
1
SUBSTANCE USE AND RECOVERY SERVICES PLAN
SUBSTANCE USE
AND RECOVERY
SERVICES PLAN
DECEMBER 2022-2023
Developed by the Substance Use
and Recovery Services Advisory
Committee in collaboration with

2
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Acknowledgements .............................................................................................................................................. 5
Health equity in tribal and rural areas ................................................................................................................ 6
Executive summary ............................................................................................................................................... 7
Subcommittees ..................................................................................................................................................... 8
Contextual setting ................................................................................................................................................. 9
Committee recommendations overview ......................................................................................................... 10
Data ................................................................................................................................................................... 10
Diversion, outreach, and engagement ....................................................................................................... 10
Treatment ......................................................................................................................................................... 10
Recovery support services ............................................................................................................................. 10
Recommendation regarding the appropriate criminal legal system response, if any, to possession
of controlled substances. .............................................................................................................................. 11
Data ....................................................................................................................................................................... 14
SURSA Committee recommendations ........................................................................................................ 15
Recommendation 6: Behavioral Health Administrative Service Organization (BH-ASO) and
Recovery Navigator Program (RNP) data reporting .................................................................................. 15
Recommendation 13: Law Enforcement (LE) and Behavioral Health (BH) data collection ................ 16
Evaluation Recommendations for the Blake-bill Interventions ............................................................... 18
Diversion, outreach, and engagement ............................................................................................................ 20
SURSA Committee recommendations ........................................................................................................ 20
Recommendation 10: Expanding investment in programs along the 0-1 intercept on the sequential
intercept model .............................................................................................................................................. 20
Recommendation 12: Stigma-reducing outreach and education regarding youth and schools ..... 22
Recommendation 5: Amend RCW 69.50.4121 – Drug paraphernalia law ........................................... 23
Treatment ............................................................................................................................................................. 25
SURSA Committee recommendations ........................................................................................................ 25
Recommendation 7: Health engagement hubs for people who use drugs ......................................... 25
Recommendation 14: Safe supply workgroup .......................................................................................... 27
Recommendation 11: SUD engagement and measurement process................................................... 27
Recommendation 15: Expanding funding for OTPs to include partnerships with rural areas .......... 29
Recovery support services ................................................................................................................................. 31
SURSA Committee recommendations ........................................................................................................ 32
Recommendation 1: Legislative policy for tax incentives and housing vouchers for respite spaces 32
Recommendation 3: LGBQTIA+ community housing .............................................................................. 33
Recommendation 4: Training of foster, kinship and family or origin, parents with children who use
substances ....................................................................................................................................................... 34
Recommendation 16: Addressing zoning issues regarding behavioral health services .................... 35

3
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Recommendation 2: Legal advocacy for those affected by SUD ........................................................... 36
Recommendation 8: Employment and education pathways .................................................................. 37
Recommendation 18: Continuum of housing ........................................................................................... 38
Recommendation 9: Expansion of the Washington Recovery Helpline and asset mapping............. 39
ESB 5476 program updates .............................................................................................................................. 41
Recovery navigator program ........................................................................................................................ 41
Peer-Run and clubhouse services expansion ............................................................................................ 42
Homeless outreach stabilization transition (HOST) expansion ............................................................... 42
Medication for opioid use disorder (MOUD) in jail .................................................................................. 43
Contingency management ........................................................................................................................... 44
Short-term housing vouchers ....................................................................................................................... 44
Substance use disorder (SUD) family navigators ....................................................................................... 44
Conclusion ........................................................................................................................................................... 45
Next steps ........................................................................................................................................................ 45
Constraints and limitations ............................................................................................................................ 45
Unmet bill requirements .................................................................................................................................... 46
Appendices .......................................................................................................................................................... 47
Appendix A – Timeline ................................................................................................................................... 47
Appendix B – Recommendation 1: Legislative policy for tax incentives and housing vouchers for
respite spaces .................................................................................................................................................. 48
Appendix C – Recommendation 2: Legal advocacy for those affected by SUD .................................. 51
Appendix D – Recommendation 3: LGBQTIA+ community housing .................................................... 54
Appendix E – Recommendation 4: Training of foster and kinship parents with children who use
substances ....................................................................................................................................................... 56
Appendix F – Recommendation 5: Amend RCW 69.50, 4121 – Drug paraphernalia law .................. 58
Appendix G – Recommendation 6: BH-ASO and RNP data reporting .................................................. 63
Appendix H – Recommendation 7: Health Hubs ...................................................................................... 76
Appendix I – Recommendation 8: Employment and education pathways ........................................... 80
Appendix J – Recommendation 9: Expansion of WHRL and Asset Mapping ...................................... 82
Appendix K – Recommendation 10: Expanding investment in programs along the 0-1 intercept on
the sequential intercept model .................................................................................................................... 85
Appendix L – Recommendation 11: SUD engagement and measurement process .......................... 89
Appendix M – Recommendation 12: Stigma-reducing outreach and education, more importantly
regarding youth and schools ........................................................................................................................ 95
Appendix N – Recommendation 13: Law Enforcement and Behavioral Health data collection ....... 98
Appendix O – Recommendation 14: Safe supply workgroup .............................................................. 106
Appendix P – Recommendation 15: Expanding funding for OTPs to include partnerships with rural
areas ................................................................................................................................................................ 114

4
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix Q – Recommendation 16: Addressing zoning issues regarding behavioral health services
......................................................................................................................................................................... 125
Appendix R – Recommendation 18: Continuum of Housing ................................................................ 129
Appendix S - Resources to inform a recommendation for the state’s criminal-legal response to
possession of controlled substances ......................................................................................................... 135
Appendix T – RDA evaluation recommendation ..................................................................................... 145
Appendix U – Current state programs ...................................................................................................... 153

5
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Acknowledgements
The Washington State Health Care Authority would like to acknowledge and give our deepest
gratitude to those who have and who are currently serving on the Substance Use and
Recovery Services Advisory (SURSA) Committee. Through their guidance and subject matter
expertise during the planning and development of the Substance Use and Recovery Services
Plan, HCA has been able to submit this robust and forwardthinking plan to help
Washingtonians affected by drug use and substance use disorders (SUD). Their enthusiasm,
eagerness for collaboration, grace, and time has been invaluable to the proces of this plan
development.
Table 1: Current SURSA Committee roster
Michael Langer
Director’s appointment
Lauren Davis
House of Representatives
Democrat
Dan Griffey
House of Representatives
Republican
Manka Dhingra
Senate
Democrat
John Braun
Senate
Republican
Amber Leaders
Governor’s Office
Caleb Banta-Green
Addictions, Drug & Alcohol
Institute at UW
Julian Saucier
Adult in recovery from SUD who
experienced criminal legal
consequences
Amber Daniel
Peer recovery services provider
Brandie Flood
Anti-racism member
Stormy Howell
Representative of a federally
recognized Tribe
Chad Enright
Prosecutors Office
John Hayden
Public defender
Kevin Ballard
Local government
Sarah Melfi-Klein
Association of Washington Health
Plans
Sherri Candelario
Recovery housing provider
James Tillett
Outreach services provider
Christine Lynch
SUD treatment provider
Sarah Gillard
Representative of experts
serving people with co-
occurring SUD and mental
health conditions
Donnell Tanksley
Washington Association of
Sheriffs and Police Chiefs
Malika Lamont
Representative of experts on the
diversion from the criminal legal
system to community-based care
for people with SUD
Chenell Wolfe
Adult in recovery from SUD
who experienced criminal
legal consequences
Alexie Orr
Adult in recovery from SUD who
experienced criminal legal
consequences
Hunter McKim
Youth in recovery from SUD with
criminal legal consequences
Kendall Simmonds
Youth in recovery from SUD
with criminal legal
consequences
Addy Adwell
SUD provider Union member

6
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Health equity in tribal and rural areas
When considering services across the state of Washington, special attention is
given to select areas, including those in rural counties, that have less access to
amenities and services than those in urban areas. The current system that makes the
distinction between these two types of counties is built on the decennial censuses and
may not be comparable due to methodological changes and absence of bridging data
among census decades. There is also notice taken into the differences in health status
indicators between rural and urban residents that might reflect underlying differences
in the economic and socio-demographic characteristics in these regions. When the
recommendations of these plans are considered and developed, distinction and
consideration is given to meet the needs of these areas.
The Committee further dedicates itself to adhere to the principles of health
equity and justice for American Indian/Alaskan Native (AI/AN) communities, people of
color, and other affected populations. The Committee provides representation from
various populations, while working in collaboration with AI/AN, people of color, and
other populations that have been oppressed by dominant culture. The Committee has
examined strategies and activities to understand how current work can be used to
address inequities in substance use disorder, treatment, and recovery services. Voices
in subcommittees provided an avenue to understand cultural barriers to treatment and
recovery and examine what we can do in the future to provide meaningful, culturally
appropriate services.
We recognize that input from tribes and tribal organizations (AI/AN), people of
color, and other affected populations is essential to help guide our initiative developed
out of the Engrossed Senate Bill 5476, in a way that respects the culture and traditions
of individual communities and impacts of systemic racism.

7
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Executive summary
In 2016, an individual was arrested. Upon jail booking, a corrections officer found a small
amount of methamphetamine in their clothing. They were subsequently charged and
convicted of Unlawful Possession of Controlled Substance under RCW 69.50.4013. The
individual appealed the ruling and argued that they did not know there was
methamphetamine in the jeans, which were gifted from a friend two days prior.
On February 25, 2021, the Washington State Supreme Court vacated the conviction and ruled
the Controlled Substance Statute unconstitutional, stating RCW 69.50.4013 violates the due
process clause as it does not protect individuals who unknowingly were in possession of a
substance.
This ruling, and the resulting decriminalization of controlled substance possession, led to the
passing of Engrossed Senate Bill 5476 and the creation of the Substance Use Recovery
Services Advisory (SURSA) Committee and eventual substance use recovery services plan.
This plan was developed on behalf of the Washington State Health Care Authority (HCA) and
made by the Substance Use Recovery Services Advisory (SURSA) Committee, as outlined in
Engrossed Senate Bill 5476 (2021): Responding to the State v. Blake decision by addressing
justice system responses and behavioral health engagement, treatment, and recovery
services.
“The authority, in collaboration with the substance use recovery services advisory
committee established in subsection (2) of this section, shall establish a substance
use recovery services plan. The purpose of the plan is to implement measures to
assist persons with substance use disorder in accessing outreach, treatment, and
recovery support services that are low barrier, person centered, informed by
people with lived experience, and culturally and linguistically appropriate. The plan
must articulate the manner in which continual, rapid, and widespread access to a
comprehensive continuum of care will be provided to all persons with substance
use disorder.”
Table 2: ESB 5476 deliverable timeline
Deliverable
Date
Preliminary report to HCA
November 24, 2021
Final plan submitted to Governor and Legislature
December 1, 2022
Annual Plan Implementation Report to Governor and
Legislature
December 1, 2023, and each
subsequent year until 2026
Adopt rules/contract necessary to implement the plan
December 1, 2023

8
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Subcommittees
The SURSA Committee (Committee)
acknowledged in March 2022 that there was
a need for more Committee time and more
expertise to advise the recommendations
requested for the Substance Use Recovery
Services Plan (Plan); see Appendix A. HCA
wants to acknowledge subcommittee
participation, involvement, commitment, and
expertise provided to inform the
recommendations put forth for the Plan.
Participation in the subcommittee included:
Voices of Community Activists and
Leaders – Washington (VOCAL-WA),
along with the community members who
VOCAL-WA brought to the table to share
their lived and living experience.
Law Enforcement Assisted Diversion
(LEAD) National Support Bureau and
technical assistance team
Washington State Association of Sheriffs
and Police Chief (WASPC)
Members of Washington Alliance for
Quality Recovery Residences (WAQRR)
Washington State Association of Drug
Court Professionals (WSADCP)
University of Washington, including
Addictions, Drug & Alcohol Institute
(ADAI) and supporting staff.
Behavioral health administrative service
organizations (BH-ASOs)
Recovery Navigator Program (RNP)
administrators.
Department of Health employees
Department of Commerce employees
Washington residents with lived and
living experience
Employees of the Department of Social
and Health Services (DSHS)
Employees of the Department of
Children, Youth, and Families (DCYF)
Employees of HCA
Community-based organizations
Washington Low Income Housing Alliance
Figure 1: Timeline outline

9
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Contextual setting
Below are various terms and definitions used in the realm of substance use, that will
provide contextual background to gain a greater understanding of the work described
in the plan. The SURSA Committee and subcommittees provided feedback and
guidance surrounding these definitions.
Harm reduction: Harm reduction is a set of practical strategies and ideas aimed at
reducing negative consequences associated with drug use. Harm reduction is also a
movement for social justice built on a belief in, and respect for, the rights of people
who use drugs.
1
Harm reduction involves safer use of supplies as well as care settings,
staffing, and interactions that are person-centered, supportive, and welcoming.
2
Recovery: Recovery is a process of change through which individuals improve their
health and wellness, live self-directed lives, and strive to reach their full potential.
Recovery support services (RSS): A collection of resources that sustain long-term
recovery from substance use disorder, including for people with co-occurring
substance use disorders and mental health conditions, recovery housing, permanent
supportive housing, employment and education pathways, peer supports and
recovery coaching, family education, technological recovery supports, transportation
and childcare assistance, and social connectedness.
Recovery residences: Recovery housing benefits individuals in recovery by reinforcing
a substance-free lifestyle and providing direct connections to other peers in recovery,
mutual support groups and recovery support services. Substance-free does not
prohibit prescribed medications taken as directed by a licensed prescriber, such as
pharmacotherapies specifically approved by the Food and Drug Administration (FDA)
for treatment of opioid use disorder and/or for the treatment of co-occurring disorder.
Low threshold-low barrier treatment: Increasing access to behavioral health-related
services and programs by creating person-centered programs that are easy to access,
offer a high quality of care, and eliminate barriers associated with accessing or
remaining in behavioral health treatment and related services. Elements include:
• Short time to the start of necessary medication (same day for most)
• Polysubstance use allowed initially and ongoing
• Counseling always offered, not mandated
• Urine drug screens are used to inform clinical care
3
1
https://harmreduction.org/about-us/principles-of-harm-reduction/
2
This term as normally presented excludes practice-based evidence developed and promulgated by indigenous communities
for generations. The Western model considers evidence in a narrower context that indigenous communities.
3
https://www.learnabouttreatment.org/for-professionals/low-barrier-buprenorphine/

10
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Committee recommendations overview
Recommendations are numbered according to the order in which they were voted on by the
Committee. Recommendation #17 – an amendment to the Good Samaritan Law – is not included, as it
did not receive SURSAC support.
Data
Table 3: Data recommendations
Recommendation
Type
Recommendation 6: BH-ASO and RNP data reporting
Policy/Funding
Recommendation 13: LE and BH data collection and reporting Policy/Funding
Diversion, outreach, and engagement
Table 4: Diversion, outreach, and engagement recommendations
Recommendation
Type
Recommendation 10: Expanding investment in programs along the 0-1
intercept on the sequential intercept model
Funding
Recommendation 12: Stigma-reducing outreach and education, more
importantly regarding youth and schools
Policy/Funding
Recommendation 5: Amend RCW 69.50.4121 – Drug paraphernalia law
Policy
Treatment
Table 5: Treatment recommendations
Recommendation
Type
Recommendation 7: Health Engagement Hubs for People Who Use Drugs
Funding
Recommendation 14: Safe supply workgroup
Funding
Recommendation 11: SUD engagement and measurement process
Policy/Funding
Recommendation 15: Expanding funding for OTPs to include partnerships
with rural areas
Funding
Recovery support services
Table 6: Recovery support services recommendations
Recommendation
Type
Recommendation 1: Tax incentives for landlords and respite space
housing vouchers
Policy/Funding
Recommendation 3: LGBTQIA+ community housing
Policy/Funding
Recommendation 4: Training of foster and kinship parents of children
who use substances
Policy/Funding

11
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Recommendation 16: Addressing zoning issues regarding behavioral
health services
Policy/Funding
Recommendation 2: Legal advocacy for those affected by SUD
Policy/Funding
Recommendation 8: Employment and education pathways
Funding
Recommendation 18: Continuum of housing
Funding
Recommendation 9: Expansion of WRHL and asset mapping Funding
Recommendation regarding the appropriate criminal legal system response, if any,
to possession of controlled substances
.
One of the more visible requirements of the SURS plan was the Committee’s
development and consideration of recommendations for an appropriate criminal legal
response to possession of a controlled substance. What follows is the outline and
strategies behind the development and eventual consensus surrounding a
recommendation for this legislative request.
RCW 71.24.546§1 - The authority, in collaboration with the substance use recovery
services advisory committee, established in subsection (2) of this section, shall
establish a substance use recovery services plan. The purpose of the plan is to
implement measures to assist persons with substance use disorder in accessing
outreach, treatment, and recovery support services that are low barrier, person
centered, informed by people with lived experience, and culturally and linguistically
appropriate. The plan must articulate the manner in which continual, rapid, and
widespread access to a comprehensive continuum of care will be provided to all
persons with substance use disorder.
The plan must consider: (RCW 71.24.546§3§l) Recommendations regarding the
appropriate criminal legal system response, if any, to possession of controlled
substances.
Preliminary discussions surrounding this recommendation from the SURSA Committee
produced considerations for various types of data that would assist in a meaningful
recommendation. Data sets were identified as:
Analysis of the racial impact of decriminalization of possession versus
legalization of supply through review of national and international models
Current state of the criminal legal system and how it is either being used to
incarcerate or used as leverage for individuals to enter treatment, and
successfully complete treatment
o What are the effects, and intent versus outcomes
Outcomes data for drug court participants, including analysis of racial
outcomes
Study of systemwide impacts on the community

12
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Research data on the efficacy of behavioral health interventions embedded
within the criminal legal system
Analysis of gaps in current system to take care of the individual diverted due to
decriminalization, into health care, child protective services (CPS), foster care,
etc.
o Looking at gaps where services are not available, like in rural areas
Health care cost savings for individuals who are diverted to harm reduction and
low-barrier services
Inclusivity (nature of the crime, race) of individuals in diversion programs and
their outcomes
Summary of which areas in the state are offering diversion programs for youth
Considerations of social determinants of health and the criminal legal system
Data on Involuntary Treatment Act (ITA), crisis stabilization centers and inpatient
treatment programs are working outside of the criminal system
Data comparison from what was or was not working prior to State v. Blake and
the current statute
A comprehensive resource document was created and distributed to the SURSA
Committee for their review. The document detailed the various areas where data had
been made available, based on those data requirements outlined by the Committee.
See Appendix S.
On August 8,
2022, the SURSA Committee met during a regularly scheduled monthly
meeting and participated in a straw poll exercise to assign a hierarchy of preference
regarding proposed recommendations. Table 7 summarizes the concepts discussed
and voted on as the more comprehensive components and direction for the
recommendation.

