
1
12/13/2021
The Centers for Medicare & Medicaid Services (CMS)
Fact Sheet for State and Local Governments
CMS Programs & Payment for Care in Hospital Alternate Care Sites
REVISED December 13, 2021
Purpose
In response to the COVID-19 public health emergency (PHE), state and local governments, hospitals, and
others are developing alternate care sites to expand capacity and provide needed care to patients. The term
alternate care site (ACS) is a broad term for any building or structure that is temporarily converted or newly
erected for healthcare use.
1
The Federal Healthcare Resiliency Task Force issued a toolkit to help state and
local governments develop an ACS.
This document provides state and local governments developing alternate care sites with information on
how to seek payments through CMS programs – Medicare, Medicaid, and the Children’s Health Insurance
Program (CHIP) – for acute inpatient and outpatient care furnished at the site.
Key Takeaway
The easiest path to obtaining payments through CMS programs for covered health care services furnished
at the ACS is for an already-enrolled hospital or health system to treat the ACS as a temporary expansion of
their existing ‘brick-and-mortar’ location. In these circumstances the local hospitals and health systems
operate, staff, and bill for care furnished at the ACS. State and local governments
2
that want to establish
(meaning to develop or build) a hospital ACS, and be paid by CMS for furnishing covered hospital inpatient
and outpatient services to enrolled beneficiaries, have three options:
1. hand over operation and billing for care delivered in the ACS to an enrolled hospital or health
system;
2. enroll the ACS as a new hospital in CMS programs; or
3. if options (1) and (2) are not available, CMS would not make facility payments, but qualified and
enrolled physicians or other non-physician practitioners could bill for covered (professional
3
)
services that they furnish at the ACS.
Because some state and local governments may not be as familiar with the process to enroll in CMS
programs as hospitals, they should contact their applicable CMS Location, previously known as the CMS
Regional Offices (see Appendix E) to discuss this process. Additional information regarding new hospital
enrollment and the flexibilities that existing hospitals and other providers have to expand capacity at ACSs
during the PHE is below.
1
These sites are often called “alternate care sites” (ACSs), but may also be referred to as “temporary expansion locations”,
“temporary expansion sites”, “field hospitals”, or by other names. This paper uses the term “alternate care sites” to align with the
language used in the Health Care Resiliency Task Force’s toolkit.
2
The term “state and local governments” is used in this fact sheet to account for state, city, county, territorial and tribal
governments and their respective agencies, including health departments.
3
When beneficiaries receive services at a traditional acute care hospital, Original Medicare will typically make two payments – one
for the hospital inpatient or outpatient facility services (e.g. room and board or nursing) and one for professional services that
physicians or non-physician practitioners furnish (e.g., evaluation and management). Under option 3, CMS would not make facility
payments to the entity operating the ACS. However, even if the ACS does not enroll as a hospital, CMS may pay for professional
services furnished to CMS beneficiaries at the ACS, as discussed in more detail in this fact sheet. In Medicaid/CHIP, specific benefit
rules will also need to be followed.

2
12/13/2021
About CMS Programs
Medicare is a federal health insurance program for people over 65, as well as certain young people with
disabilities and those with End Stage Renal Disease (ESRD). Typically, beneficiaries have a choice between
Original Medicare and Medicare Advantage. Medicare Advantage plans are a type of Medicare health plan
offered by a private company that contracts with CMS to provide Medicare benefits. Beneficiaries in
Medicare Advantage plans have their services paid for by the private plan and not Original Medicare. When
“Medicare” is discussed in this paper, it is referring to Original Medicare, and not Medicare Advantage,
unless otherwise noted.
Medicaid and CHIP provide health coverage to eligible low-income adults, children, pregnant women,
elderly adults and people with disabilities. Medicaid and CHIP are funded jointly by states and the federal
government, and the programs are administered by states, according to federal requirements. Medicaid
and CHIP generally provide comprehensive benefits to people who are determined eligible by states; some
benefits are required and some are optional.
Approaches to Hospital ACS Operations & CMS Programs
Organizations have flexibility to develop ACSs in locations that best fit the needs of their community.
Further, ACSs can provide a spectrum of health care services, from intensive care to primary care,
depending on the capability of the site. Many organizations are using ACSs to create additional inpatient
hospital capacity and are designing site operations to support care of COVID-19- patients and non-COVID-
19 patients. There are three questions CMS
4
uses to determine whether it will pay for covered hospital
facility inpatient or outpatient services furnished to enrolled beneficiaries at an ACS.
1. Is the ACS operator already enrolled in CMS programs as an acute care hospital or other provider
type
5
that is able to furnish inpatient or outpatient care during the PHE?
2. Is the ACS operator contributing resources and responsible for the care being furnished to CMS
beneficiaries at the ACS?
3. Is the ACS operator following the billing requirements of the applicable Medicare, Medicaid, or
CHIP hospital payment system?
