
Chapter 2:
Principles for
Assessing Medicaid
Nursing Facility
Payment Policies

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
28
March 2023
Principles for Assessing Medicaid Nursing
Facility Payment Policies
Recommendations
2.1 To improve transparency of Medicaid spending, the Secretary of the U.S. Department of Health and
Human Services should direct the Centers for Medicare & Medicaid Services to collect and report the
following data in a standard format that enables analysis:
•
facility-level data on all types of Medicaid payments to nursing facilities, including resident
contributions to their cost of care;
•
data on the sources of non-federal share of spending necessary to determine net Medicaid
payment at the facility level; and
•
comprehensive data on nursing facility nances and ownership necessary to compare Medicaid
payments to the costs of care for Medicaid-covered residents and to examine the eects of real
estate ownership models and related-party transactions.
2.2 To help inform assessments of whether Medicaid nursing facility payments are consistent with
statutory goals of eciency, economy, quality, and access, the Secretary of the U.S. Department of
Health and Human Services should direct the Centers for Medicare & Medicaid Services (CMS) to
update the requirement that states conduct regular analyses of all Medicaid payments relative to the
costs of care for Medicaid-covered nursing facility residents. This analysis should also include an
assessment of how payments relate to quality outcomes and health disparities. CMS should provide
analytic support and technical assistance to help states complete these analyses, including guidance
on how states can accurately identify the costs of ecient and economically operated facilities with
adequate sta to meet residents’ care needs. States and CMS should make facility-level ndings
publicly available in a format that enables analysis.
Key Points
•
Medicaid is the largest payer for nursing facility care and has an important role to play in reducing
health disparities that have been exacerbated by the COVID-19 pandemic.
•
Medicaid payment rates and methods vary widely by state, and there are limited data available about
how rates compare to costs and how Medicaid payment policies aect quality outcomes.
•
Most Medicaid-covered nursing facility residents are dually eligible for Medicare, but payment
incentives for Medicare and Medicaid are not well aligned.
•
To advance Medicaid statutory goals of eciency, economy, quality, and access, states should do the
following:
– ensure that nursing facility payment rates are sucient to cover the costs of ecient and
economically operated facilities;
– design payment methods to incentivize better quality outcomes and reduce health disparities; and,
– aim to get the maximum value for the amount that they are spending.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
29
Report to Congress on Medicaid and CHIP
CHAPTER 2: Principles
for Assessing Medicaid
Nursing Facility
Payment Policies
Medicaid is the largest payer for nursing facility care
and has an important role to play in improving the
care that nursing facility residents receive. However,
facilities that serve a high share of Medicaid-covered
residents have long had worse quality outcomes on
average than other facilities. The COVID-19 pandemic
has exposed and exacerbated many of these
disparities. In response, policymakers are considering
a variety of reforms to how they regulate and pay for
nursing facility care.
The Commission has identied several principles
for states to consider when setting Medicaid nursing
facility payment rates and payment methods. These
principles are intended to advance the statutory goals
of Medicaid payment policy: economy, eciency,
quality, and access (§1902(a)(30)(A) of the Social
Security Act (the Act)).
First, in the Commission’s view, Medicaid payments
should be sucient to cover the costs of ecient
and economically operated nursing facilities. When
assessing payment adequacy, states should consider
all types of Medicaid payments that providers receive
and review reported costs carefully. For example,
states should consider the costs of stang facilities at
appropriate levels to meet residents’ care needs and
the potential for transactions with related parties in the
same nursing facility chain to inate costs reported on
state cost reports.
Second, states should design nursing facility payment
methods to incentivize better quality outcomes and
reductions in health disparities. Although many of
the factors that aect quality care are outside of
Medicaid’s authority, the persistent disparities between
Medicaid-covered residents and those covered by
other payers are an issue that Medicaid payment
policy can help address. Doing so would also help
reduce racial and ethnic disparities.
Finally, nursing facility payment policies should be
evaluated based on whether they are ecient—that
is, whether states are getting the maximum value for
the amount they are spending. Comparing payment
rates and quality outcomes across states can help
identify potential opportunities to improve eciency,
particularly in states with relatively high payment rates
and poor outcomes. In addition, policymakers should
continue to explore opportunities to improve eciency
across payers by better aligning payment incentives
for patients dually eligible for Medicare and Medicaid.
More detailed state-level analyses are needed to
identify the best approaches for each state, which
would require increased state capacity to examine
these issues.
The Commission recommends that the Secretary of
the U.S. Department of Health and Human Services
(HHS) direct the Centers for Medicare & Medicaid
Services (CMS) to take the following actions to
improve the availability of data to assess whether state
payment policies are consistent with these principles:
•
To improve transparency of Medicaid spending,
the Secretary of HHS should direct CMS to
collect and report the following data in a standard
format that enables analysis:
– facility-level data on all types of Medicaid
payments to nursing facilities, including
resident contributions to their cost of care;
– data on the sources of non-federal share
of spending necessary to determine net
Medicaid payment at the facility level; and
– comprehensive data on nursing facility
nances and ownership necessary to
compare Medicaid payments to the costs of
care for Medicaid-covered residents and to
examine the eects of real estate ownership
models and related-party transactions.
•
To help inform assessments of whether Medicaid
nursing facility payments are consistent with
statutory goals of eciency, economy, quality, and
access, the Secretary of HHS should direct CMS
to update the requirement that states conduct
regular analyses of all Medicaid payments
relative to the costs of care for Medicaid-covered
nursing facility residents. This analysis should
also include an assessment of how payments
relate to quality outcomes and health disparities.
CMS should provide analytic support and
technical assistance to help states complete

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
30
March 2023
these analyses, including guidance on how states
can accurately identify the costs of ecient and
economically operated facilities with adequate
sta to meet residents’ care needs. States and
CMS should make facility-level ndings publicly
available in a format that enables analysis.
The Commission reviewed data on Medicaid payment
methods, payment amounts, and quality outcomes
to better understand the factors that aect the
development of nursing facility payment policies and
whether they are achieving their intended goals. This
chapter summarizes the Commission’s analyses, which
informed the development of the Commission’s payment
principles and recommendations. The chapter begins
with background information on nursing facility industry
trends and Medicaid’s role relative to other payers. Then
it discusses current Medicaid payment policies, how they
can be used to improve quality, and how they align with
other payers. The chapter concludes by discussing the
payment principles, recommendations, and supporting
rationale in more detail.
As more information on Medicaid nursing facility
payments becomes available, the Commission
will continue to monitor state payment policies. In
particular, the Commission will closely follow how any
future changes in federal regulatory requirements (e.g.,
minimum stang standards) aect states, providers,
and beneciaries.
Background
Nursing facilities are institutions certied by a state
to oer 24-hour medical and skilled nursing care,
rehabilitation, or health-related services to individuals
who do not require hospital care.
1
Medicaid is the
primary payer for most nursing facility residents, but
it generally pays less than other payers. The nursing
facility industry faces a number of challenges, which
are generally worse for facilities that serve a high
share of Medicaid-covered residents and have been
exacerbated by the COVID-19 pandemic.
Role of nursing facilities in the
continuum of care
Nursing facilities provide both short-term care for
patients recovering from a hospital stay and long-
term care for residents who need ongoing assistance
with activities of daily living. Of the approximately 1.1
million patients and residents receiving care in nursing
facilities on September 30, 2019, about half had short
stays of less than 100 days, and half had long stays of
more than 100 days (Abt Associates 2020).
2
The short-term care that nursing facilities provide
(referred to as “skilled nursing facility (SNF) services”)
is part of the continuum of post-acute care after a
hospital stay. Nursing facilities generally provide more
intensive care than home health providers and less
intensive care than rehabilitation or long-term care
hospitals. In 2019, nursing facilities accounted for
about half of all Medicare hospital discharges to post-
acute care providers (MedPAC 2022a).
The long-term care that nursing facilities provide is
also part of the continuum of long-term services and
supports (LTSS). Nursing facility services remain an
important site of care for beneciaries who are not able
to receive care in the community. In scal year 2019,
nursing facility services accounted for about 80 percent
of Medicaid spending on institutional LTSS, 33 percent
of total Medicaid LTSS expenditures, and 11 percent of
total Medicaid spending (Murray et al. 2021).
3
Medicaid coverage of nursing
facility care
In 2019, Medicaid was the primary payer for 59
percent of nursing facility residents (Figure 2-1). Most
Medicaid-covered nursing facility residents had long
stays, but about one-quarter of Medicaid-covered
residents had short stays of less than 100 days.
Medicare is the largest payer of short-stay nursing
facility residents. About 19 percent of nursing facility
residents were not covered by either Medicare or
Medicaid. Long-stay residents not covered by Medicare
or Medicaid likely paid for their care out of pocket
because private insurance coverage for long-term care
is rare.
4
About 90 percent of Medicaid-covered nursing facility
residents are older than age 65 (Abt Associates 2020).
Non-elderly Medicaid beneciaries with a need for
institutional LTSS are often served in other settings,
such as intermediate care facilities for individuals with
intellectual or developmental disabilities, which are
outside the scope of this chapter (ASPE 2013).

