
Through Title V, MCHB addresses ongoing and emerging health care priorities across the five MCH population
domains: women/maternal health, perinatal health, child health, children with special health care needs, and adolescent
health. Title V staff continued to respond to the COVID-19 pandemic in FY21 by conducting surveillance and outreach
activities, permitting flexibility with partners in funding, developing guidance for programs, rapidly providing resources and
information to partners, and addressing the emergent needs of families.
Maryland Title V implements evidence-informed strategies to support the state’s identified priorities and selected
National Performance Measures (NPMs), as well as State Performance Measures (SPMs) that align with other health
improvement initiatives in the state. These Title V priorities and performance measures provide a centralized framework
and unifying plan for MCH initiatives.
Maryland Title V funds support direct, enabling, and public health systems services at the state health department, all
twenty-four of the state’s local health departments, higher educational institutions, community-based organizations, and
health care systems. Partnerships are key to the success of Title V to expand reach to the MCH population and address
their needs. Maryland Title V also serves as the central connector amongst various maternal and child health initiatives.
Finally, Title V funding supports critical public health infrastructure such as epidemiology, surveillance, program managers
and other initiatives which are not covered by state funding.
This annual report and application provides an overview of Maryland Title V activities and accomplishments across
the five domains, as well as continued progress towards the selected NPMs and SPMs.
Program Framework: The three guiding frameworks for Maryland Title V are the Life Course Model, Socio-Ecological
Framework, and the Health Equity Framework. The life course model recognizes that structurally patterned exposures
during critical and sensitive periods of the life course results in shifts in health trajectories that may endure despite later
interventions.
[1]
The Socio-Ecological Model considers the impact of and interplay between individual factors, relationships,
community factors and societal factors such as policies on health and health outcomes. The Health Equity Framework
brings together the Life Course and Socio-Ecological Model to look at class, race/ethnicity, gender, sexual orientation, and
immigration status and recognizes how institutional and structural inequities can create unequal living conditions. The
unequal living conditions can then shape the health behaviors and health outcomes.
Created on 8/11/2022 at 8:37 PM
Page 6 of 296 pages

Needs Assessment and State Action Plan: Title V completed an updated Needs Assessment and State Action plan in FY
2020. Through a ten-month process that included both primary and secondary data collection and analysis, nine National
Performance Measures were identified. Title V has also identified the need for four additional State Performance Measures
to align with statewide health improvement plans.
Title V Population Domains:
Women/ Maternal Health: Maryland has identified “ensuring all birthing people are in optimal health before, during, after
birth” as a priority need in Women/Maternal Health. To this end, the National Performance Measures selected include NPM
13.1 Percent of women who have a preventive dental visit during pregnancy, and NPM 14.1 Percent of women who smoke
during pregnancy. There are two State Performance Measures: SPM 1: Overdose Mortality Rate for Women, ages 15-49 in
Maryland per 100,000 population and SPM2: Excess Rate of Black Non-Hispanic Severe Maternal Morbidity Rate to White
Non-Hispanic Severe Maternal Morbidity rate. Both SPMs align with Maryland’s Statewide Integrated Health Improvement
Strategy (SIHIS) that focuses on maternal and child health and decreasing overdose fatalities.
NPM 13.1: Percent of women who have a preventive dental visit during pregnancy: Title V continues to work
with the Office of Oral Health (OOH) to update and disseminate the “Oral Health Care During Pregnancy: Practice
Guidance for Maryland’s Prenatal and Dental Providers and Oral Health During Pregnancy – a health literacy/social
marketing campaign.
NPM 14.1: Percent of women who smoke during pregnancy: Title V funds programs at the local health
department who provide services to prenatal/postpartum people through home visiting, home birth certification, early
intervention, and family planning clinics, routinely screen women for tobacco use and offer referrals to the state’s
QuitLine. The local health departments report the number of women referred on a quarterly basis. Additionally, in
partnership with the Center for Tobacco Control and Prevention, Title V is able to track the total number of pregnant
people who are referred by all providers throughout the state. The Maryland Family Planning Program has also
worked to implement SBIRT (Screening, Brief Intervention, Referral to Treatment) into their clinic sites.
SPM 1: Number of Overdose Mortalities for Women, ages 15-49 in Maryland per 100,000 population. Title V
has added a State Performance Measure related to Overdose Mortality Rate for women, ages 15-49 to reflect the
urgent need to address the increasing number of overdose deaths in the state and align with the Statewide
Integrated Health Improvement Strategy (SIHIS). SIHIS is designed to engage State agencies and private sector
partners to collaborate and invest in improving health, addressing disparities, and reducing overall health care costs.
The strategy has identified opioid overdose fatalities as a population health priority as well as maternal health. In
Maryland, overdose deaths are the leading cause of maternal mortality. Strategies to prevent overdose fatalities
include facilitating linkages to substance use disorder treatment using the prenatal risk assessment tool with State
Medicaid and Centers for Disease Control and Prevention Overdose Data to Action partners, updating the
postpartum infant maternal referral form, developing a linkage to care toolkit for providers of birthing people, and
understanding opioid use through PRAMS surveillance. In addition, Maryland is a recipient of the Centers for
Medicare and Medicaid Innovation Maternal Opioid Misuse Model to partner with Managed Care Organizations for
robust case management for treatment and addressing social needs.
SPM 2: Excess Rate of Black Non-Hispanic Severe Maternal Morbidity Rate to White Non-Hispanic Severe
Maternal Morbidity rate: In order to address maternal disparities, Title V is aligning with the Statewide Integrated
Health Improvement Strategy goals to reduce the disparity gaps within the severe maternal morbidity rate. Overall,
work towards addressing disparities will improve health for all Maryland birthing people. Title V supports activities and
efforts with federal and matching funds to improve maternal health and decrease disparities through the Perinatal
Support Program, Perinatal Neonatal Quality Collaborative, Maternal Mortality Review Program, home visiting and
care coordination through the local health departments, and collaboration with the State Maternal Health Innovation
Program.
Perinatal/Infant Health: Maryland has identified the following priority needs in Perinatal/Infant Health as “ensuring that all
babies are born healthy and prosper in their first year” by addressing the racial disparities in infant outcomes. The National
Created on 8/11/2022 at 8:37 PM
Page 7 of 296 pages

Performance Measures selected for this population domain include NPM 3: Percent of Very Low Birth Weight (VLBW) and
Low Birth Weight (LBW) infants delivered at appropriate level hospitals; NPM 4: Percent of infants ever breastfed; and NPM
5: Percent of infants placed on their back to sleep.
NPM 3: Percent of VLBW and LBW infants born at appropriate level hospitals: Title V supports several
initiatives that focus on improving perinatal/infant health including the Maryland Perinatal System Standards that
provides standards for all Maryland birthing hospitals. Compliance to these standards are assessed by the Maryland
Institute for Emergency Medical Services Systems (MIEMSS) and the Morbidity, Mortality, Quality, Review
Committee. Other initiatives include the Maryland Perinatal Support Program, and the Maryland Perinatal Quality
Collaborative.
NPM 4: Percent of infants ever breastfed: Recognizing the importance of breastfeeding for optimal health in
childhood and across the life course, Title V supports activities that promote breastfeeding. Local health
departments provide breastfeeding information/education through home visiting and care coordination programs.
Title V also collaborates with the Maryland WIC program on the Breastfeeding Policy Committee that provides
support to hospitals across the state to become certified “Breastfeeding Friendly,” through maternity staff training
modules and physician webinars.
NPM 5: Percent of infants placed on their back to sleep: Maryland’s infant health domain NPM is the placement
of infants on their back to sleep, as sleep-related infant deaths are the third leading cause of overall infant mortality
and the leading cause of post-neonatal deaths in Maryland. Through Title V funding, local health departments and
Babies Born Healthy Initiative, infant safe sleep education and portable cribs are distributed. Title V supports local
Fetal and Infant Mortality Review (FIMR) activities to investigate causes of infant death. Title V also supports infant
mortality reduction activities in local health departments across the state through home visiting and care coordination
services for high-risk women and infants that screen and refer for mental health and substance use, and provide
education on prenatal nutrition support.
Children’s Health: Maryland has identified the following priority needs for Child Health, “ensuring that all children have the
opportunity to develop and reach their full potential.” Title V efforts in Maryland continue to focus on children with Medicaid
who receive a developmental screen (NPM 6). Title V has added a State Performance Measure (SPM) 3 on the receipt of
primary care during early childhood as well as a State Performance Measure related to childhood asthma (SPM 4). In an
effort to align with the Statewide Integrated Health Improvement Strategy (SIHIS), Maryland also has the SPM 4: Annual ED
visit per 1,000 for ages 2-17 for the primary diagnosis of asthma.
NPM 6: Percent of children age 19-35 who have completed a developmental screen: Through Title V
funding, local health departments implement programs and services related to child development. Local
health departments that choose to focus on child health services support programs such as lead case
management, early intervention, and hearing and vision screening. Parents enrolled in home visiting
programs (maternal health services) also receive information regarding the importance of child
developmental screenings through their medical home.
SPM 3: Receipt of primary care during early childhood: (Percent of children enrolled in Medicaid who
reached 15 months who had 5 or more well care visits in their first 15 months of life) Title V will continue to
monitor and track receipt of primary care in early childhood through Medicaid data. Title V staff at Local Health
Departments provide essential services such as vaccinations and vision and hearing screenings. Title V also
funds home visiting programs who help coordinate and promote primary care services. Finally, Title V will
partner with the Maryland State Department of Education (MSDE) for school-based health centers and
school health services.
SPM 4: Number of ED visits per 1,000 for children ages 2-17 with a primary diagnosis of asthma:
Beginning in FY 2022, local health departments will have the option to use Title V funds to support asthma
programming/services. These programs/services will include asthma home visiting, asthma collaboratives,
and/or regional partnerships. Title V will also partner with the Environmental Health Bureau to support
existing asthma programs such as asthma home visiting through the State Plan Amendment (SPA) and the
Created on 8/11/2022 at 8:37 PM
Page 8 of 296 pages

Children’s Health Insurance Program (CHIP) in the jurisdictions across the state that have high incidence of
emergency department visits for asthmatic children.
Adolescent Health: Title V has identified as priority needs in adolescent health to “Ensure that adolescents ages 12-17
receive comprehensive well visits that address physical, reproductive, and behavioral health needs” and “ensure that
adolescents with asthma and their families have the tools and support necessary to manage their conditions.” There is one
NPM, Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year (NPM 10) and SPM 4:
Annual ED visit per 1,000 for ages 2-17 for the primary diagnosis of asthma. NPM 10 was selected since it informs the
SPM.
NPM 10: Percent of adolescents ages 12 through 17, with a preventive medical visit in the past year: Title V
supports adolescent health through funding to local health departments for school-based health services. These
services include physical health assessments as well as screening and referral for mental health and/or substance
use. Additionally, Title V funds support an Adolescent Health Coordinator at the state level who manages the Sexual
Risk Avoidance, Pregnancy Responsibility Education Program and Maryland Optimal Adolescent Health Program
grants. Starting in FY2023, Title V will also oversee the Maryland School-Based Health Center Program.
SPM 4: Number Asthma ED visits per 1,000 for ages 2-17: Beginning in FY 2022, local health departments will
have the option to use Title V funds to support asthma programming/services. These programs/services will include
asthma home visiting, asthma collaboratives, and/or regional partnerships. Title V will also partner with the
Environmental Health Bureau to support existing asthma programs such as asthma home visiting through the State
Plan Amendment (SPA) and the Children’s Health Insurance Program (CHIP) in the jurisdictions across the state
that have high incidents of emergency department visits for asthmatic children and adolescents.
Children with Special Health Care Needs (CSHCN): Maryland has identified, “ensure optimal health and quality of life for
all children and youth with special health care needs and their families by providing all services within an effective system of
care in alignment with the six core outcomes'' as its priority area. These priorities focus on medical home access and
transition support/services for children and youth with special health care needs (CYSHCN).
NPM 11: Percent of children with and without special health care needs, ages 0-17, who have a medical
home: Maryland recognizes that the medical home approach to providing comprehensive and high-quality primary
care is the best practice for children with and without special health care needs. Despite the model’s introduction
fifty-plus years ago, more progress needs to be made for universal implementation. OGPSHCN will continue to
explore challenges to medical home implementation in MD and strategize effective outreach and training
opportunities.
NPM 12: Percent of adolescents with and without special health care needs, ages 12-17, who received
services to prepare for the transition to adult health care: Maryland continues the overarching goal of
increasing the percent of adolescents with and without special health care needs who have received the services
necessary to make transitions to adult health care but will be conducting a thorough analysis of current strategies
and evaluating the need for revised strategies in SFY2023.
Cross Cutting: SPM 5: Percentage of MCH Bureau committees/workgroups that include community
members/persons with lived experience
For FY 2023, Maryland Title V added a cross cutting state performance measure. Title V continues to shift towards achieving
equity and reducing disparities. Title V will work on reviewing various committees and workgroups to include community
members/persons with lived experience.
[1]
Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, Geronimus AT. Life Course Approaches to the Causes of Health Disparities. Am J
Public Health. 2019;109(S1):S48-S55. doi:10.2105/AJPH.2018.304738
Created on 8/11/2022 at 8:37 PM
Page 9 of 296 pages

III.A.2. How Federal Title V Funds Complement State-Supported MCH Efforts
Through the Title V Maternal and Child Health Services Block Grant, Maryland is able to provide core public health
services funding to all 24 jurisdictions (23 counties and Baltimore City) in the state to advance vital maternal and
child health services and initiatives that are specific to the needs of each community. Funding is used for direct,
enabling, and public health systems services/initiatives for children, children and youth with special health care
needs, and maternal health. Additionally, funds are used for population-based services through community education
of emerging public health issues and through the continued development and advancement of public health
infrastructure to ensure the health and well-being of Title V eligible populations. These services highlight the mission
and vision of the Department of Health’s Prevention and Health Promotion Administration, in which Maryland Title V
resides.
Without critical Title V funding, the State would be unable to maintain the level of support necessary to continue to
successfully improve the health outcomes of the State’s women, infants, children, adolescents and children/youth with
special health care needs. Title V funds State staff who serve essential roles for the MCH population such as
epidemiology and surveillance, program management and coordination, policy development and analysis,
partnership coordination, and outreach. Title V funding supports the efforts of local health departments to advance
Title V priorities at the community level through the implementation of evidence-based and evidence-informed
programs, activities, and initiatives.
Each fiscal year, Maryland receives approximately $11,800,000 in federal Title V funding for maternal and child
health services. The state’s FY 1989 required Maintenance of Effort (MOE) amount is $8,262,484. Historically,
Maryland has matched federal Title V funds above the required MOE to ensure that services are adequately funded
across all population and service domains. In FY 2021, the state match totalled $10,999,716 and supported
services such as family planning/reproductive health clinics, care coordination services for pregnant women (Babies
Born Healthy), Child Fatality Review (CFR), various perinatal infrastructure projects, and medical day care for
children and youth with special health care needs.
Created on 8/11/2022 at 8:37 PM
Page 10 of 296 pages

III.A.3. MCH Success Story
The Title V Program works with and funds the network of Maryland Child Abuse Medical Providers (CHAMP). They
are a group of medical professionals who are experts in the area of child maltreatment. CHAMP’s goal is to develop
medical expertise related to maltreatment in Maryland. CHAMP activities include: recruiting and training medical
professionals in the area of child maltreatment, providing ongoing training and support for medical professionals
working in the field, providing expert medical evaluations when concerns of child maltreatment arise, providing
consultation to the Child Protective Services (CPS), law enforcement, state attorney’s offices, pediatricians and
other professionals.
One of the CHAMP initiatives includes the Forensic Nurse Examiner (FNE) Training Program at Frederick Health
Hospital that provides technical assistance and guidance. The FNE Training program was recently commended by
a Maryland regional medical center. Healthcare facilities not only are required to provide physical care for victims of
abuse, but also have a program for the forensic exam and evidence collection for cases that involve law
enforcement. Many facilities in the more rural parts of Maryland cannot afford to shoulder their own training program.
The Regional Medical Center acknowledged and praised the FNE training for providing didactic and clinical
simulation training experiences necessary for a nurse to meet the requirements of the Maryland Board of Nursing to
obtain an FNE certification. The FNE program also provided information, material, updated references, and time to
discuss programmatic changes. The Regional Medical Center called the training center a “beacon for the State of
Maryland.”
Created on 8/11/2022 at 8:37 PM
Page 11 of 296 pages

III.B. Overview of the State
Introduction
Maryland is a small but diverse state comprising 24 jurisdictions, including 23 counties and the city of Baltimore.
According to the U.S. Census Bureau, Maryland had an estimated population of nearly 6.2 million in 2020, and
ranked as the nation’s 18th most populous state. However, Maryland ranks as the ninth smallest state according to
land area. Although a small state in size and population, Maryland has great geographic diversity. The State is
characterized by mountainous rural areas in the western part of the State, densely populated urban and suburban
areas in the central and southern regions along the I-95 corridor between Baltimore and Washington DC, and flat
rural areas on the eastern shore. Maryland is geographically unique with the Allegheny Mountains and Chesapeake
Bay separating its western and eastern regions from the population centers of the state. These geographic
“barriers'' often create special challenges in the procurement of health care services due to lack of access
(transportation and distance), lack of providers, and lack of specialty care.
The State’s Maternal and Child Health (MCH) population includes an estimated 1.2 million women of childbearing
age (ages 15-45), 1.5 million children and adolescents (ages 0-19), and 368,767 young adults (ages 20-24) in 2020.
According to the National Survey of Children’s Health in 2019-2020, an estimated 273,531 Maryland children and
youth (ages 0-17) have special health care needs (NSCH 2019-2020 Survey).
Maryland’s Health Care Environment
Maryland’s health care system includes 24 local health departments (LHDs), 77 hospitals, 21 federally qualified
health centers (FQHCs), the Medicaid Program, private insurers, regulatory agencies, provider groups, advocacy
groups and countless health practitioners. MCH specific resources include 32 birthing hospitals, nearly 2,600
pediatricians and/or adolescent practitioners, over 1,200 obstetricians and/or gynecologists, and nearly 1,900
family/general practitioners. Maryland is home to Johns Hopkins University consistently ranked as one of the nation’s
top hospitals and several of the best diagnostic centers for developmental conditions in children, including Kennedy
Krieger Institute, University of Maryland Division of Behavioral and Developmental Pediatrics, Sheppard Pratt and
Mount Washington Pediatric Hospital.
Maryland was one of the initial six states approved to begin a Health Benefit Exchange under the Affordable Care
Act (ACA). The Maryland Health Benefit Exchange, known as Maryland Health Connection (MHC), was launched in
2013 and has implemented ongoing efforts to increase knowledge among individuals and communities about the
importance and availability of health insurance coverage. Within local health departments and through regional
consumer assistance organizations, health navigators assist individuals with applying for health insurance options
available through MHC. Maryland also expanded Medicaid eligibility through the ACA to cover income eligible
adults ages 19-64 regardless of parental status.
The Maryland Medicaid Program serves as the major source of publicly sponsored health insurance coverage for
children, adolescents, and pregnant women. According to Medicaid data (December 2021), there were 1,674,096
Marylanders who were enrolled in Medicaid. During calendar year 2020, 688,533 children and adolescents (ages 0-
22) were enrolled in the Medicaid Program at some point during the year, representing a 4 percent increase from
2020 enrollment. Maryland has generally been supportive of expanding health insurance coverage for uninsured
children and pregnant women. The Maryland Children's Health Program (MCHP) began operating as a Medicaid
expansion program on July 1, 1998. The MCHP program expanded comprehensive health insurance coverage to
children up to the age of 19 with family incomes at or below 200% of the federal poverty level (FPL). In 2001,
Created on 8/11/2022 at 8:37 PM
Page 12 of 296 pages

Maryland initiated a separate children's health insurance program expansion, MCHP Premium. MCHP also provides
insurance coverage for pregnant women with incomes between 185% and 250% of the federal poverty level. In
2020, according to the National Vital Statistics System, Medicaid covered hospital delivery costs for 39.2 percent of
Maryland births.
Health care workforce shortages/distribution affects many Maryland communities. There are federally designated
health professional shortage areas and medically underserved areas/populations located throughout the State,
particularly in urban and rural areas. This shortage is expected to be exacerbated by the COVID-19 Pandemic and
the loss of health care workers due to fatigue and burnout. Data from the HRSA Data Warehouse indicates that 19
of Maryland's 24 jurisdictions are currently either entirely or partially federally designated as health professional
shortage areas for primary care and/or dental services, and 18 are shortage areas for mental health. Twenty three of
the State’s 24 jurisdictions are currently either fully or partially designated as medically underserved areas. Federally
qualified health centers are located in 22 jurisdictions in the State.
Maryland was ranked by the Census Bureau as the wealthiest state in the nation as measured by median household
income in 2020. Its health care environment is also one of the most robust in the nation as measured by physician to
population ratio and the availability of internationally recognized high quality health services. In spite of Maryland's
relative affluence and significant health care assets, progress on health measures for the State is often mixed due to
the geographic factors that limit access to care.
The 2021 Kids Count Data Book (Annie E. Casey Foundation), ranked Maryland 24 in overall child well-being,
slipping three spots from its ranking in 2020. Despite the State’s overall wealth, Maryland still faces many
challenges related to maternal and child health outcomes. Poverty, which is a significant social determinant of health,
measured 9.0% in 2020 according to the American Community Survey. The infant mortality rate in Maryland
continues to see stable declines from 7.4 in 2005 to 5.7 in 2020, a 3% decline from 2019. However, in Maryland
there remains persistent disparities in infant mortality rates by race/ethnicity. For example, in 2020 the infant
mortality rate for Non-Hispanic Whites was 3.3 compared to 9.9 for Non-Hispanic Blacks. Additionally, 12.4% of the
state’s children (ages zero to five) live in poverty and 14% of children (age 0-18) do not have health insurance based
on Census data. For children with special health care needs, successful transition to adult health care is often
inconsistent due to the lack of adult specialty care providers for congenital and childhood onset conditions.
Maternal and Child Health Bureau and Title V
Maryland’s lead public health agency is the Maryland Department of Health (MDH), led by Secretary Dennis
Schraeder, who was appointed in 2021. Maryland Department of Health houses Title V in the Maternal and Child
Health Bureau (MCHB) within the Prevention and Health Promotion Administration (PHPA). The Bureau’s mission is
to reduce health inequities and improve the health and wellbeing of all individuals, families, and communities in
Maryland. The vision for the Bureau is that all individuals and families are valued, safe, and informed, with equitable
access to resources and services. The tagline for the bureau is “Healthy pregnancies, healthy children, healthy
families, healthier communities.”
MCHB focuses on prevention across the lifespan for children and women of childbearing age and serves as MDH's
primary prevention unit for unintended and adolescent pregnancy; infant mortality and low birth weight reduction;
breastfeeding promotion, preventive and primary care for children and adolescents; and systems development for
children and youth with special health care needs. MCHB also has the lead responsibility for reducing racial
Created on 8/11/2022 at 8:37 PM
Page 13 of 296 pages

disparities/inequities in perinatal health outcomes for women and children.
Key goals of the Maternal and Child Health Bureau, which intersect with Title V priorities, include improving
pregnancy and birth outcomes, improving the health of children and adolescents, including those with special health
care needs, assuring access to quality health care services, eliminating health disparities, and strengthening the
MCH infrastructure. Title V programs and services are provided across the three levels of the MCH pyramid to
protect and promote the health of all women, children, and families.
Title V funds support programs and activities in three of the four offices of the Maternal Child Health Bureau. These
offices include the Office of Family and Community Health Services (OFCHS); the Office of Quality Initiatives (OQI);
and the Office for Genetics and People with Special Health Care Needs (OGPSHCN). In addition, Title V funds
support the Operations Unit for the Bureau and the Healthcare Systems Coordination and School-Based Health
Centers Unit.
Title V and the Bureau collaborate with other MDH units as well as other State agencies to address access to
prenatal care, breastfeeding promotion, childhood lead screening, access to family planning, screening and
treatment of sexually transmitted infections, immunizations, postpartum depression, school based health, substance
use screening and referral, and tobacco use prevention. A leading strategy is systems building through partnerships
with Medicaid and Behavioral Health (also housed within MDH); other State agencies (e.g., Education, Juvenile
Services); local health departments; academic institutions; health care systems, professional organizations (ACOG,
AAP); private non-profits; FQHCs; and community based organizations.
Title V provides $4.4 million in funding to all 24 local health departments each year to drive improvements in the
health of women, children, and families at the community level. Title V works with state and local agencies to ensure
coordination of services for all women and children, but particularly those with limited access to care and children
and youth with special health care needs (CYSHCN).
In addition to Title V, MCHB manages programs and budgets drawn from several different federal grants, including
the Women’s and Infants Program (WIC); Title X Family Planning; Maternal, Infant and Early Childhood Home
Visiting Program (MIECHV); Abstinence Education / Title V Sexual Risk Avoidance Education (Section 510);
Maryland Optimal Adolescent Health Program; and the Personal Responsibility Education Program (PREP).
MCHB’s staff is multidisciplinary and includes physicians, nurses, social workers,epidemiologists, educators,
community health outreach specialists, public health administrators, and administrative support staff. At any given
time, there are also as many as four public health interns and two preventive medicine residents contributing to the
work of MCHB.
Maternal and Child Health Needs
Perinatal Health:
In 2020, the Maryland infant mortality rate was 5.7 deaths per 1,000 live births, a decrease of three percent from the
2019 rate of 5.9 deaths per 1,000 live births. Although infant mortality has declined over the last few years, significant
racial disparities still exist. Between 2019 and 2020, the non-Hispanic (NH) White infant mortality rate decreased by
20 percent from 4.1 to 3.3 deaths per 1,000 live births and the Hispanic infant mortality rate decreased by 10
percent, from 5.1 to 4.6 deaths per 1,000 live births. The NH Black rate increased by six percent from 9.3 to 9.9
deaths per 1,000 live births. Additionally, Maryland jurisdictions continue to experience regional disparities in infant
mortality rates, including Dorchester County (13.3 per 1,000), Wicomico County (11.2 per 1,000) Baltimore City
(10.3 per 1,000), and Allegany County (9.5 per 1,000).
Created on 8/11/2022 at 8:37 PM
Page 14 of 296 pages

Infant mortality reduction remains a State priority. While Maryland has made tremendous progress in reducing
overall rates of infant deaths, racial/ethnic disparities continue and will thus remain a focus of Title V activities
throughout the next budget year. Title V supported Fetal and Infant Mortality Review (FIMR) activities in all 24
jurisdictions from 1998-2020, and currently supports 8 regional FIMR teams as of FY 2021. FIMR not only provides
important insight into opportunities for systems improvement, it also serves as a mechanism for local and regional
communication, coordination, and collaboration on broader maternal and child health issues.
Babies Born Healthy, funded with Title V state match funds, was established in 2007 to reduce infant mortality,
improve birth outcomes, and reduce racial disparities. Babies Born Healthy provides funds to eight sites located in
the seven jurisdictions in Maryland with the highest infant mortality rates and highest racial disparities in infant
mortality. Jurisdictions focus their resources on care coordination for tobacco cessation, substance use prevention
and treatment, prenatal care, long acting reversible contraception, and other strategies driven by site-specific data to
promote healthy maternal and infant outcomes.
Preventing child and adolescent deaths through Child Fatality Review (CFR) is another Title V priority. CFR was
established in Maryland statute in 1999. Title V supports a 24 member State CFR Team whose purpose is to
prevent child deaths by: (1) understanding the causes and incidence of child deaths; (2) implementing changes
within the agencies represented on the State CFR Team to prevent child deaths; and (3) advising the State
leadership on child death prevention. The State CFR Team also sponsors an all-day training for local CFR team
members on select topics related to child fatality issues.
The State CFR Team oversees the efforts of local CFR teams operating in each jurisdiction. Each month the local
CFR teams receive notice from the Office of the Chief Medical Examiner (OCME) of unexpected resident child
(under age 18) deaths, and are required to review each of these deaths. Local teams meet at least quarterly to
review cases and make recommendations for local level systems changes in statute, policy, or practice to prevent
future child deaths, and work to implement these recommendations.
The OCME referred 157 child deaths to local CFR teams during CY2020, of which 156 were reviewed by local CFR
teams. The leading manner of child fatalities in 2020 was undetermined, accounting for 30% of child deaths
reviewed, followed by accidents at 25% of child deaths reviewed. Approximately 50 cases reviewed were Sudden
Unexpected Infant Deaths (SUID). Infant safe sleep promotion continues to be a Title V priority.
Child and Adolescent Health:
OFCHS partners with Medicaid to monitor the percentage of children and adolescents who follow through with well
visits. With lead support from OGPSHCN and in collaboration with MDH-PHPA, youth transition to adult health care
remains an MCHB priority focus area. Strengthening systems of care for children and youth with special health care
needs through the Medical Home model is another priority for OGPSHCN. The Medical Home and Health
Care Transition efforts have expanded throughout the State of Maryland to include promotion, implementation, and
evaluation of care within most statewide health systems. Developing “Best Practice Models'' to improve and build
strong infrastructures to support providers who serve CYSHCN while focusing on direct access, effective care
coordination, and family involvement are all targeted efforts. Continued collaboration with existing programs and
community-based organizations will remain a priority as well as developing new collaborations, both internally and
externally.
Created on 8/11/2022 at 8:37 PM
Page 15 of 296 pages

Children and Youth with Special Health Care Needs:
In previous years, OGPSHCN has focused efforts around the “six core outcomes” for CYSHCN: Family-Professional
Partnership; Medical Home; Adequate Insurance; Early and Continuous Screening; Easy-to-Use Services and
Supports; and Youth Transition to Adult Health Care. These ‘core outcomes’ have been assessed and updated, with
the most recent “Version 2.0 of the National Standards for CYSHCN” released in 2017 as a result of a partnership
between The Association of Maternal & Child Health Programs (AMCHP) and the National Academy for State
Health Policy (NASHP). Version 2.0 organizes the standards into eight core domains and introduces four
Foundational Standards for Systems of Care for CYSHCN.
[1]
Foundational Standards for Systems of Care for CYSHCN:
Children and families of CYSHCN are active, core partners in decision making in all levels of care
All services and supports for CYSHCN are implemented and delivered in a culturally competent, linguistically
appropriate, and accessible manner
Insurance coverage for CYSHCN is accessible, affordable, comprehensive, and continuous
All care provided to CYSHCN and their families is evidence-based where possible
Core Domains for System Standards
Identification, Screening, Assessment, and Referral
Eligibility and Enrollment in Health Coverage
Access to Care
Medical Home
Pediatric Preventive and Primary Care
Medical Home Management
Care Coordination
Pediatric Specialty Care
Community-Based Services and Supports
Respite Care
Palliative and Hospice Care
Home-Based Services
Transition to Adulthood
Health Information Technology
Quality Assurance and Improvement
OGPSHCN reaches every child born in Maryland with the dual initial birth screenings for hearing and congenital
metabolic disorders, as well as critical congenital heart disease and birth defects surveillance. Outreach and
intervention continue for some children across the life course, with follow up for any out of range screening results,
referral to early intervention services where warranted, continued information dissemination and education for certain
diagnosed conditions, and ongoing efforts to effect transition to adult systems of care.
Through the varied programs housed under the office umbrella and through grant funding to LHDs, community-based
organizations, and academic and clinical institutions, OGPSHCN endeavors to impact each of the Core Domains for
System Standards, with a focus on the national performance measures of medical home and health care transition.
Family-Professional Partnership (FPP) was previously categorized as an individual outcome, though OGPSHCN
strived to incorporate FPP into all programs as an integral component of the workflow. With Version 2.0, FPP is no
longer an individual outcome, but is a Foundational Standards for Systems of Care for CYSHCN. OGPSHCN will
explore opportunities to impact each of the core domains while maintaining focus on the foundational standards.
Created on 8/11/2022 at 8:37 PM
Page 16 of 296 pages

COVID -19 Impact:
The COVID-19 pandemic continued to impact the State significantly in 2021. The State continued to focus on
providing vaccinations, and on January 26, 2021, Governor Hogan announced the opening of mass vaccination sites
in the state of Maryland. In addition, Maryland’s COVID-19 Vaccination Support Center, a call-line, was set up to
provide support to individuals needing additional assistance. By May 21, 2021, about 70 percent of adults in
Maryland had received their COVID-19 vaccines. In addition to expanding vaccinations, the Maryland Department of
Health with local health departments and partners continued to provide contact tracing operations, testing, and
information about COVID-19 and vaccinations.
Activities that Maryland Department of Health have taken in response to the pandemic include:
Developing COVID-19 data dashboards that present case rates by county, testing by county and zip code,
Intensive Care Units (ICUs) and acute hospital beds, testing volume, testing per day, and percent positive rate
over 7 days, school outbreak data, nursing home outbreak data, and COVIDLink Contact tracing data
Updating public health partners including local health departments, schools, healthcare facilities, college and
universities, and health emergency preparedness teams with the most up to date guidelines
Established and leads Maryland’s COVID-19 Vaccination Support Center, a call-line,
Launched COVIDConnect, a free platform for individuals who have been affected by COVID to connect with
other individuals who are recovering
Developed public and private partnerships with pharmacies, health care facilities, community based
organizations to launch mass testing and vaccination sites throughout Maryland
Developed frequently asked questions for COVID-19
Launched the GoVax Campaign, a communication campaign on the importance of COVID vaccinations
Implemented MD Covid Alert that uses exposure notification technology to notify users who may have been
exposed to an infected person
During 2021, many staff, including Title V staff at both the state and local level, were deployed to provide assistance
related to the COVID-19 pandemic through providing testing, serving on outbreak and contact tracing teams,
developing guidance for partners, or providing vaccinations. Title V staff developed COVID-19 Vaccine Facts for
Pregnant and Breastfeeding Individuals in 2021.
[1]
National Standards for Systems of Care for Children and Youth with Special Health Care Needs, Version 2.0 Informational website
Created on 8/11/2022 at 8:37 PM
Page 17 of 296 pages

III.C. Needs Assessment
FY 2023 Application/FY 2021 Annual Report Update
During Fiscal Year 2021, the Maternal and Child Health Bureau welcomed a new Director. Dr. Shelly Choo began
with MCHB on July 15, 2020. Ms. Alena Troxel continued in her role as Deputy Director which she began in
December 2019. Melissa Beasley served as the Director of the Office of Family and Community Health Services
until the end of July 2020. Maisha Douyoncover served as the Director of the Office of Quality Initiatives until the end
of May 2021. Dr. Jed Miller served as the Director for Children and People with Special HealthCare Needs, and
Jennifer Wilson served as Director of the Maryland WIC program. Teresa Pfaff started as the Director of the Office
of Quality Initiatives in September 2021. In addition, Paula Reynolds started as the Chief Operating Officer in
September 2021.
During State Fiscal Year 2022 and 23, the Bureau aligned positions within Title V domains. A maternal health
coordinator position was developed to focus on the maternal health workstreams. In addition, an infant and child
health coordinator position was developed to focus on infant health workstreams. A child and adolescent health
program manager position was developed to focus on child and adolescent health workstreams.
Data Updates
The following section provides an overview of population level data updates available during the reporting period.
Women’s/Maternal Health:
Substance Use/Misuse/Disorder: Due to Maryland Department of Health’s network security event, additional data
are not available. However, in Maryland from January to September 2021, preliminary data show that there were
2,129 unintentional intoxication events compared to 2,076 from January to September 2020.
The Maryland Vital Statistics Administration (VSA) reported that in 2020, there were 2,773 unintentional intoxication
deaths involving drugs and alcohol, a 16.6% increase from 2019. Ninety percent of these deaths were categorized
as opioid-related, higher than at any other point during the opioid crisis. The number of opioid-related unintentional
intoxication fatalities increased 18.7%, from 2,106 in 2019, to 2,499 in 2020. This is substantially less than the 70%
increase between 2015 and 2016, which was the largest single year increase that has been recorded. Fentanyl-
related deaths continue to rise, increasing 20.7% from 1,927 in 2019 to 2,326 in 2020. Maryland Vital Statistics data
indicates that drug and alcohol intoxication deaths among women increased from 640 deaths in 2018 to 654 deaths
in 2019, a two percent increase.
Mental Health: According to 2020 Pregnancy Risk Assessment Monitoring System (PRAMS) data, 18.1% of women
reported depression three months before pregnancy and 14.3% of mothers reported symptoms of postpartum
depression. During the three months before pregnancy, 25.2% of women reported they had anxiety.
Maternal Mortality and Morbidity: While the report for cases reviewed in FY2021 are still being finalized due to delays
related to COVID-19 and the Department’s network security incident, preliminary data demonstrate that there were
31 pregnancy-associated deaths in 2019, resulting in a pregnancy-associated mortality rate of 44.2 deaths per
100,000 live births in Maryland. The 2015-2019 maternal mortality rate (MMR) in Maryland is 17.2 maternal deaths
per 100,000 live births, which is a 33 percent decrease from the 2010-2014 rate. The 2015-2019 MMR among
Black women is 27.8 maternal deaths per 100,00 live births, which is 58 percent higher than the MMR of White
women. The leading cause of pregnancy-related deaths were hemorrhage (29 percent of these deaths) and non-
Created on 8/11/2022 at 8:37 PM
Page 18 of 296 pages

cardiovascular medical conditions (24 percent of these deaths). The leading cause of pregnancy-associated deaths
in 2019 was substance use with unintentional overdose, accounting for 50 percent of non-pregnancy-associated
deaths.
Preventive Dental Visits in Pregnancy: According to preliminary 2020 PRAMS data, 47.0% of women reported
having their teeth cleaned during pregnancy, a decrease from 54.1% in 2019. This number was most likely impacted
by COVID.
Smoking in Pregnancy: According to preliminary 2020 PRAMS data, 10.6% of women reported that they smoked
during the three months before pregnancy (down from 16.1% in 2013), 4.0% of women reported that they smoked
during the last three months of pregnancy (down from 7.8% in 2013), and 5.4% reported that they smoked
postpartum. Non-Hispanic White women reported the highest rates of smoking during the three months before
pregnancy (14.0%), Black Non-Hispanic women reported the highest rates postpartum (8.4%), and non-Hispanic
White women reported the highest rates of smoking during the last three months of pregnancy (5.7%). All smoking
rates were highest among women under the age of 25. Prenatal smoking rates in Maryland are slightly higher than
the Healthy People 2030 objective for smoking during pregnancy (4.3%).
Perinatal Health of Maryland Women and Infants:
Prenatal Care: The annual percentage of Maryland women who initiated prenatal care during the first trimester has
risen to 86.0% in 2020, a 1.9% increase from 84.8% in 2019, according to preliminary PRAMS data. Among non-
Hispanic White women, 94.4% initiated prenatal care during the first trimester, compared to 85.4% among non-
Hispanic Black women, and 68.3% among Hispanic women.
Infant Mortality: Maryland VSA reported the infant mortality rate in Maryland in 2020 was 5.7 per 1,000 live births, a
3.0% decrease from 5.9 per 1,000 live births in 2019, and down from 8.5 per 1,000 live births in 2004. The leading
causes of death were disorders related to short gestation and low birth weight, congenital abnormalities, maternal
complications of pregnancy, SIDS, circulatory system disorders, infectious diseases, and complications of the
placenta, cord, and membranes. Maternal complications of pregnancy include conditions such as premature rupture
of membranes and cervical incompetence.
Low Birth Weight: Maryland VSA reported in 2020, 8.5% of live births in Maryland were low birth weight (LBW),
weighing less than 2,500 grams at birth. Non-Hispanic Black mothers were nearly twice as likely to have a LBW
infant (12.1%) than Non-Hispanic White mothers (6.4%).
Very Low Birth Weight: Maryland VSA reported in 2020, 1.6% of all live births in Maryland were very low birth weight
(VLBW), weighing less than 1,500 grams at birth. Non-Hispanic Black mothers were over twice as likely as other
races to have VLBW infants (2.7% Non-Hispanic Blacks, 1.0% Non-Hispanic Whites, and 1.3% for Hispanics).
Preterm Birth: Maryland VSA reported in 2020, 10.1% of live births occurred before 37 weeks of gestation in
Maryland, a 2.0% decrease from 10.3% in 2019. Non-Hispanic Black mothers were more likely to have a preterm
birth than other races at 12.6%, compared to 8.6% and 9.9% for Non-Hispanic White and Hispanic births,
respectively.
Breastfeeding: In 2020, according to preliminary PRAMS data, 89.9% of Maryland mothers reported having ever
breastfed their babies, a slight decrease from 91.4% in 2019. Rates of breastfeeding in Maryland were high across
all races and ethnicities ranging from 84.8% for Non-Hispanic Black mothers to 93.9% among Hispanic mothers.
Infant Safe Sleep: In 2020, according to preliminary PRAMS data, 16.3% of mothers in Maryland reported not
Created on 8/11/2022 at 8:37 PM
Page 19 of 296 pages
placing their infants on their back to sleep and 37.8% of mothers reported that their baby slept with a blanket, 7.6%
slept with toys, cushions or pillows, and 13.7% slept with bumper pads. Over 83 percent of mothers reported that
their baby slept in the same room as the mother.
Child Health:
Mortality: According to Maryland VSA data, in 2020, there were 669 infants and child deaths ages 0 to 18 years old
in Maryland. Most of these deaths occurred in infancy - 58 percent were under the age of one year. The 2019 child
death rate decreased by 1.3% compared to 2019. Accidents were the leading cause of death for the 60 children
ages 1 to 4 years. Neoplasms were the leading cause of death for the 82 children ages 5 to 14, followed by
intentional self-harm.
Preventive Health Care: According to 2021 Medicaid data, 71.7% of Medicaid enrolled patients who turned 15
months old during 2021 had five or more well-child visits during their first 15 months of life.
Child Development Screenings: Data from the National Survey of Children’s Health (NSCH), 2019-2020, showed
that 40.3% of children ages 9 through 35 months received a developmental screening using a parent-completed
screening tool in the past year, unchanged from 40.9% during the 2018-2019 survey period.
Asthma: Data from the Health Services Cost Review Commission (HSCRC) showed that emergency department
visits for asthma among children ages 2 to 17 was 3.5 per 1,000 population in 2020.
Adolescent Health:
Mental Health and Suicide: According to Maryland VSA data, the rate of suicide deaths among youth ages 15-19
years was 7.4 per 100,000 population in 2020. This represented a 15% decrease from the 2019 rate of 8.7 per
100,000 population. The actual numbers of suicides in this age range decreased from 33 cases in 2019 to 28 cases
in 2020. The suicide rate remained highest for non-Hispanic White male teens in 2020 at 10 cases, or 36 percent of
suicide deaths.
Teen Pregnancy and Reproductive/Sexual Health: Maryland VSA data showed that the adolescent birth rate
decreased 52.2% from 27.2 births per 1,000 adolescent females ages 15-19 years in 2010 to 13.0 births per 1,000
adolescent females in 2020. Hispanic females had the highest adolescent birth rate with 35.0 births per 1,000
adolescent females, which was more than double the adolescent birth rate for Black, non-Hispanic females (16.7 per
1,000 adolescent females) and more than five times the adolescent birth rate for White, non-Hispanic females (6.0
per 1,000 adolescent females).
Children and Youth with Special Health Care Needs:
Medical Home: According to the 2019-2020 National Survey of Children’s Health, there are an estimated 273,531
children and youth ages 0 to 17 with special health care needs in the state. The survey estimated that 44.9% of these
children have a medical home.
Transition to Adult Care: The 2019-2020 National Survey of Children’s Health estimated that 23.8% of adolescents
ages 12-17 with special health care needs received services necessary to make transitions to adult health care.
Program Capacity:
The Title V program is managed by the Maternal and Child Health Bureau (MCHB) in the Prevention and Health
Promotion Administration (PHPA) at the Maryland Department of Health (MDH).
Created on 8/11/2022 at 8:37 PM
Page 20 of 296 pages

Maryland Department of Health’s Prevention and Health Promotion Administration leadership includes:
Donna Gugel, MHS, serves as the Director of PHPA. Ms. Gugel has been the Director since 2016 and
previously served as Deputy Director.
Courtney McFadden, MPH, serves as Deputy Director of PHPA. Ms. McFadden has been the Deputy
Director since 2018 and previously served as the Director of the Maternal and Child Health Bureau.
Maryland Department of Health’s Maternal and Child Health Bureau leadership includes:
Shelly Choo, MD, MPH serves as the Director of the Maternal and Child Health Bureau.
Alena Troxel, MPH serves as the Deputy Director of the Maternal and Child Health Bureau.
Jed Miller, MD, MPH served as the Director of the Office of Genetics and People with Special Health Care
Needs and as the State Title V CSHCN Director until February 2022.
Stacy Taylor, JD serves as the Deputy Director of the Office of Genetics and People with Special Health Care
Needs and as Acting Director since Dr. Miller’s departure.
Jennifer Wilson, MEd, RD, LDN, serves as the Director of the Maryland WIC Program.
Samantha Ritter, MPH serves as the Director of the Office of Family and Community Health Services.
Teresa Pfaff, MPH, MSN, RN, PHNA-BC, CPH serves as the Director of the Office of Quality Initiatives.
Kristin Silcox, MS served as the Epidemiology Program Manager within the Office of Quality Initiatives. Ms.
Silcox departed July 2022.
Colleen S. Wilburn, MPA, served as the Title V Manager since 2019. Ms. Wilburn departed June 2022.
Created on 8/11/2022 at 8:37 PM
Page 21 of 296 pages

$11,673,326 $11,673,326 $11,673,326 $11,850,506
$8,754,995 $8,754,995 $8,754,995 $8,887,880
$0 $0 $0 $0
$0 $0 $0 $0
$0 $0 $0 $0
$20,428,321 $20,428,321 $20,428,321 $20,738,386
$128,630,107 $128,949,674 $117,178,515 $87,533,536
$149,058,428 $149,377,995 $137,606,836 $108,271,922
$11,673,326 $11,872,645 $11,850,506
$8,754,995 $10,999,716 $8,887,880
$0 $0 $0
$0 $0 $0
$0 $0 $0
$20,428,321 $22,872,361 $20,738,386
$118,199,750 $88,972,950 $111,489,625
$138,628,071 $111,845,311 $132,228,011
III.D. Financial Narrative
2019 2020
Budgeted Expended Budgeted Expended
Federal Allocation
State Funds
Local Funds
Other Funds
Program Funds
SubTotal
Other Federal Funds
Total
2021 2022
Budgeted Expended Budgeted Expended
Federal Allocation
State Funds
Local Funds
Other Funds
Program Funds
SubTotal
Other Federal Funds
Total
Created on 8/11/2022 at 8:37 PM
Page 23 of 296 pages
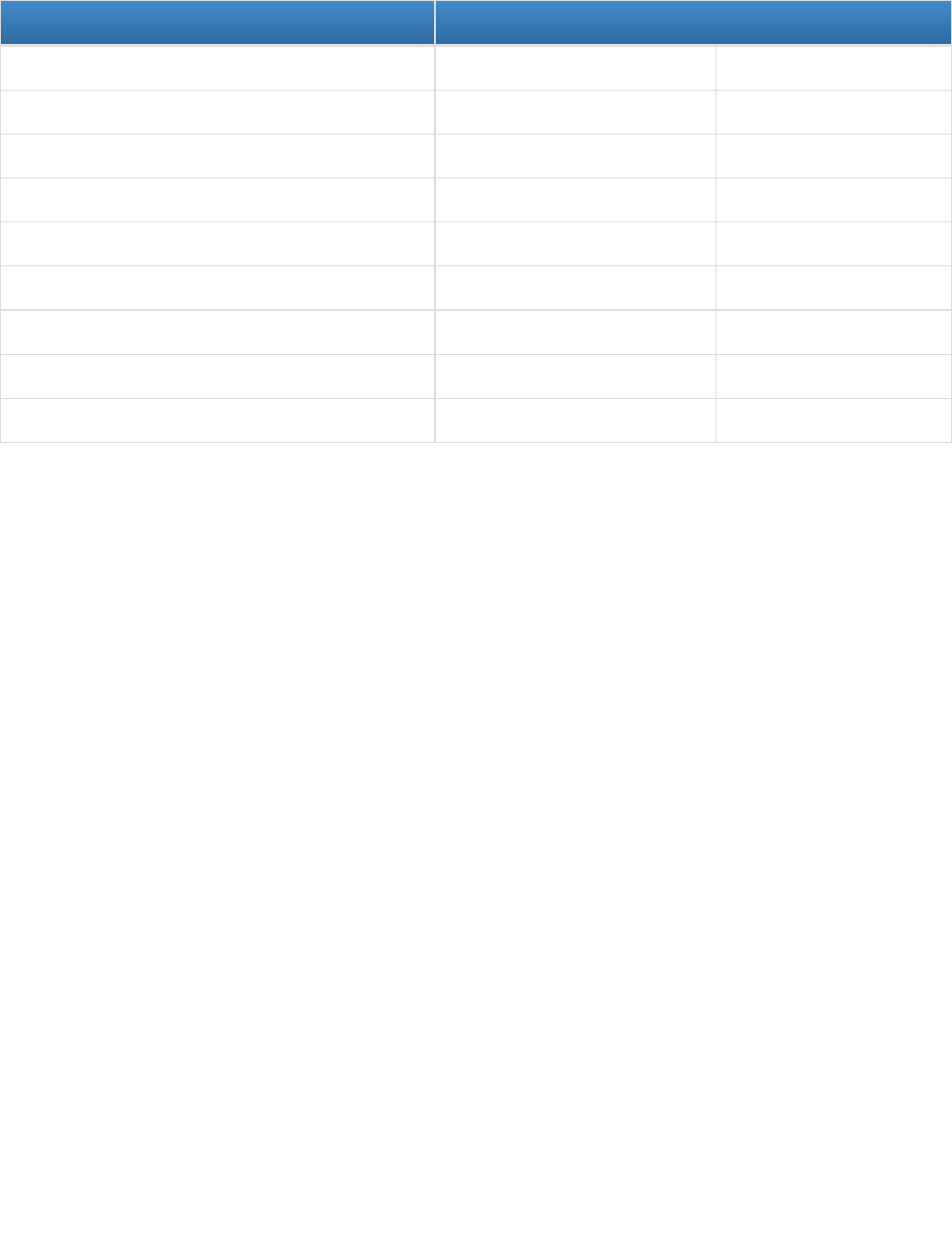
$11,981,449
$9,023,964
$0
$0
$0
$21,005,413
$123,038,688
$144,044,101
2023
Budgeted Expended
Federal Allocation
State Funds
Local Funds
Other Funds
Program Funds
SubTotal
Other Federal Funds
Total
Created on 8/11/2022 at 8:37 PM
Page 24 of 296 pages

III.D.1. Expenditures
In FY 2021, the Maryland joint federal-state Title V program expended $22,872,361 for services and activities to
promote the health of women, infants, and children including those with special health care needs. Federal
expenditures amounted to $11,872,645 and included the required 30-30-10 funding obligation to primary and
preventive services for children, children with special health care needs, and Title V administrative costs. The 30-30-
10 requirement in FY 2021 was met with 33.3% of federal funds expended for preventive and primary care services
for children, 44.5% expended for children with special health care needs. Less than ten percent of federal funds were
used for Title V administrative costs.
With regards to the MCH pyramid, federal FY 2021 funds supported direct services ($4,607,864), enabling services
($4,517,481), and public health services and systems ($2,747,300).
The $4,607,864 in direct services represents direct medical care for CYSHCN including medical day care,
Children’s Medical Services, and genetic services. Additionally, direct services were provided to pregnant people,
and people with infants up to one year through local health department reproductive health clinics.
Total Children's Medical Services expenditures for FY 2021 were greater than projected total expenditures for FY21
due to the extended eligibility secondary to the COVID-19 Pandemic State of Emergency. This resulted in the
highest number of children enrolled in CMS since its inception. The range of diagnoses enrolled children have results
in variable treatment plans and medication costs, making it challenging to predict annual allocation amounts even
when not in a state of emergency. Nevertheless, strategies to contain CMS expenditures, all of which are for direct
services, received a considerable level of internal discussion during FY 2021 and will continue in FY 2023.
Enabling service expenditures during FY 2021 included services for families, children, and pregnant people such as:
Case management and care coordination services to pregnant people, high risk infants, children with
elevated blood lead levels, children in the Infants and Toddlers Program, and children and youth with
special health care needs
Reproductive Health services
Home Visiting services
Referrals of adolescents and women of childbearing age to dental care, tobacco cessation, substance
use treatment, and/or mental health care; and,
Health education to parents and families around infant/child health topics including safe sleep,
breastfeeding, primary care, developmental screening, oral health, tobacco and substance use, and
exposure to secondhand smoke.
Enabling service expenditures also included services for CYSHCN, comprising the aforementioned case
management services, linking families with state and local resources for their children, family support and education
on navigating health systems, funding to health care institutions to enhance medical home services, and care
coordination related to newborn screening results.
Public health services and systems expenditures primarily targeted supporting perinatal infrastructure projects such
as the Perinatal Support Program, Perinatal Quality Collaborative, Perinatal Transport Services, and public health
infrastructure activities such as Child Fatality Review and Maternal Mortality Review. In addition, expenditures were
used for staff for epidemiology, program planning, policy analysis and planning.
Maryland expended $10,999,716 in matching funds in FY 2021 exceeding its required 1989 Maintenance of Effort
Created on 8/11/2022 at 8:37 PM
Page 25 of 296 pages

match of $8,262,484. Direct services ($5,826,159), enabling services ($3,452,784) and public health services and
systems ($1,720,773) comprised the totality of matching fund expenditures. For the direct services it includes the
$3,132,160 within preventive and primary care services for pregnant individuals, mothers, and infants as well
services for CSHCN as well as the direct services through the family planning clinics that provides essential care for
Maryland residents.
Direct service expenditures supported gap filling reproductive health services through state funded family planning
clinics across the state.
Enabling expenditures included grants to local jurisdictions to provide home visiting for high-risk pregnant women
and infants as well as asthma and immunization care coordination, state health department staff who provided care
coordination for CYSHCN, and reproductive health services to women, adolescents and others.
Public health services and systems included local oversight of Fetal and Infant Mortality Review and Child Fatality
Review activities in each jurisdiction, awards to organizations to implement policy changes to enhance systems of
care for pregnant individuals and infants and state health department staff who provide epidemiology and data
support, surveillance through the Pregnancy Risk Assessment Monitoring System (PRAMS), provide oversight to
women’s and infant health initiatives (Babies Born Healthy), coordinate specific adolescent health activities, and
coordinate CYSHCN activities related to systems development.
Created on 8/11/2022 at 8:37 PM
Page 26 of 296 pages

III.D.2. Budget
Maryland's Maternal and Child Health Block Grant supports vital programs and services for women, children,
including those with special health care needs, and adolescents throughout Maryland. The Title V Program is jointly
administered by the Maternal and Child Health Bureau and the Office of Genetics and People with Special Health
Care Needs. Funding is also provided to all 24 local health department programs to support MCH populations.
Maryland's projected Title V budget for FY 2023 is $21,005,413, including $11,981,449 in federal funds and
$9,023,964 in state funds. This match amount exceeds the FY 1989 maintenance of effort requirement of Sec. 505
(a) (4) and represents the required match of $3 of state funds for every $4 of federal funds.
Throughout the funding period (state fiscal year), Title V funds are monitored to ensure that the funding levels adhere
to the “30-30-10” Title V requirement. For FY 2023, it is proposed that federal funding will be distributed
accordingly: 31.4% for preventive and primary care for children, 39.6% for CYSHCN, and 4% for administration.
Remaining funds will support services for pregnant women and mothers with infants up to one year. By level of the
MCH pyramid, it is proposed that the projected federal funding level of $11,981,449 will be distributed as follows:
approximately $1,800,000 for direct services; approximately $6,300,000 for enabling services; and approximately
$3,900,000 for public health services and systems.
For FY 2023, nearly $4.5 million in federal funding is budgeted for the 24 local health departments throughout the
state to provide services in one of three domains: 1) pregnant women and mothers with infants up to one year; 2)
child health services; and 3) children and youth with special health care needs. In addition, another $1.3 million in
federal funding is budgeted to the local health department for primary and preventive child health services, and
$85,000 specifically for asthma related activities. Allowable services under each domain include:
Title V Health Domains Allowable Services
Primary and Preventive
Child Health Services
Hearing and Vision Screening
School Based Health Services including
screening and referral for mental health
and/or substance use
Immunizations
Childhood Asthma Related
Programming/Services
Primary and Preventive
Health Services for
Pregnant Women,
Mothers, and Infants up
to one year
Home Birth Certification
Home Visiting
Care Coordination for Pregnant or Recently
Postpartum Individuals
Children and Youth with
Special Health Care
Needs
Care Coordination for CYSHN
Infants and Toddlers
Lead Case Management
Created on 8/11/2022 at 8:37 PM
Page 27 of 296 pages

Funded services represent primarily enabling and public health systems services. During FY2022, family
planning/reproductive health services were removed as there was funding available through Title X and state general
funds. Shifting from direct services to care coordination has allowed funds to be shifted to enabling services.
In FY 2023, a total of $3,770,104 in federal funds is budgeted to support preventive and primary care programs and
services for children and adolescents. These funds will support activities that promote and protect the health of
Maryland's children and adolescents by assuring that comprehensive, quality preventive and primary services are
accessible, and will include: hearing and vision screening, immunizations, promotion of child development
screenings, asthma programming/services, and promotion of access to a medical home.
In FY 2023, a total of $4,747,066 in federal funds is budgeted for programs and services to address the needs of
CYSHCN. Activities and strategies will include:
● Children's Medical Services Program which provides specialty care and related services for uninsured and
underinsured children who meet the medical and financial eligibility criteria;
● Genetic Services which provides funds for a statewide system of clinical genetic services, including
infrastructure support for genetics centers, Sickle Cell Disease clinics, and specialized biochemical genetics
laboratory services;
● Birth Defects Reporting and Information System (BDRIS) which collects data on birth defects to conduct
surveillance for changes in trends that could be related to environmental hazards, and provides families with
information and referrals;
● Medical Day Care for CYSHCN which provides Medical day care programs for medically fragile infants and
young children;
● Local Health Department Grants that support services for CYSHCN such as gap-filling care coordination,
outreach, information/referral, dissemination of resource information, and needs assessment activities;
● Parent Involvement Activities; and,
● CYSHCN Systems-Building Activities including grants to specialty health care systems to support resource
liaisons and policy/systems changes.
During FY 2023, the $9,023,964 proposed state match will be used to support direct services, enabling services,
and public health services and systems across all three population domains. Matching funds will support the following
activities and strategies:
● Surveillance and quality initiative grants in every jurisdiction to support local Child Fatality Review and Fetal
and Infant Mortality Review teams working to review and prevent infant and child deaths;
● Babies Born Healthy grants to jurisdictions to reduce infant mortality and eliminate racial disparities in birth
outcomes;
● Perinatal Care Coordination;
● Prenatal support groups through Babies Born Healthy grants;
● Child abuse and neglect education and support for health care providers;
● Medical Day Care for CYSHCN which provides funding for medical day care programs for medically fragile
infants and young children;
Family Planning grants to the Family Planning clinics across the state
Additional maternal and child health initiatives through the Statewide Integrated Health Improvement Strategy.
Created on 8/11/2022 at 8:37 PM
Page 28 of 296 pages

III.E. Five-Year State Action Plan
III.E.1. Five-Year State Action Plan Table
State: Maryland
Please click the links below to download a PDF of the Entry View or Legal Size Paper View of the State Action Plan Table.
State Action Plan Table - Entry View
State Action Plan Table - Legal Size Paper View
Created on 8/11/2022 at 8:37 PM
Page 29 of 296 pages

III.E.2. State Action Plan Narrative Overview
III.E.2.a. State Title V Program Purpose and Design
The Title V program is administered by the Maternal and Child Health Bureau (MCHB), Prevention and Health
Promotion Administration (PHPA), Public Health Services at the Maryland Department of Health (MDH).
Current leadership includes:
Maternal and Child Health Bureau:
Shelly Choo, MD, MPH, Director and Title V State Director
Alena Troxel, MPH, Deputy Director
Prevention and Health Promotion Administration:
Donna Gugel, MHS, Director
Courtney McFadden, MPH, Deputy Director
Public Health Services:
Jinlene Chan, MD, MPH, FAAP, Deputy Secretary
Maryland Department of Health:
Dennis Schrader, Secretary
Title V which is located within the Maternal and Child Health Bureau is managed by Colleen S. Wilburn, MPA. The
Title V Manager left June 2021.
Within the Maternal and Child Health Bureau, there are four offices:
The Office for Genetics and People with Special Health Care Needs (OGPSHCN) was directed by Jed Miller,
MD, MPH, who also served as the State Title V Children with Special Health Care Needs Director until January
2022. The OGPSHCN manages the Children’s Medical Services Program, the Early Hearing Detection Program,
the Newborn Screening Follow-up Program, the Genetics Services Program and the Systems Development branch.
These programs provide comprehensive support to individuals with special health care needs throughout the life
course. Stacy Taylor serves as the Deputy Director and in FY22 served as the Acting Director and the State Title V
Children with Special Health Care Needs Director.
The Office of the Maryland WIC Program (OMWIC) is directed by Jennifer Wilson, M.Ed. The OMWIC is the
State’s supplemental nutrition program for women, infants and children ages 0-5. This federally-funded program
provides healthy supplemental foods and nutrition counseling and has served the State of Maryland for more than 40
years. Strong collaboration between WIC and Title V helps to ensure that comprehensive nutrition counseling and
services are provided to eligible participants.
The Office of Quality Initiatives (OQI) was directed by Maisha DouyonCover, MPH until May of 2021. Teresa Pfaff
started as the OQI Director September 2021. This office oversees Title V efforts regarding infant mortality, maternal
mortality and morbidity, the Maryland Child Abuse Medical Provider Network, Fetal Infant Mortality Review, Child
Fatality Review, PRAMS, and other special projects of statewide maternal and child health importance. Additionally,
this office contains MCHB Epidemiologists and oversees the SSDI initiative. Such special projects provide support
to ensure infrastructure and population based initiatives are targeted to Title V populations throughout the State.
Created on 8/11/2022 at 8:37 PM
Page 30 of 296 pages

The Office of Family and Community Health Services (OFCHS) was directed by Melissa Beasley until July
2021. Samantha Ritter started December 2021. This office is charged with the management and oversight of the
State’s Title X Family Planning program as well as the Maternal, Infant and Early Childhood Home Visiting (MIECHV)
program, PREP, and SRAE, along with various other child and adolescent health initiatives. These programs
provide both direct, enabling, and population-based services across the state to Title V eligible individuals with
access to quality services aimed at improving health outcomes.
The Operations Unit is directed by a Chief Operating Officer, which is Paula Reynolds. She started September
2021. This office administers grants to the local health departments, federal grants to OFCHS, OQI, and OGPSHCN,
and administers contracts and Memorandum of Understandings. The Office of Operations coordinates with the four
other offices on Procurements and Inventories.
The Maternal and Child Health Bureau Medical Director is Dr. Benjamin Wormser. He is a board-certified
Pediatrician and oversees the healthcare systems coordination work including the Perinatal Support Program,
Morbidity, Mortality, and Quality Review Committee, the Perinatal Quality Collaborative as well as the Maryland
School-Based Health Centers. He also has been overseeing the Maternal Mortality Review Committee.
The offices and units work in collaboration to improve the health and well-being of all Marylanders, including those
eligible for Title V services through the life course. Using data from the most recent Title V Needs Assessment along
with frequent data analysis, program evaluation and feedback from consumers as well as providers across the state,
these offices work diligently to improve the health outcomes of women, infants, children, adolescents and
children/youth with special health care needs.
In addition to the MCHB, Title V provides support, outreach and subject matter expertise on MCH populations and
needs across all of PHPA’s administrative bureaus: the Environmental Health Bureau, the Cancer and Chronic
Disease Bureau, Infectious Disease Epidemiology and Outbreak Response Bureau and the Infectious Disease
Prevention and Health Services Bureau. While these respective bureaus have a variety of programs and
populations, ongoing collaborations with Title V ensure that their evidence-based and/or evidence-informed
programs are well-versed in current maternal and child health care needs and are inclusive in their design and
implementation in order to provide strong supports to Title V eligible populations. Examples of programs overseen
by these bureaus include, but are not limited to: injury prevention, oral health, cancer screening and prevention,
tobacco prevention and control, chronic disease prevention, immunizations, human immunodeficiency virus
prevention and health services and sexually transmitted infection and prevention.
Title V has a strong presence in all 24 independent jurisdictions across the state. Funding from the Title V Block
Grant, either with federal or state funds, are used by local health departments to develop and implement
programming that not only meets the needs of the maternal and child health community, but also aligns with the
priorities identified by MDH as part of the 2020 Needs Assessment. All of the maternal and child health efforts
implemented at the local level are direct service, enabling services or public health system building initiatives.
Regular, ongoing communication and technical assistance is available and provided to local health departments and
funded entities by the Title V Program Manager.
Title V is well positioned within the state health department to ensure that the funding and the programs are
strategically designed and implemented, as well as aligned with other state health initiatives, in order to have the
broadest reach and maximum benefit to Title V eligible populations.
Created on 8/11/2022 at 8:37 PM
Page 31 of 296 pages