Many acute care hospitals have established ACSs by converting existing non-clinical space for clinical use
(e.g., cafeteria repurposed for care), as well as locations outside of the traditional hospital such as tents,
retrofitted gymnasiums, convention centers, or other non-clinical locations. In these circumstances, the
hospitals are already enrolled in CMS programs and are able to treat these locations as a temporary
extension of their existing hospital footprint during the PHE under flexibility granted through so-called
“1135 waivers
” (additional information about these waivers is in Appendix A). CMS pays for inpatient and
outpatient care furnished in these ACSs as if the care had been delivered in the hospital’s traditional “brick-
and-mortar” locations. Hospitals must follow all applicable CMS coding and billing rules during the PHE.
6
State and local governments have also established ACSs, often with (non-CMS) federal support. For
example, state and local governments may seek reimbursement to develop ACSs from the Federal
4
Generally speaking, state Medicaid/CHIP programs would also use these questions to guide whether they would pay for covered
inpatient or outpatient care at the ACS. However, state Medicaid/CHIP programs may have alternate approaches – ACSs should
contact their state Medicaid agency for more information.
5
Other facilities include Long-Term Care Hospitals, Critical Access Hospitals, Inpatient Rehabilitation Facilities, and others.
Additional information about the flexibilities these facilities have to furnish acute care during the PHE is in Appendix C.
6
https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf
3
12/13/2021
Emergency Management Agency’s (FEMA) Public Assistance program (under Category B, emergency
protective measures) which was authorized under the Robert T. Stafford Disaster Relief and Emergency
Assistance Act of 1988 (Stafford Act). Other federal funding sources include the Department of Health and
Human Services’ (HHS’s) Hospital Preparedness Program and the Centers for Disease Control and
Prevention’s Crisis Response Cooperative Agreement. Some state and local governments have also
requested HHS deploy portable medical facilities called Federal Medical Stations, and provide clinical staff
through the National Disaster Medical System.
7
The Federal Healthcare Resiliency Task Force has published
a guide to the funding opportunities state and local governments (as well as other organizations) can seek
to establish and operate ACSs.
While some state and local governments operate acute care hospitals (e.g., certain county hospital and
health systems), others may not be enrolled in CMS programs and, as a result, are not usually in a position
to be paid immediately by Medicare or Medicaid/CHIP. However, state and local governments developing
an ACS have options to seek payments through CMS programs for covered inpatient and outpatient
services furnished to enrolled beneficiaries at the site.
• *Easiest Path* Partner with a hospital or health system: State and local governments can establish
the site and then hand over operations of the ACS to an enrolled hospital (or other provider
temporarily certified as a hospital
8
), which can treat the ACS as a temporary extension of their
brick-and-mortar location under 1135 waivers
and bill CMS and state Medicaid/CHIP programs for
covered hospital services furnished to enrolled beneficiaries. Importantly, hospitals may assume
operating responsibility and bill Medicare
9
for inpatient and outpatient care furnished at the ACS
even if a governmental entity provides some support. For example, the state/county emergency
management agency or public health department may provide (or coordinate the provision of)
staffing, dining, linens, or beds used in the ACS. In these circumstances, hospitals operating the site
may seek payment on the claim for the services they provide (e.g. nursing), but are instructed not
to seek payment on the claim for a service where they are not incurring the cost of the service (e.g.
dining). Hospitals would also not reflect the costs of services provided such as staffing, dining,
linens, or beds (where they did not incur the costs) on their Medicare cost reports.
10
As noted
previously, certain states and local governments may operate or be closely affiliated with certain
hospital and health systems, including county-level health systems and those health systems owned
by a state university. In these circumstances, these providers may be able to serve as an effective
ACS partner. If not, state and local governments may also work with private non-profit or for-profit
hospitals in their community. The enrolled hospital operating the site would need to ensure it
continues to meet non-waived CMS and state requirements that remain in force during the PHE.
11
• Enroll as a new hospital: If the state or local government wants to operate the site or cannot find a
hospital or health system partner, they can form a new entity and enroll that entity as a hospital in
CMS programs. For example, the state of Maryland is pursuing the creation of a new hospital to
provide care to COVID-19 patients at the Baltimore Convention Center. Though this option is
7
NDMS: https://www.phe.gov/Preparedness/responders/ndms/ndms-teams/Pages/default.aspx / FMS:
https://www.phe.gov/Preparedness/support/medicalassistance/Pages/default.aspx#fms
8
Additional information on the flexibility that providers have to furnish hospital care during the PHE is in Appendix C. We also note
that, in certain cases, state and local governments may have a state or locally-owned hospital that could operate the ACS.
9
Hospitals should contact their state Medicaid agency to determine any Medicaid/CHIP-specific payment requirements.
10
Section 1862(a) of the Social Security Act and Medicare Claims Processing Manual 100-04, Chapter 32, Transmittal 67:
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c32.pdf
11
Additional information regarding CMS rules in effect during the PHE is available here:
https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf

4
12/13/2021
available to state and local governments, it may entail additional complexity and take longer than
working with an existing hospital to assume responsibility for the site. To ensure beneficiary safety
and to reduce the potential for waste, fraud, and abuse, new hospitals must follow certain steps to
enroll in both Medicare and the state’s Medicaid/CHIP programs. Information regarding the
Medicare enrollment steps is in Appendix B. States wanting to pursue this pathway to operate an
ACS should contact their applicable CMS Location to further discuss the process (contact
information is available in Appendix E) and contact their state Medicaid agency to determine any
additional Medicaid/CHIP enrollment requirements.