13
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Table 7: Preliminary votes on initial concepts and ideas regarding possession
The Committee requested additional time and resources to assist in advising the Committee
on implications related to the various components that may go into this recommendation. A
special Committee meeting was held on September 9, 2022, that consisted of various
presentations from:
• American Civil Liberties Union (ACLU) summary of Policy Strategies from Commit to
Change Washington and the Pathways to Recovery Act
• LEAD Technical Assistance Team on pre-arrest diversion strategies from LEAD, RNP,
and Arrest and Jail Alternatives (AJA)
• University of Washington on safe supply models
• Oregon Health Justice Alliance on decriminalization successes and lessons learned
regarding Oregon Measure 110
• VOCAL- WA on disparity and inequity in criminal legal response to possession.
Through these presentations, common elements were identified to be incorporated with any
recommendation made by the Committee.
•Safe supply initiative
14
Votes
•Maintain possession of a controlled substance as a
misdemeanor with diversion options
12
Votes
•Decriminalize possession of controlled substances and
paraphernalia with no civil penalty or fines
9
Votes
•Decriminalize possession of controlled substances and
paraphernalia and make it a civil penalty
8
Votes
•Legalize possession of all controlled substances/create
a regulated market
8
Votes
•Maintain possession of a controlled substance as a
gross misdemeanor with diversion options
4
Votes
•Make possession of a controlled substance a felony,
with diversion eligibility
2
Votes
•Maintain possession of a controlled substance as a
misdemeanor, punishable only by fine
1
Vote
•Make possession of a controlled substance a felony
1
Votes

14
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Table 8: Common elements for recommendation of possession
Common elements that are required for any response to possession
Safe supply
Law enforcement
assisted diversion
and referral
options
Investments in
the behavioral
health workforce
and infrastructure
for outreach,
treatment, and
recovery services
Investment in
harm reduction
and low barrier
engagement
services
The gravity of this recommendation was taken very seriously by Committee members. While
data and additional meeting time was provided, some Committee members voiced concern
that there were some missed opportunities for a deeper understanding of the options
developed and discussed by the Committee.
The Committee made a final decision on this recommendation:
Decriminalize possession of
controlled substances and paraphernalia with no civil penalty or fines.
Data
Data requirements were identified early on as integral to a significant portion of the
outlined plan requirements, in addition to discussions about addressing the criminal
legal response to possession but also. This data subcommittee was tasked with
considering the Health Care Authority ProviderOne and Behavioral Health Data
System (BHDS) data collection systems as well as informing new data collection
parameters for the various programs within ESB 5476, such as Recovery Navigator
Program (RNP). The subcommittee addressed current concerns regarding data
collection while it developed recommendations that met the various requirements
outlined in RCW 71.24.546§3. These recommendations meet statutory requirements
found in (§1.3.h) and (§1.3.m):
(1)“ (3) The plan must consider:
(h) The design of recovery navigator programs in section 2 of this act, including
reporting requirements by behavioral health administrative services organizations
to monitor the effectiveness of the programs and recommendations for program
improvement;
(m) Recommendations regarding the collection and reporting of data that identifies
the number of persons law enforcement officers and prosecutors engage related to
drug possession and disparities across geographic areas, race, ethnicity, gender,
age, sexual orientation, and income. The recommendations shall include, but not
be limited to, the number and rate of persons who are diverted from charges to

15
SUBSTANCE USE AND RECOVERY SERVICES PLAN
recovery navigator services or other services, who receive services and what type of
services, who are charged with simple possession, and who are taken into custody;”
Below are the recommendations and outlined plans of action developed from this
subcommittee and approved by the SURSA Committee.
SURSA Committee recommendations
The Committee recommends establishing specific data collection and reporting
requirements among behavioral health administrative services organizations (BH-
ASOs) related to their regional recovery navigator programs (RNPs). This
recommendation also requests to identify data to be included in the RNP quarterly
reports for SURSAC review to monitor program effectiveness and inform
recommendations for improvements. The recommendation addresses ESB 5476
Section 1.3(h), related to “reporting requirements by behavioral health administrative
service organizations to monitor the effectiveness of the programs and
recommendations for program improvement.”
As a key aspect of the Plan
and the state’s response to
the State v. Blake supreme
court ruling, the Recovery
Navigator Program was
initiated as soon as possible
following the passing of ESB
5476. Uniform Program
Standards were established,
and HCA developed a draft
data collection workbook for
use by the BH-ASOs and
RNP contractors. The BH-
ASOs have contracted with
local providers and community-based organizations, and those providers have hired
staff who are collecting those data which are being tracked in the data collection
workbook.
This recommendation requests to:
Seek funds to implement a data integration platform that can serve both
as a common database for diversion efforts across the state and as a data
Recommendation 6: Behavioral Health Administrative Service Organization (BH-
ASO) and Recovery Navigator Program (RNP) data reporting

16
SUBSTANCE USE AND RECOVERY SERVICES PLAN
collection and management tool for practitioners. If possible, leverage
existing platforms already in use by HCA-funded efforts and any closed
loop referral systems implemented in the future.
Establish a quality assurance process for BH-ASOs to ensure that data in
the data collection workbooks are clean, complete, and accurate before
submitting to HCA, and a plan in place for data that is deemed unverified
for submission
Where applicable, add data validation to data fields in the data collection
workbook (e.g., only dates accepted under DOB and date of referral,
only 7-digit numbers accepted in ProviderOne ID, etc.)
It is expected that individuals served by RNP will be engaged in long-term, intensive
case management. While some “light touch” participants could see significant
individual benefits in a relatively short period of time, many individuals will have
complex co-occurring challenges, including extensive criminal-legal system contact.
For these participants, progress toward health, wellness, and stability is expected to
take much longer than a year, so evaluations of the RNP in its early years should
include determining measures and measures of change (in knowledge, attitudes, or
actions) for systems stakeholders, not only data that can assess participant-level
formative and outcome metrics.
While the impacts of a systems-change initiative like RNP are unlikely to be seen within
the first few years, Washington State should currently work to establish the necessary
capacities and processes to enable both formative evaluation and summative
evaluation of effectiveness. This will likely require the integration of a new data
infrastructure or processes that can exploit existing and new streams of data
pertaining to an individual’s criminal legal system encounters/involvement, and the
outreach, treatment, and recovery support services they receive through RNPs.
See Appendix G.
The recommendation requests building upon, and providing ongoing funding for, a
data integration infrastructure that can receive and analyze standardized data
gathered by law enforcement, courts, and prosecutors; Recovery Navigator Program
case management; behavioral health treatment services; and recovery support
services, to meet the mandates of Section 1.3(m) “regarding the collection and
reporting of data which identify the number of persons law enforcement officers and
prosecutors engage related to drug possession and disparities across geographic
Recommendation 13: Law Enforcement (LE) and Behavioral Health (BH) data
ll i

17
SUBSTANCE USE AND RECOVERY SERVICES PLAN
areas, race, ethnicity, gender, age, sexual orientation, and income. The
recommendations shall include, but are not limited to, the number and rate of persons
who are diverted from charges to recovery navigator services or other services, who
receive services and what type of services, who are charged with simple possession,
and who are taken into custody.”
The focus in this recommendation is on a general data infrastructure for reporting key
indicators. Data is being collected in various sectors and programs related to
substance use and behavioral health systems (law enforcement encounters, treatment,
recovery support services programs, Recovery Navigator Program, etc.)
Many of those data systems do not have a consistent identifier across systems, or
consistent standards for data collection and classification, which creates redundancies
and makes it difficult to link the data between sectors. This hinders understanding of
the patterns taking place among different communities and their outcomes following
an encounter with law enforcement. Consistent data gathering and integration
methodologies such as those described in this recommendation would meet the data
mandates of 1.3(m). A data integration infrastructure such as the one described in this
recommendation has been implemented in four Law Enforcement Assisted Diversion
(LEAD) pilot sites per RCW 71.24.589 (Whatcom, Snohomish, Mason, and Thurston
counties) and three Arrest and Jail Alternatives grantee sites per RCW 36.238A.450
(Olympia, Port Angeles, Walla Walla).
In addition to the legislative mandated collection of data addressed above, the
following data suggestions to be collected and reported are:
System utilization
• Use of emergency medical services
• Arrest, days in jail
• New charges with incident date after of referral to RNP (divided by
felony, misdemeanor), to be added to Case Management tab in RNP
Data Collection tool
• Convictions with incident date after date of referral to RNP (broken into
felony / misdemeanor), to be added to Case Management tab in RNP
Data Collection tool
• Access to and engagement with culturally appropriate, non-punitive,
community-based resources
System response
• Capacity and variety of local services aligned with RNP’s commitment to
harm reduction and holistic care

18
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Number and percent of substance possession-related law enforcement
encounters (e.g., public order) that result in arrest, booking, and/or
convictions for RNP-eligible behaviors, as well as the demographics of
those individuals engaged by law enforcement in these encounters
• Racial disparity analysis that compares demographics of individuals who
are arrested and booked into jail, compared to the demographics of
those who are referred to RNP, among diversion-eligible individuals
Quality of life
• Self-report quality life/well-being
• Improved mental and physical health
Services and access gap analysis: indicated by comparing services
needed/requested by RNP participants, referrals made, referred services
received by BH-ASO region, and reasons why services were not received (if
applicable). If the data collection burden for case managers is too great for this
level of analysis, request that case managers report areas where service gaps
are a persistent problem.
RNP participant satisfaction: collected via survey every six months following
enrollment in RNP, with procedures in place outlining minimum and maximum
contact efforts.
See Appendix N.
Department of Social and Health Services (DSHS) Research and Data Analysis Division
(RDA), provided an evaluation recommendation for programs developed from the
Blake bill decision. The programs included in this evaluation recommendation include
Recovery Navigator Program (RNP), Medication for Opioid Use Disorder (MOUD) in
Jails, Peer-Run and Clubhouse Services Expansion, Homeless Outreach Stabilization
Transition (HOST) Expansion, and Substance Use Disorder Family Navigators.
The RDA-recommended evaluation strategy focuses on efficiently estimating the
impact of each Blake intervention on the above outcomes to inform decision makers
about their overall and relative effectiveness. RDA recommends a general analysis of
outcomes broadly applicable to all Blake interventions; program-specific
strategies/outcomes may be further developed with input from the evaluator, RDA,
program staff, and other individuals designated by HCA.
Evaluation Recommendations for the Blake-bill Interventions

19
SUBSTANCE USE AND RECOVERY SERVICES PLAN
To efficiently estimate the effectiveness of the Blake interventions, RDA recommends a
strategy that employs similar methods across the programs and focuses on a common
set of relevant outcomes. The quasi-experimental evaluation will compare the
outcomes of service recipients “enrolled” in each intervention (treatment group) with
the experiences of statistically similar individuals who were not enrolled in the
intervention (comparison group) and then draw inferences about the effectiveness of a
specific intervention.
The specific construction of each outcome measure (e.g., number of arrests per year,
arrest rates, felony arrests, months of SUD treatment, etc.) will be determined in
collaboration with the evaluator, RDA, program staff, and other individuals designated
by HCA. Baseline descriptions of program participants and propensity score matching
will be possible as soon as a sufficient number of clients are enrolled in any given
program.
4
Typically analyses of this type employ 12- to 18-month pre- and post- periods to
characterize outcomes. The time periods to be used in these analyses will depend on
reporting deadlines, implementation schedules, and lags in the availability of data for
specific outcome measures.
HCA program managers should work closely with service providers and RDA to ensure
this information is routinely and systematically collected and maintained in a medium
that supports the efficient transmission of data. Some programs collect information on
disparate spread sheets; others, such as the RNP, utilize sophisticated case
management software. Future opportunities for analyses on the relative effectiveness
4
The “sufficient” number of participants will depend on the expected effect size of any given intervention. Interventions
expecting large effect sizes require small samples.
Treatment Groups
Comparison Groups
Outcome Measures
at Baseline
Outcome Measures
at Baseline
Post-period Outcome
Measures
Post-period Outcome
Measures
Blake
Intervention
Within group differences in outcomes
Between group
differences in
outcomes
Pre-Intervention
(Baseline) Measures
• Demographics
• Criminal History and incarcerations
• Substance use disorders
• Mental health diagnoses
• Chronic Medical Conditions
• Employment
• Housing status
• Etc…
Post-Intervention Outcomes
• Re-arrests and jail days
• ED utilization and hospitalizations
• Behavioral health treatment
• Access to primary care
• Housing services
• Employment

20
SUBSTANCE USE AND RECOVERY SERVICES PLAN
of different intervention service components may be possible for programs that collect
sufficient additional information on their clients.
See Appendix T.
Diversion, outreach, and engagement
Diversion services were one of the most crucial components of addressing ESB 5476
and the Blake decision. The legislation led to the creation of the Recovery Navigator
Program, providing regional resources to law enforcement diverted individuals to help
access care. This subcommittee was tasked with developing ideas on diversion along
with the subsequent engagement and outreach components of the plan. These
recommendations meet statutory requirements found in: (§1.3.a) and (§1.3.g).
(1)“ (3) The plan must consider:
(a) The points of intersection that persons with substance use disorder have
with the health care, behavioral health, criminal, civil legal, and child welfare
systems as well as the various locations in which persons with untreated
substance use disorder congregate, including homeless encampments,
motels, and casinos;
(g) Framework and design assistance for jurisdictions to assist in compliance
with the requirements of RCW 10.31.110 for diversion of individuals with
complex or co-occurring behavioral health conditions to community-based
care whenever possible and appropriate, and identifying resource gaps that
impede jurisdictions in fully realizing the potential impact of this approach;”
Below are the recommendations and outlined plans of action developed by this
subcommittee and approved by the SURSA Committee.
SURSA Committee recommendations
The SURSA Committee recommends continued and increased investments in
evidence-based diversion programs that operate along intercepts 0 and 1 on the
sequential intercept model
5
, including, the Recovery Navigator Program, Arrest/Jail
Alternative programs, LEAD, and other harm reduction, trauma-informed, and public
health-based approaches. These programs and interventions center around a racial
justice lens for providing support to underserved communities and populations.
5
For More information on the Sequential Intercept Model: https://www.prainc.com/sim/
Recommendation 10: Expanding investment in programs along the 0-1 intercept
on
the sequential intercept model

21
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Amending RCW 10.31.110 (Alternatives to Arrest – Individuals with mental disorders
or substance use disorders) and RCW 10.31.115 (Drug Possession – Referral to
assessment and services) would reflect how these programs should be used as part of
a statewide arrest and jail diversion system by mandating availability of services within
a supportive network of care.
Consistent with the Plan requirement outlined in RCW 71.24.546§3(i), this
recommendation requests shifting funding from the punishment sector to increase
and sustain investments to ensure equitable distribution of, and access to, culturally
appropriate, non-punitive, community-based resources, including treatment.
“(g)Framework and design assistance for jurisdictions to assist in compliance with the
requirements of RCW 10.31.110 for diversion of individuals with complex or co-
occurring behavioral health conditions to community-based care whenever possible
and appropriate, and identifying resource gaps that impede jurisdictions in fully
realizing the potential impact of this approach.”
To provide services, outlined below, to the Washington youth population, the request
was made to provide adequate policy changes to address systemic barriers, and
Centers for Medicaid Services (CMS) State Plan Amendment, for services made
available to youth starting at the age of 13, the minimum Medicaid enrollee age
without an adult, and incorporate Medication for Opioid Use Disorder (MOUD)
accessibility and coverage.
A range of services are noted as diversion options, those services are:
• Crisis stabilization units for youth and adults
• Triage facilities for youth and adults
• Designated 24/7 crisis responders
• Mobile crisis response services for youth and adults
• Regional entities responsible for receiving referrals
In addition, these services should be made available in all regions as well:
• ASAM-alternative SUD Assessments for youth and adults
• Syringe service programs for youth and adults
• Health Hubs for youth and adults who use drugs
• Detox/withdrawal management for youth and adults
• MOUD for youth and adults
• Outpatient treatment for youth and adults
• Ensure that long-term harm reduction-supported case management is available
after diversion so that diversion becomes meaningful
See Appendix K.

22
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Providing education related to
naloxone administration and
overdose identification in
Washington State public
schools (grade 6 – 12) helps to
reduce stigma and save lives.
Outlined in §1.3.a, this
recommendation would
provide substantial
preventative and life-saving
recognition and training in the
administration of naloxone for
students, administrators,
teachers, and other
educational professionals, at points of intersection for those that may be affected, or
know someone who is affected, by SUD.
In 2019-2020, youth under 24 years saw the highest increase in mortality, 59 percent,
compared to other age groups. With the dramatic increase in substance use mortality,
it is imperative to reduce the discrimination and judgment leveled against youth and
young adults who use drugs. This may be achieved through practical strategies
including, but not limited to naloxone distribution within school settings, overdose
education, evidenced-based drug safety curriculum starting at the sixth grade, and
partnerships with other community organizations that advance the health and well-
being of young people. Safety First is an example of learning curricula for young
people that is evidenced based and/or promising practice. The SURSA Committee
noted additional policy and statutory amendments were necessary to help support
efforts to expand services to youth and eliminate the stigma directed at people who
use illicit substances.
RCW 69.50.412: Prohibited acts: E—Penalties. (wa.gov) prohibits the distribution of
hypodermic syringes to people under the age of 18. This RCW prohibits entities
and/or individuals from distributing intramuscular syringes needed for naloxone
administration. Intramuscular naloxone is currently substantially cheaper than nasal
formulations – being limited by cost and access of naloxone due to RCWs may
exacerbate any disparities of substance use mortality among persons under the age of
18. This law will need a technical amendment to remove barriers to life saving
medication.
Recommendation 12: Stigma-reducing outreach and education regarding youth and
schools

23
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Stocking a “standing order”
(as defined in RCW
69.41.095) of “opioid
overdose reversal
medication” (e.g., Naloxone)
is required via RCW
28a.210.390 to be stocked in
high schools (grades 9-12)
already for school districts
with more than 2,000
students. These medications
can be administered by a
school nurse, a health care
professional, or trained staff
person located at a health
care clinic on public school
property under contract with
the school district or
designed trained school
personnel. Funding would
need to be provided to
increase naloxone and
overdose education among
school aged young people
(grades 6 – 12), which includes funds related to outreach and communication.
See Appendix M.
The SURSA Committee recommends amending RCW 69.50.4121 to remove language
that prohibits “giving” or “permitting to give” drug paraphernalia in any form, so that
programs that serve people who use drugs do not risk class I civil infraction charges
for providing life-saving supplies needed for comprehensive drug checking, safer
smoking equipment, and other harm-reduction supplies to engage and support
people who use drugs. The Committee recommends the state expressively preempt
the field in Washington State regarding any penalties imposed for selling/giving
paraphernalia per RCW 69.50.4121. Applying this amendment will support low-
barrier, person-centered outreach and treatment services that improve safety for
Recommendation 5: Amend RCW 69.50.4121 – Drug paraphernalia law
Figure 2: 2022 King County medical examiner data

24
SUBSTANCE USE AND RECOVERY SERVICES PLAN
people who use drugs, considering the points of intersection that people with
substance use disorder have with behavioral health systems and the places where
people with untreated substance use disorder congregate (Section 1.3(a)).
Many SUD service programs, especially harm reduction programs, are experiencing
significant barriers adapting to accommodate changing drug use patterns and
unprecedented surge of deaths from overdose, and to engage equitably with all
people who use drugs and in all manners of ways that people are using drugs. Much
of this is in due to paraphernalia laws that prohibit the distribution of drug
paraphernalia in any form. Amending this RCW would allow harm reduction programs
to provide drug testing equipment, including but not limited to fentanyl test strips,
and safer smoking equipment to engage and support people who use drugs without
risk of incurring a class I civil infraction.
See Appendix F.