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
31
Report to Congress on Medicaid and CHIP
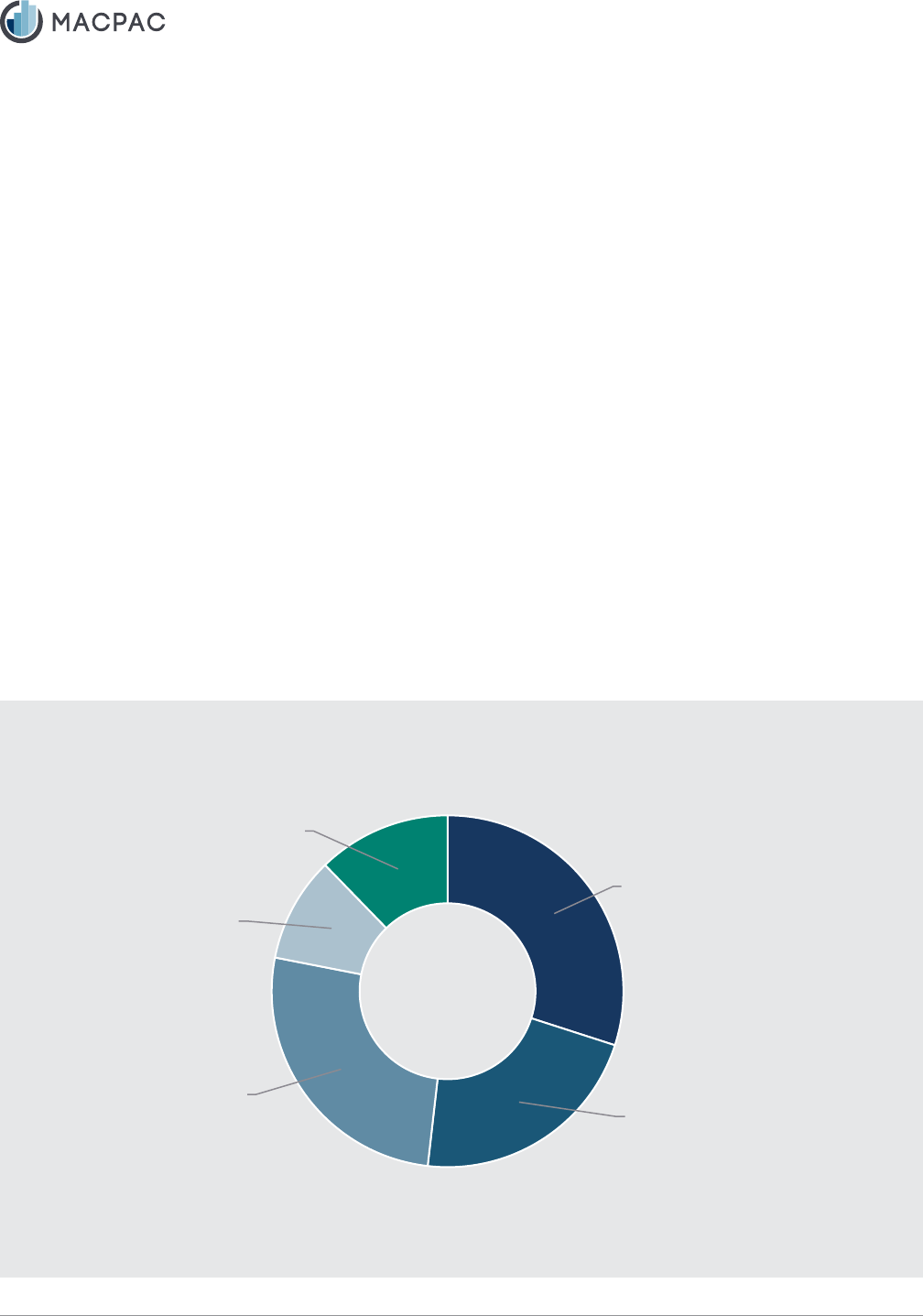
FIGURE 2-1. Characteristics of Nursing Facility Patients and Residents by Primary Payer and Length of
Stay, 2019
Medicare,
short stay,
22%
Other, short stay,
11%
Other, long stay, 8%
Medicaid,
short stay,
27%
Medicaid,
long stay,
73%
Medicaid, 59%
Notes: Short-stay patients are dened as individuals residing in the facility for less than 100 days. Long-stay
residents are dened as residing for more than 100 days. Analysis is based on nursing facility residents who were
active on September 30, 2019. Length of stay is based on the number of days between the entry date and the target
date of the latest Minimum Data Set assessment used in the analysis, not the discharge date of the stay.
Source: Abt Associates 2020.
Medicaid eligibility requirements. To qualify for
Medicaid coverage, nursing facility residents must
have low income and assets. Many Medicaid-
covered nursing facility residents are eligible through
mandatory eligibility pathways that are tied to the
receipt of supplemental security income (SSI), which
in 2022 had an income limit of $841 a month and an
asset limit of $2,000 for individuals. As of 2018, 42
states also provided Medicaid coverage to nursing
facility residents with incomes up to 300 percent of
the SSI limit (an option referred to as the “special
income rule”), 25 states used the medically needy
option to allow higher-income individuals to qualify
for Medicaid coverage by subtracting the amount that
they paid for their care from their income (a process
referred to as “spenddown”), and 21 states provided
coverage to seniors and persons with disabilities up
to 100 percent of the federal poverty level regardless
of whether they had a nursing facility level of care
(referred to as the “poverty-level pathway”) (Musumeci
et al. 2019).
5
According to an analysis by the HHS
Assistant Secretary for Planning and Evaluation using
2006–2007 data, 22 percent of Medicaid-covered
nursing facility residents qualied through SSI-related
pathways, 50 percent qualied through the special
income rule, 21 percent qualied through a medically
needy pathway, and about 7 percent qualied through
the poverty-level pathway (ASPE 2013).
Because the out-of-pocket costs for nursing facility
care are substantial and few individuals have private
long-term care insurance, many private-pay nursing
facility residents with long stays eventually become
eligible for Medicaid after spending most of their
income and assets toward the cost of their care.
6
In
2001, more than half of Medicaid-covered nursing
facility residents began their Medicaid coverage
after residing in the nursing facility, and 21 percent
of Medicaid-covered residents began coverage
after residing in the facility for more than six months
(Wenzlow et al. 2008).
Post-eligibility treatment of income. Unlike many
other Medicaid beneciaries who have little or no cost-
sharing obligations, recipients of LTSS are required
to contribute most of their income toward the cost of
their care through a process known as “post-eligibility
Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
32
March 2023
treatment of income.” The amount of income that a
beneciary can retain is set by the state’s personal
needs allowance and other exceptions.
7
In 2018, the
median state personal needs allowance for institutional
care was $50 per month, meaning that in most
states, all but a small amount of a Medicaid-covered
resident’s income went toward the cost of their care
(Musumeci et al. 2019).
Residents’ contributions to the cost of their care reduce
the amount of state and federal Medicaid payments
that a facility receives. In 2019, these contributions
accounted for about 10 percent of Medicaid payments
to nursing facilities (MACPAC 2023a).
Patients dually eligible for Medicare and Medicaid.
The vast majority (84 percent) of Medicaid-covered
nursing facility residents are dually eligible for
Medicare and Medicaid (Abt Associates 2020). For
these beneciaries, Medicare pays for SNF care
during the initial portion of their stay, and Medicaid
pays for subsequent days of care. Medicare Part
B also continues to cover physician and therapy
services for long-stay nursing facility residents after
the Medicare Part A SNF benet is exhausted.
State Medicaid programs have the option to pay for
Medicare cost sharing during the initial portion of the
stay, but most do not, which results in lower payments
to the facility (MACPAC 2013).
Medicaid payments compared with
other payers
According to the National Health Expenditure
Accounts, Medicaid accounted for 30 percent of total
revenue for all nursing facilities, including those that
were part of continuing care retirement communities,
in 2019 (Figure 2-2). Although Medicaid is the largest
payer for nursing facility services, Medicaid payments
as a share of total revenue are much lower than
the share of nursing facility residents covered by
Medicaid (59 percent) (Abt Associates 2020). Medicaid
payments are generally lower than other payers
because of dierences in the services that Medicaid
covers and because Medicare typically pays facilities
much more than the costs of care for Medicare-
covered patients.
FIGURE 2-2. Sources of Revenue for Nursing Facilities and Continuing Care Retirement Communities,
2019
Medicaid, 30%
Medicare, 22%
Private health
insurance, 10%
Other third-party
payers, 12%
Out-of-pocket
spending, 26%
Note: Analysis includes all certied nursing facilities, including those part of continuing care retirement communities.
Source: OACT 2022.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
33
Report to Congress on Medicaid and CHIP
Dierences in resident acuity and covered services.
Medicaid payment rates are not comparable to those
in Medicare because of dierences in resident acuity
and the services that Medicaid covers. First, long-stay
residents, who are predominately covered by Medicaid,
generally have less intensive nursing and therapy care
needs than short-stay patients covered by Medicare,
so the costs of their care are lower (MACPAC 2023a,
Abt Associates 2020). Second, for patients dually
eligible for Medicare and Medicaid, Medicare Part
B continues to pay for some physician and therapy
services for long-stay residents, and so these services
are not included in the Medicaid rate. Third, because
of Medicaid spenddown and post-eligibility treatment of
income rules, many Medicaid-covered residents pay for
a substantial portion of their care out of pocket, which
reduces the amount that Medicaid pays the facility.
Medicare payment rates often exceed facility
costs. According to the Medicare Payment Advisory
Commission (MedPAC), Medicare has long paid SNF
payments much more than their costs of care for
Medicare-covered patients. For example, freestanding
nursing facilities reported a 20 percent aggregate
Medicare prot margin in scal year 2019, compared
with an aggregate non-Medicare margin of -2 percent
(MedPAC 2021). Although some stakeholders contend
that high Medicare payment rates are justied because
they can oset low Medicaid payment rates, MedPAC
has long argued that this policy is inecient, since
the policy benets facilities that serve more Medicare-
covered residents instead of facilities that serve a
high share of Medicaid-covered residents (MedPAC
2022b). In addition, because Medicare payment rates
are set nationally, they do not account for dierences
in Medicaid payment rates across states. As discussed
in the following sections, state payment rates vary
widely, and in some states, facilities report positive
Medicaid margins.
Industry trends
In 2019, there were 15,462 certied nursing facilities
nationwide. Most nursing facilities (93 percent) are
certied by both Medicare and Medicaid, and most of
these facilities (97 percent) are freestanding, meaning
that they are not based within a hospital. Roughly
9 percent of facilities are part of a continuing care
retirement community, which includes assisted living
options in addition to certied nursing facility beds (Abt
Associates 2022).
Ownership. In 2022, most nursing facilities (72 percent)
were for prot, and about two-thirds of facilities (66
percent) were also part of a larger chain.
8
Nursing
facility chains vary widely in size: in 2022, about 15
percent of nursing facilities were part of chains with
10 facilities or fewer, and about 11 percent of nursing
facilities were part of chains with more than 100 facilities
(ASPE 2022a).
Between 2016 and 2021, a total of 3,254 nursing
facilities were sold, and the pace of transactions has
generally increased since 2016 (ASPE 2022b). About
one-third of these transactions involved multiple owners
(ASPE 2022b). For example, multiple related parties
can own a nursing facility when a private equity rm
purchases a nursing facility, sells the real estate to
another entity, and then leases the building to a third
entity that manages the care provided.
Declining occupancy rates. Even before the
COVID-19 pandemic, nursing facility occupancy rates
were declining, which creates nancial challenges for
facilities that must continue to pay xed overhead and
capital costs with declining revenue. Between 2010 and
2019, occupancy rates declined from 88 to 85 percent,
in part because of eorts to shift care to home- and
community-based services, and since the start of the
COVID-19 pandemic, occupancy rates have declined
even further (MedPAC 2022b). In January 2021, median
occupancy rates reached a low of 69 percent, and by
November 2022, median occupancy rates were 78
percent (CLA 2023).
Nursing facility closures. Between 2015 and 2019,
more than 500 nursing facilities closed (Flinn 2020).
Although some closures are expected as care shifts
from nursing facilities to other settings, closures can be
particularly problematic in rural areas where residents
may not have access to other facilities nearby where
their loved ones can easily visit. In 2018, 7.7 percent
of U.S. counties had no nursing facility, an increase
of 44 counties since 2008; these closures were more
common in facilities that served a higher share of
Medicaid-covered residents (Sharma et al. 2021).
New care models. Despite the challenges that
the nursing facility industry faces, some providers
are testing new models of care that reect resident
preferences for less institutional, more homelike
settings. One example is the Green House initiative
launched in 2003 with funding from the Robert Wood
Johnson Foundation. In contrast to the average

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
34
March 2023
nursing facility, which has about 100 beds with many
shared rooms, facilities participating in the Green
House initiative have about 10 to 12 beds and single-
occupancy rooms. The model has shown promising
quality outcomes, but these facilities represent less
than 2 percent of nursing facilities and serve less than 1
percent of all nursing facility residents. Moreover, these
facilities report that it has been challenging to expand
access to more Medicaid-covered nursing facility
residents because of Medicaid payment rates and state
limitations on Medicaid covering private rooms if they
are not medically necessary (Waters 2021).
Facilities that serve a high share of
Medicaid-covered residents
The payer mix of Medicaid, Medicare, and private-
pay residents varies widely and is associated with a
number of facility characteristics (Table 2-1). Although
some of these dierences may reect facility decisions
on whether to accept more short-stay patients versus
long-stay residents, they also reect facility decisions
about whether to accept Medicaid-covered residents.
Federal law prohibits facilities from discharging a
resident once they become Medicaid eligible, but
in many states, facilities can choose to not admit
residents who are likely to become Medicaid eligible.
9
As a result, there is evidence that Medicaid-covered
residents may have more diculty accessing high-
quality facilities (Sharma et al. 2020).
Quality ratings. On average, facilities that serve a
high share of Medicaid-covered residents have lower
quality ratings than other facilities on all of the domains
measured by the Medicare.gov Care Compare ve-
star rating system (Box 2-1). However, there is wide
variation in the quality of care provided to Medicaid-
covered residents, and in 2019, 12 percent of facilities
that served the highest quartile of Medicaid-covered
residents had ve-star ratings overall (the highest
on Care Compare) compared with 21 percent of all
facilities in our analysis.
TABLE 2-1. Facility Characteristics by Payer Mix, 2019
Characteristics All facilities
Share of residents whose primary support was Medicaid
Lowest
quartile
(< 48%)
Second
quartile
(48–61%)
Third
quartile
(61–71%)
Highest
quartile
(> 71%)
Average Medicare.gov Care Compare ve-star quality ratings
Overall rating 3.1 3.7 3.1 2.8 2.7
Inspection component 2.7 3.2 2.8 2.6 2.4
Stang component 2.9 3.4 2.9 2.7 2.6
Quality measure component 3.6 3.9 3.6 3.5 3.4
Race and ethnicity of nursing facility residents
White, non-Hispanic 77% 86% 81% 74% 65%
Black, non-Hispanic 13 7 10 15 21
Hispanic 5 3 4 6 7
Other 5 5 5 6 6
Ownership
Private, for prot 74% 56% 73% 82% 84%
Private, non-prot 21 38 22 13 11
Public 5 6 5 5 5
Note: Analysis excludes hospital-based nursing facilities and those that are not dually certied by Medicaid and Medicare.
Sources: MACPAC, 2022, analysis of Medicare.gov Care Compare, Medicare cost reports, and the Minimum Data Set.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
35
Report to Congress on Medicaid and CHIP
Racial and ethnic disparities. Facilities serving
a high share of Medicaid-covered residents also
serve more racial and ethnic minorities, so poor
quality ratings in these facilities contribute to health
disparities. In general, Black Medicaid beneciaries
are more likely than white Medicaid beneciaries
to receive care in nursing facilities, and when they
do, they are less likely to be admitted to high-quality
facilities (Zuckerman et al. 2018). The racial and ethnic
disparities in nursing facility care are long standing
and have persisted even as other health care settings,
such as hospitals, have been desegregated (Nolen et
al. 2020).
Facility ownership. For-prot facilities are more likely
to serve a high share of Medicaid patients than non-
prot facilities. For-prot facilities generally have lower
stang levels than other facilities and have lower
average quality ratings than other types of facilities
(Paul et al. 2016). As a result, some of the dierences
in quality by payer mix that we observe may be a
result of dierences in facility ownership. Recent
research has highlighted additional quality challenges
in for-prot facilities owned by private equity investors,
but we do not have data to distinguish these facilities
from other for-prot facilities (Braun et al. 2021, Gupta
et al. 2021).
BOX 2-1. Medicare.gov Care Compare Five-Star Ratings for Nursing
Facilities
Since 2008, the Centers for Medicare & Medicaid Services (CMS) has been reporting ve-star quality
ratings for nursing facilities on its Medicare.gov Care Compare website. The composite ve-star rating is
based on three components that have continued to be rened over time:
•
Inspection star ratings based on the ndings from on-site inspections conducted by state survey
agencies to assess practices to ensure the safety of residents.
10
Facilities receive a lower star
rating if they have more identied deciencies and if these problems persist upon follow-up visits.
Star ratings are assigned on a curve, and so the 20 percent of facilities in each state with the worst
inspection ratings are assigned one star, and the 10 percent of facilities with the best inspection
ratings in each state are assigned ve stars.
•
Stang star ratings based on nursing facilities’ reported hours of registered nurse and total nurse
stang, which includes registered nurses, licensed practical nurses, and certied nurse assistants.
After adjusting for dierences in resident acuity, facilities with higher stang hours per resident
day relative to other facilities receive higher star ratings. Historically, nursing facilities self-reported
stang data to CMS, but since 2016, CMS has required nursing facilities to submit stang data
through an auditable payroll-based journal (PBJ) system that is more accurate. CMS began using
PBJ data for star ratings in 2018. In 2022, CMS began using the PBJ data to include additional
measures of sta turnover and weekend stang in Care Compare (CMS 2022a). These additional
measures are not included in our analyses of 2019 stang ratings.
•
Quality star ratings based on performance on a range of measures used to assess quality of care
for short-stay and long-stay nursing facility residents. Many of the measures are calculated using
data from the Minimum Data Set, which collects information on all nursing facility residents. In 2019,
CMS added several additional measures based on Medicare fee-for-service claims data, which are
included in our analysis (CMS 2019). Some of these claims-based measures, such as hospitalization
and emergency department visit rates, include patients dually eligible for Medicare and Medicaid
because Medicare is the primary payer for hospital care. However, these measures do not include
patients who are enrolled in Medicare Advantage plans, including plans intended to integrate care for
dually eligible patients.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
36
March 2023
Eects of COVID-19 pandemic
The COVID-19 pandemic has had a disproportionate
eect on nursing facilities and their residents. Although
nursing facility residents account for less than 1 percent
of the U.S. population, they have accounted for about
15 percent of COVID-19 deaths as of December 2022
(CMS 2022b).
While the level of community spread is the primary
contributor to the rate of COVID-19 infections in
nursing facilities, the pandemic has also exposed
and exacerbated long-standing nursing facility quality
issues (GAO 2022). A low number of direct care sta
per resident and the use of shared rooms have been
associated with rates of COVID-19 transmission
and death (Harrington et al. 2020a, Li et al. 2020).
Because Medicaid-covered residents are more
likely to reside in facilities with these characteristics,
studies have found that these residents have been
disproportionately aected by the pandemic (Weech-
Maldonado et al. 2021).
As discussed previously, the COVID-19 pandemic has
also led to declines in nursing facility occupancy rates,
which have created nancial challenges for facilities
because of their xed overhead and capital costs.
Although some of the declining occupancy is due to
an acceleration of the shifting patterns for post-acute
care and LTSS that began before the pandemic,
some changes in the occupancy have been driven by
pandemic-specic factors, such as the high death rate
of nursing facility residents.
In response to lower occupancy rates, nursing facilities
have also decreased stang levels. For example,
between January and September 2020, the number
of direct care hours declined 9.8 percent, which was
commensurate with the decline in nursing facility
residents (Werner and Coe 2021). However, as use of
nursing facility care begins to recover from pandemic
lows, some facilities have reported challenges rehiring
sta because of increased labor costs, and without
sucient sta, facilities cannot use all available beds
(CLA 2023).
A variety of state and federal policy changes have
supported nursing facilities during the COVID-19 public
health emergency. For example, the Coronavirus Aid,
Relief, and Economic Security Act (CARES Act, P.L.
116-136) created a time-limited provider relief fund
to oset immediate losses and also provided grants
to states that some have used to increase Medicaid
payment rates (MACPAC 2021a). In addition, CMS
has authorized a number of temporary waivers of
regulatory requirements for nursing facilities, including
allowing nursing facilities to be paid Medicare’s higher
SNF rate for long-stay residents with acute care
needs without requiring a prior hospital stay. These
temporary changes have helped most nursing facilities
manage the disruption in their nances so far, but many
providers are concerned about their nancial viability
after these policies expire (CLA 2023, 2022a).
Policymakers are also using early lessons from the
pandemic to consider a variety of permanent nursing
facility regulatory and payment reforms. In 2022, the
National Academies of Sciences, Engineering, and
Medicine released a report recommending a variety
of reforms to CMS’s oversight of nursing facilities
and changes to Medicare and Medicaid policies.
Notably, the report calls for greater transparency and
stronger evaluations of Medicaid nursing facility rates,
which align with the Commission’s recommendations
discussed later in this chapter (National Academies
2022).
Medicaid Payment Policies
States have considerable exibility to set Medicaid
nursing facility payment rates and methods. MACPAC’s
analyses of these policies have found wide variation
in the types of payments that states make, how these
payments are nanced, and how Medicaid payments
compare to nursing facility costs.
Federal Medicaid payment
requirements
Nursing facility services have been a required Medicaid
benet since the program’s enactment in 1965, but
Congress has made several changes over time to the
rules governing how states pay providers. The original
statute had few limitations, but in 1972, Congress
required that states pay on a reasonable cost-related
basis, similar to Medicare, because of concerns that
states were overpaying providers (Committee on
Finance 1972).
11
In 1980, the Boren amendment to
the Omnibus Budget Reconciliation Act of 1980 (P.L.
96-499) removed this requirement and instead required
Medicaid nursing facility payments to be “reasonable