• Not enroll as a hospital; clinicians, such as physicians and other non-physician practitioners, could
seek payment for covered professional services: State and local governments not wanting to enroll a
new hospital could engage a medical group to furnish and bill for the professional services
furnished to enrolled beneficiaries at an ACS – but the state/locality may have to find separate
funding for many other hospital-related services if the state/locality wanted the ACS to function
similarly to a hospital. Original Medicare and state Medicaid/CHIP programs generally pay hospitals
for: 1) inpatient and outpatient facility services furnished to enrolled beneficiaries and 2) separately
pay physicians and other non-physician practitioners for professional services, regardless of the
setting where the covered professional service was furnished.
12
Said differently, when a beneficiary
is admitted to a hospital, there are typically Medicare facility claims (for the hospital’s services) and
Medicare professional claims (for the professional’s services, such as patient evaluation and
management). During the PHE, Medicare will pay physicians and non-physician practitioners for
covered professional health care services furnished to enrolled beneficiaries at ACSs. Similar to
hospitals, physicians and non-physician practitioners seeking payment for care furnished to
Medicare beneficiaries must be enrolled in Medicare; and likewise practitioners seeking payment
from their state Medicaid programs must be enrolled with such state and follow specific program
coverage and payment rules. State and local governments that are not able to enroll as a hospital
could partner with CMS-enrolled physicians or non-physician practitioners who would be able to
furnish and bill for ambulatory care at the ACS.
Multi-Hospital/Organization Approaches
It is important to note that, if state and local governments expect to partner with more than one private
hospital to provide services at an ACS, they should contact their CMS Location if they are interested in
being paid by Medicare or Medicaid for hospital services furnished to Medicare or Medicaid beneficiaries at
the site. A full list of CMS Location contacts is in Appendix E. Under this scenario, where more than one
hospital or health system operates the ACS, CMS would need additional information to determine whether
it could pay for services at that location. For example, CMS would need to know if there were distinct
clinical spaces to provide a safe environment for their patients.
Medicaid and CHIP Considerations
If ACSs are operated through the options presented in this paper, federal regulations would allow State
Medicaid and CHIP agencies to pay for covered services provided in them. That said, each ACS should also
reach out to the State Medicaid Agency to understand any state-based direction.
12
Please note that the applicable payment systems under Medicaid may vary by state, however this is typically how payments work
under the Original Medicare. States and local governments should contact their Medicaid agency to determine any specific
Medicaid/CHIP payment requirements.

5
12/13/2021
APPENDIX A: Hospital Requirements & 1135 Waivers
General Hospital Requirements
Under federal law, hospitals must meet CMS requirements in order to bill Medicare or Medicaid for
covered inpatient or outpatient hospital services furnished to Medicare or Medicaid / CHIP beneficiaries.
• Conditions of Participation:
13
These health and safety standards are the foundational requirements
that organizations must achieve to enroll as a hospital and furnish hospital care to CMS
beneficiaries. The Conditions of Participation include requirements for the types of services the
hospital must provide – such as pharmacy, laboratory, radiologic, 24/7 nursing services and room
and board – as well as structural requirements regarding its nursing and medical staff, quality
improvement and others. Hospitals are subject to initial and periodic surveys verifying that they
meet these requirements.
• Enrollment: Hospitals must enroll in the Medicare program and identify key information about their
organization prior to furnishing and billing for hospital care. During the PHE, CMS streamlined
certain enrollment requirements. For example, during the PHE new hospitals can call their
applicable Medicare Administrative Contractor to establish temporary billing privileges for the
duration of the PHE, instead of completing a paper or electronic CMS-855A application.
14
Once the
PHE has expired, these hospitals must be in full compliance with enrollment and certification
requirements for hospitals. States may have separate enrollment requirements for their Medicaid
programs.
• Billing Rules: Generally speaking, Medicare and Medicaid will pay for reasonable and necessary
inpatient and outpatient services for enrolled beneficiaries. However, depending on the type of
hospital and the services furnished, payments may vary. For example, Medicare pays certain acute
care hospitals differently than it does critical access hospitals.
15
Hospitals must follow the
appropriate billing rules to be paid for care.
Emergency 1135 Waivers & Health System Flexibility
In certain circumstances, the Secretary of the Department of Health and Human Services (HHS), under
authority in section 1135 of the Social Security Act can temporarily modify or waive certain Medicare,
Medicaid, CHIP, or HIPAA requirements on a provider-by-provider, geographic, or other broad-scale basis.
These actions are commonly referred to as “1135 waivers”. Under its Hospitals Without Walls initiative,
CMS waived several Medicare conditions of participation at 42 CFR Part 482 and provider-based rules at 42
CFR §413.65 on a national basis. These so-called “blanket” waivers give hospitals flexibilities to respond to
the COVID-19 PHE and to furnish care in ACSs, including retrofitted locations (e.g., tents, gymnasiums, and
even the patient’s home). Broadly speaking, these waivers streamline the process for hospitals that are
already enrolled in the Medicare program to expand access to care. The waivers do not, however,
eliminate enrollment, survey, and billing requirements for brand new hospitals that wish to furnish care
to beneficiaries. CMS has temporarily modified physician supervision requirements, physical environment,
and telehealth payment policies to promote access to care during the PHE. Additional information
regarding the waivers and CMS emergency rulemaking is available here: https://www.cms.gov/about-
cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers.