25
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Treatment
The treatment subcommittee was developed out of the need for addressing
components of the plan directly related to treatment services and Medicaid, along
with private insurance. The treatment subcommittee focused on reviewing current
state processes and improving available engagement and treatment options to adapt
to the increased need. The subcommittee consisted of researchers, behavioral health
treatment providers, and subject matter experts to inform the recommendations
below. The subcommittee was able to address ideas and develop recommendations
that met various requirements outlined in Section 3. These recommendations meet
the following statutory requirements in RCW 71.24.546: (§3.a), (§3.b), (§3.c),(§3.d),
and (§3.e).
(1)“ (3) The plan must consider:
(a) The points of intersection that persons with substance use disorder have with the
health care, behavioral health, criminal, civil legal, and child welfare systems as well
as the various locations in which persons with untreated substance use disorder
congregate, including homeless encampments, motels, and casinos;
(b) New community-based care access points, including crisis stabilization services
and the safe station model in partnership with fire departments;
(c) Current regional capacity for substance use disorder assessments, including
capacity for persons with co-occurring substance use disorders and mental health
conditions, each of the American society of addiction medicine levels of care, and
recovery support services;
(d) Barriers to accessing the existing behavioral health system and recovery support
services for persons with untreated substance use disorder, especially indigent
youth and adult populations, persons with co-occurring substance use disorders
and mental health conditions, and populations chronically exposed to criminal legal
system responses, and possible innovations that could improve the quality and
accessibility of care for those populations;
(e) Evidence-based, research-based, and promising treatment and recovery
services appropriate for target populations, including persons with co-occurring
substance use disorders and mental health conditions;”
Below are the recommendations and outlined plans of action developed from the
treatment subcommittee and approved by the SURSA Committee.
SURSA Committee recommendations
Recommendation 7: Health engagement hubs for people who use drugs

26
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Health Engagement Hubs serve as an all-in-one location where people who use drugs
can access a range of medical, harm reduction, treatment, and social services.
Developing Health Engagement Hubs for people who use drugs considers and
supports several plan elements, including points of intersection that persons with
substance use disorder have with the health care system (RCW 71.24.546§3.a),
locations in which persons with untreated substance use disorder congregate (ibid),
new community-based care access points (RCW 71.24.546§3.b), and barriers to
accessing the existing behavioral health system (RCW 71.24.546§3.d). This
recommendation draws most immediately from a State Opioid and Overdose
Response Plan (SOORP) Goal 2.2.1 and expands upon work from the Center for
Community-Engaged Drug Education, Epidemiology and Research (CEDEER) at the
UW Addictions, Drug, & Alcohol Institute, including low barrier buprenorphine
programs and expressed needs/interests from program participants at Syringe
Services Programs (SSP).
The subcommittee proposes Health Engagement Hubs to be affiliated with an existing
SSP serving each community as well as other entities as appropriate, including
federally qualified health centers (FQHCs)/community health centers (CHCs), patient
centered medical homes, overdose prevention/safe consumption sites, peer run
organizations (e.g., Club Houses), services for unhoused people, supportive housing,
and opioid treatment programs. Harm reduction services and supplies must be an
integral program component of any organization housing a health hub.
Services should address each of the care domains below, with as comprehensive a
service mix as feasible:
• Comprehensive physical and behavioral health care
• Medical case management services/care coordination
• Harm reduction services and supplies
• Community health outreach workers/navigators, peers
• Linkage to housing, transportation, and other support services
• Spiritual Connection Communities
Health Engagement Hubs should encourage community volunteers, and provide
appropriate training to staff and volunteers, including diversity, equity, and inclusion
training. Services should be offered in coordination with every willing SSP.
Communities with a SSP may also offer services in other settings described above.
Communities without a SSP may provide services in another setting given they
institute a comprehensive harm reduction service and staffing continuum.
See Appendix H.

27
SUBSTANCE USE AND RECOVERY SERVICES PLAN
As part of the discussion surrounding the criminal legal response to possession of a
controlled substance, the SURSA Committee identified safe supply as a necessary
component to address diversion by providing safe resources for people who can
benefit from this type of harm reduction service. The treatment subcommittee
recommends assembling a statewide workgroup to make recommendations on a
framework for safe supply for future inclusion in the Washington State Substance Use
Recovery Services Plan. The workgroup would detail how the state may provide a
regulated, tested supply of controlled substances to individuals at risk of drug
overdoses. The workgroup should center the voices of people who use drugs, with
lived and living experience, and who have lost loved ones. This workgroup should
consider values of non-commercialization and alternative lawful income source for
people who have been trapped in the illicit distribution economy and could be
displaced by a safe supply program, to prevent potential unintended consequences
that would disadvantage communities most impacted.
The recommendation meets individuals at points of intersection that persons with
substance use disorder have with the health care system and locations in which
persons with untreated substance use disorder congregate (RCW 71.24.546§3.a). It
also addresses barriers to accessing the existing behavioral health system and
recovery support services for persons who use drugs and/or with untreated substance
use disorder, and possible innovations that could improve the quality and accessibility
of care for those populations (RCW 71.24.546§3.d) by using evidence-based,
research-based, and promising treatment and recovery services appropriate for
priority populations, including persons with co-occurring substance use disorders and
mental health conditions (RCW 71.24.546§3.e).
See Appendix O.
The recommendation that follows covers the component of the plan focused on low-
barrier, person-centered care which should be informed by people with lived and
living experience. This recommendation asks that:
o HCA convene a workgroup that will review current processes and
workforce needs related to intake, screening, and assessment for
substance use disorder (SUD) services
o HCA determine how to build an SUD engagement and measurement
process, including developing any necessary rules and payment
mechanisms
Recommendation 14: Safe supply workgroup
Recommendation 11: SUD engagement and measurement process

28
SUBSTANCE USE AND RECOVERY SERVICES PLAN
o HCA work with people who use drugs (PWUD), care providers, state
regulators, and payors to address this recommendation within 12
months
o In the interim, any work that HCA can undertake to advance these goals
should be done
Because SUD is chronic and potentially acutely life-threatening:
Initial engagement should be person centered and address the needs expressed by
the person seeking services. Current evaluations focus on complete and lengthy
assessments designed to determine the severity of a person’s substance use disorder
and the type of treatment setting best designed to meet their needs. Recognizing not
everyone will be ready for or interested in traditional treatment at the time of
engagement, Initial assessments should center on understanding and meeting the
persons self-identified needs, for example, food, shelter, harm reduction supplies,
recovery supports information or same day treatment if available, in the order that best
suits them. This approach also helps to build trust.
Access to timely SUD assessments varies widely across Washington State. In urban
areas, people seeking or needing an assessment may go to drop-in hours multiple
times over several weeks before they obtain an assessment. In rural areas there may
be a single provider currently allowed to do assessments and they may have a multi-
week wait list. Alternatively, in some care settings all that is needed to initiate care is an
SUD diagnosis (e.g., a medical clinic with a licensed prescribing provider onsite). The
Care for people with SUD needs to be accessible and initiated as quickly as
possible.
Care for people with SUD needs to be accessible in places and care settings
that are low-barrier/crisis-oriented (e.g., Health Hubs for people who use drugs
(PWUD), emergency departments, CHC/FQHC) in addition to care settings
such as withdrawal management and specialty SUD treatment.
The initial engagement and measurement process should be focused on what
is minimally necessary to document a diagnose, determine medical necessity
and start care the same day, and be conducted in less than 15 minutes.
Initial engagement and SUD measurement must be focused on, and limited to,
client’s needs and should be limited to only the necessary domains. Trauma
and culturally informed approaches must be taken in terms of the total time,
content, and process of engagement and measurement.

29
SUBSTANCE USE AND RECOVERY SERVICES PLAN
variable access to care by geography, provider types, and care settings is an example
of state and federal rules and regulations negatively impacting equitable access to
care.
See Appendix L.
The recommendation proposes expanding funding for opioid treatment programs
(OTP), to include mobile OTPs, into rural areas. As of September 1, 2022, there are 32
OTPs in Washington State, each serving between 200 to more than 1,000 patients.
There is no federal rule limiting the number of individuals an OTP can serve, but state
law in RCW 71.24.590(2) does allow counties to set patient census limits (i.e.,
maximum capacity for a program). OTPs in Washington State collectively serve more
than 14,000 people with a primary OUD diagnosis.
This recommendation establishes new community-based care access points (RCW
71.24.546§3.b), expands regional capacity for treatment via opioid treatment
programs (RCW 71.24.546§3.c), and removes geographic barriers to accessing OTPs
(RCW 71.24.546§3.d). Additionally, this recommendation aligns with the State Opioid
and Overdose Response Plan (SOORP) Strategy 2, establishing access to the full
continuum of care for person with opioid use disorder and Strategy 3, support and
increase capacity of opioid treatment programs.
Access to opioid treatment program (OTP) services in rural areas recommendation
includes:
Encourage the Department of Health’s Health Services Quality Assurance
(HSQA) division to create a regulatory workshop with OTP provider
stakeholders in 2023 to:
o Create state rules/regulatory process for OTP that want to establish
offsite medication units (1) located as a free-standing facility; (2) co-
located within in a variety of community settings such as but not limited
to hospitals/medical primary care systems/pharmacies/FQHCs, as well as
correctional health settings, etc.
Change RCW 36.70A.200 and WAC 365-196-550 to ensure that OTP branch
sites of all kinds (including mobile, and fixed, site medication units) are clearly
seen as “essential public facilities” and that they cannot be zoned out or stalled
by moratoriums by city and/or county legislative authorities.
Recommendation 15:
Expanding funding for OTPs to include partnerships with rural
30
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Update RCW 71.24.590 to remove several requirements for the siting of opioid
treatment programs that stigmatize the treatment setting type and subject
these treatment centers to a higher burden of regulations than other behavioral
health treatment settings.
Funding for capital construction costs to help start up OTP in Central and
Eastern Washington.
Funding to a state agency such as HCA for established OTPs in Washington
State to operate an increased number of OTP medication units in order to
expand their geographic reach.
See Appendix P.

31
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Recovery support services
As one of the first subcommittees generated from the SURSA Committee, the recovery
support services subcommittee was tasked with further developing recommendations
which populated out of the preliminary SURSA Committee meetings. The
subcommittee was able to address these initial ideas and develop more
recommendations that met the various requirements outlined in Section 3 of RCW
71.24.546. The recommendations below meet statutory requirements: (§3.a), (§3.b),
(§3.c),(§3.d), and (§3.e).
(1)“ (3) The plan must consider:
(a) The points of intersection that persons with substance use disorder have
with the health care, behavioral health, criminal, civil legal, and child welfare
systems as well as the various locations in which persons with untreated
substance use disorder congregate, including homeless encampments,
motels, and casinos;
(b) New community-based care access points, including crisis stabilization
services and the safe station model in partnership with fire departments;
(c) Current regional capacity for substance use disorder assessments,
including capacity for persons with co-occurring substance use disorders and
mental health conditions, each of the American society of addiction medicine
levels of care, and recovery support services;
(d) Barriers to accessing the existing behavioral health system and recovery
support services for persons with untreated substance use disorder, especially
indigent youth and adult populations, persons with co-occurring substance
use disorders and mental health conditions, and populations chronically
exposed to criminal legal system responses, and possible innovations that
could improve the quality and accessibility of care for those populations;
(e) Evidence-based, research-based, and promising treatment and recovery
services appropriate for target populations, including persons with co-
occurring substance use disorders and mental health conditions;”
Below are the recommendations and outlined plans of action developed from this
subcommittee and approved by the SURSA Committee.

32
SUBSTANCE USE AND RECOVERY SERVICES PLAN
SURSA Committee recommendations
This recommendation stemmed from the
need to continue recovery residential
operations that offer MOUD services
along with providing more housing
options in all areas of Washington. The
recommendation attempts to provide a
strategy to mitigate the current housing
market. The 2022 housing market consists
of homeowners and recovery residences
operators/owners finding it to be more
profitable to sell their homes rather than
continue to operate. The cost of real estate is working against the community and
supportive system for those who are seeking recovery services. Operators are shifting
out of recovery housing and selling their homes to capitalize on the current market.
The recommendation also addresses an approach for providing respite spaces for
individuals who return to use or are awaiting treatment services. Housing operators
would provide these spaces or create new residences to meet these individual’s
needs.
The recommendation outlines strategies to mitigate current markets while creating
new community care access point (§3.c), at points of intersect for individuals with SUD
(§3.a), using evidence-based, research-based, and promising treatment and recovery
services appropriate for target populations (§3.e).
The subcommittee proposes:
A property tax break for landlords to incentivize leasing their rental homes to
housing operators.
o Amending RCW 84.36.043: Nonprofit organization property used in
providing emergency or transitional housing to low-income homeless
persons or victims of domestic violence. (wa.gov), to include recovery
residences under the exemption that currently only provides
opportunities to transitional homes that house people for two years
or less.
A new voucher program would be ideal for experienced and accredited
housing operators to hold bedspace for individuals who are awaiting
appropriate treatment or who have returned to use and need a place to stay
while negotiating a return to stable housing.
Recommendation 1: Legislative policy for tax incentives and housing vouchers for
it

33
SUBSTANCE USE AND RECOVERY SERVICES PLAN
ESB 5476 established housing grants provided by the Department of Commence in
conjunction with the Health Care Authority. To receive this funding, housing providers
must meet national standards and accreditation of the Washington Alliance for Quality
Recovery Residences (WAQRR). Tribes are currently establishing relationships with
WAQRR to further expand housing options. The grant funding provided previously
should continue and give priority to tribes and rural areas for these grants.
See Appendix B.
The Health Care Authority and Department of Commerce should be intentional when
it comes to housing equity and inclusivity, and to the safety of LGBTQIA+ community
members. This recommendation addresses current disparities regarding this
population while drawing from intersections of people with substance use disorder
(§3.a), addresses barriers to accessing the existing behavioral health system and
recovery support services (§3.d), creates new community care access points (§3.c) by
using evidence-based, research-based, and promising treatment and recovery
services appropriate for target populations, including persons with co-occurring
substance use disorders and mental health conditions (§3.e). Currently, housing
providers have several individuals who apply and are accepted into housing that
identify with the LGBTQIA+ community, but there are no supportive policies or
training for operators to care for this population in a profound way.
Housing policy should be inclusive of LGBTQIA+ through state funded training for
housing providers and drug courts on how to service this community in an informed
and appropriate manner.
Harassment training
Communication
Antiracism training
Gender affirming/diversity training
Cultural competency training
A low-barrier grant program where funding is contingent on implementing
inclusionary policies operated through the Department of Commerce geared at
recovery-based housing in underserved and rural areas for priority populations. To
provide appropriate staffing,and operational considerations, housing operators and
managers could identify agencies already working with the LGBTQIA+ community to
help then design inclusive practices and policies. Smaller organizations/programs that
Recommendation 3: LGBQTIA+ community housing

34
SUBSTANCE USE AND RECOVERY SERVICES PLAN
are more experienced in this area could also be utilized to create focused funding
sources to established housing programs along with adding funds for newer
programs or smaller organizations to also get a chance to establish these housing
programs that may be more experienced in this realm. These grants can be focused
on youth and rural areas along with establishing long-term funding that is sustainable,
including capital funding and operational funds.
See Appendix D.
Numerous gaps exist in services for
foster care children. The
recommendation requests to provide
and enhance substance use training
and recovery support education,
creating a supportive environment for
children and transition age youth
(TAY), for foster and kinship guardians,
and caregivers of displaced youth.
Whenever possible, training and
resources should also include family of
origin, to support chances of reunification and continued recovery and support upon
return home. This recommendation provides a new intersection for people with
substance use disorder (§3.a), addresses barriers to accessing the existing behavioral
health system and recovery support services (§3.d), and creates a new community care
access point (§3.c) by using evidence-based, research-based, and promising
treatment and recovery services appropriate for target populations, including persons
with co-occurring substance use disorders and mental health conditions (§3.e).
This recommendation would be promoted by applying supportive policy to obtain
and provide naloxone to case workers, family of origin, foster/kinship families, and
young people who use substances. This would include training around administering
naloxone and identifying overdoses and addressing stigma through the provisions of
a public education campaign and easily accessible resources.
See Appendix E.
Recommendation 4: Training of foster, kinship and family or origin, parents with
children who use substances

35
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This recommendation addresses outdated language regarding recovery residence
licensing and zoning barriers affecting treatment, harm reduction, and recovery
services, as well as the inconsistency between state, county, and city/town regulations
regarding zoning for these types of facilities. Addressing outdated language
regarding recovery house licensing and zoning barriers affecting treatment, harm
reduction, and recovery support services helps reduce barriers to accessing the
existing behavioral health system and recovery support services (§3.d) and creates
new community care access point (§3.c). Additionally, this recommendation aligns
with State Opioid and Overdose Response Plan (SOORP) Goal 5, strategy 2,
increasing and improving access to recovery housing.
Currently, WAC 365-196-550 defines the types of public facilities considered essential
when it comes to community development regulations. The processes that a city or
county would use to identify and site these essential public facilities are outlined in
RCW 36.70A.200. Current RCW language lists ‘inpatient facilities, including substance
“abuse” facilities, mental health facilities, group homes, and secure community
transition facilities’ as essential. It is left to the discretion of the city and county to
identify and site these locations within their areas.
Oftentimes, cities and counties are not provided adequate services due to the lack of
appropriate identification and a clear description of the variety of services that are
needed to address the substance use, mental health, and co-occurring population.
The language should be updated to include inpatient, outpatient, recovery
residences, harm reduction services (including SSP), community-based and treatment
related programs, including OTPs and mobile treatment services. Furthermore, there
should be consistency, regardless of demographics, for forcing cities and counties to
provide the maximum number of services within their regions.
Recovery residences are not currently defined or referenced when it comes to
licensing and zoning purposes. A definition should be established and used that
reflects what a recovery residence provides, such as:
Recovery housing benefits individuals in recovery by reinforcing a substance-free lifestyle and
providing direct connections to other peers in recovery, mutual support groups and recovery
support services. Substance-free does not prohibit prescribed medications taken as directed
by a licensed prescriber, such as pharmacotherapies specifically approved by the Food and
Drug Administration (FDA) for treatment of opioid use disorder as well as other medications
with FDA-approved indications for the treatment of co-occurring disorder.
Recommendation 16: Addressing zoning issues regarding behavioral health services

36
SUBSTANCE USE AND RECOVERY SERVICES PLAN
To help facilitate the changes to zoning regulations, municipal and county officials
would benefit from orientation to the services recommended to be sited in their
jurisdictions. When given adequate information and statistical data, officials would be
better able to make informed changes to address the current substance use crisis.
Educational campaigns should be provided to cities, counties, and communities to
provide information regarding the services that may be sited in their areas. Stigma and
misunderstanding can cause resistance that could hinder the expansion of vital
services.
See Appendix Q.
Legal advocacy should be provided for parents and families, including kinship and
foster care families, that are affected by SUD in court cases regarding custody,
parenting plans, guardianship, and Child Protective Services (CPS) cases. The
following recommendation outlines various strategies on addressing this area of need.
There are no existing laws that allow for representation of parents and or guardians
involved in parenting plan and dissolution cases. This recommendation calls for
representation in family law cases, to those affected by substance use disorders,
mental health, and behavioral health concerns. Family Law could adopt similar
language and right to counsel in the Chapter 26.12 RCW series as they have in
Chapter 13.34. Currently the only families provided services in family law case are
American Indian/Alaska Native parents and children under RCW 13.38.110: Right to
Counsel. This recommendation proposes updating language in RCW 13.34.030, the
definition of indigent (b) to read: Individuals in need of or receiving mental health,
substance use, or behavioral health services.
The Washington State Office of Public Defense currently serves all counties for those
deemed indigent but additional services should be provided to assist therapeutic
courts such as the Family Treatment Court (FTC) to provide counsel and services to
families affected by SUD. Currently only 19 out of the 39 counties have an FTC or
juvenile/family court program. Providing legislative requirements for dependency
cases with those affected by substance use disorders, mental health, and behavioral
health would require counties to utilize OPD and FTCs across the state.
Alternative solutions include providing clinics with court staff or experienced
paralegals, connecting with community partners and peer navigators to include those
Recommendation 2: Legal advocacy for those affected by SUD