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
37
Report to Congress on Medicaid and CHIP
and adequate to meet the costs which must be incurred
by eciently and economically operated facilities in
order to provide care and services in conformity with
applicable state and federal laws, regulations, and
quality and safety standards.” To help states meet
this requirement, the Boren amendment also required
nursing facilities to submit uniform Medicaid cost reports.
The Boren amendment was dicult to implement and
led to a number of provider lawsuits. CMS never formally
dened an “ecient and economically operated” facility,
so each state developed its own method to comply with
this requirement. In 1990, the U.S. Supreme Court ruled
in Wilder v. Virginia Hospital Association that the Boren
amendment created a privately enforceable right for
providers, which led to a growth of lawsuits challenging
provider payment rates and the methods that states had
used to develop them (Wiener and Stevenson 1998).
12
In 1996, Congress repealed the Boren amendment and
gave states additional exibility to set their own payment
rates as long as they developed them using a public
process (§1902(a)(13)(A) of the Act).
A separate Medicaid statutory provision, Section
1902(a)(30)(A) of the Act, still requires Medicaid
payment policies to be consistent with the principles
of eciency, economy, quality, and access to care.
13
In 2015, the U.S. Supreme Court ruled in Armstrong v.
Exceptional Child Center, Inc. that providers no longer
have a right to sue in federal court to enforce these
Medicaid payment requirements, so now they can only
be enforced by CMS.
14
Types of Medicaid payments to nursing
facilities
In 2019, nursing facilities were paid approximately
$66.5 billion for care to Medicaid-covered residents
(Figure 2-3). The two main categories of payment
are base payments, which are typically paid on a per
diem basis for a specic resident, and supplemental
payments, which are generally paid in a lump sum for a
xed period of time. Most payments are base payments
made through the fee-for-service (FFS) delivery
system, but a growing share of Medicaid payments
to nursing facilities are made through managed care
and supplemental payments. In the following sections,
we discuss each of these types of payments in more
detail as well as the limitations of available data for
measuring these payments.
FIGURE 2-3. Base and Supplemental Payments to Nursing Facilities, 2019
FFS and managed care
base payments paid by
residents (estimate),
$6.1 billion,
9%
Supplemental payments,
$3.4 billion,
5%
Managed care
payments paid
by state,
$19.4 billion,
29%
FFS base
payments
paid by state,
$37.6 billion,
57%
Notes: FFS is fee for service. Resident contributions to their share of cost are estimated based on the dierence
between allowed payment rates and actual Medicaid payment amounts in states with available data.
Sources: MACPAC, 2022, analysis of CMS-64 net expenditure data and the Transformed Medicaid Statistical
Information System (T-MSIS).

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
38
March 2023
FFS base payments. Medicaid programs typically
pay nursing facilities a daily rate for Medicaid-covered
residents according to a state fee schedule. Currently,
most states set Medicaid nursing facility payments
based on the costs for various cost centers, such as
direct care (i.e., medical supplies and wages of sta
providing direct care), indirect care (e.g., the costs of
social services and patient activities), administration,
and capital. However, Medicaid payments are not
intended to cover all costs for all facilities because
states set limits on which costs are allowable and set
ceilings on the amount of costs that can be reimbursed
for particular cost centers (e.g., a xed percentage
of the median or average costs for a particular cost
center among similar facilities in the state). Less
than a third of states use a price-based method to
set payments prospectively based on historic costs
adjusted for ination and other factors (MACPAC
2019a, 2019b).
The base payments that states pay are reduced by
resident contributions to their cost of care, which are
paid to the facility directly. Based on our analysis of
claims data in the Transformed Medicaid Statistical
Information System (T-MSIS), resident contributions
to their cost of care accounted for about 10 percent of
base payments to nursing facilities in 2019 (MACPAC
2023a).
Managed care base payments. In 2019, 24 states
paid for some or all nursing facility care through
managed care organizations, up from just 8 states
in 2004. Most states with managed LTSS (MLTSS)
include full coverage for nursing facility services,
although some states carve out long-stay nursing
facility residents from some programs (Dobson et al.
2021, Lewis et al. 2018).
In April 2016, CMS established a new option for
states to direct managed care plans to pay particular
types of providers according to specied rates or
methods, which is referred to as “directed payments.”
Based on MACPAC’s review of directed payment
arrangements approved as of December 31, 2020, 14
states established minimum fee schedules for nursing
facility services provided in managed care (typically
no less than the Medicaid FFS rate), and 6 states
required managed care plans to increase payments
to nursing facilities by a xed amount above base
payment rates, similar to supplemental payments in
FFS (MACPAC 2022a).
Managed care payments to nursing facilities are also
subject to post-eligibility treatment of income rules,
but information on resident contributions to their cost
of care is not available for all states. For example,
in our analyses of 2019 T-MSIS data, ve states
with MLTSS reported managed care base payments
paid by the state but did not report the total allowed
amount, after accounting for resident contributions
to their share of cost, and so we could not include
managed care payments in these states in our
analyses (MACPAC 2023a).
The limited data available on managed care payments
to nursing facilities suggest that they are similar to
FFS in many states. In the four states with MLTSS that
we interviewed in 2020 (Kansas, New York, Rhode
Island, and Wisconsin), managed care plans all paid
nursing facilities according to FFS rates and methods.
Many states had directed payment arrangements
that required plans to pay facilities’ FFS rates, but
plans also noted that it was administratively easier to
do so. Because many managed care plans relied on
state rate setting methods to set their own rates, the
stakeholders we interviewed noted the need for states
to maintain their FFS rate setting capacity even after
moving to MLTSS (MACPAC 2020a).
Supplemental payments. In 2019, 23 states made
a total of $3.4 billion in supplemental payments to
nursing facilities, which accounted for approximately
5 percent of total nursing facility payments. The use
of supplemental payments varies widely by state: 27
states and the District of Columbia did not make any
supplemental payments, and 6 states made payments
that were more than 30 percent of total FFS Medicaid
payments to nursing facilities (MACPAC 2020b).
Medicaid FFS base payment rates and supplemental
payments cannot exceed the upper payment limit
(UPL), which is an estimate of what Medicare would
have paid for the same service in the aggregate.
15
States are required to submit provider-level
information on base and supplemental payments to
CMS annually to demonstrate compliance with these
UPL requirements (CMS 2022c). When calculating the
UPL, states are supposed to account for dierences
in resident acuity and dierences in services that
Medicaid and Medicare cover; nevertheless, states
and CMS still face challenges accurately calculating
the UPL because Medicaid and Medicare payment
rates are not directly comparable (CMS 2022c).

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
39
Report to Congress on Medicaid and CHIP
MACPAC’s review of these UPL demonstration data
found several discrepancies between the amount
of payments reported on UPL demonstrations and
the amount of payments claimed by states on CMS-
64 reports in the Medicaid Budget and Expenditure
System (MBES), which is the ocial record of actual
Medicaid spending.
16
CMS is currently implementing
a new process for states to report provider-level
supplemental payment data through MBES, which will
hopefully help improve the reliability of these data in
future years (CMS 2021).
Financing of Medicaid payments
Similar to other Medicaid payments, states and
the federal government jointly nance Medicaid
nursing facility payments according to the state’s
federal matching assistance percentage (FMAP).
The non-federal share of Medicaid payments can
be nanced by state general funds, provider taxes,
and intergovernmental transfers (IGTs) or certied
public expenditures (CPEs) from local governments,
including publicly owned nursing facilities.
State use of nursing facility provider taxes has grown
in recent years, from 22 states in 2004 to 45 states in
2019 (Giord et al. 2019). States are allowed to use
provider taxes to nance their Medicaid programs
as long as the taxes are imposed on a broad base
of providers (i.e., not just providers who serve a high
share of Medicaid patients), are uniformly applied
based on a common tax basis (e.g., provider revenue
or the number of certied nursing facility beds), and
do not guarantee that providers are paid back the
amount that they contribute in taxes. In practice, many
states use the increased federal funding generated
by provider taxes to increase Medicaid payments,
which is permissible as long as the tax does not
exceed 6 percent of net patient revenue for the class
of providers. Many states impose taxes up to this
maximum allowable amount, and in 2019, 22 states
had nursing facility provider taxes between 5.5 and 6
percent of provider revenue (KFF 2020).
17
IGTs and CPEs are commonly used to nance nursing
facilities that are publicly owned, which accounted
for about 5 percent of all nursing facilities, according
to Medicare cost reports in 2019. However, in some
states, the number of facilities that are classied
as publicly owned for Medicaid purposes is much
higher than the number on Medicare cost reports
because of complex ownership arrangements between
public hospitals and privately operated nursing
facilities. Specically, in some states, it is common
for public hospitals to buy or lease privately operated
nursing facilities so that these facilities can receive
IGT-nanced supplemental payments targeted to
government-owned facilities. For example, in Indiana,
90 percent of nursing facilities in the state received
supplemental payments targeted to government-
owned facilities in 2019, including 181 facilities that
were classied as privately owned on Medicare cost
reports (MACPAC 2023b). Indiana reported more than
$1 billion in nursing facility supplemental payments in
2019, more than any other state, but it is unclear how
much of these payments were retained by nursing
facilities and how much of these payments were
returned to the public hospitals that nanced these
payments (Galewitz 2017).
During interviews with stakeholders about the factors
that aect their nursing facility payment methods,
we learned that state decisions to use supplemental
payments are often aected by the methods that
states use to nance the non-federal share of Medicaid
payments. Although states and nursing facilities
generally preferred that rate increases be implemented
through increases to base payments rather than
supplemental payments, these stakeholders generally
viewed supplemental payments as a better way to
target funding to providers to ensure that they were
paid back the amount that they contributed through
provider taxes or IGTs (MACPAC 2020a).
Base payment rates vary widely
According to our analyses of base payment rates
reported in T-MSIS in 2019, Medicaid nursing facility
payment rates varied widely by state and facility. Even
after adjusting for dierences in the area wage index
and dierences in resident case mix, average state
payment rates ranged from 62 to 182 percent of the
national average. Across facilities within states, we also
observed considerable variation (MACPAC 2023a).
Although Medicaid rates are often lower than costs,
we found that Medicaid payments appeared to exceed
the costs of care in some facilities in 2019 (Figure 2-4).
The median facility had payment rates that were 86
percent of costs. However, about one-fth of facilities