13
Additional information regarding CMS’ hospital Conditions of Participation is available here: https://www.cms.gov/Regulations-
and-Guidance/Legislation/CFCsAndCoPs/Hospitals, here: https://www.cms.gov/Medicare/Provider-Enrollment-and-
Certification/CertificationandComplianc/Hospitals, and here: https://www.cms.gov/files/document/covid-hospitals.pdf
14
https://www.cms.gov/files/document/provider-enrollment-relief-faqs-covid-19.pdf
15
https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS; andhttps://www.cms.gov/Outreach-
and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/CritAccessHospfctsht.pdf

6
12/13/2021
In the provision of all services, including under an 1135 waiver, recipients of HHS funds must comply with
federal civil rights non-discrimination requirements on the basis of race, color, national origin, disability,
age, sex, and exercise of conscience and religious freedom rights. States are also still subject to obligations
under the integration mandate of the Americans with Disabilities Act, to avoid subjecting persons with
disabilities to unjustified institutionalization or segregation.

7
12/13/2021
APPENDIX B: Medicare Hospital Enrollment
Prior to furnishing and billing Medicare for inpatient or outpatient hospital care delivered to Medicare
beneficiaries, a new hospital must enroll in the Medicare program. This enrollment has three critical steps:
the hospital must obtain a National Provider Identifier (NPI) from the National Plan and Provider
Enumeration System, the hospital must submit an enrollment application to Medicare, and the hospital
must undergo a survey demonstrating that it meets the conditions of participation. Additional information
regarding these steps is below.
Step 1: Obtain NPI
• New hospitals are required to obtain a new NPI from NPPES. Applying for an NPI is a process
separate from Medicare enrollment. To obtain an NPI, the new hospital may apply online at
https://NPPES.cms.hhs.gov.
• For NPI purposes, sole proprietors and sole proprietorships are considered to be “Type 1”
providers. Organizations (e.g., corporations, partnerships) are treated as “Type 2” entities. As a
result, new hospitals will want to seek “Type 2” NPIs.
• It is the new hospital’s responsibility to determine if it has “subparts.” A subpart is a component of
the organization that furnishes healthcare and is not itself a legal entity. If the new hospital does
have subparts, it must determine if it should obtain its unique NPIs for those subparts.
Step 2: Enrollment Application
• New hospitals (as well as other new institutional providers) are required to submit a CMS 855A
enrollment application to their applicable Medicare Part A/B Medicare Administrative Contractor
(MAC).
16
As noted below, providers may also enroll via the MAC’s hotline, though they may be
required to complete a paper or electronic application following the end of the PHE.
• The CMS 855A enrollment application requires new hospitals to submit certain identifying and
administrative information to Medicare, including the new hospital’s tax identification number, the
location(s) where the hospital will furnish care, information about the new hospital’s ownership
and control, and information about the individuals managing the new hospital.
• Importantly, CMS requires new hospitals to obtain all necessary state licenses, certifications or
other approvals before enrolling and treating Medicare beneficiaries. This information must also be
included in the new hospital’s 855A enrollment application. We believe that many states may have
streamlined licensing requirements during the PHE.
• The CMS 855A enrollment applications can be submitted via paper (e.g., mail or fax) or through
Medicare’s Provider Enrollment, Chain and Ownership System
(PECOS). Providers may also enroll
via the MAC’s hotline, though they may be required to complete a paper or electronic application
following the end of the PHE.
• Once the application is submitted the applicable MAC reviews the application. Due to the COVID-19
PHE, CMS is expediting enrollment application reviews. Reviews for applications submitted by
phone or through PECOS will typically be completed within 7 calendar days or less. Reviews for
applications submitted via paper (e.g., mail or fax) will be completed within 14 calendar days or
less.
16
A current map of A/B MAC regions is available here: https://www.cms.gov/Medicare/Medicare-Contracting/Medicare-
Administrative-Contractors/Downloads/AB-Jurisdiction-Map-Jun-2019.pdf . A list of the current MACs by state is available here:
https://www.cms.gov/Medicare/Medicare-Contracting/Medicare-Administrative-Contractors/Downloads/MACs-by-State-June-
2019.pdf

8
12/13/2021
Step 3: Survey
• New hospitals must demonstrate through a survey that they meet Medicare’s hospital Conditions
of Participation
17
that are in effect during the PHE. Certain conditions have been waived under
CMS’ 1135 waiver authority discussed in more detail above. A list of the Conditions of Participation
that are waived during PHE is available here: https://www.cms.gov/files/document/summary-
covid-19-emergency-declaration-waivers.pdf
• Hospitals can obtain a survey from a state survey agency or an accreditation organization (AO) with
a Medicare-approved hospital program. We encourage new hospitals to work with CMS Location
staff (please see Appendix E for contact information) and the applicable agency within their state
government to determine the quickest way to obtain a survey. In certain cases, CMS is temporarily
allowing surveys to be conducted remotely by AOs to ensure organizations can respond to the
pandemic. Please also note that the state agency that issues hospital licenses may be different than
the agency that conducts the certification survey.