37
SUBSTANCE USE AND RECOVERY SERVICES PLAN
who navigate marginalized groups, to help parents navigate how to properly create
parenting plans and to teach individuals how to navigate family law or dependency
matters. Providing support for changes to parenting or reinstatement cases which
have reunification as the goal, keeps families together and allows children to have
rights to both their parents.
See Appendix C.
The recommendation
creates a grant program to
build and sustain
community-based
behavioral health
providers. The grant would
expand availability of these
types of programs with a
low-barrier, one-page
grant application, targeted
for programs that engage
with BIPOC and other
historically underserved
communities. There could also be individual grants or a scholarship-type program for
people in recovery housing that in addition to job training would provide forchildcare
expenses,, drivers licensing testing fees, transportation, along with any costs
associated with r the job training itself.
Regional and county-wide programs have been made available to individuals who are
seeking employment, education, training/certification, and other supportive
resources. Additionally, there are programs provided for incarcerated individuals to
seek and obtain employment upon release. In King County programs like Road Map
to Success, Orion Industries, and Post Prison Education Program have assisted people
in city, county, and tribal jails, as well as the Washington State Department of
Corrections. These programs include, welding certification, entrepreneurship,
construction-related work, and Commercial Driver Licenses, to name a few. Though
there are varied programs available to those with SUD, in recovery, incarcerated, or
being released from incarceration, there are still barriers. This recommendation would
work in conjunction with current measures outlined in the State Opioid and Overdose
Recommendation 8: Employment and education pathways

38
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Response Plan (SOORP) Goal 5, Strategy 1, increasing and improving access to
employment services for individuals in recovery, along with current state programs
that provide education and employment pathways.
In less dense areas, there are few resources and an all-around barrier to receiving a
livable wage. The stigma of substance use is also a barrier, making it difficult to obtain
employment. Programs like peer support and 0-1 intercept interventions should also
connect these individuals to needed resources. This recommendation includes
expanding efforts for incorporating incarcerated individuals and recently released
from incarceration into resources available through these programs.
See Appendix I.
The SURSA Committee asks the state to provide capital and operating funding to
support housing options at various points of intersection along the continuum of care,
to include housing people who use drugs, to those who are in recovery, which may or
may not include abstinence. This includes a request for funding to support immediate
shelter options to bridge or transitional housing through long-term permanent
housing. It is urgent that the Legislature fund a continuum of housing and housing
services for individuals who use drugs, and those who are abstinent, through capital
and operating investments.
This recommendation meets several considerations for the Substance Use Recovery
Services Plan including RCW 71.24.546§3(a), 3(b), and 3(e).
The SURSA Committee acknowledges and encourages ongoing participation in, and
collaboration with, initiatives, including but not limited to:
• Permanent Supportive Housing Advisory Committee, established per HB 1724
• Behavioral Health Housing Action Plan
• Washington State Health Care Authority
• Washington State Department of Health
• Washington State Department of Commerce
• Low Income Housing Institute
• The Washington Alliance for Quality Recovery Residences
• Oxford House
• Public Defender Association (PDA) CoLEAD/JustCARE
• Evergreen Treatment Services REACH Program
Recommendation 18: Continuum of housing

39
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Downtown Emergency Service Center
• Plymouth Housing
• Catholic Community Services
Continued participation and collaboration in this work should include supporting
evidence-based and promising models and systems for consideration.
We recommend that the work is centered on people who use substances and/or
experience mental health conditions who have lived/living experience with
homelessness and/or housing instability, such as:
• Individuals who encountered barriers in the shelter and homeless housing
systems due to active drug use or being in recovery from substance use
disorder
• Individuals who used shelter and/or homeless housing systems while actively
using drugs or working on their recovery
• Individuals with expertise designing and operating bridge housing or
temporary lodging for people with high barriers including current drug use
• Individuals with expertise bridging systems and designing systems to meet the
needs of historically under-served populations
• Individuals with knowledge of current state investments in homelessness
response
• Individuals with knowledge of Trueblood Settlement Agreement housing
investments
• Individuals with knowledge of Continuums of Care/Coordinated Entry in
homeless housing
See Appendix R.
It is vital to provide a tool that maps and directs individuals to community-based care
access points and helps locate and help those currently in need of outreach,
treatment, and recovery support services. This helps achieve the requirements that
intersect people with substance use disorder (§3.a) and address barriers to accessing
the existing behavioral health system and recovery support services (§3.d). By
expanding upon the current recovery readiness asset tool built from the Roadmap to
Recovery and the Washington Recovery Helpline, we can enhance the capabilities of
the tools available to reach more Washingtonians affected by SUD and their families.
Recommendation 9: Expansion of the Washington Recovery Helpline and asset
i

40
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This tool should also work in
conjunction with the E2SHB
1477 work to designate a
primary technology system to
provide “real-time bed
availability for all behavioral
health bed types, including but
not limited to crisis stabilization
services, triage facilities,
psychiatric inpatient, substance
use disorder inpatient,
withdrawal management, peer-
run respite centers, and crisis
respite services, inclusive of both voluntary and involuntary beds, for use by crisis
response workers, first responders, health care providers, emergency departments,
and individuals in crisis.”
Campaigning and advertising for the Washington Recovery Helpline is necessary for
educating the public on the helpline and tools, along with indicating its intent as
opposed to a crisis hotline. Along with additional resources for a heartier system, the
Washington Recovery Helpline will need full-time employees (FTEs) who are non-
clinical and have lived experience, to support expansion of work on the database and
to meet the growing demands. Substantial staffing will be needed to support a tool
dynamically.
See Appendix J.

41
SUBSTANCE USE AND RECOVERY SERVICES PLAN
ESB 5476 program updates
Recovery navigator program
RCW 71.24.546§3(h): “The design of recovery navigator programs (RNPs) in RCW
71.24.115, including reporting requirements by behavioral health administrative
services organizations to monitor the effectiveness of the programs and
recommendations for program improvement.”
Each behavioral health administrative services organization (BH-ASO) has established
a recovery navigator program. RNP is a pre-arrest diversion program which provides
community-based outreach, intake, brief assessment, and connection to services and,
as appropriate, long-term intensive case management and recovery coaching services,
to youth and adults with substance use disorder, including for people with co-
occurring substance use disorders and mental health conditions, who are referred to
the program from diverse sources and shall facilitate and coordinate connections to a
broad range of community resources for youth and adults with substance use
disorder, including treatment and recovery support services.
Table 6: Recovery Navigator Program Implementation by Region
Region
Implementation
Thurston-Mason
January 2022
Salish
Kitsap/Jefferson/Clallam
Clallam (PBH)
December 2021
Feb/March 2022
Spokane
Adams
Pend Orielle/ Ferry/
Lincoln/Stevens/Spokane
February 2022
March 2022
King
April 2022
Pierce
November 2021
Great Rivers
March/April 2022
Southwest December 2021
Greater Columbia
March 2022
North Sound
Feb/March 2022
North Central
Okanogan
Chelan/Douglas/Grant
December 2021
April 2022

42
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Peer-Run and clubhouse services expansion
HCA Clubhouse
Peer Run Program
received
additional funding
from State v. Blake
with the primary
focus of expanding
peer services to
areas lacking
programming to
address substance
use disorder
throughout
Washington State.
HCA achieved its
goal, providing
funding to an additional 11 peer run agencies. Per legislative directive, the program
was able to extend to into rural and Eastern Washington, including Chelan, Grays
Harbor, Cowlitz, Kittitas, Skamania, and Klickitat counties. There are innovative
expansion efforts by providers, including pop-up locations in frontier communities and
specific program services for marginalized and underserved populations. Recovery
Café of Clark County utilized the funding to establish three Pop-up Cafes currently
operating in Washougal, Stevenson, and Goldendale. Peer WA Olympia has
expanded services to rural areas by removing transportation barriers for access to
services at their Olympia location from Grays Harbor, Lewis, and Mason counties. The
Moore Wright Group opened a new Recovery Café in Aberdeen offering recovery
support and innovative online and in-person workforce development training.
Chai Rivers Recovery Café located rural Kelso in Cowlitz County, opened its doors in a
remote area lacking recovery programming. Caring with Compassion Community
joined as an HCA provider offering services for BIPOC, marginalized communities in
Graham in Pierce County. REBOOT Recovery helps veterans, first responders and all
families heal from trauma addressing the mental health and suicide epidemic though
peer-led services. Trilogy Recovery Center is engaging youth, adults and families
impacted by justice involvement with peer services.
Homeless outreach stabilization transition (HOST) expansion
HCA has expanded homeless outreach stabilization transition (HOST) programs with
the goal of expanding access to modified assertive community treatment delivered by
multi-disciplinary teams. HCA has contracted with North Sound BH-ASO, King BH-
Figure 3: Map of peer-run and clubhouse services
North Sound
North Central
Spokane
Greater Columbia
Great Rivers
Salish
Pierce
King
Soutwest
C
C
C
C
C
C
R
R
R
R
R
R
R
R
R
R
R
R
R
R
R
R
R
R
R
R
C
C

43
SUBSTANCE USE AND RECOVERY SERVICES PLAN
ASO, Thurston Mason BH-ASO, Beacon Health Options, and Spokane BH-ASO to
implement HOST teams in Snohomish, King, Pierce, Thurston, Clark, and Spokane
counties. The teams perform outreach and engagement to individuals who are living
with SUD and are experiencing lack of, or transitioning from, housing. HCA is also
contracting with Downtown Emergency Services Center (DESC) to provide
consultation and technical assistance on delivering this services model, and
establishing guidelines regarding team staffing types, service intensity, quality fidelity
standards, and metrics to verify programs are targeting the priority population.
Medication for opioid use disorder (MOUD) in jail
Through a combination of funding in ESB 5476 and ESSB 5092, HCA contracts with
local jails to ensure they meet the medication-based need of individuals with opioid
use disorder. HCA has finalized contracts with 19 separate city, county, and tribal jails
and using the funding to provide seamless access to medications for opioid use
disorder (MOUD). These MOUD in jails programs provide incarcerated individuals the
opportunity for an OUD assessment, evidence-based medication for OUD, sustained
treatment throughout incarceration, and connection to continue treatment upon
release or transfer. Overall benefits may include reduction in morbidity and mortality
due to overdose, reduced re-offenses, reduced complications during withdrawal,
improved jail staff safety, cost savings, reduced transfers to emergency departments,
custodial costs, and overall improved relationships.

44
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Contingency management
According to RCW 71.24.145 (3), “Subject to the availability of amounts appropriated
for this specific purpose, the authority shall increase contingency management
resources for opioid treatment networks that are serving people living with co-
occurring stimulant use and opioid use disorder.”
Contingency management is an evidence-based behavioral intervention for stimulant
use disorder. It provides incentives to individuals contingent upon objective evidence
of the target behavior, such as a negative urine drug test, to increase the likelihood of
these behaviors, which are essential components and outcomes of effective treatment.
Funding for contingency management was included in ESB 5476. Program managers
developed a contingency management intervention in the Opioid Treatment
Networks and Hub and Spokes. The State Hub and Spoke project completed their
contingency management trainings in September 2021 and are working with WSU
PRISM staff to implement their programs and engage in fidelity monitoring.
Short-term housing vouchers
Through appropriations in ESB 5476, HCA provided short-term housing vouchers for
people with substance use disorders. These housing vouchers were provided through
existing contracts with Housing and Recovery through Peer Services (HARPS)
providers and were used to support individuals who required short-term or transitional
housing and had a substance use disorder.
Substance use disorder (SUD) family navigators
The substance use disorder (SUD) family navigator project focuses on implementing
navigators who can serve families and individuals of loved ones experiencing SUD.
This program was expanded to three new sites that support parents, partners, and
other adult family members of youth and young adults experiencing SUD-related
challenges navigating systems of care. Services to adult family members are provided
by trained and certified family-support peers and include one-to-one peer coaching,
socialization, peer group support, education groups, employment support, supportive
housing, and referrals. The SUD navigators are trained to provide developmentally
appropriate services to individuals and families and assist them with navigating the
system in support of their loved one.

45
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Conclusion
Next steps
ESB 5476 outlines the next steps for the Authority to take regarding the plan. The
language states:
“After submitting the plan, the authority shall adopt rules and enter into
contracts with providers to implement the plan by December 1, 2023.”
To fulfill the bill requirements, HCA will prioritize implementing accessible policies and
contracts. Currently, there are no dedicated funds to immediately implement new
programs. HCA will work in collaboration with current efforts that intersect the criminal
legal system and behavioral health systems to connect the components proposed in
the plan. The SURSA Committee will continue to meet quarterly to be provided
updates and review the quarterly reports from the Recovery Navigator Program.
Constraints and limitations
The SURSA Committee has specified early on the need for more meaningful
approaches to the plan and the recommendations. Though RCW 71.24.546 required
that the SURSA Committee include people with lived experience, it was clear that
there was need for additional, dedicated space solely for individuals with lived or
living experience to participate. HCA will continue to include the community and
underrepresented populations in ongoing work around the SURSA Committee and
SURS Plan.
The time constraints surrounding the plan and development were very limited, leaving
little to no opportunities to seek community and subject matter expertise outside of
the SURSA Committee membership within the two-hour monthly meetings. This is
what ultimately led to the creation of the subcommittees and the openness of those
groups. Time continued to be a barrier within the plan development, leading to unmet
bill requirements.
One recommendation was deferred to be addressed at a later date. Unfortunately,
time was limited to attempt to address and adjust the recommendation brought forth
by the Outreach, Engagement, and Diversion subcommittee. This recommendation
requests an amendment to the Good Samaritan law for administering life-saving
medications to prevent death from an overdose.
See Appendix U.

46
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Unmet bill requirements
• (f) Options for leveraging existing integrated managed care, medicaid waiver,
American Indian or Alaska Native fee-for-service behavioral health benefits, and
private insurance service capacity for substance use disorders, including but not
limited to coordination with managed care organizations, behavioral health
administrative services organizations, the Washington health benefit exchange,
accountable communities of health, and the office of the insurance
commissioner.
o HCA acknowledges that existing committees, such as the Behavioral
Health System Coordination Committee, enacted in RCW 71.24.861,
meets the legislative intent above. For that reason, and others, priority
was given to recommendations by subcommittee chairs based on the
anticipated impacts in communities.
• (j) Strategic grant making to community organizations to promote public
understanding and eradicate stigma and prejudice against persons with
substance use disorder by promoting hope, empathy, and recovery.
o ESB 5476 did not include proviso funding to support development and
implementation strategy for a strategic grant program. The SURSA
Committee prioritized other immediate, achievable recommendations,
and could address any future efforts if funding were made available in
subsequent biennia.

47
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendices
Appendix A – Timeline
Table 9: Committee and subcommittee meeting dates
SUSRAC
Treatment
RSS
Data
OED
Deadlines
January 3
February 7
March 7
March 9 and
23
April 4
April 6 and 20
April 27
April 26
May 2
May 3, 17 and
31
May 4 and 18
May 25
May 10 and
24
June 6
June 14 and
28
June 1, 15
and 29
June 8 and
22
June 7 and
21
July 11
July 12 and 26
July 13 and 27
July 6 and
20
July 5 and 19
August 1
August 9 and
23
August 10
and 24
August 3,
17, and 31
August 2,
16, and 30
September
12
September 6
and 20
September 7
and 21
September
14 and 28
September
13 and 27
October 3
October 4
October 5
October 11
October 13
October 11– Final
Recommendations
November
7
December
5
December 1 –
Plan Submission
to LEG

48
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix B – Recommendation 1: Legislative policy for tax incentives and housing vouchers for
respite spaces
Recommendation – Legislative policy recommendation for replicating and enhancing “good work”, tax
incentives for recovery housing services, and housing vouchers for those homes.
Bill requirement: Section 1(3)(c), (d), (e)
Synopsis – The suggestion was made for helping private locations with state or funding support such as
capital funding to help establish recovery residences. HCA shared that a potential capital loan program that
may be coming up later in the year or next year specifically for recovery residences. New recovery residence
operating funds will be open for competitive application by mid-May, more details to come as this
opportunity becomes available. There are a few factors that can hinder growth in this area including the
overall cost of housing. The cost of real estate is working against the community. Some people are getting
out of recovery housing and selling their houses to capitalize on the current market.
The Legislature works with a lot of housing programs. A property tax break for landlords to
incentivize leasing their rental homes to housing operators.
Incentivizing HUD owned homes to turn into recovery residences and matching homes with
recovery residence operators.
Low-Income Housing Institute invest in those who already own or want to invest in, or start
programing, they can help manage different programs. https://lihi.org/
Local jurisdictions sometimes sell properties to use for low-income housing. If this can happen in
an organized manner to increase the number of recovery residences, these homes would need to
be matched with recovery residence operators.
Rural communities could work together in partnerships with HCA staff to assess local needs and
seek funding to expand recovery residence capacity.
Currently there are a limited number of categories for property tax exemption. An operator can
qualify for a property tax break for emergency transitional housing, where the operator can apply
and the landlord benefits from exemption. To qualify, an operator must enforce a cap on resident
stay which is currently 2 years. This recommendation would be to add a specific category to the
exemption list to include accredited recovery residences.
o WAC 458-16-165:
o RCW 84.36.043: Nonprofit organization property used in providing emergency or
transitional housing to low-income homeless persons or victims of domestic violence.
(wa.gov)
o WAC 458-16-320:
Plan of Action:
A new voucher program would be ideal for experienced and accredited housing operators to hold
bedspace for individuals who are awaiting appropriate treatment or who have returned to use
and need a place to stay while negotiating a return to stable housing.
o Temporary secure housing would fill the large gap in the continuum of care for
individuals seeking appropriate treatment—many are overlooked and are left without
treatment.
o A weekly voucher should be made available to hold a bed in a staffed and accredited
recovery residence for those who are awaiting treatment or return to use. Vouchers