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
40
March 2023
had base payment rates greater than 100 percent of
costs, and 15 percent of facilities had base payment
rates less than 70 percent of costs.
Our estimates of Medicaid payments relative to costs
have several limitations. First, we were not able to nd
reliable data on supplemental payments to providers in
all states. In states in which data were available, they
suggested that these payments can substantially aect
the distribution of Medicaid payments relative to costs
(MACPAC 2023a). Second, we were not able to collect
information on provider contributions to the non-
federal share, which can reduce the net payments that
providers receive. Third, the Medicare cost report data
we used for this analysis does not account for state-
specic dierences in allowable costs or the potential
eects of related-party transactions, which may
inate costs reported on facility-specic cost reports
(Adelberg et al. 2022). Finally, because of the limits of
available data, we were not able to examine payments
relative to costs after the start of the COVID-19
pandemic, which has resulted in increased nursing
facility costs and also increased Medicaid payment
rates in many states.
Using Medicaid Payments
to Improve Quality
Medicaid payment policy has the potential to help
improve quality outcomes and reduce disparities. To
better understand Medicaid’s role, the Commission
has examined how nursing facility stang levels vary
by state, how they relate to Medicaid payment policies,
and which barriers states face in changing payment
policies to promote better outcomes.
FIGURE 2-4. Distribution of Medicaid Base Payment Rates as a Share of Acuity-Adjusted Costs, 2019
5%
10%
19%
25%
22%
12%
7%
0%
5%
10%
15%
20%
25%
30%
Less than 60
percent
60–69
percent
70–79
percent
80–89
percent
90–99
percent
100–109
percent
Share of facilities
Medicaid allowed amount as a share of acuity-adjusted costs
110 percent
or greater
Notes: Base payment rates include resident contributions to their share of costs. Analysis excludes Alaska, Idaho,
and New Hampshire because of unreliable or missing data. Data on resident contributions to their share of costs were
not available for managed care payments in California, Massachusetts, New Jersey, Rhode Island, and Virginia, and
so only fee-for-service spending is included for these states.
Source: Abt Associates, 2022, analysis for MACPAC of the Transformed Medicaid Statistical Information System
(T-MSIS), Medicare cost reports, and the Minimum Data Set.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
41
Report to Congress on Medicaid and CHIP
Background on stang standards
Although stang levels are just one of many measures
of quality, higher stang levels are associated with
a variety of positive health outcomes and have been
a key area of focus for states during the pandemic.
18
Moreover, because stang levels are primarily
aected by how much facilities pay nurses and nurse
aides (often referred to as “direct care sta”), payment
policy can play an important role in helping to address
this issue.
Nursing facilities are staed by a variety of nurses and
nurse aides with dierent levels of training that provide
direct care, including the following:
•
registered nurses (RNs), who have at least a two-
year degree and are responsible for overseeing
residents’ care;
•
licensed practical nurses (LPNs), who have a
one-year degree and typically provide routine
bedside care (such as taking vital signs); and
•
certied nurse aides (CNAs), who have at least
75 hours of training and generally assist residents
with activities of daily living.
19
Currently, CMS requires facilities have licensed nurse
sta (RNs or LPNs) available 24 hours a day, an RN
available eight hours a day, and a full-time director of
nursing. For a 100-bed facility, this standard equates
to 0.3 hours per resident day (HPRD) of licensed
nurse sta.
In 2001, a CMS stang study found that stang levels
of at least 0.75 HPRD of RN stang and 4.1 HPRD of
total stang of nurses and nurse aides (RNs, LPNs,
and CNAs) were associated with optimal quality. The
study did not nd improvement in quality for facilities
that staed above this level (CMS 2001). Although
some stakeholders have argued that 4.1 HPRD is
too high a standard for most nursing facilities, this
standard continues to be endorsed by a variety of
nursing groups (Schnelle et al. 2016, CGNO 2014).
Yet, according to CMS’s Care Compare website,
approximately 72 percent of nursing facilities had
total stang levels below 4.1 HPRD in 2019. CMS is
currently conducting an updated stang study using
more recent data to inform the development of new
stang standards (CMS 2022d).
CMS assigns star ratings to facilities based on how
their stang levels compare to other facilities. In our
analysis, we examined the share of facilities with one-
or two-star stang ratings, which included facilities
with less than 0.5 HPRD of RN care and 3.6 HPRD of
total stang of nurses and nurse aides in 2019.
State variation in stang levels
Overall, nursing facility stang levels vary widely
across states. For example, in three states (Alaska,
Hawaii, and North Dakota) and the District of
Columbia, fewer than 10 percent of freestanding
nursing facilities had one- or two-star stang ratings
on Medicare.gov Care Compare in 2019, while in
three other states (Georgia, Louisiana, and Texas),
more than 70 percent of facilities had these low ratings
(MACPAC 2022b).
We also found wide state variation in the disparities
between facilities that serve a high share of
Medicaid-covered residents and those that do not.
For example, in 2019, the dierence between the
average stang star rating in the quartile of facilities
that served the highest share of Medicaid-covered
residents was more than one star lower than the
quartile of facilities that served the lowest share of
Medicaid-covered residents in seven states (Kansas,
Illinois, North Carolina, Ohio, Pennsylvania, Utah,
and Virginia). In comparison, the dierence between
the quartile of facilities that served the highest and
lowest share of Medicaid-covered residents was less
than 0.1 stars in eight states (Arkansas, Delaware,
Mississippi, North Dakota, New Mexico, Oklahoma,
Oregon, and Wyoming) (MACPAC 2023c).
The wide state variation that we observe suggests
a role for state policy. Although some state variation
may be due to factors other than Medicaid, disparities
by payer mix are likely aected by Medicaid payment
policies. Moreover, the fact that some states have
relatively high stang levels and few disparities by
payer mix shows that ensuring adequate stang to
meet the needs of Medicaid-covered residents is an
achievable goal.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
42
March 2023
Relationship between payment rates
and stang
Prior research has suggested that increasing Medicaid
payment rates has the potential to improve stang.
For example, studies of rate increases in California,
Ohio, and Pennsylvania found that they were
associated with improved stang, particularly for RNs
and LPNs (Hackman 2019, Bowblis and Applebaum
2017, Bishop 2014).
However, in our analysis of 2019 data, we did not nd
a clear relationship between Medicaid payments and
stang levels (Table 2-2). Average base payment
rates were higher for facilities with a ve-star stang
rating (the highest) compared with facilities with a one-
star rating (the lowest). However, after accounting for
dierences in facility costs, the Medicaid payment-to-
cost ratio in facilities with ve-star stang ratings was
7 percentage points lower on average than facilities
with a one-star rating.
Average costs are lower in facilities with lower stang
levels in part because these facilities spend less on
sta, which is a substantial component of nursing facility
costs.
20
After estimating what costs would be if facilities
had similar stang levels, the dierence in Medicaid
margins between facilities with low stang levels and
high stang levels narrows, but Medicaid margins are
still higher for facilities with lower stang ratings.
21
Role of Medicaid payment methods
and state stang requirements
In addition to increasing payment rates, states can
also change other policies to encourage facilities to
spend more of the revenue that they receive on sta.
Two approaches that we studied are (1) changing
Medicaid payment methods to incentivize spending
on direct care sta and (2) requiring that facilities
meet minimum stang standards that exceed federal
requirements. To better understand the potential
eects of these policies, we conducted a literature
review of relevant studies published since 2008.
Medicaid payment methods. Examples of Medicaid
payment methods that may promote higher stang
levels include wage pass-through payments that
require facilities to spend a specied portion of the
TABLE 2-2. Average Medicaid Base Payments per Day and Acuity-Adjusted Costs by Five-Star Stang Rating, 2019
Five-star
stang rating
in the CMS
Nursing Home
Quality Rating
System
Number of
facilities in
analysis
Average
Medicaid base
payment rate
per day
Average cost
of care for
Medicaid-
covered
residents
Average
Medicaid base
payment as a
share of costs
Average
Medicaid base
payment as a
share of costs
if facilities
were staed
with at least 3.6
HPRD
All facilities 12,377 $199.74 $237.85 84% 82%
1 star (lowest) 1,701 183.26 209.36 88 83
2 star 3,451 195.71 227.5 4 86 83
3 star 3,739 201.93 243.94 83 82
4 star 2,572 209.66 257.41 81 81
5 star (highest) 831 230.54 286.93 80 80
Notes: CMS is Centers for Medicare & Medicaid Services. HPRD is hours per resident day. The threshold for a three-star
stang rating in 2019 was 3.6 HPRD. Base payments include resident contributions to their share of costs. Average costs
and payments are weighted by the number of Medicaid days in each facility. Alaska, Idaho, and New Hampshire were
excluded from analysis due to data quality issues. The analysis also excluded facilities with missing payment data and
outlier stang costs.
Source: Abt Associates, 2023, analysis for MACPAC of the Transformed Medicaid Statistical Information System (T-MSIS),
Medicare cost reports, the Minimum Data Set, and Medicare.gov Care Compare.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
43
Report to Congress on Medicaid and CHIP
Medicaid rate on sta wages, cost-based payment
methods that tie payment rates to spending on direct
care sta, and pay for performance (P4P) incentive
payments that tie payments to meeting stang goals.
Overall, there is limited research available about the
eectiveness of these methods. One multivariate
study using 2002 data found that cost-based payment
methods were associated with both higher RN stang
and higher total stang (Harrington et al. 2007). A
review of wage pass-through policies implemented
between 1996 and 2004 found CNA stang levels
increased in the initial years after implementation
but found no statistically signicant eect on RN or
LPN stang (Feng et al. 2010). Finally, one review
of eight Medicaid P4P programs compared with a
nationwide control group found that only one state had
a statistically signicant eect on stang measures
and that the eects on resident-level outcomes were
also limited (Werner et al. 2013).
In response to the COVID-19 pandemic, a number
of states made changes to their Medicaid payment
policies related to stang. As of fall 2021, 12 states
increased payments to direct care workers, 1 state
added a new wage pass-through policy, and 4 states
implemented new payment incentives related to
stang since 2020 (MACPAC 2022a).
22
In 2022,
Illinois implemented a new rate increase for CNAs
that was dierent from other policies that we studied
because it targeted higher wages to more experienced
sta to help improve sta retention (IL HFS 2021).
During our interviews, we heard mixed perspectives
about whether states would be able to continue rate
increases in the long term. Some states nanced
temporary rate increases using grants from the $150
billion Coronavirus Relief Fund authorized by the
CARES Act, which can be used only for expenses
incurred during the public health emergency. As a result,
to continue these rate increases after the public health
emergency using Medicaid authorities, these states
would need to provide additional state matching funds.
Minimum stang standards. States can set their
own minimum stang standards that exceed federal
requirements. According to MACPAC’s review of state
stang policies in 2021, 38 states and the District of
Columbia have state minimum stang standards
that exceed the federal requirements of 0.3 HPRD of
licensed nurse sta for a 100-bed facility. However,
state standards vary widely. For example, 9 states
have standards that are less than 2.0 HPRD, and 11
states and the District of Columbia have standards
that are greater than 3.0 HPRD. In addition, states
vary in whether they have specic requirements
for licensed nurse sta or whether the HPRD
requirements apply to all nurses and nurse aides
(including CNAs) (MACPAC 2022b).
Prior research has found that increases in minimum
stang standards are associated with improvements
in stang, particularly for CNAs. For example, an
analysis of new minimum stang requirements
in California and Ohio found a 5 percent increase
in HPRD overall but a reduction in skill mix (i.e.,
the ratio of RNs to all direct care sta) (Chen and
Grabowski 2014).
23
In another study that examined
the eects by payer mix, facilities that served a higher
share of Medicaid patients reported larger increases
in stang, including RN stang, in response to
increases in minimum stang requirements, resulting
in larger gains in other measures of quality of care
(Bowblis 2011).
Several states recently changed their stang
requirements in response to the COVID-19 pandemic.
In our review of policies enacted as of October 2021,
we identied 10 states that increased minimum stang
standards since 2020. Two states (Maine and New
Jersey) added new minimum wage requirements
specically for direct care sta, a new type of policy
that we did not nd in states before the pandemic
(MACPAC 2022a).
Minimum loss ratio requirements that cap nursing
facility prots and require facilities to spend a
minimum amount on stang are a new policy
approach to promote stang that is being developed
in Massachusetts, New Jersey, and New York. In
2019, median stang costs as share of nursing facility
revenue were 34 percent but varied widely by state.
Facilities in the 90th percentile of Medicaid-covered
days have higher median stang costs as a share of
revenue (36 percent), which suggests that policies to
increase the share of revenue spent on sta may have
less of an eect on facilities that serve a high share of
Medicaid-coverage residents (Bowblis et al. 2023).
In April 2022, CMS requested information from
stakeholders about raising federal minimum stang
standards, and a new stang study intended to inform