• Based on the survey results, the state agency or AO makes a recommendation for approval or
denial (a certification of compliance or noncompliance) to the CMS Location.
• The CMS Location makes the final decision regarding program eligibility. The CMS Location also
works with the HHS Office of Civil Rights to obtain necessary Civil Rights clearances. If approved,
the provider must typically sign a provider agreement.
17
https://www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs/Hospitals

9
12/13/2021
APPENDIX C: Frequently Asked Questions for Alternate Care Sites Initial Survey and Certification
1. Question: To request an initial certification survey, does a prospective provider or supplier work
through their state, CMS or both?
Answer: Alternate care sites that want to participate as a Medicare certified hospital provider have two
options to obtain an initial certification survey to demonstrate compliance with applicable Medicare
Conditions of Participation (CoPs) for hospitals. The prospective hospital may obtain Medicare certification
through the state survey agency (SA) process or through accreditation by a private, national accreditation
organization (AO) with a CMS-approved hospital program.
Prior to any Medicare survey activity, the prospective hospital must obtain an operating license as a
hospital in their state. Licensure requirements in the states may be more restrictive than those of Medicare
and the hospital would be required to meet those requirements in addition to the Medicare CoPs.
2. Question: Are all surveys performed by the state or a private accreditation organization?
Answer: All surveys will be performed by either the SA or AO prior to approval of Medicare certification. A
key difference between using an AO instead of the SA is that AOs have a fee associated with their
accreditation services, although AOs may be able to perform their surveys sooner than the state. These fees
and services can vary among AOs and they may have additional accreditation requirements that could
exceed Medicare CoPs.
3. Question: Does CMS require surveyors to follow a standard approach to inspections or is the
survey process determined locally by the state or accreditation organization?
Answer: CMS has a standard survey process which surveyors must use to determine compliance. This
process is specified in the CMS State Operations Manual Appendix A,
which is used by SAs as their
standards for survey activity of hospitals. AO survey processes have been approved as meeting or
exceeding CMS standards, and may vary from the SA based on their accreditation standards. Additional
survey methodology flexibilities have been offered during the public health emergency (PHE) to assist
states and AOs in performing surveys and increasing access to healthcare.
4. Question: Can alternate care sites that wish to enroll as hospitals start the Medicare enrollment
application process with CMS before getting a survey?
Answer: Yes, prospective hospital providers must submit an enrollment application, the form CMS-855A,
as
the first step in seeking Medicare certification, which should we done before getting a survey. Alternate
care sites that wish to enroll as hospitals should contact their CMS Location first, which can direct them to
the appropriate Medicare Administrative Contractor to discuss enrollment. A list of CMS Locations and
their contact information is in Appendix E of this document.
5. Question: Has CMS made any changes to the survey process as a result of the section 1135
waivers in place during the public health emergency (PHE)?
Answer: CMS has waived certain Conditions of Participation during the PHE under the authority in section
1135 of the Social Security Act. Alternate care sites that wish to enroll as hospitals will not be required by
the surveyors to demonstrate compliance with any CoPs that have been waived. However, we note that the

10
12/13/2021
waivers are only in effect through the end of the PHE or may be modified or terminated before the end of
the PHE. Additionally, there have been flexibilities granted for how surveys are performed during the PHE –
more information on these flexibilities can be found in the “survey and certification” section of this
webpage.
6. Question: Does CMS have any standard approach to inspecting an alternate care site for
conditions of participation or is that a locally made decision by the inspectors?
Answer: CMS requires all alternate care sites that wish to become a Medicare or Medicaid certified hospital
to meet all Medicare hospital CoPs that have not otherwise been waived during the PHE. State survey
agencies and AOs must assess hospitals’ compliance with these CoPs.

11
12/13/2021
APPENDIX D: Provider Flexibilities & Medicare Payment for Health Care Services Furnished at an ACS
Under the 1135 waivers and two interim final rules with comment periods
18
, CMS has given significant
flexibility to health care providers to respond to the COVID-19 PHE by expanding access and furnishing
patient care in ACSs. Some non-hospital providers, as described below, may be temporarily certified as
hospitals to build capacity during the PHE. State and local governments could partner with organizations
that use these flexibilities to furnish and bill for hospital care in a state or local government-developed ACS.
To the extent that states partner with providers using these flexibilities, states should ensure that they have
examined their legal and regulatory regimes and have made any changes necessary to allow for providers
managing ACSs to furnish the full breadth of services intended by the state.