49
SUBSTANCE USE AND RECOVERY SERVICES PLAN
should be used to support these dedicated spaces whether the beds are filled or not
(Some Drug Courts currently fund spaces for participants whether the beds are filled or
not.)
o Creating a more rapid response by providing respite spaces to be made available in a
recovery residence for those who return to use, don’t qualify for detox, or seeking
treatment and need a safe place to stay by creating a new or existing arrangement for
operators for short term stays with quick turnaround times.
Different types of facilities receive property tax breaks. Recovery residences could be added to
the list in the RCWs. Exemptions are currently only allowed for transitional homes that house
people for two years or less. A change in the current law would provide a property tax exemption
for residences that do not limit residents’ length of stay. The exemption could be claimed by a
homeowner whether they operate a recovery residence themselves or rent to an accredited
operator.
Continuing and expanding the COM/HCA housing grants provided out of 5476.
Subcontracted training that providers can go through, by HCA, from people that meet national
standards (WAQRR) then they would be eligible and accredited.
Financial Impact:
Dollars
FY23
FY24
FY25
5476 Funding
$200,000/Housing
Vouchers
525,000/Housing
Grants
$200,000/Housing
Vouchers
525,000/Housing
Grants
$200,000/Housing
Vouchers
525,000/Housing
Grants
Grant Funding
Grants (Commerce
currently is offering
$1,000,000 in
housing expansion
grants for fiscal year
2022-23.
Total Funds
Staff (FTE)
0
0
0
Consideration of youth, rural areas, and tribes:
Youth:
Additional programs will be brought up specifically for youth in this realm later.
Rural Areas:
5476 can support communities to provide regional specific recommendations to develop a response that
works for them. Incentivizing with policies but to also enforce the same policies in rural areas. Giving
priority to tribes and rural areas for the continuation of grants.
Tribes:
50
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Tribes are having conversations with WAQRR. Oxford has a few housings on tribal lands and off the
reservation specific to tribes. Tribes will retain their rights to select their providers that they work with.
Giving priority to tribes and rural areas for the continuation of grants.
Collaboration/Existing Programs:
5476 provided 7 grants of $75,000 to recovery residences in 2021-22 and will make $1,000,000 in grants
in 2022-23.
SURSA Committee feedback
No feedback on the content of the recommendation was provided from SURSAC members during the pre-
meeting review period.
51
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix C – Recommendation 2: Legal advocacy for those affected by SUD
Recommendation – Legal Advocacy for parents and families, including kinship and foster care families,
that are affected by SUD in court cases regarding custody, parenting plans, guardianship, and CPS cases.
Bill Requirement(s) –5476 Section 1.3 (a), Section 4.3(f)and(i)
Background and Supporting Data:
When an individual enters the criminal legal system, there are a number of granted resources made
available but when it comes to family court there are very limited resources. There are resources currently
available including the Office of Public Defense Parents Representation Program, The First Clinic , and
Family Treatment Court.
Dependency Cases:
Proposal of updating language in RCW 13.34.030, definition of indigent (b) to read:
Individuals in need of or receiving mental health, substance use, or behavioral health services.
Updating this language would modify RCW 13.34.090, providing appointed counsel by the court
for dependency and termination of parent-child relationship cases.
The Office of the Public Defenders currently serves all counties for those deemed indigent but
additional services should be provided to assist therapeutic courts such as the Family Treatment
Court to provide counsel and services to those familied affected by SUD. Creating FTCs is possible,
King County started by a federal SAMHSA grant and then scaled in size over the years with more
sustainability grants and county funding. Counties without FTC could utilize this possible framework
but would need to have numbers to support it, such as filing numbers, filings due to substance use
disorder, etc. and scale a foundation based upon how big the FTC initially needs to be. 1/10th
percent sales tax can then go towards supporting behavioral health treatment services, as well as
sustaining an FTC. Family Treatment Courts are modeled after drug courts and veterans’ courts,
aiding parents in regaining control of their lives and promote long-term, stabilized recovery.
Currently only 19 out of the 39 counties have an FTC or juvenile/family court program of this
nature. Providing legislative requirements for dependency cases with those affected by substance
use disorders, mental health, and behavioral health would require counties to utilize OPD and FTCs
across the state. Supplementing counties with contracts with programs such as The First Clinic to
provide support until programs are established. Working with courts to providing clinics to help
parents navigate how to properly navigate dependency matters.
Providing support for reunification cases to have reunification as the end goal or more access to
children and visitation.
Family Court:
There are no existing laws that allows for representation for parents and or guardians involved in
parenting plan and dissolution cases. This recommendation calls for representation in family law
cases, to those affected by substance use disorders, mental health, and behavioral health concerns.

52
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This recommendation request asks for the Family Law Board to work in conjunction with the Office
of the Public Defenders to provide legal representation for primary residential parent and
nonprimary residential parents(noncustodial) in parenting plan and custodial cases. Family Law
could adopt similar language and right to counsel in the Chapter 26.12 RCW series as they have in
Chapter 13.34. Currently the only families provided this service in family law case are American
Indian / Alaska Native parents and children under RCW 13.38.110: Right to counsel.
Providing clinics to have court staff or experienced paralegals, connecting with community partners
and peer navigators to include those who navigate marginalized groups,to help parents navigate
how to properly create parenting plans and to teach individuals how to navigate the family law or
dependency matters. Providing support for changing to parenting or reinstatement cases to have
reunification as the end goal and the children to have rights to both their parents.
There are situations which would require further analysis, such as one parent who does have SUD
and another who does not, so what would be the determining factor(s) for representation?
Concerns and Considerations –
- Considerations should consider building recommendation in conjunction with housing and housing
requirements. For example, there is nothing that states that a parent cannot live with their child in
a car or RV, yet those facts often are used against them.
- There is a lot of system struggle with the treatment world, and it has been decimated because
specialists are not given livable wages. Funding is primarily going into legal counsel and there
needs to be some form of scale or rubric to determine monetary need for legal representation.
- At any given time, the OPD Parent Representation Program services roughly 9,000 parents and the
program costs about $26 million annually. Family Law would most likely be much bigger than this.
- A statement was made that further enriching courts would not help parents that need legal
representation. A suggestion was made to look further into a decriminalization framework so that
issues surrounding SUD do not get to become a legal issue for parents involved in FTC.
- Changing the definition of ‘indigent’ will also prove difficult and there was concern as to whether
definition changes can be done via SURSAC work.
o There is currently another subcommittee looking at changes to the drug paraphernalia
law. Additionally, the Blake Bill calls for legal advocacy and recovery support services.
- The point was made that it is crucial to be clear in the definition of ‘indigent’ and within legal
language because family law and dependency involvement are different services.
o The recommendation will also need to expand upon the different services that would be
allotted for family law and for dependency matters.
o The recommendation was created on the basis that there are services available to
individuals who are CPS involved or who have dependency matters, however, there are no
services for non-custodial parents that are not involved with these programs.
- Concern regarding the broadness of the definition of indigent, should be directed to those that
demonstrate the need for representation.
Collaboration with Existing Resources:
• The Court Improvement Program of the state Administrative Office of the Courts was awarded a $1.75
million grant to strengthen and expand the provision of Family Treatment Court (FTC) services in
Washington. The grant was provided through the Department of Justice and integrated a coordinated

53
SUBSTANCE USE AND RECOVERY SERVICES PLAN
effort in partnership with the state Department of Children, Youth and Families (DCYF) and the state
Health Care Authority (HCA) to assist those families affected by substance use disorders.
Approximate Financial Support and Staffing Needed:
Dollars
FY23
FY24
FY25
Legislative / State Budget
Funding
$2.0 M / Expansion
of FTC to all counties
$3.75 M FTC
Funding
$3.75 M FTC
Funding
HCA Grant-Based Funding
Total Funds
Staff (FTE)
0
0
0
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

54
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix D – Recommendation 3: LGBQTIA+ community housing
Recommendation –LBGTQIA+ housing options and policy changes.
Bill requirement: Section 1(3)(a), (c), (d), (e)
Plan of Action:
Policy from Drug Court to identify individuals of the LGBTQIA+ community.
Housing policy to be inclusive of LGBTQIA+
o State funded training for housing providers on how to service this community in an
informed and appropriate manner. A mandatory training annually for those who have
direct contact with residents. This training should incorporate a multifaceted approach
including:
Harassment Training
Communication
Antiracism training
Gender affirming/diversity training
Cultural competency training
These models and training should be provided top down from the director and board to
the staff.
• Staff should also identify with the LGBTQIA+ community.
o Incorporating community members to help inform the training and policies.
Synopsis – Housing providers have several individuals who apply and are accepted into housing that they
identify with. At times, housing providers could also place individuals into single rooms for privacy
purposes. This group must be intentional when it comes to housing, and to the safety of community
members. Addressing LGBTQIA+ housing options requires more input and representation from the
community. There is a lack of affordable housing or recovery housing in rural areas. Develop housing
operator training that is culturally and linguistically inclusive and representative of this population.
Organizations invited to participate in this discussion:
o Trans Women of Color Solidarity Network
o Utopia
o Mockingbird Society – Keeping Kids in Kent
o Lambert House in Seattle was given as an example of place that supports marginalized
communities.
o Disability Rights Washington
o POCAAN
o Asian Counseling Referral Services
o Creative Justice
o Lavender Rights Project
A low-barrier grant program operated through Department of Commerce geared at recovery-
based housing in underserved and rural areas for priority populations where funding is
contingent on implementing inclusionary policies.

55
SUBSTANCE USE AND RECOVERY SERVICES PLAN
o Smaller organizations/programs that are more experienced in this area. Can utilize these
groups to share the funding component to create focused funding sources to established
housing programs along with adding funds for newer programs or smaller organizations
to also get a chance to establish these housing programs that may be more experienced
in this realm.
o Grants can be focused on youth and rural areas as part of this recommendation.
Make sure that long term funding is sustainable, something like revolving funds for other
recovery housing.
Expand the definition of Fair housing and allow more people to be housing providers.
Financial Impact:
Dollars
FY23
FY24
FY25
5476 Funding
$525,000/ Adult
Housing Grants
$525,000/ Youth
Housing Grants
$60,000/ Training
$525,000/ Adult
Housing Grants
$525,000/ Youth
Housing Grants
$60,000/ Training
$525,000/ Adult
Housing Grants
$525,000/ Youth
Housing Grants
$60,000/ Training
Grant Funding
Total Funds
$1,110,000
$1,110,000
$1,110,000
Staff (FTE)
Consideration of youth, rural areas, and tribes:
Youth: Grants in this recommendation are not only focused on adult housing but also youth housing.
Rural Areas: Rural areas will be prioritized for providing these grants.
Marginalized Communities: This recommendation is specifically focused on marginalized communities in
Washington that identity as part of the LGBTQIA+ community as well as focusing on rural areas and youth
programs.
Collaboration/Existing Programs:
COM and HCA have existing housing grants through 5476, this recommendation would be an expansion
of these grants to focus on the LGBTQIA+ community in Washington.
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

56
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix E – Recommendation 4: Training of foster and kinship parents with children who use
substances
Recommendation –Funding for training of case workers and kinship caregivers/ foster parents with
children with SUD. Along with providing equal resources to family of origin.
Bill requirement: Section 1(3)(a), (c), (d), (e)
Plan of Action:
Supportive policy to obtain and provide naloxone for case workers and foster/kinship families
along with young people who use substances to be supplied naloxone. This would include training
around administering naloxone and identifying overdoses.
o Currently, DCYF has no formal policy around carrying and administering naloxone. DCYF is
forming a workgroup to address the issue. DCYF has also consulted the Department of
Health and reviewing trainings on naloxone.
Provide/enhance SUD training and recovery support education, creating a supportive
environment (CRAFT model, or other EBP) for children and Transition Age Youth (TAY) for foster
and kinship guardians, caregivers of displaced youth. The Safety First Curriculum by Drug Policy
Alliance is designed for high school aged youth. Foster families have to go through so many hours
for training, policy change recognizing SUD, how to recognize and treat an overdose, and what is
recovery with an option to have training in trauma informed approach and developing support
groups.
Providing parity for family of origin as well.
o Incorporate behavioral health training, including suicide prevention.
Including addressing stigma by public education campaign than actual messaging about naloxone
itself.
Financial Impact:
Dollars
FY23
FY24
FY25
Synopsis –
• Numerous gaps that can exist in services for foster care children.
• The recommendation to provide/enhance substance use and SUD training and recovery support
education, creating a supportive environment (CRAFT model, or other EBP) for children and TAY
for foster and kinship guardians, caregivers of displaced youth.
• There is a concern that young people who use substances are being criminalized.
• There is a lack of supportive services for youth seeking recovery.
• Would like to include kinship care in training, wrap around services, and other benefits that foster
care families acquire.
• Would also include servicing transition age youth not only with SU concerns but mental health as
well.
• Should include other organizations in the discussion aside from DCYF, Community Youth Services
and A Way Home Washington were suggested, along with those with lived experiences.
•
Would like to hear from foster families that may be able to share gaps in the system.

57
SUBSTANCE USE AND RECOVERY SERVICES PLAN
5476 Funding
$120,000 Training
Development/Trainings
$1M Education Campaign
$1.2M Naloxone/ Foster-Kin-
Case Managers *
$40,000 Training
$1.2M Naloxone/
Foster-Kin-Case
Managers *
$40,000 Training
$1.2M Naloxone/
Foster-Kin-Case
Managers *
Grant Funding
Total Funds
$2,320,000
$1,240,000
$1,240,000
Staff (FTE)
*Based on taking data from Data from the KIDS COUNT data center and from Adoption and Foster Care
Analysis 2020 and providing kits for 20% of this population.
Consideration of youth, rural areas, and tribes:
Youth: This recommendation is focused on youth and foster/kinship individuals and families affected by
SUD and drug use.
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

58
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix F – Recommendation 5: Amend RCW 69.50, 4121 – Drug paraphernalia law
Recommendation – Amend RCW 69.50.4121 to remove language that prohibits “giving” or “permitting to
give” drug paraphernalia in any form, so that programs who serve people who use drugs do not risk class I
civil infraction charges for providing life-saving supplies needed for comprehensive drug checking, safer
smoking equipment, and other harm reduction supplies to engage and support people who use drugs. The
state shall expressively preempt the field in Washington state regarding any penalties imposed for
selling/giving paraphernalia per RCW 69.50.4121.
Bill requirement: This amendment will support low barrier, person centered outreach and treatment
services that improve safety for people who use drugs (Section 1.1); it also considers the points of
intersection that persons with substance use disorder have with behavioral health systems and the places
where persons with untreated substance use disorder congregate (Section 1.3(a)).
Is this a contract request, state plan amendment, funding request, or legislative policy change?
Legislative Policy Change
Synopsis
Many SUD service programs, especially harm reduction programs, are experiencing significant barriers
adapting to accommodate changing drug use patterns and unprecedented surge of deaths from overdose,
and to engage equitably with all people who use drugs and in all manners of ways that people are using
drugs. Much of this is in due to paraphernalia laws that prohibit the distribution of drug paraphernalia in
any form. Amending this law would allow harm reduction programs to provide drug testing equipment,
including but not limited to fentanyl test strips, and safer smoking equipment to engage and support
people who use drugs without risk of incurring a class I civil infraction.
A significant service of harm reduction programs is to also connect people who use drugs with additional
services that are aligned with their recovery. Therefore, it is essential that supplies that engage with
people who use drugs in a variety of ways are allowed for distribution.
Recent reports suggest a drastic shift in drug use patterns in Washington State. Emerging research related
to the changing West Coast drug supply, survey information from SSP participants in Washington collected
by University of Washington researchers, and anecdotal information from Washington-based SSPs
indicate that the ubiquity of fentanyl in the street drug supply is causing many people who inject drugs to
transition to smoking fentanyl, primarily due to difficulties finding accessible veins
6
and their inability to
find heroin. In addition, many people who use drugs report stimulant use, and most often report smoking
as the primary mode of administration for drugs like methamphetamine.
7
Supportive Research
6
Alex H. Kral, Barrot H. Lambdin, Erica N. Browne, Lynn D. Wenger, Ricky N. Bluthenthal, Jon E. Zibbell, Peter J. Davidson, Transition from
injecting opioids to smoking fentanyl in San Francisco, California,Drug and Alcohol Dependence,Volume 227,2021,109003,ISSN 0376-
8716,https://doi.org/10.1016/j.drugalcdep.2021.109003.
7
Kingston S, Newman A, Banta-Green C, Glick S. Results from the 2021 WA State Syringe Service Program Health Survey. Seattle, WA:
Addictions, Drug & Alcohol Institute, Department of Psychiatry & Behavioral Sciences, University of Washington, March 2022.
https://adai.uw.edu/syringe-survey-2021.

59
SUBSTANCE USE AND RECOVERY SERVICES PLAN
•
Non-Injection Routes of Drug Administration are Less Dangerous than Injection:
Injecting more
frequently is associated with a greater risk of blood-borne pathogen transmission.
8
A person’s overall
drug-related risk is lowered every time they choose to smoke instead of inject. Studies have found that
participants who inject drugs are often willing to switch to smoking or other modes of administration
when feasible
9,10
and that non-injection routes of administration may pose less risk of overdose.
11,12
Many of the harms of injection drug use, such as endocarditis, skin infections, and vein damage, are
injection-specific.
13
In addition to being harmful to individual health, endocarditis, HIV, and HCV are
expensive to treat, and place a considerable economic burden on the public health and health care
systems.
14,15
•
Sharing Smoking or Snorting Supplies May Transmit Communicable and Infectious Disease:
HCV has
been found on used pipes,
16
and sharing non-injection drug using equipment is associated with HCV
infection.
17
Pipe sharing has also been implicated in outbreaks of other diseases, such as
tuberculosis.
18,19
As with the risk of other respiratory infections, access to non-injection drug use
materials may reduce sharing and the consequent risk of COVID-19 infection: while not yet studied
with regard to illicit drugs, the sharing of tobacco cigarettes could be implicated in COVID-19
transmission through salivary droplets.
20
•
People who Smoke Drugs Need Engagement and Access to Harm Reduction Services
Making pipes and
other non-injection drug using supplies available can serve as an engagement strategy and bring harm
reduction services to people who use drugs, but do not inject. There is a marked decrease of reported
8
Thorpe LE, Ouellet LJ, Levy JR, Williams IT, Monterroso ER. Hepatitis C virus infection: prevalence, risk factors, and prevention opportunities
among young injection drug users in Chicago, 1997-1999. J Infect Dis. 2000;182:1588–1594. doi: 10.1086/317607
9
Schaeffer, D., Stoever, S., and Weichert, L. (2014), Drug consumption rooms in Europe: Models, best practice and challenges, European Harm
Reduction Network <https://www.aidshilfe.de/sites/default/files/documents/Drug%20consumption%20in%20Europe.pdf>
10
Leonard L, DeRubeis E, Pelude L, Medd E, Birkett N, Seto J. "I inject less as I have easier access to pipes": injecting, and sharing of crack-
smoking materials, decline as safer crack-smoking resources are distributed. Int J Drug Policy. 2008 Jun;19(3):255-64. doi:
10.1016/j.drugpo.2007.02.008.
11
Darke, S. and Ross, J. (2000), Fatal heroin overdoses resulting from non-injecting routes of administration, NSW, Australia, 1992–1996.
Addiction, 95: 569-573. doi:10.1046/j.1360-0443.2000.9545698.x
12
Kaye S, Darke S. Non-fatal cocaine overdose among injecting and non-injecting cocaine users in Sydney, Australia. Addiction. 2004
Oct;99(10):1315-22. PubMed PMID: 15369570.
13
Jennifer A. Frontera, Jeremy D. Gradon; Right-Side Endocarditis in Injection Drug Users: Review of Proposed Mechanisms of
Pathogenesis, Clinical Infectious Diseases, Volume 30, Issue 2, 1 February 2000, Pages 374–379, https://doi.org/10.1086/313664
14
Fleischauer AT, Ruhl L, Rhea S, Barnes E. Hospitalizations for Endocarditis and Associated Health Care Costs Among Persons with Diagnosed
Drug Dependence — North Carolina, 2010–2015. MMWR Morb Mortal Wkly Rep 2017;66:569–573.
DOI: http://dx.doi.org/10.15585/mmwr.mm6622a1.
15
Tookes, H., Diaz, C., Li, H., Khalid, R., & Doblecki-Lewis, S. (2015). A Cost Analysis of Hospitalizations for Infections Related to Injection Drug
Use at a County Safety-Net Hospital in Miami, Florida. PLoS ONE, 10(6), e0129360. http://doi.org/10.1371/journal.pone.0129360
16
Fischer B, Powis J, Cruz MF, Rudzinski K, Rehm J. Hepatitis C virus transmission among oral crack users: viral detection on crack
paraphernalia. Eur J Gastroenterol Hepatol. 2008;20:29–32. doi: 10.1097/MEG.0b013e3282f16a8c.
17
Tortu, S., McMahon, J., Pouget, E., and Hamid, R. (2004), Sharing of Noninjection Drug-Use Implements as a Risk Factor for Hepatitis C,
Substance Use and Misuse 39,2:211-224.
18
Gardy JL, Johnston JC, Ho Sui SJ, Cook VJ, Shah L, Brodkin E, Rempel S, Moore R, Zhao Y, Holt R, Varhol R, Birol I, Lem M, Sharma MK, Elwood
K, Jones SJ, Brinkman FS, Brunham RC, Tang P.
N Engl J Med. 2011 Feb 24;364(8):730-9. doi: 10.1056/NEJMoa1003176. Erratum in: N Engl J Med. 2011 Jun 2;364(22):2174.
19
Andrea A. Howard, Robert S. Klein, Ellie E. Schoenbaum, Marc N. Gourevitch; Crack Cocaine Use and Other Risk Factors for Tuberculin
Positivity in Drug Users, Clinical Infectious Diseases, Volume 35, Issue 10, 15 November 2002, Pages 1183–
1190, https://doi.org/10.1086/343827
20
Ahmed N, Maqsood A, Abduljabbar T, Vohra F. (2020). Tobacco Smoking a Potential Risk Factor in Transmission of COVID-19 Infection. Pak J
Med Sci, 36(COVID19-S4):S104-S107