III.E.2.b. State MCH Capacity to Advance Effective Public Health Systems
III.E.2.b.i. MCH Workforce Development
In consideration of the number of existing and emerging health care and public health challenges, the MCH field calls
for a workforce able to adapt and rise to many transformations in the public health, health care and health financing
sectors. An adequately prepared public health workforce is essential to address MCH needs and to provide
essential services to improve public health systems, community health care delivery, and ultimately the health of MCH
populations.
At the state level, federal Title V funds supported approximately 23 FTE positions in the Maternal and Child Health
Bureau during FY 2021. Supported staff include medical doctors, nurses, epidemiologists, public health
professionals, public health administrators, business administrators, and health educators. At the local health
department level, federal Title V funding is expected to support approximately 50 FTE positions in FY 2023 which
includes community health nurses, hearing and vision technicians, community health workers, and administrative
assistants implementing programs impacting women, infants and children, including those with special health care
needs.
Key Title V staff attend both national and state-level conferences and trainings that provide opportunities to acquire
new skills and strengthen existing ones as a part of federal funding requirements. Staff annually attend AMCHP,
CityMatCH and required federal grantee meetings. State Title V disseminates webinars and professional
development opportunities through staff mailing lists so that Title V State staff are aware of training opportunities.
Internal to MDH, Title V staff receive annual training on programmatic and fiscal operations such as contract
monitoring, fiscal and budgetary management, and change management. Title V staff training needs are assessed
regularly through twice-a year performance evaluations. During these performance evaluations, staff are to share
their goals over the next six months as well as challenges they have encountered. Staff are also encouraged to use
the MCH Navigator for training opportunities and resources on Title V, MCH key priorities and emerging issues,
social determinants of health, health equity and anti-racism, public health strategies, best practices and evidence-
based models and practices.
A few additional workforce development initiatives were started in FY2021. Bureau Month was started for State staff
in the Bureau of Maternal and Child Health. These sessions were for professional development and team building
sessions. There were four sessions organized by the Deputy Bureau Director with a small planning team. Staff
members weighed in on topics for the Bureau Month plenary sessions. Each week, there was a ninety minute
session with 30 minutes of team building and a 60 minute plenary session. The top three choices by staff were anti-
racism and equity, incorporating community voice into programs, and collaboration and communication. Speakers
included Dr. Eroll Bolden, Professor, Department of Social Work at Coppin State University, Ifetayo White, Founder
and Director of CHOICES Birthing and Wellness Support and the Lowcountry School of Reiki, Kristina Wint,
Program Manager, Women’s Health and Jessica Stieger, Program Manager, Infant Health from AMCHP.
Title V also organized key workshops during Black Maternal Health Week that were open to Title V staff and
partners. These workshops included: Intersectionality and Anti-Racism (Workshop #1) and Improving Maternal
Health with Community Doulas (Workshop #2). There were 96 attendees for Workshop #1 and 92 attendees for
Workshop #2. Attendees to the workshop reported that they will work to incorporate family voice into their work such
as home visiting and care coordination.
The Bureau also started regular all-staff and program leads meetings to provide additional opportunities for training
and professional development. During these meetings, staff presented on their programs or specific projects that
Created on 8/11/2022 at 8:37 PM
Page 32 of 296 pages

they had worked on. For example, Dr. Jed Miller, the Director of the Office for Genetics and People with Special
Health Care Needs and the Title V CYSHCN Director presented on Respiratory Syncytial Virus (RSV) and the
partnership with Medicaid to alert providers to atypical RSV activities and to encourage providers to consider
palivizumab prophylaxis for eligible patients. In another all-staff meeting, programs that received American Rescue
Act Funding discussed the funding that they received and how the funds would be spent. These opportunities allow
for the entire MCHB to learn about other programs and innovative initiatives.
In addition, Title V staff regularly host interns and rotating residents. During FY2021, Title V staff hosted preventive
medicine residents from University of Maryland and Johns Hopkins University.
Maryland’s robust health care delivery system, top tier institutions of higher education, and its proximity to
Washington, D.C., put it in an unfortunate position when it comes to staff retention within the State’s Title V staff as
well as staff in the local health departments. Although every effort is made to fill vacancies quickly, the state’s hiring
processes are an impediment that have been exacerbated due to COVID. During the pandemic, there had been
hiring freezes, and there is a limit to the number of civil/merit positions that any state agency is allocated. The delay
in hiring has further perpetuated retention challenges as existing staff need to undertake additional duties, further
causing fatigue and wear down. In order to address these barriers, Title V continues to share vacancy
announcements and job postings within peer networks and local health departments to assist with attracting qualified
candidates.
Other issues about MCH workforces are the lack of adult clinical providers for adults with special healthcare needs,
mental health care providers, and lack of specialty services in rural areas. In addition, there is a need for workforce
training in intersectionality, anti-racism, implicit bias, and cultural humility to improve the capability to serve diverse
and marginalized populations. During FY 2021, Johns Hopkins University provided implicit bias training from the
March of Dimes to all hospital employed perinatal providers.
Created on 8/11/2022 at 8:37 PM
Page 33 of 296 pages

III.E.2.b.ii. Family Partnership
Maryland’s Title V program focus on Family Partnership is addressed through grant funding to external community-
based organizations and local health departments and through internal initiatives.
In FY2021, Maryland’s CYSHCN Title V office continued to implement and operate “Strengthening Systems of Care
for Maryland’s Children and Youth with Special Health Care Needs,” a three-year initiative to improve family
partnerships and strengthen systems of care. This initiative was a result of a year-long planning process that
included multiple “brainstorming” meetings with staff at all levels, consultation with the Administration's Office of
Procurement and countless drafts and revisions. Through a competitive-bid process, applicants selected “focus
areas,” with Family Professional Partnership being an option, all applicants were required to propose projects
ensuring that family members would have a meaningful role in grant-funded activities. Awarded projects not only
serve CYSHCN and their families but include families in the planning and implementation of their projects.
The Parent Navigator Program from Children’s National Medical Center (CNMC) built on existing community
education programs and developed targeted educational programs for both community primary care pediatricians
and staff and pediatric trainees through a partnership with Children's National clinically integrated network, the
Pediatric Health Network (PHN). Parent Navigators are all parents of children being seen at CNMC and within its
network. They work directly in the electronic medical record system, which allows for documentation of new referrals,
early identification of issues, and easy monitoring of progress and updates on a given issue (which can be viewed by
other navigators who may be covering for or assisting the family’s primary navigator). The Parent Navigators are
employed and trained by CNMC, with a primary requirement of employment being that they are a parent of a
CYSHCN. Along with 11 other hospitals throughout the nation, CNMC is part of the Parent Mentor Learning
Collaborative (PMLC) sponsored by Lucille Packard Children’s Hospital Stanford, with a goal of creating a parent
mentor program framework to permit implementation in diverse settings, while adhering to a general set of
standards across sites.
The Coordinating Center (TCC) VIPKids Program convenes a “Medical Home Think Tank” as needed, which is
coordinated by the VIPKids Outreach and Resource Specialist and includes interested parents along with the
Program Director, the VIPKids Clinical Care Coordinator, pediatric providers, and other professionals at TCC with
expertise in care coordination for CYSHCN. The think tank may also invite other subject matter experts as needed to
help evolve and develop the program.
Rather than families, the National Alliance to Advance Adolescent Health solicits feedback directly from the pilot
population (transitioning youth). The project conducts focus groups with members of the pilot population at each
school - led by the University of Maryland’s Prince George’s School Mental Health Initiative (PGSMHI) transition
improvement team - to elicit their feedback about the transition intervention, using Got Transition’s customized Youth
Transition Feedback Survey.
Local Health Departments (LHDs) funded through Title V to support CYSHCN are also partnering with families. The
Calvert County LHD incorporated a peer mentor into its grant activities. Baltimore County LHD utilizes a client
satisfaction survey as a continuous quality assurance tool, assessing client and family satisfaction, measuring
program impact, and ensuring best practices are followed by the project. Baltimore County’s overall focus is on
family professional partnership, which they are advancing through care coordination, education of families, needs
assessments through focus groups, education through provider toolkits and expansion of emergency preparedness
efforts for CYSHCN - all reviewed by the aforementioned client satisfaction survey. In addition to service provision to
families, the Talbot County LHD provides family and provider engagement opportunities through the Eastern Shore
CoC. The COC-ES is a broad group of local, regional and state partners, including parents/family members, who
Created on 8/11/2022 at 8:37 PM
Page 34 of 296 pages

meet quarterly to build and strengthen connections, share data and initiatives, identify needs/challenges, and
collaborate to resolve issues. Additionally, opportunities to educate and inform group participants on relevant topics
from speakers from across the region and state are scheduled.
Title V continues to strengthen family partnerships through relationships with professional organizations, academic
tertiary/specialty care centers and community-based organizations on a state and national level. Title V utilizes these
partnerships to identify opportunities and to plan activities to engage families and improve family professional
partnerships within the state. Staff have presented and served as faculty representing the “family voice” at a national
level, frequently attend professional development opportunities focused on family partnership and engagement and
maintain administrative responsibility for the coordination of several state-wide advisory committees and serve as
members on other committees; all of which mandate some form of lived experience within their member rolls.
In addition to the above, other County Local Health Departments have worked to develop family and community
partnerships. As an example, B’more for Healthy Babies is an initiative to reduce infant mortality in Baltimore City
through policy, programs, service improvements, community mobilization, and behavior change. They have
developed a community advisory board to work closely with families and community representatives to improve
infant health across the city and in neighborhoods most impacted by premature birth, low birth weight, and unsafe
infant sleep.
The Maryland Family Planning Program (MFPP) requires Information and Education initiatives in program
promotion, community outreach, advisory committees that include family partnerships. Family partnerships
continued and examples of initiatives include engaging with families at health fairs, church fairs, and at farmers
markets. While many staff have been redirected to COVID activities, they also continue to participate in this activity
but have often shifted to virtual opportunities.
Created on 8/11/2022 at 8:37 PM
Page 35 of 296 pages

III.E.2.b.iii. MCH Data Capacity
III.E.2.b.iii.a. MCH Epidemiology Workforce
Maryland’s MCH epidemiology team is housed in the Office of Quality Initiatives. The MCH State staff consists of an
Epidemiology Program Manager who serves as the Epidemiology supervisor, a high-level Epidemiologist III, and two
contractual Epidemiologists who are assigned to the COVID-19 Surveillance for Pregnant Women and Infants
project. MCHB is currently in the process of recruiting for the vacant Epidemiologist II position who focuses on the
State Systems Development Initiative (SSDI) as well as Sudden Unexpected Infant Deaths (SUID) Initiative. The
majority of the epidemiology activities related to SSDI are performed by the Epidemiologist II, however, all
epidemiologists share duties and their work overlaps.
Created on 8/11/2022 at 8:37 PM
Page 36 of 296 pages

III.E.2.b.iii.b. State Systems Development Initiative (SSDI)
Since the mid-1990’s, Maryland’s State Systems Development Initiative (SSDI) Project has focused on the
following:enhance and maintain a strong Maternal and Child Health (MCH) data infrastructure to support Title V
needs assessment, planning, implementation, evaluation, and data driven decision-making. The intent is to align with
the SSDI Performance Measure structure and goals, supporting essential State MCH data efforts to improve
performance measurement, accountability and quality. This program addresses the needs for increased state MCH
epidemiology capacity for both state and Title V needs, improved systematic MCH data coordination, linking,
sharing, and use of data for translation to policy and program development. The program also continues technical
assistance for MCH and Children and Youth with Special Health Care Needs (CYSHCN) program staff in local health
agencies to improve MCH infrastructure and monitoring and evaluation of MCH programs and activities at the state
and jurisdiction level. The SSDI program is housed within the Office of Quality Initiatives (OQI) in the Maternal and
Child Health Bureau (MCHB) of the Prevention and Health Promotion Administration (PHPA) at the Maryland
Department of Health (MDH).
Maryland has implemented a variety of strategies including recruitment of staff with expertise in epidemiology and
database development, identification of data sources and proxy measures for monitoring Title V supported
programs, completion of Title V needs assessments, and enhanced collaboration with the Maryland Vital Statistics
Administration (VSA) to improve data linkages with surveys and surveillance systems for identification of MCH health
disparities and program development.
There have been recent noteworthy developments in achieving the goal of direct, annual access to timely electronic
maternal and child health data. First, MDH has continued to use a portion of SSDI and ELC Project W funds to
support an administrative specialist position at Maryland’s VSA to increase data support capacity within the office.
Aligned with our project plan, a Memorandum of Agreement (MOA) was maintained to use SSDI funds to support an
administrative assistant in the Vital Statistics Administration (VSA) to improve MCHB Epidemiologist access to birth
and death certificate vital statistics data. Receipt of these data in 2018 led to the production of a comprehensive
Perinatal Periods of Risk (PPOR) analysis for the years 2010-2016, and the creation of census tract level risk maps
to help coordinate and enhance local program design to improve preconception and maternal health across the
state. The PPOR analysis and VSA data were also used to create jurisdiction-level Fetal and Infant Mortality Review
(FIMR) profiles which continue to inform about fetal and infant deaths, and areas to focus prevention efforts aimed at
reducing rates and addressing disparities.
Improved access to de-identified birth and death certificate data has been crucial in Title V activities this year. The
SSDI team collected, analyzed and entered data on the outcome and performance measures in support of the
State’s Title V MCH Block Grant application and Annual Report. This data has also been integral to developing many
goals and objectives for future Title V work, such as developing performance measures for severe maternal
morbidity and childhood asthma emergency department visits, as well as Maryland’s Statewide Integrated Health
Improvement Strategy (SIHIS) and Maternal Health Improvement Strategic Plan (MHIP). These data were also linked
to Birth Defects Reporting and Information System (BDRIS) data to allow for analysis of maternal preconception and
prenatal health factors as they relate to birth defects.
The addition of an epidemiologist with SSDI funds supports the analysis of each of these data sources in addition to
the Child Fatality Review (CFR) and Maternal Mortality Review (MMR) case review data to further support Title V
needs assessment and performance measure reporting. The SSDI epidemiologist also provides data support for
the state’s CDC SUID (Sudden Unexplained Infant Death) Case Registry grant, which aims to strengthen public
health surveillance of SUID in Maryland through the efforts of the State CFR team.
New activities related to the current plan include continued participation in the CDC SUID and SDY Case Registry
Created on 8/11/2022 at 8:37 PM
Page 37 of 296 pages

surveillance grant initiative. These Child Fatality Review (CFR) initiatives will require regular data analysis and
reporting which is directly supported by SSDI funding and further supports Goal 3 of the strategic plan. The recent
acquisition of the infant birth records and BDRIS data file will allow advanced analyses of prenatal factors associated
with birth defects.
Currently, MCHB epidemiologists are examining a range of information contained in the PRAMS database,
especially the disability, opioid use, and COVID-19 supplemental questions.
Created on 8/11/2022 at 8:37 PM
Page 38 of 296 pages

III.E.2.b.iii.c. Other MCH Data Capacity Efforts
During the current reporting period, a SSDI/Title V Measure monitoring and tracking system was maintained for use
by the MCHB staff. The monitoring system contains data for numerous Title V outcome and performance indicators
and many of the SSDI minimum/core indicators, such as low birth weight, preterm birth, infant mortality, and teen
births. The data is presented at the race and jurisdictional levels, for years 2010-2019 (where data is available), in an
easy-to-use, interactive format that allows staff to print graphs and disseminate needed information. The monitoring
system also provides comparisons to United States (US) rates, where available. Additionally, the indicators in the
SSDI Minimum/Core dataset were monitored with the assistance of the Minimum/Core Dataset Implementation
Guide and Training Module, to monitor Maryland’s progress and compare it with other states.
Aligned with our project plan, a Memorandum of Agreement (MOA) was maintained to use SSDI funds to support an
administrative assistant in the Vital Statistics Administration (VSA) to improve MCHB Epidemiologist access to birth
and death certificate vital statistics data.
The annual Maternal Mortality Review (MMR) Legislative Report for 2020 was completed in December of 2020 and
released in November 2021. The annual Child Fatality Review (CFR) Legislative Report for 2020 was completed in
May of 2021 and was approved in December 2021. Data on child fatality was presented at quarterly Maryland CFR
State Team meetings in 2020 and 2021. MCHB Epidemiology staff-maintained access to ImmuNet, Maryland’s
Immunization Information System Database to allow for access to immunization records for child fatality cases. SSDI
staff continued collaboration with the Office of the Chief Medical Examiner (OCME) to solve issues related to child
fatality data collection and dissemination to the state and local teams for analysis. Maryland is also continuing
participation in the CDC Sudden Unexpected Infant Death (SUID) and Sudden Death in Young (SDY) Case Registry
surveillance grant initiative which started September 30, 2018, and ends September 29, 2023. The final 2019 SUID
data was completed and submitted to the CDC in December of 2020.
An interactive map of elevated indicators across the state of Maryland was maintained in conjunction with the
Maternal, Infant, and Early Childhood Home Visiting (MIECHV) program, after initial dissemination to the MCHB in
August 2018. The interactive map
[1]
, now publicly available, provides a visual representation of the high-risk areas
across the state. Jurisdiction specific risk levels can also be viewed by selecting individual jurisdictions. The map
features 23 indicators, including preterm birth, low birth weight, infant mortality, prenatal care, maternal education,
poverty, unemployment, Medicaid enrollment, and crime rate. The MIECHV needs assessment was updated in July
of 2021, which highlighted the elevated indicators across the state. The interactive map was updated with data from
the needs assessment in November 2021. The map was shared with all of the MIECHV program sites, home visiting
consortium members and early childhood agencies.
The MCHB hosted an intern in partnership with the Graduate Student Epidemiology Program (GSEP) within the
Association of Maternal and Child Health Programs (AMCHP). This intern used data from the Maryland Pregnancy
Risk Assessment Monitoring Survey (PRAMS) to develop a data brief about gestational hypertension. The data brief
was completed in August of 2021 and was posted on the MCHB website. The 2018 and 2019 Maryland PRAMS
responses met the CDC’s threshold for response rate, and the data was released to Maryland in March of 2021. The
annual reports will be available on the MCHB website this year. PRAMS data was used to develop a data to action
(DTA) brief which analyzed opioid use during pregnancy. The results of this analysis were presented to the
Prevention and Health Promotion Administration (PHPA) opioid meeting, which shares best practices amongst
Maryland Department of Health programs affecting those with substance use disorder.
SSDI is continuing to support the assessment and evaluation of neonatal abstinence syndrome (NAS) and
substance exposed newborns (SEN) data in Maryland. Using Health Services Cost Review Commission (HSCRC)
Created on 8/11/2022 at 8:37 PM
Page 39 of 296 pages

newborn discharge data MCH staff have examined NAS and SEN trends based on ICD-9 coding but have noticed
significant changes in the codes used to identify NAS and SEN under ICD-10. These findings are frequently shared
with internal and external stakeholders to begin a discussion about how to better measure and track NAS and SEN.
In July 2020, MDH relaunched the Maryland Perinatal-Neonatal Quality Collaborative which is being led by Health
Quality Innovators (HQI). The collaborative works with all 32 birthing hospitals in Maryland. The current collaborative
focuses on maternal hypertension and newborn antibiotic stewardship. MCHB Epidemiologists provided statistics
on maternal severe hypertension using inpatient hospitalization data using guidance from the Alliance for the
Innovation on Maternal Health (AIM) Program. MCHB Epidemiologists provide data support for these efforts using
data from HSCRC, VSA, and PRAMS.
In September 2019, Maryland was granted a funding opportunity through the Health Resources and Services
Administration (HRSA), and MDH convened the Maryland Maternal Health Improvement Task Force. This
collaboration between Johns Hopkins University, Maryland Department of Health, Maryland Patient Safety Center
and the University of Maryland, Baltimore County will address the needs of pregnant and postpartum women in
Maryland, through coordinated innovation in the areas of data, resource availability, and hospital and community
care. MCH epidemiologists support the work of the task force to provide state maternal health data, and perinatal
health data. The current work of the team is to support data related to severe maternal morbidity to create a
surveillance and review process of maternal data using HSCRC data. Participation in this workgroup will continue
the duration of the grant and will support data integration and development of a maternal health dashboard.
In July 2020, MCH was granted funding through the Centers of Disease Control and Prevention to expand current
surveillance activities to include surveillance of COVID-19 in pregnancy and monitor pregnancy and infant outcomes
through the Project W: Infants with Congenital Exposure: Surveillance and Monitoring to Emerging Infectious
Diseases and Other Health Threats. MCH epidemiologists are leading efforts to support collaborative participation
in surveillance data systems for COVID-19 in pregnant people and their exposed infants. MCHB is developing
systems to collect follow-up clinical data through linkages to data sources and medical records abstraction to ensure
identification of pregnant women and infants. Two staff were hired to assist in this work. The epidemiology team
developed a detailed data process document outlining the flow of data during the surveillance project. The project
involves multiple partners: a health information exchange system, the Chesapeake Regional Information System for
our Patients (CRISP), the Vital Statistics Administration (VSA), and the Infectious Disease Bureau (IDB). 2020
COVID-19 pregnancies identified using CRISP and IDB were linked to the VSA live birth files to analyze maternal
demographics and prenatal health. Using this linked data, epidemiologists completed a COVID-19 data brief and
presentation comparing all live births in Maryland in 2019 to births with a positive test in 2020. The epidemiologist’s
complete monthly data tasks required by the CDC and attends programmatic meetings. Epidemiologists complete
other data tasks when necessary for program advancement.
SSDI staff are continuing education and staying abreast of current health topics by attending webinars and
conferences related to maternal and child health and health equity. The MCH Epidemiology team attended the 2020
CityMatCH Leadership and MCH Epidemiology Virtual Conference in September 2020 as well as the National
Maternal Health Innovation Symposium in August 2021.
SSDI staff provided data analysis on maternal and child health indicators to support the Babies Born Health
program. The program was initiated in 2016 to target jurisdictions with the highest numbers and rates of infant
mortality in the state of Maryland. Jurisdictions were selected using data-driven methods which were updated in the
fall of 2021 to update jurisdictions with the greatest need.
An in-depth review of the organization, roles, and needs of the MCH Epidemiology team was conducted in the
Created on 8/11/2022 at 8:37 PM
Page 40 of 296 pages

summer and fall of 2021. Each task was evaluated to determine its need and importance within the Bureau and
assigned to a member within the team to better organize the workflow and structure of the MCH Epidemiology team.
The MCH Epidemiology Program Manager also consulted with Epidemiology Leads in other MDH Bureaus to better
understand their project management approach to teams and assignments.
In early 2021, the Statewide Integrated Health Improvement Strategy selected two MCH domains, 1. the reduction of
severe maternal morbidity (SMM) and 2. asthma-related emergency department visits for children ages two to 17.
The MCH epidemiology team provided data analysis expertise to determine the reduction goals for this domain
using inpatient and emergency department hospitalization data with a focus on reducing disparities.
In the spring and summer of 2021, MDH drafted a Maryland Maternal Health Improvement Plan (MHIP) to help
improve how agencies, organizations, community groups, and residents work together to reduce maternal deaths
and complications in Maryland over the next five years. MCH epidemiologists provided data analysis related to
maternal mortality (MMR) such as rates and disparity metrics. Additionally, data analysis on severe maternal
morbidity (SMM) was conducted to include racial breakdowns on SMM rates over a 10-year period with projections
through 2026. The epidemiology team assisted with calculating the projected reduction of MMR and SMM over time
to reduce racial disparities, particularly among the Black, non-Hispanic population.
MCHB implemented an Interagency Agreement (IA) with the University of Maryland College Park (UMCP) to assist
with higher level analyses of maternal and child health data. An in-depth analysis on sickle cell disease and sickle
cell disease trait was conducted and a report outlining the findings was shared. The findings helped to inform our
sickle disease strategy in Maryland.
Fetal, infant, and maternal data was used to create Maternal and Infant Health (MIH) profiles for each of the 24
jurisdictions in the state. The profiles summarize maternal and child health indicators for each jurisdiction as well as
compared to other jurisdictions and the state overall. The MIH profiles will help inform jurisdictions of at-risk
populations and areas of improvement as related to maternal and infant health. The MIH profiles are currently under
review with a planned dissemination later this fiscal year.
[1]
https://maps.health.maryland.gov/phpa/mch/indicators/ NOTE: A recent network security incident caused disruption to some of the
Maryland Department of Health (MDH) operations including ArcGIS online.
Created on 8/11/2022 at 8:37 PM
Page 41 of 296 pages

III.E.2.b.iv. MCH Emergency Planning and Preparedness
The Maryland Emergency Management Agency (MEMA) conducts statewide emergency planning in Maryland.
MEMA oversees development of four Operations Plans, including Prevention/Protection, Response, Disaster
Recovery, and Mitigations plans. These plans are part of a hierarchy that also includes a Training and Exercise Plan
and an All-Hazards Mitigation Plan, which together comprise the Maryland Emergency Preparedness Program that
serves as Maryland’s strategic plan for emergency preparedness. In addition, the Maryland Department of Health
(MDH or the Department) Office of Preparedness and Response (OPR) coordinates the state’s public health and
medical response during an emergency. OPR coordinates with local health departments, acute care hospitals,
federally qualified health centers, Emergency Medical Services (EMS) and other health care entities. OPR
additionally provides tools and resources to Maryland residents, including a Family Emergency Communication Plan
that provides families important numbers such as the Maryland Poison Control and assists the family in planning to
know the contact information for their doctors, electric companies, gas companies, and pharmacies.
While the MEMA and OPR conduct statewide emergency planning, MDH is working towards increasing its workforce
capacity to create and contribute to emergency plans, protocols, and procedures. On November 30, 2021, the
Department issued two new policies related to preparedness and response that required all current employees to
complete an online Incident Command System (ICS) prep course through the State’s online training platform and
complete the FEMA IS 100, 700, and 800 courses within the year.
During SFY 2021, Title V staff continued to respond to the COVID-19 Pandemic. Staff were reassigned to COVID
testing, vaccinations, and outbreak response. In addition, staff also developed COVID-19 vaccination materials that
provided information on the importance of vaccination.
During FY2021 and 2022, Title V staff responded to a call from MDH Office of Preparedness and Response to join
the Medically Fragile Afghan Parolee response. Title V staff were well positioned to serve in this response effort as
there was a population of parolees arriving in Maryland, including pregnant individuals who had received little or no
prenatal care and their extended families. Title V staff worked within the Incident Command Structure (ICS) to serve
as the point of contact between public health, local jurisdictions and the federal response agencies who were
coordinating to meet the needs of the parolees. Title V staff lead the development of a secure tracking system to
identify the medical needs of the parolees and facilitate collaboration among community partners and created a
triage protocol for incoming parolees, to assess medical needs as well as cultural, and social needs. MCH staff
served as a key convener between local health departments and community medical providers to identify the
capacity and identify roles of MCH providers and their response to the plan to provide comprehensive care to
parolees. MCH staff were also able to collaborate internally with WIC program leadership to identify opportunities for
parolees to enroll in WIC. One key response identified through this parolee response was the need to provide infant
safe sleep education and supplies to recent arrivals. MCH staff worked closely with Montgomery County local health
department to leverage public health nurses and in person visits to conduct safe sleep assessments and onsite
educational opportunities for families to gain knowledge and safe sleep supplies such as a pack n’play.
During FY2022, the Department experienced a Network Security Event that resulted in the Department’s information
and technology systems being taken offline out of an abundance of caution. The event started in December and was
confirmed to be as a result of a ransomware attack.
Immediately, the Continuity of Operations Plan (COOP) for the Prevention and Health Promotion Administration and
Title V was implemented. Three essential life-saving programs were identified within the Maternal and Child Health
Bureau: Newborn Screening Follow-up, Children’s Medical Services, and the Women, Infants, and Children (WIC)
Created on 8/11/2022 at 8:37 PM
Page 42 of 296 pages

services. All three COOP MCHB programs met daily to ensure operations would continue. In addition, all Title V and
MCH programs met frequently to determine workarounds to ensure operations would continue.
Newborn bloodspot screening was identified as a priority service and an emergency procurement was enacted to
complete screening through an external vendor. For both initial screens (collected just after 24 hours of life) and
second screens (usually collected around 2 weeks of age), providers were directed to continue to send specimens
to the Maryland State Laboratory for subsequent processing and transportation to the PerkinElmer Laboratory. The
Newborn Screening Follow-up team met daily to develop new follow up protocols and to troubleshoot any issues
immediately. They also met frequently with the Maryland Laboratory Administration to develop new protocols on
shared processes of follow up on laboratory results and how to report abnormal test results to providers. The nurses,
who are Title V staff, also communicated with providers about the new protocols and responded to provider
questions and concerns on behalf of the State Lab when needed. A clinician letter was prepared and sent to all
Maryland clinicians on January 10, 2022, and the Newborn Screening webpage was updated with information for
providers related to screening and follow up protocols and procedures to request specimen collection kits.
The Children’s Medical Services (CMS) Program team also met daily to plan, implement, and troubleshoot
workarounds so enrollment applications, pre-authorization requests and claims for payment could continue and that
care for enrolled children and youth with special healthcare needs would not be disrupted. While the CMS Program
is still largely paper-based, the Program relies on networked printers, scanners and fax machines. Therefore, CMS
was able to secure a non-networked printer to continue printing and scanning letters to families, pre-authorization
notifications to providers, and required documentation for claims payment.
The Maryland WIC program partnered with local health departments who were also affected by the Network Security
Event to provide guidance to local agencies.
While the aforementioned three programs are specifically noted in the COOP, all Title V programs were affected by
the Network Security Event. Although this occurred in SFY2022, the security event affected documentation and
accessibility of SFY2021 data, planning of programs and services for SFY2023 and beyond, including this Title V
application, and made even the simplest of daily tasks complex and challenging. Title V Program staff initially had to
rely on personal devices or a “hotelling” space of laptops in the state office building and did not have access to any
internal shared network drives. Data analytic programs such as SAS were not able to be used and many state-wide
data systems were locked down to MDH contact out of an abundance of caution. The Title V team developed
workarounds to continue providing services. Title V staff re-created documents, re-developed reports, developed,
implemented and trained on new operational protocols, and developed and implemented new data collection tools -
all while using personal or borrowed equipment. As challenging as the situation was and continues to be, the event
offered the opportunity for innovation. For example, the Children’s Medical Services program reviewed their
workflow, particularly how heavily paper-based it was, and looked at ways to automate processes. After a successful
pilot, they are now rolling out electronic submissions of applications, pre-authorization requests and claim
submissions.
III.E.2.b.v. Health Care Delivery System
Created on 8/11/2022 at 8:37 PM
Page 43 of 296 pages
III.E.2.b.v. Health Care Delivery System
III.E.2.b.v.a. Public and Private Partnerships
Public and Private Partnerships:
Maryland Title V partners with federal and state partners to ensure access to health care services and other needed
services. Maryland Title V leads various collaboratives and committees. For a full list, please see Supplement
Attachment: Partnerships, Collaboration, and Coordination
Key collaborations include:
Maryland Perinatal Neonatal Quality Collaborative: Title V works with Maryland birthing hospitals to
strengthen the maternal and neonatal healthcare system by implementing the Alliance for Innovation on
Maternal Health (AIM) bundles.
Maternal Health Improvement Program Taskforce: The Title V manager staffs the TaskForce. This past
year, co-chairs were elected. Members developed and implemented a strategic plan to improve the
health of birthing people in Maryland.
Morbidity, Mortality, and Quality Review Committee (MMQRC): Title V staff chairs the multi-disciplinary
committee that monitors compliance with the Maryland Perinatal Standards of care for Level I and II
hospitals. Title V staff also participate in compliance with Level III and IV Perinatal Standards of Care.
Perinatal Clinical Advisory Committee: Title V chairs the multi-disciplinary committee of other state
agencies, clinical leaders, and professional organizations that determine the standards of care for
Maryland Birthing Hospitals using the national American Academy of Pediatrics and American
College of Obstetrics guidelines.
Statewide Integrated Health Improvement Strategy: The strategy is part of Maryland’s Total Cost of
Care Model and designed to engage State agencies and private sector partners to collaborate and
invest in improving health, addressing disparities, and reducing costs for Marylanders. Title V staff lead
the maternal and child health portion of the Statewide Integrated Health Improvement Strategy.
Partners including payers, Health Information Exchange, professional societies, hospitals, and more.
Created on 8/11/2022 at 8:37 PM
Page 44 of 296 pages

III.E.2.b.v.b. Title V MCH – Title XIX Medicaid Inter-Agency Agreement (IAA)
Title V MCH-Title XIX Medicaid Inter-Agency Agreement:
Program Outreach and Enrollment
Title V has continued to collaborate with the Medicaid Program to improve access to health care services for women
and children. As a Medicaid Expansion state, Maryland has decreased the numbers of uninsured individuals over
the past 6 years. Maryland’s uninsured rate declined from 10.1% in 2012 to 5.9% in 2020 and is lower than the
national rate of 8.7%. Since 2015, the uninsured rate in Maryland decreased for all races and ethnicities but
remained highest for Hispanic individuals (21.4% in 2020, a decrease from 22.1% percent in 2019). The uninsured
rate decreased for all age groups since 2018. The uninsured rate remains highest among those aged 25 to 34
years in 2020. In 2021, birthing people’s coverage will increase from two months to 12 months postpartum.
As more eligible residents have received Medicaid coverage to enable them to access health care, Title V has
shifted its structure from a direct and gap filling model to more of a population and infrastructure-based model.
Direct, gap filling services are largely provided by the Children’s Medical Services (CMS) Program to children with
special health care needs who are ineligible for Medicaid services. Over the past several years, expenditures for
direct, gap filling services for the CMS Program have increased.
Health Care Financing
Maryland Managed Care Organizations (MCOs) provide services to Medicaid recipients by contracting with a
network of licensed/certified healthcare providers. All MCOs are responsible to provide or arrange for a wide array
of healthcare services. There are nine managed care organizations in Maryland: Aetna Better Health, Amerigroup
Community Care, Carefirst Blue Cross Blue Shield Community Health Plan, Jai Medical Systems, Kaiser
Permanente, Maryland Physicians Care, MedStar Family Choice, Priority Partners, and UnitedHealthCare. Nearly
90% of Medicaid participants were enrolled in managed care in Calendar Year 2019.
Maryland Medicaid does not participate in a Primary Care Case Management (PCCM) program as PCCM is
considered an alternative to manage care.
Through the Total Cost of Care All-Payer Model contract the State of Maryland has entered with the Federal
Government, the Maryland Primary Care Program (MDPCP) has been developed. A separate office within MDH
works with interested primary care offices to coordinate care for patients across both hospital and non-hospital
settings, improve health outcomes, and constrain the growth of health care costs in Maryland. MDPCP is a voluntary
program open to all qualifying Maryland primary care providers that provides funding and support for the delivery of
advanced primary care throughout the state.
Waivers or State Plan Amendments
Medicaid has operated a Home Visiting Services (HVS) pilot since 2017 through its §1115 waiver, which has
enabled an expansion of evidence-based home visiting services to Medicaid eligible high-risk pregnant individuals
and children up to age two. The HVS pilot program is aligned with two evidence-based models focused on the health
of pregnant individuals. The Nurse Family Partnership (NFP) model is designed to reinforce maternal behaviors that
encourage positive parent-child relationships and maternal, child and family accomplishments. The Healthy Families
Created on 8/11/2022 at 8:37 PM
Page 45 of 296 pages

America (HFA) model targets parents facing issues such as single parenthood, low income, childhood history of
abuse, substance use disorder, mental health issues or domestic violence. The current financing structure of the HVS
pilot, which requires local lead government entities to provide a local match through an intergovernmental transfer,
has garnered limited participation from additional lead entities because of the requirement to produce the required
match from non-federal 10 funding sources.
The Maryland Health Services Cost Review Commission (HSCRC) committed $8 million in annual funding to support
Medicaid initiatives to address severe maternal morbidity and pediatric asthma. Therefore, during Fiscal Year 21
and 22, Medicaid staff worked on statewide expansion of the Home Visiting Services (HVS) pilot, statewide
expansion of the Maternal Opioid Misuse (MOM) Model Pilot, Medicaid coverage for Doula/Birth Workers Services,
Medicaid Coverage for HealthySteps, and Medicaid Coverage for CenteringPregnancy.
Effective January 13, 2022, Maryland Medicaid expanded coverage for evidence-based home visiting services to all
Maryland beneficiaries through the State Plan Amendment. Home Visitors associated with one of two evidence-
based models, Healthy Families America (HFA) or Nurse-Family Partnership (NFP) are the two covered models.
Doulas are trained nonmedical professionals who provide continuous physical, emotional and informational support
to birthing parents throughout the prenatal and postpartum periods, including labor and delivery. These services will
help increase access to care and lead to fewer low birth weight babies, birth complications, and C-sections.
Coverage of doulas are through a State Plan Amendment. CenteringPregnancy is a program that offers group
prenatal care for low-risk pregnancies, including screenings for sexually transmitted infections and HIV. HealthySteps
promotes positive parenting and healthy development for babies and toddlers. The program aims to decrease
postpartum depression and emergency department usage for care, as well as to increase child vaccination rates
and well-child visits. The MOM model provides enhanced case management for pregnant and postpartum individuals
with opioid use disorder, including screenings for needs related to social determinants of health and maternal anxiety
and depression. The MOM model is authorized under 1115 waiver.
In 2017, the Maryland Department of Health submitted a successful application to the Centers for Medicare and
Medicaid Services (CMS) for a Health Services Initiative (HSI) under the Children’s Health Insurance Program
(CHIP). The program, approved as a State Plan Amendment (SPA), allowed MDH to create a $3 million home
visiting program for children who are enrolled in or eligible for Medicaid (including CHIP), based on diagnosis of
either moderate to severe asthma or lead poisoning. The program operates in nine jurisdictions: Baltimore City and
Baltimore, Charles, Dorchester, Frederick, Harford, Prince George’s, St. Mary’s, and Wicomico Counties. These are
sites with some of the highest burden of asthma ED visits. Once they are deemed eligible and enrolled in the
program, the children’s families are eligible for up to six home visits to receive education and training around home
environmental factors that trigger asthma, durable goods that can reduce or eliminate home triggers, and improved
care coordination with providers through asthma action plans. The program similarly provides home visiting for
eligible children who have been lead poisoned and is one of the first such programs in the country. The home visiting
program is built on evidence-based models that emphasize remediation of environmental factors, including the
provision of education and training for parents, and provision of durable cleaning supplies and other equipment to
assist families in reducing environmental factors including dust mites, insect and pet allergens, and other common
allergens.
Joint Policy Level Decision Making
The current IAA with Maryland Medicaid outlines agreements and guidelines on administration and policy, systems
coordination, outreach and referral activities and data sharing.
Created on 8/11/2022 at 8:37 PM
Page 46 of 296 pages

Title V staff at the local health departments work with and coordinate with the Medicaid-operated Administration
Care Coordination Unit (ACCU) to identify and enroll eligible pregnant people and children in the Medicaid
program. ACCU serves as the central link between the beneficiary, managed care organization (MCO), healthcare
provider and the Department of Health.
Title V is partnering with Medicaid to improve referrals through the Prenatal Risk Assessment and the Postpartum
Infant Maternal Referral Form to the Local Health Departments. These referrals help to navigate social needs for
birthing people who are in need of services.
In addition, Title V staff is working with Medicaid to achieve the goals for the Statewide Integrated Health
Improvement Strategy. Specifically, Title V staff is working with Medicaid and other staff to expand asthma home
visiting and maternal, infant, early childhood home visiting.
Created on 8/11/2022 at 8:37 PM
Page 47 of 296 pages

III.E.2.c State Action Plan Narrative by Domain
State Action Plan Introduction
Needs Assessment and State Action Plan
Please see the National Performance Measures for Maryland
National Performance Measure Population Domain
NPM 3 Risk-Appropriate Perinatal
Care
Perinatal/Infant Health (PIH)
NPM 4 Breastfeeding PIH
NPM 5 Safe Sleep PIH
NPM 6 Developmental Screening Child Health (CH)
NPM
10
Adolescent Well-Visit Adolescent Health (AH)
NPM
11
Medical Home Children with Special HealthCare Needs
(CSHCN), CH
NPM
12
Transition CSHCN, AH
NPM
13.1
Preventive Dental Visit -
Pregnancy
Women’s/Maternal Health (WMH)
NPM
14.1
Smoking - Pregnancy WMH
Please see the State Performance Measures:
Table 2
Created on 8/11/2022 at 8:37 PM
Page 48 of 296 pages

State Performance Measure
Population
Domain
SPM
1
Number of overdose mortalities for women, ages 15-49 in
Maryland per 100,000 population
WMH
SPM
2
The excess rate between the Black Non-Hispanic Severe
Maternal Morbidity (SMM) events to White Non-Hispanic SMM
events per 10,000 delivery hospitalizations
WMH
SPM
3
Receipt of primary care during early childhood (Percent of children
enrolled in Medicaid who reached age 15 months who had 5 or more
well care visits in their first 15 months of life)
CH
SPM
4
Number of Asthma ED visits per 1,000 for ages 2-17 CH, AH
SPM
5
Percentage of MCHB committees/workgroups that include
community members/persons with lived experience
Cross
Cutting
Women/Maternal Health
National Performance Measures
NPM 13.1 - Percent of women who had a preventive dental visit during pregnancy
Indicators and Annual Objectives
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - Pregnancy Risk Assessment Monitoring System (PRAMS)
Maryland - Pregnancy Risk Assessment Monitoring System (PRAMS)
Maryland - Objectives
Created on 8/11/2022 at 8:37 PM
Page 49 of 296 pages

Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2017 2018 2019 2020 2021
Annual Objective 57.9 58.6 59.3 60 54.9
Annual Indicator 52.6 53.3 53.3 54.1 47.0
Numerator 34,237 33,752 33,752 33,888 28,934
Denominator 65,122 63,361 63,361 62,695 61,594
Data Source PRAMS PRAMS PRAMS PRAMS PRAMS
Data Source Year 2015 2017 2017 2019 2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 55.7 56.5 57.3 59.1
Created on 8/11/2022 at 8:37 PM
Page 50 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 13.1.1 - Percentage of pregnant individuals aged 21 and older on medical assistance in Maryland who
receive a preventive dental visit
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 28.4
Annual Indicator 28.2 28.8 21.6
Numerator 7,979 8,346 6,666
Denominator 28,259 28,939 30,925
Data Source Office of Oral Health
Legislative Report
Office of Oral Health
Legislative Report
Office of Oral Health
Legislative Report
Data Source Year CY 2018 CY 2019 CY2020
Provisional or Final ? Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 29.9 31.4 32.5 34.0
Created on 8/11/2022 at 8:37 PM
Page 51 of 296 pages
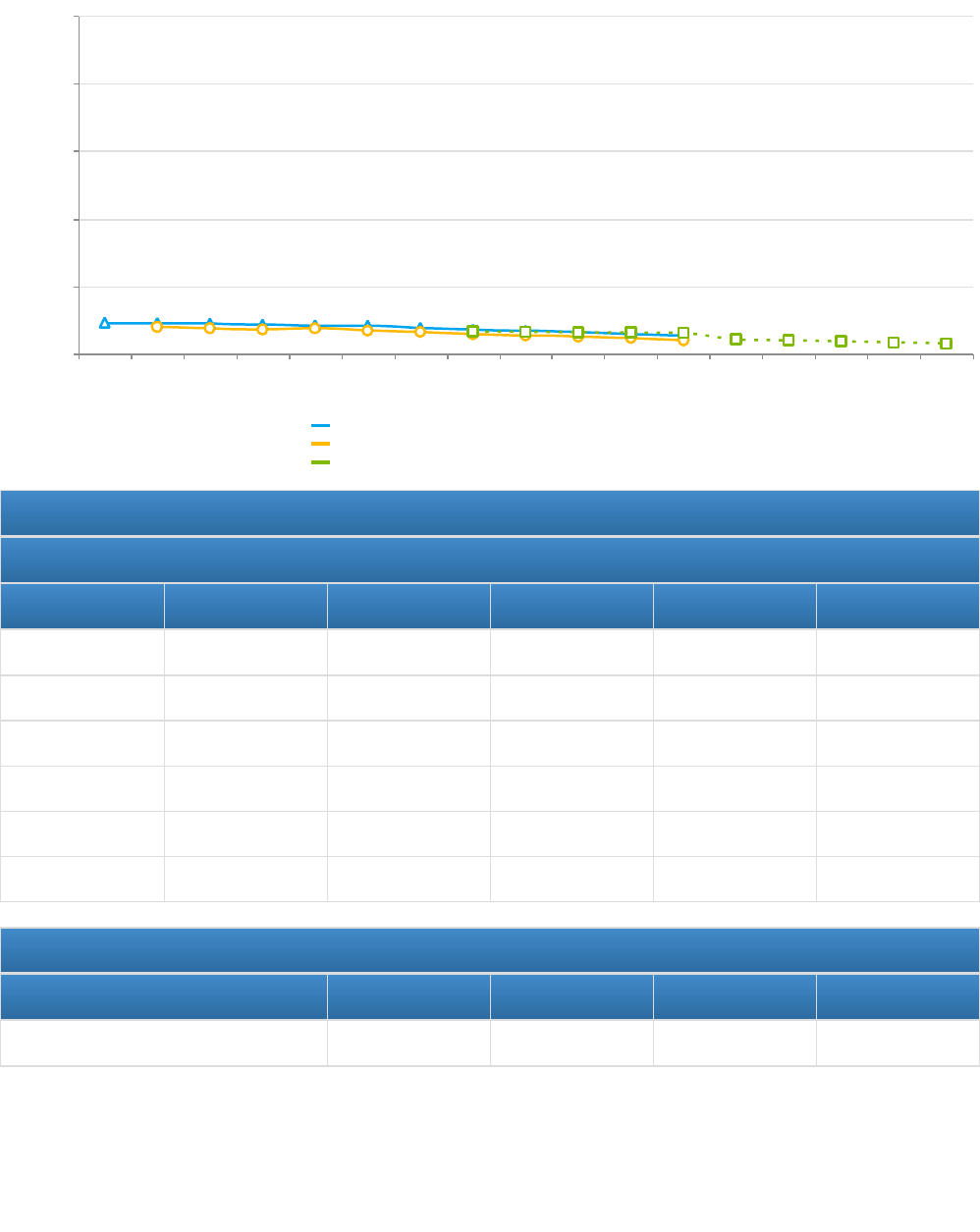
NPM 14.1 - Percent of women who smoke during pregnancy
Indicators and Annual Objectives
Federally Available Data
Data Source: National Vital Statistics System (NVSS)
2017 2018 2019 2020 2021
Annual Objective 6.6 6.5 6.4 6.3 4.4
Annual Indicator 5.9 5.5 5.3 4.7 4.2
Numerator 4,299 3,932 3,719 3,281 2,846
Denominator 72,838 71,324 70,599 69,782 68,236
Data Source NVSS NVSS NVSS NVSS NVSS
Data Source Year 2016 2017 2018 2019 2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 4.1 3.8 3.5 3.2
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - National Vital Statistics System (NVSS)
Maryland - National Vital Statistics System (NVSS)
Maryland - Objectives
Created on 8/11/2022 at 8:37 PM
Page 52 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 14.1.1 - Number of pregnant individuals who use the statewide tobacco QuitLine
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 167 136 137 139 140
Annual Indicator 135 131 99 86 67
Numerator
Denominator
Data Source MDH CTPC
Quitline Data
MDH CTPC
Quitline Data
MDH CTPC
Quitline Data
Quit Line Data Quit line Data
Data Source Year FY17 FY 18 FY 19 FY 2020 FY2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 142.0 143.0 143.0 143.0
Created on 8/11/2022 at 8:37 PM
Page 53 of 296 pages

State Performance Measures
SPM 1 - Rate of overdose mortality for women ages 15-49
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 24.1 35.7
Numerator 334 493
Denominator 1,385,375 1,381,029
Data Source VSA CDC Wonder using ICD-10 Codes
Data Source Year 2019 2021
Provisional or Final ? Final Provisional
Annual Objectives
2022 2023 2024 2025
Annual Objective 23.9 23.7 23.5 23.3
Created on 8/11/2022 at 8:37 PM
Page 54 of 296 pages

SPM 2 - Excess rate between Black Non-Hispanic Severe Maternal Morbidity (SMM) events to White Non-Hispanic
SMM events per 10,000 delivery hospitalizations
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 328.5 381.4
Numerator 640 690
Denominator 19,481 18,090
Data Source Health Services Cost Review
Commission
Health Services Cost Review
Commission
Data Source Year 2018 2021
Provisional or Final ? Final Provisional
Annual Objectives
2022 2023 2024 2025
Annual Objective 312.1 295.7 279.3 262.8
Created on 8/11/2022 at 8:37 PM
Page 55 of 296 pages

State Action Plan Table
State Action Plan Table (Maryland) - Women/Maternal Health - Entry 1
Priority Need
Ensure that all birthing people are in optimal health before, during, and after pregnancy
NPM
NPM 13.1 - Percent of women who had a preventive dental visit during pregnancy
Objectives
Increase the number of people receiving preventive dental visits from a baseline of 28% to 36% by 2025.
Strategies
1. Distribute the Maryland Oral Health Guide 2020 through local health departments and other strategic partners. 2.
Support the Office of Oral Health in providing education to prenatal providers on the importance of oral health during
pregnancy. 3. Link pregnant people who are referred to the Maternal and Child Health Care Coordination at the Local
Health Department to Oral Health resources.
NOMs
NOM 14 - Percent of children, ages 1 through 17, who have decayed teeth or cavities in the past year
NOM 19 - Percent of children, ages 0 through 17, in excellent or very good health
NOM 17.2 - Percent of children with special health care needs (CSHCN), ages 0 through 17, who receive care in a well-
functioning system
ESMs Status
ESM 13.1.1 - Percentage of pregnant individuals aged 21 and older on medical assistance in
Maryland who receive a preventive dental visit
Active
Created on 8/11/2022 at 8:37 PM
Page 56 of 296 pages

State Action Plan Table (Maryland) - Women/Maternal Health - Entry 2
Priority Need
Ensure that all birthing people are in optimal health before, during, and after pregnancy
NPM
NPM 14.1 - Percent of women who smoke during pregnancy
Objectives
To increase the number of women who abstain from smoking tobacco during pregnancy from a baseline of 95.3% to 96.3%
or more by 2025.
Strategies
1. Title V programs (e.g., Care coordination, home visiting, and other programs) will continue to refer pregnant people who
smoke to the Maryland Tobacco Quitline and other smoking cessation programs. 2. The Maryland Family Planning
Program will implement SBIRT (Screening, Brief Intervention, Referral to Treatment) with their subrecipient sites.
NOMs
NOM 2 - Rate of severe maternal morbidity per 10,000 delivery hospitalizations
NOM 3 - Maternal mortality rate per 100,000 live births
NOM 4 - Percent of low birth weight deliveries (<2,500 grams)
NOM 5 - Percent of preterm births (<37 weeks)
NOM 6 - Percent of early term births (37, 38 weeks)
NOM 8 - Perinatal mortality rate per 1,000 live births plus fetal deaths
NOM 9.1 - Infant mortality rate per 1,000 live births
NOM 9.2 - Neonatal mortality rate per 1,000 live births
NOM 9.3 - Post neonatal mortality rate per 1,000 live births
NOM 9.4 - Preterm-related mortality rate per 100,000 live births
NOM 9.5 - Sudden Unexpected Infant Death (SUID) rate per 100,000 live births
NOM 19 - Percent of children, ages 0 through 17, in excellent or very good health
ESMs Status
ESM 14.1.1 - Number of pregnant individuals who use the statewide tobacco QuitLine Active
Created on 8/11/2022 at 8:37 PM
Page 57 of 296 pages

State Action Plan Table (Maryland) - Women/Maternal Health - Entry 3
Priority Need
Ensure that all birthing people are in optimal health before, during, and after pregnancy
SPM
SPM 1 - Rate of overdose mortality for women ages 15-49
Objectives
To decrease the overdose mortality rate for women, age 15-49 from 24.1 per 100,000 to 22.9 per 100,000 by 2025.
Strategies
1. Improve linkages to care for substance use disorder treatment through implementing the electronic prenatal Risk
Assessment with State Medicaid, Overdose Data to Action partners and updating the postpartum infant maternal referral
form (PIMR) 2. Partner with Medicaid to improve lnkages with the Managed Care Organizations through the Maternal
Opioid Misuse Model. 3. Develop appendices of a Linkages to Care toolkit for providers of birthing people. 4. Monitor and
understand opioid use trends through PRAMS Surveillance
Created on 8/11/2022 at 8:37 PM
Page 58 of 296 pages

State Action Plan Table (Maryland) - Women/Maternal Health - Entry 4
Priority Need
Address the racial disparities in Severe Maternal Morbidity rates among Black NH and White NH
SPM
SPM 2 - Excess rate between Black Non-Hispanic Severe Maternal Morbidity (SMM) events to White Non-Hispanic SMM
events per 10,000 delivery hospitalizations
Objectives
Decrease the excess rate of Black NH Severe Maternal Morbidity rate to White NH Severe Maternal Morbidity rate by 25%
by 2026.
Strategies
1. Implement expansion of programs that improve maternal health through the Statewide Integrated Health Improvement
Strategy. 2. Implement the severe maternal hypertension bundle developed by the Alliance for Innovation on Maternal
Health (AIM) in the Maryland Perinatal Neonatal Quality Collaborative (MDPQC). 3. Develop and implement a maternal
health strategic plan by the Maternal Health Improvement Taskforce as part of the Maternal Health Innovation Program
(MDMOM) 4. Ensure access to the Maryland Family Planning Program. 5. Ensure access to Maternal, Infant, and Early
Childhood Home Visiting. 6. Provide accessible patient centered family planning services through the Maryland Family
Planning Program.
Created on 8/11/2022 at 8:37 PM
Page 59 of 296 pages

Women/Maternal Health - Annual Report
Maryland’s priority need for the women’s/maternal health domain is “to ensure that birthing people are in optimal
health before, during, and after pregnancy.” Maryland Title V provided preventive and primary care through direct,
enabling, and public health infrastructure services to a variety of women’s/maternal health needs in FY 2021.
Services and activities focus on the needs of women and birthing people across the Title V pyramid as outlined by
the State Action Plan. Within the maternal health priority area, there are three focus areas in maternal health:
Focus Area 1: Oral Health measured by the national performance measure (NPM 13.1) of percent of women
who had a preventive dental visit during pregnancy.
Focus Area 2: Substance use prevention and linkages to care and measured with two performance
measures:
1) NPM 14.1, percent of women who smoke during pregnancy
2) the state performance measure (SPM 1) of Overdose Mortality Rate for women, ages 15-49.
Focus Area 3: Reduce rates and eliminate disparities in maternal mortality and morbidity with the state
performance measure of reducing severe maternal morbidity rates that aligns with the Statewide Integrated
Health Improvement Strategy
Focus Area 1: Oral Health:
NPM 13.1: Percent of women who had a dental visit during pregnancy. In Maryland in 2020, 62.1% of mothers had a
cleaning during pregnancy, compared with 63.4% in 2019 (PRAMS). The percentage of mothers receiving oral
health care during pregnancy increased among non-Hispanic Black mothers, from 48.8% to 56.4%. However, the
percentage of Non-Hispanic White mothers receiving oral health care during pregnancy decreased from 72.9% to
68.7%, as did Hispanic mothers (56.5% to 53.1%) and non-Hispanic Asian mothers (69.7% to 53.0%). Among
mothers with 13 or more years of education, 66.5% had their teeth cleaned during pregnancy in 2020, a slight
decline from 68.4% in 2019, while among mothers with 12 years of education or less, 47.8% had their teeth cleaned
during pregnancy in 2020, a slight decline from 48.2% in 2019. From 2019 to 2020, the percentage of mothers who
received a teeth cleaning during pregnancy increased among mothers ages 30 to 34 years (64.7% to 66.1%),
decreased among mothers under 20 years (70.0% to 61.1%), 20 to 24 years (56.4% to 48.8%), and 25 to 29 years
(61.4% to 58.5%), and remained the same among mothers 35 years and older at 66.7 percent.
Key partners that work toward improving oral health include the Office of Oral Health (OOH), local health
departments, and local dental clinics. Planning with the OOH and working with local health departments to refer
clients to oral health offices highlight some of the work to improve oral health in FY2021.
During FY2021, the OOH updated the “Oral Health Care During Pregnancy: Practice Guidance for Maryland’s
Prenatal and Dental Providers.” The practice guidelines emphasize that pregnant individuals should make a dental
appointment early in pregnancy. In addition, the guidelines share myths versus facts and emphasize important
information such as maternal oral health affects future child health. The guidelines also provide information on the
oral conditions during pregnancy such as dental caries, pregnancy gingivitis, periodontitis, pyogenic granuloma, and
tooth erosions. The guide will be shared in FY2022 with community-based organizations, primary care providers,
and local health departments.
In FY2021, Title V funds also supported programming to pregnant people at local health departments throughout the
state. A total of 1,251 pregnant people were referred to dental care by local health departments in FY 2021. The
Created on 8/11/2022 at 8:37 PM
Page 60 of 296 pages

number of pregnant people linked with dental care in FY 2021 is an increase from FY2020, when only 627 pregnant
people were referred. However, it is lower than pre-pandemic levels. In FY 2019, 2,300 were referred to oral care.
Focus Area 2: Substance Use Prevention and Linkages to Care: This focus area has two performance
measures: 1) NPM 14.1, percent of women who smoke during pregnancy and 2) the state performance measure
(SPM 1) of Overdose Mortality Rate for women, ages 15-49
Performance Measure 1: NPM 14.1: Smoking during pregnancy: In 2020, Maryland was slightly below the national
average for women who smoked during pregnancy, with 4.2% of Maryland women who smoked during pregnancy,
compared to 5.5% nationally (National Vital Statistics System). Maryland has seen a downward trend in the
percentage of women who smoke during pregnancy since 2010 (8.9%), while the national trend reached its peak in
2014 (7.9%) and has started decreasing since 2015. The percentage of Maryland women who smoked during
pregnancy in 2019 was highest among non-Hispanic White women (7.4%), followed by non-Hispanic Black women
(4.2%), and Hispanic women (0.8%).
During Fiscal Year 2021, Title V continued the partnership with MDH’s Center for Tobacco Control and Prevention,
which provides enhanced counseling services that motivate pregnant women to quit smoking. Counseling
interventions provide motivation to quit and support to increase problem solving skills. Counseling interventions may
include motivational interviewing, cognitive behavior therapy (CBT), other psychotherapies, problem-solving and
other approaches. Pregnant people are more likely to quit when cessation counseling is combined with motivational
interviewing and is provided by a trained educator.
The QuitLine, which is funded by MDH’s Center for Tobacco Control and Prevention is a free service to all Maryland
residents age 13 and older. The program for pregnant people consists of one initial and nine proactive follow-up
coaching calls. Participants may call in for additional support at any time. The timing of proactive calls is relapse-
sensitive, and the focus of the follow-up coaching calls is relapse prevention. Medication use is monitored to assure
use compliance, assess and problem-solve potential side effects. The Quit Coach assesses the participant’s status
and progress, builds upon information previously gathered, identifies barriers, and reinforces successes. Coaches
have degrees in counseling or addiction treatment.
In FY2020, there were 82 enrollments, and in FY2021, 67 enrollments. For FY2020, where there is the latest
available detailed data, average engagement calls length were 2.3 calls. Text2Quit users average six texts.
Title V funds local health departments to routinely screen women for tobacco use and offer referrals to the State’s
QuitLine. Staff who screened were from home visiting, home birth certification, early intervention, and family planning
clinics. In FY 2021, only 68 individuals were referred to tobacco cessation programs, including the QuitLine. This is
a dramatic decrease from FY2020, when a total of 892 prenatal/postpartum people were referred to tobacco
cessation programs, including the Quitline above. Due to COVID, many local health departments were unable to
provide services.
Performance Measure 2: Overdose Mortality Rate for women of reproductive age. (SPM 1)
While overdose mortality rate for women of reproductive age was not a state performance measure during 2016-
2020, efforts to prevent overdose deaths are added below to reflect the urgent need to address overdose deaths.
The rate of overdose deaths for women ages 15-49 was 24.1 per 100,000 population in 2019 according to the
Maryland Vital Statistics Administration. Unintentional overdose was the leading cause of pregnancy associated
Created on 8/11/2022 at 8:37 PM
Page 61 of 296 pages
deaths in Maryland at 32 percent in 2018 (the most recent year data is available from the Maryland Maternal Mortality
Review). According to the Maryland Behavioral Health Administration, it is estimated that only 21 percent of pregnant
people with opioid use disorder received opioid maintenance treatment in 2019, a substantial decrease from 75
percent reported in 2018. This decrease can be explained by multiple factors: Maryland bases this metric on
Administrative Services Organization (ASO)-Optum claims data and starting on January 1, 2020, the question, “Are
you currently pregnant?” is no longer a mandatory part of the registration process. Additionally, providers have the
option to opt out of asking and providing a response to this question. According to Maryland BHA, preliminary data
shows that about 80 percent of providers are opting to not answer additional reporting questions. Finally, due to the
MDH Network Security incident, there is a delay in data reporting. It is likely that the 21 percent of pregnant people
who received maintenance treatment is an underestimate.
Incident characteristics of overdose deaths can be found in the annual Maternal Mortality Review Report, with the
latest available report from 2020, which contains data from 2018. In Maryland, from 2010-2018, there were 91
overdose-related pregnancy associated deaths in Maryland, with 75% (n=69) White Non-Hispanic, 20% (n=18)
Black non-Hispanic, 3 as other non-Hispanic. On average these overdose deaths occurred 198 days postpartum.
Fourteen percent (n=13) had not initiated prenatal care.
The State has developed the Opioid Operational Command Center (OOCC) to coordinate activities to prevent
overdose deaths. The OOCC developed an overdose dashboard in 2021 and can be found here:
https://experience.arcgis.com/experience/c546d22ec4a946cbb700a282f53c6eb7/
Strategies to decrease overdose fatalities due to unintentional opioid use
Identification and linkages to treatment with the Maryland Medicaid Maternal Opioid Misuse Model
With over 21,000 individuals of childbearing age diagnosed with Opioid Use Disorder in Maryland, substance use is
a leading cause of maternal death and has a significant impact on the approximately 1,500 infants born to Medicaid
beneficiaries with OUD in Maryland per year. State Medicaid launched its Maternal Opioid Misuse (MOM) model in
January 2020, with funding from the Center for Medicare and Medicaid Innovation (CMMI) and in collaboration with
the Centers for Medicare and Medicaid Services (CMS). The model is a five-year, multi-pronged approach to
combating the nation’s opioid crisis by addressing fragmentation in the care of pregnant and postpartum Medicaid
beneficiaries with opioid use disorder (OUD).
The MOM model focuses on improving clinical resources and enhancing care coordination to Medicaid beneficiaries
with OUD during and after their pregnancies through the special need’s coordinators in the Managed Care
Organization. Due to COVID, the launch of the model was delayed to July 2021, and the focus was moved to one
pilot jurisdiction, St. Mary’s County. The smaller service area enabled a greater focus to be placed on model
services, referral pathways, and data collection, in addition to refinement of processes as designed.
As part of the MOMS Model, the Department, through Maryland Medicaid, partnered with University of Maryland and
the Maryland Addiction Consultation Services (MACS) to provide trainings to providers. These training encourage
the use of buprenorphine for those with opioid use disorder and enrolled 198 practitioners in MACS for MOMs
during FY 2021. In addition, there were 44 perinatal calls received through the MACS warmline and they also hosted
two webinars with a total of 160 attendees. MACs also launched the MOMS TeleECHO clinic that is held monthly.
Title V Program has been partnering with the Medicaid Maternal Opioid Misuse Model team to expand referrals to
the Local Health Departments and Managed Care Organizations through the Prenatal Risk Assessments (PRA).
Created on 8/11/2022 at 8:37 PM
Page 62 of 296 pages