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
44
March 2023
these eorts is underway (CMS 2022d). Although the
relationship between higher stang levels and higher
quality care has been well documented, questions
remain about what an appropriate minimum stang
standard should be. Increasing federal standards
would help improve quality, but it would also likely
result in increased costs for facilities, which may
require some state Medicaid programs to make higher
payments (CLA 2022b).
Challenges changing state payment
methods
Despite the potential for Medicaid payment policies
to help improve the quality of nursing facility care,
progress in developing new payment models has
been relatively slow compared with other provider
types. Between 2014, when MACPAC rst reviewed
FFS nursing facility payment policies, and 2019, when
we updated our compendium, few states made any
substantial changes to their nursing facility payment
methods (MACPAC 2019a). During subsequent
interviews with state ocials, nursing facilities, and
other stakeholders in 2020, we learned that limited
state capacity, industry resistance, and a lack of clarity
about value-based payment goals were the primary
barriers to change (MACPAC 2020a).
Limited state capacity. The state ocials we
interviewed described several limits in their capacity to
make changes to their already complicated nancing
systems. Some states faced reductions in stang to
analyze Medicaid nursing facility FFS rates due to
budget cuts or the expansion of MLTSS. In addition,
states reported losing institutional knowledge because
of sta turnover, which was hard to replace because
Medicaid nursing facility payment policy is so complex.
Some states hire external consultants to support their
capacity when making new reforms, but these states
later reported a similar loss of institutional knowledge
when the consultants who initially designed the
payment system were no longer available to evaluate
future changes to payment policies.
Industry resistance to change. The nursing facility
industry associations that we interviewed were
generally active in lobbying state policymakers
against changes in payment methods that could
create winners and losers among nursing facilities
in their states. Instead, these associations primarily
advocated for increased payment rates because of a
view that state payment rates were too low to cover
costs and concerns that states would cut rates further
for budgetary reasons. In states that did get provider
support for payment changes, state ocials noted
the need to engage stakeholders early and provide
sucient time to prepare for any change.
Lack of clarity about value-based payment goals.
Twenty-ve states had P4P incentive payment
programs in nursing facilities in 2019, but the state
ocials that we interviewed in seven states noted
that P4P programs in their states did not appear
to be particularly eective (MACPAC 2019a). For
example, one state’s program was more than two
decades old, and due to secular trends and federal
policies implemented in recent years, most facilities
had already achieved most of the program’s initial
goals related to reducing survey deciencies and
meeting targets for culture change to promote more
person-centered care. States reported challenges
selecting new measures that were tied to quality
outcomes, such as reductions in rehospitalizations or
improvement in long-stay quality measures, because
of a lack of consensus among stakeholders about how
these quality measures should be dened and how the
targets should be set.
In the states we studied, interviewees did not mention
any eorts to incorporate nursing facilities into
alternative payment models that states were using
for their acute care populations, such as accountable
care organizations. Although stakeholders
acknowledged the high rate of avoidable hospital use
among Medicaid-covered nursing facility residents,
they noted that it was dicult to develop alternate
payment models for residents dually eligible for
Medicare and Medicaid because savings from
reducing hospital use for these residents accrue to
Medicare rather than Medicaid.
We also heard a lack of consensus among
stakeholders about whether a value-based measure
of cost savings is appropriate in assessing value for
nursing facility care because of the risk that facilities
may reduce costs by cutting direct care sta needed
to meet residents’ care needs. One state in our study,
New York, switched from a cost-based payment
method to a price-based system in 2017 to provide
more budget predictability for the state, uniformity
across facilities, and administrative eciency.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
45
Report to Congress on Medicaid and CHIP
Although the state still sets prices based on prior
year cost reports, the state has less control than it
would in a cost-based system on how facilities spend
the Medicaid revenue that they receive. Recently,
in response to the COVID-19 pandemic, New York
increased state minimum stang standards and added
a new requirement that facilities spend at least 70
percent of their total revenue on direct care, which
are other tools that states can use to address stang
issues in the absence of cost-based payment systems
(Reiland 2022).
Interaction between
Medicare and Medicaid
Payment Policy
Because Medicare is the second-largest payer for
nursing facility care, many of the payment standards
used by Medicare are also used by Medicaid programs.
In addition, because most Medicaid-covered nursing
facility residents are dually eligible for Medicare and
Medicaid, Medicare payment incentives can aect
the care that Medicaid-covered residents receive.
To understand these interactions in more detail, the
Commission has been monitoring the eects of recent
changes to Medicare’s acuity adjustment system and
the ndings of recent evaluations of eorts to reduce
avoidable hospital use for dually eligible residents.
Acuity adjustment changes
In October 2019, Medicare changed the method it uses
to classify SNF patient acuity from Resource Utilization
Group Version IV (RUG-IV) to the Patient-Driven
Payment Model (PDPM). Under the RUG-IV model,
nursing facilities were incentivized to provide additional
therapy services because the measure of a resident’s
therapy care needs was predominately determined by
the number of minutes of therapy the facility provided.
PDPM corrects these incentives by setting a case-
mix weight based on a resident’s primary diagnosis.
The case-mix weights for PDPM were developed
over several years but used data only for Medicare-
covered nursing facility residents, not Medicaid-covered
residents (Acumen 2018).
As of July 2019, 34 states used RUG-based payment
methodologies for Medicaid-covered residents, and
so Medicare’s change has prompted many states to
reassess their acuity-adjustment methods (MACPAC
2019a). As of October 1, 2023, CMS will no longer
collect information needed to determine RUG case-
mix groups on the Minimum Data Set, which will
make it more dicult for states to continue RUG-
based methods. CMS has provided states the option
of requiring facilities to report additional information
through a state supplement to the Minimum Data Set
until September 30, 2025, if needed to help ease the
transition (CMS 2022c).
Because PDPM was not developed to measure their
acuity or resource use, some components of PDPM
are not a good measure of the care needs for long-
stay residents. The PDPM includes ve components
for measuring the acuity of an SNF patient: nursing,
physical therapy, occupational therapy, speech-
language pathology, and non-therapy ancillary. Although
the nursing component is similar to the previous RUG-
IV model, the therapy components are dierent and
substantially overstate the needs of long-stay residents
(Abt Associates 2020). Because of the challenges
adapting the PDPM therapy components to long-stay
residents and the fact that most therapy services are
not included in the Medicaid nursing facility benet,
CMS issued guidance in 2022 recommending that
states exclude the therapy portions of the PDPM from
their Medicaid payment methods (CMS 2022c).
Another limitation of PDPM is that the underlying data
used to develop the nursing component were based
on a 2007 study of nursing sta time, the latest that
CMS has completed. Some stakeholders have noted
the need for an updated time study that reects current
stang patterns at high-quality facilities and also
considers the unique needs of long-stay Medicaid-
covered residents (Harrington et al. 2020b).
Incentives to reduce avoidable
hospital use
About one-quarter of nursing facility residents are
transferred to hospitals each year, and many of these
hospitalizations could be avoided if residents received
quick diagnoses and treatments in nursing facilities.
Overall, avoidable hospital use for nursing facility

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
46
March 2023
residents is estimated to cost Medicare and Medicaid
more than $1.9 billion a year (RTI 2019).
Unfortunately, misaligned payment incentives between
Medicare and Medicaid do not reward states or
providers for addressing this issue. Because Medicare
is the primary payer for hospital care, the savings from
delivery system reforms typically accrue to Medicare
rather than Medicaid. Moreover, nursing facilities do
not have strong incentives to reduce hospital use for
Medicaid-covered residents because Medicare pays
for a new SNF stay at a higher rate than a Medicaid-
covered stay when a resident is hospitalized and later
returns to a nursing facility.
Policymakers have been exploring a number of
dierent approaches to address these misaligned
incentives, but the results have been mixed so far.
CMS demonstrations. In 2009, CMS launched
the Nursing Home Value-Based Purchasing
Demonstration, which provided incentive payments
to nursing facilities if they reduced avoidable
hospitalizations.
24
However, the nal evaluation found
that there were not major pre- and post-intervention
performance dierences for participating nursing
facilities, and the resulting cost savings were limited
(L&M Policy Research 2013).
25
The CMS Center for Medicare and Medicaid
Innovation (CMMI) has tested two models to reduce
avoidable hospitalization among nursing facility
residents by helping Medicaid-covered long-stay
nursing facility residents access additional skilled
care at a nursing facility instead of being transferred
to the hospital. Although the CMS evaluation of these
initiatives found that the care coordination services
helped to reduce hospital use, the payment incentives
did not meaningfully aect outcomes, and the overall
model did not meet CMMI’s cost-eectiveness test
(RTI 2019).
Managed care plans. During our interviews in
2020, we spoke to representatives from a variety of
Medicaid managed care plans with dierent degrees
of integration with Medicare Advantage plans, but
we heard little about eorts to better coordinate the
Medicare and Medicaid nursing facility benets. In
2022, 49 percent of all Medicare beneciaries were
enrolled in a Medicare Advantage plan, including 4.2
million beneciaries in dual-eligible special needs
plans (D-SNPs) and 98,000 in institutional special
needs plans (I-SNPs), which are limited to long-stay
nursing facility residents (MedPAC 2022c).
The D-SNPs that we spoke with that were aligned
with the Medicaid managed care plans in their states
primarily focused their eorts on helping beneciaries
with long-term care needs access services in the
community rather than the nursing facility. However, the
MLTSS models in these states (Rhode Island and New
York) covered only short-term nursing facility stays, and
so the views of these plans may not reect the range of
strategies being used by other aligned D-SNPs in states
that cover more nursing facility residents through their
MLTSS programs.
Two of the states that we studied (Alabama and
Wisconsin) had a growing presence of I-SNPs that
were exploring new models to avoid hospitalizations
by providing additional care to residents in nursing
facilities. In Alabama, the I-SNP we spoke with had
some facilities that participated in the CMMI model to
reduce avoidable hospitalizations by embedding nurse
practitioners in the facility and was planning to continue
some aspects of the initiative with all participating
facilities in the I-SNP after the demonstration expired.
In Wisconsin, providers identied a similar opportunity
to improve care and believed that they could compete
favorably with other Medicare special needs plans,
so they reported that they were in the early stages of
developing a provider-owned I-SNP.
Payment Principles
Overall, Medicaid can play an important role in helping
to address many of today’s challenges with assuring
access to quality nursing facility care. For Medicaid to
achieve its potential, it is important for policymakers
to design payment policies that advance the statutory
goals of eciency, economy, quality, and access. In
2014, MACPAC developed an overarching provider
payment framework for assessing whether payments
are consistent with these goals, which has guided the
Commission’s development of the following principles
for nursing facility payment policy (MACPAC 2014).

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
47
Report to Congress on Medicaid and CHIP
Payment rates should cover the costs
of economic and ecient providers
Although costs are an imperfect measure of payment
adequacy, the Boren amendment standard that
payments be sucient to cover the costs for ecient
and economically operated facilities is a useful
benchmark for assessing Medicaid nursing facility
payment rates. As discussed earlier in this chapter,
Medicare payment rates are not an appropriate
benchmark for Medicaid because of the dierences
in the acuity of short- and long-stay residents and
the dierent services covered by the Medicaid and
Medicare nursing facility benets. Although the Boren
amendment led to a number of provider lawsuits and
was dicult for CMS to enforce, the underlying payment
principle is sound and is consistent with the current
requirements of Section 1902(a)(30)(A).
In the Commission’s view, it is also important to
consider the costs of ensuring adequate stang and
compliance with other quality and safety standards. As
illustrated in our analyses of Medicaid payments relative
to costs, facilities with lower stang levels have lower
costs on average, but much of these dierences are
explained by the fact that these facilities spend less on
direct care sta overall.
The Commission is also concerned about the potential
for related-party transactions to increase costs above
what would be expected for an economically operated
facility. As a result, states should collect more data on
related parties using consolidated cost reports for the
larger nursing facility chain to better understand the
eects of these transactions.
Finally, when states assess Medicaid payment rates, it
is important to consider all types of Medicaid payments
that nursing facilities receive, including supplemental
payments, which were not available for our analyses. It
is also important to consider how provider contributions
to the non-federal share reduce the net payments that
facilities receive even though these data were also not
readily available.
Payment methods should incentivize
better quality and reductions in
health disparities
The persistent disparities that Medicaid-covered
nursing facility residents face are not consistent with the
statutory requirement that Medicaid beneciaries have
access to care “at least to the extent that such care and
services are available to the general population in the
geographic area” (§1902(a)(30)(A) of the Act). Although
the nursing facility industry overall may continue to
face quality challenges because of factors outside of
Medicaid’s control, Medicaid payment policy can help
ensure that Medicaid-covered residents have access
to the same quality of care available to other nursing
facility residents.
Our work so far has highlighted a number of ways
that states can change payment policies to incentivize
higher stang levels and other quality measures. It
is also important for states to consider other state
policy levers to promote quality and health equity, such
as minimum stang standards and policies to help
Medicaid-covered residents access care in high-quality
facilities. Current evaluations of these policies are
limited, and so more research would help policymakers
identify strategies that are most eective.
States should aim to get the maximum
value for the amount they are spending
Eciency is a measure of whether states are getting
the most value (in terms of quality and access) for the
amount that they are spending. To identify opportunities
to improve eciency, it is helpful to compare payment
rates and quality outcomes across states. States with
the highest payment rates and lowest quality outcomes
likely have the greatest opportunity to improve eciency
by changing payment methods to get better outcomes
for the same level of spending.
Our work on payment rates and stang has illustrated
potential opportunities for states to improve the
eciency of their programs by requiring or incentivizing
facilities to spend more of their Medicaid revenue on
direct care sta. Although our work has identied some
promising practices, more detailed state-level analyses

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
48
March 2023
are needed to identify the best policy approach for
each state.
Similarly, for states with large supplemental payments,
there may be opportunities to improve eciency by
tying more payments to meaningful quality outcomes
or incorporating supplemental payments into base
payment rates that have stronger quality incentives.
Although it can be politically and budgetarily dicult for
states to change supplemental payments because of
how they are nanced, most of the funding for these
payments is provided by the federal government, and
so it is important that the payments are consistent with
statutory payment goals.
Finally, there are several opportunities to improve
the eciency of Medicare and Medicaid payment
for dually eligible patients. The Commission agrees
with MedPAC’s assessment that it is inecient to use
high Medicare payment rates as a tool for osetting
low Medicaid payment rates and encourages
policymakers to set appropriate payment rates for
each program as a rst step toward aligning payment
incentives (MedPAC 2022b). In addition, it will be
important for policymakers to grapple with the fact
that savings from reducing avoidable hospital use
accrue to Medicare rather than Medicaid. Although
prior CMMI demonstrations to correct these
incentives have had mixed results, it is important to
continue testing new models. D-SNPs, I-SNPs, and
Medicaid managed care plans can also play a role in
testing new approaches to better coordinate care for
long-stay nursing facility residents.
Commission
Recommendations
The Commission makes two recommendations on
actions that HHS and CMS can take to improve the
data available to help policymakers evaluate whether
Medicaid nursing facility payments are consistent with
MACPAC’s payment principles and the statutory goals
of eciency, economy, quality, and access.
Recommendation 2.1
To improve transparency of Medicaid spending,
the Secretary of the U.S. Department of Health
and Human Services should direct the Centers for
Medicare & Medicaid Services to collect and report
the following data in a standard format that enables
analysis:
•
facility-level data on all types of Medicaid
payments to nursing facilities, including resident
contributions to their cost of care;
•
data on the sources of non-federal share of
spending necessary to determine net Medicaid
payment at the facility level; and
•
comprehensive data on nursing facility nances
and ownership necessary to compare Medicaid
payments to the costs of care for Medicaid-
covered residents and to examine the eects of
real estate ownership models and related-party
transactions.
Rationale
Transparency of Medicaid payments has been
a long-standing goal of the Commission since
complete data on Medicaid payments to providers are
needed to inform assessment of payment policies.
This recommendation is similar to MACPAC’s prior
recommendation calling for greater transparency
of Medicaid hospital payments (MACPAC 2016).
In 2020, Congress partially implemented this
recommendation by requiring reporting of provider-
level supplemental payment data, but CMS has not
taken any action to date on the other components
of the recommendation related to the transparency
of managed care payments or data on provider
contributions to the non-federal share.
Our review of available federal data on Medicaid
nursing facility payments found several gaps in the
data on base payments, supplemental payments, and
provider contributions to the non-federal share that this
recommendation would help address.
First, although base payment information is available
for many states in the T-MSIS, the base payment data
that are available do not always include information on
resident contributions to their cost of care. Because of
Medicaid post-eligibility treatment of income rules for
long-term care, these contributions are often large and
can substantially aect measures of Medicaid payment
rates. In states with available data, these contributions
accounted for approximately 10 percent of total