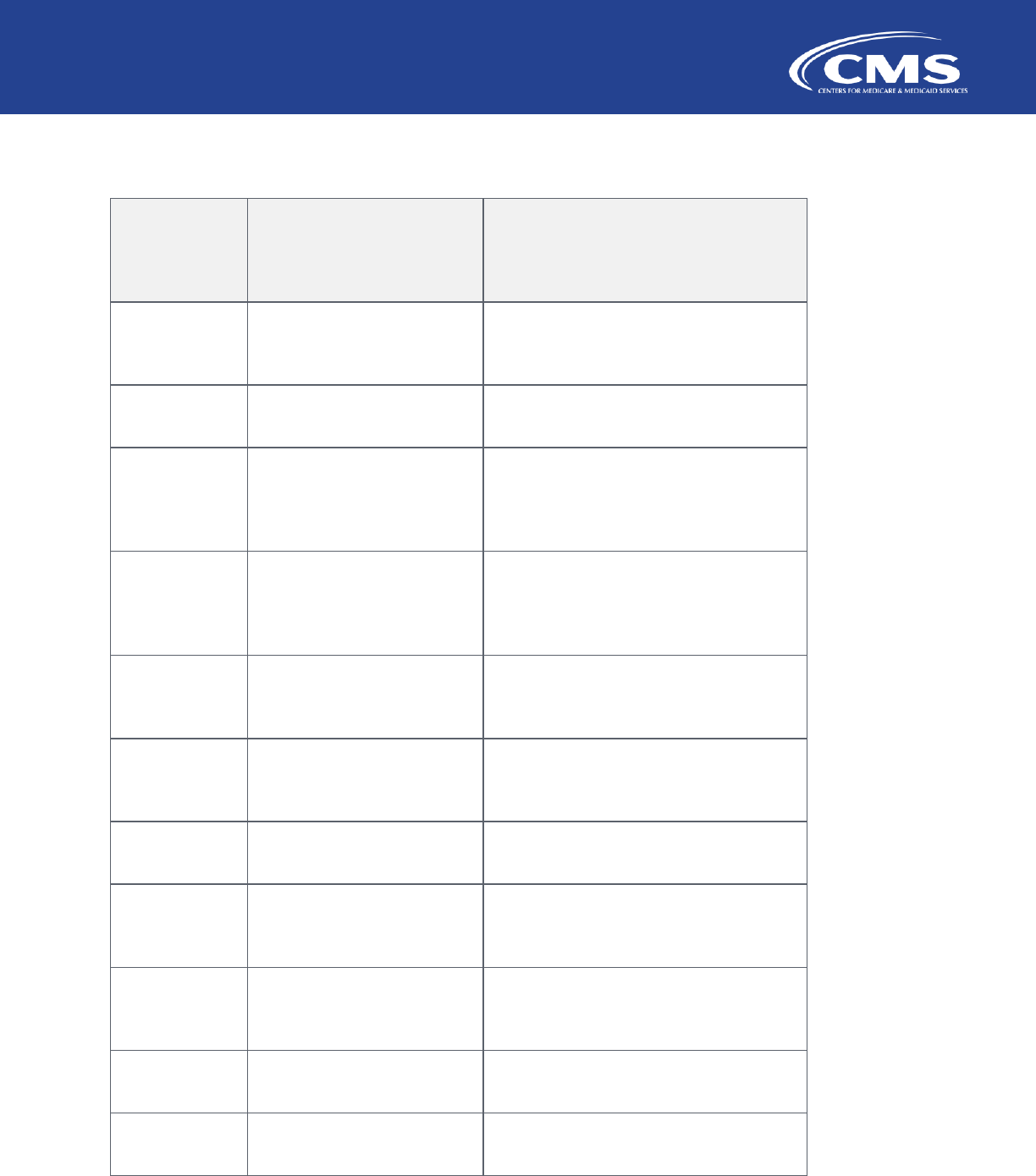
Partner that Assumes
Operating Responsibility
From State, Local,
Territorial or Tribal
Government
Prerequisites to furnishing
care at off-campus
state/locality-developed
ACS
Covered Health Care
Services Medicare Will Pay
For at ACS
Professional Services Also
Billed?
Acute Care Hospital
• 1135 Waivers
• Develop remote
“provider-based”
19
location of the hospital
at the ACS
• Inpatient hospital care
• Outpatient hospital
care
• Specific payments
would depend on
hospital type
20
and
arrangement
• Professional services
can be furnished and
billed for separately.
• Professionals should
use place of service
codes “19” or “21”
depending on whether
the ACS is considered
an outpatient or
inpatient facility.
Long-Term Care Hospital
• 1135 Waivers
• Develop remote
location of the hospital
at the ACS
• Inpatient hospital care
• Payments made
through the LTCH
Prospective Payment
System
• Professional services
can be furnished and
billed for separately
using place of service
code “21”.
Inpatient Rehabilitation
Facility
• 1135 Waivers
• Develop remote
location of the hospital
at the ACS
• Inpatient hospital care
• Payments made
through the IRF
Prospective Payment
System
• Professional services
can be furnished and
billed for separately
using place of service
code “21”.
Ambulatory Surgical Center
to Hospital Conversion (no
longer accepting new
enrollees as of 12/01/2021)
• 1135 Waivers
• Temporarily enroll in
Medicare as a hospital
at own location
• Develop remote
“provider-based”
location of the
converted hospital at
the ACS
• Inpatient hospital care
• Outpatient hospital
care
• Payments would be
made under the
Inpatient Prospective
Payment System and
the Outpatient
Prospective Payment
System
• Professional services
can be furnished and
billed for separately.
• Professionals should
use place of service
codes “19” or “21”
depending on whether
the ACS is considered
an outpatient or
inpatient facility.
Licensed Independent
Freestanding Emergency
• 1135 Waivers
• Inpatient hospital care
• Outpatient hospital
care
• Professional services
can be furnished and
billed for separately.