Under COMAR 10.09.68.05 the PRA should be completed for Medicaid participants at the first prenatal care visit.
Specifically, the Title V Program has emphasized the importance of the PRA during the local health department
technical assistance calls. During SFY2021, a pilot to integrate the PRA into an electronic format was conducted in
the Baltimore metro region. A couple of clinics were selected to develop the PRA into an electronic format and
integrate it into the Electronic Medical Record System.
Screening, Brief Intervention, and Referral to Treatment with the Maryland Family Planning Program
Given the importance to identify substance misuse and the need to link to treatment, the Maryland Family Planning
Program (MFPP) has implemented a program-wide training to implement SBIRT (Screening, Brief Intervention,
Referral, and Treatment) in FY 2021 among all MFPP subrecipient sites. Maryland Family Planning Program has 62
sites across the State and sees approximately 40,000 to 50,000 individuals a year
After providing time for implementation, particularly during the COVID-19 pandemic, MFPP will collect data on
screening and referral to treatment in FY23 and implement a continuous quality improvement plan. Pending the
availability of funds, MFPP also intends to provide additional funding to sites to strengthen relationships with
substance use disorder treatment centers.
Babies Born Healthy Initiative
During FY 2021, eight sites across seven local jurisdictions implemented state funded Babies Born Healthy (BBH)
programs, which directed resources to engage women and communities in an effort to provide supportive
coordinated care and address disparities in infant mortality rates in Maryland. A total of 1,389 women had accessed
BBH services, and there was a total of 311 births among program participants and 8 fetal/neonatal deaths. The sites
also provide linkages to care to further treatment for those who are experiencing opioid misuse or opioid use
disorder.
Focus Area 3: Reduce rates and eliminate disparities in maternal mortality and morbidity
This focus area is tied to the new State Performance Measure (SPM 2) that aims to reduce Black NH to White NH
severe maternal morbidity gaps. In addition, this focus area is linked to the national outcome measure (NOM 2) of
Severe Maternal Morbidity and NOM 3 of Maternal Mortality. In FY 2021, Centers for Medicare and Medicaid
Innovation (CMMI) approved the State’s proposal to focus on Severe Maternal Morbidity and asthma as part of the
Statewide Integrated Health Improvement Strategy and the State’s healthcare finance model with the Total Cost of
Care.
In 2021, the State’s Severe Maternal Morbidity (SMM) rate was 287.0 events per 10,000 delivery hospitalizations
(Health Services Cost Review Commission). SMM rates were highest among non-Hispanic Black women (381.4 per
10,000) and women ages 40 and over (428.4 per 10,000). The rate is an increase from the SIHIS baseline of 2018
and 2019.
Further analysis was conducted by the MCH Epi team. Using the data source of the Health Services Cost Review
Commissions inpatient hospitalizations, the MCH epi team reviewed trends in Severe Maternal Morbidity (SMM)
and COVID-19 diagnosis for Maryland live births from January 1, 2019, through June 30, 2021. The Alliance for
Innovation on Maternal Health (AIM) ICD-10 codes for SMM were used to determine SMM events and the ICD-10
code U07.1 was used to determine a COVID-19 diagnosis during the birth hospitalizations.
Results of the analysis indicated that COVID-19 diagnoses contributed to the rising rates of SMM in Maryland
Created on 8/11/2022 at 8:37 PM
Page 63 of 296 pages

birthing people, especially among the Hispanic population. Overall, there was an increase in SMM rate in Maryland
by 30%, from 226.0 SMM diagnoses per 10,000 delivery hospitalizations in the Q1 period of 2019, to 292.5 per
10,000 in the Q2 period of 2021. When analyzing the increase in SMM rate by race and ethnicity, the largest
increase was seen among Hispanic birthing people, at 52% (from 227.4 per 10,000 in 2019-Q1 to 346.3 per 10,000
in 2021-Q2). SMM rates were analyzed both including and excluding a COVID-19 diagnosis, to try to determine the
effect that a COVID-19 diagnosis had on SMM rates. When the SMM events that included a COVID-19 diagnosis
were removed from the data, the SMM rate increased only 20% from 2019-Q1 to 2021-Q2. Additionally, there was a
large disparity between the COVID-19 positive SMM diagnoses and the COVID-19 negative SMM diagnoses
among Hispanic birthing people in 2020-Q2. The rate of SMM diagnoses that included a COVID-19 diagnosis was
56% higher than the rate of SMM diagnoses without a
COVID-19 diagnosis during that time period. The rates of the individual conditions that contribute to SMM were
compared between three different scenarios: 2019, before the COVID-19 pandemic; 2020-2021 SMM cases
excluding a COVID-19 diagnosis, and 2020-2021 SMM cases including a COVID-19 diagnosis. The rate of SMM
COVID-19 positive cases with blood products transfusions was 204.5 per 10,000 delivery hospitalizations, 3%
higher than the rate of SMM COVID-19 negative cases, and 11% higher than 2019 SMM cases. Similar disparities
were seen amongst most of the SMM contributing conditions, but it is also especially noticeable among cases
requiring ventilation, where the rate among COVID-19 positive SMM cases was 43% higher than among COVID-19
negative SMM cases. Low numbers prohibit calculating rates for many of the individual conditions by race and
ethnicity, however, a similar disparity in rates of SMM cases requiring blood products transfusions was seen among
Hispanic birthing people. The rate of COVID-19 positive SMM cases requiring blood products transfusion was 8%
higher than that of COVID-19 negative SMM cases, and 20% higher than 2019 SMM cases. Results of the analysis
concluded that COVID-19 has contributed to the increase in the SMM events. These results indicate that COVID-19
diagnoses contributed to the rising rates of SMM in Maryland birthing people, especially among the Hispanic
population.
While the results were analyzed in FY2021 and 2022, the Title V team used this information in FY2022 to provide
further information and work with local health departments on their efforts to increase information on COVID
vaccinations. This included developing a printable and electronic version of a brochure of why vaccination for
pregnant and breastfeeding people were important. This brochure was translated into several languages including
Spanish, French, Tagalog, Chinese, Russian, and Korean.
Strategies to reduce rates and eliminate disparities in maternal mortality and morbidity
Overall, there is a statewide Maternal Health Improvement Program Strategic and Action plan through the
Maternal Health Improvement Task Force that focuses on reducing disparities in maternal mortality and morbidity.
Please see the Strategic and Action plan here. Please see below for further information on Title V contributions to
improve maternal health in the state as well as more information on the Maryland Maternal Health Innovation
Program.
Maternal Mortality Review Program
The Maternal Mortality Review Program reviews all pregnancy-associated (PA) deaths (deaths during or within one
year after pregnancy from any cause). While the report for cases reviewed in FY2021 are still being finalized due to
delays related to COVID-19 and the Department’s network security incident, preliminary data for 2019 demonstrate
that the leading cause of pregnancy-associated deaths are from unintentional overdoses, like that of previous years.
In addition, fentanyl or fentanyl analogs have been the most frequently detected opioid.
Based on the most recent public data, which is the 2020 report that contains data from 2018, there were 38
pregnancy-associated deaths, resulting in a pregnancy-associated mortality rate of 53.5 deaths per 100,000 live
births. Of the 38 pregnancy-associated deaths, 18 were determined to be pregnancy-related, for a pregnancy-
Created on 8/11/2022 at 8:37 PM
Page 64 of 296 pages

related mortality rate of 25.3 deaths per 100,000 live births. Among the 18 pregnancy-related deaths in 2018, the
leading causes of death were non-cardiovascular conditions, cardiovascular conditions, and suicide, each
accounting for three deaths. Homicide, amniotic fluid embolism, and thrombotic pulmonary embolism each
accounted for two deaths. The remaining pregnancy-related deaths were single cases of substance use with
unintentional overdose, infection, and pregnancy-induced hypertension.
Of the 18 pregnancy-related deaths occurring in 2018, six cases (33 percent) involved non-Hispanic White women,
ten cases (56 percent) involved non-Hispanic Black women, and two cases (11 percent) involved Asian/Pacific
Islander women. Among the 20 non-pregnancy-related deaths, 11 cases (55 percent) involved non-Hispanic White
women, seven cases (35 percent) involved non-Hispanic Black women, one case involved a Hispanic woman, and
one case involved a non-Hispanic woman whose race was identified as other. The rate of pregnancy-related deaths
in non-Hispanic Black women was 2.2 times higher than that of non-Hispanic White women.
Further information of the Maternal Mortality Review Report can be found on the Maternal and Child Health Bureau
webpage here: https://health.maryland.gov/phpa/mch/pages/mmr.aspx .
The Maryland Maternal Mortality Review Program has focused increased attention on disparities in pregnancy-
related deaths. In 2018, the Maryland General Assembly enacted legislation to establish a Maternal Mortality
Stakeholder Group composed of the Maryland Office of Minority Health and Health Disparities, the Maryland Patient
Safety Center, the Maryland Healthy Start Program, women’s health advocacy groups, community organizations,
local health departments, health care providers serving minority women, and families that have experienced a
maternal death. This Stakeholder Group is tasked with reviewing the findings and recommendations in the annual
Maternal Mortality Review Report, examining issues resulting in disparities, and identifying new recommendations
with a focus on disparities in maternal deaths.
In 2021, the Stakeholder group reviewed the results of the 2020 report including that among women initiating
prenatal care during the first trimester, the pregnancy-related mortality rate was over three times higher in non-
Hispanic Black women compared to non-Hispanic White women. Early initiation of prenatal care did not eliminate
the racial disparity in pregnancy-related deaths. The pregnancy-related mortality rate increased by 270% with late or
no prenatal care for non-Hispanic White women, and 52% for non-Hispanic Black women. The Stakeholder group
discussed and recommended the need to focus on upstream factors such as preconception health, implicit bias and
congruent care training for perinatal providers, and warm handoffs between providers and improving
communications between healthcare providers. They also discussed the need for increased surveillance of pregnant
and postpartum individuals with hypertension or other cardiovascular risks, and the need for coordinated care with
perinatology and cardiology specialists.
Sexual and Reproductive Health through Maryland Family Planning:
The mission of the Maryland Family Planning Program (MFPP) is to reduce unintended pregnancies and to improve
pregnancy outcomes by ensuring access to quality, comprehensive family planning services for those individuals with
incomes below 250% Federal Poverty Level (FPL). Services include: a broad range of family planning methods,
breast and cervical cancer screening, prevention and treatment of sexually transmitted infections, HIV testing and
prevention education, infertility and preconception services, and health education/counseling and referrals to
community resources. There are 62 family planning sites. State Match Title V dollars were used to support the
Maryland Family Planning program in FY2021. In May 2019, Maryland became the first state to formally withdraw
from Title X federal funding for family planning services in the setting of new restrictions. Therefore, Title V partnered
with the Maryland Family Planning Program to continue essential service delivery.
In Fiscal Year 2021, there were a total of 49,440 clients and 67,425 visits. Overall, there was an 18% decrease in the
Created on 8/11/2022 at 8:37 PM
Page 65 of 296 pages

number of clients, and a 21% decrease in visits compared to FY 2020. Of the unduplicated clients seen this
reporting period, 32,559 were new clients and 16,881 were continuing clients. This was a slight decrease from
FY2020 with 38,428 new clients (↓ 15.3%) and 21,799 continuing clients (↓ 22.6%). The decrease is thought to be
due to COVID.
In FY21, MFPP served 5,991 people who were less than 20 years old. Nearly seventy percent of the clients seen at
Maryland Family Planning clinics were at 100% or below the poverty line.
The racial and ethnic breakdown for clients served by the Maryland Family Planning Program include: 40.6% Black,
34.3% White, 2.3% Asian, American Indian, 0.2%, 16.7% Hispanic origin.
During FY 2020 and 2021, many of the MFPP clinics had to adapt their services for COVID-19. Specifically, they
embraced telehealth/telemedicine as well as new administrative guidelines. Family Planning providers linked clients
to community partners, when necessary, proactively called scheduled patients to best assess their needs, and even
provided birth control by mail.
Babies Born Healthy Initiative
During FY 2021, eight sites across seven local jurisdictions implemented state funded Babies Born Healthy (BBH)
programs, which directed resources to engage women and communities in an effort to provide supportive
coordinated care and address disparities in infant mortality rates in Maryland. A total of 1,389 women had accessed
BBH services, and there was a total of 311 births among program participants and 8 fetal/neonatal deaths. These
jurisdictions were selected to receive funding after the Perinatal Periods of Risk Assessment (PPOR) was
conducted and concluded that these jurisdictions were key to effectively curbing disparities and rates of infant
mortality. Services provided were focused on the promotion of prenatal care, reduction of substance use, tobacco
cessation, long-acting reversible contraception, accessing health insurance, and other strategies driven by site-
specific data to promote healthy maternal and infant outcomes. Specific activities included home visiting strategies,
nurse and paraprofessional case management services for high-risk women and infants, family planning services,
screening and referrals for mental health and substance use.
During FY2021, COVID-19 continued to present barriers to both families and staff. Many staff are public health
nurses in LHDs, as such they were pulled into Maryland’s COVID-19 response which left BBH sites with very limited
capacity at times. Families faced numerous challenges including job loss and eviction, difficulty in accessing food,
loss of childcare, lack of transportation, intimate partner violence, technology limitations, issues in accessing
necessary baby supplies, and others. Many BBH sites responded by doing emergency supply drop-offs to their
participants and were a crucial lifeline at the height of the pandemic.
State Maternal Health Innovation Program
In September 2019, the Health Resources Service Administration awarded Johns Hopkins University (JHU)
$2,134,389 as part of a nationwide State Maternal Health Innovation Program. The Hopkins-led initiative, MDMOM,
is a 5-year project to assist in addressing disparities in maternal health and improving maternal health outcomes,
with a particular emphasis on preventing and reducing maternal mortality and severe maternal morbidity (SMM). For
the program areas, JHU has partnered with several other organizations, and specifically to coordinate the Maternal
Health Improvement Task Force, JHU has partnered with the Department. Title V staff members support the Task
Force and their activities.
The Task Force and Title V staff spent the entirety of FY 2021 developing a Maternal Health Improvement Strategic
Plan. The Maternal Health Strategic Plan process was structured into six stages: 1) scan of existing needs
assessments and plans including the Title V State Action plan, Maternal Mortality Review Committee and
Created on 8/11/2022 at 8:37 PM
Page 66 of 296 pages

Stakeholder Group recommendations, as well as strategic plans from other states; 2) identification of state-level
strengths and challenges; 3) identification of key priorities, goals, and desired outcomes based on identified
strengths and challenges; 4) stakeholder and public input; 5) strategic plan revisions based on feedback; and 6)
report finalization. Members of the Maternal Health Improvement Task Force with support from Title V staff led the
development of the Maternal Health Strategic Plan. Overall, approximately 15 stakeholder input sessions were held.
Many of these input sessions occurred through existing stakeholder meetings. The Strategic Plan, which was
submitted to HRSA in September 2021, has five focus areas to improve maternal health, particularly in BIPOC
populations:
1. Promote Equity and Mobilize Against Racism in Maternal Health
2. Achieve Health (Preconception, Prenatal and Birth, Post Partum, and Interconception Periods) Using
the Life Course Model to Support Maryland Birthing People Through Advocacy and Implementation of
Effective Policies.
3. Develop Strategies that Acknowledge the Influence of the Social Determinants of Health and Historical
Racism to Improve Resiliency for Birthing People, Families, and Communities and to Promote an Optimal
Quality of Life.
4. Improve Access and Utilization of Data and Improve Surveillance of Data on Structural Racism and its
Impact to Make Informed Decisions.
5. Develop a Maternal Health Provider Workforce that will be Available, Accessible, and that Offers
Services Based on the Principles of Cultural Humility, Equity, and Racial Justice.
In addition, as part of the strategic plan, the mission and vision of the Task Force was clarified. These sessions were
led by Title V staff. The mission of the Task Force is to identify and support effective policies and initiatives that
optimize current delivery systems in order to: meet the needs of communities that have been silenced as a result of
structural racism; improve the quality of the full spectrum of reproductive, perinatal, and postpartum care; and
strengthen service delivery systems for the medically- underserved. The vision of the Task Force is for all people in
Maryland who give birth are in optimal health and thriving.
The Values and Guiding Principles of the Strategic plan include:
• Promote policies and practices that support racial equity and community inclusivity;
• Acknowledge that cumulative and intergenerational stress impacts health;
• Apply a strengths-based approach for all programs, policies, and procedures;
• Partner with community members who have lived experience through community-based and faith-based
organizations;
• Ensure that programs, policies, and practices are data-driven and are evidence-informed;
• Honor and respect that families are formed with unique and diverse characteristics and a multi- generational, whole
family, modernistic approach is required.
Title V staff drafted a charter to provide clarity in the Task Force’s role and to provide foundational agreements,
particularly since there was confusion on the MDMOMs program and the role of the Task Force. The purpose of the
Task Force is to develop and implement a statewide maternal health improvement strategic plan that incorporates
activities outlined in the state’s most recent Title V Maternal and Child Health Services Needs Assessments. The
charter included operating procedures including that the Task Force would meet quarterly. Group agreements were
included in the Charger that included: Be Present, Call Each Other In as We Call Each Other Out, Recognize the
Difference of Intent versus Impact, Create Space for Multiple Truths, Notice Power Dynamics, and Center Learning
and Growth. A draft of the charter was presented to the Task Force during the July 2021 meeting and was finalized at
the end of FY21.
Created on 8/11/2022 at 8:37 PM
Page 67 of 296 pages

In addition, the election process to elect co-chairs of the Task Force started in order to emphasize and practice
inclusion. Previously, the Title V manager has been serving as Chair of the Task Force with support from the Director
of the Bureau of Maternal and Child Health and the Deputy Director. However, Title V led the process to have the
Task Force be led by co-chairs, who would strategically plan for agenda items and facilitate the activities and
conversations moving forward.
Maryland Perinatal Quality Collaborative
Maryland’s Perinatal Quality Collaborative (MDPQC) is a network of perinatal care providers and public health
professionals working to improve health outcomes for women and newborns through continuous quality
improvement. The Collaborative provides participating birthing hospitals with educational resources, technical
assistance and a platform for communication and sharing of best practices.
During Fiscal Year 2021, two new initiatives were started based on guidance from a Steering Committee that
included physicians, nurses, and nurse midwives from hospitals across the state, as well as public health
stakeholders. The first initiative focuses on improving management of maternal hypertension through implementation
of the Alliance for Innovation on Maternal Health (AIM) Patient Safety Bundle. All 32 delivery hospitals in Maryland
participate in this collaborative. The second quality initiative focuses on antibiotic stewardship in the Neonatal
Intensive Care Unit (NICU). 25 delivery hospitals in Maryland are enrolled in this collaborative.
Created on 8/11/2022 at 8:37 PM
Page 68 of 296 pages

Women/Maternal Health - Application Year
Maryland Title V identifies the priority for women’s maternal health as ensuring that birthing people are in optimal
health before, during, and after pregnancy.
To this end, in FY 2023, Title V will employ the following strategies to improve maternal health outcomes statewide.
Please note that for FY2023, Maryland Title V shifted from Oral Health to a broader focus of well women’s health.
Focus Area 1: Oral health: To increase the number of pregnant people receiving preventive dental visits from a
baseline of 28% (2019) to over 36% by 2025 (Healthy People 2030 Target: 45%)
During Fiscal Year (FY23), the Office of Oral Health (OOH) will leverage its established partnership with the Maryland
section of the American Congress of Obstetricians and
Gynecologists (ACOG) to disseminate Oral Health During Pregnancy: Practice Guidance for Maryland’s Prenatal
and Dental Providers through local health departments and other providers. The practice guidance contains
essential information on oral health during pregnancy, including background on oral conditions during pregnancy,
myths and facts about the safety of oral health care for pregnant women, pharmacological considerations for dental
care for pregnant women, and detailed practice guidance for prenatal providers. The document also includes a
variety of associated resources for use in practices and for patients. In addition, the OOH will also provide detailed
information on how to apply the document’s guidance in their practices. The Office of Oral Health team will conduct
outreach to providers to assist them in establishing local referral networks for their pregnant patients, with the goal of
increasing access to oral health care for this population.
Maternal and Child Health Care Coordination at the Local Health Department will continue linking pregnant people
who are referred through the Maryland Prenatal Risk Assessment to Oral Health providers as part of their care
coordination.
In the future, Maryland Title V will propose transitioning from the National Performance Measure of oral health to a
broader national performance measure: Women’s health by the national performance measure (NPM 1) of percent
of women who had a preventive dental visit during pregnancy. Feedback was obtained on this transition, and overall,
the feedback thought that this national performance measure aligned with work that was already occurring, including
work at the local health departments.
Potential Future Objective 1: To increase the number of well-women visits from a baseline of 73% (2020; BRFSS) to
over 78% by 2025.
If the broader national performance measure is approved, the Title V team will continue to work on increasing the
number of well-women visits through partnership. The Title V team and the Maryland Family Planning Program
(MFPP) will expand telehealth services in family planning and preventive care services. Maryland Family Planning
Services will not only provide family planning services, but also navigate social needs identified through the visits,
and link to other primary care providers. For the telehealth expansion, the MFPP will work with 11 local health
departments including Baltimore City, Calvert, Carroll, Dorchester, Garrett, Harford, Howard, Prince George’s,
Somerset, St. Mary’s, and Worcester and three non-profit organizations. These efforts promote the goal to increase
well women visits as these visits provide preventive care and provide further coordination and referrals to
comprehensive primary care visits. During FY2023, the team will begin by assessing existing telehealth resources in
local health department family planning sites, identifying needs, barriers and opportunities to enhance services. The
collected data will be used to plan and implement a virtual telehealth training and technical assistance program for
Created on 8/11/2022 at 8:37 PM
Page 69 of 296 pages

participating sites. After the training and technical assistance program, MDH will disseminate a comprehensive
telehealth toolkit to the 62 MFPP sites, 24 local health departments and all family planning service sites in Maryland.
During the Maryland General Assembly 2021 Legislative Session, Senate Bill 923 was passed that required
Medicaid to extend coverage for eligible pregnant individuals with family incomes up to 250% of the federal poverty
level (FPL) for one year immediately following the end of the birthing individual’s pregnancy. This coverage would
include dental care as well as comprehensive medical care. The extended coverage became effective starting April
1, 2022. Title V staff will continue to work with Maryland families to inform them about the extension of the coverage
during provision of services such as care coordination and home visiting.
In addition, for FY2023, Title V staff will focus on increasing linkages to care, specifically through expanding the
Postpartum Infant Maternal Referral Form (PIMR). During FY21 and 22, Title V staff released a PIMR best practices
form that reviewed the process of the PIMR. The best practices document explained the purpose of the form,
including referring mothers and infants who need additional support and information on community-based services at
the local health departments. During the next year, Title V staff will focus on understanding workflows from the local
health departments as well as expand the electronic PIMR through the Regional Information Health Exchange,
CRISP.
Care Coordination
Title V staff will continue to improve the quality and expand care coordination at the Local Health Departments to link
pregnant and postpartum people to navigate their social needs and to navigate primary care. In FY2022, Title V
allowed funding for Local Health Departments, which is mandated by House Bill 314, Laws of 1995 that the Federal
Title V Maternal Child Health Block grant must go towards the local health department. Local Health Departments will
continue linking pregnant people who are referred through the Maryland Prenatal Risk Assessment and PIMR. Title V
has aligned care coordination through the Babies Born Healthy Program, an initiative focused on perinatal care
coordination.
Focus Area 2: Substance use prevention and linkages to care through 1) NPM 14.1, percent of women who smoke
during pregnancy and 2) the state performance measure (SPM 1) of Overdose Mortality Rate for women, ages 15-
49.
Objective 1 for Focus Area 2: To increase the number of women who abstain from smoking tobacco during
pregnancy from a baseline of 95.3% (2019) to 96.3% or more (Healthy People 2030).
Smoking During Pregnancy
Referrals to Maryland QuitLine
For Fiscal Year 2023, Title V will continue and strengthen the partnership with MDH’s Center for Tobacco Control and
Prevention. Specifically, Title V will work with local health departments for care coordination and connect individuals
who smoke tobacco to the QuitLine or local health department tobacco cessation programs. QuitLine Coaches use
cognitive behavioral coaching and practical skill-building to reinforce effective coping strategies, help the participant
manage stress, and build self-efficacy. The QuitLine is a free service to all Maryland residents age 13 and older.
Title V will also collaborate with the Center for Tobacco Control and Prevention to update a tobacco cessation toolkit
Created on 8/11/2022 at 8:37 PM
Page 70 of 296 pages

for OB/GYN providers.
In FY2023, the Maryland Family Planning Program will continue to focus on expanding SBIRT (Screening, Brief
Interventions, and Referrals to Treatment) throughout their 62 service sites across Maryland. In addition, the program
will focus on improving partnerships between substance use disorder clinics and family planning clinics particularly in
Western and Northern Maryland.
Objective 2 for Focus Area 2: To decrease the overdose mortality rate for women, ages 15-49 from 24.1 per
100,000 to 22.9 per 100,000 by 2025.
Improve Linkages to Care through Overdose Data to Action
Title V will continue to partner with Medicaid and the Overdose Data to Action (OD2A) funded under Centers for
Disease Control and Prevention to improve linkages to care, specifically implementing an electronic version of the
Prenatal Risk Assessment (ePRA). During FY2023, Title V will explore the feasibility of implementing an ePRA
statewide to increase the number of prenatal clinics referring clients to local health departments for care
coordination. This work will be informed by the lessons learned during the pilot projects in FY22. In addition, Title V
will partner with OD2A to implement an electronic version of the postpartum infant maternal referral form (PIMR), that
is used to link birthing people and infants to care coordination at local health departments, statewide. Title V will
partner with the State’s Health Information Exchange (HIE), called CRISP, to achieve this.
In addition, Title V and OD2A will conduct a Gap Analysis of resources available to pregnant people experiencing
Opioid Use Disorder (OUD), to better understand the landscape of OUD in the state, and areas in need of support.
This gap analysis will understand opioid use through PRAMS by analyzing the supplemental questions on opioid use
that will be used for further public health action as well as discussions with stakeholders. This gap analysis will serve
as a basis for future planning and collaborations with partners such as Maryland Behavioral Health Administration,
the Opioid Operational Command Center, Maryland Medicaid, Clinical Providers, Community-based organizations,
local health departments and more.
Title V will continue to partner with Maryland Medicaid on the Maternal Opioid Misuse Model. Title V staff will continue
to serve on the MOM model advisory council. The MOM model advisory council provides input into the model and
how to further expand the model in the State. In addition, the Advisory Council will provide input in the partnership
with the Maryland Addiction Consult Services.
Focus Area 3: Reduce rates and eliminate disparities in Maternal mortality and morbidity with the state
performance measure of reducing severe maternal morbidity rates that aligns with the Statewide Integrated Health
Improvement Strategy.
Objective 1 for Focus Area 3: By 2026, reduce the Severe Maternal Morbidity Rate from a baseline of 242.5 per
10,000 delivery hospitalizations to 197.1 per 10,000 delivery hospitalizations and decrease disparities between
Black to White SMM rates by at least 20% .
Statewide Integrated Health Improvement Strategy (Severe Maternal Morbidity)
Overall, Focus Area 3 is based on the Statewide Integrated Health Improvement Strategy goals. Through an
agreement with the Centers for Medicare and Medicaid Innovation (CMMI), the aim of SIHIS is to advance hospital
quality, care transformation across the health care system, and population health. The last goal, total population
Created on 8/11/2022 at 8:37 PM
Page 71 of 296 pages

health, has three domains: diabetes, opioids, and maternal and child health. The maternal and child health goal has
two specific outcomes of interest: severe maternal morbidity and childhood asthma. CMMI approved the State’s
strategy proposal on March 17, 2021.
Overall, as Title V staff will focus on 1) incorporating equity principles into practice either by partnering and working
with more community-based organizations 2) shifting committee structures to include people with lived experiences
3) looking for sustainable funding for essential supportive services by partnering with Medicaid.
Maternal Health Innovation Program
In Fiscal Year 2023, the Title V Program will continue to work with the Maternal Health Innovation Program, also
called “MDMOMs,” by Johns Hopkins University, by monitoring the maternal health improvement Strategic Plan.
During FY2022, Title V worked with the Task Force to elect co-chairs for the Task Force. Previously, the Title V
manager with support from the Bureau Director chaired the Task Force. Two co-chairs were elected, and Title V staff
worked with the Equity Advisor from the Bizell Group on a mechanism to compensate the co-chairs. Approval for
compensation required internal approval and as the Task Force is not in statute or in regulations, compensation for
the co-chairs was allowed. Often, compensation in committees or boards that are in statutes or regulation disallow
compensation.
For FY2023, the Title V program will continue to home in on recommendations and coordination’s of the Task Force,
based on the Maryland Maternal Health Improvement Strategic Plan. The Task Force focuses on five goals: 1)
promote equity and mobilize against racism in maternal health, 2) achieve maternal health (preconception, prenatal
and birth, postpartum and inter-partum periods) using the life course models to support Maryland mothers through
advocacy and implementation of policies, 3) improve resiliency for birthing people, families and communities that
acknowledge the importance of relationships and social determinants of health for an optimal quality of life, 4)
improve access to and utilization of data to make informed decisions, and 5) develop a maternal health workforce
that will be available, accessible, and culturally relevant and based on principles of racial equity and justice. With the
Equity Advisor, Title V will incorporate equity principles and provide recommendations on analysis and
contextualization of data to demonstrate the impact of racism, determinants of equity, and determinants of health.
Statewide Integrated Health Improvement Strategy Funds
As Maternal and Child Health was identified as the third domain within population health, the Health Service Cost
Review Commission approved an additional $40 million dollars over four years to meet the SIHIS Maternal and Child
Health goals. The majority (80%) of the funds goes towards Medicaid to increase linkages to care for birthing
people with opioid use disorder, reimburse for doula/birth worker support services, and expand group based
prenatal care and maternal and infant home visiting. These are services that provide additional support for the most
impacted populations and communities. Through partnership with Medicaid, these services can be more sustainable
beyond the SIHIS grant fund periods.
A portion of the MCH SIHIS funds went toward grant funds to allow expansion of promising practice programs. For
example, while Nurse Family Partnerships and Healthy Families America are the two evidence-based models
supported by Medicaid reimbursement, these models are prohibitive in jurisdictions where they have not already
implemented the model. The reason is due to start-up costs. For example, starting a Nurse Family Partnership Home
visiting program may cost more than $1 million dollars and maintaining fidelity to this model incurs high ongoing
costs. During FY2022, four home visiting sites in priority jurisdictions with elevated SMM events were selected after
an open bid procurement. During FY23, Title V will continue to implement the grant funds and continue the expansion
of their home visiting services. These organizations are: Montgomery County Health Department, the Family Tree,
Created on 8/11/2022 at 8:37 PM
Page 72 of 296 pages

Washington County Health Department, and Baltimore Healthy Start. In addition, in order to expand
CenteringPregnancy, a group-based prenatal care, Mercy Medical Center was selected as a site to implement the
CenteringPregnancy Model. During FY23, Title V will also put forward a competitive procurement to further expand
CenteringPregnancy in Maryland.
The remaining SIHIS funds will go towards public health services to expand asthma home visiting, promising practice
and evidence-based home visiting, as well as expanding group prenatal care for birthing people, regardless of
payor. During FY2022, the Title V program and Maternal and Child Health staff will be working to expand the
programs identified through SIHIS.
Maryland Perinatal Neonatal Quality Collaborative
The Maryland Perinatal Neonatal Quality Collaborative (MDPQC) is focused on addressing maternal hypertension
and neonatal antibiotic stewardship. For FY2023, the MDPQC will focus on sustained implementation of quality
improvement initiatives, which will include identifying barriers, assisting low performers, and continuing regular
check-in calls, learning events, and data reporting. An in-person learning event is scheduled for Summer 2022 to
provide updates and invite high performers to share best practices and lessons learned. The effectiveness of the
collaborative will also be assessed at the midpoint of each initiative, with the Steering Committee and participating
hospitals providing feedback, and a root-cause analysis will be conducted for any under-performing measures, as
needed. The MDPQC will continue to heavily focus on health disparities and will push out data-driven improvement
activities and resources to promote health equity.
Maternal Mortality Review Program
During Fiscal Year 2023, the Maternal Mortality Review Program will continue to conduct de-identified, confidential
case reviews for all pregnancy-associated deaths to identify clinical and non-clinical factors and systems issues
contributing to these deaths. There will be additional focus on streamlining medical records requests as there were
challenges in obtaining records during COVID-19 pandemic. More attention will be focused on understanding the
broader context of the cases and environments by reviewing the social determinants of health (e.g., poverty level of
the area, high food priority area), maternal and child health services (e.g., home visiting, WIC, administration care
coordination unit) in addition to the medical records. During Fiscal Year 2023, the administration of the MMR
Program will be overseen by the Maryland Patient Safety Center after a competitive bid process, allowing for the
expansion of the scope of work of the coordination activities.
Through the support from the Centers for Disease Control and Prevention Enhancing Reviews and Surveillance to
Eliminate Maternal Mortality (ERASE MM) program, Maryland plans to move towards a multi-disciplinary review
team in FY23 instead of a predominantly physician-led, medical review team to conduct comprehensive case
reviews in line with the national best practices. The Multi-disciplinary review team, called the Statewide Maternal
Mortality Review Team (MMRT) will identify and review pregnancy-associated deaths, identify factors that contribute
to these deaths, and propose recommendations that aim to prevent future deaths. The overall mission of the
Program is to review the issues surrounding the pregnancy-associated deaths, to identify interventions, and to
promote change among individuals, health care systems, and communities in order to prevent maternal deaths,
reduce maternal morbidities and improve population health. Members of the MMRT will represent the diversity of
Maryland’s population and will consist of individuals with both clinical and non-clinical expertise as recommended by
national best practices. There will be approximately 20 members on the Review Team.
The member positions that will be included on the team include: individuals who work with pregnant or postpartum
individuals and have expertise in Clinical Social Work, Community Doula Work, Community Birth Work, provision of
behavioral health services, or social services such as housing or food insecurity; individuals with expertise in
Created on 8/11/2022 at 8:37 PM
Page 73 of 296 pages

Community Health Nursing/Maternal, Infant, and Early Childhood Health Home Visiting or Nursing Care for Pregnant
Individuals, Postpartum Individuals, or Families of Pregnant or Postpartum Individuals; Individuals with expertise in
quality improvement for pregnant or postpartum patients or pregnant or postpartum patient safety; Physicians with
expertise or specialization in Obstetrics and Gynecology; individual with expertise in Public Health Epidemiology;
physicians with expertise or specialization in Maternal Fetal Medicine; physicians with expertise or specialization in
Addiction Medicine, Family Medicine, Internal Medicine, Anesthesiology, Critical Care, Emergency Medicine,
Pediatrics, Adolescent Medicine, Preventive Medicine, or Cardiology, specifically Cardio-Obstetrics; advanced
Practice Clinician in Women’s Health (Certified Nurse Midwife or Women’s Health Nurse Practitioner),
representative from the Maternal Mortality Stakeholder Group, public health officials, State Medicaid, a
representative from the Office of the Chief Medical Examiner.
The Maternal Mortality Stakeholder Group will continue to review the findings and recommendations in the annual
Maternal Mortality Review Report, examining issues resulting in disparities, and identifying new recommendations
with a focus on disparities in maternal deaths. These findings will inform the Maternal Health Improvement Program
Task Force as the implementers of the Maryland Strategic Plan.
Maryland Family Planning Program
The Maryland Family Planning Program will continue to promote optimal health outcomes for men, women and
families through ensuring access to breast and cervical cancer screening, prevention and treatment of sexually
transmitted infections, HIV testing and prevention education, infertility and preconception services, health education
and counseling and referrals to community resources. This program provides access to affordable, broad range of
family planning methods to assist individuals with their reproductive life plan, which includes postponing, preventing,
achieving and the spacing of their pregnancies. In FY23, the Maryland Family Planning Program will focus on
expanding SBIRT (Screening, Brief Interventions, and Referrals to Treatment) throughout their 62 service sites
across Maryland. In addition, the program will focus on improving partnerships between substance use disorder
clinics and family planning clinics particularly in Western and Northern Maryland. In FY23, the Maryland Family
Planning Program remains committed to providing support to subrecipients as they continue their innovative
telehealth practices, as well as assist with strategic efforts to return to safe practices while clinics reopen post-Covid.
Created on 8/11/2022 at 8:37 PM
Page 74 of 296 pages

Perinatal/Infant Health
National Performance Measures
NPM 3 - Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care
Unit (NICU)
Indicators and Annual Objectives
Federally available Data (FAD) for this measure is not available/reportable.
State Provided Data
2019 2020 2021
Annual Objective 93.7
Annual Indicator 79.2 93.4 91.6
Numerator 954 891 854
Denominator 1,205 954 932
Data Source VSA VSA VSA
Data Source Year 2018 2019 2020
Provisional or Final ? Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 94.0 94.3 94.6 95.0
Created on 8/11/2022 at 8:37 PM
Page 75 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 3.1 - Percentage of Level III & IV Perinatal Referral Centers who received their re-designations based on the
2019 MD Perinatal System Standards
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 93.7
Annual Indicator 0 15.4 46.2
Numerator 0 2 6
Denominator 14 13 13
Data Source Program Data Program Data Program Data
Data Source Year 2019 2020 2021
Provisional or Final ? Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 62.0 85.0 100.0 100.0
Created on 8/11/2022 at 8:37 PM
Page 76 of 296 pages
NPM 4 - A) Percent of infants who are ever breastfed B) Percent of infants breastfed exclusively through 6 months
Indicators and Annual Objectives
NPM 4A - Percent of infants who are ever breastfed
Federally Available Data
Data Source: National Immunization Survey (NIS)
2019 2020 2021
Annual Objective 88.9
Annual Indicator 84.1 88.6 86.8
Numerator 51,263 55,833 59,613
Denominator 60,967 63,040 68,676
Data Source NIS NIS NIS
Data Source Year 2016 2017 2018
Annual Objectives
2022 2023 2024 2025
Annual Objective 89.2 89.5 89.8 90.1
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - National Immunization Survey (NIS) (4A)
National - National Immunization Survey (NIS) (4B)
Maryland - National Immunization Survey (NIS) (4A)
Maryland - National Immunization Survey (NIS) (4B)
Maryland - Objectives (4A)
Maryland - Objectives (4B)
Created on 8/11/2022 at 8:37 PM
Page 77 of 296 pages

NPM 4B - Percent of infants breastfed exclusively through 6 months
Federally Available Data
Data Source: National Immunization Survey (NIS)
2019 2020 2021
Annual Objective 30.8
Annual Indicator 28.0 29.4 26.6
Numerator 16,851 17,961 17,625
Denominator 60,103 61,137 66,307
Data Source NIS NIS NIS
Data Source Year 2016 2017 2018
Annual Objectives
2022 2023 2024 2025
Annual Objective 32.2 33.6 35.0 36.4
Created on 8/11/2022 at 8:37 PM
Page 78 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 4.1 - Number of birthing hospitals designated as breastfeeding friendly
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 10
Annual Indicator 10 10
Numerator
Denominator
Data Source MDH Breastfeeding Policy
Committe
MDH Breastfeeding Policy
Committee
Data Source Year FY 2020 FY2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 11.0 12.0 13.0 15.0
Created on 8/11/2022 at 8:37 PM
Page 79 of 296 pages

NPM 5 - A) Percent of infants placed to sleep on their backs B) Percent of infants placed to sleep on a separate
approved sleep surface C) Percent of infants placed to sleep without soft objects or loose bedding
Indicators and Annual Objectives
NPM 5A - Percent of infants placed to sleep on their backs
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2017 2018 2019 2020 2021
Annual Objective 79 75.8 77.3 78.8 80.3
Annual Indicator 74.6 78.2 78.2 81.6 78.5
Numerator 47,705 48,293 48,293 50,368 47,476
Denominator 63,975 61,753 61,753 61,754 60,460
Data Source PRAMS PRAMS PRAMS PRAMS PRAMS
Data Source Year 2015 2017 2017 2019 2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 81.8 83.3 84.8 85.3
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - Pregnancy Risk Assessment Monitoring System (PRAMS) (5A)
National - Pregnancy Risk Assessment Monitoring System (PRAMS) (5B)
National - Pregnancy Risk Assessment Monitoring System (PRAMS) (5C)
Maryland - Pregnancy Risk Assessment Monitoring System (PRAMS) (5A)
Maryland - Pregnancy Risk Assessment Monitoring System (PRAMS) (5B)
Maryland - Pregnancy Risk Assessment Monitoring System (PRAMS) (5C)
Maryland - Objectives (5A)
Maryland - Objectives (5B)
Maryland - Objectives (5C)
Created on 8/11/2022 at 8:37 PM
Page 80 of 296 pages

NPM 5B - Percent of infants placed to sleep on a separate approved sleep surface
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2018 2019 2020 2021
Annual Objective 70.5 71.9 33.3
Annual Indicator 29.0 29.0 32.9 34.5
Numerator 16,948 16,948 19,188 19,974
Denominator 58,441 58,441 58,412 57,908
Data Source PRAMS PRAMS PRAMS PRAMS
Data Source Year 2017 2017 2019 2020
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 70.5 71.9 33.3
Annual Indicator 69.1
Numerator 45,750
Denominator 66,226
Data Source PRAMS
Data Source Year 2015
Provisional or
Final ?
Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 33.7 34.1 34.5 34.9
Created on 8/11/2022 at 8:37 PM
Page 81 of 296 pages

NPM 5C - Percent of infants placed to sleep without soft objects or loose bedding
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2018 2019 2020 2021
Annual Objective 68.1 69.5 57.6
Annual Indicator 51.7 51.6 56.6 55.0
Numerator 30,441 30,441 32,851 31,754
Denominator 58,942 58,942 58,015 57,742
Data Source PRAMS PRAMS PRAMS PRAMS
Data Source Year 2017 2017 2019 2020
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 68.1 69.5 57.6
Annual Indicator 66.8
Numerator 44,268
Denominator 66,226
Data Source PRAMS
Data Source Year 2015
Provisional or
Final ?
Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 58.6 59.6 60.6 61.6
Created on 8/11/2022 at 8:37 PM
Page 82 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 5.1 - Percentage of infants less than 6 months who are placed on their backs to sleep
Measure Status: Inactive - Replaced
State Provided Data
2019 2020 2021
Annual Objective 80.3
Annual Indicator 78.2 81.6 80.3
Numerator 48,293 50,368 48,530
Denominator 61,753 61,754 60,415
Data Source PRAMS PRAMS PRAMS
Data Source Year 2017 2019 2020
Provisional or Final ? Final Final Final
ESM 5.2 - Number of home visiting or care coordination clients, providers, and other Title V program participants
that received infant safe sleep counseling and information
Measure Status: Active
Annual Objectives
2023 2024 2025
Annual Objective 6,900.0 7,000.0 7,100.0
Created on 8/11/2022 at 8:37 PM
Page 83 of 296 pages

State Action Plan Table
State Action Plan Table (Maryland) - Perinatal/Infant Health - Entry 1
Priority Need
Ensure that all babies are born healthy and prosper in their first year
NPM
NPM 3 - Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care Unit
(NICU)
Objectives
Increase the percentage of very low birth weight babies delivered at an appropriate level hospital from 93.4% to greater
than 95% by 2025.
Strategies
1. Continue with oversight of standardizing definitions for birthing hospitals levels of care through the Maryland Perinatal
Standards of Care and with site visits for Level I, II, III, and IV birthing hospitals. 2. Provide maternal fetal medicine support
and technical assistance through the Maryland Perinatal Support Program. 3. Continue to implement the maternal
hypertension bundle and the neonatal antibiotic stewardship through the Maryland Perinatal-Neonatal Quality
Collaborative. 4. Continue with The Maryland Health Innovation Program and Task Force to address maternal and
perinatal health through data, policy, quality initiatives, training and telemedicine. 5. Continue with Surveillance Quality
Initiatives such as Child Fatality Review and Fetal and Infant Mortality Review to identify systemic preventive factors.
NOMs
NOM 8 - Perinatal mortality rate per 1,000 live births plus fetal deaths
NOM 9.1 - Infant mortality rate per 1,000 live births
NOM 9.2 - Neonatal mortality rate per 1,000 live births
NOM 9.4 - Preterm-related mortality rate per 100,000 live births
ESMs Status
ESM 3.1 - Percentage of Level III & IV Perinatal Referral Centers who received their re-designations
based on the 2019 MD Perinatal System Standards
Active
Created on 8/11/2022 at 8:37 PM
Page 84 of 296 pages

State Action Plan Table (Maryland) - Perinatal/Infant Health - Entry 2
Priority Need
Ensure that all babies are born healthy and prosper in their first year
NPM
NPM 4 - A) Percent of infants who are ever breastfed B) Percent of infants breastfed exclusively through 6 months
Objectives
Increase the number of infants who are ever breastfed from a baseline of 88.6% to 90% by 2025
Strategies
1.Provide training for providers and encourage hospitals to adopt policies that are conducive to breastfeeding. 2. Provide
breastfeeding education through home visiting, care coordination, and Babies Born Healthy.
NOMs
NOM 9.1 - Infant mortality rate per 1,000 live births
NOM 9.3 - Post neonatal mortality rate per 1,000 live births
NOM 9.5 - Sudden Unexpected Infant Death (SUID) rate per 100,000 live births
ESMs Status
ESM 4.1 - Number of birthing hospitals designated as breastfeeding friendly Active
Created on 8/11/2022 at 8:37 PM
Page 85 of 296 pages

State Action Plan Table (Maryland) - Perinatal/Infant Health - Entry 3
Priority Need
Ensure that all babies are born healthy and prosper in their first year
NPM
NPM 5 - A) Percent of infants placed to sleep on their backs B) Percent of infants placed to sleep on a separate approved
sleep surface C) Percent of infants placed to sleep without soft objects or loose bedding
Objectives
Increase the number of babies who are placed on their back to sleep as reported by PRAMS from 81.6% to 88.9% by
2025.
Strategies
1. Assess the feasability of implementing a Safe Sleep Communication Plan developed from Morgan State University's
previous research, 2. Provide infant safe sleep eductation through Local Health Departments and Babies Born Healthy
Sites. 3. Continue to support the Surveillance and Quality Improvement Program to gather information from mothers who
had a fetal or infant loss through Fetal and Infant Mortality Review.
NOMs
NOM 9.1 - Infant mortality rate per 1,000 live births
NOM 9.3 - Post neonatal mortality rate per 1,000 live births
NOM 9.5 - Sudden Unexpected Infant Death (SUID) rate per 100,000 live births
ESMs Status
ESM 5.1 - Percentage of infants less than 6 months who are placed on their backs to sleep Inactive
ESM 5.2 - Number of home visiting or care coordination clients, providers, and other Title V program
participants that received infant safe sleep counseling and information
Active
Created on 8/11/2022 at 8:37 PM
Page 86 of 296 pages
Perinatal/Infant Health - Annual Report
Maryland Title V has three priorities for Perinatal Health:
1. Ensure that all babies are born healthy and prosper in their first year
2. Increase the number of infants that are ever breastfed
3. Reduce the number of sleep-related infant deaths statewide.
The Title V program conducted and supported activities to address national perinatal health performance measures
in 2021.
Priority 1: Ensure that all babies are born healthy and prosper in their first year
Infant Mortality: Infant mortality is a significant indicator of the overall health of a population. Infant mortality reflects
the broader community health status, poverty and other social determinants of health, and the availability and quality
of health services. In 2020, the Maryland infant mortality rate was 5.7 deaths per 1,000 live births, a decrease of
three percent from the 2019 rate of 5.9 deaths per 1,000 live births, and reflecting a six percent overall decrease
from the average rate of 6.6 deaths per 1,000 live births from 2011-2015. The non-Hispanic (NH) White infant
mortality rate decreased by 20 percent from 4.1 to 3.3 deaths per 1,000 live births and the Hispanic infant mortality
rate decreased by 10 percent, from 5.1 to 4.6 deaths per 1,000 live births The NH Black rate increased by six
percent from 9.3 to 9.9 deaths per 1,000 live births. The neonatal mortality rate (deaths under 28 days of age)
increased by five percent from 3.9 in 2019 to 4.2 in 2020, with the rate increasing by six percent among NH Black
infants, from 6.4 to 6.8, and increasing six percent from 3.3 to 3.5 among Hispanic neonates and decreasing 11
percent from 2.7 to 2.4 among NH white infants. The statewide post-neonatal mortality (deaths from 28 days through
11 months of age) rate decreased by 20 percent, from 2.0 in 2019 to 1.6 deaths per 1,000 live births in 2020. The
rate decreased 36 percent among NH White infants from 1.4 to 0.9 deaths per 1,000 live births and decreased 37
percent among Hispanic infants from 1.9 to 1.2 deaths per 1,000 live births. The post neonatal rate increased by
seven percent among non-Hispanic black infants from 2.9 to 3.1 deaths per 1,000 live births. The leading causes of
infant death in 2020 were disorders related to short gestation and low birth weight (LBW) account for 19 percent of
losses, congenital abnormalities (14 percent), sudden unexpected infant death (SUID) including Sudden Infant Death
Syndrome (SIDS) (12 percent), and maternal complications of pregnancy (12 percent).
Preliminary data show that there were 46 Sudden Unexpected Infant Deaths in 2020, with an annual rate of 67.1
deaths per 100,000 live births. Comparing two five-year periods over the last decade (2011-2015 and 2016-2020),
the overall infant mortality rate in Maryland has declined by six percent. The average rate for NH Black infants
decreased by eight percent and the average rate among Hispanic infants increased by two percent between these
two time periods. The post-neonatal mortality rate increased slightly among NH Black (six percent), NH White (nine
percent), and Hispanic infants (nine percent). The largest declines in infant mortality over the past ten years were
seen in the National Capital area, especially in Prince George’s County, which had a statistically significant
decrease of 14.5 percent, as well as in the Baltimore Metro Area, with Anne Arundel County seeing a 22.3 percent
decrease in infant mortality rates. The Eastern Shore Area also experienced an overall decrease of 8.3 percent with
Talbot, Caroline, and Worcester counties experiencing decreases of 44.7, 33.8, and 19.8 percent, respectively.
Rates of infant mortality increased in the Northwest, Southern, and Eastern Shore regions, with increases in
Dorchester (57.3 percent), Somerset (31.2 percent) Washington (25.9 percent), and Allegany (22.5 percent)
counties.
Fetal and Infant Mortality Review (FIMR): Title V funds support Fetal and Infant Mortality Review (FIMR) activities
Created on 8/11/2022 at 8:37 PM
Page 87 of 296 pages

through the required state match. FIMR is an important quality improvement strategy to improve maternal and child
health. FIMR not only provides important insight into opportunities for systems improvement, but they also serve as a
mechanism for local and regional communication, coordination and collaboration on other MCH issues. In FY2021,
FIMR programs operated in eight of the 24 jurisdictions experiencing the highest number of fetal and infant deaths.
During FY2021, FIMR process improvements previously identified through the Quality Improvement Council
continued. The process improvements included quarterly calls with all local coordinators to allow for cross-
jurisdictional collaboration and data sharing. To enhance infant mortality prevention efforts at the local level, quarterly
meetings were held with the Babies Born Healthy teams to align on prevention strategies and share best practices.
In several jurisdictions, Babies Born Healthy (BBH) staff participated in FIMR and Community Action Team (CAT)
meetings, and BBH was also involved in the follow up and outreach process for maternal interviewing. FIMR teams
were required to review all cases that were identified as meeting the following criteria: Substance use during
pregnancy, birth defects or congenital anomalies, or a maternal history of fetal loss. CAT teams were required to
address Statewide FIMR recommendations and develop strategies to increase education on safe sleep practices,
improving preconception care and early initiation and access to quality clinical care. The CAT teams also explored
how to improve referral, tracking and follow up of high-risk pregnant people and improve resources and referral to
SUD and SEN services.
Quarterly FIMR meetings focused on the ongoing congenital syphilis outbreak in Maryland and included updates
from the MDH Center for Sexually Transmitted Infections Program. Our FIMR program also worked closely with
NCFRP FIMR staff to explore efforts to better align congenital syphilis case review standards with national best
practices. Congenital syphilis case review will transition to the MDH Center for STI Programs in FY2022 and will no
longer be the responsibility of FIMR teams.
FIMR coordinators were surveyed on receipt and utilization of the MDH Postpartum Infant and Maternal Referral
Form (PIMR) and the Medicaid Pregnancy Risk Assessment (PRA) form. The purpose of both forms is to identify
pregnant and postpartum people in need of resources and services and to connect them to the local health
department for care coordination. There was wide variation on the use of the PIMR form though it is seen to be
underutilized in most jurisdictions due to lack of awareness of the form, lack of clarity of the workflow, and the paper-
based nature of the form creating gaps in the referral pathway. For example, it was reported that the faxed forms
were difficult to track and sometimes got lost in staff offices, creating unnecessary challenges to connecting with
clients. The Medicaid PRA form is more widely used since completion of the form is reimbursed by Medicaid and its
value is clearly communicated to prenatal providers.
Community Action Teams (CAT) review the findings of the CRT and are charged with advocating for creating large-
scale systems change to benefit all pregnant or postpartum women, with particular emphasis on those identified as
being most at-risk and vulnerable to poor pregnancy outcomes. Membership of Community Action Teams consists of
those with the political will and fiscal resources to create systems changes. These members can develop a
community perspective on how to best create the desired changes within the community. In FY 2021, Community
Action Teams provided recommendations and developed a distribution plan for Safe Sleep, Kick Count resources,
developed patient empowerment campaigns to encourage pregnant people to “Speak Up” about their pregnancy
concerns to care providers, addressed care collaboration and continuity of care starting with preconception health,
provided public presentations to local government officials on Infant Mortality and racial disparities in their
jurisdiction, and continued to participate in local Substance Exposed Newborn (SEN) workgroups with Department
of Social Services (DSS) to implement the START (Sobriety Treatment and Recovery Teams) model within the
jurisdiction, among many other activities executed. Also, in FY2021, MCHB began work on several SUID and safe
sleep data visualization briefs for dissemination to local health departments and other partners.
Created on 8/11/2022 at 8:37 PM
Page 88 of 296 pages

Child Fatality Review (CFR):
During FY2021 MCHB provided Surveillance and Quality Initiatives (SQI) grants to all twenty-four jurisdictions to
support ongoing Child Fatality Review (CFR) Activities. Multidisciplinary case review teams (CRT) conduct
confidential, de-identified reviews of fetal and infant deaths within the jurisdiction to identify non-clinical factors and
systems issues contributing to poor pregnancy outcome and deaths. The teams develop prevention strategies to
address health care delivery systems and identify community resource needs, in order to reduce preventable child
deaths.
Throughout FY2021, both FIMR and CFR teams continued to readjust to the COVID-19 Pandemic. Local Health
Department members were re-deployed to help with the pandemic efforts. In addition, teams no longer met in-person
and adjusted to secure virtual meetings. The majority of teams found that virtual meetings improved attendance and
availability of members, and many teams were able to add new members that were previously unable to attend in
person meetings consistently.
For the NPM 3: Risk Appropriate Perinatal Care, the number of VLBW (very low birth weights, < 1,500g) births at all
Maryland hospitals decreased slightly from 2018 to 2019, from 1,050 VLBW deliveries in 2018 to 954 VLBW births
in 2019 across all hospital levels. Due to the Network Security Event, 2020 data is still pending.
A total of 17,775 babies were born at Level I and Level II delivering hospitals in 2020, with 78 of these babies (8.4%
of all VLBW births) born at weights less than or equal to 1,500g. There were 43,500 births at Maryland Level III/IV
delivering hospitals in 2020, of which 854 were VLBW, making up 91.6% of all VLBW births, keeping ahead of the
Healthy People 2020 goal of 83.7% of VLBW births occurring at Level III or Level IV facilities. This is a slight
decrease from 2019 with 93.4%.
Maryland Perinatal System Standards:
The Maryland Perinatal System Standards was developed in the mid-1990s by a Maryland Department of Health
advisory committee as a set of voluntary standards for Maryland hospitals providing obstetric and neonatal services.
Level III and Level IV hospitals are designated perinatal referral centers that have both specialized care for pregnant
women, as well as the baby. The Standards have since been incorporated into the regulations for designation of
perinatal referral centers by the Maryland Institute for Emergency Medical Services Systems (MIEMSS), as well as
the Maryland Health Care Commission’s State Plan regulations for obstetrical units and neonatal intensive care
units. MIEMSS regulates Level III and Level IV Hospitals. Level I and Level II are voluntary designations as delivering
hospitals but do not have the specialized care as Level III and Level IV hospitals.
The Maternal Child Health Bureau (MCHB) convenes and leads the Perinatal Clinical Advisory Committee that
develops, reviews, and updates the Maryland Perinatal System Standards for all levels of obstetric and neonatal
care. The Perinatal Standards were updated in April 2019 to be consistent with the most recent edition of the
Guidelines for Perinatal Care, a joint manual of the American Academy of Pediatrics (AAP) and the American
College of Obstetrics and Gynecology (ACOG). All Level III and Level IV perinatal referral hospitals were notified of
this update, and MIEMSS (Maryland Institute for Emergency Medical Services Systems) Regulation Compliance
Verification packages were sent to these hospitals in order to verify compliance with the Standards. Of the 32
delivery hospitals in Maryland, seven (7) are Level I, twelve (12) are Level II, eleven (11) are Level III, and two (2) are
Level IV. The most recent Standards are incorporated in regulations governing the Level III and IV hospitals, and
compliance with the Standards is required for designation at these levels. In FY21, MCHB continued to work with the
Maryland Institute for Emergency Medical Services Systems in the compliance reviews of Level III and IV hospital
centers.
Created on 8/11/2022 at 8:37 PM
Page 89 of 296 pages

The Standards specify that very low birth weight (VLBW) births should occur at Level III and IV hospitals which have
the necessary subspecialty obstetric care and neonatal intensive care. VLBW infants, who weigh 1,500g or less at
birth, are the most fragile newborns. They are more likely to survive and thrive when born in a facility with a Level III or
IV neonatal intensive care unit (NICU). MCHB and Vital Statistics monitor the number of VLBW births born in
Maryland, and track where these infants were born. Each Maryland delivering hospital receives a report showing
VLBW births and neonatal mortality rates by hospital of delivery and level of care.
One role of the MCHB Morbidity, Mortality, and Quality Review Committee is to monitor voluntary compliance of Level
I and Level II hospitals with the Standards. During site visits conducted every four to five years, Level I and Level II
hospitals are asked to review all VLBW births at their site and to determine if any could have been avoided by
transfer of the mother to a higher level of care prior to delivery. During Fiscal Year 2021, the MMQRC reviewed the
VLBW data from 2018, and conducted virtual site visits at three Level II hospitals (prioritizing those with higher
VLBW deliveries than other Level I and II hospitals). Additional site visits are planned in FY 2023.
Maryland Perinatal-Neonatal Quality Collaborative (MDPQC):
Perinatal Collaboratives are networks of perinatal care providers and public health professionals working to improve
health outcomes for women and newborns through continuous quality improvement (QI). The Collaborative provides
participating birthing hospitals with educational resources, technical assistance, and a platform for communication
and sharing best practices.
The MDPQC Steering Committee was reestablished in August 2020, consisting of physicians, nurses, midwives,
and public health experts from hospitals and organizations across the state of Maryland. The Steering Committee,
after reviewing relevant data and soliciting hospital input, decided to focus on maternal hypertension and neonatal
antibiotic stewardship for our quality improvement topics. The maternal hypertension topic area is being
implemented in partnership with the Alliance for Innovation on Maternal Health (AIM). Hospitals were recruited,
implementation and data collection plans established, and a kick-off event was held for each topic area
(Hypertension on 1/25/21, and Antibiotic Stewardship on 5/7/21). All 32 birthing hospitals were recruited for the
maternal hypertension initiative, and 20 hospitals were recruited for the neonatal antibiotic stewardship initiative.
The MDPQC also created a baseline assessment of hospital engagement and readiness, and hospitals continue to
submit data to the Collaborative on a quarterly or monthly basis. On the administrative side, a Mission Statement
was written, a website created, and a listserv including contacts from all birthing hospitals was launched. Learning
events hosted included COVID-19 Information for Birthing Hospitals, Maternal Safety Bundle Implementation, and the
first two events of a Respectful Care Webinar Series – “Respectful Care for All Families: Introduction to the Unique
Families Program and How it Betters Care for All Patient Populations'', and “Respectful Care While Addressing our
Implicit Bias”.
Neonatal Abstinence Syndrome (NAS):
The rate of neonatal abstinence syndrome (NAS) among Maryland resident newborns born in Maryland hospitals has
decreased 30.2%, from 14.2 per 1,000 newborn discharges in 2017, to 9.9 per 1,000 newborn discharges in 2021
(Case-mix data, Health Services Cost Review Commission). From 2016-2020, Maryland had the State Performance
Measure (SPM) on Hospital Policy change to improve quality of care for infants with neonatal Abstinence Syndrome.
The Department of Human Services recently updated their Substance Exposed Newborn Policy to reduce the
number of SEN out-of-home placements and to improve the quality and effectiveness of services for SEN and
Created on 8/11/2022 at 8:37 PM
Page 90 of 296 pages

families impacted by substance use disorder. To address the need for cross-system coordination of services and
providers, MCHB program staff participated in statewide training for DHS staff to increase knowledge of community
resources for families with a substance exposed newborn. Any newborn displaying effects of withdrawal from a
controlled substance exposure as determined by medical personnel will trigger a SEN notification to DHS. MCHB
Program staff provided training on the Postpartum Infant and Maternal referral form (PIMR), which allows hospital
staff to refer families to their local health department for resources to address the child and family needs. Local DSS
staff were encouraged to support delivery hospitals in utilizing the PIMR form for any SEN notification, and
information about the PIMR was included in supplemental resources available for those who completed the SEN
policy training.
The Maryland Department of Health led a work group to establish a Statewide definition of Neonatal Abstinence
Syndrome. The purpose of this effort is to strengthen and standardize NAS reporting and inform program planning.
A multidisciplinary team agreed to the following definition and has communicated the definition to all Maryland
birthing hospitals:
Evidence of maternal use of opioids, benzodiazepines or barbiturates; and at least one of the following:
Presence of two or more infant withdrawal signs related to NAS
Birth hospitalization length of stay >three days
Perinatal Support Program: The purpose of the Maryland Perinatal Support Program (MPSP) is to support and
improve the perinatal system of care in Maryland. Specifically, MPSP brings maternal-fetal medicine consultation,
education and technical assistance, as well as obstetric nursing outreach and education, to Level I and II birthing
hospitals in the State. Maternal-fetal medicine specialists can provide unique support in the evaluation and
management of pregnant and postpartum patients with pre-existing medical conditions, pregnancy complications, or
known/suspected fetal anomalies.
During Fiscal Year 2021, providers from Johns Hopkins Hospital conducted 66 physician and advanced practitioner
outreach events and 14 nurse outreach visits. The providers continued to provide technical assistance, education,
and case reviews for conditions such as gestational diabetes, antiphospholipid syndrome, and substance use
disorders. Due to COVID, many of the outreach visits were limited to remote and telephone meetings. The providers
answered questions related to COVID and its effects on pregnant people and their fetuses. The University of
Maryland won a competitive project to take over the Perinatal Support Program beginning in FY 2022.
Babies Born Healthy: In FY21, nine sites across eight local jurisdictions implemented state funded Babies Born
Healthy (BBH) programs, which directed resources to engage women and communities to provide supportive
coordinated care and address disparities in infant mortality rates in Maryland. A total of 1,389 women had accessed
BBH services, and there was a total of 311 births among program participants and 8 fetal/neonatal deaths. These
jurisdictions were selected to receive funding after they had been identified by the Perinatal Periods of Risk
Assessment (PPOR) was conducted and concluded that these jurisdictions were key to effectively curbing
disparities and rates of infant mortality.
Services provided were geared towards the promotion of prenatal care, reduction of substance use, tobacco
cessation, infant safe sleep education, long-acting reversible contraception, accessing health insurance, and other
strategies driven by site-specific data to promote healthy maternal and infant outcomes. Specific activities included
home visiting strategies, nurse and paraprofessional case management services for high-risk women and infants,
family planning services, screening and referrals for mental health and substance use. Also in FY 2020, sites began
to utilize prenatal care groups following research pointing towards their effectiveness in promoting prenatal health
and birth outcomes.
Created on 8/11/2022 at 8:37 PM
Page 91 of 296 pages