60
SUBSTANCE USE AND RECOVERY SERVICES PLAN
drug-related health problems among people who obtain new pipes through SSPs
21
and SSPs serve as a
point of entry to other services, including access to overdose education and naloxone, infectious
disease testing (e.g., HIV, HCV, and syphilis), linkage to care, primary care, and recovery support and
treatment services.
22
•
Opioid and Psychostimulant Overdose are a Public Health Crisis Requiring Innovative Approaches
Per
provisional DOH overdose surveillance data, drug-related overdose deaths surpassed 2,000 in 2021, a
more than 66 percent increase compared to 2019. In 2019, the number of overdose deaths involving a
synthetic opioid (mostly fentanyl and fentanyl analogs) was 337; in 2020 there were 672 (an increase
of 99%), and preliminary 2021 data has this number as 1181 (a 250% increase from 2019). In addition,
psychostimulant and polydrug overdose are on the rise: in 2019, the number of overdose deaths
involving a psychostimulant was 540; in 2020, there were 728 (an increase of 35%), and preliminary
2021 data counts 1,112 (a 105% increase from 2019). In 2021, overdose deaths in Washington
disproportionately affected people 45 years of age and younger, and Black, Indigenous/Native
American/Alaska Native, and Hispanic/Latino/Latina/Latinx communities. Increases in overdose
deaths demonstrate the need to expand services to engage all people who use drugs, and particularly
people from disparately impacted communities, in overdose prevention and naloxone distribution, as
well as linkages to health and social services.
•
Syringe exchange program participants are more likely to reduce or end use of injection drugs and to
remain in treatment
: A study published in the Journal of Substance Abuse Treatment in 2000
23
found
that injection drug users who had formerly been exchange users were more likely than never-
exchangers to report a substantial reduction in injection, to stop injecting altogether, and to remain in
drug treatment. New users of the exchange were five times more likely to enter drug treatment than
never-exchangers. The researchers concluded that reduced drug use and increased drug treatment
enrollment associated with needle exchange participation may have many public health benefits,
including prevention of blood-borne viral transmission.
•
Needle exchange programs are a bridge to treatment
: Another study, published in the Journal of
Urban Health: Bulletin of the New York Academy of Medicine, assessed the role of needle-exchange
programs (NEPs) as a bridge to treatment
24
. Researchers found that needle-exchange attendance was
associated independently with entering detoxification for both HIV-infected and uninfected injection
drug users.
21 Prangnell, A., Dong, H., Daly, P., Milloy, M. J., Kerr, T., & Hayashi, K. (2017). Declining rates of health problems associated with crack smoking
during the expansion of crack pipe distribution in Vancouver, Canada. BMC Public Health, 17, 163. http://doi.org/10.1186/s12889-017-4099-9
22 Fischer B, Rehm J, Patra J, Kalousek K, Haydon E, Tyndall M, El-Guebaly N. (2006) Addiction. Dec;101(12):1760-70.
23
Holly Hagan, MPH, PhD., et al., “Reduced injection frequency and increased entry and retention in drug
treatment associated with needle-exchange participation in Seattle drug injectors,” Journal of Substance Abuse
Treatment, Volume 19, Issue 3 (2000), pgs 247-252
24
Stephanie A. Strathdee, et al., “Needle-exchange attendance and health care utilization promote entry into
detoxification,” Journal of Urban Health: Bulletin of the New York Academy of Medicine, Vol 76, Number 4 (1999).

61
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Financial Impact:
Dollars
FY23
FY24
FY25
5476 Funding
N/A
N/A
N/A
Grant Funding
N/A
N/A
N/A
Total Funds
N/A
N/A
N/A
Staff (FTE)
0
0
0
Consideration of youth, rural areas, and tribes:
Youth: Youth are dying from drug use at higher rates than they ever have (although rates of drug use
itself has not necessarily increased) This recommendation should consider and allow programs to legally
provide supplies to people 18 and younger.
Rural Areas: It is becoming increasingly difficult in rural areas to engage those most at risk of overdose
with limited supplies allowed. Traditional harm reduction services are not accommodating the needs of
people at risk of overdose, and the ability to distribute harm reduction supplies would strengthen
programs’ ability to engage and support these rural communities. When transportation to services is
difficult – such as in rural areas –receiving drug checking supplies, etc., serve as the necessary incentive
for engagement. Due to limited resources and treatment options in rural areas, harm reduction may be
the only option for some people who use drugs to receive support services that improve their health,
safety, and wellbeing.
Tribes: American Indian/Alaska Native people in Washington State have disproportionately high rates of
fatal overdoses and experience higher rates of stigma when accessing conventional services. Expanding
access to and engagement with harm reduction services is critical and necessary to improve the health
and save the lives of AIAN people in Washington.
Collaboration/Existing Programs:
RCW 69.50.4121: Drug paraphernalia—Selling or giving—Penalty. (wa.gov)
(3)
Nothing in subsection (1)
of this section prohibits legal distribution of injection syringe equipment through public health and
community based HIV prevention programs, and pharmacies.
RCW 69.50.4121 (3) is a technical
amendment which allows certain entities to distribute syringe injection equipment – an additional
technical amendment would impact all programs/individuals engaging to support the health of people
who use drugs.
WA HCA contracted with ADAI to implement community drug checking services at harm reduction sites
across WA. The project includes the use of fentanyl and benzodiazepine test strips and Fourier
Transformation Infrared Spectroscopy chemical analysis. It is expected that these services will encourage
the participation of new clients, including those who smoke drugs who did not previously attend syringe
services programs. In turn some harm reduction programs may wish to expand their supplies to include
safer smoking equipment.
SURSA Committee feedback

62
SUBSTANCE USE AND RECOVERY SERVICES PLAN
2022 King County medical examiner data suggest a substantial proportion of people dying from drug
overdoses involving fentanyl smoked their drugs, a major shift from heroin in previous years which was
predominantly injected. Data from William Barbour in the KCME office via Caleb Banta-Green. These are
214 deaths from 1/1/22-7/13/22 from data provided on 7/14/22.
The Tacoma Needle Exchange (TNE) reported seeing hundreds of new clients when they began offering
safer smoking equipment/pipes. From the ADAI report with data provided by Paul LaKosky from TNE:
The Tacoma Needle Exchange launched a pilot project to distribute smoking supplies at one of their sites
in December 2020. In one year, 1,146 unique individuals received services at that site, of whom 742
(64%) were new participants, many coming to the site for the first time specifically to access smoking
equipment. Over the year, participants received safer smoking supplies in 94% (3,237) of the 3,979 total
encounters at the site, which demonstrates the high demand for safer smoking supplies.
25
25
Singh S, Banta-Green C, Kingston S. Distribution of Safer Drug Smoking Supplies as a Public Health Strategy.
Seattle, WA: Addictions, Drug & Alcohol Institute, University of Washington, January 2022.
https://adai.uw.edu/wordpress/wp-content/uploads/SaferSmokingBrief_2022.pdf

63
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix G – Recommendation 6: BH-ASO and RNP data reporting
Recommendation – (1) Establish specific data collection and reporting requirements among Behavioral
Health Administrative Services Organizations (BH-ASOs) related to their regional recovery navigator
programs (RNPs); (2) Identify data to be included in the RNP quarterly reports for SURSAC review to
monitor program effectiveness and inform recommendations for improvements.
Bill Requirement(s) – This recommendation pertains to ESB 5476 Section 1.3(h), related to “reporting
requirements by behavioral health administrative service organizations [BH-ASOs] to monitor the
effectiveness of the [Recovery Navigator] programs and recommendations for program improvement,” as
well as Section 2.5: “Each recovery navigator program must submit quarterly reports to the authority with
information identified by the authority and the substance use recovery services advisory committee
[SURSAC] for discussion at meetings following the submission of the reports.”
Background
As a key aspect of the Plan and the state’s response to the State v. Blake supreme court ruling, the
Recovery Navigator Program was initiated as soon as possible following the passing of 5476. Uniform
Program Standards were established, and HCA developed a draft data collection workbook for use by the
BH-ASOs and RNP contractors to enable data collection as soon as the programs became operational and
open to referrals. The data collection workbook was further informed by meetings with the LEAD Bureau
and input from the BH-ASOs.
At the monthly meetings on March 7
th
and April 4
th
, the SURSAC was asked to provide feedback for the
RNPs regarding what data to include in the quarterly reports that would help the SURSAC assess the
effectiveness of the programs and make recommendations for program improvement. Those notes were
collected and forwarded to the RNP leads at HCA on April 25th in a document titled, “Section 1.3(h) – RNP
Data Collection and Reporting.”
Although the feedback from SURSAC has already been provided to the RNPs for immediate
implementation where feasible, this formal recommendation aims to summarize and confirm the
following:
Part I: Current BH-ASO data collection activity, which was informed by meetings with the LEAD
Bureau, input from the BH-ASOs, and SURSAC
Part II: New BH-ASO data collection recommendations that could be implemented immediately
given current staffing, funding, and other capacities

64
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Part III: Recommendations for RNP Quarterly Report content to be provided to SURSAC as part of
RNP monitoring
Part IV: Data collection and reporting recommendations that are contingent on the
implementation of a data integration system that would make them possible
Part I: Current State of BH-ASO Data Collection
The BH-ASOs are not collecting data directly. The BH-ASOs have contracted with local providers, and
those providers have hired staff who are collecting the data that is being tracked in the data collection
workbook described below. The staff collecting these data do not have full knowledge of, or access to, the
comprehensive system of services that people are utilizing.
The following data elements are being collected via the Data Collection Tool Excel workbooks in a uniform
manner across all regions so they can be combined and reviewed for statewide, as well as regional,
analysis (see Appendix A for details).
The workbooks that contain these data are shared with HCA, from which HCA can summarize (and
conduct analyses when possible) and share, in aggregate, within the RNP Quarterly Reports that are
provided to SURSAC for review.
Referral and Outreach Data
Unique identifiers that can be linked to outcomes (i.e., services received, arrests, health) to
demonstrate overall impact of each RNP and prevent unintentional client duplication. Currently,
BH-ASOs are collecting clients’ first and last names, dates of birth, social security numbers, and
Provider One IDs as forms of unique identifying information, as well as creating a unique client ID
for each individual who enrolls in RNP case management.
Referral source (e.g., child welfare, law enforcement, self-referral, etc.)
Referral reason (e.g., safety concern, in crisis, frequent contact with law enforcement, etc.)
Referral location (address/location from which referral call is made)
Demographic Information: BH-ASOs are collecting individual-level demographic data at referral
intake, which can be used to provide a demographic distribution summary for all other data
points collected by the RNP. Each Policy Coordination Group (PCG) is required to gather individual
demographic data for all RNP participants, including (but not limited to) age, gender identify,
sexual orientation, race, and ethnicity. In the aggregate, such data are necessary and relevant to
enable robust analysis, including analyses related to racial equity. BH-ASOs are collecting the
following demographic data for each person referred to the RNP:
o Race
o Ethnicity
o Gender
o Sexual Orientation
o Source of Income / Support (to identify who may qualify for state benefits such as ABD or
social security disability)
65
SUBSTANCE USE AND RECOVERY SERVICES PLAN
o Housing Status
Outreach Outcome (e.g., not interested in services, consent signed, individual could not be
reached, etc.)
Screening Outcome and Case Management Level (e.g., declined services, enrolled in intensive
care, etc.)
Direct Client Services Provided by RNP (e.g., Naloxone, bus pass, clothing, hygiene products,
shelter, etc.)
Case Management Data
Case management phase / engagement level (light or intensive case management)
Contingency Management Participation (yes/no)
Outreach follow-up (yes/no)
Referral to services made (multiple selection, see Appendix A for options)
Linkage to Care / Warm Hand Off (multiple selection, see Appendix A for options)
Release of Information (ROI) signed (yes/no)
Consent form signed (yes/no)
Individualized Service Plan Created/Updated (yes/no)
Engagement Report
The following information is also provided quarterly to HCA within each BH-ASO’s Data Collection Tool
(PCG = Policy Coordinating Group; OWG = Operational Workgroup):
Frequency of PCG and OWG meetings (measure of stakeholder engagement)
Partner attendance at PCG and OWG meetings (measure of stakeholder engagement)
o Number of attendees
o Representation from law enforcement, prosecution, public defense, government
agencies, community advocacy groups, service providers, other relevant local
stakeholders

66
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Part II: New Recommendations for BH-ASO Data Collection (Immediate Implementation)
BH-ASO Data Collection
Seek funds to implement a data integration platform that can serve both as a common database
for diversion efforts across the state and as a data collection and management tool for
practitioners. If possible, leverage existing platforms already in use by HCA-funded efforts and
any closed loop referral systems implemented in the future.
Establish a quality assurance process for BH-ASOs to ensure that data in the data collection
workbooks are clean, complete, and accurate before submitting to HCA, and a plan in place for
data that is deemed out of bounds / unverified for submission
Where applicable, add data validation to data fields in the data collection workbook (e.g., only
dates accepted under DOB and date of referral, only 7-digit numbers accepted in Provider One
ID, etc.)
Part III: Recommendations for RNP Quarterly Report Content

67
SUBSTANCE USE AND RECOVERY SERVICES PLAN
It is expected that RNP clients will be engaged in long-term, intensive case management. While some
“light touch” participants could see significant individual benefits in a relatively short period of time,
many individuals will have complex co-occurring challenges, including extensive criminal-legal system
contact. For these participants, progress toward health, wellness, and stability is expected to take much
longer than a year, so evaluations of the RNP in its early years should include formative measures and
measures of change (in knowledge, attitudes, or actions) for systems stakeholders, not only data that can
assess participant-level formative and outcome metrics. These metrics should include:
Referral Response Time (average and range)
Narrative description of referral processes available for the RNP and any changes to referral
processes that have occurred in the quarter
Frequency of community referral source and referral source percentages, statewide and for each
BH-ASO: Number of referrals from different community sources (e.g., casinos, child welfare,
family member, etc.)
o Implement system to add and track referral sources based on submissions in “other”
category into the tracking sheets
Demographic summaries of RNP outreach and referral data, statewide and by BH-ASO): Total
number, racial/ethnic composition, gender composition, sexual orientation composition, and
housing status of populations:
o Referred to RNP through law enforcement diversion
o Referred through law enforcement social contact
o Referred through community referral processes
o Referred but not enrolled (outreach referral)
o Agreeing to outreach but not case management (outreach status)
o Enrolled in light case management
o Enrolled in intensive case management
Frequency of reasons for referral statewide and for each BH-ASO: Number of referrals made for
different reasons (e.g., concern for public safety, concern for self-harm, unlawful possession of
controlled substances, etc.)
Number and Types of Direct Client Services Received, statewide and by BH-ASO: Number and
types of services received directly from RNP (e.g., Naloxone, housing voucher, bus pass, etc.)
Number and types of services participants have been referred to, statewide and by BH-ASO (e.g.,
healthcare, transportation, behavioral health services, legal services, employment assistance,
public benefits, withdrawal management, SUD assessment, outpatient treatment, inpatient
treatment, community support organization, housing support, etc.)
Number and types of services to which participants have received warm hand-off and engaged in
services, statewide and by BH-ASO (e.g., healthcare, transportation, behavioral health services,
legal services, employment assistance, public benefits, withdrawal management, SUD
assessment, outpatient treatment, inpatient treatment, community support organization,
housing support, etc.)

68
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Number and attendance of PCG meetings, statewide, by BH-ASO, and by local RNP: Number of
PCG meetings, attendance by representatives with decision-making power from law
enforcement, prosecution, public defense, service providers, local behavioral health and other
government agencies, advocacy organizations, and other local community partners as relevant.
State Census Data (source: Office of Financial Management)
Part IV: Future Evaluation Recommendations Contingent on New Data Infrastructure
While the impacts of a systems-change initiative like RNP are unlikely to be seen within the first few
years, Washington State should currently work to establish the necessary capacities and processes to
enable both formative evaluation and summative evaluation of effectiveness. This will likely require the
integration of a new data infrastructure or processes that can exploit existing and new streams of data
pertaining to an individual’s criminal legal system encounters/involvement, and the outreach, treatment,
and recovery support services they receive through RNPs.
Collection of the metrics below should commence – and be included in RNP quarterly reports -- once a
data infrastructure has been established that supports user-friendly data collection and management for
practitioners:
System utilization
• Use of emergency medical services
• Emergency Department utilization
• Arrest, days in jail
• New charges with incident date after of referral to RNP (broken into felony,
misdemeanor), to be added to Case Management tab in RNP Data Collection tool
• Convictions with incident date after date of referral to RNP (broken into felony /
misdemeanor), to be added to Case Management tab in RNP Data Collection tool
• Access to and engagement with culturally appropriate, non-punitive, community-based
resources
System response
• Capacity and variety of local services aligned with RNP’s commitment to harm reduction
and holistic care
• Number and percent of substance-possession related law enforcement encounters that
result in arrest, booking, and/or convictions for RNP-eligible behaviors, as well as the
demographics of those individuals engaged by law enforcement in these encounters
• Racial disparity analysis that compares demographics of individuals who are arrested and
booked into jail, compared to the demographics of those who are referred to RNP,
among diversion-eligible individuals
Quality of life

69
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Self-report quality life/well-being
• Improved mental and physical health
Services and Access Gap Analysis: Indicated by comparing services needed/requested by RNP
participants, referrals made, referred services received by BH-ASO region, and reasons why
services were not received (if applicable). If the data collection burden for case managers is too
great for this level of analysis, request that case managers report areas where service gaps are a
persistent problem.
Participant Satisfaction: Collected via survey every six months following enrollment in RNP, with
procedures in place outlining minimum and maximum contact efforts and whether anyone (e.g.,
those who un-enroll from RNP case management, or move out of state) should not be included in
follow-up data
Number and percent of substance-possession related law enforcement encounters that result in
RNP referral: The BH-ASOs will be tracking “source of referral” for each RNP participant, which
includes referrals from law enforcement officers, so the quarterly reports can include # and % of
referrals from LEO to the RNP. However, this new recommendation refers to numbers indicating
the percent of LEO encounters or arrests that do and do not lead to RNP referral – and the
associated demographics. Since the BH-ASOs do not have access to this law enforcement
encounter data, implementation of this recommendation is contingent on having a method for
collecting such data.
Demographics of non-diverted arrests for RNP-eligible behaviors
Approximate Financial Support and Staffing Needed:
Funding to execute Parts I-III are secured with the existing RNP budgets (approximately $20 million per
year).
Implementation of Part IV would require additional funding to support the following:
• Investment in the software selected by the state to create the necessary infrastructure
• Technical Assistance to setup and provide ongoing technical support to every BH-ASO to
implement the new data
• At least one FTE to manage data coordination with the new infrastructure and prepare data for
RNP quarterly reports that are out of scope for the BH-ASOs to collect
Collaboration with Existing Resources:
Law Enforcement jurisdictions
Behavioral Health Administrative Services Organizations
Community behavioral health treatment and recovery support services providers
SURSA Committee feedback
The overall data structure/architecture isn’t clear – it would be helpful if this were diagrammed.