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
49
Report to Congress on Medicaid and CHIP
Medicaid base payments to nursing facilities in 2019
(MACPAC 2023a).
To improve the availability of data on allowed base
payment amounts (which are inclusive of resident
contributions to the cost of their care), CMS could
provide states with more guidance on how to report
them in T-MSIS, particularly for managed care
encounters. CMS could also revisit how resident
contributions to their cost of care are reported on UPL
demonstrations (which include provider-level data on
FFS base and supplemental payments). Based on
our review of 2019 UPL demonstrations, most states
reported allowed payment amounts, but six states
reported only amounts paid by the state.
Second, we found that the provider-level supplemental
payment data reported on state UPL demonstrations
were incomplete and often did not match data that
were reported on CMS-64 expenditure reports.
Because supplemental payments are such a large
share of Medicaid spending for nursing facilities in
many states, a lack of complete provider-level data
severely limits our ability to assess total Medicaid
payment rates.
In response to MACPAC’s prior supplemental payment
recommendations, Congress required CMS to develop
a new system for states to submit supplemental
payment data in a standard format beginning October
1, 2021, but these data are not yet available for
MACPAC’s analysis. CMS is implementing this new
reporting requirement through the same nancial
management system that is used for CMS-64
expenditure reports so that supplemental payment
data are reported consistently in these dierent
sources (CMS 2021).
Third, data on provider contributions to the non-federal
share of nursing facility payments are important
because they reduce the net payments that providers
receive. CMS does not currently have a good process
in place to collect provider-level data on sources
of non-federal share, so implementing this part
of the recommendation would likely require more
administrative eort for CMS than the eort required
to improve the completeness of the payment data that
they already collect.
To help stakeholders evaluate Medicaid nursing facility
payments, it is also important to collect comprehensive
data on nursing facility nances necessary to compare
Medicaid payments to the costs of care for Medicaid-
covered residents. Although Medicare cost reports do
provide some information on nursing facility nances
in a standard format, our review of available cost data
found several gaps that could be addressed if CMS
required greater transparency. Some states may
already collect these data on state-specic Medicaid
cost reports, but these data are not collected in a
standard format that enables cross-state analysis.
First, at the facility level, we found that the estimated
costs of care for Medicaid-covered residents was
generally much lower than the costs of care for other
nursing facility residents because of dierences
in resident acuity and dierences in the types of
costs that are paid for by Medicaid and other payers
(MACPAC 2023a).
26
To help stakeholders better
assess the costs of care for Medicaid-covered
residents, CMS could improve the completeness
and availability of the resident acuity information by
payer that it currently collects through the Minimum
Data Set.
27
In addition, CMS could work with states
to further clarify state denitions of allowable costs
and how they relate to Medicare cost reports or other
standard reports of nursing facility costs. Requiring
more standardization of cost information reported
to CMS would not limit a state’s exibility to dene
allowable costs for their Medicaid program, but it
would provide a useful baseline for comparing costs
and payments across states.
Second, more transparency of related-party
transactions would help shed light on practices that
may inate costs above what they would be if a facility
were operated more economically and eciently
(Adelberg et al. 2022). States currently have the
exibility to develop state-specic cost reports that
collect these data, and some states, such as California
and Virginia, have already developed consolidated
cost reports to track these expenditures that could be
a potential model for other states.
28
Third, more transparency of real estate ownership
models is also important for understanding related-
party transactions, especially arrangements in which
the facility real estate is owned by one entity and
then leased to another. Section 6101 of the Patient
Protection and Aordable Care Act (P.L. 111-148, as
amended) included new requirements for nursing
facilities to report additional ownership information

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
50
March 2023
in the Provider Enrollment, Chain, and Ownership
System (PECOS), which was made publicly available
by CMS in 2022 (ASPE 2022a). However, these data
do not include information on the ultimate owners
of some chains, and they do not separately identify
specic types of arrangements that stakeholders
have raised concerns about, such as real-estate
investment trusts and private equity ownership
(Braun et al. 2023, GAO 2023, Braun et al. 2021). In
addition, these data do not identify public or private
ownership, which is important for analyses of Medicaid
supplemental payments to publicly owned nursing
facilities. To address these limitations, CMS could
expand its interpretation of disclosable parties and
other information required to be reported in PECOS. On
February 15, 2023, CMS proposed additional reporting
requirements for nursing facilities owned by private
equity entities and real-estate investment trusts, but this
proposed rule has not yet been nalized (CMS 2023).
Finally, making the payment and cost data that are
collected publicly available in a standard format
will help improve transparency and enable further
analyses by other researchers. To improve the
usability of these data, it would be particularly helpful
for CMS to identify facilities by their CMS certication
numbers (CCNs), if available. CCNs are used to
identify facilities on CMS’s Care Compare website,
which can be used to help compare Medicaid
payments and costs to quality outcomes. CCNs are
also used on Medicare cost reports, which have
additional information on total nursing facility revenue
and margins that may be helpful for understanding
Medicaid payments and costs in the context of
overall nursing facility nances. States currently have
the option to provide the CCN on their state UPL
demonstrations, but our review of these data found
that this eld was often missing.
Implications
Federal spending. This recommendation would
result in increased administrative eort for the federal
government, but these changes are not expected
to result in increased federal spending. Federal
administrative burden could be reduced if eorts to
collect Medicaid nursing facility payment and cost data
are coordinated with existing systems and federal
reporting requirements.
States. Depending on how the recommendation is
implemented, it could aect state administrative eort.
Improving the transparency of base and supplemental
payments can be implemented by improving existing
reporting structures, but collecting and reporting data
on sources of non-federal share would require new
reporting by states.
Enrollees. This policy would not have a direct eect
on enrollees. However, over time greater transparency
of Medicaid payments and costs may lead to changes
in state payment rates and methods that aect the
extent to which Medicaid payments to nursing facilities
are spent on direct care sta and other activities
related to patient care.
Plans. Health plans may need to provide additional
information about managed care payments to nursing
facilities. However, health plans are already required to
submit payment information to states and the federal
government through T-MSIS, and it is unlikely that
this recommendation would substantially increase
administrative burden for health plans.
Providers. This policy would not directly aect
Medicaid payments to providers. However, over
time greater transparency may lead to changes in
state payment rates and methods by allowing more
stakeholders to participate in the rate development
process. This recommendation could also increase
administrative burden for providers to the extent to
which data on provider nances and related-party
transactions are not currently collected by states and
the federal government.
Recommendation 2.2
To help inform assessments of whether Medicaid
nursing facility payments are consistent with statutory
goals of eciency, economy, quality, and access,
the Secretary of the U.S. Department of Health
and Human Services should direct the Centers for
Medicare & Medicaid Services (CMS) to update the
requirement that states conduct regular analyses of
all Medicaid payments relative to the costs of care
for Medicaid-covered nursing facility residents. This
analysis should also include an assessment of how
payments relate to quality outcomes and health
disparities. CMS should provide analytic support

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
51
Report to Congress on Medicaid and CHIP
and technical assistance to help states complete
these analyses, including guidance on how states
can accurately identify the costs of ecient and
economically operated facilities with adequate sta to
meet residents’ care needs. States and CMS should
make facility-level ndings publicly available in a
format that enables analysis.
Rationale
Information on how Medicaid payment rates compare
with costs and quality outcomes is important for
assessing whether payment policies are consistent with
the statutory goals. State-level analyses are needed for
an accurate assessment of these issues due to a lack
of complete data at the federal level and state-specic
dierences in denitions of allowable costs.
Federal regulations currently require states to make
annual ndings that FFS nursing facility rates are
reasonable and adequate to meet the costs of
eciently and economically operated providers (42
CFR 447.253). However, CMS has not enforced
this requirement since the Boren amendment was
repealed, and even when the Boren amendment was
in place, CMS did not provide states with guidance
about how to conduct these studies.
Although the Boren amendment has been repealed,
it is still important for states to conduct rate studies to
inform the public process for developing nursing facility
rates, which is required in Section 1902(a)(13)(A) of
the Act. In addition, Section 1902(a)(30)(A) of the Act
still requires payments to be consistent with eciency,
economy, quality, and access.
To strengthen this requirement, CMS should update
existing regulations to clarify what states should
review and the process for making the results
of these reviews publicly available. Although the
existing regulation describes only assessments
of payment rates, it is also important for states
to consider payment rates in relation to quality
outcomes and health disparities to assess whether
states are maximizing eciency. The measures used
in Medicare.gov Care Compare can be a starting
point for assessing nursing facility quality, but states
should also consider whether to examine additional
measures that are specic to the needs of Medicaid-
covered residents.
When updating existing regulations, CMS can provide
more clarity about what information states should
include in their assessments of nursing facility rates.
Although current regulations require only rate studies
for FFS payments, it would be helpful for states to
also include information on all Medicaid payments
to nursing facilities, including managed care and
supplemental payments. Because most states already
provide managed care payment data in T-MSIS,
including this additional data may not add much more
administrative burden.
CMS can also provide more guidance in regulation
or subregulatory guidance about how states should
compare payments to the costs of eciently and
economically operated facilities. Such guidance could
also include a model approach that states could follow.
Because state denitions of allowable costs dier,
it would be helpful for states to document how the
methods that they use are the same or dierent from
commonly accepted standards, such as those used on
Medicare cost reports. Similarly, because Medicaid-
covered residents often have dierent care needs
than other nursing facility residents, it is important that
states describe their methods for adjusting costs to
account for dierences in resident acuity.
Ultimately, an assessment of whether Medicaid
payments are sucient requires states to make
policy judgments about which facilities are operating
eciently and economically. Although CMS should
continue to allow states to make these policy
judgments, CMS could provide specic standards that
states can use as a starting point. In addition, it would
help improve transparency if states made the criteria
that they use to assess payment rates available to all
interested stakeholders.
Implications
Federal spending. This recommendation could
result in increased administrative eort for the federal
government, but these changes are not expected to
result in increased federal spending.
States. This recommendation is likely to increase
administrative eort for states that are not currently
conducting regular assessments of nursing facility
rates. However, states should be able to use the
information that they already collect from state cost
reports and state payment systems to conduct these

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
52
March 2023
analyses. Moreover, the administrative eort could
be reduced if CMS provided increased technical
assistance and analytic support to states.
Enrollees. This policy would not have a direct
eect on enrollees. However, over time increased
transparency about how payment rates relate to
quality and access goals may result in changes in
state nursing facility payment policies to better achieve
these goals.
Plans. Depending on how this recommendation
is implemented, health plans may need to provide
additional information about managed care payments
to nursing facilities. However, health plans are already
required to submit payment information to states and
the federal government through T-MSIS, and it is
unlikely that this recommendation would substantially
increase administrative burden for health plans.
Providers. This policy would not directly aect
Medicaid payments to providers. However, over
time greater transparency may lead to changes in
state payment rates and methods by allowing more
stakeholders to participate in the rate development
process. Because most nursing facilities already
submit cost report information to states, it is unlikely
that this recommendation would substantially increase
administrative burden for providers.
Endnotes
1
Although the term “nursing home” is commonly used
by stakeholders, we use the term “nursing facility” in this
chapter because it is the term used to dene these services
in the Medicaid statute. Historically, the Medicaid statute
used the terms “skilled nursing facility” to refer to short-
term, post-acute care and “intermediate care facility” to refer
to long-term services and supports provided by nursing
facilities. The Nursing Home Reform Act of 1987, which was
part of the Omnibus Budget Reconciliation Act of 1987 (P.L.
100-203), changed the statute to refer to both types of care
as “nursing facility care” and to require common standards
regardless of resident length of stay.
2
The number of individuals served by nursing facilities
throughout the year is greater than the number of individuals
served at a point in time. For example, in 2020, about 1.2
million Medicare fee-for-service beneciaries had at least
one nursing facility stay during the year, while only 247,500
in Medicare beneciaries were included in our analyses
of individuals receiving care in nursing facilities as of
September 30, 2019 (MedPAC 2022b, Abt Associates 2020).
3
Other institutional LTSS providers include intermediate
care facilities for individuals with intellectual disabilities and
institutions for mental diseases, which are outside the scope
of this chapter.
4
As of 2017, approximately 7 percent of individuals age 50
and older had long-term care insurance (LIMRA 2017).
5
The Patient Protection and Aordable Care Act (P.L. 111-
148, as amended) provided states with the option to expand
Medicaid coverage to non-elderly adults with incomes
below 138 percent of the federal poverty level. However,
most nursing facility residents (89 percent) are older than
age 65 and thus do not qualify for this eligibility group (Abt
Associates 2020).
6
In 2015, the median annual private-pay charge for a
semiprivate nursing facility room was $80,300 (Genworth
Financial, Inc. 2015).
7
For example, if a Medicaid-covered resident has a spouse
residing in the community, the resident can protect a greater
portion of their income from post-eligibility treatment of
income rules.
8
This analysis was limited to nursing facilities that are
certied by Medicare and excluded nursing facilities that are
only certied by Medicaid.
9
Some states require that nursing facilities admit residents
regardless of payer. However, in practice, Medicaid residents
in these states often still have diculty nding a nursing
facility bed, as evidenced by secret shopper studies showing
that nursing facilities respond more favorably to hypothetical
private pay applicants (Kowalczyk and Arsenault 2020).
10
States must conduct in-person surveys of facilities at
least once a year, according to standards set by CMS.
These surveys are unannounced and include assessments
of a variety of issues that aect patient safety and quality
of life, such as infection control, medication management,
and protection from physical and mental abuse. Medicaid
nances state survey activities at a 75 percent federal
medical assistance percentage (FMAP) (§1903(a)(2)(D) of
the Act).

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
53
Report to Congress on Medicaid and CHIP
11
In 1968, the Social Security Amendments of 1967 (P.L.
90-248) also added the requirement that states “assure
that payments are not in excess of reasonable charges
consistent with eciency, economy, and quality of care.”
12
Wilder v. Virginia Hospital Association, 88-2043, (SCT
June 14, 1990).
13
The Medicaid payment principles of eciency, economy,
and quality in Section 1902(a)(30)(A) of the Act were added
by the Social Security Amendments of 1967, and the
standard that payments assure access to care similar to
what is available to the general population was added by the
Omnibus Budget Reconciliation Act of 1989 (P.L. 101-239).
14
Armstrong v. Exceptional Child Center, Inc., et al., 14-15,
(SCT July 7, 2014).
15
Because Medicare’s SNF payment covers therapy costs
and Medicaid nursing facility payments typically do not,
CMS requires states to adjust Medicare payment rates used
in UPL calculation to exclude non-covered services (CMS
2022c).
16
In 14 of the 23 states reporting supplemental payments
on CMS-64 expenditure reports, the reported spending on
UPL demonstrations was similar, while in 2 states spending
reported did not match. In several states, supplemental
payments were recorded on CMS-64 expenditure reports
but not on UPL demonstrations (three states) or no UPL
demonstration was submitted (four states). Nine states
reported supplemental payments on UPL demonstrations
that are not listed as supplemental payments on CMS-64
expenditure reports.
17
Provider taxes for which 75 percent or more of taxpayers
in a class receive 75 percent or more of their total tax costs
back from Medicaid are generally limited to 6 percent of
providers’ net patient revenue. More information about
provider taxes is available in MACPAC’s issue brief Health
Care-Related Taxes in Medicaid (MACPAC 2021b).
18
The relationship between higher stang levels and better
quality care has been well documented. For example,
a recent systematic review found that higher registered
nurse (RN) stang levels were associated with fewer
pressure ulcers, decreased urinary tract infections, reduced
emergency department use, fewer hospitalizations, and
decreased mortality (Delleeld 2015). Although RN stang
has the strongest link to quality, higher levels of total direct
care stang (i.e., RNs, licensed practical nurses, and
certied nurse aides) are also associated with improved
outcomes (Harrington et al. 2020b).
19
During the COVID-19 pandemic, CMS has allowed states
to waive or reduce training requirements for CNAs. Other
non-nursing sta, such as therapists, social workers, and
activities sta, also provide direct care, but they are not
included in measures of nurse stang levels.
20
In 2019, wages for sta accounted for 51 percent of costs
for nursing care at nursing facilities (MACPAC 2023a).
21
In our analysis, we estimated what costs would be if
facilities were staed at 3.6 HPRD, which was the threshold
for a three-star stang rating in 2019.
22
We also identied four states with pending legislation to
increase minimum stang requirements.
23
Specically, this study reviewed California’s increase
of minimum standards from 3.0 to 3.2 HPRD in 2000 and
Ohio’s increase of minimum stang standards from 1.6 to
2.75 HPRD in 2002 (Chen and Grabowski 2014).
24
In the Nursing Home Value-Based Payment
Demonstration, nursing home performance was assessed
using measures from four domains: nurse stang (30
percent of performance weight), quality outcomes (20
percent), survey deciencies (20 percent), and potentially
avoidable hospitalization rates (30 percent).
25
During the three years of the Nursing Home Value-Based
Payment Demonstration, savings were realized in Arizona
(year one) and Wisconsin (years one and two); no savings
were generated in Arizona (years two and three), New York
(years one through three), and Wisconsin (year three) (L&M
Policy Research 2013).
26
For example, in 2019, the average acuity-adjusted costs
per day for Medicaid-covered nursing facility residents were
$239.35, compared with average costs of $293.36 per day
for all nursing facility residents (MACPAC 2023a).
27
The Minimum Data Set does not currently identify
payer source explicitly, but it does include information on
a resident’s Medicare and Medicaid enrollee identication
number that can be used to infer the payer source (Abt
Associates 2020).
28
Calif. Health and Safety Code § 128734.1 (2021) and
Virginia Code tit. 12, § 30-70-450 (2000).