COVID-19 continued to present barriers to both families and staff. Many staff are public health nurses in local health
departments (LHDs), as such they were pulled into Maryland’s COVID-19 response which left BBH sites with very
limited capacity at times. Families faced numerous challenges including job loss and eviction, difficulty in accessing
food, loss of childcare, lack of transportation, domestic violence, technology limitations, issues in accessing
necessary baby supplies, and others. Many BBH sites responded by doing emergency supply drop-offs to their
participants and were a crucial lifeline at the height of the pandemic.
Priority Area 2: Increase the number of infants who are breastfed
Breastfeeding:
The progress of Priority Area 2 is measured by NPM 4: Percent of infants who are ever breastfed. In 2020,
according to PRAMS data, 89.9 percent of Maryland mothers reported having ever breastfed their babies, a slight
decrease from 91.4% in 2019. Rates of breastfeeding in Maryland were high across all races ranging from 84.8%
for Non-Hispanic Black mothers to 93.9% among Hispanic mothers.
The Maryland Department of Health’s Breastfeeding Policy Committee provides technical assistance to birthing
hospitals related to the Maryland Breastfeeding Policy Recommendations. The committee consists of 11 members:
6 MDH staff members including the Title V Manager and 5 birthing hospital representatives. MCHB continues to
support all delivery hospitals in the state to become “Maryland Best Practices Hospitals,” by either attaining Baby
Friendly certification through the Baby Friendly Hospital Initiative (BFHI) or by meeting the ten criteria in the Maryland
Hospital Breastfeeding Policy Recommendations. At the implementation of the Maryland Hospital Breastfeeding
Policy Recommendations, Maryland had no Baby Friendly designated hospitals. For FY 2021, there were ten that
held current designation. Due to the COVID-19 Pandemic, many of the activities of the Breastfeeding Policy
Committee were halted including regular committee meetings, redesignation of Baby Friendly Hospitals, updating of
training modules, and technical assistance site visits.
Maryland WIC Program:
The Maryland WIC Program is committed to helping families have positive, successful breastfeeding experiences.
WIC provides resources, such as a FAQ sheet, handouts and a breastfeeding checklist available in both English and
Spanish, as well as videos that provide information on various breastfeeding-related topics. Maryland WIC employs
31 breastfeeding peer counselors who provide ongoing one on one support to pregnant and breastfeeding
participants. Maryland WIC staff provided breastfeeding education and support to parents and caregivers of 28,127
(unduplicated) infants during SFY2021 (July 2020-June 2021.) Additionally, Maryland WIC staff provided prenatal
breastfeeding education to 27,949 unduplicated participants during the same reporting period.
WIC Breastfeeding coordinators started training for their staff on diversity, equity, and inclusion to provide an
inclusive environment. In October 2021, WIC Breastfeeding coordinators received a presentation entitled “Equity in
Breastfeeding: Voices of Black Mothers.” In December 2021, Nekisha Killings, an IBCLC, provided a presentation
on breastfeeding and normalizing brown breasts.
Home Visiting: During FY 2021, six local health departments used Title V funds through Core Public Health funding,
Child Health Systems Improvement funding, and High-Risk Infants funding to support home visiting services to at-risk
women and infants. These programs link women to needed community resources such as WIC and breastfeeding.
Created on 8/11/2022 at 8:37 PM
Page 92 of 296 pages

In FY 2021, nearly 3,800 pregnant women enrolled in home visiting services and infants received home visiting
services through a local health department. Local health departments reported challenges due to COVID-19 that
ranged from local health departments temporarily closing and then adapting to changes after reopening to an
overflow of patients in other local health departments that remained open during COVID-19 and the decline in the
number served from past years was directly related to COVID-19 closures and restrictions.
Priority Area 3: Reduce the number of sleep-related infant deaths statewide
Promoting infant safe sleep continued to be a priority for Maryland in FY 2020. Progress of infant safe sleep is
measured by NPM 5. PRAMS data for 2020 births indicated that 78.5% of new mothers placed their babies on their
backs to sleep, similar to what was reported in 2016 at 79.4 percent. This exceeds the Healthy People 2020 target
of 75%. The prevalence was highest among NH white mothers (88%) and mothers 30 to 34 years of age (89%), but
lowest among NH Black mothers (67%) and mothers 20 to 24 years of age (60%).
In FY 2021, infant safe sleep education was provided to 6,728 families, providers, and other community members
through Title V. Jurisdictions such as Baltimore City have a dedicated provider outreach program to inform providers
including pediatricians, obstetrics and gynecologists, Department of Social Service providers on the importance on
focusing on infant safe sleep and how infants can sleep safely.
In addition, through Title V, 2,463 families received information on second hand/environmental smoke exposure.
CFR teams continued to review all sleep-related infant deaths and a detailed analysis and review was provided in
the annual CFR legislative report.
As part of FY 2021 SQI efforts, local CFR and FIMR teams prioritized dissemination of information and education on
sleep-related infant death and Safe Sleep best practices. Teams reported distribution of safe sleep materials, pack-
n-plays and sleep sacks, as well as ongoing community-based safe sleep education training conducted throughout
the state. Between Babies Born Healthy (BBH) and SQI grantees a total of 886 portable cribs were distributed in the
state during FY 2021.
Created on 8/11/2022 at 8:37 PM
Page 93 of 296 pages

Perinatal/Infant Health - Application Year
The Health Resources and Services Administration (HRSA) has identified three National Performance Measures
(NPM) for perinatal/infant health: 1) ensuring that higher risk mothers and newborns delivery at hospitals that are able
to provide appropriate care (NPM 3); 2) increasing the number of infants who are breastfed and those who are
exclusively breastfed through 6 months (NPM 4); and 3) increasing the number of infants placed to sleep on their
backs (NPM 5).
To this end, the state of Maryland, as a result of the 2021-2025 Needs Assessment, has identified all three
perinatal/infant health performance measures as priorities over the next five years. As part of the objective to
improve perinatal/infant health, Maryland will also look to reduce the racial disparities within these performance
measures.
Objective 1: Increase the number of very low birth weight babies from 93.4% (Baseline, 2019) to greater than 95%
by 2025 will be born in hospitals with the appropriate level of care.
NPM 3: Risk Appropriate Perinatal Care
The strategy selected for this NPM is to continue with the oversight and compliance review of the standardized
definitions for birthing hospital levels of care. Maryland has had a systematic approach focused on improving the
perinatal care system and reducing infant mortality for over ten years. Since the mid-1990s, Maryland has had a
systematic approach to improving the perinatal system of care and assuring delivery of very low birthweight (VLBW)
infants at hospitals with the appropriate level of care.
The Maryland Perinatal Standards of Care defines hospital levels of neonatal care and levels of maternal care using
American Academy of Pediatrics (AAP) and American College of Obstetrics and Gynecology (ACOG)/ Society of
Maternal Fetal Medicine (SMFM) guidelines. The standardized classification system includes: basic care (level I),
specialty care (level II), subspecialty care (level III) and regional perinatal health care centers (level IV)
[1]
.
The Maryland’s Perinatal Clinical Advisory Committee reconvened in 2018 to revise the Standards in order to be
consistent with the 8th edition of the Guidelines for Perinatal Care, issued in 2017 jointly by AAP and ACOG.
Standards are incorporated into the regulations for designation of perinatal referral centers (Level III and Level IV
hospitals) by the Maryland Institute for Emergency Medical Services Systems (MIEMSS) , as well as the Maryland
Health Care Commission’s State Plan regulations for obstetrical units and neonatal intensive care units.
For FY 2023, MIEMSS will continue with the Level III and IV Perinatal Referral Center re-designation with eight site
reviews. In addition, the MIEMSS Perinatal Advisory Committee will meet quarterly.
For FY2023, the Morbidity, Mortality, and Quality Review Committee (MMQRC) will continue to monitor voluntary
compliance of Level I and Level II hospitals with the Standards with four site reviews. The MMQRC will continue to
meet quarterly.
Maryland Perinatal Support Program
The purpose of the Maryland Perinatal Support Program (MPSP) is to support and improve the perinatal system of
care in Maryland. While Level III and Level IV perinatal hospitals (as defined in the Maryland Perinatal System
Standards and designated by MIEMSS) are required to have maternal-fetal medicine physicians on staff, the Level I
and II hospitals, community health clinics, and obstetric care providers often do not have access to such specialists.
Created on 8/11/2022 at 8:37 PM
Page 94 of 296 pages

Maternal-fetal medicine specialists can provide unique support in the evaluation and management of pregnant and
postpartum patients with pre-existing medical conditions, pregnancy complications, or known/suspected fetal
anomalies. Support provided by a maternal-fetal medicine specialist through consultation, education, and technical
assistance to obstetric providers may allow a woman to continue care within her community. Such support may also
assist an obstetric provider in determining whether a pregnant patient would need to transfer her prenatal care to a
specialty center. MPSP brings maternal-fetal medicine consultation, education and technical assistance, as well as
obstetric nursing outreach and education, to providers in all regions of the State. Consultation and other technical
assistance are provided virtually via secure internet hosts, through scheduled webinars and online meetings, and
also onsite (e.g. at the hospitals, clinics, or offices), as needed. These services are provided without charge to the
hospital or obstetric provider.
The three goals of the Maryland Perinatal Support Program are 1.) to assist in providing risk appropriate perinatal
care, 2.) to assist providers with determining if a prenatal patient will need to transfer her care to a specialty center,
and 3.) provide evidence-based guidelines for obstetrical care.
Following a competitive bid, University of Maryland was selected to lead the Maryland Perinatal Support Program.
During FY2023, University of Maryland will use the learnings from a needs assessment of Level I and II hospitals,
Federally Qualified Health Centers (FQHCs), and obstetric care provider practices across the state conducted in
FY2022 meet the needs of specialized perinatal care in Maryland. In addition, University of Maryland will provide
maternal-fetal medicine consultation, education, and technical assistance to community obstetric providers and other
individual groups, or organizations. They will do so through a website created for the Perinatal Support Program.
They will also continue to coordinate with other state initiatives such as Maryland Maternal Health Innovation
Program, the Morbidity, Mortality, Quality Review Committee.
Maryland Perinatal- Neonatal Quality Collaborative
Fiscal Year 2023 will mark the two-year maternal (hypertension) and neonatal (antibiotic stewardship) initiatives
selected by the MDPQC Steering Committee. Steering Committee members consist of providers, public health
officials, payors, patient representatives, and representatives of professional societies. The MDPQC will focus on
sustained implementation of quality improvement initiatives, which will include identifying barriers, assisting low
performers, and continuing regular check-in calls, learning events, and data reporting. An in-person learning event
will be organized to provide updates and invite high performers to share best practices and lessons learned. The
effectiveness of the collaborative will also be assessed at the midpoint of each initiative, with the Steering
Committee and participating hospitals providing feedback, and a root-cause analysis will be conducted for any
under-performing measures, as needed. The MDPQC will continue to heavily focus on health disparities and will
push out data-driven improvement activities and resources to promote health equity.
Maryland Maternal Health Innovation Program, MDMOM
MDMOM, the Maryland Health Innovation Program, is a five-year HRSA funded program to improve maternal health
across the state. MDMOM is a collaboration between Johns Hopkins University, Maryland Department of Health,
Maryland Patient Safety Center and the University of Maryland, Baltimore County who work together to coordinate
innovation in the areas of data, resource availability and hospital and community care.
The Maryland Maternal Health Task Force was convened by the MDH to address the needs of pregnant and
postpartum women in Maryland. While the Task Force was previously chaired by the Title V Manager, in order to
have a committee led by partners, an election was held to vote for co-chairs. Two co-chairs were elected from a
community-based organization and another from an academic university. The Task Force developed a statewide
strategic plan with five areas of focus: 1) Equity and antiracism, 2) Achieve health using the life course model, 3)
Families and Communities, 4) Data, and 5) Workforce. During the next Fiscal Year, the co-chairs will continue
Created on 8/11/2022 at 8:37 PM
Page 95 of 296 pages

implementing the strategic plan through coordination through multiple partners.
Surveillance Quality Initiatives
In FY2023, Surveillance Quality Initiatives such as Child Fatality Review and Fetal and Infant Mortality review will
continue to identify systemic preventive factors to improve perinatal health in Maryland. The goal of the SQI funding to
local jurisdictions is to develop, implement, and align recommendations aimed at improving rates of infant and child
fatalities. For Fiscal Year 2023, jurisdictions will continue to address the following priorities as part of their funding:
Dissemination of information and education on sleep-related infant death and Safe Sleep
Practices, particularly among communities at highest risk of sleep-related infant death;
Conduct screening, provide referrals to reduce incidence of substance use disorder in pregnancy
Increasing social supports for women during the perinatal and postpartum periods
In addition, jurisdictions will now include a health equity strategy into their program efforts using one of the following
priority areas:
Measure and assess health equity indicators and use that data to inform program design and community
involvement in program implementation
Identify gaps in workforce health equity competencies by assessing needs and providing opportunities for
professional development to all levels of staff. This includes the completion of the Kirwan training series on
implicit bias for all FIMR/CFR staff.
Use surveys, interviews or focus groups to include the community’s voice in the design and implementation of
the program and to promote accountability
All CFR/FIMR Coordinators will also attend a Maryland Department of Health-funded implicit bias training series led
by a diversity, equity, and inclusion expert consultant. The focus of this training will be to provide definitions,
recognition of intentional and unintentional biases, identifying root causes of inequity, and working in teams to take
action steps towards reducing inequities and systemic racism in the fetal/infant and child fatality review process and
program implementation.
FIMR
The Maternal and Child Health Bureau, housed within the Maryland Department of Health, serves as the lead agency
for Maryland’s Fetal Infant Mortality Review (FIMR) Program. Funded by Title V, our FIMR program works with
program staff in jurisdictions with the highest rates of fetal and infant mortality. Infant and child mortality are two of the
most critical indicators of the overall health of a population, and Maryland has made significant strides to improve
infant and child health. In 2020, the infant mortality rate in Maryland was 5.7/1,000, representing a 3% decrease from
the 2019 rates, and a 6% overall decrease from the average of 6.6/1,000 from 2011-2015. This is the lowest infant
mortality rate recorded in Maryland’s history. While infant and child mortality rates in Maryland have declined,
significant disparities persist and work remains to be done: there was a 6% increase in the non-Hispanic Black
infant mortality rate, from 2019 to 2020 additionally, the non-Hispanic Black infant mortality rate (9.9/1,000) is triple
that of the non-Hispanic White infants (3.3/1,000). There was a decrease in the rate of infant mortality for Hispanic
infants, from 5.11,000 to 4.6/1,000, however that is still higher than the 2018 rate of 3.8/1,000.
There are currently 8 funded FIMR projects in Maryland, operating in the jurisdictions identified via PPOR analysis as
having the highest rates of infant mortality in the state. They include Anne Arundel, Charles, Prince George’s,
Montgomery, Caroline, Wicomico, and Baltimore Counties and Baltimore City. The Fetal Infant Mortality Review was
designed to be a community-owned action-oriented process to improve service systems, and works to examine the
Created on 8/11/2022 at 8:37 PM
Page 96 of 296 pages

medical, non-medical and systems related factors contributing to fetal and infant death at the community level. Each
local team works with their Community Action Teams (CAT) to develop program and policy recommendations to
improve maternal and fetal outcomes. Leveraging the recommendations of the CAT teams, health departments will
now be required to implement interventions aimed at addressing factors contributing to preventable maternal and
infant deaths in Maryland.
In FY 2023, FIMR CAT teams will be asked to identify gaps and expand interventions to reduce infant mortality, with
specific focus on substance use disorder, reducing disparities, and reducing sleep-related infant deaths.
In FY 2023, FIMR teams will select cases for review based on the categories of fetal and infant death where the
largest disparities are present within their jurisdictions. Teams are also expected to conduct case reviews with one
or more of the following risk factors present: substance use during pregnancy; birth defects or fetal anomalies;
significant maternal health conditions (hypertension, gestational diabetes); maternal history of fetal loss; or SARS-
CoV-2 infection during pregnancy. Teams will work to identify various findings, recommendations and action steps for
improving systems of care for pregnant people and infants. Recent recommendations include developing
educational materials for providers and patients on the importance of early prenatal care and “counting kicks”,
improving access to family planning, bereavement and other mental health services and substance use disorder
services. A significant part of the review is incorporating the voices of postpartum people who experience a fetal loss
in addition to reviewing the medical aspects of the case, with Maternal Interviews being central to the FIMR process.
In FY23, FIMR teams will focus on Maternal Interviews as a strategy area for quality improvement. FIMR teams will
address health equity in their review process and FIMR CAT program to improve health disparities in their local
jurisdiction.
Objective 2: Increase the number of infants who are breastfed from a baseline of 88.6% to 90% (National
Immunization Survey).
NPM 4: Breastfeeding
The strategy selected for this NPM is to provide all postpartum mothers with breastfeeding information and providing
appropriate referrals to lactation consultant services before discharge. This strategy entails informing pregnant
women and new mothers about lactation consultant services and ensuring that lactation consultants have access to
new mothers after birth. As part of this strategy, Title V may consider utilizing doulas/birth workers in a similar role as
lactation consultant to promote breastfeeding.
This strategy is considered to have moderate evidence, where “dedicated lactation specialists may play a role in
providing education and support to pregnant women and new mothers wishing to breastfeed and to continue
breastfeeding to improve breastfeeding outcomes” was shown in various systematic literature reviews
[2]
.
Maryland Hospital Breastfeeding Policy
The Maryland Department of Health (MDH) formed an 11-member committee, which includes the Title V Manager, to
develop breastfeeding policy recommendations that will strengthen and improve current maternity care practices.
The first finalized policy recommendations were completed in September 2012. These policy recommendations,
based on WHO/UNICEF Ten Steps to Successful Breastfeeding, include evidence-based hospital practices to
increase rates of breastfeeding initiation, duration and exclusivity for healthy, fully term infants whose mothers have
chosen to breastfeed. The committee currently meets biannually and provides provider training and hospital policies
for Baby-Friendly hospitals.
Created on 8/11/2022 at 8:37 PM
Page 97 of 296 pages

In 2012, MDH launched a statewide initiative to help hospitals improve the support that hospitals give to
breastfeeding mothers. All 32 birthing hospitals committed to this quality improvement process. In 2016, almost 85%
of the birthing hospitals reaffirmed their commitments. Hospitals are encouraged to sign a letter of intent to become
designated as Baby-Friendly through the Baby-Friendly Hospital initiative, or to follow the Maryland Hospital
Breastfeeding Policy Recommendations. As of 2020, 10 hospitals reaffirmed their commitments, representing
approximately 31% of birthing hospitals.
Maternity Staff Training
Under the guidance of the Hospital Breastfeeding Policy Committee, and in a collaboration between International
Board-Certified Lactation Consultants (IBCLCs) at the Maryland Department of Health and the University of Maryland
Upper Chesapeake Medical Center, a series of 15 maternity staff training modules were developed. The modules
provide education and expertise needed to meet both the Maryland Hospital Breastfeeding Policy
Recommendations and the Baby Friendly Hospital Initiative. During SFY23, these state trainings will be updated.
They were planned to be updated in FY22 but were unable to do so due to the network security event and the inability
to view these modules on the shared drive.
Technical Assistance Calls
The Maryland Hospital Breastfeeding Policy Committee offers technical assistance conference calls three to four
times a year, on average, to help hospitals with implementation of the Maryland Breastfeeding Policy
Recommendations and Baby Friendly Ten Steps. These calls include practical steps and information from IBCLCs,
staff nurses, administrators and policy committee members from across Maryland. The experts on the call,
professionals from hospitals achieving the topic at hand, lead the conversation about best-practices and ideas on
how to best implement the topic being discussed. Past recordings on Auditing and Quality Improvement, Skin-to-
Skin and Breastfeeding Training Resource Webinar are still available for listening and will continue to be available in
FY23.
Physician Webinar Series
In 2016, the Maryland Hospital Breastfeeding Policy Committee coordinated a six-lecture series of free webinars
about breastfeeding-related topics
[3]
. These webinars provided continuing medical education (CME) credits, as well
training sessions help fulfill the Baby Friendly USA and the Maryland Hospital Breastfeeding Policy
Recommendations. CME credits were available at no cost until June 2019. These sessions continue to be online. In
Fiscal Year 23, these series will be updated. They were not updated in FY22 due to the network security event.
Maryland WIC Program
The Maryland WIC Program continues to be committed to helping families have positive, successful breastfeeding
experiences. WIC will continue to provide resources, such as a FAQ sheet, handouts and a breastfeeding checklist
available in both English and Spanish, as well as videos that provide information on various breastfeeding-related
topics. Maryland WIC employs 31 breastfeeding peer counselors who will continue to provide ongoing one on one
support to pregnant and breastfeeding participants.
Objective 3: Increase the number of babies who are placed on their back to sleep as reported by PRAMS from
78.5% to the Healthy People 2030 target of 88.9%
NPM 5: Safe Sleep
The Maryland Department of Health will conduct a literature scan, review strategies from other states, and review
existing data about infant safe sleep. We will procure a vendor to lead a Statewide infant safe sleep conference in
FY2023. This conference will focus on integrating evidence-informed infant safe sleep strategies into practical
Created on 8/11/2022 at 8:37 PM
Page 98 of 296 pages

messaging for a variety of stakeholders. The conference will gather community members with lived experience,
community-based organizations, local health departments, and other entities to share the strategy selected for this
NPM is to build on infant safe sleep campaigns by engaging Title V programs and community partners. This strategy
entails a professional training made available to Home Visitors, Healthy Start providers and other direct service
providers in the community who work directly with expecting and new mothers and families to emphasize a nuanced
approach to take family needs, beliefs and context into account when talking about safe sleep.
This strategy is a new approach and is supported by the “Building on Campaigns with Conversations” series of
modules developed by the National Center for Education in Maternal and Child Health (NCEMCH). The modules
received extensive input from the National Action Partnership to Promote Safe Sleep (NAPPSS) coalition of more
than 70 national organizations. Furthermore, this approach is based on Ajzen’s Theory of Planned Behavior and
follows current American Academy for Pediatrics (AAP) recommendations for safe sleep.
Local Health Departments
Local Health Departments through Babies Born Healthy (BBH) and Care Coordination Units will continue to provide
information related to Infant Safe Sleep. In addition, sites with portable crib programs will continue to provide
portable cribs for families in need.
Babies Born Healthy (BBH)
The goal of Babies Born Healthy (BBH) is to identify and link at-risk pregnant people to essential services that have
been associated with improved birth outcomes. To achieve the Healthy People 2030 Objective of 5.0 infant deaths
per 1,000 live births the objectives of BBH are to: (1) Reducing overall infant mortality rates in Maryland by 5%
In FY 2023, there will be stronger guidelines on how programs should plan and execute their care coordination
services, including guidance on screening, care planning, and engagement. In FY23, programs will be required to
provide services to program participants through 6-months postpartum, when they had previously been required to
provide services through 6-weeks postpartum. Additionally, there will be stronger guidelines for the inclusion of an
equity strategy for each program. Babies Born Healthy has also been brought into closer alignment with FIMR/CFR
programming in order to synergize reports and incidents of deaths and the jurisdictional response to address the
causes of death.
The Babies Born Healthy strategy will undergo a refresh in FY2023 for FY 2024-2028. The purpose of the refresh
process is to assess the most up to date data and evidence and align with other major infant mortality initiatives such
as the Statewide Integrated Health Improvement Strategy. The renewed focus will be on decreasing disparities,
strengthened outcome measures, and building evaluation into the program.
The refresh will consist of further examining the following outcome measures to determine jurisdictional priorities:
infant mortality rate and numbers by jurisdiction, disaggregated by race and ethnicity, low birth weight, preterm birth
weight, access to prenatal care, and other indicators such as social determinants of health indicators and maternal
health indicators. Existing programmatic data such as quarterly reports, surveys, and key informant interviews and
scan evidence-based practices that improve infant health will also be reviewed.
[1]
https://www.acog.org/clinical/clinical-guidance/obstetric-care-consensus/articles/2019/08/levels-of-maternal-care
[2]
https://www.mchevidence.org/documents/NPM-Webinar-3-04-22-20.pdf
Created on 8/11/2022 at 8:37 PM
Page 99 of 296 pages

Child Health
National Performance Measures
NPM 6 - Percent of children, ages 9 through 35 months, who received a developmental screening using a parent-
completed screening tool in the past year
Indicators and Annual Objectives
Federally Available Data
Data Source: National Survey of Children's Health (NSCH)
2017 2018 2019 2020 2021
Annual Objective 34.2 34.6 35 41.9
Annual Indicator 43.1 36.6 34.7 40.9 40.3
Numerator 60,201 49,586 47,097 55,907 57,317
Denominator 139,848 135,327 135,685 136,579 142,190
Data Source NSCH NSCH NSCH NSCH NSCH
Data Source Year 2016 2016_2017 2017_2018 2018_2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 42.9 43.9 44.9 45.9
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - National Survey of Children's Health (NSCH)
Maryland - National Survey of Children's Health (NSCH)
Maryland - Objectives
Created on 8/11/2022 at 8:37 PM
Page 101 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 6.1 - Number of parents who receive information/education on the importance of developmental screenings
from Home Visiting and Care Coordination Title V providers
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 2,832 1,181 1,201 1,220 1,239
Annual Indicator 1,162 1,035 1,022 749 2,325
Numerator
Denominator
Data Source MCHB Data MCHB Data MCHB MCHB Data MCHB Data
Data Source Year 2017 2018 2019 FY 2020 2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 1,259.0 1,278.0 1,278.0 1,300.0
Created on 8/11/2022 at 8:37 PM
Page 102 of 296 pages

State Performance Measures
SPM 3 - Receipt of Primary Care During Early Childhood
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 67.4 64.6 65.8 67.1 68.2
Annual Indicator 63.5 65.9 67.1 67 71.7
Numerator 25,389 30,621 25,794 24,969 27,940
Denominator 39,994 46,466 38,455 37,253 38,989
Data Source Medicaid Medicaid Medicaid Medicaid Medicaid
Data Source Year 2017 (CY) 2018 (CY) 2019 (CY) 2020 (CY) 2021 (CY)
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 69.4 70.6 71.8 73.0
Created on 8/11/2022 at 8:37 PM
Page 103 of 296 pages

SPM 4 - Number of Asthma Emergency Room Visits per 1,000 for Children age 2-17 with a primary diagnosis of
asthma
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 9.2 3.5
Numerator 10,974 4,213
Denominator 1,195,993 1,193,543
Data Source Health Services Cost Review
Commission
Health Services Cost Review
Commission
Data Source Year 2018 2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 8.5 7.2 6.7 6.2
Created on 8/11/2022 at 8:37 PM
Page 104 of 296 pages

State Action Plan Table
State Action Plan Table (Maryland) - Child Health - Entry 1
Priority Need
Ensure that all children have an opportunity to develop and reach their full potential
NPM
NPM 6 - Percent of children, ages 9 through 35 months, who received a developmental screening using a parent-
completed screening tool in the past year
Objectives
Increase the percentage of children who receive a developmental screen from 40.9% to 46% by 2025.
Strategies
1. Local health departments will educate parents on the importance of developmental screenings. 2. Track and monitor
Medicaid data regarding developmental screenings.
NOMs
NOM 13 - Percent of children meeting the criteria developed for school readiness (DEVELOPMENTAL)
NOM 19 - Percent of children, ages 0 through 17, in excellent or very good health
ESMs Status
ESM 6.1 - Number of parents who receive information/education on the importance of developmental
screenings from Home Visiting and Care Coordination Title V providers
Active
Created on 8/11/2022 at 8:37 PM
Page 105 of 296 pages

State Action Plan Table (Maryland) - Child Health - Entry 2
Priority Need
Ensure that all children have an opportunity to develop and reach their full potential
SPM
SPM 3 - Receipt of Primary Care During Early Childhood
Objectives
Increase the percentage of children receiving at least five well visits by fifteen months from 67% to 73% by 2025.
Strategies
1. Continue to monitor and track receipt of primary care in early childhood through Medicaid data. 2. Coordinate with local
health departments to provide primary care services such as childhood vaccinations, and vision and hearing screenings.
3. Home visiting programs will continue to promote primary care. 4. Support school based health centers to deliver primary
care to children.
Created on 8/11/2022 at 8:37 PM
Page 106 of 296 pages

State Action Plan Table (Maryland) - Child Health - Entry 3
Priority Need
Ensure children with asthma and their families have the tools and supports necessary to manage their condition so that it
does not impede their daily activities
SPM
SPM 4 - Number of Asthma Emergency Room Visits per 1,000 for Children age 2-17 with a primary diagnosis of asthma
Objectives
Decrease the number of asthma ED visits per 1,000 for ages, 2-17 from 9.2 to 5.3 by 2026.
Strategies
1. Support asthma home visiting through the local health departments and in collaboration with the Environmental Health
Bureau. 2. Support School Based Health Centers (transfer to MDH in 2022) 3. Support regional asthma collaborations to
coordinate asthma related activities. 4. Partner with CRISP (HIE) to strengthen linkages amongst pediatric care teams
including school health providers, EDs, primary care, and specialists.
Created on 8/11/2022 at 8:37 PM
Page 107 of 296 pages
Child Health - Annual Report
Maryland’s Priority Need for the child health domain is “to ensure that all children have the opportunity to develop and
reach their full potential”. Maryland Title V provided preventive and primary care through direct, enabling, and public
health infrastructure services to a variety of child health needs in FY 2021. Services and activities focus on the
needs of children across the Title V pyramid as outlined by the State Action Plan. Child health activities for which Title
V provides state leadership including local child fatality reviews, access to developmental screenings and medical
homes, school-based health services such as hearing and vision screening and referral, behavioral and substance
use screening and referral, immunizations, and early intervention services.
NPM 6 Developmental Screen: According to the National Survey of Children’s Health 2019-2020 data, 40.3% of
children ages 9 through 35 months received a developmental screening using a parent-completed screening tool in
the past year.
SPM 3 Receipt of Primary Care During Early Childhood (receiving at least 5 well-care visits by 15 months): Maryland
state Medicaid data reported that in 2021, 71.7% of children enrolled in Medicaid who reached age 15 months
received five or more well-care visits in their first 15 months of life.
Local Health Departments: Local health departments serve as Title V’s primary delivery arm for preventive and
primary care services for children. Each of the 24 local health departments receives federal Title V funding through a
state core funding process to support direct, enabling, and public health services and systems. In FY 2021, ten local
health departments used Title V core funding to support child health services including services such as
immunizations, hearing and vision screening (in collaboration with local public and private school systems); and
school-based health services (elementary through high school) including wellness care and behavioral health
screening.
Title V requires local health departments that provide child health services to submit performance measure data
quarterly to demonstrate how their activities align with the Title V state action plan. This includes activities such as
providing linkages to medical homes, providing information on developmental screenings and subsequent linkages
to early intervention or specialty care when indicated, linkages to mental health or substance use treatment, and
education on secondhand smoke exposure.
The ongoing COVID-19 Pandemic in FY 2021 limited the local health department’s efforts to provide critical child
health services across Maryland. The dual burden of redeployed public health workers as well as the shifting school
and work closures for community members contributed to the ability of local health departments to provide child
health services through Title V funded programs. As many of our local health departments not only deliver essential
public health services, but they also serve as the first responders for the COVID-19 pandemic response. With the
scope and severity of the pandemic many local health departments had to shift their public health workforce capacity
to administer vaccines, outbreak investigations and contact tracing activities. As a result, there were clinic closures,
limited capacity/hours of local health department programs, and reduced workforce for staffing core services had a
tremendous impact on the number of children reached. As a core component of Title V funding is utilized to support
child health services that are administered or connected to school systems, the pandemic driven school closures,
quarantine requirements for those exposed to COVID-19 and parental shifting work environments drastically reduced
the number of children served in FY 2021. The table below shows the dramatic difference in numbers served
between FY 2020 and FY 2021.
Created on 8/11/2022 at 8:37 PM
Page 108 of 296 pages

Type of Service Number of Children
Served FY 2020
Number of Children
Served FY 2021
Immunizations 16,199 2,934
Hearing Screen 51,073 4,141
Vision Screen 46,948 5,091
School Based Well Visits 20,943 2,509
Total 135,163 14,675
Medicaid continues to be a significant Title V partner. The current MOU outlines agreements and guidelines on
administration and policy, systems coordination, outreach and referral activities, and data sharing. Local health
department Title V funded staff work with the Medicaid Administrative Care Coordination Unit (ACCU) within their
health department to identify and enroll eligible children in the Medicaid Program and other child health services.
Child Fatality Review: A critical activity of the Maternal Child Health Bureau and Title V is the prevention of child
and adolescent deaths through Child Fatality Review (CFR). CFR was established by Maryland statute in 1999.
Maryland CFR program’s mission is to develop plans, implement change and advise on policy and practice to
prevent child deaths in every jurisdiction in the state. Maryland CFR comprises 24 local teams and the state team.
Local CFR programs review all unexpected deaths of children under the age of 18, in order to understand the cause
and incidence of child deaths and make community level recommendations for the prevention of child deaths. The
State CFR Team, in turn, reviews statewide child fatality data to make state-agency level recommendations,
implement recommended changes within the agencies represented on the State CFR team, and to advise State
leadership on preventing child deaths. Title V supports the 24-member State CFR Team, which meets quarterly, as
well as each of the 24 local CFR teams.
The State CFR Team oversees the efforts of local CFR teams that operate in each jurisdiction. Each month the local
CFR teams receive notice from the Office of the Chief Medical Examiner (OCME) of unexpected resident child
(under age 18) deaths and are required to review each of these deaths. Local teams meet at least quarterly to
review cases and make recommendations for local level systems changes in statute, policy, or practice to prevent
future child deaths, and work to implement these recommendations.
State CFR efforts to reduce the number of preventable child deaths continued as mandated by the Maryland
Legislature. In FY 2021, CFR received 181 referrals from the Office of the Chief Medical Examiner (OCME), and
teams reviewed 172 deaths, 95% of all cases referred.
In FY 2021, the CFR Coordinator continued to be an active participant in the Department of Human Services Social
Services Administration’s Substance Use Disorder Workgroup to collaborate on interagency efforts to reduce the
risk of harm for substance exposed newborns and their families. As part of those efforts, the CFR Coordinator
developed training materials on the Postpartum Infant and Maternal Referral form and presented to several hundred
DHS staff receiving training on DHS’ new Substance Exposed Newborn referral policy. The Maryland Postpartum
and Infant Referral Form (PIMR) l is an often-underutilized tool to refer and follow higher risk infants and families.
Historically, there have been low rates of PIMR referrals completed for infant death cases, which indicates that there
are significant systems gaps in identifying higher risk newborns and families that must be addressed to prevent
these infant deaths.
Created on 8/11/2022 at 8:37 PM
Page 109 of 296 pages

The CFR program continues to participate in the ongoing efforts of the CDC SUID Case Registry, and local teams
and coordinators received training and technical assistance on the utilization of the SUID Categorization Algorithm,
which was utilized in all SUID reviews that occurred during FY2021. Teams continued to work towards meeting the
timeliness goals set by the CDC (270 days from date of death to case cleaning by CFR epidemiologist) with 52
cases entered in the SUID case registry during FY2021, with 37% of cases meeting desired timeliness benchmarks,
and over 79% cleaned within 120 days of data entry.
The COVID-19 pandemic proved incredibly challenging to local CFR programs, with teams being unable to meet in
person for several months after the start of pandemic and delays in development in protocols in each jurisdiction to
allow for remote reviews. Additionally, CFR coordinators were partially or fully detailed to pandemic related duties for
several months.
Child Abuse Medical Providers (CHAMP) Initiative:
Chapter 334 of the Acts of 2005 (SB 782) charged the Secretary of the Maryland Department of Health (the
Department) to establish the Child Abuse and Neglect Centers of Excellence Initiative and to appoint and convene
the Child Abuse and Neglect Expert Panel. In 2008, pursuant to Md. Ann. Code Health-General Art., §13-2201, the
Child Abuse and Neglect Centers of Excellence Initiative was renamed Maryland Child Abuse Medical Providers
(CHAMP). The CHAMP initiative was developed to provide expert consultation and training to local multidisciplinary
teams (MDTs) and child advocacy centers in the diagnosis and treatment of child abuse.
According to the Maryland Department of Human Services’ Child Protective Services, in Fiscal Year (FY) 2021, there
were 41,567 cases of alleged child abuse and neglect in Maryland. This represents a significant decrease in cases
of alleged child abuse and neglect in FY 2019 and FY 2020 but is likely an artifact of the decreased reporting by
school staff due to school closures due to the COVID-19 pandemic and does not reflect actual decreases in child
abuse and neglect.
Multidisciplinary teams (MDTs) comprised of medical professionals, Child Protective Services staff, law
enforcement, mental health providers, forensic interviewers, State’s Attorneys and victim advocates are used to
enhance and improve investigations and responses for children and families. These teams are required due to the
complex nature of child abuse and neglect investigations. These MDTs staff child advocacy centers (CACs), which
are child-friendly facilities where children and families engaged in child abuse investigations can access services. In
Maryland, 24 local CACs respond to over 5,000 children each year with allegations of sexual abuse, sexual assault,
and other maltreatment of children. The CHAMP initiative was developed to provide training and ongoing support to
local providers, and expert consultation to local or regional CACs in the diagnosis and treatment of child physical
abuse, sexual abuse, and neglect.
During FY 2021 the Department’s Maternal and Child Health Bureau administered the CHAMP initiative through staff
support of six CHAMP faculty members contracted to provide ongoing training, consultation, and case review to local
providers.
CHAMP Activities
The CHAMP initiative was administered through a grant agreement with Lifebridge Health. In FY 2021, the CHAMP
initiative maintained a faculty of six child abuse medical experts. The faculty met monthly to discuss future
educational activities, recruitment of network providers, and child maltreatment prevention efforts. The CHAMP
faculty provided educational and case review support in the diagnosis and treatment of child maltreatment to local
Created on 8/11/2022 at 8:37 PM
Page 110 of 296 pages

health care providers, and expert consultation to State agencies involved in child abuse and neglect investigations,
such as Child Protective Services and law enforcement. CHAMP faculty provide case review to local providers via a
secure, HIPAA-compliant online program called Telecam. Local providers can upload case information and images
to the secure website, which is accessible only to CHAMP faculty for review.
In FY 2021, CHAMP held three half-day continuing education events for health care providers to review a variety of
child maltreatment topics. In FY 2021, CHAMP held three half-day continuing education events for health care
providers to review a variety of child maltreatment topics, including: Child Sex Abuse Prevention- the Intersection of
Legal Reform, Research, and Training; Interpreting Findings in Child Sexual Abuse; Research for Practice; Basic
Child Maltreatment Examination; and Forensic Evidence Testing. Each educational event also included an
interactive case review session, where providers presented child abuse cases and participated in a discussion of
the case, their evaluations, and findings. The case review sessions were led by a faculty member and were an
opportunity for providers to review and discuss suspected incidents of child abuse and neglect. The case review
sessions were particularly helpful for those who practice in lower volume jurisdictions and may not have opportunities
to observe and assess fewer common findings in a clinical setting. The Forensic Nurse Examiner Faculty members
conducted seven adult and seven pediatric forensic nurse examiner trainings in FY 2021.
In FY 2019, the Department partnered with the Maryland Children’s Alliance to conduct a statewide assessment of
each CAC’s resources for helping assess and address child maltreatment. Maryland Children's Alliance is a private
nonprofit organization accredited by the National Children’s Alliance as a State Chapter to serve as a convener of
CACs across Maryland. The Maryland Children’s Alliance plays a vital role in providing accreditation support and
professional development for local member centers. In FY 2021, the CHAMP Initiative responded to the 2019 MCA
Statewide Needs Assessment of each CAC’s resources for assessing and addressing child maltreatment. Several
actions and activities were undertaken to address the primary areas of concern identified by the Statewide Needs
Assessment:
Medical Evaluation Capacity
Insufficient medical evaluation capacity has been a persistent challenge across the State. The CHAMP Faculty
identified all the medical partners associated with Maryland’s CACs, and conducted significant outreach throughout
FY 2021 to identify both CACs lacking medical support, and those medical partners that were not yet engaged with
CHAMP training and peer review services. The NCA standards require that specialized medical evaluations for
pediatric clients be available on-site, or with other appropriate agencies or providers through written linkage
agreements. In FY 2021, an additional CAC gained the capacity to provide on-site medical evaluations, and
CHAMP funds were used to purchase needed medical examination equipment in order to allow for these on-site
evaluations. Many CACs operate under a memorandum of understanding (MoU) with a local hospital or medical
center for needed examinations. The majority of CACs that provide medical examinations offer services at the
convenience of the family and provider and are generally performed within one to two weeks of initial family contact
with the CAC.
Medical staff who serve the CACs include physicians and pediatricians, sexual assault forensic nurse examiners,
medical directors, and medical representatives for the multi-disciplinary team. The vast majority of centers do not
employ their own medical providers. Almost all centers work with local hospitals to provide medical staff on a part-
time, as-needed basis. In order to enhance medical evaluation capacity, especially in Southern Maryland, CHAMP
Faculty have initiated training for a group of pediatric Hospitalists employed at MedStar St. Mary’s Hospital. The
team was also provided with a Cortexflo camera, to ensure their ability to take evidence grade photographs and
videos with secure storage capacity for forensic medical examinations. Additionally, several nurses from Southern
Created on 8/11/2022 at 8:37 PM
Page 111 of 296 pages
Maryland were engaged in FNE-A education and clinical training by CHAMP Faculty member Pamela Holtzinger.
Training and Standards
The 2019 CAC needs assessment found most centers are not currently providing any training to medical providers
and rely on local hospitals to provide necessary training. NCA standards require ongoing, continuous quality
improvement for the medical components of the CAC. In addition, NCA standards require medical professionals
providing services to the CAC to demonstrate continuing education in the field of child abuse medicine. These
continuing education requirements consist of a minimum of eight contact hours every two years.
The CHAMP Faculty has spent FY 2021 revising and updating their curriculum, referral criteria, and peer review
standards to ensure the offered trainings continue to meet NCA standards as well as providing sufficient preparation
for CHAMP trained medical providers performing child abuse medical evaluations at CACs or hospitals.
CHAMP Faculty have continued to provide additional outreach to CAC Medical Providers to ensure that there is
greater utilization of Telecam, helps CACs meet NCA medical standard “C.” Standard C requires medical
professionals providing services to CAC clients to demonstrate that, at minimum, 50 percent of all abnormal findings
undergo expert review by an “advanced medical consultant.” As the result of recently increased reporting
requirements for CACs, the additional functionality of Telecam to increase data collection capacity has been an
important improvement.
Accreditation Process
Along with MCA, CHAMP Faculty have committed to continue to ensure medical providers at the currently
unaccredited CACs have access to the required training and advanced medical consultation needed to meet the
medical evaluation standards for gaining NCA accreditation. Additionally, CHAMP Faculty will continue to assist
CACs in meeting newly updated medical evaluation standards.
The Department intends to assist the CHAMP Initiative in engaging other key stakeholders who work with children
and child maltreatment. The CAC needs assessment provided the Department with a starting point in bridging gaps
in the continuum of care. Recommendations in the needs assessment included providing more training opportunities
for school nurses on child maltreatment, as well as a recommendation that all Maryland medical staff who see
children should screen for Adverse Childhood Experiences at their well visits. The Department intends to work more
closely with the Maryland Children’s Alliance, the CACs, and the CHAMP Faculty to increase collaboration and
reduce gaps in the identification and evaluation of victims of child abuse and maltreatment.
Created on 8/11/2022 at 8:37 PM
Page 112 of 296 pages

Child Health - Application Year
The state of Maryland identifies the objective for child health as “ensuring all children have the opportunity to develop
and reach their full potential.” To this end, in FY 2023, Title V will employ the following strategies to improve child
health outcomes statewide:
Local Health Departments: In FY 2023, Title V will continue to provide federal Core Public Health funding to all 24
of the state’s local health departments. Local health departments have the opportunity to focus their efforts in one or
any of a combination of the three Title V domains: child health, maternal health, and/or children and youth with special
health care needs. Local health departments choose their domain of focus based on alignment with the Title V State
Action Plan and with local needs assessments. Allowable services within the child health services domain will
continue to include hearing and vision screening, school-based health services including well visits, screening and
referral for behavioral health and/or substance use, immunizations, and childhood asthma programming. In FY 2023,
eleven (11) out of the 24 local health departments focused on child health services.
Asthma: Beginning in FY 2022, local health departments were able to use Title V funding for the new State
Performance Measure related to reducing child asthma ER visits. Addition of this measure/service was to align with
the Statewide Integrated Health Improvement Strategy (SIHIS).
In 2019, the State of Maryland collaborated with the Center for Medicare and Medicaid Innovation (CMMI) to
establish the domains of healthcare quality and delivery that the State could impact under the Total Cost of Care
(TCOC) Model. The State entered a Memorandum of Understanding (MOU) that required Maryland to provide a
proposal for the Statewide Integrated Health Improvement Strategy (SIHIS) to CMMI by December 31, 2020. The
strategy aligns statewide efforts across three domains that are interrelated and, if addressed successfully, have the
potential to make significant improvement in not just Maryland’s healthcare system, but in the health outcomes of
Marylanders.
● Domain 1: Hospital Quality
● Domain 2: Care Transformation Across the System
● Domain 3: Total Population Health
Asthma (along with Severe Maternal Morbidity referenced in Women’s Health) is included within Domain 3: Total
Population Health. The strategy identifies a goal of reducing the number of asthma related Emergency Room visits
for children age 2-17 and decreasing the disparities between Black, Non-Hispanic to White Non-Hispanic rates by
30% by 2026.
In FY 2023, local health departments again may use Title V funding for asthma related programming/services
including asthma home visiting or asthma school-based management programs (in collaboration with PHPA’s
Environmental Health Bureau); provide health care education opportunities on asthma management; developing
asthma regional collaboratives to coordinate asthma related activities within the region; or partnering with CRISP
(the designated Health Information Exchange (HIE) for Maryland) to strengthen linkages among pediatric care teams
including school health providers, Emergency Departments, primary care and specialists.
Child Fatality Review: In FY 2023, all 24 jurisdictions in the state will continue to review all OCME-referred
unexpected child deaths. In FY 2023, CFR, FIMR and Babies Born Healthy programs will continue to complete a joint
planning process to ensure that all efforts related to infant, child and maternal health at local health departments are
aligned. Teams are asked to align their goals and objectives with recommendations from the 2019 Legislative
Report of the State Child Fatality Review Team, specifically: reduce sleep related infant deaths, enhance data quality
Created on 8/11/2022 at 8:37 PM
Page 113 of 296 pages

for SUID cases through continued participation in the CDC SUID Case Registry, and develop recommendations to
address racial disparities in child deaths. All jurisdictions are required to track their progress towards meeting
identified performance measures through quarterly reporting. Child Fatality Review teams will continue to work
towards data quality improvement for Sleep-related SUID deaths through our work with the CDC SUID case registry,
with a focus on decreasing the number of days between review and entry into the NCDR-CRS for SUID case and
decreasing the number and percent of missing and unknown priority variables for all SUID cases. To this end, the
Office of the Chief Medical Examiner has provided Doll Scene Reenactment training to their entire Forensic
Investigation staff, as well as revised their Infant Death Scene Investigation form to align with the CDC SUID IRF
document. As of July 2021, all infant deaths have a completed doll scene reenactment performed by a forensic
investigator and include scene reenactment photography to ensure that teams are better able to categorize these
deaths using the CDC Categorization algorithm.
During FY 23, the State CFR Team will develop an Advanced Review process for selected CFR cases, upon request
of local teams. The purpose of the Advanced Review team is to review cases that were deemed to have an
undetermined cause of death; where there was disagreement about the preventability of the death; when the death
was directly related to the COVID-19 pandemic; or upon special request of the local team.
Local teams will continue to provide letters to birthing hospitals upon review of an infant-sleep related death of a child
born at that hospital, to ensure that there is ongoing engagement around safe-sleep education from delivering
hospitals.
In FY 23, the local teams will participate in a Diversity, Equity, Inclusion, and Implicit Bias webinar training series to
promote health equity and a better understanding of systemic issues that lead to infant and child deaths. The training
will offer a foundation for a review team’s fatality review process with an equity lens, enabling the team to improve
data quality and identify prevention recommendations that target the root causes of deaths and reduce disparities.
School-Based Health Centers: In FY 2023, the Maternal and Child Health Bureau will formally begin administering
the Maryland School-Based Health Center (SBHC) Program. Maryland’s SBHCs represent an essential and
innovative strategy for improving the health and educational achievement of Maryland’s children and their families.
SBHCs are conveniently located where students spend most of their day and can therefore address the unique
needs of children and youth through increased access to medical, mental, dental and/or other health related
services. As of FY 22, there are 94 SBHCs located in 17 of the 24 Maryland jurisdictions. The Maryland SBHC
Program will conduct a statewide needs assessment in FY23 to inform further expansion of the program. SBHCs will
be integrated with Title V-funded programming through shared performance measures, alignment of initiatives
across the state, and coordination of services.
(CHAMP) Child Abuse Medical Provider Network: In FY 2023, the Child Abuse Medical Provider Network will be
maintained under the grant agreement with LifeBridge Health. Our six CHAMP faculty and two network providers will
continue to provide training and support to CAC multidisciplinary teams, in addition to providing peer review via
Telecam, a HIPAA-compliant chart review platform that allows medical providers to upload exam documentation for
advanced review by a member of the CHAMP faculty. Due to recent updates to the National Children’s Alliance
Standards for medical providers at accredited Child Advocacy Centers, the CHAMP Faculty will take a more
proactive role in ensuring that all accredited CACs in Maryland are utilizing the Telecam system for peer review to
ensure that 50% of all findings deemed abnormal or diagnostic of trauma from sexual abuse have undergone expert
review by an advanced medical consultant.
Created on 8/11/2022 at 8:37 PM
Page 114 of 296 pages

The initiative will also continue to provide educational activities, consultation, and case review support to local
providers, and to explore opportunities for child maltreatment prevention efforts. Additionally, the CHAMP faculty will
finalize development of a new training curriculum based on the findings of the 2019 CAC needs assessment. The
CHAMP Faculty have added an additional forensic nurse examiner trainer to the Initiative and are working to expand
forensic nurse examiner training options, as well as training for Pediatricians, in underserved areas of the State.
Created on 8/11/2022 at 8:37 PM
Page 115 of 296 pages

Adolescent Health
National Performance Measures
NPM 10 - Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year.
Indicators and Annual Objectives
Federally Available Data
Data Source: National Survey of Children's Health (NSCH)
2017 2018 2019 2020 2021
Annual Objective 87.3 87.7 88 82.2
Annual Indicator 88.7 87.1 87.1 81.4 78.7
Numerator 393,976 386,469 386,469 359,586 355,101
Denominator 444,207 443,800 443,800 441,589 451,033
Data Source NSCH NSCH NSCH NSCH NSCH
Data Source Year 2016 2016_2017 2016_2017 2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 83.0 83.8 84.6 85.4
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - National Survey of Children's Health (NSCH)
Maryland - National Survey of Children's Health (NSCH)
Maryland - Objectives
Created on 8/11/2022 at 8:37 PM
Page 116 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 10.2 - Number of adolescent (12-17) who receive well visits through school based health centers
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 45,000
Annual Indicator 37,578 798
Numerator
Denominator
Data Source MCHB Data MCHB Data
Data Source Year FY 2020 FY2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 60,000.0 75,000.0 90,000.0 110,000.0
Created on 8/11/2022 at 8:37 PM
Page 117 of 296 pages

State Performance Measures
SPM 4 - Number of Asthma Emergency Room Visits per 1,000 for Children age 2-17 with a primary diagnosis of
asthma
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 9.2 3.5
Numerator 10,974 4,213
Denominator 1,195,993 1,193,543
Data Source Health Services Cost Review
Commission
Health Services Cost Review
Commission
Data Source Year 2018 2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 8.5 7.2 6.7 6.2
Created on 8/11/2022 at 8:37 PM
Page 118 of 296 pages

State Action Plan Table
State Action Plan Table (Maryland) - Adolescent Health - Entry 1
Priority Need
Ensure that adolescents age 12-17 receive comprehensive well visits that address physical, reproductive, and behavioral
health needs.
NPM
NPM 10 - Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year.
Objectives
Increase the percentage of adolescents (12-17) who receive a preventive medical visit from a baseline of 81.4% to 85% by
2025.
Strategies
1. Continue the Healthy Kids Program under the EPSDT Program to enhance the quality of health services delivered by
Medicaid providers. 2. Continue the Sexual Risk Avoidance Education grant program to promote sexual risk avoidance. 3.
Continue the Personal Responsibility and Education Program to promote positive youth development. 4. Implement the
Maryland Optimal Adolescent Health Program to reduce teen pregnancy. 5. Continue to support local health departments
school based health services. 6. Support the network of school based health centers across the state.
ESMs Status
ESM 10.2 - Number of adolescent (12-17) who receive well visits through school based health centers Active
Created on 8/11/2022 at 8:37 PM
Page 119 of 296 pages

NOMs
NOM 16.1 - Adolescent mortality rate ages 10 through 19, per 100,000
NOM 16.2 - Adolescent motor vehicle mortality rate, ages 15 through 19, per 100,000
NOM 16.3 - Adolescent suicide rate, ages 15 through 19, per 100,000
NOM 18 - Percent of children, ages 3 through 17, with a mental/behavioral condition who receive treatment or counseling
NOM 19 - Percent of children, ages 0 through 17, in excellent or very good health
NOM 20 - Percent of children, ages 2 through 4, and adolescents, ages 10 through 17, who are obese (BMI at or above
the 95th percentile)
NOM 22.2 - Percent of children, ages 6 months through 17 years, who are vaccinated annually against seasonal influenza
NOM 22.3 - Percent of adolescents, ages 13 through 17, who have received at least one dose of the HPV vaccine
NOM 22.4 - Percent of adolescents, ages 13 through 17, who have received at least one dose of the Tdap vaccine
NOM 22.5 - Percent of adolescents, ages 13 through 17, who have received at least one dose of the meningococcal
conjugate vaccine
NOM 23 - Teen birth rate, ages 15 through 19, per 1,000 females
NOM 17.2 - Percent of children with special health care needs (CSHCN), ages 0 through 17, who receive care in a well-
functioning system
Created on 8/11/2022 at 8:37 PM
Page 120 of 296 pages

Adolescent Health - Annual Report
Maryland’s identified Priority Need for adolescent health is to “ensure that adolescents age 12-17 receive
comprehensive well visits that address physical, reproductive, and behavioral health needs.”
NPM 10 Adolescent Well Visit: According to the National Survey of Children’s Health 2019-2020 data,
78.7% of adolescents ages 12 to 17 received a preventive medical visit in the past year.
In FY 2021, Maryland Title V provided funding to local health departments to address adolescent health needs.
Additionally, MCHB’s Office of Family and Community Health Services (OFCHS) administered the Maryland Optimal
Adolescent Health (MOAHP), Personal Responsibility Education Program (PREP), and the Sexual Risk Avoidance
Education Program (SRAE) grants focused on adolescent reproductive health/wellness.
Local Health Departments: Title V funding directly supported four local health departments efforts to provide
school-based health services to middle and high school aged youth. School-based health services included
comprehensive wellness visits, mental/behavioral health screenings and care plans, and referrals to substance use
disorder treatment. In FY 2021, school-based health services were dramatically affected by the COVID-19
Pandemic response. Only 798 students received a comprehensive wellness visit, compared to over 30,000 in FY
2020. Schools in Maryland were closed in most jurisdictions until the end of March/beginning of April 2021. Upon re-
opening, schools were in a hybrid format where students were in school only 2-3 days per week. School closures
severely impacted the LHDs ability to assess students in need of health services.
In FY 2021, Title V also supported family planning/reproductive health clinics at the local health departments. During
FY 2021, 3,193 adolescents received a comprehensive reproductive health exam. Additionally, 749 adolescents
received counseling for behavioral health and substance use, and 108 adolescents received a referral for care or
treatment through a partner focusing on substance use and behavioral health. Through Title V funds and through Title
V matching funds, the Maryland Family Planning Program provided services to 7,071 individuals who were less than
20 years old. This represented 13.2% of the total clients served by the Maryland Family Planning Program.
Maryland Optimal Adolescent Health (MOAHP): In July 2020, the Maternal and Child Health Bureau, Office of
Family and Community Health Services (OFCHS) was awarded a three-year federal teen pregnancy prevention
grant. The Maryland Optimal Adolescent Health Program (MOAHP), (re-branded as True You Maryland), is a
collaborative effort between Healthy Teen Network, Johns Hopkins University Center for Adolescent Health, local
health departments and school and community-based programs in 6 rural jurisdictions. True You Maryland programs
have been established in Allegany, Dorchester, Somerset, Washington, Wicomico and Worcester counties. All
grantees will offer sexual education programming to teens aged 14-19 living in areas of the state with high rates of
teen birth and sexually transmitted infections.
The True You Maryland program promotes equity in reaching optimal health by preventing teen pregnancy and
sexually transmitted infections in rural counties of the state by creating an infrastructure to develop and support highly
effective health education and parent/caregiver programs.
During FY 2021, approximately 381 youth were served by the program. Local True You Maryland programs provided
training for county health education teachers in 4 counties and worked to get the Positive Prevention Plus (3Ps)
evidence-based curriculum approved for implementation by local county school boards. The curriculum was
implemented during the spring semester in one county. Each county also formed local systems teams, which are
composed of a variety of stakeholders including, but not limited to, health department and school system staff,
medical professionals, parents, youth, educators, social service organizations, law enforcement, child welfare
Created on 8/11/2022 at 8:37 PM
Page 121 of 296 pages

agencies, businesses, faith-based and youth serving organizations.
Each local program is required to form a youth advisory board to ensure that youth voice plays a critical role in the
local priorities set forth by the program and that the program activities are relevant and responsive to the needs of
county youth.
Program challenges included the global Covid-19 pandemic causing school scheduling disruptions, the
reassignment of some local health department staff to Covid-19 focused work, and delays in approval of the Positive
Prevention Plus (3Ps) curriculum by local school boards.
PREP: Title V federal funds are also used to support the salaries of two state-level staff to coordinate efforts related
to adolescent health through the Personal Responsibility Education Program (PREP) and the Sexual Risk
Avoidance Education Program (SRAE). During the past year, adolescent and young adult health program
coordinators have focused their efforts on strengthening collaborative relationships within the state health department
as well as with the Maryland State Department of Education (MSDE) in addressing adolescent health priorities
including access school based reproductive health services, sexuality education (comprehensive and abstinence-
based) and production and dissemination of adolescent health data briefs.
PREP program implementation occurred in 8 jurisdictions across the state, including Allegany, Anne Arundel,
Baltimore City, Dorchester, Prince George’s, Washington, Wicomico, and Worcester counties. PREP’s sub-
grantees provided services to approximately 1,088 youth through various evidence-based curricula, outreach, and
supportive program activities in community and faith-based organizations and local health departments. PREP
programs were implemented in a variety of settings across the state including a YMCA, county high schools and
churches.
PREP also funded Project KISS (Keeping It Safe Sexually), a college-based peer educator training model through a
collaboration of MDH, University of Maryland Eastern Shore, and Salisbury University. In its fourth year, Project KISS
provided training for 23 peer educators. This training equips peer educators with the skills required to provide
reproductive health education to fellow students on campus. In FY 2021, approximately 631 students were seen
between the two campuses. Project KISS also supports health screenings; 84 students received HIV testing and 9
students were screened for Hepatitis C at local health departments.
PREP peer educators were able to develop leadership skills, provide valuable insight regarding program activities,
and increase program impact through participation in programs at Coppin State University (Coppin CARESS) in
Baltimore City and Project KISS on Maryland’s Eastern Shore.
The global COVID-19 pandemic impacted recruitment and engagement efforts, and the number of students enrolled
in the program decreased.
SRAE: The SRAE program is implemented statewide by grantees in 7 jurisdictions through local health departments
in Baltimore City, Caroline County, Garrett County, Somerset County, Washington County, Wicomico County, and
Worcester County as well as one community-based organization grant that was selected through a Request for
Application (RFA) process.
The SRAE program approach is guided by a Positive Youth Development Framework which teaches self-regulation,
healthy relationship skills, goal setting, and risk reduction strategies related to sexual coercion, dating violence, illicit
drug use, and underage drinking to middle and high school age students. In FY 2021, the SRAE program was
Created on 8/11/2022 at 8:37 PM
Page 122 of 296 pages

impacted by the global pandemic, and some local programs shifted to virtual or hybrid implementation formats to
observe COVID-19 safety guidelines. Despite these barriers, 1,372 students participated in programmatic activities
statewide.
Specific program activities in FY 2021 included youth summer camps, virtual and in-person parent education
workshops, community service projects and a Parent-Child cookout for 8th graders transitioning to high school and
their parents.
Created on 8/11/2022 at 8:37 PM
Page 123 of 296 pages