70
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Unfortunately, we don’t have time to create a diagram in time to provide prior to the SURSAC vote, but
this could be provided at a later point for clarification. The data infrastructure that could provide these
types of diagrams are captured in the 2
nd
data recommendation, #13.
“Services received” isn’t an outcome. “Effectiveness,” which is the standard in the law, is a measure of
actual outcomes, e.g., health, arrest, not process or services received.
When the subcommittee discussed this, the general consensus was that “services received” can be
considered an outcome if providing services to RNP enrollees is one of the goals of the program.
However, the point was well taken that “receiving services” does not measure improvement of quality of
life in and of itself, and “arrests” and “health” have been added as examples of outcomes that could more
directly capture overall effectiveness.
Collecting Provider One IDs as a unique identifier only helps for people who get public funding. What
about SSN, and trying to link to the all payer claims database?
Omitting “social security numbers” from the initial list of unique identifiers was an oversight, and that has
been added. First name, last name, date of birth, and social security number should be sufficient unique
identifiers. During implementation, the feasibility of using these unique identifiers to link to data from
the All Payers Claims Database can be explored.
(Referring to page 2, “Direct Client Services Provided by RNP”): Naloxone, bus passes, clothing, hygiene
products, etc. are supplies, not services.
The subcommittee views “providing supplies” as a service, and this is the language used in the RNP
Workbooks. If this issue should be pursued further, “Direct Client Supports” could be an alternate way to
phrase this in the workbooks and reports.
Somewhere there should be a safety/harm reduction plan and services identified separately from direct
services provided.
These types of services are outlined in the client’s individualized service plan
How is contingency management measured – that they indicate they want to start, that they do start,
how many sessions, results? Y/N is inadequate to document receipt of contingency management.
Contingency Management participation is tracked in the workbook (see Appendix A) with a new entry for
each engagement, so each engagement prompts a Y/N outcome, as opposed to a single Y/N response to
indicate whether they are participating in CM in general or not.
Unless “referral response time” is tracked in real time, it doesn’t seem such summary data would be
available.
While a warm hand-off is ideal – in which case there would be effectively no time between referral and
response – there will be situations when there will still be a time gap between the initial referral and
when the RNP can respond to that referral. This data (date/time of referral, date/time of response, and
time elapsed between the two) is being collected in the workbooks (see Appendix A), so it will be
available. The subcommittee would like clarification for what is meant by “real time,” if this response
does not address the concern.

71
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Not sure what you mean by “formative and summative evaluation.” The law specifies “effectiveness”
which mean real world outcomes utilizing individual level data. Presumably with some quasi-experimental
design, either within-person longitudinal or a comparison group.
We may be able to use quasi experimental design to assess effectiveness, as well as other measures of
effectiveness.
“Use of Emergency Medical Services” data is very hard to get, vs. health care utilization, e.g., Emergency
Department of hospitalization/CHARS. Do you think you’ll get this from WEMSIS?
The source of this data would need to be determined if/when new data infrastructure (outlined in the
other data recommendation, #13) is implemented. In the meantime, “Emergency Department utilization”
has been added below “Use of Emergency Medical Services,” as that is a measure of interest as well.
Appendix C-1: BH-ASO Data Collection Tool for RNPs
BHDS
= Dropdown options (demographic fields) aligned with Behavioral Health Data System
Referral and Outreach Data
Data Element
Data Type / Validation
Provide One ID
7-digit numeric-only entry (data validated)
Client ID
8-character alpha-numeric: Aa11aa11
First Name
Letters only
Last Name
Letters only
Alternate Name / AKA
Letters only
Date of Birth
Indicate “unknown” if not collected
Date of Referral
mm/dd/yy
Time of Referral
Please use 24 Hour clock (3:15pm = 15:15)
Referral Response Time
Please use 24 Hour clock (3:15pm = 15:15)
URBAN response time goal: within 30-45 minutes
RURAL response time goal: within 60-90 minutes
Referral Source
SINGLE SELECTION:
• Business Community
• Casinos
• Child Welfare
• Community Based Organization
• Criminal Legal System (e.g., Probation, Pretrial Services)
• Emergency Department
• Faith-Based Organization
• Family Member
• Fire/EMS
• Harm Reduction Program (SSP)
• HealthCare Referral
• Homeless Encampment
• Law Enforcement – Arrest Diversion
• Law Enforcement – Social Contact Referral
• Motels
• Outreach
• Self-Referral

72
SUBSTANCE USE AND RECOVERY SERVICES PLAN
•
Social Contact
• Other
Referral Reason
SINGLE SELECTION:
• Concern about safety of others
• Concerns about self-harm
• Unlawful possession of controlled substance (ESB 5476)
• Frequent contact with law enforcement (LE)
• In crisis
• Interfering with business
• Solicitation
• Theft
• Other
Location of Referral /
Outreach
Full street address if known
Alternatively: list location and zip code (e.g., Seeley Lake Park, 98499)
Race
BHDS
MULTIPLE SELECTION:
• American Indian / Alaska Native
• Asian Indian
• Black or African American
• Cambodian
• Chinese
• Filipino
• Guamanian or Chamorro
• Native Hawaiian
• Japanese
• White
• Korean
• Laotian
• Middle Eastern
• Other Asian
• Other Pacific Islander
• Other Race
• Unknown
Ethnicity
BHDS
MULTIPLE SELECTION:
• Cuban
• Hispanic – Specific Origin Unknown
• Mexican
• Not of Hispanic Origin
• Other Specific Hispanic (e.g. Chilean)
• Puerto Rican
• Unknown
• Refused
• Not Collected
Gender
BHDS
SINGLE SELECTION:

73
SUBSTANCE USE AND RECOVERY SERVICES PLAN
•
Female
• Male
• Transgender
• Intersex
• Transgender Female
• Transgender Male
• Unknown
Sexual Orientation
BHDS
SINGLE SELECTION:
• Heterosexual
• Gay/Lesbian/Queer/Homosexual
• Bisexual
• Questioning
• Choosing not to disclose
Source of Income / Support
per Sec 1.3(m)
SINGLE SELECTION
• Wage/Salary
• Public Assistance
• Retirement pension
• Disability
• Other
• None
• Unknown
• Not collected
Housing Status
BHDS
SINGLE SELECTION:
• Homeless without housing
• Foster home/ foster care
• Residential care
• Crisis residence
• Institutional setting
• Jail / correctional facility
• Private residence
• Independent living
• Dependent living
• Private residence – youth
• Other residential status
• Homeless with Housing
• Unknown
Screening Outcome / Case
Management Level
SINGLE SELECTION:
• Outreach referral (declined services)
• Outreach status
• Enrolled in light case management
• Enrolled in intensive case
Direct Client Services
MULITPLE SELECTION:
• Naloxone
• Shelter (e.g. housing, motel voucher, sleeping bag)
• Coffee

74
SUBSTANCE USE AND RECOVERY SERVICES PLAN
•
Food/Gift Card
• Hygiene Products
• Family Support Services (e.g. childcare, diapers, food)
• Bus pass
• Medical expenses
• Clothing
• Other
• Multiple Resources Provided
Outreach Outcome
MULITPLE SELECTION:
• Not interested in services
• Consent signed
• Exchanged contact information
• ROI signed – enrolled
• Unsuccessful contact attempt (i.e., person absconded)
• Provided list of resources
• Called Crisis Services
• Scheduled Follow-up meeting
• Individual arrested after referral
• Other
Case Management Data
New entry (row of data) created for each case management event
Provider One ID
7-digit numeric-only entry (data validated)
Client ID
8-character alpha-numeric: Aa11aa11
Date of Case Management Event
Mm/dd/yy
Case Management Phase / Engagement Level
SINGLE SELECTION:
• Light case management
•
Engaged/intensive case management
Contingency Management (Participation)
SINGLE SELECTION:
• Yes
•
No
Outreach Follow-Up
SINGLE SELECTION:
• Yes
•
No
Referral to Services Made
MULITPLE SELECTION:
• Basic Needs e.g. hygiene, food, clothing
• Public Benefits (e.g. DES, Social Security,
Health Insurance)
• Physical healthcare referral
• SUD Referral – Withdrawal Management
• SUD Referral – Assessment
• SUD Referral – Outpatient
• SUD Referral – Inpatient

75
SUBSTANCE USE AND RECOVERY SERVICES PLAN
•
Community Support Organization (Recovery
Café, other nonprofit)
• Self Help Support Group (AA/NA/
Alanon/SMART recovery/etc)
• Faith-based organization
• Housing
Linkage to Care (Warm Hand-Off)
MULITPLE SELECTION:
• Basic Needs e.g. hygiene, food, clothing
• Public Benefits (e.g. DES, Social Security,
Health Insurance)
• Physical healthcare referral
• SUD Referral – Withdrawal Management
• SUD Referral – Assessment
• SUD Referral – Outpatient
• SUD Referral – Inpatient
• Community Support Organization (Recovery
Café, other nonprofit)
• Self Help Support Group (AA/NA/
Alanon/SMART recovery/etc)
• Faith-based organization
•
Housing
ROI Signed
SINGLE SELECTION:
• Yes
•
No
Consent Form Signed
SINGLE SELECTION:
• Yes
•
No
Individualized Service Plan Created / Updated
SINGLE SELECTION:
• Yes
•
No

76
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix H – Recommendation 7: Health Hubs
Recommendation – Establishing Health Engagement Hubs to serve as an all-in-one location where people
who use drugs can access a range of medical, harm reduction, and social services
Bill Requirement(s) – Developing Health Engagement Hubs for people who use drugs considers and
supports several elements that 5476 outlined for inclusion in the Substance Use Recovery Services Plan:
• Points of intersection that persons with substance use disorder have with the health care system
(ESB 5476 §1.3.a)
• Locations in which persons with untreated substance use disorder congregate (ESB 5476 §1.3.a)
• New community-based care access points (ESB 5476 §1.3.b)
• Barriers to accessing the existing behavioral health system (ESB 5476 §1.3.d)
• Innovations that could improve the quality and accessibility of care for persons with co-occurring
substance use disorders and mental health disorders, and populations chronically exposed to
criminal legal system responses (ESB 5476 §1.3.d)
Consideration of youth, rural areas, and tribes:
Youth: These Health Engagement Hubs would be open to youth as well as adults. Ryther/YouthCare in
Seattle provides young adult models that combine outreach with fixed site, which can be used to help
inform ways to make these hubs appropriate and effective for youth.
Rural Areas: Health Hub mobile treatment services will provide support to rural areas that do not have a
brick-and-mortar hub.
Tribes: Sufficient funding will be provided to each tribe to establish, or invest in already existing, hubs for
people who use drugs, so that they can decide which services to provide via the Health Hubs that are best
suited to each tribe’s needs.
Recommendation Details
We propose Health Engagement Hubs to be affiliated with an existing SSP serving each community as well
as other entities as appropriate, including Federally Qualified Health Centers (FQHCs)/Community Health
Centers (CHCs), patient centered medical homes, overdose prevention/safe consumption sites, peer run
organizations (e.g., Club Houses), services for unhoused people, supportive housing, and opioid
treatment programs. Harm reduction services and supplies must be an integral program component of
any organization housing a health hub.
The hubs would prioritize communities disproportionately impacted by the harms associated with opioid
and other drug related harm, including American Indian/Alaska Native communities, Black/African
American communities, Latino/Hispanic communities, people experiencing homelessness, and
communities impacted by the criminal-legal system. Programs may operate in fixed sites or could be
mobile clinics.
Services should address each of the care domains below, with as comprehensive a service mix as feasible:

77
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Comprehensive physical and behavioral health care including: primary care, wound care, infectious
disease vaccination, testing, and treatment, and sexual and reproductive health care services
(including pre- and post-natal supports like doulas), dental care, ophthalmology, low-barrier
buprenorphine (and other medications for SUD as available), contingency management services,
appropriate client-centered-assessment and linkage for diverse substance use disorder treatment
services e.g., harm reduction counseling and treatment services, “traditional”, and mental health care
services.
• Medical case management services/care coordination (could include doula support).
• Harm reduction services and supplies- Overdose education, naloxone distribution, and drug checking
services. Safer drug use supplies and safer sex supplies. Other basic needs including food, clothing,
and basic hygiene supplies.
• Community health outreach workers/navigators, peer health educators, and peer recovery coaches
with the ability to engage community members about the hub, engage people who use drugs in
services, transport people to the hub, and to transport people to other service locations, as needed.
These staff will participate in community provider meetings including ED, jail, public health,
behavioral health, detox, housing, and others to create referral pathways and professional
relationships that support clients accessing a complete continuum of care with no wrong door.
o The job is about non-judgmental support, not about “putting people in their place”. Power
dynamics need to be carefully considered.
o Quality staff supervision and support is essential to promote high quality care and staff
wellbeing.
• Linkage to housing, transportation, and other support services.
• Spiritual Connection Communities: Among those for whom substance addictions are experienced as
spiritual crises, spaces for spiritual and social connection are essential to restoring a hopeful and self-
directed life. Therefore, it is important that these hubs create space for, or provide linkage to,
spiritually-oriented communities that are as diverse as the communities and the people they would
like to engage. Spirituality is one of the biggest drivers, motivators, and natural “community” for
people to connect and be well with, especially for tribes. People who use are in a form of community,
and that sense of community needs to be maintained as they transition into healthier environments.
Pulling them out into isolation, marginalization does not promote healing.
Health Engagement Hubs should encourage community volunteers, and provide appropriate training to
staff and volunteers, including diversity, equity, and inclusion training.
Services should be offered in coordination with every willing SSP. Communities with an SSP may also offer
services in other settings described above. Communities without an SSP may provide services in another
setting given they institute a substantial harm reduction service and staffing continuum.
A health hub should be available within a one-hour drive of every location in Washington State, with the
exception of frontier designated areas where they should be available within a two-hour drive.
Background and Supporting Data

78
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This recommendation draws most immediately from a State Opioid and Overdose Response Plan (SOORP)
proposal authored by the Washington State Department of Health (DOH) including Emalie Huriaux. It
draws from and expands upon work from the Center for Community-Engaged Drug Education,
Epidemiology and Research (CEDEER) at the UW Addictions, Drug, and Alcohol Institute, including low
barrier buprenorphine programs and expressed needs/interests from program participants at SSP
surveys.
Low-barrier health engagement “one stop shop” health care and social services are needed for people
who use drugs who are not well served by the current health care system and experience significant
health disparities. Syringe service programs (SSPs) provide a culturally appropriate and trusted setting in
which to provide these services in collaboration with participants and regional health care
providers/systems and local health jurisdictions. Similar holistic programs to support people living with
HIV have been shown to be successful and cost-effective.
In 2019, the Addictions, Drug and Alcohol Institute (ADAI) at the University of Washington launched the
“Meds First” program to provide onsite, low-barrier access to buprenorphine in partnership with the six
syringe services programs (SSPs) across Washington State. Given that Health Hubs would operate in a
similar way, key findings from the Meds First program
26
provide evidence that this could be an effective
service for Washington residents who use drugs:
• Care navigation fits flexibly and productively within community-based harm reduction programs
• Participants of harm reduction programs want—and use—care navigation services, especially in-
person support
• Providing opioid use disorder treatment with a harm reduction orientation supports honest
conversations about drug use
A full report on the Meds First program can be found at Care Navigation at Harm Reduction Programs
(uw.edu), and related research findings have been published in Addiction Science and Clinical Practice:
“The Community-Based Medication-First program for opioid use disorder: a hybrid implementation study
protocol of a rapid access to buprenorphine program in Washington State.”
27
Additionally, a study published in Substance Abuse in 2020
28
found that a low-barrier buprenorphine
program co-located with an SSP in Seattle served as an effective point of entry for a low-barrier MOUD
program: a large proportion of enrolled patients demonstrated sustained retention and reductions in
opioid use, despite housing instability and polysubstance use.
Concerns and Considerations
• Concerns related to the workforce demand v. supply to run these Health Hubs
• May need to build capacity within SSPs to prepare for this integration; creative partnering needed
26
https://adai.uw.edu/care-navigation-2022/
27
The Community-Based Medication-First program for opioid use disorder: a hybrid implementation
study protocol of a rapid access to buprenorphine program in Washington State - PMC (nih.gov)
28
Engaging an unstably housed population with low-barrier buprenorphine treatment at a syringe
services program: Lessons learned from Seattle, Washington - PubMed (nih.gov)

79
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Additional work will need to be done to determine details pertaining to services billing at these
health engagement hubs. Billing for primary care services is often not financially viable except for
Federally Qualified Health Centers (FQHCs), and mental health licensure is necessary to receive the
higher Medicaid rate for mental health care. If the health hubs cannot be qualified as FQHCs, and
licensed mental health clinics, this could put a serious financial strain on the health hubs and
jeopardize their sustainability.
• Due to the high acuity level of care needed, and because Health Hubs are not Behavioral Health
Agencies eligible to bill for withdrawal management services, withdrawal management services
have been deemed out of scope for Health Hubs
Collaboration with Existing Resources:
• Suggested Lead Agency: DOH in partnership with UW ADAI and HCA
• Partners:
o Syringe Service Programs (SSPs)
o Accountable Communities of Health (ACHs)
o Local Health Jurisdictions (LHJs)
o Federally Qualified Health Centers (FQHCs)
o Community Health Centers (CHCs)
Approximate Financial Support and Staffing Needed:
Calculating the financial estimates and overall investment required to stand up these Health Engagement
Hubs with sufficient geographic access points will need to be undertaken by fiscal analysts and experts,
with due consideration given to the following:
• The number of Health Engagement Hubs needed throughout the state to meet recommendation
for one within a 1-2 hour drive of any location in the state
• Staffing needed for each of the domains listed above
• Competitive compensation for staff, to minimize burnout and turnover
• Medical supplies
• Construction costs for any new structures needed
• Vehicles/gas for mobile services
• Projected revenue from billing services
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

80
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix I – Recommendation 8: Employment and education pathways
Recommendation – Education and employment pathways, including training, placement, and supported
services.
Bill Requirement(s) – Section 1.8, Section 4.2(b),(c),(e),(h)
Background and Supporting Data
Regional and county-wide programs have been made available to individuals who are seeking
employment, education, training/certification, and other supportive resources. Additionally, there are
programs provided within the local/county jails for incarcerated individuals to seek and obtain employment
upon release. In King County programs like road map to success, Orion industries, and Post Prison Education
Program have been able to assist individuals. These programs include, welding certification,
entrepreneurship, construction related work, and CDL licensing to name a few. Though there are varied
programs available to those with SUD, in recovery, or incarcerated/being released from incarceration, there
are still a number of barriers that they individuals experience.
In less dense areas, there are few resources for individuals and there is an all-around barrier of
these individuals receiving a livable wage. The stigma of substance use is also a barrier for individuals,
making it difficult to obtain employment. Programs like peer support and 0-1 intercept interventions
should also be able to connect these individuals to the need resources. Include expanding efforts for
incorporating individuals incarcerated and released from incarceration into these programs. Current
successful models include:
Stone Bridge Re-entry a re-entry service that provides various services for those experiencing poverty,
homelessness, incarceration, addiction through community-based services and treatment services.
Brothers United in Leadership Development (B.U.I.L.D) an organization providing services to the black and
brown community by developing community partnerships targeting adults and youth to provider
leadership and employment, through community groups and services to develop the future generations
of leaders.
Programs are also needed that are directed for youth, including community passages for job
placement, GED certification, and education pathways through a peer program or mentorship programs.
Current successful model, Community Passageways , which is a Seattle based program that has worked
with youth that intersect the criminal legal system through community support teams, school-based
programs, while using evidence-based interventions to tailor to the needs of youth.
The recommendation creating a grant program to build and sustain community based mental
health providers to expand availability of these types of programs with a low barrier one page grant
application, targeted for programs that engage with BIPOC and other historically underserved
communities. There could also be individual grants or scholarship type program for individuals in recovery
housing that includes more that job training but incorporate the cost to get childcare costs covered, drivers
licensing testing, transportation, along with cost associated with the training or the training itself.
HCA could create a centralized location for these kinds of resources based on region and resource
type for all supportive services, including education and employment.