18
March 30, 2020 Emergency Interim Final Rule with Comment: https://www.cms.gov/files/document/covid-final-ifc.pdf / April 30,
2020 Emergency Interim Final Rule with Comment: https://www.cms.gov/files/document/covid-medicare-and-medicaid-ifc2.pdf
19
The terms “provider-based entity” and “remote location of the hospital” are defined at 42 CFR § 413.65.
20
Acute care hospitals may be paid under the Inpatient Prospective Payment System. Hospitals may also be exempt from the
prospective payment systems and rather paid on a cost-basis, such as Critical Access Hospitals, PPS-Exempt Cancer Hospitals, and
Children’s Hospitals.

12
12/13/2021
Departments to Hospital
Conversion
• Temporarily enroll in
Medicare as a hospital
at own location
• Develop remote
“provider-based”
location of the
converted hospital at
the ACS
• Payments would be
made under the
Inpatient Prospective
Payment System and
the Outpatient
Prospective Payment
System
• Professionals should
use place of service
codes “19” or “21”
depending on whether
the ACS is considered
an outpatient or
inpatient facility.
Physicians and Medical
Groups
• Waivers not necessary
• ACS cannot be
considered a hospital
inpatient or outpatient
location and no facility
claim can be submitted
to Medicare
• Professional services
furnished in “non-
facility” location
• Professionals should
use place of service
codes “11” to identify
practice location
• Services paid under
the Medicare Physician
Fee schedule
N/A
Additional Detail Regarding Each Option
Acute Care Hospital – New Provider-based Department: CMS waived several Medicare Conditions of
Participation at 42 CFR Part 482 and provider-based rules at 42 CFR § 413.65 for the duration of the COVID-
19 PHE. These waivers give hospitals flexibilities to respond to the COVID-19 PHE and to furnish care in
ACSs, including retrofitted locations (e.g., tents, gymnasiums, and other temporary locations). This
temporary expansion must not be inconsistent with the state’s emergency preparedness or pandemic plan.
In the March 30, 2020 interim final rule with comment period, CMS established a temporary policy to allow
hospitals to furnish routine inpatient care “under arrangements” with other providers (85 FR 19278-19280).
Importantly, state and local governments that want to partner with an existing hospital could hand-off
operations of the ACS to the hospital, where it would be provider-based location of the hospital. Hospitals
would need to ensure they could continue to meet the Conditions of Participation that remain in effect
during the PHE, continue to exercise sufficient control and responsibility over the use of hospital resources
in treating patients, and obtain any state licensing requirements or other approvals as necessary. During
the PHE, if the hospital intends to bill Medicare for the services under the main hospital, no additional
provider enrollment actions are required (for example, hospitals do not need to submit an updated CMS
855A enrollment form for the ACS).
Long-term Care Hospital (LTCHs) – New Remote Location: The same waivers and rule flexibilities provided to
acute care hospitals (described directly above) also apply to LTCHs. In addition, CMS has implemented
Section 3711(b) of the CARES Act (P.L. 116-136) which requires CMS to waive the LTCH 50% rule (requiring
that at least 50% of patients meet LTCH criteria), as well as the site-neutral payment rate (lower rate
applied when LTCH criteria not met) during the PHE.
21
Importantly, state and local governments that want
to partner with an existing hospital could hand-off operations of the ACS to the LTCH, which would in turn
need to make the ACS a remote location of the LTCH. LTCHs would also need to ensure they could continue
to meet the Conditions of Participation that remain in effect during the PHE, as well as obtain any state
licensing requirements or other approvals as necessary. During the PHE, if the LTCH intends to bill Medicare
for the services under the main hospital, no additional provider enrollment actions are required (for
example, LTCHs do not need to submit an updated CMS 855A enrollment form for the ACS).
21
https://www.cms.gov/files/document/MM11742.pdf

13
12/13/2021
Inpatient Rehabilitation Facility (IRF) – New Remote Location: The same waivers and rule flexibilities
provided to acute care hospitals and LTCHs (described directly above) also apply to IRFs. In addition, CMS
has implemented Section 3711(a) of the CARES Act (P.L. 116-136), which requires CMS to waive the
requirement that IRF patients generally receive at least 15 hours of therapy per week. In the May 8, 2020
interim final rule (85 FR 27550), CMS further modified the IRF coverage and classification requirements for
freestanding IRF hospitals to exclude patients admitted solely to relieve acute care hospital capacity in a
state (or region, as applicable) that is experiencing a surge during the PHE.
Importantly, state and local governments that want to partner with an existing hospital could hand-off
operations of the ACS to the IRF, which would in turn need to make the ACS a remote location of the IRF.
IRFs would also need to ensure they could continue to meet the Conditions of Participation that remain in
effect during the PHE, as well as obtain any state licensing requirements or other approvals as necessary.
During the PHE, if the IRF intends to bill Medicare for the services under the main hospital, no additional
provider enrollment actions are required (for example, IRFs do not need to submit an updated CMS 855A
enrollment form for the ACS).