Adolescent Health - Application Year
Maryland Title V identifies the objective for adolescent health as “ensuring adolescents receive a comprehensive well
visit that addresses physical, reproductive, and behavioral health needs.” To this end, in FY 2022, Title V will employ
the following strategies to improve adolescent health outcomes statewide:
SPM 4: Decrease the number of asthma Emergency Department (ED) visits from a baseline of 0.3 ED visits per
1,000 for ages 12-17 (2019) to 0.1 in 2026
Local Health Departments: Title V will continue to provide federal Core Public Health funding to local health
departments in FY 2023 to support school based health efforts related to school based health clinics and asthma
programming and services which specifically target middle and high school students. In FY 2021, there were three
local health departments who focused their Title V funding on school based health services.
Asthma: Beginning in FY 2022, local health departments were able to use Title V funding for the new State
Performance Measure related to asthma programming. Addition of this measure/service is to align with the
Statewide Integrated Health Improvement Strategy (SIHIS). These services include expanding home visiting,
collaborating with providers and the health information exchange in their region, and school based health services to
improve asthma health in Maryland.
In 2019, the State of Maryland collaborated with the Center for Medicare and Medicaid Innovation (CMMI) to
establish the domains of healthcare quality and delivery that the State could impact under the Total Cost of Care
(TCOC) Model. The collaboration also included an agreed upon process and timeline by which the State would
submit proposed goals, measures, milestones, and targets to CMMI. As a result of the collaboration with CMMI, the
State entered into a Memorandum of Understanding (MOU) that required Maryland to provide a proposal for the
Statewide Integrated Health Improvement Strategy (SIHIS) to CMMI by December 31, 2020. The SIHIS aligns
statewide efforts across three domains that are interrelated and, if addressed successfully, have the potential to
make significant improvement in not just Maryland’s healthcare system, but in the health outcomes of Marylanders.
● Domain 1: Hospital Quality
● Domain 2: Care Transformation Across the System
● Domain 3: Total Population Health
Asthma is included within Domain 3: Total Population Health. The strategy identifies a goal of reducing the number
of asthma related Emergency Room visits for children aged 2-17. Title V will specifically collect data on adolescents
age 12-17 receiving these services.
In FY 2023, local health departments may use Title V funding on asthma related programming/services including
asthma school based management programs (in collaboration with PHPA’s Environmental Health Bureau); provide
health care education opportunities on asthma management; developing asthma regional collaboratives to
coordinate asthma related activities within the region; or partnering with CRISP (the designated Health Information
Exchange for Maryland) to strengthen linkages among pediatric care teams including school health providers,
Emergency Departments, primary care and specialists.
NPM 10: Increase the percentage of adolescents (12-17) who receive a preventive medical visit from a baseline of
81.4% (2019) to 85% by 2025.
School-Based Health Centers (SBHCs): In FY 2023, the Maternal and Child Health Bureau will formally begin
Created on 8/11/2022 at 8:37 PM
Page 124 of 296 pages

administering the Maryland School-Based Health Center (SBHC) Program. Maryland’s SBHCs represent an
essential and innovative strategy for improving the health and educational achievement of Maryland’s children and
their families. SBHCs are conveniently located where students spend the majority of their day and can therefore
address the unique needs of adolescents through increased access to medical, mental, dental and/or other health
related services. As of FY 22, there are 95 SBHCs program locations in 17 of the 24 Maryland jurisdictions. The
Maryland SBHC Program will conduct a statewide needs assessment in FY23 to inform further expansion of the
program. SBHCs will be integrated with Title V-funded programming through shared performance measures,
alignment of initiatives across the state, and coordination of services. Fourteen SBHCs also serve as Maryland
Family Planning/Title X Program subrecipient sites.
Other adolescent health programs that will continue to be supported by Title V funded staff in FY 2023 include:
Maryland Optimal Adolescent Health Program (MOAHP): In July 2020, the Maternal and Child Health Bureau,
Office of Family and Community Health Services (OFCHS) was awarded a three year federal teen pregnancy
prevention grant. Project funds will be distributed to grantees (e.g., Healthy Teen Network, Johns Hopkins University
Center for Adolescent Health, local health departments, school, and community-based programs) located throughout
the state. In year 3 , grantees will continue to offer sexual education programming to teens aged 14-19 living in
areas of the state with high rates of teen birth and sexually transmitted infections.
The teen pregnancy prevention initiative was rebranded as True You Maryland by Youth Advisory Board members
from across the state and is formally named the Maryland Optimal Adolescent Health Program (MOAHP). MOAHP
promotes equity in reaching optimal health by preventing teen pregnancy and sexually transmitted infections in rural
counties of the state by creating an infrastructure to develop and support highly effective health education and
parent/caregiver programs. MOAHP will increase the capacity of health education programs to develop students’
positive attitudes and values towards sexual and reproductive health and increase opportunities to reinforce skills
and positive behaviors. Parent/caregiver programs will increase healthy communication between adults and youth.
Healthy Teen Network (HTN) will continue to lead this effort by providing instruction and guidance to health educators
and administrators to improve program outcomes and promote the sustainability of highly effective health education
programming in Maryland.
The MOAHP consortium will continue to use the Positive Prevention Plus curriculum, which has seen a statistically-
significant delay in the onset of sexual activity and statistically-significant increases in student-parent communication
around sexual health issues. HTN will model and enforce behaviors that create an environment in which students feel
valued and emphasize individual and group norms that support optimal health-enhancing behaviors as well as
demonstrate effective instructional and behavior management strategies that support social-emotional learning.
OFCHS will continue to create networks of support for health educators and students to effectively engage youth,
parents/caregivers, and the community in MOAHP. OFCHS and HTN will partner with local school system and
community stakeholders to replicate, with fidelity, effective programs, and supportive services that are culturally and
age appropriate, medically-accurate, and trauma-informed. Johns Hopkins University Center for Adolescent Health
will evaluate and inform the program throughout the project period.
PREP: In FY 2023 the Maryland Personal Responsibility Education Program (PREP) will continue to provide
comprehensive sex education in eight (8) counties throughout the state. Jurisdictions implementing PREP activities
include Baltimore City, Allegany, Anne Arundel, Dorchester, Prince Georges, Washington, Wicomico, and Worcester
Counties. Youth will receive PREP education in middle, high school, foster care homes and detention centers across
the state. Additionally, activities also include a college-based Peer Educator model implemented on the campuses
of the University of Maryland Eastern Shore and Salisbury State University. As COVID-19 restrictions for schools
Created on 8/11/2022 at 8:37 PM
Page 125 of 296 pages
lessen, PREP programs will return to an in-person format of instruction in place of virtual lessons. Local health
departments will continue to collaborate with faith-based and community organizations to implement PREP. The
PREP program will continue to reach a minimum of 1700 youth as well as 160 parents/caregivers with a combination
of evidenced based curriculum instruction, parent education and enrichment programs.
Sexual Risk Avoidance Education (SRAE): In FY 2023 the Maryland SRAE program will continue to provide
Sexual Risk Avoidance education to middle and high school students across the state. As schools begin to re-open
for in person instruction, local health departments and community partners will begin to return to curriculum
implementation in health classes, on campus after school programs and community settings. The SRAE program will
continue to reach a minimum of 500 youth as well as 100 parents/caregivers with a combination of evidenced
based curriculum instruction, parent education and enrichment programs. A request for applications (RFA) has been
released and will determine community based grantees. Ongoing topical training and professional development will
be provided to meet the needs of program staff as a means to enhance their work.
Created on 8/11/2022 at 8:37 PM
Page 126 of 296 pages
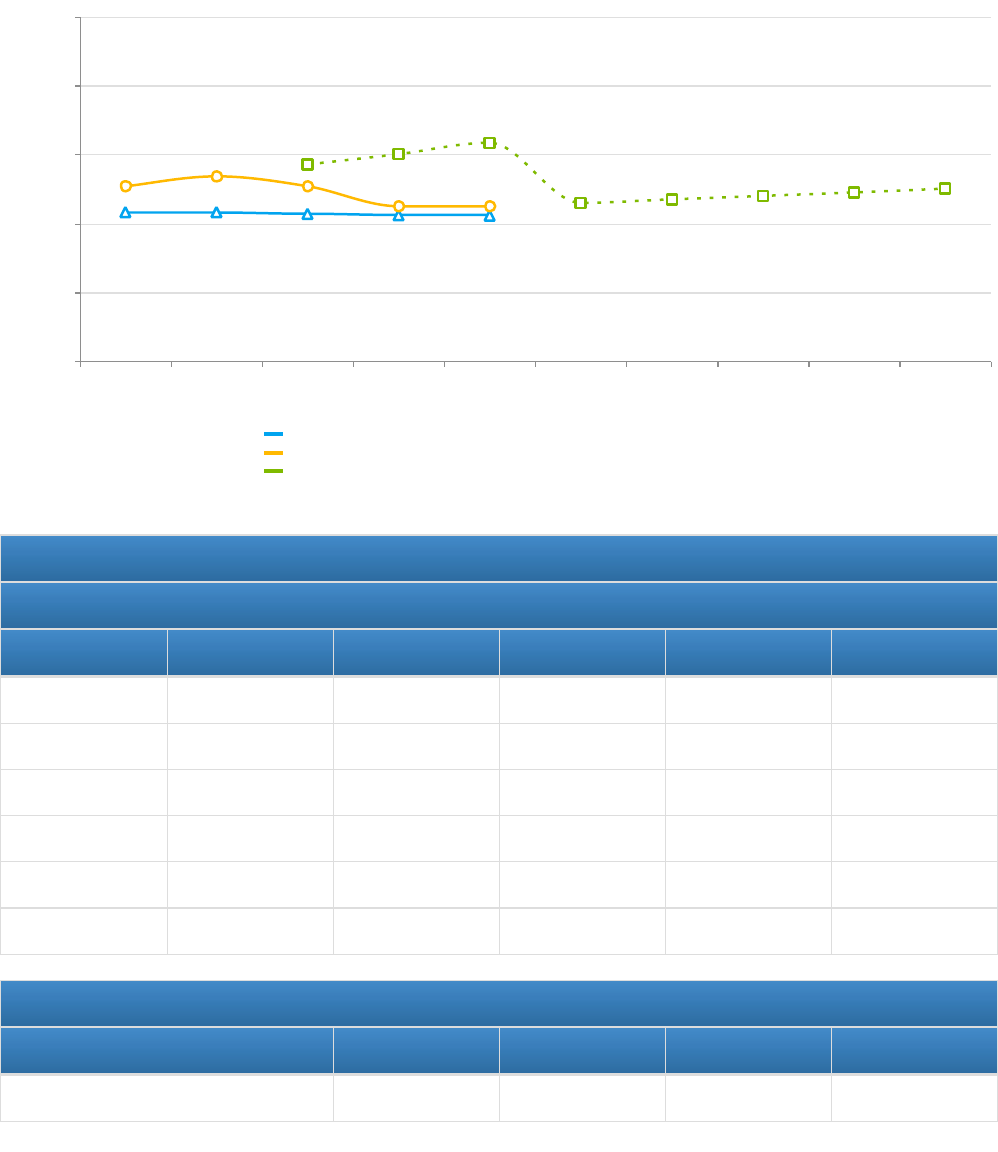
Children with Special Health Care Needs
National Performance Measures
NPM 11 - Percent of children with and without special health care needs, ages 0 through 17, who have a medical
home
Indicators and Annual Objectives
NPM 11 - Children with Special Health Care Needs
Federally Available Data
Data Source: National Survey of Children's Health (NSCH) - CSHCN
2017 2018 2019 2020 2021
Annual Objective 57 60 63.3 45.9
Annual Indicator 50.8 53.4 50.6 44.9 44.9
Numerator 127,072 137,990 130,334 117,076 122,840
Denominator 250,000 258,184 257,564 260,596 273,531
Data Source NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN
Data Source Year 2016 2016_2017 2017_2018 2018_2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 46.9 47.9 48.9 50.0
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - National Survey of Children's Health (NSCH) - CSHCN
Maryland - National Survey of Children's Health (NSCH) - CSHCN
Maryland - Objectives (CSHCN)
Created on 8/11/2022 at 8:37 PM
Page 127 of 296 pages

Evidence-Based or –Informed Strategy Measures
ESM 11.1 - Number of CYSHCN who receive patient and family-centered care coordination services
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 0 61 5,300 5,400 5,500
Annual Indicator 60 5,362 5,770 1,463 1,502
Numerator
Denominator
Data Source OGPSHCN Data OGPSHCN Data OGPSHCN Data OGPSHCN Data OGPSHCN Data
Data Source Year FY 2017 FY 18 FY 19 FY 2020 FY 2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 5,600.0 5,700.0 5,800.0 6,000.0
Created on 8/11/2022 at 8:37 PM
Page 128 of 296 pages

NPM 12 - Percent of adolescents with and without special health care needs, ages 12 through 17, who received
services to prepare for the transition to adult health care
Indicators and Annual Objectives
NPM 12 - Children with Special Health Care Needs
Federally Available Data
Data Source: National Survey of Children's Health (NSCH) - CSHCN
2017 2018 2019 2020 2021
Annual Objective 40 43 45.3 27.9
Annual Indicator 13.4 16.2 21.6 26.9 23.8
Numerator 14,817 21,034 28,923 31,754 28,346
Denominator 110,803 129,507 133,731 118,003 119,301
Data Source NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN
Data Source Year 2016 2016_2017 2017_2018 2018_2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 28.9 29.9 30.9 31.9
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
20
40
60
80
100
Percent
National - National Survey of Children's Health (NSCH) - CSHCN
Maryland - National Survey of Children's Health (NSCH) - CSHCN
Maryland - Objectives (CSHCN)
Created on 8/11/2022 at 8:37 PM
Page 129 of 296 pages
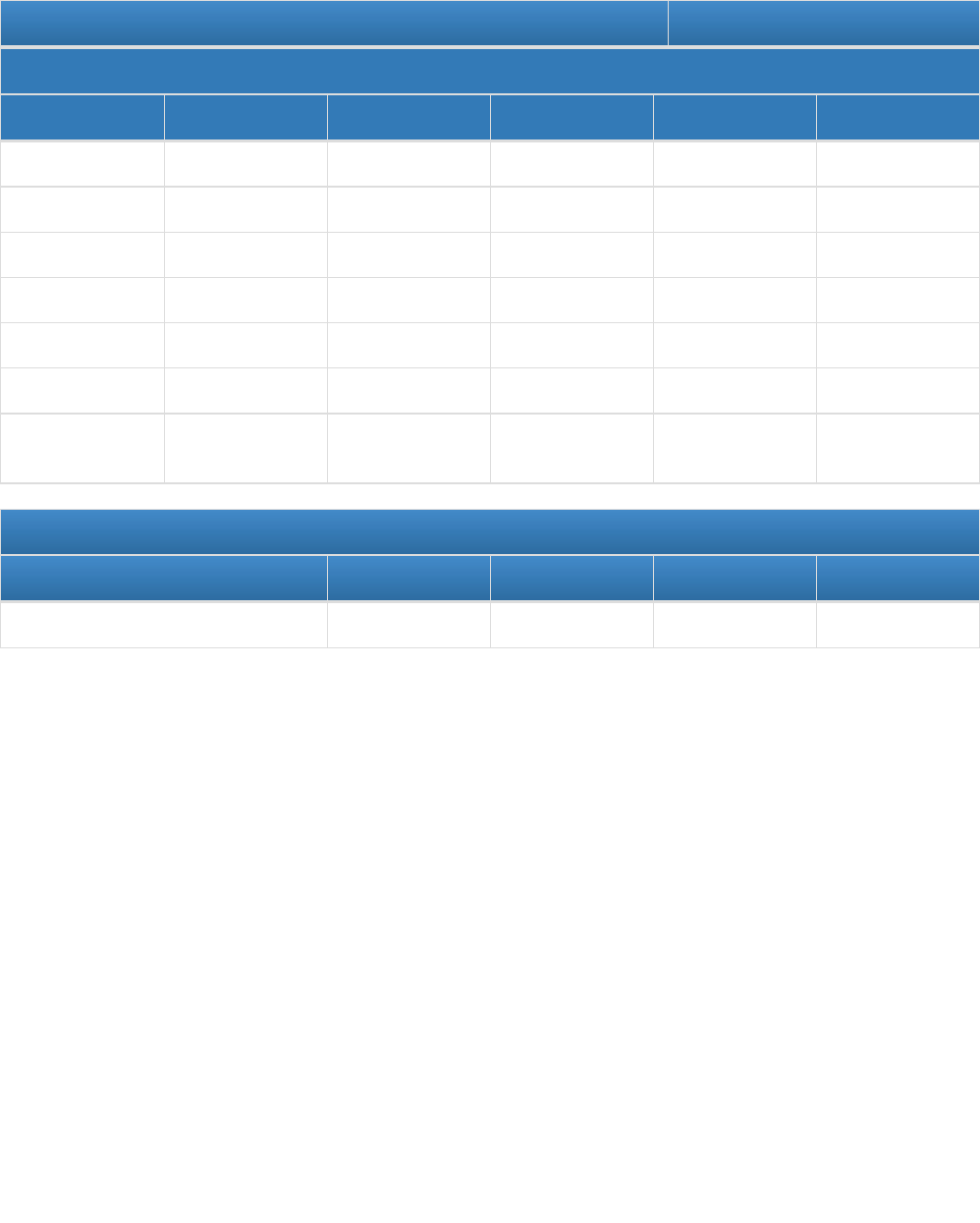
Evidence-Based or –Informed Strategy Measures
ESM 12.1 - Number of CYSCHN and their families who participate in health care transition planning activities
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 0 61 62 63 64
Annual Indicator 60 5,697 1,308 416 81
Numerator
Denominator
Data Source MCHB Data OGPSHCN OGPSHCN OGPSHCN Data OGPSHCN Data
Data Source Year FY 2017 FY2018 FY 2019 FY 2020 FY 2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 65.0 66.0 67.0 1,300.0
Created on 8/11/2022 at 8:37 PM
Page 130 of 296 pages

State Action Plan Table
State Action Plan Table (Maryland) - Children with Special Health Care Needs - Entry 1
Priority Need
Ensure optimal health and quality of life for all CYSHCN and their families by providing all services within an effective
system of care in alignment with the Six Core Outcomes
NPM
NPM 11 - Percent of children with and without special health care needs, ages 0 through 17, who have a medical home
Objectives
Increase the proportion of children and adolescents with special health care needs who receive care in a family-centered,
comprehensive, and coordinated system.
Strategies
1) Encourage implementation of the Medical Home model in pediatric primary care practices through education and
training opportunities, particularly with providers-in-training and early career providers to inform and educate about the
medical home, and to provide some practical tips on how to implement a medical home in their practice. 2) Discuss
expansion, replication, and sustainability of medical home-focused initiatives currently underway by current OGPSHCN
grantees who were awarded under the 2020 competitive request for applications. 3) Educate family members on factors of
the medical home they can control: recognizing good medical care; engaging in clear and respectful communication, and
effective advocacy for their CYSHCN 4) Conduct trainings for families on resource , identification and advocacy, 5)
Continue to seek opportunities to provide family sensitivity trainings to internal and external partners who serve CYSHCN
6) Implement a schedule to review and edit all public-facin
NOMs
NOM 17.2 - Percent of children with special health care needs (CSHCN), ages 0 through 17, who receive care in a well-
functioning system
NOM 18 - Percent of children, ages 3 through 17, with a mental/behavioral condition who receive treatment or counseling
NOM 19 - Percent of children, ages 0 through 17, in excellent or very good health
NOM 25 - Percent of children, ages 0 through 17, who were unable to obtain needed health care in the past year
ESMs Status
ESM 11.1 - Number of CYSHCN who receive patient and family-centered care coordination services Active
Created on 8/11/2022 at 8:37 PM
Page 131 of 296 pages

State Action Plan Table (Maryland) - Children with Special Health Care Needs - Entry 2
Priority Need
Ensure optimal health and quality of life for all CYSHCN and their families by providing all services within an effective
system of care in alignment with the Six Core Outcomes
NPM
NPM 12 - Percent of adolescents with and without special health care needs, ages 12 through 17, who received services
to prepare for the transition to adult health care
Objectives
Increase the proportion of adolescents with and without special health care needs who have received the services
necessary to make transitions to adult health care.
Strategies
1) Increase and enhance parent/family education and training around HCT, 2) Implement the Six Core Elements of
Healthcare Transition 3.0, 3) Promote Got Transition’s “Six Core Elements” to transition and principles of successful
transition, 4) Continue to provide information and resources for youth to young adult health care transition through the
Office of Genetics and People with Special Health Care Needs (OGPSHCN), 5) Establish a collaborative relationship with
the Governor’s Transitioning Youth Initiative (GTYI), coordinated through the Maryland Developmental Disabilities
Administration (DDA), 6) Explore strategies to engage families in the transition process for their youth with special health
care needs, 7) explore how information from the National Resource Center for Supported Decision Making and other
organizations, as well as feedback from self-advocates, can be incorporated into HCT materials, 8) review resources
related to sex education for CYSHCN, 9) Establish training prot
NOMs
NOM 17.2 - Percent of children with special health care needs (CSHCN), ages 0 through 17, who receive care in a well-
functioning system
ESMs Status
ESM 12.1 - Number of CYSCHN and their families who participate in health care transition planning
activities
Active
Created on 8/11/2022 at 8:37 PM
Page 132 of 296 pages

Children with Special Health Care Needs - Annual Report
In 2008, HRSA's Maternal and Child Health Bureau (MCHB), together with its partners, identified six core outcomes
to promote the community-based system of services mandated for all children with special health care needs under
Title V. These outcomes give us a concrete way to measure our progress in making family-centered care a reality
and in putting in place the kind of systems all children with special health care needs deserve
[1]
. The six core
outcomes are:
Families of children and youth with special health care needs partner in decision making at all levels and are
satisfied with the services they receive;
Children and youth with special health care needs receive coordinated ongoing comprehensive care within a
medical home;
Families of CSHCN have adequate private and/or public insurance to pay for the services they need;
Children are screened early and continuously for special health care needs;
Community-based services for children and youth with special health care needs are organized so families
can use them easily;
Youth with special health care needs receive the services necessary to make transitions to all aspects of adult
life, including adult health care, work, and independence.
For the 2021-2025 MCH Block Grant needs assessment reporting cycle, Maryland identified, “ensuring optimal
health and quality of life for all children and youth with special health care needs and their families by providing
services within an effective system of care in alignment with the six core outcomes” as a continued State Priority.
National priority measures and associated evidence-based strategy measures selected for programmatic focus to
impact this overarching state priority were:
NPM 11: Medical Home
Percent of children with and without special health care needs, ages 0 through 17, who have a medical home
ESM 11.1: Number of CYSHCN who receive patient and family-centered care coordination services
NPM 12: Transition
Percent of adolescents with and without special health care needs, ages 12 through 17, who received
services to prepare for the transition to adult health care
ESM 12.1: Number of CYSHCN and their families who participate in health care transition planning
activities
Medical Home
The National Survey for Children’s Health reported in their 2018-2019 data that 44.9% of children ages 0-17 with
special health care needs have a medical home, compared to 46.4% of children ages 0-17 without special health
care needs.
Maryland recognizes that the medical home approach to providing comprehensive and high-quality primary care is
the best practice for children with and without special health care needs. Despite the model’s introduction fifty years
ago, limited progress has been made in universal implementation.
Health Care Transition
The National Survey for Children’s Health reported in their 2019-2020 data that 23.8% of adolescents age 12-17
with special health care needs received services necessary to make transitions to adult health care, compared to
Created on 8/11/2022 at 8:37 PM
Page 133 of 296 pages
15.8% of adolescents age 12-17 without special health care needs.
Maryland continued the overarching goal of increasing the percent of adolescents with and without special health
care needs who have received the services necessary to make transitions to adult health care.
State Fiscal Year 2021
The Office for Genetics and People with Special Health Care Needs (OGPSHCN) is MDH’s Children and Youth with
Special Health Care Needs (CYSHCN) office. OGPSHCN is housed in the Prevention and Health Promotion
Administration’s Maternal and Child Health Bureau and includes five programs:
Children’s Medical Services
Early Hearing Detection and Intervention
Newborn Screening Follow-Up and Critical Congenital Heart Disease Surveillance
Operations and Support
Systems Development, which includes
Birth Defects Surveillance
Sickle Cell Disease Long-term Follow Up
CYSHCN Title V Block Grant Coordination
Grants to local health departments, community-based non profit organizations, and academic
clinical centers
Internal projects
OGPSHCN served 17,380 CYSHCN and their families through Title V-supported programs and efforts in SFY2021.
This figure reflects counts of unduplicated children and/or families served through direct health care services or
enabling services.
In SFY2020 and SFY2021, OGPSHCN engaged in an intensive review of the internal process for awarding grants. In
conjunction with a greater focus on competitive procurement processes from Department leadership and an effort to
maintain fidelity to MCH Block Grant Program goals, OGPSHCN leadership took a significant portion of the year to
analyze and edit the Request for Applications (RFA) for Systems Development grants. This included multiple
strategic planning meetings with staff at all levels, consultation with the Administration's Office of Procurement and
countless drafts and revisions. Secondary to the COVID-19 pandemic, SFY2020 funding to local health departments
and certain other grantees was extended through the first quarter of SFY2021. The final competitive RFA,
“Strengthening Systems of Care for Maryland’s Children and Youth with Special Health Care Needs,” was posted in
July 2020, with the first segment of the anticipated 3-year grant cycle being shortened to quarters 2, 3 and 4 (October
1, 2020 to June 30, 2021). These grant awards were eligible for continued funding for two subsequent years upon
satisfactory completion of project objectives and at OGPSHCN’s discretion.
In their submissions, applicants were required to select at least one “focus area” corresponding to one of the core
outcomes identified by HRSA as critical indicators of success in implementing community-based systems or
services for CYSHCN (Table 1). Projects could incorporate elements of more than one focus area but were required
to identify one as primary.
Table 1. Focus Areas from Maryland's CYSHCN Request for Applications
Created on 8/11/2022 at 8:37 PM
Page 134 of 296 pages
Focus Area Corresponding Core Outcome
Family
Professional
Partnership
Families of CYSHCN partner in decision making at all levels and
are satisfied with the services they receive.
Medical Home
Implementation
CYSHCN receive coordinated ongoing comprehensive care within a
medical home
Health Care
Transition
YSHCN receive the services necessary to make transitions to all
aspects of adult life, including adult health care, work, and
independence.
Workforce
Development
The RFA also noted that while projects employing direct or indirect/enabling service provision would be considered,
the driving force was the need for high-yield efforts that impact systems and translate into meaningful benefits for
Maryland’s CYSHCN.
The RFA further stated:
The Federal Health Resources and Services Administration’s (HRSA’s) Title V Maternal and Child Health
Services Block Grant Program (CFDA No. 93.994) provides funding to States to support infrastructure
building for systems of care. The conceptual framework for maternal and child health services under the
Title V Block Grant is envisioned as a pyramid with four tiers of services: Direct Services (top of pyramid),
Enabling Services, Population-Based Services, and Infrastructure-Building Services (bottom of pyramid).
Population-Based Services and Infrastructure-Building Services serve as the base of the pyramid and are
the primary focus of this RFA. An overarching goal of all projects should be to build capacity and
strengthen systems―capacity of families to manage and coordinate complex systems of care for their
CYSHCN; capacity for youth to transition from pediatric to adult care and to live as independently as
possible; and capacity of providers to provide comprehensive, coordinated, culturally effective, and
consumer-friendly care.
During SFY2021, the budgeted amount for the CYSHCN grants was $1,101,811 compared to $1,174,605 in
SFY2020. The reason for the decrease for these grants is to accommodate other CYSHCN initiatives including Child
Medical Services and preventive and child health programming through the Child Health Improvement Systems.
OGPSHCN received and evaluated applications from community-based organizations, local health departments,
and university centers. After the evaluation process was complete, a total of six grants were awarded for Quarters 2,
3 and 4 of SFY2021.
Table 2. SFY2021 / Q2-4 OGPSHCN Grantees
Grantee Focus
Area(s)
Project Description
Children’s National
Medical Center Parent |
Family
Professional
Provide peer to peer support to families of
Maryland children with special health care
Created on 8/11/2022 at 8:37 PM
Page 135 of 296 pages

Navigator Program Partnership needs followed in the Goldberg Center for
Community Pediatric Health and the Complex
Care Program.
Build on existing community education
programs at Children's National and develop
targeted transition and educational programs
for both community primary care pediatricians
and staff and pediatric trainees through a
partnership with Children's National clinically
integrated network, the Pediatric Health
Network (PHN)
National Alliance to
Advance Adolescent
Health
Healthcare
Transition
Increase school mental health professional
training in evidence-informed transition
practices and replicate a new school mental
health transition
initiative modeled after Got Transition’s Six
Core Elements of Health Care Transition.
Ensure expanded access to transition
supports via school mental health programs
The Coordinating Center Medical
Home
Expand on the VIPhysicians&Kids pilot
program, which received OGPSHCN funding
in FY2020)
VIPhysicians&Kids is The Coordinating
Center’s exclusive, medical home service for
families with CYSHCN. Patients of pediatric
practices enrolled in VIPhysicians&Kids have
access to the VIPhysicians&Kids Care Team.
The Care Team supports the development of
a shared care plan that is centered on
achieving personal goals. The Care Team
supports practices so that providers can focus
on medical treatment for their patients, and
families can focus on parenting their children,
while the Care Team works to resolve issues
that impact the patient’s health.
The Center aims to increase the number of
participating practices from two to five (with
one focused on Sickle Cell), strengthen the
family professional partnership, and develop
strategies to become a scalable, replicable
and sustainable model supported by
practices, health care systems and third-party
Created on 8/11/2022 at 8:37 PM
Page 136 of 296 pages

payers once the grant has ended.
Baltimore County Health
Department
Family
Professional
Partnership
Improve family professional partnerships in
Baltimore County by utilizing several
strategies including: care coordination,
education of families, needs assessments
through focus groups, education through
provider toolkits and expansion of emergency
preparedness efforts for CYSHCN
Calvert County Health
Department
Medical
Home
Coordinate with the Calvert County Behavioral
Health Services to provide a patient-centered
behavioral health medical home to families of
infants under two years old whose parents
have a history of substance use disorder,
severe mental health disorder and/or
homelessness.
Use an intensive case management model,
with monthly contacts to families and twice
monthly support meetings. Families will be
directed to needed financial resources and
workforce-development resources. Families
will be taught the components of the medical
home model so that they can develop a
patient-centered medical home with adult and
primary care providers. Appointment
compliance will be monitored from the
participating family member and the child’s
well visits, and the child will be continuously
screened for developmental and immunization
delays.
For other CYSHCN from birth to age 12 who
are not currently being case managed by
another source, resource assistance and
case management will be provided as
needed, including educating families in the
benefits of a patient-centered medical home.
Talbot County Health
Department
Medical
Home,
Family
Professional
Partnership,
and Health
Care
Transition
Create a systematic approach for the
transition of care coordination competencies
to families of CYSHCN and the Medical
Home.
Regional systems approach focusing on
addressing gaps and barriers will overlap to
support these efforts
Additional FY21 / Q2-4 (not awarded as part of the aforementioned RFA) Grantees were:
Created on 8/11/2022 at 8:37 PM
Page 137 of 296 pages

The Arc Montgomery County: Supporting the Karasik Family Infant & Child Care Center, a fully inclusive
childcare program for children 6 week to 10 years old with and without special health care needs and
disabilities.
Clinical genetic centers: These awards provided continuous consultation support to OGPSHCN Newborn
Screening Follow-Up Program and clinical care to Maryland children identified by newborn screening.
Children’s National Medical Center, Division of Genetics and Metabolism - To support operation of
the Genetics and Newborn Screening Follow-up program.
Johns Hopkins University, McKusick-Nathans Institute of Genetic Medicine - To provide genetic
services through The Johns Hopkins University Department of Genetic Medicine.
Kennedy Krieger Hospital-Biochemical Genetics Laboratory - To provide diagnostic and follow-up
testing for metabolic disorders identified by the Maryland newborn screening program and for other
metabolic conditions not identified by the newborn screening process.
University of Maryland, Baltimore - To provide diagnostic and long-term follow-up for CYSHCN
identified by newborn screening.
OGPSHCN continued to monitor and review reporting requirements from all grantees to ensure fidelity to
Department goals and grant agreement scopes of work, while also planning for future iterations of the request for
applications to be posted and the work that needs to be done across the state.
In SFY2021, Maryland’s Title V Program continued to structure activities around the six core systems outcomes
developed in 2008 by HRSA's Maternal and Child Health Bureau (MCHB) for CYSHCN including:
Family-Professional Partnership
Medical Home
Adequate Insurance
Early and Continuous Screening
Easy-to-Use Services and Supports
Youth Transition to Adult Health Care.
Family-Professional Partnership
During FY21, OGPSHCN built upon previous efforts to enhance family engagement and family-professional
partnership (FPP) by assessing internal programs and identifying opportunities for change.
OGPSHCN’s Parent Resource Coordinator position was staffed from July 1, 2019 to mid-December, 2019. During
that time the Parent Resource Coordinator, who is also a parent of YSHCN, served to help families find local and
State resources for their child, and to provide education and training to families of CYSHCN. Upon her departure,
OGPSHCN engaged in a thorough search to fill the Parent Resource Coordinator position, hindered by the fact that
State guidelines do not allow targeted recruitment of specific groups (in this case, a parent/caregiver of a CYSHCN
or a former CYSHCN). In the absence of a dedicated FPP “expert,” the Systems Development Program Chief, the
Health Care Transition and Medical Home Coordinator and the OGPSHCN Deputy Director all participated in FPP
efforts and in helping families find appropriate resources, while additional office staff also participated in various
Created on 8/11/2022 at 8:37 PM
Page 138 of 296 pages

ventures pertaining to CYSHCN.
OGPSHCN staff hold administrative responsibility for the coordination of several state-wide advisory committees,
including: the Advisory Council to the Maryland Early Hearing Detection and Intervention Program; the Advisory
Council on Hereditary and Congenital Disorders; and Statewide Steering Committee on Services for Adults with
Sickle Cell Disease. Each of these committees mandates some degree of membership from those with lived
experience, either parents/caregivers, affected adults, or some combination thereof. In addition to staffing the
aforementioned committees, OGPSHCN staff served as members of numerous advisory councils as the expert
voice on CYSHCN, a person with lived experience, or in a clinical advisory role. Those committees include: Maryland
Commission on Caregiving; Mortality Quality Review Committee, Maryland Developmental Disabilities Council,
Youth Camp Advisory Council, Sinerge (Northeast Sickle Cell Grant Collaborative) Advisory Board, ASH-CTN (ASH
RC Sickle Cell Disease Clinical Trials Network) Community Advisory Board, Disability Health Inclusion Program
Advisory Committee, United Healthcare Community Advisory Council, Traumatic Brain Injury Advisory Board and
Charting the Lifecourse Community of Practice Leadership Team.
OGPSHCN staff are always striving to improve understanding of successful Family Professional Partnership and to
discover and implement new best practices. To that end, staff members attended various professional development
opportunities focused on FPP and family engagement, including the June 2021 Family Voices Leadership
Conference and multiple other webinars and workshops. In January 2021, the Maryland Maternal and Child Health
Bureau (MCHB) initiated a series of “Bureau Month” trainings, including a session on Incorporating the Community
Voice, and in February 2021, initiated the MCHB Equity Workgroup which includes staff representation from all
Bureau Offices, including OGPSHCN.
As a parent of CYSHCN, the OGPSHCN Deputy Director was also once again invited by The American Academy of
Pediatrics (AAP) to participate in the Managing Students with Seizures ECHO (Extension for Community Health
Care Outcomes), a multi-cohort learning opportunity and forum for health care professionals to learn and improve
access to quality healthcare for children and youth with epilepsy. The OGPSHCN Deputy Director served as the
“parent voice” faculty from January 2021 through June 2021, working alongside and presenting to clinical
professionals to ensure that the family voice was heard. Additionally, the Deputy Director presented on “Supporting
Families in Telehealth Visits for Epilepsy” for the Access Improvement and Management for Epilepsy through
Telehealth ECHO for the AAP National Coordinating Center for Epilepsy.
The Deputy also participated in the AMHCP Family Engagement Community of Practice (CoP), the goal of which
was to increase Title V capacity to engage families in their work. The CoP provided a platform to share ideas,
innovations, lessons learned, successes, and best practices from subject matter experts. The CoP cohort explored
topics including: Intersection of equity and family engagement; Challenges/barriers of availability of family members
able to participate in training, public awareness, and policy development; Engaging/partnering with families without
additional funding or increased funding levels for programs; and discussion on institutionalizing family engagement
and reaching younger families.
In September 2020, the Deputy was invited to serve as an advisor and speaker for the Maryland “Launching Family
and Youth Engagement” project from the Maryland Chapter of the American Academy of Pediatrics (MDAAP). The
project was funded by a Family Engagement Chapter Grant from the The FamilY Partnerships Network. Over the
course of several months, family engagement experts, including the OGPSHCN Deputy Director, presented at an
Initial kickoff meeting, a MD AAP Board meeting and a general membership meeting to introduce strategies of
family engagements, implementation and evaluation tools, and map next steps.
From December 2020 through March 2021, the Deputy participated in the Family Voices Telehealth CARES Act
Created on 8/11/2022 at 8:37 PM
Page 139 of 296 pages

Community of Practice (CoP) in partnership with The Parents’ Place of Maryland (PPMD). PPMD is Maryland’s
Parent Training and Information Center, Family-to-Family Health Information Center and Family Voices State Affiliate
Organization. The purpose of the CoP was to share and discuss best practices around the delivery of telehealth
including strategies for reaching families who are diverse, vulnerable, medically underserved and hard to reach.
During previous grant cycles, OGPSHCN provided funding to PPMD to provide one-on-one assistance and
navigation services to families around the core outcomes of Medical Home and Health Care Transition. As part of
this funding, PPMD coordinated the statewide Maryland Community of Care Consortium (CoC), a working group of
diverse stakeholders, including families, providers, advocates, consumers, administrators, and professionals from
the public and private service systems. Using the national agenda for CSHCN and core outcomes as a starting
point, the CoC worked to create systems of care that promote optimal health, functioning, and quality of life for
Maryland CSHCN and their families. Membership in the CoC was open to anyone with an interest in improving the
systems of care and family members were particularly encouraged to join. In FY20, there were three separate
Community of Care Consortia (statewide, Southern Maryland, and Eastern Shore).
In FY2021, there was one Community of Care Consortia in the Eastern Shore and was supported by one of the
region’s local health departments. State Title V staff had planned to coordinate a Statewide CoC but due to the
pandemic and staffing transitions, it was unable to occur.
Additionally, several of the aforementioned SFY2021 grantees indicated Family Professional Partnership as a
primary or secondary focus area.
The Talbot County Health Department, which has coordinated the aforementioned Eastern Shore CoC for many
years through funding from OGPSHCN, also planned a tiered approach to create a systematic transition of care
coordination competencies to families of CYSHCN and the Medical Home. In response to the OGPSHCN request
that proposed projects focus on Population-Based Services and Infrastructure-Building Services, Talbot County
devised a plan to identify families with the highest need for intervention and implement a tiered system of family
education. In SFY2021, Talbot LHD served 102 CYSHCN utilizing this tiered approach.
Baltimore County Health Department proposed and implemented a project to improve family professional
partnerships in Baltimore County by utilizing several strategies including: care coordination, education of families,
needs assessments through focus groups, education through provider toolkits and expansion of emergency
preparedness efforts for CYSHCN. This project served 84 CYSHCN in SFY2021.
Finally, the Parent Navigator Program at Children’s National Medical Center in Washington DC helps to reduce
family stress by providing peer-to-peer support and connecting parents or caregivers to resources, assisting with
care navigation, finding educational tools for parents and children, and providing emotional support so that managing
a child’s healthcare journey is a little easier. The navigators are parents of CYSHCN and bring a unique perspective
and understanding to every parent enrolled in the program. In SFY2021, Parent Navigators provided support and
assistance to the families of 121 CYSHCN. The Parent Navigator Program was a previous grantee of OGPSHCN. In
response to the RFA guidance to focus on building capacity and strengthening systems, the Program developed a
proposal to build on existing community education programs and materials and develop targeted transition and
educational programs for both community primary care pediatricians and staff and pediatric trainees through a
partnership with Children's National clinically integrated network, the Pediatric Health Network (PHN)
Medical Home
In FY2021 OGPSHCN continued to focus on expanding awareness of the medical home model through educating
Created on 8/11/2022 at 8:37 PM
Page 140 of 296 pages

families, training providers and developing new partnerships around the state. The Medical Home (MH) Coordinator
conducted outreach efforts and dissemination of information across the state through workshop presentations at The
University of Maryland and at Kennedy Krieger Institute, participation in planning and presenting at the state-wide
School Health Interdisciplinary Program (SHIP) conference, and attendance at community resource fairs and other
outreach opportunities. The COVID-19 Pandemic greatly reduced the opportunities to attend in-person events, which
so many outreach efforts are, but as sponsoring organizations shifted their events to the virtual environment, the MH
Coordinator was also able to pivot to this different style of outreach and engagement. A total of 225 individuals were
educated on Medical Home implementation within their respective roles. In particular, the presentation at the SHIP
conference educated school health staff on the Medical Home model, what a patient-centered MH looks like, and
their role in coordination of care for CYSHCN. The participation with SHIP conference planning and implementation
exhibits a cohesiveness between multiple OGPSHCN-funded grantees and office staff, as it supports several priority
focus areas. The MH Coordinator additionally provided technical assistance and resources in support of medical
home implementation to local health departments and pediatric provider practices, school health professionals and
educational medical institutions.
With OGPSHCN’s shift to the new RFA, increased competitiveness in the procurement process, and budget
limitations not as many grants were awarded in FY21 as in previous years. Local Health Departments (LHDs) were
particularly impacted by these changes. In FY20, OGPSHCN provided funding to CYSHCN programs in 13 of
Maryland’s 24 LHDs; programs that utilized nurse care coordinators to provide care coordination services to
CYSHCN in their respective jurisdictions in support of a Medical Home model of care. In anticipation of SFY2021,
LHDs and community-based non-profit organizations (CBOs) were evaluated and awarded funds based on the
same competitive RFA. Those that indicated Medical Home as a primary or secondary focus area include The
Coordinating Center, Calvert County Health Department and Talbot County Health Department.
The Coordinating Center (TCC) expanded on the VIPhysicians&Kids pilot program (which received OGPSHCN
funding in FY2020), an exclusive, medical home service for families with CYSHCN. Patients of pediatric practices
enrolled in VIPhysicians&Kids have access to the VIPhysicians&Kids Care Team. The Care Team supports the
development of a shared care plan that is centered on achieving personal goals. The Care Team supports practices
so that providers can focus on medical treatment for their patients, and families can focus on parenting their children,
while the Care Team works to resolve issues that impact the patient’s health. In SFY2021, the Center added three
new practices, the Pediatric Sickle Cell Program at The Herman & Walter Samuelson Children's Hospital at Sinai
Hospital, the University of Maryland Children’s Hospital Behavioral and Developmental Pediatrics Division, and
Dundalk Pediatric Associates to the program, which served a total of 75 unduplicated CYSHCN.
Calvert County Local Health Department proposed an intensive case management model to provide a patient-
centered behavioral health medical home to families of infants under two years old whose parents have a history of
substance use disorder, severe mental health disorder and/or homelessness. Implementing this intensive model, the
LHD provided case management services to the families of ten CYSHCN. Additionally, this LHD proposed resource
assistance and case management on an as needed basis, including educating families in the benefits of a patient-
centered medical home, for CYSHCN from birth to age 12 not currently being case managed by another source.
Created on 8/11/2022 at 8:37 PM
Page 141 of 296 pages

Through implementation of a triage system, Talbot County Local Health Department, proposed a tiered system
of determining family/CYSHCN needs and providing care coordination services based on identified level of need,
while beginning the process of educating and assisting families to manage care coordination independently. The
Children with Special Health Care Needs (CSHCN) Screener© - developed by the Child and Adolescent Health
Measurement Initiative (CAHMI) - was used to identify level of need. The CHSCN Screener© is a five item, parent
survey-based tool by which children are identified on the basis of experiencing one or more current functional
limitations or service use needs that are the direct result of an on-going physical, emotional, behavioral,
developmental or other health condition. The county also made use of the KS-CYSHCN “Holistic Care
Coordination
[2]
” model to assist families in navigating health care systems by first assessing individual needs, then
tailoring support to meet those needs. A portion of the funding to Talbot County LHD focuses on regional
infrastructure building, regional consultations and special projects, including support for the aforementioned Eastern
Shore CoC. For FY 21, a total of 101 youth were served,
Not funded as part of the ‘Strengthening Systems of Care for Maryland’s Children and Youth with Special Health
Care Needs’ RFA, but still supporting the Medical Home model:
The Arc Montgomery County Karasik Family, Infant & Child Care Center (KFICCC) is a fully inclusive
childcare program for children 6 weeks to 10 years old with and without special health care needs and disabilities.
The program provides various services including childcare, special education, nursing, therapies, PreK, and family
resources in a single location. KFICCC's medical home model provides services in four areas: 1) nursing care and
monitoring; 2) developmental growth; 3) education; and 4) family support. They provided service support to 27
families and provided 26 professional and cultural sensitivity staff development training for the staff. They provided
services to 31 (unduplicated) CYSHCN youth.
While other grantees did not specify Medical Home as a primary area of focus, arguably all grantees are working
toward components of the Medical Home model.
Children's National Medical Center supports the MH model by providing integrated access to services and care
coordination for Maryland’s CYSHCN through Parent Navigator and Complex Care Programs. The navigators
provide peer-to-peer support for families and share knowledge and resources for families to effectively navigate their
health care system. The Complex Care Program supports medical homes by bridging the gap between primary care
providers and tertiary services. In SFY2021,175 families were served through the Parent Navigator and Complex
Care Programs, and 311 individual CYSHCN received care coordination services.
OGPSHCN also continued to provide funding for clinical genetics services to the University of Maryland, Children’s
National Medical Center, John Hopkins University, and the Kennedy Krieger Institute Biochemical Genetics
Laboratory. These genetics services are provided, in furtherance of medical home concepts, to reduce or prevent
adverse outcomes from heritable conditions; provide opportunities for CYSHCN and their families to receive
services necessary to manage genetic conditions; offer culturally-competent and family-oriented services; and
increase the number of primary care, specialty care, and other related providers who are informed about genetic
contributions to health and illness and able to apply of genetic information to improve the health of individuals and
families in their care. In FY 2021, 6,174 children and their families received clinical genetic services.
Adequate Health Insurance
OGPSHCN’s Children’s Medical Services (CMS) Program pays for specialty care for qualifying CYSHCN who are
underinsured or uninsured and whose family income does not exceed 200% of the federal poverty level. In FY2021,
the CMS Program processed 265 applications, determined that 184 CYSHCN were eligible for services, and paid
for services for 537 CYSHCN. Relative to FY2020, these figures represent a 3.8 percent increase in applications, a
Created on 8/11/2022 at 8:37 PM
Page 142 of 296 pages

3.8 percent increase in eligible CYSHCN, and a 4.8 percent increase in CYSHCN served. In addition to the fee-for-
service payment structure, the CMS Program also purchased health insurance for 41 of the 537 eligible children,
which represented a 7.8 percent increase from FY20. Insurance coverage was purchased for children with the
costliest diagnoses so these children could receive health services that were more comprehensive than those
covered by the CMS Program, such as general pediatric care, sick visits, emergency room visits and admissions,
dental, vision and mental health services. The CMS Program covered the cost of health insurance premiums as well
as costs of co-pays, co-insurance and deductibles. Additionally, there was one insurance-enrolled child enrolled in
the Kaiser Permanente’s Community Health Access Program. For this child, the CMS Program paid for services not
covered by the Community Health Access Program.
The open enrollment period for health insurance plans occurs over a limited period and represents the only time in
which health insurance can be purchased for the upcoming year. Since enrollment into the CMS Program occurs
throughout the year, the CMS Program continued to cover the cost of care and services for children deemed
appropriate for purchase of health insurance plans but who could not be enrolled until the open enrollment period.
During the last 4 months of FY2021, no child was disenrolled from the CMS Program as a result of the Governor’s
Executive Order extending eligibility during the COVID-19 Pandemic State of Emergency. Existing enrollees
remained eligible until 30 days after termination of the State of Emergency. The state of emergency terminated on
July 15, 2021, thus the eligibility extension ended on August 15, 2021.
The CMS Program is the costliest program within OGPSHCN, and SFY2021 proved true to that rule. Extended
eligibility secondary to the COVID-19 Pandemic State of Emergency resulted in the highest number of children
enrolled in CMS since its inception. The range of diagnoses enrolled children have results in variable treatment plans
and medication costs, making it challenging to predict annual allocation amounts even when not in a state of
emergency. The cost of one prescription for one child can conceivably deplete the entire budget. CMS, OGPSHCN
and MCHB leadership engaged in several ‘brainstorming’ sessions in SFY2021 to discuss strategies for cost
containment. OGPSHCN contacted The Catalyst Center to discuss opportunities for technical assistance or other
support. Unfortunately, competing priorities stalled those conversations in SFY2021, but that is something we hope to
pursue in the future.
Early and Continuous Screening
Newborn Screening (NBS)
Newborn screening in Maryland is performed using a two-screen method. The first being obtained at greater than 24
hours of age and after the infant has received 24 hours of feeding, and the second at 10-14 days of age. To
differentiate between a newborn and a subsequent specimen, the laboratory identifies all specimens collected at
less than 7 days of age as a newborn specimen and specimens collected over 7 days of age as a subsequent
specimen.
In CY 2021, a total of 73,009 babies have been identified as having a specimen collected in the newborn period,
identified as less than 7 days of age. In previous reports, the number of refusal notifications have been used to
identify babies who have not been screened. However, secondary to a network security incident at the beginning of
December 2021, this data is inaccessible at this time. Additionally, the Maryland State Newborn Screening
Laboratory has not been able to perform any of the newborn screening testing for Maryland babies since December
3, 2021. Specimens received as of December 1, 2021, are being sent to an outside laboratory for evaluation and
results are returned to Maryland.
Created on 8/11/2022 at 8:37 PM
Page 143 of 296 pages

The total number of babies screened is higher than the total recorded births in Maryland which is most likely
secondary to the potential overlap of specimens received between December 1st and December 3rd and the
inability to filter the data received from the outside laboratory to exclude babies born to military facilities out of state
and overseas. Additionally, the outside laboratory is not currently linking multiple specimens from one baby together.
Although efforts have been made to verify each record is for a unique baby, there may still be some duplication in the
babies screened in December 2021.
FY21 marks the completion of the first year and a half of the addition of DNA for cystic fibrosis (CF) to the newborn
screen. Maryland has retained the two-screen process in screening for CF using an IRT/IRT/DNA model, unless the
initial IRT is over 200 which results in DNA being tested on the initial specimen. The DNA panel usually performed on
the second elevated IRT specimen consists of 60 mutations, determined through consultation with our pulmonology
specialist to be the most common mutations in our population. Since Maryland has remained a two-screen state, the
NBS Follow-up program is notified of the initial elevated IRT result only if DNA was tested and was positive or if a
routine repeat specimen has not been received on the infant.
If there is no repeat specimen received by the laboratory at 3 weeks of age to rescreen the IRT, the NBS Follow-up
program is notified and then identifies and locates the infant in order to determine if a repeat specimen has been
collected and may still be in transit to the lab or if a repeat specimen is still needed. Since the cut-off for IRT was
reduced as well with implementation of DNA, the number of babies who had elevated IRTs on the first screen
increased resulting in a substantial increase in the number of babies reported for follow-up for an initial IRT
elevation. This increase in the number of babies reported has been further exacerbated by the U.S. Postal service
delays, which have resulted in repeat specimens not being received until 3.5-6 weeks of age. The NBS Follow-up
program is currently working with the NBS laboratory to determine the best timing for notification to reduce burden on
the follow-up team and ultimately to eliminate undue anxiety on the part of the family. More in depth data analysis and
discussion with our pulmonology specialists is also needed to determine if the IRT cut-off needs to remain at 60 with
the addition of DNA; the previous cut-off was 100, without DNA.
In FY21, the multiplexed screening for the lysosomal storage disorders (LSD) consisting of Pompe,
Mucopolysaccharidosis Type 1 (MPS-1) and Fabry Disease continues to identify a large number of pseudo
deficiencies in both Pompe and MPS-I. Further analysis of cut-offs related to final diagnosis is needed to further
refine the screening process to reduce this false positive rate, particularly in the absence of second tier testing.
The timeframe for implementation of screening for X-Linked Adrenoleukodystrophy (X-ALD) remains unknown at this
time. X-ALD was approved in September 2016 for inclusion on the Maryland Newborn Screening panel when the
laboratory has the financial and personnel resources necessary for implementation. Since screening for X-ALD
cannot be multiplexed with any of the other disorders and requires purchase of dedicated equipment, this
implementation has been delayed. The NBS laboratory has initiated the procurement process for the equipment at
this present time.
The total number of babies requiring follow-up services for metabolic newborn screening in CY21 is 1993 babies.
NBS short-term follow-up services are provided by staff consisting of the program chief and two full-time nurses. The
nurses provide consultation with hospitals, primary care providers and specialists regarding results obtained through
newborn metabolic screening, as well as reporting unsatisfactory specimens. Cases are followed and updated until
there is a confirmed diagnosis or final resolution of the case. The team of nurses share 24/7 on-call responsibility,
including weekends and holidays. Since teleworking during the COVID-19 pandemic proved to be a relatively
seamless transition, the nurses are continuing to telework three days per week and working in the office two days per
week to foster relationships with NBS laboratory staff.
Created on 8/11/2022 at 8:37 PM
Page 144 of 296 pages

Critical Congenital Heart Disease (CCHD) Screening Program
OGPSHCN conducts surveillance for the Critical Congenital Heart Disease (CCHD) Screening Program. The
CCHD screening results and follow-up actions are completed prior to the baby’s discharge from the hospital and
entered the OZ Systems database by birth facilities. The CCHD screening data is used to identify variations in
hospital compliance and to determine final diagnosis for abnormal screens. In CY21, there were 64,859 reported
births in the OZ database that are listed as eligible for CCHD screening, and 54,772 babies reported as being
screened for CCHD. The combined screening rate for the state is 84.5%. This screening rate has decreased since
the last reporting period, which was 92.1% in CY20. A more extensive review of the data will be conducted to
determine if the decrease is an overarching problem with the documentation of CCHD results into the database or a
concentrated problem at a few birth facilities of the screened babies, 11 babies are documented as failing the
CCHD screen, one of which has a critical congenital heart defect that was not suspected prenatally or clinically prior
to screening. The remainder of these babies had non-critical cardiac defects, delayed transition or pneumonia. Of
note, 21 babies were documented as having a critical congenital heart defect identified either prenatally or clinically
prior to screening, indicating prenatal screening and postnatal assessment remains a vital part of identification of
critical congenital heart defects.
Review of the most recent CCHD data reveals that birth facilities may be over utilizing the category of Physician
Override. This category was created for babies who had an ECHO already performed secondary to findings on a
prenatal ultrasound or for babies who require urgent attention clinically. If the Physician Override category is chosen,
the birth facility must choose a reason why the override is performed. Of the 158 cases documented as Physician
Override, 71 of these cases are identified as having no prenatal suspicion of a cardiac defect, with 34 cases
documented as not having clinical symptoms either. Education efforts with the birth facilities need to focus on
documentation in general, as well as clearly defining the category of Physician Override.
Sickle Cell Disease Follow up Program
OGPSHCN’s Sickle Cell Disease Long-Term Follow up Program follows children diagnosed with sickle cell disease
through age 18. The program continues to focus on childhood preventive care standards and provide education and
assistance through transition into adulthood. In FY21 563 children were being followed in the program. In May 2015,
a pilot parent mentor program was formed to assist parents of newborns with sickle cell disease. This program
continues to grow and develop as new parent mentors are added. In November of 2018, the program conducted a
survey of providers to determine awareness of and preparation to discuss Sickle Cell Trait (SCT) testing outcomes,
via Newborn Screening, and health concerns with families. The outcome showed that while most providers were
aware of SCT potential health risks, the breadth of knowledge was limited. This lead OGPSHCN to explore
opportunities to expand knowledge related to SCT among providers, parents of those affected, those affected, and
the community at large. FY20 legislation prompted the reconvening of the Statewide Steering Committee on
Services for Adults with Sickle Cell Disease,” in which OGPSHCN plays a key role both in planning and
implementation. SCT Follow-up opportunities are being discussed in the statewide Adult Sickle Cell Disease
Steering Committee.
Early Hearing Detection and Intervention (EHDI)
The Maryland Early Hearing Detection and Intervention (EHDI) Program, housed within the OGPSHCN, provides
Created on 8/11/2022 at 8:37 PM
Page 145 of 296 pages

surveillance and follow up to ensure newborns and infants receive a newborn hearing screening and recommended
follow up, including referral to early to intervention services, when appropriate. During FY21, there were 64,522 births
reported to the Maryland EHDI OZ Systems database. 63,467 newborns were documented as screened. Out of the
newborns screened, 62,400 passed the newborn hearing screen; 1,346 infants missed or did not pass their inpatient
screen; 95 were identified as deaf or hard of hearing and documented as referred to early intervention services; 441
infants (270 of these are home births) have files that are closed as lost to follow up or lost to documentation (LTF/D),
and there are currently an additional 447 infants whose files are still open and unresolved as of this writing. CY20
LTF/D was 30.9% and the CY19 LTF/D was 27.12%.
Follow up for newborn hearing screening suffered greatly due to the COVID-19 pandemic. Clinics had limited
appointment availability, parents did not want to expose themselves or their newborns, and staffing issues were
prevalent. Many of these issues remain even now, but CY20 certainly saw what we hope was the pinnacle with many
“non-essential” medical services being stopped or postponed during months of that year.
The MD EHDI program staff and MD EHDI Advisory Council board members obtained and shared input on how the
pandemic affecting newborn hearing screening, follow up, and early intervention services. The information obtained
allowed MD EHDI staff to better assist families and provide them with up-to-date information and realistic
expectations as they navigate the EHDI process. In addition, in response to changes in the status of nonessential
health care services in Maryland and inquiries received, the MD EHDI program developed a statement that was
provided to birthing staff when necessary. In part, it states: “the newborn hearing screen is a critical step in identifying
children who are deaf or hard of hearing. Birthing facilities should make every effort to complete a hearing screen on
newborns prior to hospital discharge and to report those findings to MDH following the usual protocols. Hearing
screens should be provided safely and consistent with available guidance to minimize the risk of exposure to
COVID-19 and other pathogens.” Despite efforts from MD EHDI staff and stakeholders, CY20 showed an increase
in LTF/D percentages; one which will be explored further going forward.
Birth Defects Reporting and Information Systems (BDRIS)
In FY21, the BDRIS program continued to use the OZ Systems database to monitor birth defects. Birth facility
training continued, using a virtual platform subsequent to the COVID-19 pandemic, to make sure staff and
administrators were using the system appropriately and effectively, and to increase reporting compliance rates. In
FY21, no training sessions were conducted for birthing facilities due to pandemic restrictions. Questions regarding
OZ were handled on an individual basis. Hospital site visits normally are conducted in collaboration with the CCHD
screening program chief and the EHDI Program audiologist to reinforce appropriate screening and reporting
procedures. These site visits were also useful to obtain documentation of the protocols being used by birth facilities
for CCHD screening. BDRIS program staff continued to reach out to specialty clinics to encourage reporting of birth
defects that are not diagnosed until an infant is discharged from the nursery. The program also continued to send out
letters and fact sheets to families with infants identified as having a birth defect. With the emergence of COVID-19,
all birthing facilities in Maryland were updated on appropriate reporting. In FY21, 1,177 babies were identified via the
birth defects reporting system and linked to resources.
Easy to Use Services and Supports
The overarching mission of the OGPSHCN is to ensure a comprehensive, coordinated, culturally effective, and
consumer-friendly system of care that meets the needs of Maryland's CYSHCN and their families. Having community-
based services for CYSHCN organized so families can use them easily is integral to accomplishing this mission but
implementing strategies to foster ease of use is significantly easier said than done. Services and supports for
Created on 8/11/2022 at 8:37 PM
Page 146 of 296 pages

CYSHCN are complex and convoluted, made unnecessarily more so by regional differences and a lack of a
centralized resource repository for families. Through both internal efforts and funding to community-based
organizations and to local health departments, OGPSHCN seeks to ameliorate some of the challenges to accessing
supports and services.
OGPSHCN continued the regional liaison relationship with Talbot County Local Health Department on the Eastern
Shore of Maryland in FY21. This relationship, which includes a full-time nurse devoted to the role, has proven to be
very beneficial. As a result of this unique partnership, all nine counties of Maryland’s Eastern Shore engage in
collaboration to identify and share information about community-based services throughout the state.
Regional liaisons are employed by a local health department in a given region and provide support, education and
mentoring to LHD nurses/care coordinators within their region.They are the designated local contact from
OGPSHCN to regional stakeholders, including families, and utilize regional partners to develop an ongoing system
of information collection for the region, which can direct services by identifying gaps and unmet needs and assist in
implementing regional initiatives as determined by OGPSHCN.
To further support collaboration amongst programs serving CYSHCN around the state, OGPSHCN conducted a
Grantee Meeting in January 2021, inviting all awardees from the competitive RFA to participate in a sharing session
allowing each to learn more about the others’ respective projects. Through this communication, OGPSHCN grantees
can learn about additional resources and opportunities for collaboration. This is something OGPSHCN plans to
pursue with more focus in the coming year.
Along the same goals of increasing opportunities for collaboration and resource knowledge, OGPSHCN also
increased engagement with internal Department of Health partners. The Maryland Developmental Disabilities
Administration (DDA) and the Center for Chronic Disease Prevention and Control (the Center) are both natural allies
to the Office for Genetics and People with Special Health Care Needs. In FY21, OGPSHCN leadership and
leadership from both DDA and the Center to explore partnership opportunities. This, too, is something OGPSHCN
plans to pursue with more focus in the coming year.
Resource Line and Resource Locator
In FY21 there were a total of 26,728 visits to the OGPSHCN website with 2195 unique visits. Average time spent on
the website was approximately 2 minutes. In FY21, the OGPSHCN Resource Line and Resource Locator continued
to grow and serve as a valuable resource for accessing community-based services. The Resource Line is a live
resource service that was staffed by OGPSHCN’s Parent Resource Coordinator prior to their departure. After their
departure, the “Systems Development” Program Chief took the lead on responding to calls for assistance. The
Resource Locator is an online resource with over 1,100 listings. In FY21, the most requested topics were general
resource information and questions regarding funding sources. Due to the network security incident that the
Department experienced in December 2021, FY21 numbers for the Resource Locator are not available. Between
July 1, 2019, and June 30, 2020, there were 5,125 unique visits to the Resource Locator. Approximately 13.8% of
users returned to the site after the initial visit. A majority of the users came from the United States (91%) with users
from the Philippines, India, France, and Indonesia making up the remainder (9%). OGPSHCN promoted use of the
Resource Line and Resource Locator through partners’ online listservs, newsletters and dissemination of fliers at
local events. The Resource Locator is translatable into 50 languages and uses a language link translation service for
those that choose to call in for assistance.
Created on 8/11/2022 at 8:37 PM
Page 147 of 296 pages

Internal Case Presentation and Training opportunities
In our FY21 application, it was noted that OGPSHCN staff would continue to identify opportunities for cross-program
integration between the Systems Development Program, which manages the grants, and OGPSHCN’s other
programs, with a focus on how the Systems Development grant activities might act in synergy with other programs or
expand the functional capacity of those programs to address specific programmatic needs that have a direct
outcome on Maryland’s CYSHCN. In an effort to support cross-program collaboration and integration, a case
presentation opportunity was added to routine senior staff meetings. OGPSHCN “Program Chiefs” meet monthly;
time was allotted on each agenda and a case presentation form template was provided to each chief with a rotating
schedule. The intent was and is to foster increased communication and collaboration between OGPSHCN programs
and to share resources that could support the families we serve.
OGPSHCN also conducts bi-monthly “all-staff” meetings during which training. opportunities have been implemented,
some focused-on Title V-specific topics (Block grant summary overview) and others focused more on office or state-
specific topics (Quality improvement, Maryland’s legislative process), but all with the overarching goal of increasing
staff knowledge of sister programs, familiarity with federal and state programs and requirements, and capacity to
service Maryland’s CYSHCN
Youth Transition to Adult Health Care
During FY21, OGPSHCN focused efforts on education and awareness, interagency partnerships, technical
assistance and systems development activities to increase the number of youths with special health care needs
(YSHCN) that receive the services necessary to make a successful transition to adult health care. Due to the COVID-
19 Pandemic beginning in March of 2020 many of the in-person activities were canceled and/or switched to virtual
which was a hindrance for some health care transition activities and services. Many of the programs funded by
OGPSHCN created effective and supportive outreach initiatives that were very successful in keeping youth, families
and partners engaged in health care transition initiatives.
Again, through both internal efforts and through funding to community-based organizations and to local health
departments, OGPSHCN sought to increase the number of YSHCN that receive the services necessary to make a
successful transition to adult health care.
In FY21, The Health Care Transition Program (HCT) collaborated with other state agencies to incorporate HCT into
program planning and increase overall education and awareness about HCT, including the Maryland Department of
Social Services - Foster Care Programs, the Specialized Health Needs Interagency Collaboration program (a
collaborative partnership between the Kennedy Krieger Institute and the Maryland State Department of Education),
and United Health Care Community Advisory Board. The OGPSHCN Health Care Transition Coordinator also again
served on the planning committee for the School Health Interdisciplinary Program (SHIP) conference, a project of the
National Center for School Mental Health.
In an effort to offset the challenges presented by COVID-19 and to keep parents/caregivers, youth, providers, support
systems, and school health professionals engaged in health care transition training and educational activities,
OGPSHCN Health Care Transition Coordinator updated the HCT-specific webpage with current content and
developed a new online virtual presentation request form.
For the Strengthening Systems of Care for Maryland’s Children and Youth with Special Health Care Needs RFA, only
one applicant selected Health Care Transition as a primary focus area.
Created on 8/11/2022 at 8:37 PM
Page 148 of 296 pages