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
54
March 2023
References
Abt Associates. 2022. Analyses for MACPAC of Medicare
cost report data, Medicare.gov Care Compare, the
Transformed Medicaid Statistical Information System
(T-MSIS), and state upper payment limit demonstrations.
Abt Associates. 2020. Comparison of nursing facility acuity
adjustment methods. Washington, DC: MACPAC. https://
www.macpac.gov/publication/comparison-of-nursing-facility-
acuity-adjustment-methods/.
Acumen, LLC (Acumen). 2018. Skilled nursing facilities
patient-driven payment model technical report. Baltimore,
MD: CMS. https://www.cms.gov/Medicare/Medicare-Fee-for-
Service-Payment/SNFPPS/Downloads/PDPM_Technical_
Report_508.pdf.
Adelberg, M., A. Dobosenski, and E. Prendergast. 2022.
Report on data transparency related to skilled nursing
facilities. Minneapolis, MN: Faegre Drinker. https://www.
faegredrinker.com/en/services/experience/2022/1/report-on-
data-transparency-related-to-skilled-nursing-facilities.
Assistant Secretary for Planning and Evaluation (ASPE),
U.S. Department of Health and Human Services. 2022a.
Ownership of skilled nursing facilities: An analysis of
newly-released federal data. Washington, DC: ASPE.
https://aspe.hhs.gov/sites/default/les/documents/
fd593ae970848e30aa5496c00ba43d5c/aspe-data-brief-
ownership-snfs.pdf.
Assistant Secretary for Planning and Evaluation (ASPE),
U.S. Department of Health and Human Services. 2022b.
Changes of ownership of hospital and skilled nursing
facilities: An analysis of newly-released CMS data.
Washington, DC: ASPE. https://aspe.hhs.gov/sites/default/
les/documents/be6f3366294bd30a08a8ae90c84f3894/
aspe-datapoint-change-ownership-pecos.pdf.
Assistant Secretary for Planning and Evaluation (ASPE),
U.S. Department of Health and Human Services. 2013.
Medicaid-Financed Institutional Services: Characteristics
of nursing home and IF/IDD residents and their patterns of
care. Washington, DC: ASPE. https://aspe.hhs.gov/reports/
medicaid-nanced-institutional-services-characteristics-
nursing-home-icid-residents-their-1.
Bishop, C.E. 2014. High-performance workplace practices
in nursing homes: An economic perspective. Gerontologist
54, supplement 1: S46–S52. https://pubmed.ncbi.nlm.nih.
gov/24443605/.
Bowblis, J.R., C. Brunt, H. Xu, et al. 2023. Understanding
nursing home spending and sta levels in the context of
recent nursing sta recommendations. Health Aairs 42, no.
2: 197–206. https://www.healthaairs.org/doi/full/10.1377/
hltha.2022.00692.
Bowblis, J.R., and R. Applebaum. 2017. How does Medicaid
reimbursement impact nursing home quality? The eects
of small anticipatory changes. Health Services Research
52, no. 5: 1729–1748. https://pubmed.ncbi.nlm.nih.
gov/27581748/.
Bowblis, J.R. 2011. Stang ratios and quality: An analysis
of minimum direct care stang requirements for nursing
homes. Health Services Research 46, no. 5: 2495–1516.
https://pubmed.ncbi.nlm.nih.gov/21609329/.
Braun, R.T., D. Williams, D. Stevenson, et al. 2023. The role
of real estate investment trusts in stang US nursing homes.
Health Aairs 42, no. 2: 207–216. https://www.healthaairs.
org/doi/pdf/10.1377/hltha.2022.00278.
Braun, R.T., H. Jung, L.P. Casalino, et al. 2021. Association
of private equity investment in U.S. nursing homes with the
quality and cost of care for long-stay residents. JAMA Health
Forum 2, no. 11: 1–13. https://jamanetwork.com/journals/
jama-health-forum/fullarticle/2786442.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2023. Medicare
and Medicaid programs: Disclosures of ownership and
additional disclosable parties information for skilled nursing
facilities and nursing facilities. Proposed rule. Federal
Register 88, no. 31 (February 15): 9820–9830. https://www.
federalregister.gov/public-inspection/2023-02993/medicare-
and-medicaid-programs-disclosures-of-ownership-and-
additional-disclosable-parties.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2022a. CMS
enhances nursing home rating system with stang and
turnover data. July 27, 2022, press release. Baltimore, MD:
CMS. https://www.cms.gov/newsroom/press-releases/
cms-enhances-nursing-home-rating-system-stang-and-
turnover-data.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2022b.
COVID-19 nursing home data. Baltimore, MD: CMS. https://
data.cms.gov/covid-19/covid-19-nursing-home-data.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
55
Report to Congress on Medicaid and CHIP
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2022c. Letter
from Daniel Tsai to state Medicaid directors regarding
“Guidance on nursing facility state plan payment and
upper payment limit approaches in Medicaid relying on the
Medicare patient-driven payment model.” September 21,
2022. https://www.medicaid.gov/federal-policy-guidance/
downloads/smd22005.pdf.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2022d. Medicare
program; Prospective payment system and consolidated
billing for skilled nursing facilities; Updates to the quality
reporting program and value-based purchasing program for
federal scal year 2023; Request for information on revising
the requirements for long-term care facilities to establish
mandatory minimum stang levels. Proposed rule. Federal
Register 87, no. 73 (April 15): 22720–22809. https://www.
federalregister.gov/documents/2022/04/15/2022-07906/
medicare-program-prospective-payment-system-and-
consolidated-billing-for-skilled-nursing-facilities.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2021. Letter
to state Medicaid directors regarding new supplemental
payment reporting and Medicaid disproportionate share
hospital requirements under the Consolidated Appropriations
Act, 2021. December 10, 2021. https://www.medicaid.gov/
federal-policy-guidance/downloads/smd21006.pdf.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2019. CMS
improving nursing home compare in April 2019. March 5,
2019, press release. Baltimore, MD: CMS. https://www.cms.
gov/newsroom/press-releases/cms-improving-nursing-home-
compare-april-2019.
Centers for Medicare & Medicaid Services (CMS), U.S.
Department of Health and Human Services. 2001.
Appropriateness of minimum nurse stang ratios in
nursing homes: Phase II nal report. Baltimore, MD: CMS.
http://www.phinational.org/wp-content/uploads/legacy/
clearinghouse/PhaseIIVolumeIofIII.pdf.
Chen, M., and D. Grabowski. 2014. Intended and unintended
consequences of minimum stang standards for nursing
homes. American Journal of Health Economics 24, 7:
822–839. https://pubmed.ncbi.nlm.nih.gov/24850410/.
CliftonLarsonAllen (CLA). 2023. Factsheet: State of the
nursing home sector. Washington, DC: American Health
Care Association/National Center for Assisted Living. https://
www.ahcancal.org/News-and-Communications/Fact-Sheets/
FactSheets/State-of-Nursing-Homes-Infographic.pdf.
CliftonLarsonAllen (CLA). 2022a. State of skilled nursing
facility (SNF) industry. Washington, DC: American Health
Care Association/National Center for Assisted Living.
https://publish.ahcancal.org/News-and-Communications/
Fact-Sheets/FactSheets/2022%20State%20of%20the%20
SNF%20Industry%20Report.pdf.
CliftonLarsonAllen (CLA). 2022b. Stang mandate analysis:
In-depth analysis on minimum stang levels. Washington,
DC: American Health Care Association/National Center
for Assisted Living. https://www.ahcancal.org/News-and-
Communications/Fact-Sheets/FactSheets/CLA-Stang-
Mandate-Analysis-Dec2022.pdf.
Coalition of Geriatric Nursing Organizations (CGNO). 2014.
Nursing stang requirements to meet the demands of
today’s long term care consumer: Recommendations from
the Coalition of Geriatric Nursing Organizations (CGNO).
Silver Spring, MD: American Nursing Association. https://
www.nursingworld.org/practice-policy/nursing-excellence/
ocial-position-statements/id/nursing-stang-requirements-
to-meet-the-demands-of-todays-long-term-care-consumer/.
Committee on Finance, U.S. Senate. 1972. Report of
the Committee on Finance, United States Senate to
accompany H.R. 1 to amend the Social Security Act,
and for other purposes (together with additional views).
Senate Report 92–1230. https://archive.org/details/
socialsecurityam00unit_10/page/59/mode/1up?ref=ol&_
autoReadAloud=show&view=theater&q=249.
Delleeld, M.E., N.G. Castle, K.S. McGilton, and K.
Spilsbury. 2015. The relationship between registered
nurses and nursing home quality: An integrative review
(2008–2014). Nursing Economics 33, no. 2: 95–108. https://
pubmed.ncbi.nlm.nih.gov/26281280/.
Dobson, C., A. Mosey, R. Plasencia, et al. 2021.
Demonstrating the value of Medicaid MLTSS programs.
Washington, DC: ADvancing States. http://www.
advancingstates.org/sites/nasuad/les/2021%20-%20
Demonstrating%20the%20Value%20of%20MLTSS.pdf.
Feng, Z., Y.S. Lee, S. Kuo, et al. 2010. Do Medicaid wage
pass-through payments increase nursing home stang?
Health Services Research 45, no. 3: 728–747. https://www.
ncbi.nlm.nih.gov/pmc/articles/PMC2875757/.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
56
March 2023
Flinn, B. 2020. Nursing home closures and trends: June
2015–June 2019. Washington, DC: Leading Age. https://
leadingage.org/wp-content/uploads/drupal/Nursing%20
Home%20Closures%20and%20Trends%202020.pdf.
Galewitz, P. 2017. Chasing millions in Medicaid dollars,
hospitals buy up nursing homes. October 13, 2017.
Washington Post. https://www.washingtonpost.com/
business/economy/chasing-millions-in-medicaid-dollars-
hospitals-buy-up-nursing-homes/2017/10/13/2be823ca-
a943-11e7-92d1-58c702d2d975_story.html.
Genworth Financial, Inc. 2015. Cost of care survey: Home
care providers, adult day health care facilities, assisted
living facilities and nursing homes. Richmond, VA: Genworth
Financial, Inc. https://secure.wpsic.com/sales-materials/les/
supplemental-long-term-cost-of-care-report.pdf.
Giord, K., E. Ellis, A. Lashbrook, et al. 2019. A view from
the states: Key Medicaid policy changes: Results from a
50-state Medicaid budget survey for state scal years 2019
and 2020. San Francisco, CA: Kaiser Family Foundation.
https://www.k.org/report-section/a-view-from-the-states-key-
medicaid-policy-changes-provider-rates-and-taxes/.
Gupta, A., S.T. Howell, C. Yannelis, and A. Gupta. 2021.
Does private equity investment in healthcare benet
patients? Evidence from nursing homes. National Bureau of
Economic Research, working paper 28474. https://www.nber.
org/system/les/working_papers/w28474/w28474.pdf.
Hackman, M.B. 2019. Incentivizing better quality of care:
The role of Medicaid and competition in the nursing home
industry. American Economic Review 109, no. 5: 1684–1716.
https://www.aeaweb.org/articles?id=10.1257/aer.20151057.
Harrington, C., L. Ross, S. Chapman, et al. 2020a.
Nurse stang and coronavirus infections in California
nursing homes. Policy, Politics, & Nursing Practice
21, no. 3: 174–186. https://journals.sagepub.com/doi/
full/10.1177/1527154420938707.
Harrington, C., M.E. Delleeld, E. Halifax, et al. 2020b.
Appropriate nurse stang levels for U.S. nursing homes.
Health Services Insights 13: 1–14. https://www.ncbi.nlm.nih.
gov/pmc/articles/PMC7328494/.
Harrington, C., J.H. Swan, and H. Carrillo. 2007. Nurse
stang levels and Medicaid reimbursement rates in nursing
facilities. Health Services Research 42, no. 3: 1105–1129.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1955251/.
Illinois Department of Healthcare and Family Services (IL
HFS). 2021. A comprehensive review of nursing home
payment with recommendations for reform. Springeld, IL:
IL HFS. https://www2.illinois.gov/hfs/NursingHomeUpdate/
Pages/default.aspx.
Kaiser Family Foundation (KFF). 2020. E-mail to MACPAC
sta, April 17, 2020.
Kowalczyk, L. and M. Arsenault. 2020. Potential Medicaid
discrimination at Massachusetts nursing homes.
Boston Globe, September 28. https://www.bostonglobe.
com/2020/09/28/metro/spotlight-team-probe-potential-
medicaid-discrimination-massachusetts-nursing-homes/.
Lewis, E., S. Eiken, A. Amos, and P. Saucier. 2018. The
growth of managed long-term services and supports
programs: 2017 update. Baltimore, MD: Centers for
Medicare & Medicaid Services. https://www.medicaid.gov/
media/3406.
Li, Y., H. Temkin-Greener, S. Gao, and X. Cai. 2020.
COVID-19 infections and deaths among Connecticut nursing
home residents: Facility correlates. American Journal of
Geriatric Psychiatry 68, no. 9: 1899–1906. https://pubmed.
ncbi.nlm.nih.gov/32557542/.
Life Insurance Marketing and Research Association (LIMRA).
2017. Combination products giving life back to long-term
care market. November 9, 2017, press release. Windsor,
CT: LIMRA. https://www.limra.com/en/newsroom/industry-
trends/2017/combination-products-giving-life-back-to-long-
term-care-market/.
L&M Policy Research. 2013. Evaluation of the nursing
home value-based purchasing demonstration. Contract no.
HHSM-500-2006-00009I/TO#7. Washington, DC: Centers for
Medicare & Medicaid Services. https://innovation.cms.gov/
les/reports/nursinghomevbp_evalreport.pdf.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2023a. Estimates of Medicaid nursing facility
payments relative to costs. Washington, DC: MACPAC.
https://www.macpac.gov/wp-content/uploads/2023/01/
Estimates-of-Medicaid-Nursing-Facility-Payments-Relative-
to-Costs-1-6-23.pdf.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2023b. Analysis of state upper payment limit
demonstrations.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
57
Report to Congress on Medicaid and CHIP
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2023c. Analysis of Medicare.gov Care Compare.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2022a. Compendium: State policies related to
nursing facility stang. Washington, DC: MACPAC. https://
www.macpac.gov/publication/state-policies-related-to-
nursing-facility-stang/.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2022b. State policy levers to address nursing
facility stang issues. Washington, DC: MACPAC. https://
www.macpac.gov/wp-content/uploads/2022/03/State-Policy-
Levers-to-Address-Nursing-Facility-Stang-Issues.pdf.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2021a. COVID relief funding for Medicaid
providers. Washington, DC: MACPAC. https://www.macpac.
gov/publication/covid-relief-funding-for-medicaid-providers/.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2021b. Health care-related taxes in Medicaid.
Washington, DC: MACPAC. https://www.macpac.gov/
publication/health-care-related-taxes-in-medicaid/.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2020a. Themes from interviews on the
development of nursing facility payment methods.
Washington, DC: MACPAC. https://www.macpac.gov/
publication/themes-from-interviews-on-the-development-of-
nursing-facility-payment-methods/.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2020b. Exhibit 25: Medicaid supplemental
payments to non-hospital providers by state, FY 2019
(millions). In MACStats: Medicaid and CHIP Databook.
December 2020. Washington, DC: MACPAC. https://www.
macpac.gov/wp-content/uploads/2020/12/MACStats-
Medicaid-and-CHIP-Data-Book-December-2020.pdf.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2019a. States’ Medicaid fee-for-service nursing
facility payment policies. Washington, DC: MACPAC. https://
www.macpac.gov/publication/nursing-facility-payment-
policies/.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2019b. Twenty years later: Implications of
Olmstead v. L.C. on Medicaid’s role in providing long-term
services and supports. Washington, DC: MACPAC. https://
www.macpac.gov/wp-content/uploads/2019/07/Twenty-
Years-Later-Implications-of-Olmstead-on-Medicaids-Role-in-
LTSS.pdf.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2016. Report to Congress on Medicaid
Disproportionate Share Hospital Payments. Washington,
DC: MACPAC. https://www.macpac.gov/publication/report-
to-congress-on-medicaid-disproportionate-share-hospital-
payments/.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2014. Framework for evaluating Medicaid
provider payment policy. Washington, DC: MACPAC. https://
www.macpac.gov/wp-content/uploads/2014/10/Framework-
for-Evaluating-Medicaid-Provider-Payment-Policy-
October-2014.pdf.
Medicaid and CHIP Payment and Access Commission
(MACPAC). 2013. Chapter 4: Medicaid coverage of
premiums and cost sharing for low-income Medicare
beneciaries. In Report to the Congress on Medicaid and
CHIP. Washington, DC: MACPAC. https://www.macpac.
gov/wp-content/uploads/2013/03/Medicaid-Coverage-of-
Premiums-and-Cost-Sharing-for-Low-Income-Medicare-
Beneciaries.pdf.
Medicare Payment Advisory Commission (MedPAC). 2022a.
Chart 8-3: Use of skilled nursing facilities and home health
agencies after an inpatient hospital stay shifted in 2020.
In Data Book: Health Care Spending and the Medicare
Program. June 2022. Washington, DC: MedPAC. https://
www.medpac.gov/wp-content/uploads/2022/07/July2022_
MedPAC_DataBook_Sec8_SEC.pdf.
Medicare Payment Advisory Commission (MedPAC). 2022b.
Chapter 7: Skilled nursing facility services: Assessing
payment adequacy and updating payments. In Report
to the Congress: Medicare payment policy. Washington,
DC: MedPAC. https://www.medpac.gov/wp-content/
uploads/2022/03/Mar22_MedPAC_ReportToCongress_Ch7_
SEC.pdf.
Medicare Payment Advisory Commission (MedPAC). 2022c.
Section 9: Medicare Advantage. In Data Book: Health
Care Spending and the Medicare Program. June 2022.
Washington, DC: MedPAC. https://www.medpac.gov/wp-
content/uploads/2022/07/July2022_MedPAC_DataBook_
Sec9_SEC.pdf.
Medicare Payment Advisory Commission (MedPAC). 2021.
E-mail to MACPAC, August 21.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
58
March 2023
Murray, C., A. Tourtellotte, D. Lipson, and A. Wysocki.
2021. Medicaid long term services and supports
annual expenditures report: Federal scal year
2019. Report to CMS, contract no. HHSM-500-2014-
00034I/75FCMC19F0007. Chicago, IL: Mathematica. https://
www.medicaid.gov/medicaid/long-term-services-supports/
downloads/ltssexpenditures2019.pdf.
Musumeci, M., P. Chidambaram, and M. Watts. 2019.
Medicaid nancial eligibility for seniors and people with
disabilities: Findings from a 50-state survey. Washington,
DC: Kaiser Family Foundation. https://www.k.org/report-
section/medicaid-nancial-eligibility-for-seniors-and-people-
with-disabilities-ndings-from-a-50-state-survey-issue-brief.
National Academies of Sciences, Engineering, and Medicine
(National Academies). 2022. The national imperative to
improve nursing home quality. Washington, DC: National
Academies Press. https://nap.nationalacademies.org/
catalog/26526/the-national-imperative-to-improve-nursing-
home-quality-honoring-our.
Nolen, L.T., A.L. Beckman, and E. Sandoe. 2020. How
foundational moments in Medicaid’s history reinforced rather
than eliminated racial health disparities. Health Aairs Blog,
September 1. https://www.healthaairs.org/do/10.1377/
hblog20200828.661111/full/.
Oce of the Actuary (OACT), Centers for Medicare &
Medicaid Services. 2022. National health expenditures
by type of service and source of funds: CY 1960–
2020. Baltimore, MD: OACT. https://www.cms.gov/
Research-Statistics-Data-and-Systems/Statistics-
Trends-and-Reports/NationalHealthExpendData/
NationalHealthAccountsHistorical.
Paul, D.P., T. Godby, S. Saldanha, et al. 2016. Quality
of care and protability in not-for-prot versus for-prot
nursing homes. Proceedings of the Business and Health
Administration Association annual conference, May 3, 2016,
Chicago, IL. https://mds.marshall.edu/mgmt_faculty/155/.
Reiland, J. 2022. Nursing home stang minimum law takes
eect in New York. Skilled Nursing News. April 3. https://
skillednursingnews.com/2022/04/nursing-home-stang-
minimum-law-takes-eect-in-new-york/.
RTI International (RTI). 2019. Evaluation of the initiative to
reduce avoidable hospitalizations among nursing facility
residents—payment reform. Baltimore, MD: Centers for
Medicare & Medicaid Services. https://www.cms.gov/
Medicare-Medicaid-Coordination/Medicare-and-Medicaid-
Coordination/Medicare-Medicaid-Coordination-Oce/
InitiativetoReduceAvoidableHospitalizations/Evaluation-.
Schnelle, J.F., L.D. Schroyer, A.A. Saraf, and S.F. Simmons.
2016. Determining nurse aide stang requirements to
provide care based on resident workload: A discrete event
simulation model. JAMDA 17, no. 11: 970–977. https://www.
promodel.com/media/pdf/Determine%20Nurse%20Aide%20
Stang%20Rqt%20with%20MedModel.pdf.
Sharma, H., R. Bin Abdul Baten, F. Ullrich, et al. 2021.
Trends in nursing home closures in nonmetropolitan and
metropolitan counties in the United States, 2008–2018. Issue
brief no. 2021-1. Iowa City, IA: RUPRI. https://rupri.public-
health.uiowa.edu/publications/policybriefs/2021/Rural%20
NH%20Closure.pdf.
Sharma, H., M.C. Perraillon, R.M. Werner, et al. 2020.
Medicaid and nursing home choice: Why do duals end up in
low-quality facilities? Journal of Applied Gerontology 76, no.
6: 758–783. https://pubmed.ncbi.nlm.nih.gov/30957619/.
U.S. Government Accountability Oce (GAO). 2023. Nursing
homes: CMS should make ownership information more
transparent for consumers. Report no. GAO-23-104813.
Washington, DC: GAO. https://www.gao.gov/products/gao-
23-104813.
U.S. Government Accountability Oce (GAO). 2022.
COVID-19 in nursing homes: Outbreak duration averaged 4
weeks and was strongly associated with community spread.
Report no. GAO-23-104291. Washington, DC: GAO. https://
www.gao.gov/products/gao-23-104291.
Waters, R. 2021. The big idea behind a new model of small
nursing homes. Health Aairs 40, no. 3: 378–383. https://
www.healthaairs.org/doi/10.1377/hltha.2021.00081.
Weech-Maldonado, R., J. Lord, G. Davlyatov, et al. 2021.
High-minority nursing homes disproportionately aected
by COVID-19 deaths. Frontiers in Public Health 22,
no. 9: 1–8. https://www.frontiersin.org/articles/10.3389/
fpubh.2021.606364/full.