Ambulatory Surgical Center (ASC) to Hospital Conversion: CMS created a streamlined and temporary
enrollment process for ASCs that wished to convert to a hospital to expand capacity and treat inpatients
and outpatients. During the pandemic, ASCs were identified as a critical resource to assist in expanding
capacity for inpatient and outpatient hospital services for patients requiring a higher level of care. CMS
believes states and hospitals have developed effective strategies for managing capacity and safely resuming
elective surgery. Given the low volume of inpatient services delivered in ASCs under this flexibility, CMS
believes there is no longer a need for expanded hospital capacity through ASCs. Therefore, effective
12/01/2021, CMS will no longer accept new temporary enrollment requests from ASCs seeking to enroll as
hospitals. More information can be found here:
https://www.cms.gov/files/document/qso-22-03-asc-
hospital.pdf.
Licensed Independent Freestanding Emergency Department to Hospital Conversion: Due to their existing
infrastructure, independent freestanding emergency departments (ED), which have no hospital affiliation
and are specifically licensed by the state to operate independently to provide emergency services, have
been identified as a resource to assist in expanding capacity for inpatient and outpatient hospital services
22
https://www.cms.gov/files/document/provider-enrollment-relief-faqs-covid19.pdf
14
12/13/2021
for patients requiring a higher level of care. Currently, only four states license independent freestanding
EDs to operate without hospital affiliation: Colorado, Delaware, Rhode Island, and Texas.
Working in coordination with their State and State’s pandemic plan, licensed independent freestanding EDs
began participating in Medicare and Medicaid to help address the need to increase hospital capacity to
provide additional care to patients during the PHE in the following ways:
• As hospital-affiliated EDs under the 1135 emergency waiver;
• As Medicaid-certified clinics under the state’s clinic benefit; and
• As a Medicare-certified hospital by temporarily enrolling in Medicare as a hospital through the
attestation process developed under the 1135 emergency waiver.
• As a physician practice
As with ASCs, CMS created the same streamlined approach for the temporary enrollment of IFEDs during
the COVID-19 PHE, which allowed them to provide care to inpatients to expand capacity and reduce
hospital burden. Although they were not previously treating patients in this manner, CMS believed that
certain IFEDs had an appropriate infrastructure to be able to deliver care to patients requiring acute care.
Unlike ASCs, the IFEDs are not a recognized Medicare provider-type. CMS believes that states and hospitals
have developed strategies to manage capacity and meet the needs of patients they serve across the
nation. Given the low volume of inpatient services delivered in IFEDs under this flexibility, CMS believes
there is no longer a need for expanded hospital capacity from IFEDs. Therefore, effective 12/01/2021, CMS
will no longer accept new temporary enrollment requests from IFEDs seeking to enroll as hospitals. More
information can be found here: https://www.cms.gov/files/document/qso-22-03-asc-hospital.pdf
.
Physicians and Medical Groups: Medicare pays physicians and non-physician practitioners for covered
professional health care services furnished to Medicare beneficiaries. During the PHE, Medicare-enrolled
physicians and non-physician practitioners can bill Medicare for covered professional services that are
furnished to Medicare beneficiaries at ACSs, including gymnasiums, or other non-clinical locations. In the
case when the ACS is considered part of a hospital, physicians and non-physician practitioners would use
the applicable place of service code depending on whether the ACS is furnishing outpatient (place of service
code “19”) or inpatient care (place of service code “21”). However, when the ACS is not enrolled as part of a
hospital or other facility, and no facility claim is being submitted to Medicare, physicians and non-physician
practitioners should use place of service code “11” for a non-facility practice location. When a covered
professional service is furnished in non-facility locations, Medicare payments are typically increased to
account for the higher practice expense required to furnish the service. As a result, state and local
governments with expansion sites that are not able to enroll as hospitals or other Medicare facility types
could partner with Medicare-enrolled physicians or non-physician practitioners to be able to furnish and bill
for ambulatory care at the ACS.
15
12/13/2021
APPENDIX E: CMS Location Contact List
CMS
Location
Contact
States served by the CMS Location
Boston
ROBOSORA@cms.hhs.gov
Connecticut, Maine, Massachusetts,
New Hampshire, Rhode Island, Vermont
New York
RONYCORA@cms.hhs.gov
New Jersey, New York
Philadelphia
Delaware, District of Columbia,
Maryland, Pennsylvania, Virginia, West
Virginia
Atlanta
ROATLORA@cms.hhs.gov
Alabama, Florida, Georgia, Kentucky,
Mississippi, North Carolina, South
Carolina, Tennessee
Chicago
Illinois, Indiana, Michigan, Minnesota,
Ohio, Wisconsin
Dallas
Arkansas, Louisiana, New Mexico,
Oklahoma, Texas
Kansas City
ROKCMORA@cms.hhs.gov
Iowa, Kansas, Missouri, Nebraska
Denver
ROREAORA@cms.hhs.gov
Colorado, Montana, North Dakota,
South Dakota, Utah, Wyoming
San Francisco
ROSFOORA@cms.hhs.gov
Arizona, California, Hawaii, Nevada,
Pacific Territories
Seattle
ROSEA_ORA2@cms.hhs.gov
Alaska, Idaho, Oregon, Washington
Puerto Rico
prfo@cms.hhs.gov
Puerto Rico, US Virgin Islands