The National Alliance to Advance Adolescent Health is a new grantee for OGPSHCN in SFY2021. The overall
project goal for their grant Year 1 was to increase school mental health professional training in evidence-informed
transition practices through a new school mental health transition initiative modeled after Got Transition’s structured
approach called the Six Core Elements of Health Care Transition. This goal was accomplished by customizing and
piloting mental health transition tools produced by The National Alliance to Advance Adolescent Health/Got
Transition and the University of Maryland’s Prince George’s School Mental Health Initiative (PGSMHI) transition
improvement team.
Workforce Development
In FY21 OGPSHCN continued the ongoing effort to incorporate workforce development activities into the office
programs by accepting student interns from various colleges and universities within the state. These interns range
from health education majors to nursing and public health majors, from both undergraduate and graduate level
programs. The office is utilizing student interns to introduce concepts of public health, needs of the CYSHCN
population, newborn screening, surveillance and follow up activities, as well as to enhance the work of the office.
In the past few years, OGPSHCN has hosted students from Morgan State University and Coppin State University -
both HBCUs - and from the University of Maryland and Stevenson University. The interns have worked on various
projects ranging from updating and developing health education materials, to developing discussion sessions, and
assisting with programmatic work. Interns are welcomed to OGPSHCN through a “meet and greet '' style meeting
with OGPSHCN leadership and any Program Chiefs and staff with whom they will be working directly. Upon the end
of their internship, they are invited to present their work and what they have learned at an office-wide meeting
specifically for this purpose.
Additionally, OGPSHCN has prioritized the professional development of existing staff. Through a structured calendar
of meetings for all staff and selected staff groupings, along with an intentional increase in learning opportunities,
OGPSHCN hopes to keep staff engaged and coordinated, and continue to build capacity to serve effectively.
[1]
Core Outcomes: Key Measures of Performance
[2]
Kansas Department of Health, Special Health Care Needs
Created on 8/11/2022 at 8:37 PM
Page 149 of 296 pages

Children with Special Health Care Needs - Application Year
The Office for Genetics and People with Special Health Care Needs (OGPSHCN) administers Title V funds specific
to children and youth with special health care needs (CYSHCN)
In 2008, HRSA's Maternal and Child Health Bureau (MCHB), together with its partners, identified six core outcomes
to promote the community-based system of services mandated for all children with special health care needs under
Title V. These outcomes gave us a concrete way to measure our progress in making family-centered care a reality
and in putting in place the kind of systems all children with special health care needs deserve
[1]
. The six core
outcomes were:
Families of children and youth with special health care needs partner in decision making at all levels and are
satisfied with the services they receive;
Children and youth with special health care needs receive coordinated ongoing comprehensive care within a
medical home;
Families of CSHCN have adequate private and/or public insurance to pay for the services they need;
Children are screened early and continuously for special health care needs;
Community-based services for children and youth with special health care needs are organized so families
can use them easily;
Youth with special health care needs receive the services necessary to make transitions to all aspects of adult
life, including adult health care, work, and independence.
In previous years, OGPSHCN has used these six core outcomes as a framework for activities and for the 2021-2025
MCH Block Grant needs assessment reporting cycle, Maryland identified, “ensuring optimal health and quality of life
for all children and youth with special health care needs and their families by providing services within an effective
system of care in alignment with the six core outcomes” as a continued State Priority. However, those six core
outcomes have been revised and updated over the years. Beginning with the FY2022 annual report and moving
forward through FY2023 and beyond, revised and updated outcomes will be discussed.
In 2014 the National Consensus Framework for Improving Quality Systems of Care for Children and Youth with
Special Health Care Needs project released a core set of structure and process standards for systems of care for
CYSHCN adding cultural competence as a seventh outcome and introducing 10 core domains for system
standards
[2]
. Version 2.0 of the National Standards for CYSHCN, released in 2017 as a result of a partnership
between The Association of Maternal & Child Health Programs (AMCHP) and the National Academy for State
Health Policy (NASHP) organizes the standards into eight core domains and introduces four Foundational
Standards for Systems of Care for CYSHCN.
[3]
As stated in the report, “These four principles are the foundation for
all standards in each domain, and should be in place to ensure a comprehensive, quality system of care for children
and youth with special health care needs.”
[4]
Foundational Standards for Systems of Care for CYSHCN:
Children and families of CYSHCN are active, core partners in decision making in all levels of care.
All services and supports for CYSHCN are implemented and delivered in a culturally competent, linguistically
appropriate, and accessible manner to best serve CYSHCN and their families. All written materials provided
to CYSHCN and their families are culturally appropriate, provided in the primary language of the CYSHCN
and their family, and in a manner and format appropriate for children and their parents or caregivers who have
limited English proficiency, lower levels of literacy, or sensory impairments.
Insurance coverage for CYSHCN is accessible, affordable, comprehensive, and continuous.
All care provided to CYSHCN, and their families is evidence-based where possible, and evidence-informed
Created on 8/11/2022 at 8:37 PM
Page 150 of 296 pages

and/or based on promising practices where evidence-based approaches do not exist.
Core Domains for System Standards
Identification, Screening, Assessment, and Referral
Eligibility and Enrollment in Health Coverage
Access to Care
Medical Home
Pediatric Preventive and Primary Care
Medical Home Management
Care Coordination
Pediatric Specialty Care
Community-Based Services and Supports
Respite Care
Palliative and Hospice Care
Home-Based Services
Transition to Adulthood
Health Information Technology
Quality Assurance and Improvement
In 2022, the Blueprint for Change: A National Framework for a System of Services for CYSHCN was released via a
special supplement to Pediatrics. The Blueprint for Change is the result of work led by the Maternal Child Health
Bureau (MCHB) in partnership with families, health professionals, and other stakeholders. In the Blueprint, four
critical areas are addressed: health equity, family and child well-being, access to services, and financing of services.
In FY23, OGPSHCN will spend some time evaluating and assessing how the Standards of Care and the Blueprint
are related and how to integrate our current work.
SFY2023 is an ideal time for OGPSHCN to shift to the updated standards of care for CYSHCN as a programmatic
blueprint, as the last few years have exposed the need for adjustments to internal organizational structures and
refreshed program strategies.
In SFY2020 and SFY2021, OGPSHCN engaged in an intensive review of the internal process for awarding grants. In
SFY2022, OGPSHCN and the Bureau began the work of assessing current programs and developing forward-
looking strategic plans. This will continue and expand in SFY2023
HRSA identifies its key strategic goal for children and youth with special health care needs as creating an effective
system of care to allow for optimal health and quality of life for all CYSHCN and their families. An effective system of
care ensures:
Families are partners in care
Screening occurs early and continuously
Families can easily use community-based services
Children and youth have access to an accessible family-centered, comprehensive medical home
There is adequate insurance and funding to cover services
Families and providers plan for transition to adult care and services.
The State of Maryland identifies the objective for this population as improved health through comprehensive,
coordinated care for CYSHCN and support for successful transition to adult health care.
For the 2021-2025 Five-Year Action Plan, the Maryland Steering Committee selected Medical Home (NPM 11) and
Created on 8/11/2022 at 8:37 PM
Page 151 of 296 pages

Health Care Transition (NPM 12) as the National Performance Measures (NPMs) for children and youth with special
health care needs. These NPMs include children and youth with and without special health care needs crossing both
CSHCN and Child Health population domains.
One of the many challenges in improving health systems for CYSHCN when there are so many opportunities for
improvement is creating a set of goals, benchmarks and measures of success that is SMART (specific, measurable,
achievable, relevant and timebound). In discussing plans for SFY2023, Maryland will primarily look at the
Foundational Standards for Systems of Care within the context of the selected National Performance Measures and
will secondarily look at those core domains for system standards not named as performance measures but still
foundational to provide effective systems of care for CYSHCN. Thirdly, Maryland will explore ways in which to
integrate the four critical areas addressed in the Blueprint for Change to ensure access to a well-functioning system
of services for CYSHCN.
MEDICAL HOME
Medical Home
According to the 2018-2019 National Survey of Children’s Health, 44.9% of children ages 0 to 17 with special health
care needs had a medical home, compared to 46.4% of children ages 0 to 17 without special health care needs.
NPM 11: Medical Home
The strategy selected for this NPM is to encourage implementation of the Medical Home model in pediatric primary
care practices through education and training opportunities. OGPSHCN will explore the possibility of providing a
continuing education course on Medical Home Implementation for MDs, PAs, NPs, nurses, and other medical
providers, with a focus on engaging providers-in-training and early career providers.
In addition, discussions will be sought around expansion, replication, and sustainability of medical home-focused
initiatives currently underway by current OGPSHCN grantees who were awarded under the 2020 competitive request
for applications. Specific topics for these discussions include patient/family-centered care, sustainable care
coordination and/or case management and shared plans of care between primary care providers and specialists.
Looking at the Foundational Standards for Systems of Care, in the context of the medical home model:
Children and families of CYSHCN are active, core partners in decision making in all levels of care (shortened to
Family-Professional Partnership)
A great deal of effort in the past has focused on educating families about the Medical Home system of care,
however, the reality is that families are more of a recipient of the medical home framework once it has been
implemented and have very little control of how, when or even if, a given provider can and will adopt this framework.
Awareness of the existence of the concept is important, but awareness alone will not increase its implementation
within the provider community. OGPSHCN will endeavor to engage providers-in-training and early career providers
to inform and educate about the medical home, and also to provide some practical tips on how to implement a
medical home in their practice.
This does not preclude educating family members. Rather, the shift is in educating family members on factors they
can control: recognizing good medical care; engaging in clear and respectful communication, and effective advocacy
for their CYSHCN.
Created on 8/11/2022 at 8:37 PM
Page 152 of 296 pages

In FY20/21, OGPSHCN drafted and posted the newly revised competitive RFA previously discussed with the explicit
requirement that all proposed projects ensure family members have a meaningful role in grant-funded activities. This
requirement continues in FY23 and beyond. As current grantees enter their third and final year of funded project
activities, OGPSHCN begins drafting the scope of work for grant projects beginning in FY24. Again, Family-
Professional partnership will take center stage.
OGPSHCN's dedicated Parent Resource Coordinator departed in late 2019, which posed a challenge for delivering
parent perspective training and providing FPP resources. However, OGPSHCN saw an opportunity to integrate
Family Professional Partnership into all facets of the work. All too often, a single family member is identified and the
box for family engagement is checked. OGPSHCN wants to see the family voice fully incorporated into all facets of
program development, implementation and administration. Without the conscious, valued, and sustained involvement
of family, none of the other goals will ever be fully and meaningfully accomplished. Collaboration with those with lived
experience is essential to determining what is needed, why needs are not currently being met, and what can be done
to address those needs. Family Professional Partnership is not a separate outcome but is the very foundation upon
which all other desired outcomes can be achieved.
OGPSHCN will continue to seek opportunities to provide family sensitivity trainings to internal and external partners
who serve CYSHCN, as well as trainings for families on resource identification and advocacy, and will also identify
additional opportunities and strategies to integrate the family voice.
All services and supports for CYSHCN are implemented and delivered in a culturally competent, linguistically
appropriate, and accessible manner to best serve CYSHCN and their families. All written materials provided to
CYSHCN and their families are culturally appropriate, provided in the primary language of the CYSHCN and
their family, and in a manner and format appropriate for children and their parents or caregivers who have limited
English proficiency, lower levels of literacy, or sensory impairments. (Shortened to Cultural Competency)
Maryland Title V humbly changes this foundational standard to read: All services and supports for CYSHCN are
implemented and delivered in a culturally respectful, linguistically appropriate, and accessible manner to best serve
CYSHCN and their families. Through an equity lens, we acknowledge that “cultural competence” is an improbable
accomplishment. The word “competence” itself implies proficiency; an end to learning. But can one be competent in
a culture one is not a part of? The standard we aspire to and will endeavor to demonstrate is one on cultural humility.
This implies respect for others’ culture as well as a mindset of continuous learning.
The clinical setting naturally comes with a power imbalance, but through a shared decision-making model, the
strengths each party brings to the table are recognized and respected. In FY23, OGPSHCN will develop
informational materials and learning opportunities on shared decision making in the context of the medical home
(shared decision making between provider and patient/family) and in the context of health care transition, discussed
further below.
One of the frameworks around which Title V is structured in the Health Equity Framework. The health equity
framework looks at class, race/ethnicity, gender, sexual orientation, and immigration status and recognizes how
institutional and structural inequities can create unequal living conditions. The unequal living conditions can then
shape the health behaviors and health outcomes. Thinking about this framework in the context of CYSHCN,
intersectionality - how race, class, gender and other characteristics intersect with one another to overlap and create
different forms of discrimination - adds another layer of complexity for families of CYSHCN and for YSHCN
navigating the journey to adulthood. Through existing and planned outreach and education efforts to providers and
families, OGPSHCN has the opportunity to inform about factors contributing to, or impeding, health equity as well. In
FY23, OGPSHCN will explore how to integrate discussion and learning opportunities on health equity into existing
Created on 8/11/2022 at 8:37 PM
Page 153 of 296 pages

learning opportunities.
OGPSHCN boasts fact sheets and resource information on multiple individual diagnoses as well as the medical
home model in general. In FY23 and beyond, OGPSHCN will implement a schedule to review and edit all public-
facing and internal fact sheets and presentation materials, including website materials.
In addition to considerations of accessibility related to limited English proficiency, lower levels of literacy, or sensory
impairments, OGPSHCN recognizes the need to modernize communication approaches. Some programs are still
using communication methodologies established 20+ years ago; it is time to consider not only ‘modern’
communication methods, but post-COVID communication methods and needs. In FY23, OGPSHCN will explore the
utilization of increased electronic communication and record-keeping.
Insurance coverage for CYSHCN is accessible, affordable, comprehensive, and continuous. (Shortened to
Insurance Coverage)
Federal and State legislation dictates much about insurance coverage, however, there are some areas OGPSHCN
can impact through outreach and education. In FY23, OGPSHCN will endeavor to ensure CYSHCN have access to
continuous health coverage, all benefits they are eligible to receive, and relevant care where they learn and live.
Through enrollment in the Children’s Medical Services Program, uninsured/underinsured CYSHCN have specialty
care paid for and, in some cases, private insurance purchased on their behalf. This will continue in FY23.
Additionally, through restoring previous relationships and forging new partnerships among community-based
organizations, healthcare providers, sister State programs and local health departments, OGPSHCN can increase
awareness of resources across the board, which will increase access to benefits and care for CYSHCN and their
families. Specific to those families, insurance and other benefits navigation is complex and often difficult to
understand. Through outreach and education to families, this confusion can be alleviated within the confines of
providing general information applicable to all programs.
All care provided to CYSHCN, and their families is evidence-based where possible, and evidence-informed
and/or based on promising practices where evidence-based approaches do not exist. (Shortened to evidence-
based care)
Evidence-based care or Evidence Based Health Care can be defined as, “the integration of the best research
evidence, clinical expertise and the patient’s unique values and circumstances.
[5]
This approach to health care
embraces the concepts of family professional partnership wherein a clinician “uses the best evidence available, in
consultation with the patient (evidence-based patient choice), to decide upon which option best suits the patient.”
OGPSHCN will continue to educate on best practices for family-professional partnership.
Sub-categories within the Medical Home Core Domain for System Standards include:
Pediatric Preventive and Primary Care
Medical Home Management
Care Coordination
Pediatric Specialty Care
Care Coordination has long been a focus of OGPSHCN’s efforts, however in recent years this focus has wavered.
Defining care coordination (as opposed to case management), determining the current landscape of care
coordination, and developing feasible, sustainable plans for care coordination in consideration of the many carried
Created on 8/11/2022 at 8:37 PM
Page 154 of 296 pages

needs of CYSHCN, and their families seems an almost insurmountable challenge. Two of OGPSHCN current
grantees are doing some exciting and innovative work around the medical home and care coordination which can
potentially be expanded. OGPSHCN will endeavor to further develop and refine the role of care coordination and
case management within the context of future grant requests for applications, with a focus on outcome measures,
quality improvement, and sustainability of local care coordination services.
In 2022, the National Academy of State Health Policy released National Care Coordination Standards for CYSHCN
Implementation Guide to outline the core system-level components of high-quality care coordination for this
population. OGPSHCN will use these standards as a guide to further inform care coordination activities in FY23.
Collaboration among multiple partners is key in providing care to CYSHCN and pediatric specialty care is no
exception. It is imperative that pediatric primary care and specialty
providers are able to communicate and collaborate without leaving the CYSHCN and their family feeling like they are
playing a game of “telephone.” A relatively easy mode of collaboration that can be as high-tech or low-tech as
needed is to establish a shared plan of care.
[6]
In FY23, OGPSHCN will increase provider and family use of shared
plans of care.
HEALTH CARE TRANSITION
Health Care Transition. In 2017, 15.3% of children in Maryland received services necessary to transition to adult
health care, compared with 14.2% nationally. 21.6% of children and youth with special health care needs received
services necessary for transition to adult health care, compared to the national average of 18.9%.
NPM 12: Transition
The strategy selected for this NPM is to increase and enhance parent/family education and training around HCT.
Internally, OGPSHCN will explore strategies to engage families in the transition process for their youth with special
health care needs. Provider knowledge and willingness to treat is essential for successful transition, but only with the
concentrated efforts of engaged families and youth will we truly see an increase in the measures. Similar to plans
under Medical Home, discussions will be sought around expansion, replication, and sustainability of health care
transition-focused initiatives
underway by current OGPSHCN grantees who were awarded under the 2020 competitive request for applications.
Specific topics for these discussions include increasing adult provider willingness and capacity to provide quality
care for youth with special health care needs, increasing family awareness of transition benchmarks, and increasing
health care and school-based professional awareness of transition benchmarks.
Looking at the Foundational Standards for Systems of Care, the context of Health Care Transition:
Family-Professional Partnership
Without the engagement of an involved adult, successful health care transition (HCT) for our YSHCN is unlikely to
happen. While there are systems and structures in place to support HCT through certain provider offices, and to
support transition to adulthood in general through school, those systems are overwhelmed and inefficient. A goal for
FY23 is to revitalize parent/family training around HCT. While the focus of efforts around the Medical Home may rest
within the provider community, the focus of activities around HCT awareness would ideally rest with the family. There
are numerous challenges to successful health care transition — including a dearth of adult providers willing to see
youth and adults with special health care needs — but families not knowing how, when, and why to focus on transition
efforts is also a significant challenge and one that might be tackled more effectively within OGPSHCN's scope of
influence.
Created on 8/11/2022 at 8:37 PM
Page 155 of 296 pages

In years past, the HCT Program within OGPSHCN convened a Health Care Transition Leadership Team, produced
fact sheets, and engaged in meaningful partnerships with stakeholders. While some of those efforts continued in
more recent years, staffing issues and other internal challenges have led to a decline in HCT-focused activities. In
FY23, OGPSHCN will explore how efforts around HCT can take the forefront again, beginning with efforts to solicit
input from families, youth and adult self-advocates. The Center for Chronic Disease Prevention and Control within the
Maryland Department of Health coordinates the Disability Health Inclusion Advisory Council, on which OGPSHCN
holds a seat. In FY22, that Advisory Council established a transition of care workgroup to impact successful health
care transition for disabled youth. The advisory council includes family-led organizations and self-advocates.
Additionally, The Association of Maternal and Child Health Programs (AMCHP) partnered with Title V Block Grants
and Got Transition® to develop AMCHP’s Implementation Toolkit for National Performance Measure 12. The toolkit
provides various relevant resources and tools Title V programs and public health professionals can use to address
NPM 12 and encourage successful youth transitions to adult health care. The toolkit explores five strategic
approaches, which include: 1) youth and family education and leadership development, 2) health care professional
workforce development, 3) care coordination, 4) communications and 5) social media, and 5) measurement and
assessment. In FY23, OGPSHCN will review this tool to aid in the design and implementation of training programs.
Educating families is only part of the equation; we must also educate and empower youth to take charge of their own
health outcomes. Many years ago, OGPSHCN designed and offered a Health Care Notebook for caregivers and for
youth. In FY23, OGPSHCN will explore electronic medical record keeping systems specifically for youth/young adults,
particularly in consideration of varying intellectual capacity.
Cultural Competency (i.e. Cultural Humility)
Efforts to demonstrate the standard of cultural humility extends to health care transition. The shared decision model
is applicable not only to the medical home (shared decision making between provider and patient/family) but to HCT
as well. Supported decision making has long been considered an alternative to guardianship for adults with
disabilities. In FY23, OGPSHCN will explore how information from The National Resource Center for Supported
Decision Making
[7]
and other organizations, as well as feedback from self-advocates, can be incorporated into HCT
materials. As previously noted, OGPSHCN boasts fact sheets and resource information on health care transition.
Along with plans to review medical home fact sheets, OGPSHCN will implement a schedule to review and edit all
public-facing and internal fact sheets focused on HCT.
Insurance Coverage
The Children’s Medical Services (CMS) Program pays for specialty care for children and youth who are uninsured or
underinsured up to age 22. The eligibility age cutoff can be extended to age 25 in certain circumstances. There are
very few safety nets for these young adults after enrollment in the CMS Program terminates. In FY22, the Program
began sending a letter to families prior to enrollment termination with health care resources for their adult child. In
FY23, additional resources will be added to the information being sent to families. OGPSHCN will also explore
opportunities to educate this cohort of families and youth with whom we already have a strong connection on
insurance and other benefits navigation.
Evidence-Based Care
Throughout FY23, OGPSHCN plans to conduct more statewide presentations on best practices related to health
care transition. The focus will be on early-career providers to increase the capacity and willingness of adult providers
to see youth and young adults with special health care needs.
Created on 8/11/2022 at 8:37 PM
Page 156 of 296 pages

In FY23, OGPSHCN will also explore a collaboration with the Adolescent Health Program within the Maryland
Maternal and Child Health Bureau to review resources related to sex education for CYSHCN. Special health care
needs and disabilities can have significant impact on sexual health and increase the risk of victimization.
Researching evidence-based best practices concerning sex education for CYSHCN will be the first stage of
educating and informing providers, parents and youth.
ADDITIONAL CORE DOMAINS FOR SYSTEM STANDARDS
Identification, Screening, Assessment, and Referral
Eligibility and Enrollment in Health Coverage
Access to Care
Community-Based Services and Supports
Respite Care
Palliative and Hospice Care
Home-Based Services
Health Information Technology
Quality Assurance and Improvement
Identification, Screening, Assessment, and Referral
OGPSHCN houses several Programs related to identification, screening, assessment and referral, including:
Newborn Screening (NBS) Follow up; Critical Congenital Heart Disease (CCHD) Screening; Birth Defects
Reporting and Information System (BDRIS); Sickle Cell Long-Term Follow-Up; and Early Hearing Detection and
Intervention (EHDI). The aforementioned Standards for Systems of Care for Children and Youth with Special Health
Care Needs Version 2.0
[8]
lists numerous factors needed for success in this standard. OGPSHCN will review these
factors in FY23 to determine where Program improvements can be made and/or where outreach to providers or
other stakeholders would be warranted.
In the area of Newborn Screening Follow-Up, OGPSHCN has begun development on an educational webinar
providing technical assistance on specimen collection to reduce the number of unsatisfactory specimens.
One area needing significant attention in FY23 and beyond is refusal and loss to follow up for certain screening
programs. One can surmise several factors contributing to increased refusal for certain screenings and assessments
over the past several years. In FY23, OGPSHCN will assess the current status of refusals and loss to follow up in
current programs and develop plans to determine causes and enact strategies to reduce those numbers.
Eligibility and Enrollment in Health Coverage
Thinking about factors involved in eligibility and enrollment in health coverage that are within OGPSHCN’s sphere of
influence, in FY23, outreach and education to families will focus on insurance and other benefits navigation.
Additionally, OGPSHCN will explore increased partnership and collaboration with Maryland Medicaid to inform and
ensure best practices for CYSHCN enrolled in Medicaid Managed Care Organizations. With the renewed
Community of Care Consortium, discussed elsewhere, OGPHSCN will provide a forum for health coverage
providers and other stakeholders of the CYSHCN community to interact.
Access to Care
Access to care involves CYSHCN having geographic and timely access to primary and specialty services.
Created on 8/11/2022 at 8:37 PM
Page 157 of 296 pages

Through the CMS Program, access to specialty care on an individual level is directly supported for enrolled
CYSHCN. On a more-systemic level, The Maryland Community of Care Consortium for CYSHCN (COC) served as a
forum for learning, networking, and communication among various stakeholder groups for years. The COC was
coordinated by The Parents’ Place of Maryland (PPMD) through grant funding through FY20. COC work was not
included in the FY21 competitive RFA and discussions between OGPSHCN, Bureau and Administrative leadership
are ongoing to plan and implement continuation of the COC. This has been a challenge over the last year; one
OGPSHCN hopes to address in FY23. The COC was a valuable statewide collaborative effort that enhanced access
to care by sharing information and resources among multiple stakeholders. In rebuilding the COC, OGPSHCN will
look at the previous structure, but also consider current needs and technology in a post-COVID world. The Florida
Family Leaders Network brings together family leaders from across the state who work or volunteer at local regional
or state level - with healthcare systems, agencies and government offices, community based or family run
organizations. Organizations and systems like this will be assessed to determine how we can integrate their
successes into Maryland Title V for CYSHCN.
Additional opportunities for information sharing and collaboration will be afforded to OGPSHCN grantees with the
long-awaited implementation of grantee meetings in FY23. This has also been a challenge over the last year.
The aforementioned efforts to ensure a shared plan of care for CYSHCN will additionally enhance the capacity of
system stakeholders to provide care no matter where the CYSHCN present themselves.
Finally, a significant “silver lining” of the COVID-19 pandemic has been the increase in telemedicine/telehealth.
Providers rapidly shifted to what had previously, for years, been an emerging practice. The shift was so rapid that an
assessment of the current state of telemedicine in Maryland would be beneficial. Upon the outcome of that
assessment, OGPSHCN can determine what additional educational and advocacy efforts are needed.
Community-Based Services and Supports
Strategies to impact access to care will have the added benefit of impacting community-based services and
supports. However, to truly provide comprehensive home and community-based supports, OGPSHCN will
additionally pursue collaborative opportunities with health systems, and community agencies including family
organizations, education, Early Intervention (Part C), Special Education, child welfare, mental health, and home
health care organizations. Through the aforementioned Community of Care Consortium, stakeholders such as these
will have the opportunity to interact with and learn from each other.
Sub-categories within the Community-Based Services and Supports Core Domain for System Standards include:
Respite Care, Palliative and Hospice Care and Home-Based Services. While OGPSHCN has encouraged grantees
to focus on some of these categories - respite care, specifically - those efforts have declined in recent years. In
FY23, OGPHSCN will review components of success for each of these standards and determine the best next steps.
Health Information Technology
Several years ago, OGPSHCN developed a Health Care Notebook and a Maryland Youth to Young Adult Care
Notebook. These care notebooks were designed for parents and caregivers of a child with special health care
needs and provided a helpful central tool to store all of a child’s health care information. The care notebooks allowed
parents and caregivers to provide any health information about their child, including reports from recent doctor’s
visits, recent summaries of hospital stays, current school plans, test results and informational pamphlets to new
providers. Additionally, parents and caregivers could provide pertinent information about their child that they felt a
paid caregiver might need. At the time of development, they were invaluable record-keeping, organization and
information-sharing tools. In 2022, however, the idea of carrying around a binder full of papers is outdated and, in the
case of youth, unrealistic. In FY23, OGPSHCN will review the care notebooks to update for current needs and
Created on 8/11/2022 at 8:37 PM
Page 158 of 296 pages

technology options, including ensuring that youth with special health care needs play a role in creating their own care
notebook.
Quality Assurance and Improvement
Effective quality assurance and improvement requires data.
OGPSHCN recently inherited the management of an existing agreement between Maryland’s Office of Quality
Initiatives and the University of Maryland, College Park Epidemiology Doctoral Internship Program. In FY22, doctoral
interns focused on sickle cell data, assessing hospital utilization, and morbidity and mortality among young adults
with sickle cell disease and sickle cell trait. Analysis of Maryland data will allow for comparison with national data and
permit identification of priority needs for young adults with these conditions. In addition, sickle cell analyses will serve
as a template for analyses of all CYSHCN and for specific conditions. In FY23, this relationship will continue. In
addition to the opportunities afforded by that agreement, OGPSHCN will invest time and efforts into data capacity,
creating opportunities for data sharing and data linkages among partners and stakeholders. With increased data,
OGPSHCN can develop additional measurable objectives.
Overarching internal goals for FY23 and Beyond
Many plans for FY23 and beyond for OGPSHCN are overarching goals pertaining to program assessment, refresh
and redesign. Through necessity (staffing changes, network security incident) and desire, FY22 has brought
numerous opportunities to evaluate the structure of OGPSHCN, its programs, and the processes by which those
programs are run. Frankly, Title V CYSHCN programs have stagnated in the last few years. In many respects FY23
will be a year of assessment and planning across all programs, with the evaluation and possible reconfiguration that
began in FY22 continuing to focus on innovative and modern program design and implementation.
Beginning with a comprehensive review of current literature and best practices, and culminating in a determination of
priorities, strategies and measures of success, FY23 should be a year of significant change for OGPSHCN.
Structural changes
In FY23, components of the OGPSHCN organizational structure will shift. Some due to staffing challenges and some
due to a very intentional review of staff capacity and ideal structure. OGPSHCN plans to hire and onboard a new
CYSHCN Title V manager, a new Medical Director and a new epidemiologist, as well as a new EHDI program
manager within FY23.
Measures of Success
Goals regarding measures of success are two-fold; one specific to internal programs and processes, and the other
specific to OGPSHCN Title V-funded grantees.
Development of measures for NPM 11 and NPM 12
In FY23, OGPSHCN will assess data needs and availability related to medical home and health care transition
specifically. Through the aforementioned contract with University of Maryland, a review of data available through
Maryland’s Health Services Cost Review Commission
[9]
regarding health care transition for CYSHCN has already
begun. A detailed data request to Maryland Medicaid will also be submitted after consideration of what data fields
would be most beneficial. Through this data, OGPSHCN will be better able to determine accurate baseline numbers
for Maryland CYSHCN, thereby more accurately identifying needs and assessing the value of planned strategies and
interventions.
Program Assessment and Evaluation
As a result of aforementioned opportunities to evaluate OGPSHCN programs and the processes by which those
programs are run, certain programs have been asked to implement new or increased tracking systems in FY22. This
Created on 8/11/2022 at 8:37 PM
Page 159 of 296 pages

review and expansion of tracking mechanisms will continue in FY23. In order to determine if OGPSHCN programs
are reaching targeted populations, data must be collected on stakeholder outreach and contacts. Additionally,
evaluation tools will be developed and implemented for education and training opportunities to determine value and
effectiveness.
Grant Management
Services provided by grantee organizations vary by design. OGPSHCN endeavors to keep scopes of work in
requests for applications as broad as possible to allow community-based organizations and local health
departments to design projects that will reflect the needs of the communities they serve. Each applicant is asked to
submit their plans to evaluate program efforts within their initial application and to update theri evaluation plan in any
non-competitive applications. This allows grantees to design their own program, however, it also allows them to tell
the State how they will measure success. In future requests for applications, OGPSHCN will endeavor to include a
more explicit statement of work and evaluation measures. The State Title V office should and will tell grantees how
success will be measured and have them provide the needed information.
In FY23 OGPSHCN will continue to monitor and review reporting requirements from all grantees to ensure fidelity to
Department goals and grant agreement scopes of work, while also planning for future iterations of the request for
applications to be posted and the work that needs to be done across the state.
Collaboration
An important goal in FY23 will be to establish or maintain connections to other State offices, community-based
organizations, local health departments, provider organizations, and more.
The Community of Care Consortium (COC) will afford OGPSHCN an opportunity to liaise with multiple stakeholders
across many categories. The first step in re-introducing the COC will be to conduct an internal assessment of
partners and stakeholders to be invited. The first task of the newly re-formed COC will likely be to conduct a more
thorough partnership assessment of sorts to determine additional stakeholders who should be invited to participate.
An additional requirement for FY21 grantees and continued with the FY22 grants was the establishment of routine
grantee meetings to discuss topics identified as priorities by OGPSHCN. Much of the planning for these meetings
took place internally during FY21, with the intent to implement fully in FY22, however, planning and implementation
was stalled due to internal challenges. In FY23, grantee meetings will begin. Genetic Center grantees funded to
provide support to the newborn screening follow up program will have their own meetings to discuss challenges and
opportunities specific to their work, while other grantees will meet to discuss topics such as: social return on
investment;
addressing health and wellness equity; performance measures and outcome measures; and grant work intersections
with OGPSHCN’s programs and opportunities for complementary activities.
OGPSHCN also hopes to host a more structured “all-grantee” meeting that will require the attendance of each
grant’s Project Director, along with one CYSHCN or family member who is a contributor to the grantee’s project.
Maternal and Child Health Bureau and Prevention and Health Promotion Administration leadership will also be
invited to these ‘all-grantee’ meetings.
Collaboration with other state offices and agencies serving the same population is already happening on some level
through sponsoring or serving on certain advisory councils and committees (e.g. Disability Health Inclusion Advisory
Council and Transition of Care Workgroup), but it will be important in FY23 to map missing partners and establish
connections. For example, the Maryland Health Care Commission (MHCC) is an independent regulatory agency
whose mission is “to plan for health system needs, promote informed decision-making, increase accountability and
Created on 8/11/2022 at 8:37 PM
Page 160 of 296 pages

improve access in a rapidly changing health care environmental by providing timely and accurate information on
availability, cost and quality of services to policy makers, purchasers, providers and the public.” The MHCC oversees
the Patient Centered Medical Home (PCMH) workgroup. OGPSHCN will endeavor to connect with MHCC in FY23.
In FY23, OGPSHCN will also continue to have leadership representation on the Maryland Community of Practice for
Supporting Families and Charting the Lifecourse Framework (MD-CoP), which is coordinated by the Maryland
Department of Health’s Developmental Disabilities Administration. The goal of the MD-CoP is to “build capacity
across and within the state to create policies, regulations, systems and practices to enhance the lives of people with
intellectual and developmental disabilities and their families enabling all people to live, love, work, play, learn and
pursue their aspirations in their community.” This collaborative effort will help to improve policies, programs and
practices around HCT, workforce development and more. There are additional opportunities for partnership with the
Developmental Disabilities Administration that will also be explored in FY23 and beyond.
Opportunities to collaborate with organizations at the national level will also be explored. OGPSHCN had reached
out to The Catalyst Center to discuss technical assistance options for the Children’s Medical Services Program
previously. This will be an item for follow up in FY23.
Family-Professional Partnership
Family-Professional Partnership is perhaps the highest priority for OGPSHCN. OGPSHCN wants to see the family
voice fully incorporated into all facets of program development, implementation and administration. Without the
conscious, valued, and sustained involvement of family, none of the other goals will ever be fully and meaningfully
accomplished. Collaboration with those with lived experience is essential to determining what is needed, why needs
are not currently being met, and what can be done to address those needs. Family Professional Partnership is not a
separate outcome but is the very foundation upon which all other desired outcomes can be achieved.
As the lead agency on Family-Professional Partnership (FPP), OGPSHCN will assess how to increase FPP within
State systems, as well as providing training and support to external stakeholders. In FY23, a review of evaluation
tools will be conducted with plans to evaluate the current status of internal FPP, determine areas of relative weakness
and develop strategies to increase FPP. Depending upon the results of the evaluation and staff bandwidth,
OGPSHCN hopes to introduce Leading by Convening
[10]
to staff, including Maternal and Child Health Bureau Staff.
This “blueprint for authentic engagement”
[11]
provides a framework to engage stakeholders. The companion, Serving
on Groups
[12]
can also be shared with family members wishing to serve on a decision-making group, whether within
OGPSHCN or not.
In addition to Leading by Convening as a professional development opportunity, OGPSHCN staff will continue to
engage in other opportunities for learning and enhancing family-professional partnership.
Since her onboarding, the OGPSHCN Deputy Director has served as the Title V Family Delegate; In FY23,
OGPSHCN will identify a new family delegate outside of the Title V agency. OGPSHCN leadership will additionally
seek out pathways for targeted recruitment of specific groups (e.g., a parent/caregiver of a CYSHCN or a former
CYSHCN) within the framework of approved state hiring practices. This will provide a foundation for future
recruitment efforts which have proven challenging in the past.
A word about COVID-19
COVID-19 has had a profound impact on the entire world. Children and youth with special health care needs
represent a population that may be at increased risk for complications with COVID-19. Children with chronic
conditions, disabilities and those with medically complex conditions are especially vulnerable.
Created on 8/11/2022 at 8:37 PM
Page 161 of 296 pages

The Developmental Disabilities Administration (DDA), a sister State administration, has gathered informational
materials and developed guidance for community-based services in response to COVID-19. The DDA is working
with the Maryland Department of Health (MDH) Administrations and the Maryland Department of Disabilities
(MDOD), as well as Maryland and National Advocacy Organizations to inform and support people in services,
family members, direct support professionals and providers. OGPSHCN supports the efforts of the DDA and will
seek opportunities to collaborate and disseminate information in FY23.
There have been some unforeseen benefits from COVID-19, including increased availability of
telehealth/telemedicine. Telemedicine has been a component to successful access to care for CYSHCN for years.
In FY23, OPGSHCN will assess the current state of telemedicine in Maryland and determine what additional
educational and advocacy efforts are needed.
Emergency Preparedness
As we've seen during the pandemic, people with disabilities are often left out of disaster preparedness and
response, compounding the risk to CYSHCN and their families.
The Partnership for Inclusive Disaster Strategies is a “disability-led organization with a focused mission of equity for
people with disabilities and people with access and functional needs throughout all planning, programs, services and
procedures before, during and after disasters and emergencies.”
[13]
In FY23, OGPSHCN will assess the current
state of emergency preparedness for CYSHCN and their families in Maryland and determine the best next steps.
Looking forward
Finally, while the current grantees resulting from the FY21 competitive RFA should remain in effect until June 30,
2023, now is the time to assess the needs of the communities we serve and discuss desired edits to applicant
scopes of work beyond FY23. The recent Maternal and Child Health strategic plan and the recent Needs
Assessment will aid in this effort, as carefully review of reporting requirements from all grantees. The last year or two
were a bit of a turning point for OGPSHCN grants administration. This has been a difficult transition on many levels,
but the fervent hope is that with more focused attention to a truly competitive process and a strenuous application
review process, we will see innovative and sustainable programs that can change the landscape for CYSHCN in
Maryland for the better.
If there were one phrase to describe OGPSHCN efforts in the past years and continuing into FY23, it would be
“increasing capacity.” Ultimately, the goal is to increase the capacity of staff to effectively and efficiently serve the
people of Maryland - particularly CYSHCN and their families, to increase the capacity of providers to provide care for
CYSHCN within a medical home, and to increase the capacity of families to support their CYSHCN now and in the
future while allowing for as much independence as possible.
[1]
Core Outcomes: Key Measures of Performance
[2]
Standards for Systems of Care for Children and Youth with Special Health Care Needs
[3]
National Standards for Systems of Care for Children and Youth with Special Health Care Needs, Version 2.0 Informational website
[4]
National Standards for Systems of Care for Children and Youth with Special Health Care Needs, Version 2.0 report
[5]
Bhargava, K., & Bhargava, D. (2007). Evidence Based Health Care: A scientific approach to health care. Sultan Qaboos University
medical journal, 7(2), 105–107.
[6]
National Resource Center for Patient/Family Centered Medical Home
[7]
The National Resource Center for Supported Decision Making
Created on 8/11/2022 at 8:37 PM
Page 162 of 296 pages
[8]
Standards for Systems of Care for Children and Youth with Special Health Care Needs Version 2.0
[9]
Health Services Cost Review Commission
[10]
Leading by Convening
[11]
Cashman, C., Linehan, P., Purcell, L., Rosser, M., Schultz, S., and Skalski,S. (2013). Leading by Convening: A Blueprint for Authentic
Engagement. Alexandria, VA: National Association of State Directors of Special Education.
[12]
Serving on Groups
[13]
The Partnership for Inclusive Disaster Strategies
Created on 8/11/2022 at 8:37 PM
Page 163 of 296 pages

Cross-Cutting/Systems Building
State Performance Measures
SPM 5 - Cross-Cutting Measure: Percentage of MCHB committees/workgroups that include community
members/persons with lived experience
Measure Status: Active
Annual Objectives
2023 2024 2025
Annual Objective 27.0 36.0 45.0
Created on 8/11/2022 at 8:37 PM
Page 164 of 296 pages
State Action Plan Table
State Action Plan Table (Maryland) - Cross-Cutting/Systems Building - Entry 1
Priority Need
Ensure that MCHB policies and processes are centered on equity and anti-racism principles
SPM
SPM 5 - Cross-Cutting Measure: Percentage of MCHB committees/workgroups that include community members/persons
with lived experience
Objectives
To increase the percentage of MCHB committees/workgroups that include community members/persons with lived
experiences from a baseline of 18% to at least 50% by 2025.
Strategies
1) Continue to convene the MCHB Equity Work Group, 2) Facilitate a webinar and/or training related to disparities in
maternal and child health, which will be open to internal and external stakeholders, 3) Conduct an internal assessment of
family engagement using an evaluation tool, 4) Work towards stakeholders of committees/workgroups represent racially,
ethnically, and geographically diverse communities (ex. FIMR Teams) through assessment and creation of
tools/guidance/templates that support the development of committees/workgroups that are diverse , 5) Recruitment and
onboarding of an Advanced Health Policy Analyst and Outreach Manager. A part of this person’s role will convene the
MCHB Equity workgroup to help implement a plan to help Title V further focus on equity, 6) request grantees to
disaggregate data by race and ethnicity to better understand health disparities, 7) Participate in the Root Causes of
Health Initiative (ROCHI), an initiative led by the Institute for Healthcare.
Created on 8/11/2022 at 8:37 PM
Page 165 of 296 pages

Cross-Cutting/Systems Builiding - Annual Report
Maryland’s identified priority need for cross cutting/systems building is “to ensure that Maternal and Child Health
Bureau (MCHB) policies and processes are centered on equity principles.” This is a new priority area proposed for
FY2023 to reflect the State’s Title V effort on equity.
During Fiscal Year 21, State Title V staff developed an internal equity workgroup that initially focused on developing
shared language, definitions, and understanding within the Bureau, discussing and planning ways to strengthen
partnerships and collaborations, using data and information systems to strengthen equity, influence policy and
strategic resources where there is an impact to promote an equity and anti-racist lens. Representatives from each
office joined the internal working group that started December 2020.
The group developed the following ground rules to start each workgroup meeting:
Listen deeply;
Accept one another’s reality;
Step up, step back;
Ask compassionate questions;
Challenge yourself;
Expect and accept non-closure;
Expect to experience discomfort;
Allow others to learn what you already know;
Respect confidentiality— take the stories, leave the names;
Commit to be open minded;
Treat people the way they want to be treated and not just how you want to be treated;
Willingness to own mistakes, be honest, and learn;
Be courageous when undertaking this work;
All these elements take time. So, take care of yourself.
The group then developed a self-assessment for Title V State staff and Maternal and Child Health Bureau staff that
was based on the self-assessment tool developed by the Bay Area Regional Health Inequities Initiatives for Local
Health Departments. In total, there were 43 respondents which is nearly 50% of the MCHB Staff. The respondents
were associated with 16 different programs.
Questions included asking the staff about the top unjustly distributed health issues, and top environmental, social,
and economic conditions that impact health. The top unjustly distributed health issues included: 1) Infant Mortality, 2)
Food Insecurity/Hunger, 3) Maternal Mortality, and 4) Overweight/Obesity. The top environmental, social, and
economic conditions that impacted health included: 1) transportation, 2) housing, 3) education,4) access to care, 5)
food insecurity, and 6) poverty.
Approximately 11% of the 43 respondents reported that they were not certain or did not know if their program was
addressing health inequities. In addition, approximately 56% of the respondents said that there is some focus on
addressing health inequities in their program, and 37% reported that “there is a lot of focus” on addressing health
inequities. When asked about ways that staff can work towards addressing equity and eliminating health disparities
in their role, some reported having grantees focus on eliminating health disparities (44% of the respondents) and
focus funding on more community-based organizations (33%). Respondents also reported that hosting regular
discussions on equity can help Title V and the Bureau address equity and eliminate health disparities (58%) and
provide additional training about toolkits to focus on equity and eliminating health disparities. All respondents agreed
or strongly agreed to the statement that it is important to understand the beliefs and values of the residents and
Created on 8/11/2022 at 8:37 PM
Page 166 of 296 pages

communities served by the Bureau.
As part of the equity workgroup, members developed a recruitment dissemination list for Title V recruitment postings.
The dissemination list includes Historically Black Colleges and Universities, organizations who serve people with
disabilities, as well as other academic universities. The dissemination list was provided to supervisors to ensure that
open recruitments are shared broadly with the organizations on the dissemination list.
In addition, the State Title V staff developed an interview format to make the recruitment process more inclusive for
positions with Title V. This was after the Equity Workgroup led a discussion on the importance of inclusivity and the
need to include sharing pronouns in the workspace. During the recruitment process, the interview panels shared
their pronouns and asked the applicant if they would be willing to share their pronouns. Title V staff have also
included their pronouns in the signatory line of their emails.
Title V staff also organized key workshops during Black Maternal Health Week that were open to Title V staff and
partners. This was part of the Maternal Health Improvement Program or MDMOMs initiative. These workshops
included: Intersectionality and Anti-Racism (Workshop #1) and Improving Maternal Health with Community Doulas
(Workshop #2) both led by Andrea Williams- Muhammad. Andrea Williams-Muhammad is the Director of Nzuri
Malkia Birth Cooperative and is a birth worker who has combined her experience in Social Work, as a Family
Support Counselor with the Housing Authority of Baltimore, and as a HRIS Policy and Implementation Analyst along
with her grassroot community building and advocacy. She unapologetically centers her work in the advocacy and
sustainability of Black cultural traditions in birthing, Black female-led scholarship, and creating sustainable pathways
for community building.
During Workshop #1, participants learned the definitions of key terms such as intersectionality that was coined and
defined by professor Kimberlé Crenshaw, understand how the systems within which we work can perpetuate
oppression, and how staff can work within those systems for sustainable change. She also reviewed how historical
trauma affects current Title V work. In Workshop #2, participants learned the scope of practice of community doulas
and the evidence supporting their contribution to reductions in maternal mortality as well as challenges and
misconceptions of doula care, highlighting examples in urban and rural settings in Maryland. In addition to Andrea
Williams-Muhammad, Patricia Liggins, Founder/Owner of Birthers United spoke and Tanay Lynn Harris, Co-Founder
of the Bloom Collective. There were 96 attendees for Workshop #1 and 92 attendees for Workshop #2. Attendees to
the workshop reported that they will work to incorporate family voice into their work such as home visiting and care
coordination.
Through the Equity workgroup, activities related to equity were tracked within the Bureau. Offices shared training
that was being implemented on the program level, and other programs were inspired to implement additional
trainings. For example, in July 2021, an outside presenter facilitated a presentation, “Words Matter” to make sure
language for gender inclusiveness was being used in a WIC Breastfeeding Coordinators meeting. In addition, an
implicit bias training was conducted to approximately one half of all the statewide WIC paraprofessionals with
another training that was held in September 2021.
As Title V staff were participating in the Maternal Health Improvement Program or MDMOMs, Title V staff led an open
bid procurement for an equity advisor for the Maternal Health Improvement Program Task Force. The equity advisor
would provide strategic guidance prior to and during the Task Force meeting to ensure inclusivity, in collaboration
with the Task Force Chair, develop objectives and recommendations for the statewide Maternal Health Strategic
Plan through an equity and anti-racist lens and lead strategic planning sessions with Task Force members and
community partners in the development of the Maternal Health Strategic Plan. Dr Kanika Harris, of the Bizell Group,
Created on 8/11/2022 at 8:37 PM
Page 167 of 296 pages

was selected as the Equity Advisor in FY2021 and began working with the Task Force members and the Chair of the
Task Force, which was the Title V Manager to provide strategic guidance to this Statewide program.
In addition, Title V staff, including the Bureau Director and the Title V Manager, worked with the Maternal Health
Improvement Task Force to help develop the Maternal Health Improvement Program Strategic Plan. The Maternal
Health Strategic Plan process was structured into six stages: 1) scan of existing needs assessments and plans
including the Title V State Action plan, Maternal Mortality Review Committee and Stakeholder Group
recommendations, as well as strategic plans from other states; 2) identification of state-level strengths and
challenges; 3) identification of key priorities, goals, and desired outcomes based on identified strengths and
challenges; 4) stakeholder and public input; 5) strategic plan revisions based on feedback; and 6) report finalization.
Members of the Maternal Health Improvement Task Force led the development of the Maternal Health Strategic Plan.
Overall, approximately 15 stakeholder input sessions were held. Many of these input sessions occurred through
existing stakeholder meetings.
Members of the Equity workgroup were also involved in the MCHB staff’s professional development and learning
event called, “Bureau Month.” The inaugural Bureau Month started in January 2021 and was led by the Deputy
Director of the Bureau in collaboration with a planning committee. Staff members weighed in on topics for the
Bureau Month plenary sessions. The top three choices by staff were to focus on anti-racism and equity, incorporating
community voice into programs, and collaboration and communication.
Bureau month consisted of weekly 90-minute sessions, in which staff members from each of the offices led team
building sessions for 30-minutes, and 60-minute plenary sessions that had been voted on by the Bureau. Dr. Eroll
Bolden, Professor, Department of Social Work at Coppin State University served as the plenary speaker for session
four of Bureau Month, Communication and Collaboration. In addition, there was a session on Mental Health and Self
Care that was presented by Ifetayo White, Founder and Director of CHOICES Birthing and Wellness Support and the
Lowcountry School of Reiki. A member from the Office of Family and Community Health Services led the team
building exercise that was related to Lean Six Sigma and circles. There was a session on Incorporating the
Community Voice into Our Programs that was led by Kristina Wint, Program Manager, Women’s Health and Jessica
Stieger, Program Manager, Infant Health from AMCHP. A staff member from WIC led the team building exercise of
two truths and a lie. A presentation on Anti-racism and equity was led by Stephanie Slowly, Director of Systems
Management, from the Behavioral Health Administration. The team building exercise was led by a staff member by
the Office for Genetics and People with Special Health Care needs.
Created on 8/11/2022 at 8:37 PM
Page 168 of 296 pages

Cross-Cutting/Systems Building - Application Year
Maryland’s identified priority need for cross cutting/systems building is “to ensure that Maternal and Child Health
Bureau (MCHB) policies and processes are centered on equity principles.” This is a new priority area proposed for
FY 2023 to reflect the State’s Title V efforts on achieving equity.
State Title V staff started an internal equity workgroup that initially focused on developing shared language,
definitions, and understanding within the Bureau, discussing and planning ways to strengthen partnerships and
collaborations, using data and information systems to strengthen equity, influence policy and strategic resources
where there is an impact to promote an equity and anti-racist lens. Representatives from each office joined the
internal working group that started December 2020. Since then, the Title V staff have met monthly.
For FY 2023, to continue with focusing on equity, Title V staff and the Bureau of Maternal and Child Health Staff will
continue to convene the MCHB/Title V Internal Equity Group. Starting in FY 2022, the workgroup started shared
learning by reading and discussing articles. Readings have included books such as Not in My Neighborhood: How
Bigotry Shaped a Great American City. This was selected after equity workgroup members decided that reading
this book would enhance the group’s learning. Discussion questions are led by various Equity Workgroup members.
In addition, the Equity workgroup has moved towards 25% learning and a 75% action format. This was based on a
needs assessment of the group of the direction to move towards more action-oriented activities. The group will
develop a workplan to determine and prioritize activities that will help Title V and the Bureau move towards achieving
equity. Some of the priorities include hiring a Health Policy and Outreach Manager, whose focus will also be leading
the Equity Workgroup along with the Maternal and Infant Health Program Manager and Adolescent Health
Coordinator.
Title V staff, through the Equity Workgroup will facilitate a webinar and/or training related to disparities in maternal
and child health, which will be open to internal and external stakeholders. Starting in FY 2021, Title V staff organized
key workshops during Black Maternal Health Week that were open to Title V staff and partners. This was part of the
Maternal Health Improvement Program (MDMOMs Initiative). These workshops included: Intersectionality and Anti-
Racism (Workshop #1) and Improving Maternal Health with Community Doulas (Workshop #2) both led by Andrea
Williams- Muhammad. Andrea Williams-Muhammad is the Director of Nzuri Malkia Birth Cooperative. In FY 2023,
Title V will continue to plan to organize workshops during Black Maternal Health Week working with external
partners.
In addition, during FY 2021, the inaugural Bureau Month was started for Bureau of Maternal and Child Health staff.
The purpose of the sessions are for team building and professional development. The sessions were organized by
the Deputy Bureau Director with a small workgroup, which had a few members of the Equity workgroup. MCHB Staff
voted on the topics. The topics included Communication and Collaboration, Mental Health and Self Care,
Incorporating the Community Voice into Our Programs, and Anti-racism and Equity. During FY 2023, planning for
professional development and training opportunities will continue. One of the measures that Title V staff will review is
to see how many staff have undergone Diversity, Equity, and Inclusion (DEI) training with the goal that 100% of all
staff have undergone training by 2025.
Title V staff will participate in the Root Causes of Health Initiative (ROCHI), an initiative led by the Institute for
Healthcare Improvement and the National Association of Chronic Disease Departments that is championed by the
Prevention and Health Promotion Administration (PHPA). This initiative is a learning collaborative where PHPA
participants receive technical assistance and have an opportunity to gain a deeper understanding of adaptive
leadership and how to use these skills to address the root causes of health inequities. As part of ROCHI, staff will
Created on 8/11/2022 at 8:37 PM
Page 169 of 296 pages

participate in an Equity Action Lab, which is a proven method for involving end-users and front-line staff in the co-
design and co-implementation of an initiative. This is a model for setting an ambitious goal, designing a preliminary
plan to achieve this goal, and taking action. The Equity Action Lab structure consists of four phases: Prep Phase,
Planning phase, Spring phase and sustainability. The Prep phase which takes approximately 2-3 months consists of
data collection to understand the needs, interventions, and the development of ideas. The formation of the team
occurs during this phase as well as the narrowing of the focus. In the planning phase, an ambitious goal is set,
potential solutions are brainstormed, and action plans are developed. Then in the Spring Phase, which lasts
approximately 100 days, the plan is implemented to test the idea, plans are adapted as needed to achieve goals,
and there are weekly team meetings. PHPA aims to implement a quality improvement process that will systematically
assess the operationalization of equity of the program, with the long-term goal of reaching health equity in Maryland.
The questions that participating programs will ask is: 1. Equity of reach: is the racial/ethnic distribution of the
program participants a match to an expected or desired racial/ethnic distribution based on who is eligible and
disproportionate risk considerations and 2. Equity of impact: is the rate of achieving a milestone the same for
participants across different racial/ethnic groups. For FY 2023, Title V staff will participate in the 100-day challenge
and look within its programs to determine equity of reach and equity of impact. Title V staff will examine its own data
system and see if equity of reach can be examined. This will lead to recommendations for its data system.
Title V staff will participate in the Prevention and Health Promotion Administration (PHPA)'s Equity workgroup that
also supports staff by increasing knowledge and skills in equity, inclusion, and resilience as well as developing
language and resources for equitably awarding grantees. Title V staff will continue to work with the larger PHPA
Equity workgroup to conduct an environmental scan of PHPA Offices and Centers through a survey to obtain a
baseline focus on health equity and conduct key informant interviews with the PHPA Office of Procurement and Office
of Minority Health and Health Disparities.
Title V Staff supported the development of the Maternal Health Improvement Strategic Plan which was led by the
Maternal Health Improvement Taskforce. The Strategic Plan, which was submitted to HRSA as part of the MD MOM
Initiative, has five main focus areas to improve maternal health, particularly in BIPOC populations:
1. Promote Equity and Mobilize Against Racism in Maternal Health
2. Achieve Health (Preconception, Prenatal and Birth, Post Partum, and Interconception Periods) Using
the Life Course Model to Support Maryland Birthing People Through Advocacy and Implementation of
Effective Policies.
3. Develop Strategies that Acknowledge the Influence of the Social Determinants of Health and Historical
Racism to Improve Resiliency for Birthing People, Families, and Communities and to Promote an Optimal
Quality of Life.
4. Improve Access and Utilization of Data and Improve Surveillance of Data on Structural Racism and its
Impact to Make Informed Decisions.
5. Develop a Maternal Health Provider Workforce that will be Available, Accessible, and that Offers
Services Based on the Principles of Cultural Humility, Equity, and Racial Justice.
In addition, the Task Force elected co-chairs in order to emphasize and practice inclusion. Previously, Title V
Manager chaired the Task Force. Title V staff with the co-chairs will continue to strategically plan for agenda items
and facilitate the activities and conversations moving forward. In FY 2023, Title V staff will work with the Co-Chairs to
review, execute, and manage the strategic plan and further work to understand individuals and organizations who
should be part of the Maternal Health Improvement Task Force and review policies that would improve maternal
health services across the State.
Created on 8/11/2022 at 8:37 PM
Page 170 of 296 pages

In addition, in FY2023, Title V staff will work to ensure stakeholders of committees/workgroups represent racially,
ethnically, and geographically diverse communities (ex. FIMR Teams) through assessment and creation of
tools/guidance/templates that support the development of committees/workgroups that are diverse. Through the
support from the Centers for Disease Control and Prevention Enhancing Reviews and Surveillance to Eliminate
Maternal Mortality (ERASE MM) program, Maryland plans to move towards a multi-disciplinary review team versus a
predominantly physician-led, medical review team to conduct comprehensive case reviews in line with the national
best practices. The multi-disciplinary review team, called the Statewide Maternal Mortality Review Team (MMRT) will
identify and review pregnancy-associated deaths, identify factors that contribute to these deaths, and propose
recommendations that aim to prevent future deaths. The overall mission of the Program is to review the issues
surrounding the pregnancy-associated deaths, to identify interventions, and to promote change among individuals,
health care systems, and communities in order to prevent maternal deaths, reduce maternal morbidities and improve
population health. Members of the MMRT will represent the diversity of Maryland’s population and will consist of
individuals with both clinical and non-clinical expertise as recommended by national best practices. There will be
approximately 20 members on the Review Team.
The member positions include: individuals who work with pregnant or postpartum individuals and have expertise in
Clinical Social Work, Community Doula Work, Community Birth Work, provision of behavioral health services, or
social services such as housing or food insecurity; individuals with expertise in Community Health Nursing/Maternal,
Infant, and Early Childhood Health Home Visiting or Nursing Care for Pregnant Individuals, Postpartum Individuals, or
Families of Pregnant or Postpartum Individuals; Individuals with expertise in quality improvement for pregnant or
postpartum patients or pregnant or postpartum patient safety; Physicians with expertise or specialization in
Obstetrics and Gynecology; individuals with expertise in Public Health Epidemiology; physicians with expertise or
specialization in Maternal Fetal Medicine; physicians with expertise or specialization in Addiction Medicine, Family
Medicine, Internal Medicine, Anesthesiology, Critical Care, Emergency Medicine, Pediatrics, Adolescent Medicine,
Preventive Medicine, or Cardiology, specifically Cardio-Obstetrics; Advanced Practice Clinician in Women’s Health
(Certified Nurse Midwife or Women’s Health Nurse Practitioner), representative from the Maternal Mortality
Stakeholder Group, public health officials, State Medicaid, a representative from the Office of the Chief Medical
Examiner.
Title V staff will continue to assess its funding and work towards open competitive procurements to allow various
organizations to apply for funding. Of note, a significant portion of federal Title V funds go towards local health
departments as core public health funding for essential maternal and child health infrastructure. House Bill 314,
Laws of 1995 defined core public health services to include: Communicable Disease Control, Environmental Health,
Maternal and Child Health, Family Planning, Wellness Promotion, Adult Health and Geriatric Services, and
Administration. As a result of House Bill 314, a significant amount of funds from the Maternal Child Health Block
grant must be allocated to the local health departments for maternal and child health-related activities. These
essential activities include addressing elevated lead levels, care coordination for pregnant individuals and infants,
home visiting, school health services, hearing screens and vision screens.
Created on 8/11/2022 at 8:37 PM
Page 171 of 296 pages

III.F. Public Input
During the FY 2022 Application/FY 2020 Annual Report, public input was obtained. The Application/Annual Report
was posted on the Maternal and Child Health Bureau’s Title V webpage for a week after submission. Stakeholder
groups, including local health department grantees were alerted to the posting and provided a direct link. Public
comments were then integrated when applicable and feasible into the Application/Report in FY 2021/FY 2023.
Stakeholders were pleased to see that the equity framework was included in the Title V application. In addition, there
were suggestions to create a comprehensive template/curriculum of how to assess/educate and implement the
MCHB priorities for care coordination for birthing people, infants, and children. One of the comments also noted the
change in a healthcare facility name, and another respondent noted that Maryland Title V used to work with traditional
organizations that worked with families with children and youth with special health care needs, and the change due to
a competitive procurement for organizations to provide services changed the organizations that Maryland Title V
works with.
Based on the feedback, the Maryland Title V team continued to incorporate the equity framework into the Title V
application. In addition, during FY21 and FY22 the Maryland Title V team assessed various care coordination
templates and curricula to incorporate into various care coordination initiatives including Babies Born Healthy and
Title V. The Title V team will continue to build upon the assessments done to improve care coordination in Maryland.
The Office for Genetics and People with Special HealthCare Needs will incorporate the feedback during the next
cycle of competitive procurements to expand relationships with families, medical homes, and transition of care.
Maryland Title V elicited public input on the changes to performance measures particularly to change the national
performance measure from preventive dental care visits to the well woman visit. This change was proposed to further
align Title V with the Statewide Integrated Health Improvement Strategy. Feedback was obtained in late June and
early July 2022, and will be considered for the Title V 2022/2024 application. In addition, feedback was obtained in
June and July to add in a cross cutting measure on equity for the Title V 21/23 application. Feedback was positive
amongst stakeholders, including local health department representatives and therefore added for the Title V 23
application.
After submission of the Application/Annual Report to HRSA and following our Annual Review, the FY 2023
Application/FY 2021 Annual Report will be posted to the Title V webpage on the MDH website. This webpage also
includes the ability for visitors to leave public comments. The website link will be disseminated to local health
departments and other maternal and child health stakeholders for feedback. The Title V Manager is responsible for
addressing the public comments that are received, provide responses, and make recommendations for
incorporation into Title V practice and interventions.
Created on 8/11/2022 at 8:37 PM
Page 172 of 296 pages

III.G. Technical Assistance
Maryland Title V team continued to engage in technical assistance with the MCH Evidence team from Georgetown
University. The Maryland Title V Team assessed ways to align with the Maryland Diabetes Action Plan and the
Statewide Integrated Health Improvement Strategy, specifically in gestational diabetes. The MCH Evidence team
shared information about gestational diabetes with the Maryland Title V Team including various evidence informed
strategies, National Performance Measures, and other states’ Performance Measures. This information was used to
discuss potential performance and strategy measures that Maryland could use. Ultimately because of limited data
availability for gestational diabetes, the Maryland Title V team decided to use a broader measure for women’s health
beginning in FY24, specifically the National Performance Measure of the Well Women Visit and leveraging existing
work with the Maryland Family Planning Program which provides essential reproductive and sexual health services.
In addition, based on the feedback from last year, Maryland Title V worked on a cross cutting state performance
measure, objectives, and evidence-based strategy with the assistance of the MCH Evidence team from Georgetown
University. The Title V team reviewed examples from other states that pursued equity, cross cutting measures and
developed objectives that were specific, measurable, and realistic with the updated SPMs and also for the NPMs.
Maryland Title V will continue its progress with addressing alignment of the State Action Plan and will request
technical assistance to develop more robust evidence-based strategy measures with the MCH Evidence team from
Georgetown University. The Equity Workgroup within the Bureau shared learnings, readings, and developed goals
for the Bureau and Title V.
Given that the Maryland Department of Health’s Network Security Event and staffing transitions delayed work with the
Title V team, Maryland Title V will focus on continuing with health equity technical assistance and the development of
a Title V data system, as well as workforce retention.
Title V Data System
Currently, many local health departments use separate case management systems for their clients. Several local
health departments use paper, spreadsheets, or other databases. A centralized data collection system would allow
the opportunity to collect data in a consistent manner and would benefit Title V greatly. Identifying necessary
components for a Statewide- Title V data system to prevent duplication of data would be helpful. Currently, there are
limited resources and funding to develop a Title V statewide data collection system. However, providing resources or
sharing best practices from other states would assist in reporting to Title V.
Public Health
Overall, local health departments have been working many hours and assumed additional duties to address the
COVID-19 pandemic through testing, contact tracing, linkages to resources, and vaccinations. Many staff have been
re-assigned to COVID duties while still trying to maintain their primary duties. Many staff have been fatigued due to
the workload. Providing resources or sharing best practices from other states would assist in ways that Title V can
help with retaining the MCH workforce.
Created on 8/11/2022 at 8:37 PM
Page 173 of 296 pages