Chapter 2: Principles for Assessing Medicaid Nursing Facility Payment Policies
59
Report to Congress on Medicaid and CHIP
Wenzlow, A.T., R. Schmitz, and J. Gurvey. 2008. Medicaid-
nanced nursing home services: Characteristics of people
served and their patterns of care, 2001–2002. Report to
ASPE, contract no. HHS-100-97-0013. Washington, DC:
ASPE. https://aspe.hhs.gov/reports/medicaid-nanced-
nursing-home-services-characteristics-people-served-their-
patterns-care-2001-2002.
Werner, R.M., and N.B. Coe. 2021. Nursing home stang
levels did not change signicantly during COVID-19. Health
Aairs 40, no. 5: 795–801. https://www.healthaairs.org/
doi/10.1377/hltha.2020.02351.
Werner, R.M., R.T. Konetzka, and D. Polsky. 2013. The eect
of P4P in nursing homes: Evidence from state Medicaid
programs. Health Services Research 48, no. 4: 1393–1414.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3657568/pdf/
hesr0048-1393.pdf.
Wiener, J.M., and D.G. Stevenson. 1998. Repeal of the
“Boren amendment”: Implications for quality of care in
nursing homes. Series A, No. A-30. Washington, DC:
Urban Institute. https://www.urban.org/sites/default/les/
publication/70621/308020-Repeal-of-the-Boren-Amendment.
PDF.
Zuckerman, R.B., S. Wu, L.M. Chen, et al. 2018. The
ve-star skilled nursing facility rating system and care of
disadvantaged populations. Journal of American Geriatric
Society 67, no. 1: 108–114. https://deepblue.lib.umich.edu/
handle/2027.42/146941.

Commission Vote on Recommendations
60
March 2023
Commission Vote on Recommendations
In its authorizing language in the Social Security Act (42 USC 1396), Congress requires MACPAC to review
Medicaid and CHIP program policies and make recommendations related to those policies to Congress, the
Secretary of the U.S. Department of Health and Human Services, and the states in its reports to Congress, which
are due by March 15 and June 15 of each year. Each Commissioner must vote on each recommendation, and the
votes for each recommendation must be published in the reports. The recommendations included in this report,
and the corresponding voting record below, fulll this mandate.
Per the Commission’s policies regarding conicts of interest, the Commission’s conict of interest committee
convened prior to the vote to review and discuss whether any conicts existed relevant to the recommendations.
It determined that, under the particularly, directly, predictably, and signicantly standard that governs its
deliberations, no Commissioner has an interest that presents a potential or actual conict of interest.
The Commission voted on these recommendations on January 27, 2023.
_________________________________________________________________________________________
Nursing Facility Provider Payment Principles
2.1 To improve transparency of Medicaid spending, the Secretary of the U.S. Department of Health and Human
Services should direct the Centers for Medicare & Medicaid Services to collect and report the following data
in a standard format that enables analysis:
•
facility-level data on all types of Medicaid payments to nursing facilities, including resident contributions
to their cost of care;
•
data on the sources of non-federal share of spending necessary to determine net Medicaid payment at
the facility level; and
•
comprehensive data on nursing facility nances and ownership necessary to compare Medicaid
payments to the costs of care for Medicaid-covered residents and to examine the eects of real estate
ownership models and related-party transactions.
2.2 To help inform assessments of whether Medicaid nursing facility payments are consistent with statutory
goals of eciency, economy, quality, and access, the Secretary of the U.S. Department of Health and Human
Services should direct the Centers for Medicare & Medicaid Services (CMS) to update the requirement
that states conduct regular analyses of all Medicaid payments relative to the costs of care for Medicaid-
covered nursing facility residents. This analysis should also include an assessment of how payments relate
to quality outcomes and health disparities. CMS should provide analytic support and technical assistance to
help states complete these analyses, including guidance on how states can accurately identify the costs of
ecient and economically operated facilities with adequate sta to meet residents’ care needs. States and
CMS should make facility-level ndings publicly available in a format that enables analysis.
2.1-2.2 voting
results # Commissioner
Yes 16 Allen, Bella, Bjork, Brooks, Carter, Cerise, Davis, Duncan, Gerstor,
Giardino, Gordon, Heaphy, Johnson, Medows, Scanlon, Weno
Not present 1 Herrera Scott