VII. Appendix
+
This page is intentionally left blank.
Created on 8/11/2022 at 8:37 PM
Page 177 of 296 pages

Form 2
MCH Budget/Expenditure Details
State: Maryland
FY 23 Application Budgeted
1. FEDERAL ALLOCATION
(Referenced items on the Application Face Sheet [SF-424] apply only to the
Application Year)
$ 11,981,449
A. Preventive and Primary Care for Children $ 3,770,104 (31.4%)
B. Children with Special Health Care Needs $ 4,747,066 (39.6%)
C. Title V Administrative Costs $ 469,509 (4%)
2. Subtotal of Lines 1A-C
(This subtotal does not include Pregnant Women and All Others)
$ 8,986,679
3. STATE MCH FUNDS
(Item 18c of SF-424)
$ 9,023,964
4. LOCAL MCH FUNDS
(Item 18d of SF-424)
$ 0
5. OTHER FUNDS
(Item 18e of SF-424)
$ 0
6. PROGRAM INCOME
(Item 18f of SF-424)
$ 0
7. TOTAL STATE MATCH
(Lines 3 through 6)
$ 9,023,964
A. Your State's FY 1989 Maintenance of Effort Amount
$ 8,262,484
8. FEDERAL-STATE TITLE V BLOCK GRANT PARTNERSHIP SUBTOTAL
(Total lines 1 and 7)
$ 21,005,413
9. OTHER FEDERAL FUNDS
10. OTHER FEDERAL FUNDS(Subtotal of all funds under item 9) $ 123,038,688
11. STATE MCH BUDGET/EXPENDITURE GRAND TOTAL
(Partnership Subtotal + Other Federal MCH Funds Subtotal)
$ 144,044,101
Please refer to the next page to view the list of Other Federal Programs provided by the State on Form 2.
Created on 8/11/2022 at 8:37 PM
Page 178 of 296 pages
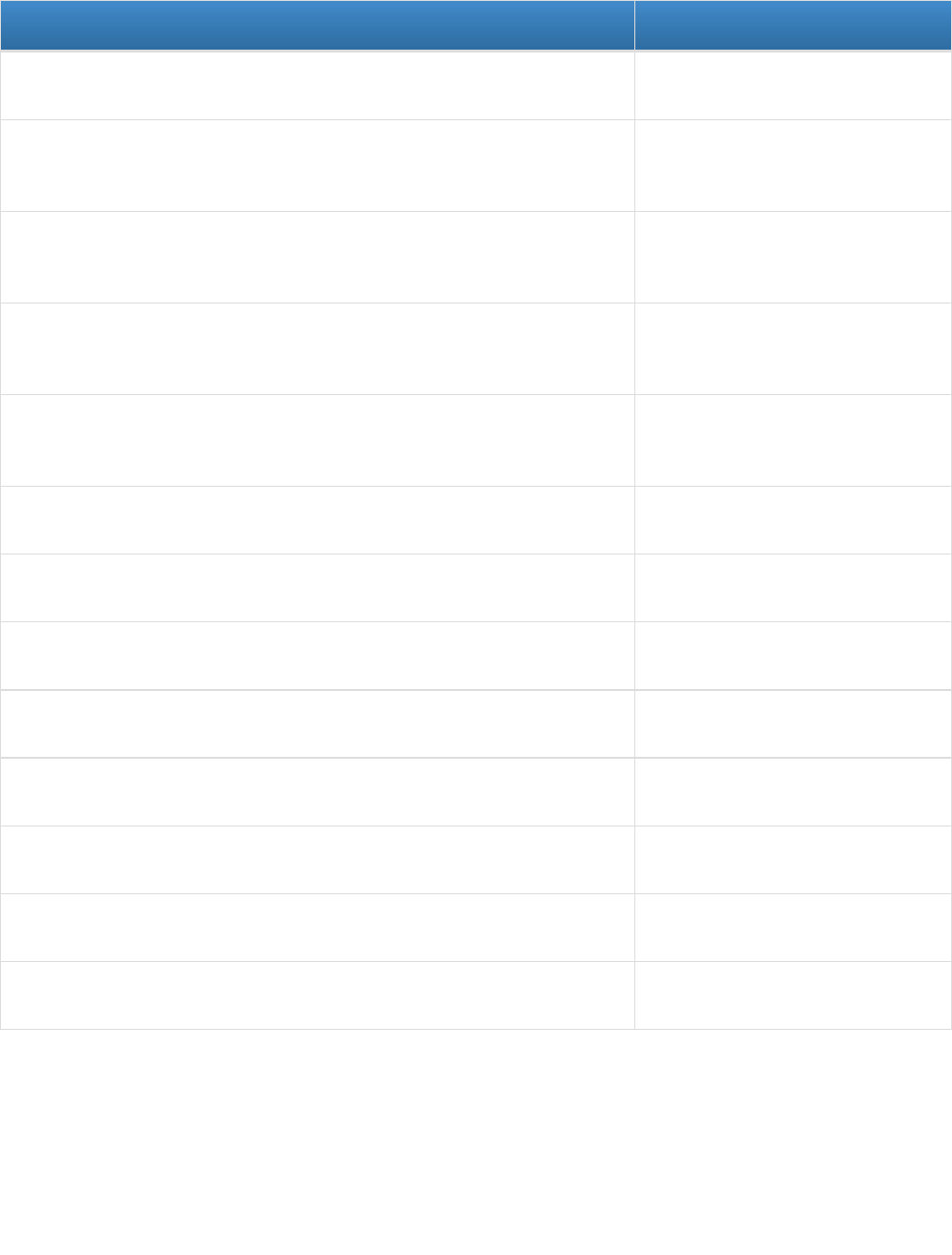
OTHER FEDERAL FUNDS
FY 23 Application Budgeted
Department of Health and Human Services (DHHS) > Administration for Children &
Families (ACF) > Sexual Risk Avoidance Education (SRAE)
$ 760,253
Department of Health and Human Services (DHHS) > Centers for Disease Control
and Prevention (CDC) > Pregnancy Risk Assessment Monitoring System
(PRAMS)
$ 160,020
Department of Health and Human Services (DHHS) > Centers for Disease Control
and Prevention (CDC) > Sudden Unexpected Infant Death (SUID) Case Registry
Program
$ 86,095
Department of Health and Human Services (DHHS) > Health Resources and
Services Administration (HRSA) > Maternal, Infant, and Early Childhood Home
Visiting Program (MIECHV) Formula Grants
$ 7,506,158
Department of Health and Human Services (DHHS) > Health Resources and
Services Administration (HRSA) > Universal Newborn Hearing Screening and
Intervention
$ 370,907
Department of Health and Human Services (DHHS) > Health Resources and
Services Administration (HRSA) > State Systems Development Initiative (SSDI)
$ 38,630
Department of Health and Human Services (DHHS) > Office of Population Affairs
(OPA) > Title X Family Planning
$ 4,000,000
US Department of Agriculture (USDA) > Food and Nutrition Services > Women,
Infants and Children (WIC)
$ 106,147,025
Department of Health and Human Services (DHHS) > Administration for Children &
Families (ACF) > PREP
$ 935,663
Department of Health and Human Services (DHHS) > Office of Population Affairs
(OPA) > State Optimal Adolescent Health Program
$ 1,697,965
Department of Health and Human Services (DHHS) > Health Resources and
Services Administration (HRSA) > MIECHV Expansion
$ 802,559
Department of Health and Human Services (DHHS) > Centers for Disease Control
and Prevention (CDC) > Optimization of EHDI Surveillance
$ 160,000
Department of Health and Human Services (DHHS) > Centers for Disease Control
and Prevention (CDC) > Strengthening Maternal Mortality Surveillance
$ 373,413
Created on 8/11/2022 at 8:37 PM
Page 179 of 296 pages
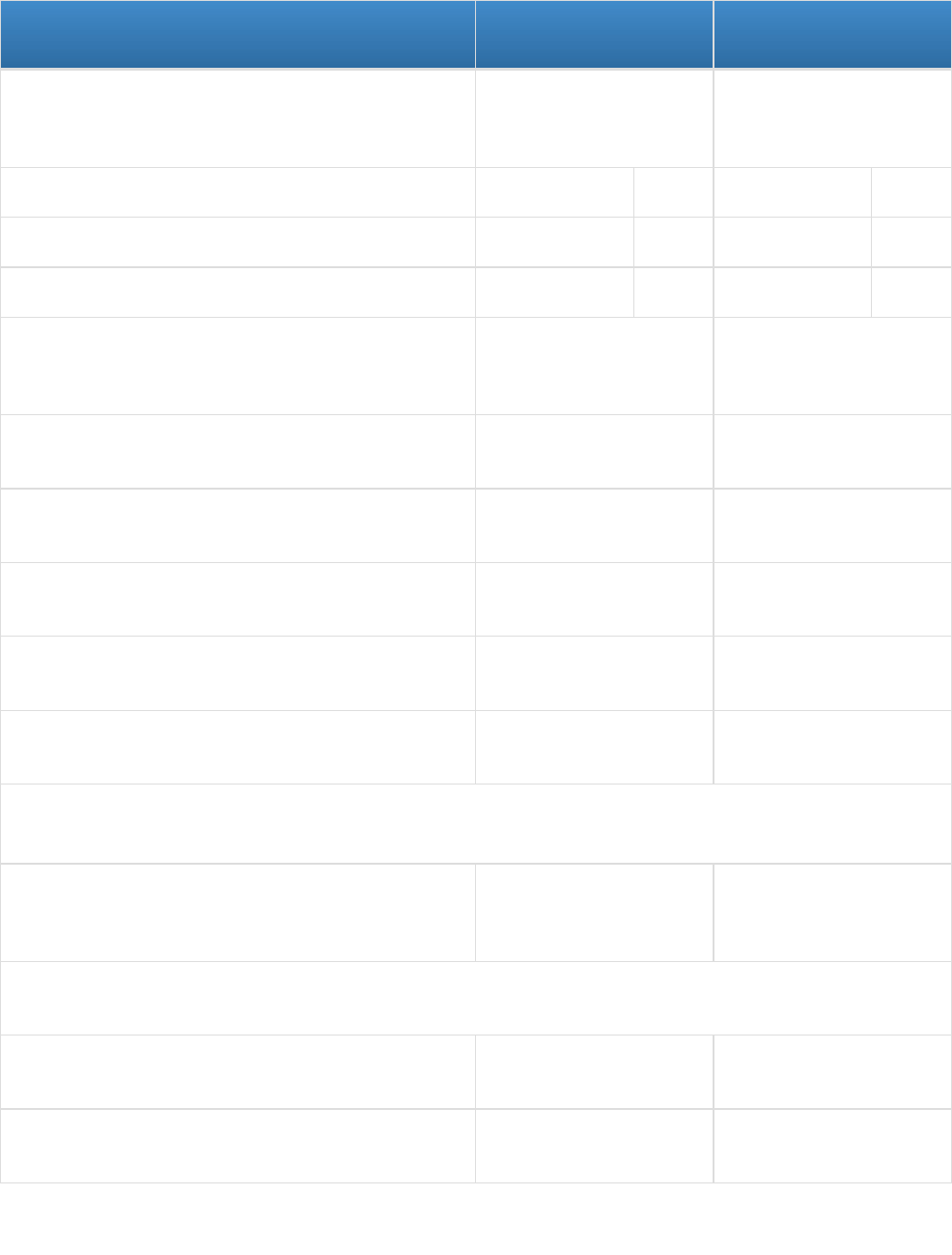
FY 21 Annual Report
Budgeted
FY 21 Annual Report
Expended
1. FEDERAL ALLOCATION
(Referenced items on the Application Face Sheet [SF-424]
apply only to the Application Year)
$ 11,673,326
(FY 21 Federal Award:
$ 11,872,645)
$ 11,872,645
A. Preventive and Primary Care for Children $ 3,649,163 (31.3%) $ 3,954,551 (33.3%)
B. Children with Special Health Care Needs $ 3,671,343 (31.5%) $ 5,291,767 (44.5%)
C. Title V Administrative Costs $ 453,200 (3.9%) $ 237,976 (2.1%)
2. Subtotal of Lines 1A-C
(This subtotal does not include Pregnant Women and All
Others)
$ 7,773,706 $ 9,484,294
3. STATE MCH FUNDS
(Item 18c of SF-424)
$ 8,754,995 $ 10,999,716
4. LOCAL MCH FUNDS
(Item 18d of SF-424)
$ 0 $ 0
5. OTHER FUNDS
(Item 18e of SF-424)
$ 0 $ 0
6. PROGRAM INCOME
(Item 18f of SF-424)
$ 0 $ 0
7. TOTAL STATE MATCH
(Lines 3 through 6)
$ 8,754,995 $ 10,999,716
A. Your State's FY 1989 Maintenance of Effort Amount
$ 8,262,484
8. FEDERAL-STATE TITLE V BLOCK GRANT
PARTNERSHIP SUBTOTAL
(Total lines 1 and 7)
$ 20,428,321 $ 22,872,361
9. OTHER FEDERAL FUNDS
10. OTHER FEDERAL FUNDS (Subtotal of all funds under
item 9)
$ 118,199,750 $ 88,972,950
11. STATE MCH BUDGET/EXPENDITURE GRAND TOTAL
(Partnership Subtotal + Other Federal MCH Funds Subtotal)
$ 138,628,071 $ 111,845,311
Please refer to the next page to view the list of Other Federal Programs provided by the State on Form 2.
Created on 8/11/2022 at 8:37 PM
Page 180 of 296 pages

OTHER FEDERAL FUNDS
FY 21 Annual Report
Budgeted
FY 21 Annual Report
Expended
Department of Health and Human Services (DHHS) >
Administration for Children & Families (ACF) > Sexual Risk
Avoidance Education (SRAE)
$ 831,903 $ 573,626
Department of Health and Human Services (DHHS) >
Administration for Children & Families (ACF) > State
Personal Responsibility Education Program (PREP)
$ 944,604 $ 808,466
Department of Health and Human Services (DHHS) >
Centers for Disease Control and Prevention (CDC) >
Pregnancy Risk Assessment Monitoring System (PRAMS)
$ 161,000 $ 161,000
Department of Health and Human Services (DHHS) >
Centers for Disease Control and Prevention (CDC) >
Sudden Unexpected Infant Death (SUID) Case Registry
Program
$ 75,000 $ 22,767
Department of Health and Human Services (DHHS) > Health
Resources and Services Administration (HRSA) > Maternal,
Infant, and Early Childhood Home Visiting Program (MIECHV)
Formula Grants
$ 751,102 $ 8,248,192
US Department of Agriculture (USDA) > Food and Nutrition
Services > Women, Infants and Children (WIC)
$ 115,191,574 $ 79,049,808
Department of Health and Human Services (DHHS) > Health
Resources and Services Administration (HRSA) > Universal
Newborn Hearing Screening and Intervention
$ 244,567 $ 109,091
Created on 8/11/2022 at 8:37 PM
Page 181 of 296 pages

Form Notes for Form 2:
None
Field Level Notes for Form 2:
1. Field Name: 1. FEDERAL ALLOCATION
Fiscal Year: 2023
Column Name: Application Budgeted
Field Note:
$11,872,645
2. Field Name: Federal Allocation, B. Children with Special Health Care Needs:
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
Amount is higher than originally annual budgeted as CMS enrollment was high during FY21 and during the COVID
pandemic
3. Field Name: Federal Allocation, C. Title V Administrative Costs:
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
FY21, the Title V administrative costs were lower due to staffing transitions due to COVID-19 Pandemic
4. Field Name: 3. STATE MCH FUNDS
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
State MCH Funds were higher as originally budgeted as state funds for the Maryland Family Planning Program
were not previously accounted for in developing the FY21 budget
5. Field Name: Other Federal Funds, Department of Health and Human Services (DHHS) >
Health Resources and Services Administration (HRSA) > Maternal, Infant,
and Early Childhood Home Visiting Program (MIECHV) Formula Grants
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
Budget expenditures were higher than the original budget amount, that listed the budget amount for FY21
incorrectly.
Created on 8/11/2022 at 8:37 PM
Page 182 of 296 pages

Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 183 of 296 pages

Form 3a
Budget and Expenditure Details by Types of Individuals Served
State: Maryland
IA. Federal MCH Block Grant
FY 23 Application
Budgeted
FY 21 Annual Report
Expended
1. Pregnant Women $ 1,527,945 $ 1,800,811
2. Infants < 1 year $ 1,466,825 $ 587,540
3. Children 1 through 21 Years $ 3,770,104 $ 3,954,551
4. CSHCN $ 4,747,066 $ 5,291,767
5. All Others $ 0 $ 0
Federal Total of Individuals Served $ 11,511,940 $ 11,634,669
IB. Non-Federal MCH Block Grant
FY 23 Application
Budgeted
FY 21 Annual Report
Expended
1. Pregnant Women $ 4,790,614 $ 4,281,182
2. Infants < 1 year $ 1,788,342 $ 1,517,184
3. Children 1 through 21 Years $ 1,545,008 $ 2,107,351
4. CSHCN $ 900,000 $ 400,000
5. All Others $ 0 $ 2,693,998
Non-Federal Total of Individuals Served $ 9,023,964 $ 10,999,715
Federal State MCH Block Grant Partnership Total $ 20,535,904 $ 22,634,384
I. TYPES OF INDIVIDUALS SERVED
Created on 8/11/2022 at 8:37 PM
Page 184 of 296 pages

Form Notes for Form 3a:
None
Field Level Notes for Form 3a:
1. Field Name: IB. Non-Federal MCH Block Grant, 1. Pregnant Women
Fiscal Year: 2023
Column Name: Application Budgeted
Field Note:
Includes: Family Planning, Babies Born Healthy, Perinatal Support Program, Perinatal Quality Collaborative,
Thrive by Three
2. Field Name: IB. Non-Federal MCH Block Grant, 2. Infant < 1 Year
Fiscal Year: 2023
Column Name: Application Budgeted
Field Note:
Includes Babies Born Healthy, Perinatal Support Program, Perinatal Quality Collaborative, Thrive by Three
3. Field Name: IB. Non-Federal MCH Block Grant, 3. Children 1 through 21 years
Fiscal Year: 2023
Column Name: Application Budgeted
Field Note:
Includes Surveillance Quality Initiatives, Child Abuse Medical Provider Network,
4. Field Name: IB. Non-Federal MCH Block Grant, 4. CSHCN
Fiscal Year: 2023
Column Name: Application Budgeted
Field Note:
Direct services for Medical Day Care and funding for Children Medical Services
5. Field Name: IB. Non-Federal MCH Block Grant, 1. Pregnant Women
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
Includes: Family Planning, Babies Born Healthy, Perinatal Support Program, Perinatal Quality Collaborative,
Thrive by Three
6. Field Name: IB. Non-Federal MCH Block Grant, 2. Infant < 1 Year
Fiscal Year: 2021
Created on 8/11/2022 at 8:37 PM
Page 185 of 296 pages
Column Name: Annual Report Expended
Field Note:
Includes Babies Born Healthy, Perinatal Support Program, Perinatal Quality Collaborative, Thrive by Three
7. Field Name: IB. Non-Federal MCH Block Grant, 3. Children 1 through 21 years
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
Included SQI, CHAMP and Child Health Systems Improvement
8. Field Name: IB. Non-Federal MCH Block Grant, 4. CSHCN
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
Direct services for Medical Day Care
9. Field Name: IB. Non-Federal MCH Block Grant, 5. All Others
Fiscal Year: 2021
Column Name: Annual Report Expended
Field Note:
Includes Family Planning
Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 186 of 296 pages

Form 3b
Budget and Expenditure Details by Types of Services
State: Maryland
IIA. Federal MCH Block Grant
FY 23 Application
Budgeted
FY 21 Annual Report
Expended
1. Direct Services $ 1,758,114 $ 4,607,864
A. Preventive and Primary Care Services for all
Pregnant Women, Mothers, and Infants up to Age One
$ 0 $ 1,133,192
B. Preventive and Primary Care Services for Children $ 0 $ 0
C. Services for CSHCN $ 1,758,114 $ 3,474,672
2. Enabling Services $ 6,348,186 $ 4,517,481
3. Public Health Services and Systems $ 3,875,149 $ 2,747,300
4. Select the types of Federally-supported "Direct Services", as reported in II.A.1. Provide the total amount of Federal MCH
Block Grant funds expended for each type of reported service
Pharmacy $ 1,019,523
Physician/Office Services $ 1,299,286
Hospital Charges (Includes Inpatient and Outpatient Services) $ 1,725,151
Dental Care (Does Not Include Orthodontic Services) $ 13,885
Durable Medical Equipment and Supplies $ 146,136
Laboratory Services $ 0
Other
Purchase of Care for CMS $ 225,495
Genetic Services $ 178,388
Direct Services Line 4 Expended Total $ 4,607,864
Federal Total $ 11,981,449 $ 11,872,645
II. TYPES OF SERVICES
Created on 8/11/2022 at 8:37 PM
Page 187 of 296 pages

IIB. Non-Federal MCH Block Grant
FY 23 Application
Budgeted
FY 21 Annual Report
Expended
1. Direct Services $ 3,708,724 $ 3,132,160
A. Preventive and Primary Care Services for all
Pregnant Women, Mothers, and Infants up to Age One
$ 2,808,724 $ 2,732,160
B. Preventive and Primary Care Services for Children $ 0 $ 0
C. Services for CSHCN $ 900,000 $ 400,000
2. Enabling Services $ 2,351,797 $ 3,452,784
3. Public Health Services and Systems $ 2,963,443 $ 1,720,773
4. Select the types of Non-Federally-supported "Direct Services", as reported in II.B.1. Provide the total amount of Non-
Federal MCH Block Grant funds expended for each type of reported service
Pharmacy $ 0
Physician/Office Services $ 2,732,160
Hospital Charges (Includes Inpatient and Outpatient Services) $ 0
Dental Care (Does Not Include Orthodontic Services) $ 0
Durable Medical Equipment and Supplies $ 0
Laboratory Services $ 0
Other
Medical Day Care $ 400,000
Direct Services Line 4 Expended Total $ 3,132,160
Non-Federal Total $ 9,023,964 $ 8,305,717
Created on 8/11/2022 at 8:37 PM
Page 188 of 296 pages

Form Notes for Form 3b:
None
Field Level Notes for Form 3b:
None
Created on 8/11/2022 at 8:37 PM
Page 189 of 296 pages

Form 4
Number and Percentage of Newborns and Others Screened Cases Confirmed and Treated
State: Maryland
Total Births by Occurrence: 73,009 Data Source Year: 2021
1. Core RUSP Conditions
Program Name
(A) Aggregate
Total Number
Receiving at
Least One Valid
Screen
(B) Aggregate
Total Number of
Out-of-Range
Results
(C) Aggregate
Total Number
Confirmed
Cases
(D) Aggregate
Total Number
Referred for
Treatment
Core RUSP Conditions 73,009
(100.0%)
1,729 191 191
(100.0%)
Program Name(s)
3-Hydroxy-3-
Methyglutaric
Aciduria
3-Methylcrotonyl-
Coa Carboxylase
Deficiency
Argininosuccinic
Aciduria
Biotinidase
Deficiency
Carnitine Uptake
Defect/Carnitine Transport
Defect
Citrullinemia,
Type I
Classic
Galactosemia
Classic
Phenylketonuria
Congenital Adrenal
Hyperplasia
Critical Congenital Heart
Disease
Cystic Fibrosis Glutaric Acidemia
Type I
Glycogen Storage
Disease Type II
(Pompe)
Hearing Loss Holocarboxylase Synthase
Deficiency
Homocystinuria Isovaleric Acidemia Long-Chain L-3
Hydroxyacyl-Coa
Dehydrogenase
Deficiency
Maple Syrup Urine
Disease
Medium-Chain Acyl-Coa
Dehydrogenase Deficiency
Methylmalonic
Acidemia
(Cobalamin
Disorders)
Methylmalonic
Acidemia
(Methylmalonyl-
Coa Mutase)
Mucopolysaccharidosis
Type 1
Primary Congenital
Hypothyroidism
Propionic Acidemia
S, ßeta-
Thalassemia
S,C Disease S,S Disease (Sickle
Cell Anemia)
Severe Combined
Immunodeficiences
Spinal Muscular Atrophy
Due To Homozygous
Deletion Of Exon 7 In SMN1
ß-Ketothiolase
Deficiency
Trifunctional
Protein Deficiency
Tyrosinemia, Type I Very Long-Chain
Acyl-Coa
Dehydrogenase
Deficiency
X-Linked
Adrenoleukodystrophy
Created on 8/11/2022 at 8:37 PM
Page 190 of 296 pages

2. Other Newborn Screening Tests
Program Name
(A) Total
Number
Receiving at
Least One
Screen
(B) Total
Number
Presumptive
Positive
Screens
(C) Total
Number
Confirmed
Cases
(D) Total
Number
Referred for
Treatment
Fabry Disease 73,009
(100.0%)
91 6 6
(100.0%)
3. Screening Programs for Older Children & Women
None
4. Long-Term Follow-Up
The Sickle Cell Disease Long-Term Follow up Program follows children diagnosed with sickle cell disease through age
18. The program continues to focus on childhood preventive care standards and provide education and assistance
through transition into adulthood. In FY 2021, 596 children were being followed in the program.
Created on 8/11/2022 at 8:37 PM
Page 191 of 296 pages

Form Notes for Form 4:
None
Field Level Notes for Form 4:
1. Field Name: Total Births by Occurrence
Fiscal Year: 2021
Column Name: Total Births by Occurrence Notes
Field Note:
The discrepancy from Form 6 is due to the fact that these numbers may also include out-of-state residents
and repeat screens. Of note, this form uses data from 2021 and not 2020.
2. Field Name: Core RUSP Conditions - Total Number of Out-of-Range Results
Fiscal Year: 2021
Column Name: Core RUSP Conditions
Field Note:
Due to the Network Security Event, the number of out of range results are unavailable from MDH laboratories.
Current numbers are based on referrals made for diagnostic testing for each of the conditions, so the number
of out of range results does not include cases where a repeat specimen was included.
Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 192 of 296 pages

Form 5
Count of Individuals Served by Title V & Total Percentage of Populations Served by Title V
State: Maryland
Annual Report Year 2021
Form 5a – Count of Individuals Served by Title V
(Direct & Enabling Services Only)
Primary Source of Coverage
Types Of Individuals Served
(A) Title V Total
Served
(B)
Title
XIX %
(C)
Title
XXI %
(D)
Private
/ Other
%
(E)
None
%
(F)
Unknown
%
1. Pregnant Women 2,991 39.0 0.0 58.0 3.0 0.0
2. Infants < 1 Year of Age 4,055 0.0 39.0 58.0 3.0 0.0
3. Children 1 through 21 Years of Age 167,491 0.0 32.0 63.0 4.0 1.0
3a. Children with Special Health
Care Needs 0 through 21
years of age^
64,330 0.0 32.0 65.0 3.0 0.0
4. Others 53,875 14.0 0.0 79.0 7.0 0.0
Total 228,412
Form 5b – Total Percentage of Populations Served by Title V
(Direct, Enabling, and Public Health Services and Systems)
Populations Served by Title V
Reference
Data
Used
Reference
Data? Denominator
Total %
Served
Form 5b
Count
(Calculated)
Form 5a
Count
1. Pregnant Women 68,554 Yes 68,554 100.0 68,554 2,991
2. Infants < 1 Year of Age 65,536 Yes 65,536 100.0 65,536 4,055
3. Children 1 through 21 Years of
Age
1,565,086 Yes 1,565,086 100.0 1,565,086 167,491
3a. Children with Special Health
Care Needs 0 through 21
years of age^
335,107 Yes 335,107 100.0 335,107 64,330
4. Others 4,421,133 Yes 4,421,133 1.5 66,317 53,875
^Represents a subset of all infants and children.
Created on 8/11/2022 at 8:37 PM
Page 193 of 296 pages

Form Notes for Form 5:
None
Created on 8/11/2022 at 8:37 PM
Page 194 of 296 pages

Field Level Notes for Form 5a:
1. Field Name: Pregnant Women Total Served
Fiscal Year: 2021
Field Note:
Due to the COVID-19 pandemic, clinics and programs were serving at limited capacity. Pregnant people receiving
services though Title V funded programs including Local Health Department, Child Health System Improvements,
BBH, Family Planning Clinics
2. Field Name: Infants Less Than One YearTotal Served
Fiscal Year: 2021
Field Note:
Includes all Newborn Screenings, local health department data for Title V programs providing home visits, case
management for elevated blood levels, immunizations, home birth certification, and health education for parents
and linkages to primary care.
3. Field Name: Children 1 through 21 Years of Age
Fiscal Year: 2021
Field Note:
Due to the COVID-19 pandemic, clinics and programs were serving at limited capacity. Children receiving services
through LHDs including school-based health services and family planning clinics. This includes Child Health
Systems Improvement
4. Field Name: Children with Special Health Care Needs 0 through 21 Years of Age
Fiscal Year: 2021
Field Note:
Due to the COVID-19 pandemic, clinics and programs were serving at limited capacity. CYSHCN receiving services
through grantees of the Office for Genetics and People with Special HealthCare Needs and local health
departments.
5. Field Name: Others
Fiscal Year: 2021
Field Note:
Others receiving services through local health department reproductive health clinics.
6. Field Name: Total_TotalServed
Fiscal Year: 2021
Field Note:
Overall, due to the COVID-19 pandemic, clinics and programs were serving at limited capacity
Created on 8/11/2022 at 8:37 PM
Page 195 of 296 pages
Field Level Notes for Form 5b:
1. Field Name: Pregnant Women Total % Served
Fiscal Year: 2021
Field Note:
Pregnant individuals delivering at hospitals that are participating in the Maryland Perinatal Collaborative, Babies
Born Healthy program, local health department home visiting program, PRAMS, and perinatal Regionalization
guidelines who focus on all pregnant people in Maryland.
2. Field Name: Infants Less Than One Year Total % Served
Fiscal Year: 2021
Field Note:
Number reflects the efforts of newborn screening and early hearing detection which reaches 100% of infants in
Maryland
3. Field Name: Children 1 through 21 Years of Age Total % Served
Fiscal Year: 2021
Field Note:
*Represents efforts of local health departments from direct and enabling services, communication health
campaigns, vision and hearing screenings, immunizations, and injury prevention. Child Fatality Review has also
developed recommendations for children ages, 1-17.
4. Field Name: Children with Special Health Care Needs 0 through 21 Years of Age Total
% Served
Fiscal Year: 2021
Field Note:
Represents direct, enabling, and population bases services through CYSHCN through complex care, navigation
services, training/education, accessing medical homes, care coordination, genetic services, medical services,
follow-up to newborn screening, birth defects, sickle cell program, early intervention for hearing, resource locator,
adult transitions through OGPSHCN, local health departments, and Title V grantees
5. Field Name: Others Total % Served
Fiscal Year: 2021
Field Note:
Overall, these numbers represent health education sessions for providers, parents, local health departments,
communications, as well as direct and enabling services from local health departments and other programs.
Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 196 of 296 pages

Form 6
Deliveries and Infants Served by Title V and Entitled to Benefits Under Title XIX
State: Maryland
Annual Report Year 2021
I. Unduplicated Count by Race/Ethnicity
(A)
Total
(B) Non-
Hispanic
White
(C) Non-
Hispanic
Black or
African
American
(D)
Hispanic
(E) Non-
Hispanic
American
Indian or
Native
Alaskan
(F) Non-
Hispanic
Asian
(G) Non-
Hispanic
Native
Hawaiian
or Other
Pacific
Islander
(H) Non-
Hispanic
Multiple
Race
(I) Other
&
Unknown
1. Total
Deliveries in
State
68,546 28,782 21,631 13,020 114 4,739 0 0 260
Title V
Served
68,546 28,782 21,631 13,020 114 4,739 0 0 260
Eligible for
Title XIX
43,610 10,161 17,651 5,784 113 1,865 0 0 8,036
2. Total
Infants in
State
69,583 28,399 22,322 14,059 169 4,634 0 0 0
Title V
Served
69,583 28,399 22,322 14,059 169 4,634 0 0 0
Eligible for
Title XIX
36,214 5,672 9,015 2,638 108 1,545 0 0 17,236
Created on 8/11/2022 at 8:37 PM
Page 197 of 296 pages

Form Notes for Form 6:
Data in this form is based on the most recently available date, which is from 2020.
Field Level Notes for Form 6:
1. Field Name: 2. Total Infants in State
Fiscal Year: 2021
Column Name: Total
Field Note:
The discrepancy between Total # of Infants in State on Form 6 and Total Births on Form 4 is due to different
reporting years. VSA data used for Form 6 are from 2020. Births used for Form 4 are from 2021 and from the
Office for Genetics and People with Special Health Care Needs. In addition, the Form 4 numbers may include
repeat screens and births from out of state residents.
Created on 8/11/2022 at 8:37 PM
Page 198 of 296 pages

Form 7
State MCH Toll-Free Telephone Line and Other Appropriate Methods Data
State: Maryland
A. State MCH Toll-Free Telephone Lines 2023 Application Year 2021 Annual Report Year
1. State MCH Toll-Free "Hotline" Telephone Number (800) 456-8900 (800) 456-8900
2. State MCH Toll-Free "Hotline" Name MDH Medicaid for Pregnant
Women
MDH Medicaid for Pregnant
Women
3. Name of Contact Person for State MCH "Hotline" Maryland HealthChoice Maryland HealthChoice
4. Contact Person's Telephone Number (800) 456-8900 (800) 456-8900
5. Number of Calls Received on the State MCH "Hotline" 507
B. Other Appropriate Methods 2023 Application Year 2021 Annual Report Year
1. Other Toll-Free "Hotline" Names N/A N/A
2. Number of Calls on Other Toll-Free "Hotlines" 0
3. State Title V Program Website Address https://health.maryland.gov/p
hpa/mch/Pages/titlev.aspx
https://health.maryland.gov/p
hpa/mch/Pages/titlev.aspx
4. Number of Hits to the State Title V Program Website 45,628
5. State Title V Social Media Websites N/A N/A
6. Number of Hits to the State Title V Program Social Media
Websites
0
Created on 8/11/2022 at 8:37 PM
Page 199 of 296 pages

Form Notes for Form 7:
None
Created on 8/11/2022 at 8:37 PM
Page 200 of 296 pages

Form 8
State MCH and CSHCN Directors Contact Information
State: Maryland
1. Title V Maternal and Child Health (MCH) Director
Name Shelly Choo, MD, MPH
Title Director, Maternal and Child Health Bureau
Address 1 201 W. Preston Street
Address 2
City/State/Zip Baltimore / MD / 21201
Telephone (443) 571-3424
Extension
Email [email protected]
2. Title V Children with Special Health Care Needs (CSHCN) Director
Name Stacy Taylor
Title Acting Director, Office of Genetics and People with Special Health Care Needs
Address 1 201 W. Preston Street
Address 2
City/State/Zip Baltimore / MD / 21201
Telephone (443) 997-0433
Extension
Email [email protected]
Created on 8/11/2022 at 8:37 PM
Page 201 of 296 pages

3. State Family or Youth Leader (Optional)
Name N/A
Title N/A
Address 1 N/A
Address 2
City/State/Zip Baltimore / MD / 21201
Telephone (410) 550-2021
Extension
Email [email protected]
Created on 8/11/2022 at 8:37 PM
Page 202 of 296 pages

Form Notes for Form 8:
None
Created on 8/11/2022 at 8:37 PM
Page 203 of 296 pages
Form 9
List of MCH Priority Needs
State: Maryland
Application Year 2023
No. Priority Need
1. Ensure that all babies are born healthy and prosper in their first year
2. Ensure that adolescents age 12-17 receive comprehensive well visits that address physical, reproductive,
and behavioral health needs.
3. Ensure optimal health and quality of life for all CYSHCN and their families by providing all services within an
effective system of care in alignment with the Six Core Outcomes
4. Ensure that all birthing people are in optimal health before, during, and after pregnancy
5. Ensure that all children have an opportunity to develop and reach their full potential
6. Ensure children with asthma and their families have the tools and supports necessary to manage their
condition so that it does not impede their daily activities
7. Address the racial disparities in Severe Maternal Morbidity rates among Black NH and White NH
8. Ensure that MCHB policies and processes are centered on equity and anti-racism principles
Created on 8/11/2022 at 8:37 PM
Page 204 of 296 pages

Form Notes for Form 9:
Additional Priority Need for SFY 23:
Ensure that MCHB policies and processes are centered on equity and anti-racism principles
Field Level Notes for Form 9:
None
Created on 8/11/2022 at 8:37 PM
Page 205 of 296 pages

Form 9 State Priorities – Needs Assessment Year – Application Year 2021
No. Priority Need
Priority Need Type (New,
Revised or Continued
Priority Need for this five-
year reporting period)
1. Risk Appropriate Perinatal Care New
2. Breastfeeding New
3. Safe Sleep Continued
4. Adolescent Well Visit Continued
5. Medical Home Continued
6. Transitions Continued
7. Preventive Dental Visit-Pregnancy Continued
8. Smoking-Pregnancy Continued
9. Child Developmental Screenings Continued
Created on 8/11/2022 at 8:37 PM
Page 206 of 296 pages
Form 10
National Outcome Measures (NOMs)
State: Maryland
Form Notes for Form 10 NPMs, NOMs, SPMs, SOMs, and ESMs.
None
NOM 1 - Percent of pregnant women who receive prenatal care beginning in the first trimester
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 75.1 % 0.2 % 49,581 65,990
2019 74.5 % 0.2 % 49,981 67,069
2018 74.6 % 0.2 % 50,559 67,772
2017 73.8 % 0.2 % 50,375 68,265
2016 72.0 % 0.2 % 49,044 68,127
2015 71.1 % 0.2 % 48,674 68,505
2014 70.6 % 0.2 % 48,351 68,446
2013 67.4 % 0.2 % 44,741 66,393
2012 68.0 % 0.2 % 47,698 70,186
2011 67.7 % 0.2 % 45,046 66,571
2010 68.9 % 0.2 % 41,490 60,199
Legends:
NOM 1 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20, a confidence interval width >20% points or >1.2 times the estimate, or >10% missing data and should be interpreted with
caution
Created on 8/11/2022 at 8:37 PM
Page 207 of 296 pages

NOM 2 - Rate of severe maternal morbidity per 10,000 delivery hospitalizations
Data Source: HCUP - State Inpatient Databases (SID)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 79.3 3.5 517 65,195
2018 82.9 3.5 566 68,272
2017 80.3 3.4 554 68,950
2016 66.0 3.1 466 70,576
2015 67.7 3.6 357 52,704
2014 73.2 3.2 514 70,180
2013 77.7 3.4 532 68,449
2012 81.2 3.5 532 65,480
2011 99.8 3.9 648 64,928
2010 115.7 4.2 758 65,530
2009 102.8 3.9 688 66,896
2008 88.0 3.6 602 68,385
Legends:
NOM 2 - Notes:
None
Data Alerts: None
Indicator has a numerator ≤10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 208 of 296 pages

NOM 3 - Maternal mortality rate per 100,000 live births
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2016_2020 17.8 2.2 63 354,589
2015_2019 17.5 2.2 63 359,651
2014_2018 18.7 2.3 68 363,394
Legends:
NOM 3 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 209 of 296 pages
NOM 4 - Percent of low birth weight deliveries (<2,500 grams)
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 8.5 % 0.1 % 5,792 68,521
2019 8.7 % 0.1 % 6,111 70,147
2018 8.8 % 0.1 % 6,266 71,038
2017 8.9 % 0.1 % 6,375 71,599
2016 8.5 % 0.1 % 6,248 73,085
2015 8.6 % 0.1 % 6,297 73,585
2014 8.6 % 0.1 % 6,345 73,878
2013 8.5 % 0.1 % 6,088 71,913
2012 8.8 % 0.1 % 6,417 72,839
2011 8.9 % 0.1 % 6,466 73,037
2010 8.8 % 0.1 % 6,474 73,766
2009 9.1 % 0.1 % 6,836 75,014
Legends:
NOM 4 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20, a confidence interval width >20% points or >1.2 times the estimate, or >10% missing data and should be interpreted with
caution
Created on 8/11/2022 at 8:37 PM
Page 210 of 296 pages

NOM 5 - Percent of preterm births (<37 weeks)
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 10.1 % 0.1 % 6,941 68,524
2019 10.3 % 0.1 % 7,211 70,130
2018 10.2 % 0.1 % 7,231 71,034
2017 10.5 % 0.1 % 7,491 71,592
2016 10.1 % 0.1 % 7,408 73,088
2015 10.0 % 0.1 % 7,380 73,567
2014 10.1 % 0.1 % 7,455 73,871
2013 9.8 % 0.1 % 7,053 71,758
2012 10.3 % 0.1 % 7,461 72,698
2011 10.2 % 0.1 % 7,469 72,875
2010 10.4 % 0.1 % 7,662 73,613
2009 10.4 % 0.1 % 7,820 74,936
Legends:
NOM 5 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20, a confidence interval width >20% points or >1.2 times the estimate, or >10% missing data and should be interpreted with
caution
Created on 8/11/2022 at 8:37 PM
Page 211 of 296 pages

NOM 6 - Percent of early term births (37, 38 weeks)
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 27.4 % 0.2 % 18,765 68,524
2019 27.3 % 0.2 % 19,129 70,130
2018 26.1 % 0.2 % 18,564 71,034
2017 26.1 % 0.2 % 18,669 71,592
2016 25.4 % 0.2 % 18,585 73,088
2015 25.0 % 0.2 % 18,376 73,567
2014 24.6 % 0.2 % 18,160 73,871
2013 24.6 % 0.2 % 17,686 71,758
2012 24.6 % 0.2 % 17,860 72,698
2011 24.4 % 0.2 % 17,771 72,875
2010 24.9 % 0.2 % 18,357 73,613
2009 25.1 % 0.2 % 18,835 74,936
Legends:
NOM 6 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20, a confidence interval width >20% points or >1.2 times the estimate, or >10% missing data and should be interpreted with
caution
Created on 8/11/2022 at 8:37 PM
Page 212 of 296 pages

NOM 7 - Percent of non-medically indicated early elective deliveries
Data Source: CMS Hospital Compare
Multi-Year Trend
Created on 8/11/2022 at 8:37 PM
Page 213 of 296 pages

Year Annual Indicator Standard Error Numerator Denominator
2020/Q3-2021/Q2 2.0 %
2019/Q4-2020/Q3 2.0 %
2019/Q1-2019/Q4 2.0 %
2018/Q4-2019/Q3 2.0 %
2018/Q3-2019/Q2 1.0 %
2018/Q2-2019/Q1 1.0 %
2018/Q1-2018/Q4 1.0 %
2017/Q4-2018/Q3 1.0 %
2017/Q3-2018/Q2 1.0 %
2017/Q2-2018/Q1 1.0 %
2017/Q1-2017/Q4 1.0 %
2016/Q4-2017/Q3 1.0 %
2016/Q3-2017/Q2 1.0 %
2016/Q2-2017/Q1 1.0 %
2016/Q1-2016/Q4 1.0 %
2015/Q4-2016/Q3 4.0 %
2015/Q3-2016/Q2 9.0 %
2015/Q2-2016/Q1 10.0 %
2015/Q1-2015/Q4 12.0 %
2014/Q3-2015/Q2 5.0 %
2014/Q2-2015/Q1 6.0 %
2014/Q1-2014/Q4 3.0 %
2013/Q4-2014/Q3 3.0 %
2013/Q3-2014/Q2 3.0 %
Legends:
NOM 7 - Notes:
None
Created on 8/11/2022 at 8:37 PM
Page 214 of 296 pages

Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 215 of 296 pages

NOM 8 - Perinatal mortality rate per 1,000 live births plus fetal deaths
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 6.2 0.3 439 70,383
2018 6.2 0.3 440 71,277
2017 6.6 0.3 471 71,847
2016 6.9 0.3 507 73,359
2015 7.2 0.3 531 73,856
2014 7.0 0.3 518 74,152
2013 7.0 0.3 504 72,185
2012 6.9 0.3 507 73,105
2011 7.6 0.3 559 73,321
2010 7.2 0.3 535 74,039
2009 7.3 0.3 547 75,291
Legends:
NOM 8 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 216 of 296 pages

NOM 9.1 - Infant mortality rate per 1,000 live births
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 5.8 0.3 410 70,178
2018 6.0 0.3 428 71,080
2017 6.4 0.3 461 71,641
2016 6.5 0.3 478 73,136
2015 6.6 0.3 485 73,616
2014 6.5 0.3 480 73,921
2013 6.6 0.3 477 71,953
2012 6.4 0.3 463 72,883
2011 6.8 0.3 498 73,093
2010 6.8 0.3 504 73,801
2009 7.2 0.3 542 75,059
Legends:
NOM 9.1 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 217 of 296 pages

NOM 9.2 - Neonatal mortality rate per 1,000 live births
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 3.9 0.2 274 70,178
2018 4.1 0.2 293 71,080
2017 4.5 0.3 319 71,641
2016 4.7 0.3 344 73,136
2015 4.8 0.3 351 73,616
2014 4.6 0.3 338 73,921
2013 4.5 0.3 327 71,953
2012 4.7 0.3 344 72,883
2011 5.2 0.3 378 73,093
2010 4.7 0.3 350 73,801
2009 5.1 0.3 383 75,059
Legends:
NOM 9.2 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 218 of 296 pages

NOM 9.3 - Post neonatal mortality rate per 1,000 live births
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 1.9 0.2 136 70,178
2018 1.9 0.2 135 71,080
2017 2.0 0.2 142 71,641
2016 1.8 0.2 134 73,136
2015 1.8 0.2 134 73,616
2014 1.9 0.2 142 73,921
2013 2.1 0.2 150 71,953
2012 1.6 0.2 119 72,883
2011 1.6 0.2 120 73,093
2010 2.1 0.2 154 73,801
2009 2.1 0.2 159 75,059
Legends:
NOM 9.3 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 219 of 296 pages

NOM 9.4 - Preterm-related mortality rate per 100,000 live births
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 260.8 19.3 183 70,178
2018 270.1 19.5 192 71,080
2017 269.4 19.4 193 71,641
2016 317.2 20.9 232 73,136
2015 311.1 20.6 229 73,616
2014 292.2 19.9 216 73,921
2013 309.9 20.8 223 71,953
2012 306.0 20.5 223 72,883
2011 335.2 21.5 245 73,093
2010 323.8 21.0 239 73,801
2009 333.1 21.1 250 75,059
Legends:
NOM 9.4 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 220 of 296 pages

NOM 9.5 - Sudden Unexpected Infant Death (SUID) rate per 100,000 live births
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 74.1 10.3 52 70,178
2018 97.1 11.7 69 71,080
2017 97.7 11.7 70 71,641
2016 72.5 10.0 53 73,136
2015 92.4 11.2 68 73,616
2014 89.3 11.0 66 73,921
2013 82.0 10.7 59 71,953
2012 75.5 10.2 55 72,883
2011 79.4 10.4 58 73,093
2010 75.9 10.1 56 73,801
2009 98.6 11.5 74 75,059
Legends:
NOM 9.5 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 221 of 296 pages

NOM 10 - Percent of women who drink alcohol in the last 3 months of pregnancy
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 6.7 % 1.0 % 4,131 61,487
2019 7.7 % 1.0 % 4,852 62,661
2018 8.7 % 1.1 % 5,591 64,037
2017 8.3 % 1.0 % 5,224 62,971
2016 8.9 % 0.9 % 5,825 65,120
2015 9.7 % 1.0 % 6,335 65,364
2014 9.5 % 0.9 % 6,225 65,780
2013 7.7 % 0.9 % 4,921 64,306
2012 9.4 % 1.1 % 6,104 65,289
2011 8.9 % 1.1 % 5,818 65,300
2010 8.9 % 1.1 % 5,840 65,772
2009 9.9 % 1.1 % 6,592 66,417
2008 8.8 % 1.0 % 5,921 67,517
2007 7.4 % 0.9 % 4,914 66,622
Legends:
NOM 10 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has an unweighted denominator between 30 and 59 or confidence interval width >20% points or >1.2 times the estimate and should be interpreted
with caution
Created on 8/11/2022 at 8:37 PM
Page 222 of 296 pages

NOM 11 - Rate of neonatal abstinence syndrome per 1,000 birth hospitalizations
Data Source: HCUP - State Inpatient Databases (SID)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 12.4 0.4 811 65,634
2018 12.7 0.4 877 68,983
2017 13.3 0.4 920 69,180
2016 13.1 0.4 920 70,422
2015 13.2 0.5 701 53,099
2014 13.4 0.4 948 70,870
2013 13.0 0.4 904 69,306
2012 11.6 0.4 774 66,584
2011 10.5 0.4 691 66,119
2010 9.5 0.4 634 66,665
2009 8.3 0.4 562 67,937
2008 7.3 0.3 504 69,472
Legends:
NOM 11 - Notes:
None
Data Alerts: None
Indicator has a numerator ≤10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 223 of 296 pages

NOM 12 - Percent of eligible newborns screened for heritable disorders with on time physician notification for out
of range screens who are followed up in a timely manner. (DEVELOPMENTAL)
Federally available Data (FAD) for this measure is not available/reportable.
NOM 12 - Notes:
None
Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 224 of 296 pages

NOM 13 - Percent of children meeting the criteria developed for school readiness (DEVELOPMENTAL)
Federally available Data (FAD) for this measure is not available/reportable.
NOM 13 - Notes:
None
Data Alerts: None
Created on 8/11/2022 at 8:37 PM
Page 225 of 296 pages
NOM 14 - Percent of children, ages 1 through 17, who have decayed teeth or cavities in the past year
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 11.3 % 1.3 % 141,990 1,260,919
2018_2019 10.6 % 1.4 % 136,722 1,286,835
2017_2018 10.0 % 1.5 % 127,239 1,267,442
2016_2017 9.0 % 1.2 % 113,081 1,252,855
2016 9.0 % 1.2 % 112,430 1,252,032
Legends:
NOM 14 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 226 of 296 pages

NOM 15 - Child Mortality rate, ages 1 through 9, per 100,000
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 15.0 1.5 99 660,668
2019 14.6 1.5 97 662,566
2018 15.5 1.5 103 664,105
2017 15.6 1.5 104 667,948
2016 15.8 1.5 106 670,711
2015 20.3 1.7 136 670,836
2014 17.7 1.6 119 671,448
2013 16.7 1.6 111 666,603
2012 18.0 1.7 119 662,541
2011 16.2 1.6 107 659,217
2010 15.2 1.5 100 659,833
2009 16.0 1.6 105 655,038
Legends:
NOM 15 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 227 of 296 pages

NOM 16.1 - Adolescent mortality rate ages 10 through 19, per 100,000
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 33.2 2.1 251 755,284
2019 31.3 2.0 237 757,229
2018 28.7 1.9 218 760,010
2017 33.4 2.1 254 761,565
2016 33.4 2.1 254 759,740
2015 29.9 2.0 227 759,736
2014 22.8 1.7 174 763,694
2013 27.3 1.9 209 765,139
2012 31.3 2.0 242 773,432
2011 32.3 2.0 251 776,406
2010 30.8 2.0 242 785,270
2009 33.0 2.0 261 790,570
Legends:
NOM 16.1 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 228 of 296 pages

NOM 16.2 - Adolescent motor vehicle mortality rate, ages 15 through 19, per 100,000
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2018_2020 7.6 0.8 87 1,138,999
2017_2019 7.9 0.8 91 1,146,283
2016_2018 8.7 0.9 100 1,152,302
2015_2017 8.2 0.8 95 1,156,115
2014_2016 6.9 0.8 80 1,158,159
2013_2015 6.9 0.8 80 1,161,768
2012_2014 8.7 0.9 102 1,173,032
2011_2013 11.0 1.0 130 1,184,125
2010_2012 11.4 1.0 137 1,200,823
2009_2011 11.3 1.0 137 1,214,384
2008_2010 12.0 1.0 148 1,229,879
2007_2009 14.7 1.1 182 1,236,839
Legends:
NOM 16.2 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 229 of 296 pages

NOM 16.3 - Adolescent suicide rate, ages 15 through 19, per 100,000
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2018_2020 8.1 0.8 92 1,138,999
2017_2019 7.8 0.8 89 1,146,283
2016_2018 7.1 0.8 82 1,152,302
2015_2017 6.5 0.8 75 1,156,115
2014_2016 6.5 0.8 75 1,158,159
2013_2015 6.3 0.7 73 1,161,768
2012_2014 6.1 0.7 72 1,173,032
2011_2013 5.7 0.7 68 1,184,125
2010_2012 5.3 0.7 64 1,200,823
2009_2011 5.9 0.7 72 1,214,384
2008_2010 5.9 0.7 72 1,229,879
2007_2009 6.4 0.7 79 1,236,839
Legends:
NOM 16.3 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 230 of 296 pages

NOM 17.1 - Percent of children with special health care needs (CSHCN), ages 0 through 17
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 20.5 % 1.4 % 273,531 1,331,754
2018_2019 19.4 % 1.5 % 260,596 1,339,840
2017_2018 19.2 % 1.6 % 257,564 1,344,597
2016_2017 19.2 % 1.4 % 258,184 1,343,836
2016 18.6 % 1.6 % 250,000 1,343,874
Legends:
NOM 17.1 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 231 of 296 pages

NOM 17.2 - Percent of children with special health care needs (CSHCN), ages 0 through 17, who receive care in a
well-functioning system
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 18.3 % 3.1 % 49,950 273,531
2018_2019 18.8 % 3.3 % 48,870 260,596
2017_2018 8.3 % 1.9 % 21,436 257,564
2016_2017 14.7 % 2.6 % 37,919 258,184
2016 26.0 % 4.3 % 64,987 250,000
Legends:
NOM 17.2 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 232 of 296 pages

NOM 17.3 - Percent of children, ages 3 through 17, diagnosed with an autism spectrum disorder
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 3.0 % 0.8 % 34,572 1,143,062
2018_2019 3.1 % 0.9 % 35,921 1,156,312
2017_2018 2.0 % 0.6 % 22,126 1,132,008
2016_2017 2.5 % 0.6 % 28,463 1,120,237
2016 4.1 % 1.0 % 45,908 1,116,162
Legends:
NOM 17.3 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 233 of 296 pages

NOM 17.4 - Percent of children, ages 3 through 17, diagnosed with Attention Deficit Disorder/Attention Deficit
Hyperactivity Disorder (ADD/ADHD)
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 9.1 % 1.1 % 103,332 1,135,411
2018_2019 8.2 % 1.1 % 93,322 1,141,804
2017_2018 10.3 % 1.3 % 115,075 1,113,679
2016_2017 11.8 % 1.3 % 129,569 1,100,731
2016 10.8 % 1.4 % 117,992 1,093,513
Legends:
NOM 17.4 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 234 of 296 pages

NOM 18 - Percent of children, ages 3 through 17, with a mental/behavioral condition who receive treatment or
counseling
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 55.7 % 5.0 % 87,278 156,698
2018_2019 51.8 % 5.5 % 81,415 157,080
2017_2018 52.8 % 6.2 % 79,416 150,539
2016_2017 63.6 % 5.7 % 89,108 140,147
2016 68.1 % 6.4 % 94,282 138,528
Legends:
NOM 18 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 235 of 296 pages

NOM 19 - Percent of children, ages 0 through 17, in excellent or very good health
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 94.2 % 0.8 % 1,254,834 1,331,754
2018_2019 93.5 % 1.1 % 1,250,085 1,337,302
2017_2018 93.1 % 1.2 % 1,249,389 1,342,059
2016_2017 93.9 % 0.9 % 1,261,384 1,343,503
2016 93.7 % 1.1 % 1,258,778 1,343,208
Legends:
NOM 19 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 236 of 296 pages
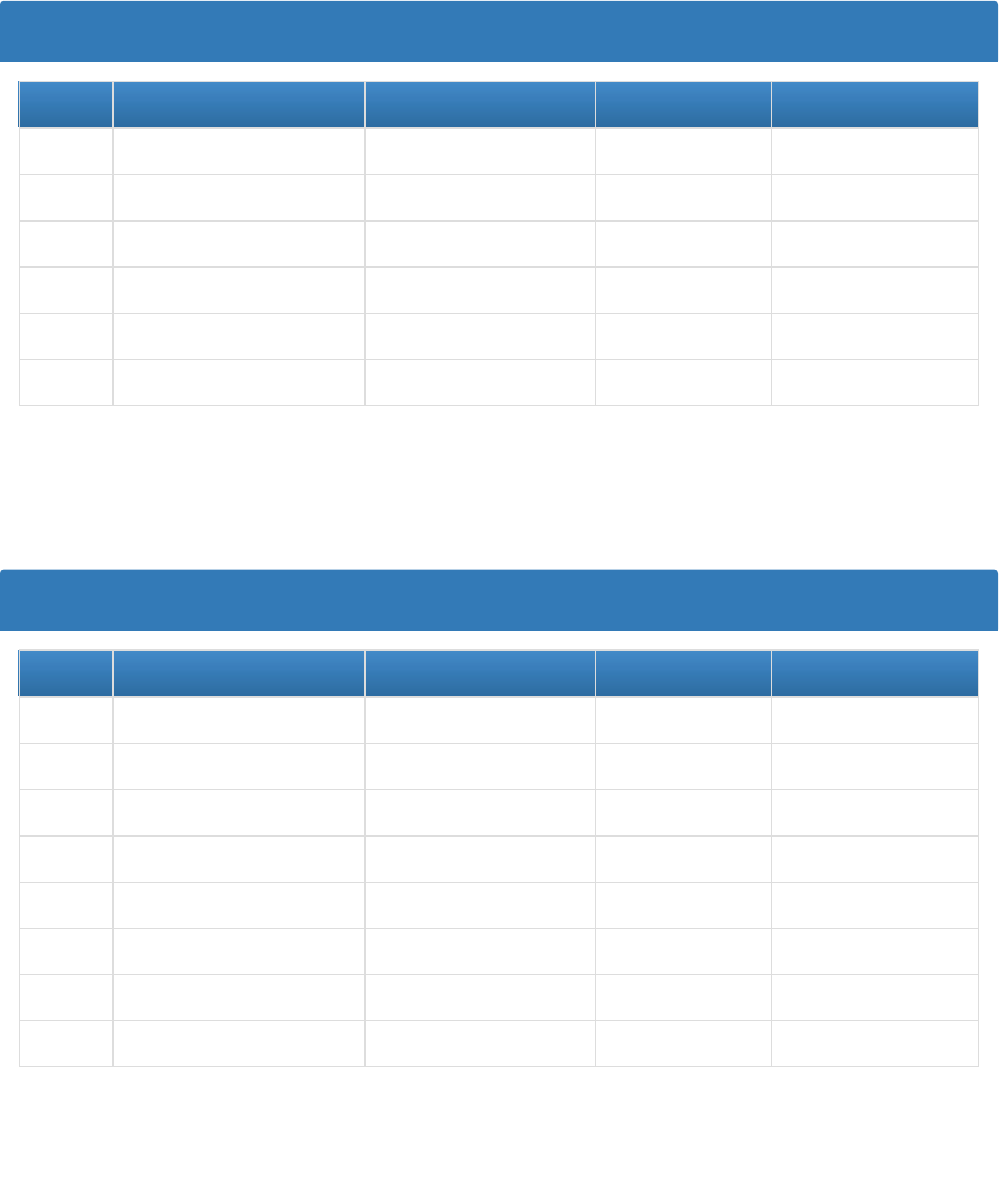
NOM 20 - Percent of children, ages 2 through 4, and adolescents, ages 10 through 17, who are obese (BMI at or
above the 95th percentile)
Data Source: WIC
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2018 16.4 % 0.2 % 7,721 47,153
2016 15.6 % 0.2 % 7,891 50,469
2014 16.5 % 0.2 % 8,100 49,008
2012 16.2 % 0.2 % 8,363 51,503
2010 17.1 % 0.2 % 8,758 51,280
2008 16.3 % 0.2 % 6,596 40,557
Legends:
Data Source: Youth Risk Behavior Surveillance System (YRBSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 12.8 % 0.4 % 28,910 226,200
2017 12.6 % 0.3 % 28,487 226,002
2015 11.5 % 0.2 % 26,316 228,179
2013 11.0 % 0.2 % 25,455 231,036
2011 12.0 % 0.8 % 29,379 245,278
2009 12.0 % 1.1 % 30,848 257,496
2007 12.9 % 1.1 % 32,855 254,909
2005 12.6 % 1.1 % 31,387 249,623
Legends:
Indicator has a denominator <50 and is not reportable
Indicator has a confidence interval width >20% points or >1.2 times the estimate and should be interpreted with caution
Indicator has an unweighted denominator <100 and is not reportable
Indicator has a confidence interval width >20% points or >1.2 times the estimate and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 237 of 296 pages

Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 16.7 % 2.3 % 99,293 593,904
2018_2019 17.6 % 2.5 % 100,089 568,211
2017_2018 14.5 % 2.6 % 79,529 549,812
2016_2017 15.7 % 2.4 % 89,354 567,381
2016 16.9 % 2.4 % 96,856 571,754
Legends:
NOM 20 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 238 of 296 pages

NOM 21 - Percent of children, ages 0 through 17, without health insurance
Data Source: American Community Survey (ACS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019 3.0 % 0.3 % 40,425 1,331,209
2018 3.0 % 0.3 % 40,114 1,336,906
2017 3.9 % 0.4 % 52,934 1,345,120
2016 3.3 % 0.4 % 43,863 1,346,368
2015 4.2 % 0.3 % 55,893 1,346,012
2014 3.4 % 0.3 % 45,150 1,347,272
2013 4.3 % 0.3 % 57,589 1,344,277
2012 3.8 % 0.3 % 51,552 1,342,323
2011 4.5 % 0.4 % 60,555 1,346,032
2010 4.9 % 0.3 % 65,771 1,350,668
2009 4.7 % 0.3 % 63,797 1,349,602
Legends:
NOM 21 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 239 of 296 pages

NOM 22.1 - Percent of children who have completed the combined 7-vaccine series (4:3:1:3*:3:1:4) by age 24
months
Data Source: National Immunization Survey (NIS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2017 75.4 % 2.4 % 55,000 73,000
2016 73.5 % 3.3 % 54,000 74,000
2015 73.9 % 3.6 % 55,000 75,000
2014 70.0 % 3.8 % 52,000 75,000
2013 72.5 % 3.6 % 54,000 74,000
2012 66.7 % 4.2 % 50,000 75,000
2011 75.6 % 4.1 % 57,000 75,000
Legends:
NOM 22.1 - Notes:
None
Data Alerts: None
Estimate not reported because unweighted sample size for the denominator < 30 or 95% confidence interval width/estimate >1.2
Estimates with 95% confidence interval widths >20 or that are inestimable might not be reliable
Created on 8/11/2022 at 8:37 PM
Page 240 of 296 pages

NOM 22.2 - Percent of children, ages 6 months through 17 years, who are vaccinated annually against seasonal
influenza
Data Source: National Immunization Survey (NIS) – Flu
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020_2021 70.1 % 1.1 % 885,932 1,263,811
2019_2020 74.8 % 1.1 % 941,973 1,259,322
2018_2019 74.5 % 1.5 % 940,620 1,262,916
2017_2018 67.5 % 1.6 % 848,968 1,257,723
2016_2017 68.5 % 2.5 % 868,723 1,268,024
2015_2016 72.8 % 2.1 % 915,983 1,258,218
2014_2015 64.5 % 3.0 % 810,079 1,255,158
2013_2014 66.0 % 2.3 % 836,263 1,267,127
2012_2013 67.6 % 2.7 % 853,540 1,263,588
2011_2012 64.0 % 3.6 % 824,711 1,289,465
2010_2011 62.7 % 2.7 % 771,223 1,230,020
2009_2010 49.5 % 2.3 % 588,753 1,189,401
Legends:
NOM 22.2 - Notes:
None
Data Alerts: None
Estimate not reported because unweighted sample size for the denominator < 30 or because the relative standard error is >0.3.
Estimates with 95% confidence interval half-widths > 10 might not be reliable
Created on 8/11/2022 at 8:37 PM
Page 241 of 296 pages

NOM 22.3 - Percent of adolescents, ages 13 through 17, who have received at least one dose of the HPV vaccine
Data Source: National Immunization Survey (NIS) - Teen
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 83.1 % 1.9 % 314,970 378,813
2019 78.9 % 2.8 % 297,815 377,552
2018 74.7 % 3.1 % 283,824 379,953
2017 69.2 % 3.5 % 263,244 380,264
2016 64.5 % 3.2 % 245,374 380,245
2015 60.3 % 3.3 % 229,471 380,246
Legends:
NOM 22.3 - Notes:
None
Data Alerts: None
Estimate not reported because unweighted sample size for the denominator < 30 or 95% confidence interval width/estimate > 1.2
Estimates with 95% confidence interval widths > 20 or that are inestimable might not be reliable
Created on 8/11/2022 at 8:37 PM
Page 242 of 296 pages

NOM 22.4 - Percent of adolescents, ages 13 through 17, who have received at least one dose of the Tdap vaccine
Data Source: National Immunization Survey (NIS) - Teen
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 90.2 % 1.5 % 341,560 378,813
2019 91.6 % 1.9 % 345,693 377,552
2018 88.4 % 2.1 % 336,034 379,953
2017 88.3 % 2.6 % 335,786 380,264
2016 85.1 % 2.4 % 323,385 380,245
2015 86.5 % 2.3 % 328,905 380,246
2014 85.0 % 2.7 % 323,794 380,851
2013 83.2 % 3.2 % 318,664 383,012
2012 78.1 % 3.4 % 300,758 385,101
2011 73.0 % 2.7 % 284,003 389,332
2010 61.2 % 3.3 % 234,929 383,916
2009 51.9 % 4.1 % 202,186 389,944
Legends:
NOM 22.4 - Notes:
None
Data Alerts: None
Estimate not reported because unweighted sample size for the denominator < 30 or 95% confidence interval width/estimate > 1.2
Estimates with 95% confidence interval widths > 20 or that are inestimable might not be reliable
Created on 8/11/2022 at 8:37 PM
Page 243 of 296 pages

NOM 22.5 - Percent of adolescents, ages 13 through 17, who have received at least one dose of the
meningococcal conjugate vaccine
Data Source: National Immunization Survey (NIS) - Teen
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 94.0 % 1.1 % 356,030 378,813
2019 94.9 % 1.4 % 358,427 377,552
2018 91.8 % 2.0 % 348,823 379,953
2017 91.8 % 2.2 % 348,975 380,264
2016 84.9 % 2.6 % 322,627 380,245
2015 87.3 % 2.3 % 331,887 380,246
2014 86.5 % 2.5 % 329,314 380,851
2013 78.0 % 3.4 % 298,661 383,012
2012 74.9 % 3.5 % 288,608 385,101
2011 78.5 % 2.4 % 305,702 389,332
2010 68.9 % 3.1 % 264,513 383,916
2009 59.3 % 4.1 % 231,140 389,944
Legends:
NOM 22.5 - Notes:
None
Data Alerts: None
Estimate not reported because unweighted sample size for the denominator < 30 or 95% confidence interval width/estimate >1.2
Estimates with 95% confidence interval widths > 20 or that are inestimable might not be reliable
Created on 8/11/2022 at 8:37 PM
Page 244 of 296 pages

NOM 23 - Teen birth rate, ages 15 through 19, per 1,000 females
Data Source: National Vital Statistics System (NVSS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 13.1 0.3 2,431 185,978
2019 13.9 0.3 2,603 186,613
2018 14.1 0.3 2,645 187,101
2017 14.2 0.3 2,667 188,265
2016 15.9 0.3 3,017 189,190
2015 17.0 0.3 3,214 189,152
2014 17.8 0.3 3,379 189,695
2013 19.3 0.3 3,690 191,242
2012 22.1 0.3 4,286 193,953
2011 24.4 0.4 4,797 196,427
2010 27.3 0.4 5,396 197,629
2009 30.7 0.4 6,140 199,852
Legends:
NOM 23 - Notes:
None
Data Alerts: None
Indicator has a numerator <10 and is not reportable
Indicator has a numerator <20 and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 245 of 296 pages

NOM 24 - Percent of women who experience postpartum depressive symptoms following a recent live birth
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2020 14.3 % 1.5 % 8,840 61,648
2019 15.6 % 1.5 % 9,718 62,162
2018 16.1 % 1.5 % 10,296 63,824
2017 12.4 % 1.2 % 7,680 61,977
2016 13.3 % 1.1 % 8,480 63,932
2015 11.9 % 1.1 % 7,612 64,089
2014 12.0 % 1.1 % 7,734 64,505
2013 11.4 % 1.1 % 7,145 62,837
2012 12.3 % 1.3 % 7,826 63,627
Legends:
NOM 24 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has an unweighted denominator between 30 and 59 or a confidence interval width >20% points or >1.2 times the estimate and should be interpreted
with caution
Created on 8/11/2022 at 8:37 PM
Page 246 of 296 pages
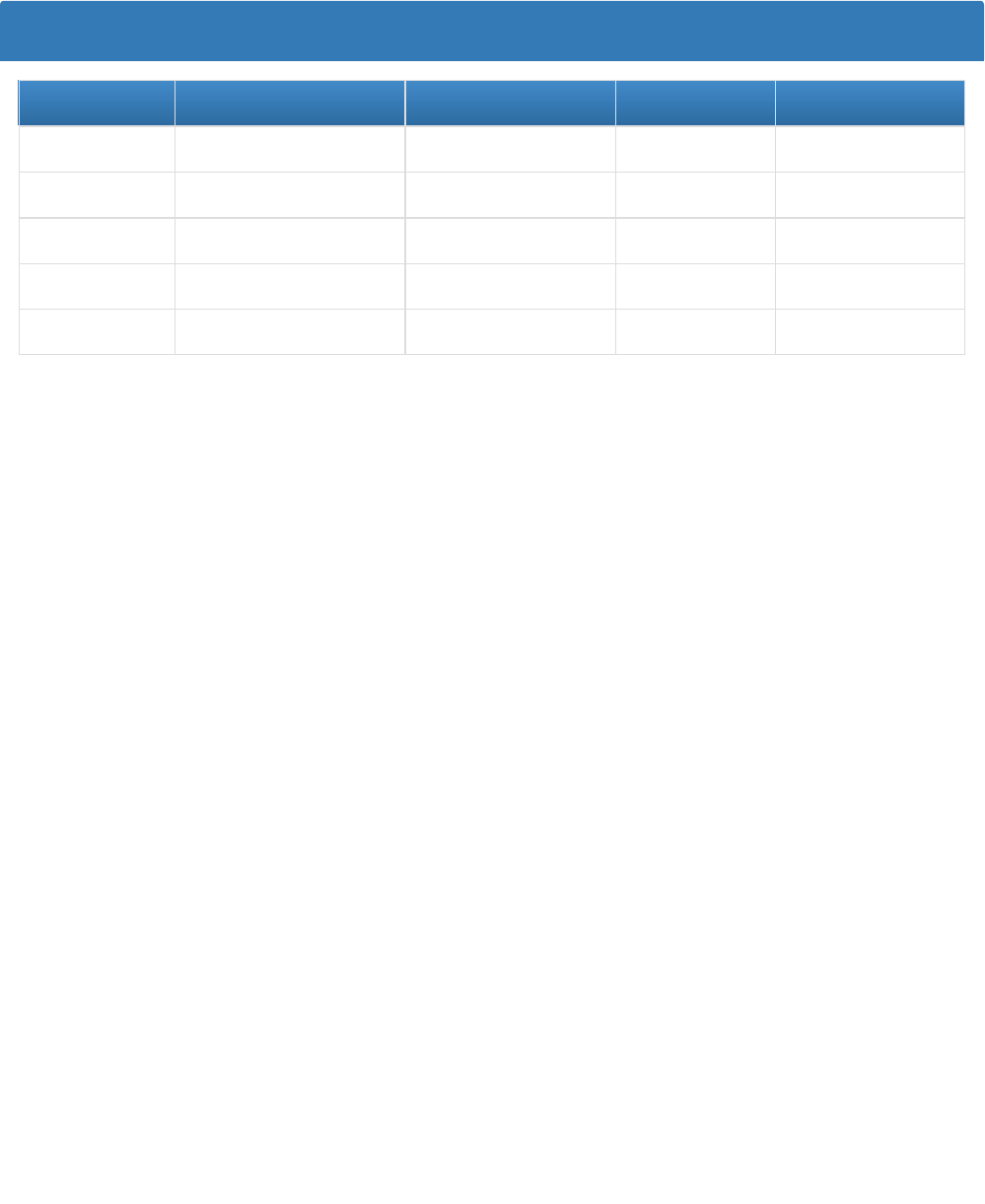
NOM 25 - Percent of children, ages 0 through 17, who were unable to obtain needed health care in the past year
Data Source: National Survey of Children's Health (NSCH)
Multi-Year Trend
Year Annual Indicator Standard Error Numerator Denominator
2019_2020 2.3 % 0.5 % 30,088 1,319,601
2018_2019 2.3 % 0.5 % 30,815 1,331,725
2017_2018 2.1 % 0.6 % 27,505 1,337,635
2016_2017 1.7 % 0.5 % 22,648 1,338,569
2016 1.3 % 0.5 % 17,042 1,343,874
Legends:
NOM 25 - Notes:
None
Data Alerts: None
Indicator has an unweighted denominator <30 and is not reportable
Indicator has a confidence interval width >20% points, >1.2 times the estimate, or that is inestimable and should be interpreted with caution
Created on 8/11/2022 at 8:37 PM
Page 247 of 296 pages

Form 10
National Performance Measures (NPMs)
State: Maryland
NPM 3 - Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care
Unit (NICU)
Federally available Data (FAD) for this measure is not available/reportable.
State Provided Data
2019 2020 2021
Annual Objective 93.7
Annual Indicator 79.2 93.4 91.6
Numerator 954 891 854
Denominator 1,205 954 932
Data Source VSA VSA VSA
Data Source Year 2018 2019 2020
Provisional or Final ? Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 94.0 94.3 94.6 95.0
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 248 of 296 pages

NPM 4A - Percent of infants who are ever breastfed
Federally Available Data
Data Source: National Immunization Survey (NIS)
2019 2020 2021
Annual Objective 88.9
Annual Indicator 84.1 88.6 86.8
Numerator 51,263 55,833 59,613
Denominator 60,967 63,040 68,676
Data Source NIS NIS NIS
Data Source Year 2016 2017 2018
Annual Objectives
2022 2023 2024 2025
Annual Objective 89.2 89.5 89.8 90.1
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 249 of 296 pages

NPM 4B - Percent of infants breastfed exclusively through 6 months
Federally Available Data
Data Source: National Immunization Survey (NIS)
2019 2020 2021
Annual Objective 30.8
Annual Indicator 28.0 29.4 26.6
Numerator 16,851 17,961 17,625
Denominator 60,103 61,137 66,307
Data Source NIS NIS NIS
Data Source Year 2016 2017 2018
Annual Objectives
2022 2023 2024 2025
Annual Objective 32.2 33.6 35.0 36.4
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 250 of 296 pages

NPM 5A - Percent of infants placed to sleep on their backs
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2017 2018 2019 2020 2021
Annual Objective 79 75.8 77.3 78.8 80.3
Annual Indicator 74.6 78.2 78.2 81.6 78.5
Numerator 47,705 48,293 48,293 50,368 47,476
Denominator 63,975 61,753 61,753 61,754 60,460
Data Source PRAMS PRAMS PRAMS PRAMS PRAMS
Data Source Year 2015 2017 2017 2019 2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 81.8 83.3 84.8 85.3
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 251 of 296 pages
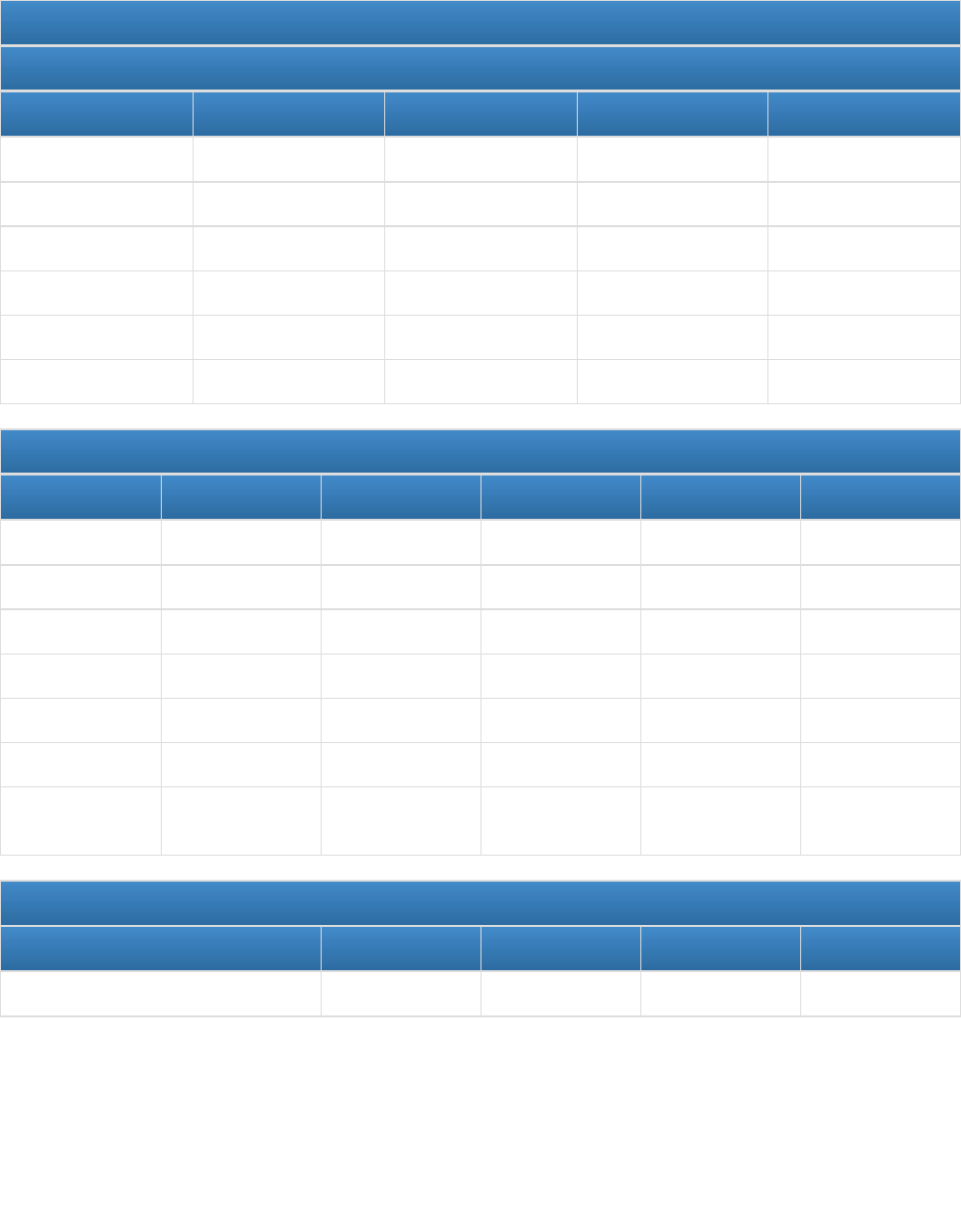
NPM 5B - Percent of infants placed to sleep on a separate approved sleep surface
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2018 2019 2020 2021
Annual Objective 70.5 71.9 33.3
Annual Indicator 29.0 29.0 32.9 34.5
Numerator 16,948 16,948 19,188 19,974
Denominator 58,441 58,441 58,412 57,908
Data Source PRAMS PRAMS PRAMS PRAMS
Data Source Year 2017 2017 2019 2020
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 70.5 71.9 33.3
Annual Indicator 69.1
Numerator 45,750
Denominator 66,226
Data Source PRAMS
Data Source Year 2015
Provisional or
Final ?
Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 33.7 34.1 34.5 34.9
Created on 8/11/2022 at 8:37 PM
Page 252 of 296 pages

Field Level Notes for Form 10 NPMs:
1. Field Name: 2017
Column Name: State Provided Data
Field Note:
Indicator reflects the estimated percentage of recent mothers reporting their new baby usually sleeps in a crib or
portable crib AND did not report their new baby sleeps with themselves or another person.
Created on 8/11/2022 at 8:37 PM
Page 253 of 296 pages

NPM 5C - Percent of infants placed to sleep without soft objects or loose bedding
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2018 2019 2020 2021
Annual Objective 68.1 69.5 57.6
Annual Indicator 51.7 51.6 56.6 55.0
Numerator 30,441 30,441 32,851 31,754
Denominator 58,942 58,942 58,015 57,742
Data Source PRAMS PRAMS PRAMS PRAMS
Data Source Year 2017 2017 2019 2020
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 68.1 69.5 57.6
Annual Indicator 66.8
Numerator 44,268
Denominator 66,226
Data Source PRAMS
Data Source Year 2015
Provisional or
Final ?
Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 58.6 59.6 60.6 61.6
Created on 8/11/2022 at 8:37 PM
Page 254 of 296 pages

Field Level Notes for Form 10 NPMs:
1. Field Name: 2017
Column Name: State Provided Data
Field Note:
Indicator reflects the estimated percentage of recent mothers who did not report their new baby usually sleeps
with pillows, bumper pads, plush or thick blankets, stuffed toys, or an infant positioner.
Created on 8/11/2022 at 8:37 PM
Page 255 of 296 pages

NPM 6 - Percent of children, ages 9 through 35 months, who received a developmental screening using a parent-
completed screening tool in the past year
Federally Available Data
Data Source: National Survey of Children's Health (NSCH)
2017 2018 2019 2020 2021
Annual Objective 34.2 34.6 35 41.9
Annual Indicator 43.1 36.6 34.7 40.9 40.3
Numerator 60,201 49,586 47,097 55,907 57,317
Denominator 139,848 135,327 135,685 136,579 142,190
Data Source NSCH NSCH NSCH NSCH NSCH
Data Source Year 2016 2016_2017 2017_2018 2018_2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 42.9 43.9 44.9 45.9
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 256 of 296 pages

NPM 10 - Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year.
Federally Available Data
Data Source: National Survey of Children's Health (NSCH)
2017 2018 2019 2020 2021
Annual Objective 87.3 87.7 88 82.2
Annual Indicator 88.7 87.1 87.1 81.4 78.7
Numerator 393,976 386,469 386,469 359,586 355,101
Denominator 444,207 443,800 443,800 441,589 451,033
Data Source NSCH NSCH NSCH NSCH NSCH
Data Source Year 2016 2016_2017 2016_2017 2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 83.0 83.8 84.6 85.4
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 257 of 296 pages

NPM 11 - Percent of children with and without special health care needs, ages 0 through 17, who have a medical
home - Children with Special Health Care Needs
Federally Available Data
Data Source: National Survey of Children's Health (NSCH) - CSHCN
2017 2018 2019 2020 2021
Annual Objective 57 60 63.3 45.9
Annual Indicator 50.8 53.4 50.6 44.9 44.9
Numerator 127,072 137,990 130,334 117,076 122,840
Denominator 250,000 258,184 257,564 260,596 273,531
Data Source NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN
Data Source Year 2016 2016_2017 2017_2018 2018_2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 46.9 47.9 48.9 50.0
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 258 of 296 pages

NPM 12 - Percent of adolescents with and without special health care needs, ages 12 through 17, who received
services to prepare for the transition to adult health care - Children with Special Health Care Needs
Federally Available Data
Data Source: National Survey of Children's Health (NSCH) - CSHCN
2017 2018 2019 2020 2021
Annual Objective 40 43 45.3 27.9
Annual Indicator 13.4 16.2 21.6 26.9 23.8
Numerator 14,817 21,034 28,923 31,754 28,346
Denominator 110,803 129,507 133,731 118,003 119,301
Data Source NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN NSCH-CSHCN
Data Source Year 2016 2016_2017 2017_2018 2018_2019 2019_2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 28.9 29.9 30.9 31.9
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 259 of 296 pages

NPM 13.1 - Percent of women who had a preventive dental visit during pregnancy
Federally Available Data
Data Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
2017 2018 2019 2020 2021
Annual Objective 57.9 58.6 59.3 60 54.9
Annual Indicator 52.6 53.3 53.3 54.1 47.0
Numerator 34,237 33,752 33,752 33,888 28,934
Denominator 65,122 63,361 63,361 62,695 61,594
Data Source PRAMS PRAMS PRAMS PRAMS PRAMS
Data Source Year 2015 2017 2017 2019 2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 55.7 56.5 57.3 59.1
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 260 of 296 pages

NPM 14.1 - Percent of women who smoke during pregnancy
Federally Available Data
Data Source: National Vital Statistics System (NVSS)
2017 2018 2019 2020 2021
Annual Objective 6.6 6.5 6.4 6.3 4.4
Annual Indicator 5.9 5.5 5.3 4.7 4.2
Numerator 4,299 3,932 3,719 3,281 2,846
Denominator 72,838 71,324 70,599 69,782 68,236
Data Source NVSS NVSS NVSS NVSS NVSS
Data Source Year 2016 2017 2018 2019 2020
Annual Objectives
2022 2023 2024 2025
Annual Objective 4.1 3.8 3.5 3.2
Field Level Notes for Form 10 NPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 261 of 296 pages
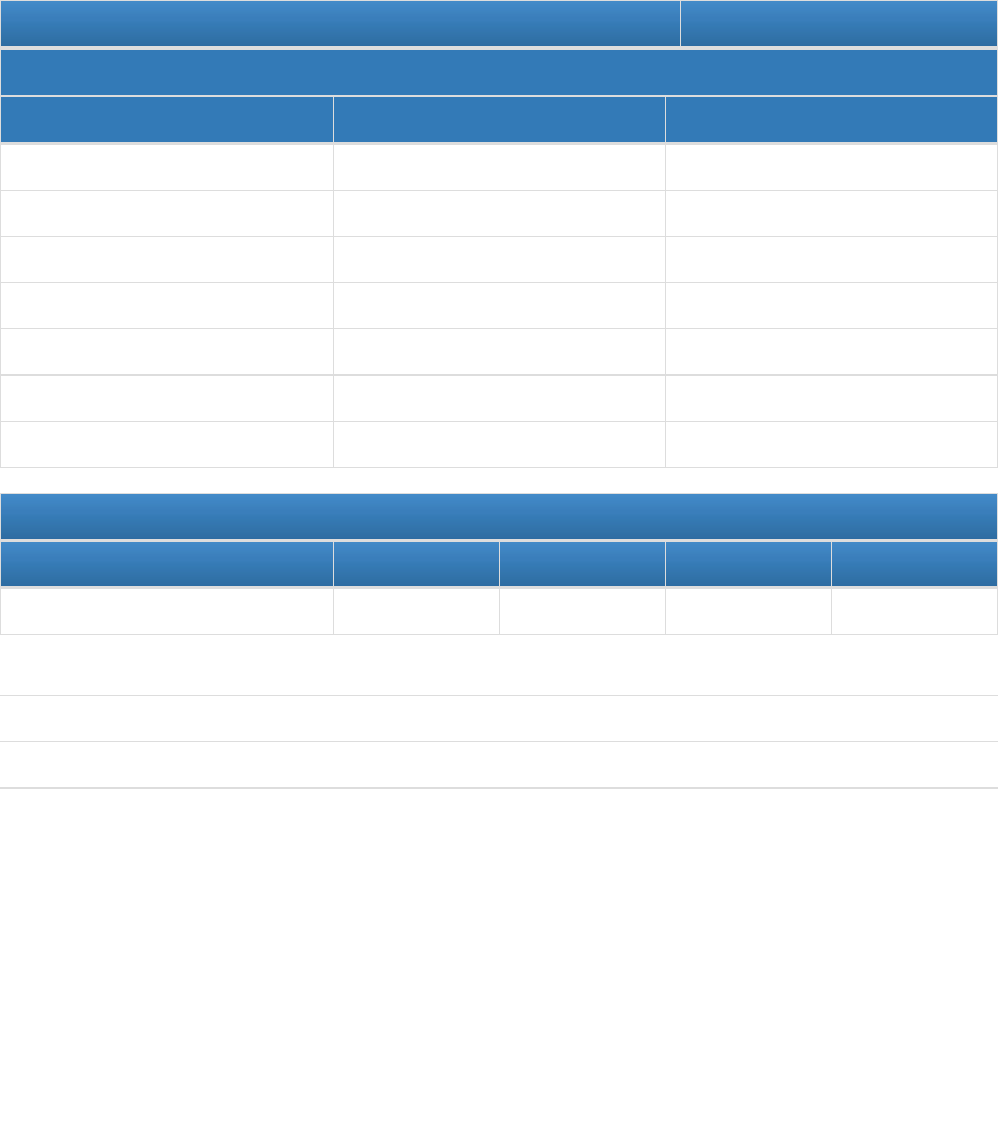
Form 10
State Performance Measures (SPMs)
State: Maryland
SPM 1 - Rate of overdose mortality for women ages 15-49
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 24.1 35.7
Numerator 334 493
Denominator 1,385,375 1,381,029
Data Source VSA CDC Wonder using ICD-10 Codes
Data Source Year 2019 2021
Provisional or Final ? Final Provisional
Annual Objectives
2022 2023 2024 2025
Annual Objective 23.9 23.7 23.5 23.3
Field Level Notes for Form 10 SPMs:
1. Field Name: 2021
Column Name: State Provided Data
Field Note:
Of note, because of the Network Security Incident, 2021 data are not available from the VSA. Therefore, CDC
Wonder data was used using ICD-10 codes from SAMSA's guidance.
Created on 8/11/2022 at 8:37 PM
Page 262 of 296 pages
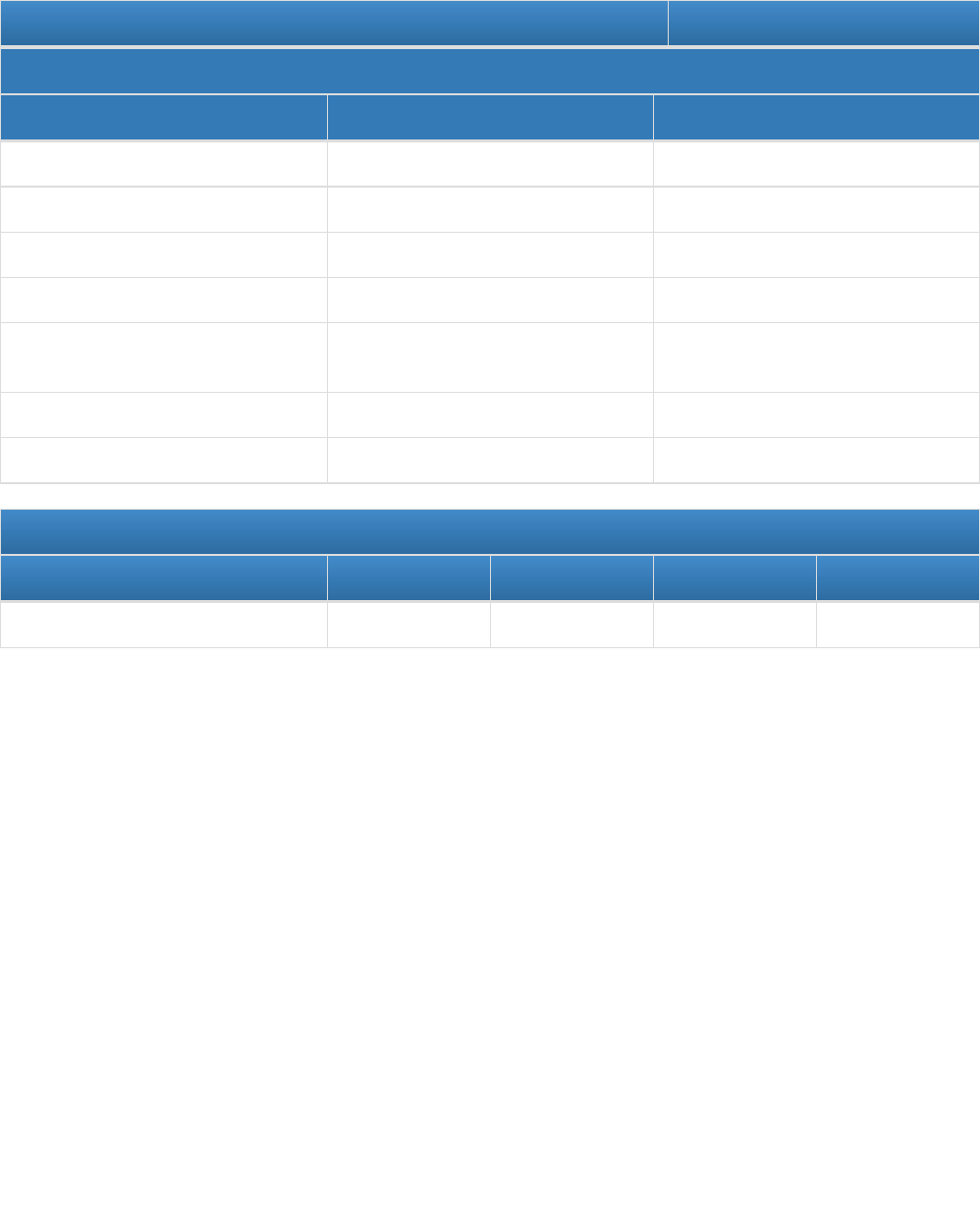
SPM 2 - Excess rate between Black Non-Hispanic Severe Maternal Morbidity (SMM) events to White Non-Hispanic
SMM events per 10,000 delivery hospitalizations
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 328.5 381.4
Numerator 640 690
Denominator 19,481 18,090
Data Source Health Services Cost Review
Commission
Health Services Cost Review
Commission
Data Source Year 2018 2021
Provisional or Final ? Final Provisional
Annual Objectives
2022 2023 2024 2025
Annual Objective 312.1 295.7 279.3 262.8
Field Level Notes for Form 10 SPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 263 of 296 pages

SPM 3 - Receipt of Primary Care During Early Childhood
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 67.4 64.6 65.8 67.1 68.2
Annual Indicator 63.5 65.9 67.1 67 71.7
Numerator 25,389 30,621 25,794 24,969 27,940
Denominator 39,994 46,466 38,455 37,253 38,989
Data Source Medicaid Medicaid Medicaid Medicaid Medicaid
Data Source Year 2017 (CY) 2018 (CY) 2019 (CY) 2020 (CY) 2021 (CY)
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 69.4 70.6 71.8 73.0
Field Level Notes for Form 10 SPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 264 of 296 pages
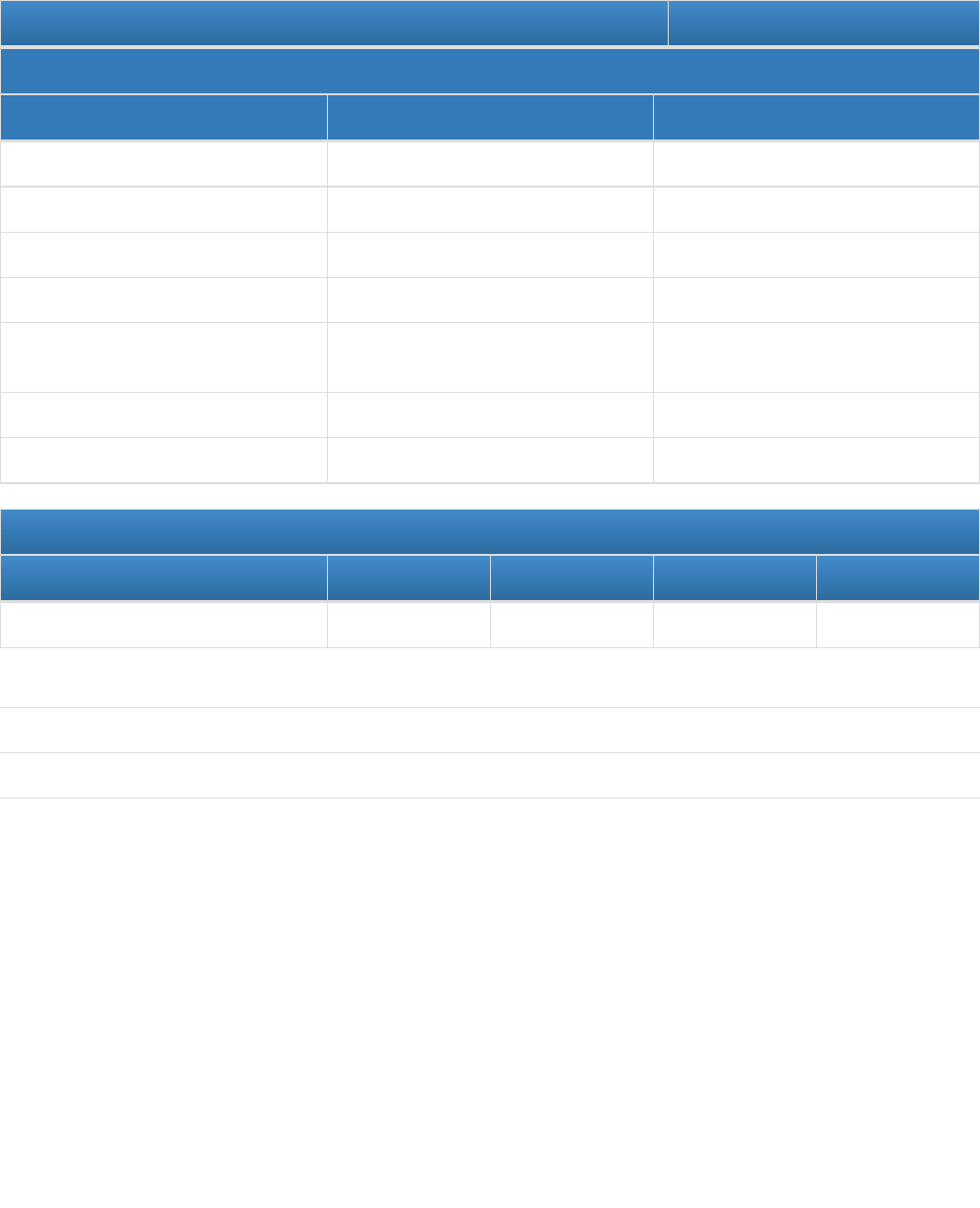
SPM 4 - Number of Asthma Emergency Room Visits per 1,000 for Children age 2-17 with a primary diagnosis of
asthma
Measure Status: Active
State Provided Data
2020 2021
Annual Objective
Annual Indicator 9.2 3.5
Numerator 10,974 4,213
Denominator 1,195,993 1,193,543
Data Source Health Services Cost Review
Commission
Health Services Cost Review
Commission
Data Source Year 2018 2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 8.5 7.2 6.7 6.2
Field Level Notes for Form 10 SPMs:
1. Field Name: 2021
Column Name: State Provided Data
Field Note:
We hypothesize that the rate has decreased due to the COVID-19 Pandemic.
Created on 8/11/2022 at 8:37 PM
Page 265 of 296 pages
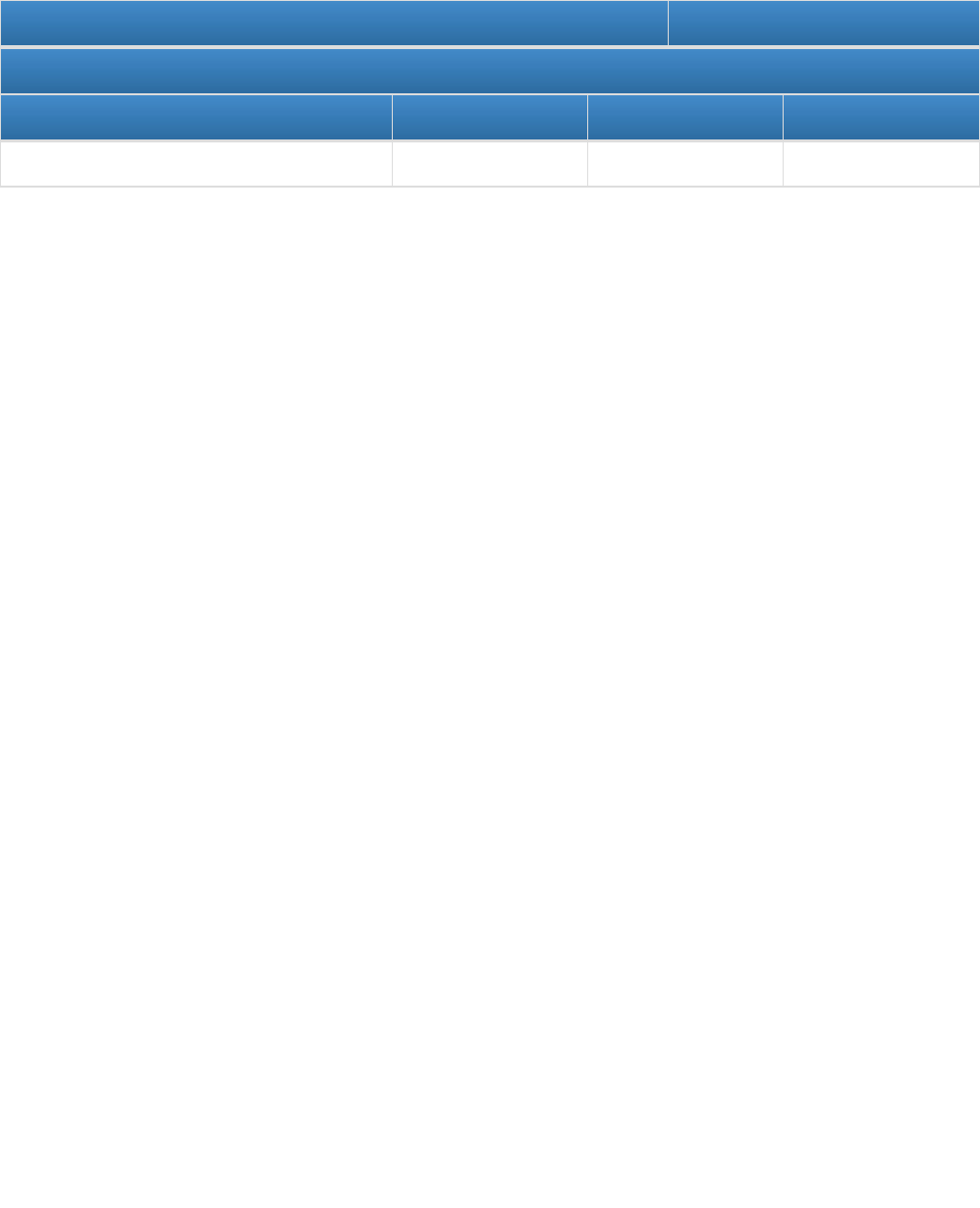
SPM 5 - Cross-Cutting Measure: Percentage of MCHB committees/workgroups that include community
members/persons with lived experience
Measure Status: Active
Annual Objectives
2023 2024 2025
Annual Objective 27.0 36.0 45.0
Field Level Notes for Form 10 SPMs:
None
Created on 8/11/2022 at 8:37 PM
Page 266 of 296 pages

Form 10
Evidence-Based or –Informed Strategy Measures (ESMs)
State: Maryland
ESM 3.1 - Percentage of Level III & IV Perinatal Referral Centers who received their re-designations based on the
2019 MD Perinatal System Standards
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 93.7
Annual Indicator 0 15.4 46.2
Numerator 0 2 6
Denominator 14 13 13
Data Source Program Data Program Data Program Data
Data Source Year 2019 2020 2021
Provisional or Final ? Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 62.0 85.0 100.0 100.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2020
Column Name: State Provided Data
Field Note:
Of note during 2021, there were 13 Level III and IV Perinatal Referral Standards.
Created on 8/11/2022 at 8:37 PM
Page 267 of 296 pages

ESM 4.1 - Number of birthing hospitals designated as breastfeeding friendly
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 10
Annual Indicator 10 10
Numerator
Denominator
Data Source MDH Breastfeeding Policy
Committe
MDH Breastfeeding Policy
Committee
Data Source Year FY 2020 FY2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 11.0 12.0 13.0 15.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2020
Column Name: State Provided Data
Field Note:
Due to the COVID-19 Pandemic outreach to the hospitals was severely limited during FY 2020.
2. Field Name: 2021
Column Name: State Provided Data
Field Note:
Due to emphasis on addressing COVID, the number of baby-friendly hospitals remain the same.
Created on 8/11/2022 at 8:37 PM
Page 268 of 296 pages

ESM 5.1 - Percentage of infants less than 6 months who are placed on their backs to sleep
Measure Status: Inactive - Replaced
State Provided Data
2019 2020 2021
Annual Objective 80.3
Annual Indicator 78.2 81.6 80.3
Numerator 48,293 50,368 48,530
Denominator 61,753 61,754 60,415
Data Source PRAMS PRAMS PRAMS
Data Source Year 2017 2019 2020
Provisional or Final ? Final Final Final
Field Level Notes for Form 10 ESMs:
None
Created on 8/11/2022 at 8:37 PM
Page 269 of 296 pages

ESM 5.2 - Number of home visiting or care coordination clients, providers, and other Title V program participants
that received infant safe sleep counseling and information
Measure Status: Active
Annual Objectives
2023 2024 2025
Annual Objective 6,900.0 7,000.0 7,100.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2021
Column Name: State Provided Data
Field Note:
For 2021, the number was 6,728
Created on 8/11/2022 at 8:37 PM
Page 270 of 296 pages

ESM 6.1 - Number of parents who receive information/education on the importance of developmental screenings
from Home Visiting and Care Coordination Title V providers
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 2,832 1,181 1,201 1,220 1,239
Annual Indicator 1,162 1,035 1,022 749 2,325
Numerator
Denominator
Data Source MCHB Data MCHB Data MCHB MCHB Data MCHB Data
Data Source Year 2017 2018 2019 FY 2020 2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 1,259.0 1,278.0 1,278.0 1,300.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2020
Column Name: State Provided Data
Field Note:
Home Visiting services through the Local Health Departments was severly limited during the COVID-19 Pandemic.
As a result, fewer families were provided with developmental screening education.
Created on 8/11/2022 at 8:37 PM
Page 271 of 296 pages

ESM 10.2 - Number of adolescent (12-17) who receive well visits through school based health centers
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 45,000
Annual Indicator 37,578 798
Numerator
Denominator
Data Source MCHB Data MCHB Data
Data Source Year FY 2020 FY2021
Provisional or Final ? Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 60,000.0 75,000.0 90,000.0 110,000.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2020
Column Name: State Provided Data
Field Note:
School closures due to the COVID-19 Pandemic, limited the number of well visits completed at school based
health clinics during FY 2020
2. Field Name: 2021
Column Name: State Provided Data
Field Note:
The numbers dramatically decreased due to COVID. Many schools were operating virtually and therefore school
health services and school-based clinics were not open.
Created on 8/11/2022 at 8:37 PM
Page 272 of 296 pages

ESM 11.1 - Number of CYSHCN who receive patient and family-centered care coordination services
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 0 61 5,300 5,400 5,500
Annual Indicator 60 5,362 5,770 1,463 1,502
Numerator
Denominator
Data Source OGPSHCN Data OGPSHCN Data OGPSHCN Data OGPSHCN Data OGPSHCN Data
Data Source Year FY 2017 FY 18 FY 19 FY 2020 FY 2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 5,600.0 5,700.0 5,800.0 6,000.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2017
Column Name: State Provided Data
Field Note:
This number, is based on several grantees who have not yet separated out care coordination from transition
services.
2. Field Name: 2018
Column Name: State Provided Data
Field Note:
Total number of children who received basic or complex care coordination through Nurse Care Coordinators at the
24 local health departments in the state.
Created on 8/11/2022 at 8:37 PM
Page 273 of 296 pages

ESM 12.1 - Number of CYSCHN and their families who participate in health care transition planning activities
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 0 61 62 63 64
Annual Indicator 60 5,697 1,308 416 81
Numerator
Denominator
Data Source MCHB Data OGPSHCN OGPSHCN OGPSHCN Data OGPSHCN Data
Data Source Year FY 2017 FY2018 FY 2019 FY 2020 FY 2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 65.0 66.0 67.0 1,300.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2017
Column Name: State Provided Data
Field Note:
Includes count of children who have received transition services. This number includes reports from several
grantees who did not separate out care coordination from transition services.
2. Field Name: 2019
Column Name: State Provided Data
Field Note:
Previous data included counts for both care coordination and transition services. Changes have occurred that
has grantees providing data on each service separately to better assess progress in meeting the measure.
3. Field Name: 2021
Column Name: State Provided Data
Field Note:
The 2021 numbers are significantly low because of COVID.
Created on 8/11/2022 at 8:37 PM
Page 274 of 296 pages

Created on 8/11/2022 at 8:37 PM
Page 275 of 296 pages

ESM 13.1.1 - Percentage of pregnant individuals aged 21 and older on medical assistance in Maryland who
receive a preventive dental visit
Measure Status: Active
State Provided Data
2019 2020 2021
Annual Objective 28.4
Annual Indicator 28.2 28.8 21.6
Numerator 7,979 8,346 6,666
Denominator 28,259 28,939 30,925
Data Source Office of Oral Health
Legislative Report
Office of Oral Health
Legislative Report
Office of Oral Health
Legislative Report
Data Source Year CY 2018 CY 2019 CY2020
Provisional or Final ? Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 29.9 31.4 32.5 34.0
Field Level Notes for Form 10 ESMs:
1. Field Name: 2019
Column Name: State Provided Data
Field Note:
Data is from CY 2018. Source Office of Oral Health's Legislative Report
2. Field Name: 2021
Column Name: State Provided Data
Field Note:
Numbers impacted by the COVID-19 Pandemic
Created on 8/11/2022 at 8:37 PM
Page 276 of 296 pages

ESM 14.1.1 - Number of pregnant individuals who use the statewide tobacco QuitLine
Measure Status: Active
State Provided Data
2017 2018 2019 2020 2021
Annual Objective 167 136 137 139 140
Annual Indicator 135 131 99 86 67
Numerator
Denominator
Data Source MDH CTPC
Quitline Data
MDH CTPC
Quitline Data
MDH CTPC
Quitline Data
Quit Line Data Quit line Data
Data Source Year FY17 FY 18 FY 19 FY 2020 FY2021
Provisional or
Final ?
Final Final Final Final Final
Annual Objectives
2022 2023 2024 2025
Annual Objective 142.0 143.0 143.0 143.0
Field Level Notes for Form 10 ESMs:
None
Created on 8/11/2022 at 8:37 PM
Page 277 of 296 pages

Form 10
State Performance Measure (SPM) Detail Sheets
State: Maryland
SPM 1 - Rate of overdose mortality for women ages 15-49
Population Domain(s) – Women/Maternal Health
Measure Status: Active
Goal: To reduce the number of overdose fatalities for women age 15-49
Definition:
Unit Type: Rate
Unit Number: 100,000
Numerator: # of overdose fatalities for women age 15-49
Denominator: # of women age 15-49
Data Sources and Data
Issues:
VSA Data and Health Services Cost Review Commission (HSCRC)
Significance: There were 38 pregnancy-associated deaths in 2018. Twelve of the 38 total deaths (32
percent) resulted from substance use and unintentional overdose deaths. In nine of the 12
cases, two or more drugs were found by postmortem toxicology testing. From 2010 to 2018
of opioid identified postmortem, pregnancy-associated unintentional overdose deaths in
Maryland, Fentanyl or fentanyl analogs have been the most frequently detected opioid.
Created on 8/11/2022 at 8:37 PM
Page 278 of 296 pages

SPM 2 - Excess rate between Black Non-Hispanic Severe Maternal Morbidity (SMM) events to White Non-Hispanic
SMM events per 10,000 delivery hospitalizations
Population Domain(s) – Women/Maternal Health
Measure Status: Active
Goal: A 20% reduction in Black Non-Hispanic SMM events by 2026
Definition:
Unit Type: Rate
Unit Number: 10,000
Numerator: # of Black Non-Hispanic SMM events
Denominator: # of Black Non-Hispanic delivery hospitalizations
Data Sources and Data
Issues:
Health Services Cost Review Commission (HSCRC)
Significance: Reduce and eliminate the racial disparities in SMM. This is part of the Statewide Integrated
Health Improvement Strategy that is part of the Maryland Total Cost of Care Model.
Created on 8/11/2022 at 8:37 PM
Page 279 of 296 pages

SPM 3 - Receipt of Primary Care During Early Childhood
Population Domain(s) – Child Health
Measure Status: Active
Goal: All children in Maryland will be screened for developmental needs
Definition:
Unit Type: Percentage
Unit Number: 100
Numerator: % of Medicaid patients age 15 months who had 5 or more well child
visits during the first 15 months of life
Denominator: % of Medicaid patients age 15 months
Data Sources and Data
Issues:
Medicaid data
Significance: Early identification of developmental disorders is critical to the well-being of children and
their families. It is an integral function of the primary care medical home. The percent of
children with a developmental disorder has been increasing, yet overall screening rates
have remained low. The American Academy of Pediatrics recommends screening tests begin
at the nine month visit. MCHB chose NPM 6 to measure developmental screening using a
parent completed screening tool, however developmental screening is also appropriate in
the primary care setting for infants and young children. MCHB will focus on receipt of primary
care for young children as a precursor to developmental screening in the primary care
setting. MCHB will partner with Medicaid and local health departments to track data and
develop future strategies.
Created on 8/11/2022 at 8:37 PM
Page 280 of 296 pages

SPM 4 - Number of Asthma Emergency Room Visits per 1,000 for Children age 2-17 with a primary diagnosis of
asthma
Population Domain(s) – Child Health, Adolescent Health
Measure Status: Active
Goal: Reduce the number of ED visits for children age 2-17 with asthma
Definition:
Unit Type: Rate
Unit Number: 1,000
Numerator: # of children age 2-17 with primary diagnosis of asthma during an
ED visit
Denominator: # of children age 2-17
Data Sources and Data
Issues:
Maryland Health Care Cost Review Commission
Significance: Asthma is a priority for MDH and is one of the largest racial and ethnic health disparities in
terms of ED visit rates. Asthma is responsible for more Emergency Department (ED) visits
than some other major chronic disease such as hypertension and diabetes ED visits.
Created on 8/11/2022 at 8:37 PM
Page 281 of 296 pages

SPM 5 - Cross-Cutting Measure: Percentage of MCHB committees/workgroups that include community
members/persons with lived experience
Population Domain(s) – Cross-Cutting/Systems Building
Measure Status: Active
Goal: To have at least 50% of MCHB State Committees/workgroups include community
members/persons with lived experiences by SFY2025
Definition:
Unit Type: Percentage
Unit Number: 100
Numerator: Number of MCHB commissions/workgroups that include persons
with lived experience or community members
Denominator: Number of MCHB commissions that Title V staff coordinate
Data Sources and Data
Issues:
Title Data
Significance: Working towards MCHB policies and practices are centered on equity and anti-racism
principles will support Title V activities achieve inclusion and equity. The Title V staff would
like to see more MCHB commissions/workgroups that include persons with lived experience
or community members.
Created on 8/11/2022 at 8:37 PM
Page 282 of 296 pages

Form 10
State Outcome Measure (SOM) Detail Sheets
State: Maryland
No State Outcome Measures were created by the State.
Created on 8/11/2022 at 8:37 PM
Page 283 of 296 pages

Form 10
Evidence-Based or –Informed Strategy Measures (ESM) Detail Sheets
State: Maryland
ESM 3.1 - Percentage of Level III & IV Perinatal Referral Centers who received their re-designations based on the
2019 MD Perinatal System Standards
NPM 3 – Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive
Care Unit (NICU)
Measure Status: Active
Goal: To have 100% of Level III & IV Perinatal Referral Centers receive their re-designations based
on the 2019 MD Perinatal System Standards
Definition:
Unit Type: Percentage
Unit Number: 100
Numerator: Number of Level III & IV Perinatal Referral Centers who receive
their re-designations
Denominator: Total Number of Level III & IV Perinatal Referral Centers
Data Sources and Data
Issues:
Programmatic Data
Significance: Infants who are born at facilities that are equipped to meet the need of both the infant and
the birthing individual is important to improve both maternal and neonatal outcomes. Infants
born in appropriate level hospitals have a decreased risk of adverse outcomes. Since the
mid-1990s, Maryland has developed voluntary standards for Maryland hospitals providing
obstetric and neonatal services. The Standards have been incorporated into regulations for
designation of perinatal referral centers (Level III, and Level IV) by the Maryland Institute for
Emergency Medical Service Systems (MIEMSS). The re-designation of the Perinatal Referral
Center ensures that these Centers are equipped to meet the need of both the infant the
birthing individual
Created on 8/11/2022 at 8:37 PM
Page 284 of 296 pages

ESM 4.1 - Number of birthing hospitals designated as breastfeeding friendly
NPM 4 – A) Percent of infants who are ever breastfed B) Percent of infants breastfed exclusively through 6
months
Measure Status: Active
Goal: Increase the number of birthing hospitals promoting breastfeeding
Definition:
Unit Type: Count
Unit Number: 32
Numerator: Number of birthing hospitals that achieve Baby-Friendly
accreditation status
Denominator:
Data Sources and Data
Issues:
The information is from the Breastfeeding Policy Committee that tracks and monitors the
number of hospitals that have received the baby-friendly designation.
Significance: Increased support from hospitals will have a positive impact on the number of women who
initiate breastfeeding
Created on 8/11/2022 at 8:37 PM
Page 285 of 296 pages

ESM 5.1 - Percentage of infants less than 6 months who are placed on their backs to sleep
NPM 5 – A) Percent of infants placed to sleep on their backs B) Percent of infants placed to sleep on a separate
approved sleep surface C) Percent of infants placed to sleep without soft objects or loose bedding
Measure Status: Inactive - Replaced
Goal: Increased numbers of infants will be placed on their backs to sleep. Challenges to safe sleep
practices will be addressed
Definition:
Unit Type: Percentage
Unit Number: 100
Numerator: Number of infants less than 6 months placed on their backs to
sleep
Denominator: Total number of infants less than six months old
Data Sources and Data
Issues:
PRAMS, home visiting programs assessing safe sleep environments
Significance: Reduction in infant mortality
Created on 8/11/2022 at 8:37 PM
Page 286 of 296 pages

ESM 5.2 - Number of home visiting or care coordination clients, providers, and other Title V program participants
that received infant safe sleep counseling and information
NPM 5 – A) Percent of infants placed to sleep on their backs B) Percent of infants placed to sleep on a separate
approved sleep surface C) Percent of infants placed to sleep without soft objects or loose bedding
Measure Status: Active
Goal: To overall see an increase percentage of infants placed to sleep on their backs, on a
separate approved sleep surface, and placed to sleep without soft objects or loose bedding
with increased safe sleep counseling and information
Definition:
Unit Type: Count
Unit Number: 10,000
Numerator: Number of home visiting or care coordination clients, providers,
and other Title V program participants that received infant safe
sleep counseling and information
Denominator:
Data Sources and Data
Issues:
Title V Data Source
Evidence-based/informed
strategy:
The American Academy of Pediatrics recommend that infants sleep on their back, on a firm
surface without any loose bedding or soft objects. The strategy is to provide infant safe
sleep counseling and information to families as well as providers who work with families.
According to Ashley et al, receiving provider advice was associated with increased use of
safe sleep practices ( Prevalence and Factors Associated With Safe Infant Sleep Practices.
Pediatrics November 2019). By providing information and counselling to families and
providers who can provider counseling, this may increase the number of infants who are
sleeping safely.
Significance: This ESM measures the number of families and providers who are trained on the importance
of infant safe sleep, how infants can sleep safely. To change the culture of infant safe sleep,
it is important for all families to know how infants can sleep safely.
Created on 8/11/2022 at 8:37 PM
Page 287 of 296 pages

ESM 6.1 - Number of parents who receive information/education on the importance of developmental screenings
from Home Visiting and Care Coordination Title V providers
NPM 6 – Percent of children, ages 9 through 35 months, who received a developmental screening using a parent-
completed screening tool in the past year
Measure Status: Active
Goal: Increase the number of parents who receive education about developmental screening tools
from Home Visiting and Care Coordination Title V providers
Definition:
Unit Type: Count
Unit Number: 5,000
Numerator: Home Visiting, Care Coordination, and other Title V program
clients/parents who receive education about developmental
screening tools
Denominator:
Data Sources and Data
Issues:
MCHB Data
Significance: Early identification of developmental disorders is critical to the well-being of children and
their families. It is an integral function of the primary care medical home. The percent of
children with a developmental disorder has been increasing, yet overall screening rates
have remained low. The American Academy of Pediatrics recommends screening tests begin
at the nine month visit. Title V funds local health departments to educate parents of children
at risk for developmental delays or behavioral health issues about developmental screening.
Education is primarily focused on parents of children who are receiving local health
department case management for elevated blood lead levels or Infants & Toddlers Program
services.
Created on 8/11/2022 at 8:37 PM
Page 288 of 296 pages

ESM 10.2 - Number of adolescent (12-17) who receive well visits through school based health centers
NPM 10 – Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year.
Measure Status: Active
Goal: Increase the number of adolescents receiving annual well visits
Definition:
Unit Type: Count
Unit Number: 750,000
Numerator: Number of adolescents 12-17 receiving an annual well visit
Denominator:
Data Sources and Data
Issues:
MCHB Data
Evidence-based/informed
strategy:
Adolescents receiving well visits through school based health clinics
Significance: Preventive well visits for adolescents promote healthy behaviors, help reduce risk taking
behaviors and can detect conditions that may interfere with an adolescent's physical, social
and emotional growth and well-being.
Created on 8/11/2022 at 8:37 PM
Page 289 of 296 pages

ESM 11.1 - Number of CYSHCN who receive patient and family-centered care coordination services
NPM 11 – Percent of children with and without special health care needs, ages 0 through 17, who have a medical
home
Measure Status: Active
Goal: Increase the number of CYSHCN who receive patient and family-centered care coordination
services (CCS).
Definition:
Unit Type: Count
Unit Number: 70,000
Numerator: Number of CYSHCN who received CCS
Denominator:
Data Sources and Data
Issues:
DHMH/MCHB Data
Significance: The American Academy of Pediatrics (AAP) specifies seven qualities essential to medical
home care: accessible, family-centered, continuous, comprehensive, coordinated,
compassionate and culturally effective. CYSHCN who receive quality care coordination
services are less likely to experience medication errors, unnecessary or repetitive diagnostic
tests, unnecessary emergency room visits, and ultimately experience better health
outcomes.
Created on 8/11/2022 at 8:37 PM
Page 290 of 296 pages
ESM 12.1 - Number of CYSCHN and their families who participate in health care transition planning activities
NPM 12 – Percent of adolescents with and without special health care needs, ages 12 through 17, who received
services to prepare for the transition to adult health care
Measure Status: Active
Goal: Increase the number of CYSHCN and their families who participating in transition planning
activities
Definition:
Unit Type: Count
Unit Number: 50,000
Numerator: Number of YSHCN and families that participate in transition
planning activities.
Denominator:
Data Sources and Data
Issues:
DHMH/MCHB Data
Significance: According to American Academy of Pediatrics, Supporting the health care transition from
adolescence to adulthood in the medical home, as teens grow into adulthood, their health
care needs change. During this transition, most teens may begin to take more responsibility
for their health care and most will need to leave their pediatricians for adult health care
providers. As teens with special health care needs become adults, receiving proper health
care can be a challenge. Youth participating in their Health Care Transition Planning is part
of the process of becoming independent and learning to manage one’s own health while
preventing periods of gaps in services. Losing access to primary care, even for a short time,
can affect the long-term health of a youth with special health care needs.
Created on 8/11/2022 at 8:37 PM
Page 291 of 296 pages

ESM 13.1.1 - Percentage of pregnant individuals aged 21 and older on medical assistance in Maryland who
receive a preventive dental visit
NPM 13.1 – Percent of women who had a preventive dental visit during pregnancy
Measure Status: Active
Goal: To increase the number of pregnant individuals who have a preventive dental visit during
pregnancy
Definition:
Unit Type: Percentage
Unit Number: 100
Numerator: Number of pregnant women with Medicaid who have a dental visit
during pregnancy
Denominator: Total number of pregnancy women with Medicaid
Data Sources and Data
Issues:
Medicaid Data from Office of Oral Health
Significance: Preventive dental visits are indicative of overall health of both mother and infant.
Created on 8/11/2022 at 8:37 PM
Page 292 of 296 pages

ESM 14.1.1 - Number of pregnant individuals who use the statewide tobacco QuitLine
NPM 14.1 – Percent of women who smoke during pregnancy
Measure Status: Active
Goal: By 2022, increase by 5% the number of pregnant smokers who call the Quitline annually.
Definition:
Unit Type: Count
Unit Number: 200
Numerator: # of pregnant individuals who use the Maryland tobacco quitline
Denominator:
Data Sources and Data
Issues:
2016-2022 MDH Center for Tobacco Prevention and Control Quitline Data
Significance: Women who smoke during pregnancy are more likely to experience a fetal death or deliver a
low birth weight baby. Further, secondhand smoke (SHS) is a mixture of mainstream smoke
(exhaled by smoker) and the more toxic side stream smoke (from lit end of nicotine product)
which is classified as a “known human carcinogen” by the US Environmental Protection
Agency, the US National Toxicology Program, and the International Agency for Research on
Cancer. Adverse effects of parental smoking on children have been a clinical and public
health concern for decades and were documented in the 1986 U.S. Surgeon General
Report. The MDH Center for Tobacco Prevention and Control launched a Pregnancy
Rewards Program in 2014, which offers pregnant and postpartum women (up to six months)
rewards for series of completed calls with a Quit Coach. Though initially requiring referral by
physician, that barrier was removed and now a pregnant smoker can simply call and let the
Quitline know that she is pregnant and interested in the rewards/incentive program. This
ESM will measure the impact of the Pregnancy Rewards Program and
accompanying media campaigns/health communication interventions on the number of
pregnant Quitline callers.
Created on 8/11/2022 at 8:37 PM
Page 293 of 296 pages

Form 12
MCH Data Access and Linkages
State: Maryland
Annual Report Year 2021
Access Linkages
Data Sources
(A)
State Title V
Program has
Consistent
Annual Access
to Data
Source
(B)
State Title V
Program has
Access to an
Electronic
Data Source
(C)
Describe
Periodicity
(D)
Indicate Lag
Length for
Most Timely
Data Available
in Number of
Months
(E)
Data
Source
is Linked
to Vital
Records
Birth
(F)
Data
Source is
Linked to
Another
Data
Source
1) Vital Records Birth Yes Yes Annually 10
PRAMS
2) Vital Records Death Yes No Annually 10 No
3) Medicaid Yes No Quarterly 6 No
4) WIC Yes Yes More often than
monthly
2 No
5) Newborn Bloodspot
Screening
Yes Yes More often than
monthly
0 No
6) Newborn Hearing
Screening
Yes Yes More often than
monthly
0 No
7) Hospital Discharge Yes Yes Quarterly 4 No
8) PRAMS or PRAMS-like Yes Yes Annually 24 Yes
Created on 8/11/2022 at 8:37 PM
Page 295 of 296 pages

Form Notes for Form 12:
None
Field Level Notes for Form 12:
None
Created on 8/11/2022 at 8:37 PM
Page 296 of 296 pages