81
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Concerns and Considerations – What are the potential downsides of implementing this recommendation?
Record any dissenting opinions, concerns, or considerations here
Collaboration with Existing Resources:
• Foundational Community Supports (FCS)
FCS provides supportive housing and supported employment services to vulnerable Medicaid
beneficiaries by helping participants find and maintain stable housing and employment. Eligibility
is determined by risk factors such as chronic homelessness, complex BH and co-occurring SUD,
disability, and other long-term care needs.
• HCA is working with peer programs to bring CPC trainings both into Walla Walla and into Mission
Creek, to train folks to become CPC's.
Approximate Financial Support and Staffing Needed:
Dollars
CY23
CY24
CY25
Legislative / State Budget Funding
440,000 grant funding for a biennium
225,000
maintenance
funding
HCA Grant-Based Funding
Total Funds
Staff (FTE)
1
1
1
SURSA committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

82
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix J – Recommendation 9: Expansion of WHRL and Asset Mapping
Recommendation – Expansion of the WA Recovery Helpline and the Recovery Readiness Asset Tool to
provide a robust resource database for those seeking or directing to services.
Bill Requirement(s) –5476 Section 1.3 (a),(b),(c),(d),(e),(f),and (g)
Background and Supporting Data:
Providing a tool that maps and directs individuals to community-based care access points, along
with safe station entities with a tool that helps locate and help those currently in need of outreach,
treatment, and recovery support services is vital to the requirements and plays the role as an assistive
tool to meet other items outlined in section 3 of RCW 71.24.546, as part of the Blake Bill(ESB 5476). By
expanding upon the current recovery readiness asset tool (this does not indicate an individual’s readiness
to enter recovery) built from the Roadmap to Recovery and the WA Recovery Helpline, we can enhance
the capabilities of the tools available to reach more Washingtonians affected by SUD and their families.
This tool will work in conjunction with the E2SHB 1477 work to designate a primary technology system to
provide “Real-time bed availability for all behavioral health bed types, including but not limited to crisis
stabilization services, triage facilities, psychiatric inpatient, substance use disorder inpatient, withdrawal
management, peer-run respite centers, and crisis respite services, inclusive of both voluntary and
involuntary beds, for use by crisis response workers, first responders, health care providers, emergency
departments, and individuals in crisis.”
This Committee also recommends a referral system to be incorporated with the locator tool to
help facilitate the connection between an individual and a facility to address capacity concerns.
Local counties like King County have developed county specific resources, Emerald City Resource
Guide by Real Change: Emerald City Resource Guide. WA211 provides community resources Home -
Washington 2-1-1 - WA 2-1-1 (wa211.org) MOUD resource finder helps people connect to medications
MOUD Locator - Washington Recovery Help Line (warecoveryhelpline.org) and DOH is releasing resource
finder that utilizes WA211 data for a resource finder specifically for substance use during pregnancy and
for parents. DOH is working to create a data system that holds all of the data for the different resource
finders, so they are kept current and have all the same data. HCA has a number of resources including a
pamphlet of integrated behavioral health community resources and DOH Green book.
Beyond providing treatment and recovery support service locations, this database should also
include the community-based resources, including locations for SSPs, peer and care navigators, opioid
treatment network care partners (hub and spoke), and RNP community resources. This tool should also
consider including infectious disease services that are systemic to the overdose crisis (e.g., hepatitis C
services). Creating a more robust system to include civil legal, and welfare locations as well, will provide a
better full continuum of care for individuals in an easily accessible way. DCYF is currently working toward
a similar grassroots map for their child welfare and family resources regarding SUD and recovery support
services. There are several legal systems throughout the state that have similar maps that also provide
legal resources for those impacted by SUD. To eventually gather and include those various groups would
make this the most robust resource system available to date.
Other states including Kentucky, and even local jurisdictions such as Spokane County have similar
tools that have proven to be effective in their geographical regions and we would like to expand these types
of tools across Washington State.

83
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Foundation infrastructure is key to providing the most up to date services and resources
according to Third Horizons and Atlas Shatter Proof, who already have been contacted to quote on similar
work being done. Pipelines are created from existing and future data sources to a single system to
provide the locator and referral tools as described above. This creates real-time updated systems. To
ensure data streams are updated regularly by the information provider, legislative mandates shall be
imposed to enforce the need for updated data. The proposed expansion of the MOUD locator and
recovery readiness asset tool includes the development of a larger database of resource and a dual
interface program, one for the public and one for internal use. These two interfaces include, and external
page made to public including crisis stabilization, care access points, and families with a mapping tool,
and asset list. The internal interface will have tools for HCA staff, MCO provider networks, and policy
makers including, dashboards, gap analysis tools, regional capacity, and workforce checklists.
Pipelines to current and future data tables, that should be incorporated within the system are:
• RDA Data/Geo data from ProviderOne
• DOH Licensure data
• Recovery Helpline data
• Grant and other non-Medicaid care access points (opioid treatment network care partners,
syringe services, etc.)
• DCYF available data
Campaigning and advertising for Recovery Helpline is a crucial component for educating the public on the
helpline and tools, along with indicating its intent as opposed to a crisis hotline.
Along with additional resources for a heartier system, the WA Recovery Helpline will need non-clinical,
people with lived experience, full-time employees (FTEs) to support this expansion work on the database
and to meet the growing demands the Recovery Helpline will experience.
Concerns and Considerations –
Displaying accurate information regarding billing location as opposed to service location for providers. A
quality assurance process should be developed and incorporated into the system.
Collaboration with Existing Resources:
Recovery Helpline
Provides MOUD locator resources through the hotline and website on a google maps platform. This
information is updated monthly and manually by recovery helpline staff. This information would play into
resources that may not be directly connected to Medicaid and the ProviderOne data and will be kept
current by staff and shared to make sure geolocations are being updated properly.
988/SB 1477
Establishes crisis call center hubs and an expanded response system for those experience mental health
and suicide. It proposes to create technology and platforms necessary to manage and operate the
behavioral health crisis response and a suicide prevention system. This system is currently be worked
through the Department of Health data before being handed over the authority. This system will have a
similar type of map or list of resources to submit individuals to services through a referral mechanism.

84
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This tool will be helpful to ensure the current connection to behavioral health services is similar with SUD
and co-occurring mental health conditions.
Approximate Financial Support and Staffing Needed:
Dollars
FY23
FY24
FY25
Legislative / State Budget
Funding
$1,000,000/System
Development
$1,000,000/Campaign/Ads
$360,000/System
Maintenance
$360,000/System
Maintenance
HCA Grant-Based Funding
Total Funds
Staff (FTE)
8
6
6
Estimations are based off previous quotes from technical developers, along with adding more funding for
referral technology and required FTEs to support education, training, and technical assistance.
Substantial staffing will be need for this to do this dynamically. The above numbers are minimalistic and
there will most likely be greater need for more FTEs to uphold system throughout the various agencies
consistently providing resources.
SURSA committee feedback
From Sarah Melfi-Klein: received September 15, 2022 –
Q: Would this plan include mapping for Tribal-specific recovery resources as well or as a parallel to this
work?
A: This is entirely dependent on willingness and participation to provide local resources.
From Caleb Banta-Green: received September 16, 2022 –
Q: Is there possibility of the database being part of a closed loop referral database so that RHL collected
data are provided to downstream referrals and so RHL gets feedback on client flow to improve their
processes?
A: Recovery Help Line does not collect data beyond general demographics. We want to continue to
provide that anonymity to individuals seeking services.

85
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix K – Recommendation 10: Expanding investment in programs along the 0-1 intercept on
the sequential intercept model
Recommendation – Continue and further increase investment in evidence-based diversion programs that
operate along intercepts 0 and 1 on the sequential intercept model, including, but not limited, to the
Recovery Navigator Program, Arrest/Jail Alternative programs, LEAD, and other harm reduction, trauma-
informed, and public health-based approaches, especially programs and interventions that center a racial
justice lens; and amend RCW 10.31.110 (Alternatives to Arrest – Individuals with mental disorders or
substance use disorders) and RCW 10.31.115 (Drug Possession – Referral to assessment and services) to
reflect how these programs should be used as part of a statewide arrest and jail diversion system by
mandating availability of services within a supportive network of care. Proposing state, regions, and
counties to provide proportionate and adequate funding as supplied into the criminal legal system.

86
SUBSTANCE USE AND RECOVERY SERVICES PLAN
To provide services, outlined below, to the Washington youth population the request was made to
provide adequate policy changes to address the youth barrier, and CMS State Plan Amendment, for
services made available to youth starting at the age of 13, the minimum Medicaid enrollee age without an
adult, and incorporate MAT accessibility and coverage.
Consistent with the Plan requirement outlined in ESB 5476 Section 1.3(i), this recommendation requests
shifting funding to increase and sustain investments to ensure equitable distribution of, and access to,
culturally appropriate, non-punitive, community-based resources, including treatment.
A range of services are noted as diversion options in 10.31.110, and each of these should be made
available in all regions – at least one in every BH-ASO at a minimum -- so that when law enforcement
officers make referrals within their jurisdictions as part of the arrest and jail alternatives / diversion
strategies, those referrals are met with a range of available behavioral health options to best meet the
needs of the individual who has been diverted from legal system involvement.
Those services are:
• Crisis stabilization units for youth and adults, as defined in RCW 71.05.020 – “A short-term facility
or a portion of a facility licensed or certified by the department, such as an evaluation and
treatment facility or a hospital, which has been designed to assess, diagnose, and treat individuals
experiencing an acute crisis without the use of long-term hospitalization” -- at which the
individual must be examined by a mental health professional or substance use disorder
professional within 3 hours of arrival
• Triage facilities for youth and adults, as defined in RCW 71.050.020 – “A short-term facility or a
portion of a facility licensed or certified by the department, which is designed as a facility to
assess and stabilize an individual or determine the need for involuntary commitment of an
individual and must meet department residential treatment facility standards. A triage facility
may be structured as a voluntary or involuntary placement facility”
• Designated 24/7 crisis responders for evaluation for initial detention and proceeding under 71.05
RCW
• Mobile crisis response services for youth and adults
• Regional entities responsible for receiving referrals in lieu of legal system involvement, such as
Recovery Navigator Program
In addition, these services should be made available in all regions as well:
• ASAM-alternative SUD Assessments (15 mins max) for youth and adults (contingent on
assessment recommendation approval)
• Syringe Service Programs for youth and adults
• Health Hubs for youth and adults who use drugs (contingent on Health Hub recommendation
approval)
• Detox/Withdrawal management for youth and adults
• MOUD (Suboxone) for youth and adults
• Outpatient treatment for youth and adults
• Ensure that long-term harm reduction supported case management is available after diversion so
that diversion becomes meaningful
87
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Bill Requirement(s) – This recommendation directly addresses 5476 Section 1.3:
“(g)Framework and design assistance for jurisdictions to assist in compliance with the requirements of
RCW 10.31.110 for diversion of individuals with complex or co-occurring behavioral health conditions to
community-based care whenever possible and appropriate, and identifying resource gaps that impede
jurisdictions in fully realizing the potential impact of this approach.”
“(i)The proposal of a funding framework in which, over time, resources are shifted from punishment
sectors to community-based care interventions such that community-based care becomes the primary
strategy for addressing and resolving public order issues related to behavioral health conditions;”
Youth: As more services for youth are available, RNP services will be directing youth into those services
Rural Areas: This funding will expand RNP programs in rural areas
Tribes: The subcommittee recognizes that each tribe are sovereign entities and will not impose
requirements for RNP or diversion programs but would like to extend equal funding to provide these
types of resources within their tribe. Each tribe would get the option to participate or establish their own
diversion programs, or expand existing programs, and would get proportional investment as any BH-
ASO/region, regardless of participation in or collaboration with local region BH-ASO RNP program.
Background and Supporting Data
Specific models like LEAD and other evidence-based, public health, and harm reduction approaches have
been effective but under-utilized in Washington State. Interventions that are outreach-based and that
operate on a shared decision-making model, offering low-barrier engagement and trust-building
relationships with clients deserve more investment and support. The emphasis among these
interventions should target the zero and one locations on the sequential intercept model.
The Recovery Navigator Program is receiving $25 million in 2022, and $20 million in 2023, from the
general-state fund to initiate and implement recovery service navigation in each of the 10 Behavioral
Health Administrative Service Organizations throughout Washington State. However, these programs will
need more than two years of funding to establish trust within communities and demonstrate efficacy as
an alternative to a criminal-legal approach to substance use in communities, and increased annual
funding is needed to expand services in BH-ASOs that cover multiple counties with rural areas that would
also benefit from transportation services.
Concerns and Considerations
•
Some concern was expressed that money would continue to flow to programs without a system
for accountability around outcomes, and that money should be withheld if the programs are not
generating desired results
Collaboration with Existing Resources:
Arrest and Jail Alternatives (AJA), per HB 1767, RCW 36.28A.450

88
SUBSTANCE USE AND RECOVERY SERVICES PLAN
LEAD Pilot Project, per 5380 Section 29, RCW 71.24.589
Recovery Navigator Program, per 5476, RCW 71.24.115
Federal COSSAP funds
Approximate Financial Support and Staffing Needed
The Recovery Navigator Program is receiving $25 million in 2022 and $20 million in 2023 from the
general-state fund
Look at funds provided to BH-ASOs for RNP for program estimates
Settlement funds are also a potential source of funding
Allocating funding through RNP for transportation needs based on regional needs and capacity. To
including purchasing vehicles, contracting local public transportation services, and per mile
reimbursements.
Financial Impact: Recovery Navigator Program
Dollars
FY23
FY24
FY25
5476 Funding
$20 million
general-state fund
Additional 25 M
$20 million
general-state fund
Additional 25 M**
$20 million
general-state fund
Additional 25 M**
HCA Grant-Based Funding
Total Funds
Staff (FTE)
0
0
0
**incremental increasing over the years for increased services, increased population, outcomes
Financial Impact: Arrest and Jail Alternatives and LEAD Expansion
NOTE: Decision Package has been submitted to expand this program
Dollars
FY23
FY24
FY25
General State Funding
$4,300,000
$4,300,000
$4,300,000
Grant Funding
Total Funds
Staff (FTE)
0
0
0
SURSA committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period
89
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix L – Recommendation 11: SUD engagement and measurement process
Recommendation for a new SUD engagement and measurement process
Because Substance Use Disorder (SUD) is chronic and potentially acutely life-threatening:
• Care for people with SUD needs to be accessible and initiated as quickly as possible.
• Care for people with SUD needs to be accessible in places and care settings that are low
barrier/crisis oriented (e.g., Health hubs for people who use drugs (PWUD), Emergency
departments, CHC/FQHC) in addition to care settings such as withdrawal management and
specialty SUD treatment.
• The initial engagement and measurement process should be focused on what is minimally
necessary to document a diagnosis, determine medical necessity and start care the same day and
be conducted in less than 15 minutes:
o This could include brief screening, diagnosis, documentation of a person’s care
preferences, and if the client wants, initial discussion about the level of care/care setting
or lead to a full assessment.
• Initial engagement and SUD measurement must be focused on, and limited to, client’s needs and
should be limited to only the necessary domains. Trauma and culturally informed approaches
must be taken in terms of the total time, content, and process of engagement and measurement.
We ask that:
o The Washington State Health Care Authority (HCA) convene a workgroup who will review
current processes and workforce needs related to intake, screening, and assessment for
SUD services,
o HCA determine how to build an SUD engagement and measurement process including
developing any necessary rules and payment mechanisms,
o HCA work with PWUD, care providers, state regulators, and payors to address this
recommendation within 12 months, and,
o In the interim, any work that HCA can undertake to advance these goals should be done.
Initial engagement and measurement goals:
● Be as brief as possible and only what is necessary to initiate care the same day whenever
possible, typically less than 15 minutes.
● Be available on demand whether in person or virtually at centralized and accessible community
access points.
● Be available in diverse health care, behavioral health, emergency, and SUD settings.
● Be available within four hours of request 8am-8pm and within 12- hours 8pm-8am.
● Be culturally appropriate and trauma informed.
29
● Consider the patient’s self-identified needs and preferences when evaluating direction of
treatment and/or referral to services.
29
https://www.hca.wa.gov/about-hca/trauma-informed-approach-tia
https://www.hca.wa.gov/about-hca/who-we-are/health-equity

90
SUBSTANCE USE AND RECOVERY SERVICES PLAN
● Eliminate financial barriers to accessing immediate and individualized services.
● Be administered by a range of health professionals, guided by the scope of practice of a service
provider.
● Assessments should be conducted if only necessary and not more than one per 12-month
period.
30
Bill Requirement(s) – Low barrier, person-centered care should be informed by people with lived
experience.
Reducing the time required during initial assessments to center on the self-identified need and desire for
care that guide the direction of treatment, harm reduction services, recovery supports, and other
necessary services based on the needs identified by the client and for the Plan to assist persons with
timely access to all services, including treatment.
Defining Terms
Intake: There is no definition for intake established within WAC or RCW. For the purposes of this
recommendation, intake would be the process through which an individual gains access to behavioral
health services and the associated subprocesses, forms, and declarations associated with that process.
This includes the administration of screening tools and assessments done to diagnose and determine
medical necessity.
Screening: Per RCW 71.24.630, HCA is directed to maintain an integrated and comprehensive screening
and assessment process for substance use and mental health disorders. Under this section, the process
shall include an initial screening tool which can be used by intake personnel systemwide and which will
identify the most common types of co-occurring disorders, and through screening, identify triggers which
would indicate the need to begin an assessment. This could include utilization of screening tools like the
GAIN-SS, AUDIT, DAST, ASSIST, etc.
Assessment: Per WAC 246-341-0200 "Assessment" means the process of obtaining all pertinent bio-
psychosocial information, as identified by the individual, and family and collateral sources, for
determining a diagnosis and to plan individualized services and supports. Per WAC 246-341-0460, the
Clinical Record must include “an assessment which is an age-appropriate, strengths-based psychosocial
assessment that considers current needs and the individual's relevant behavioral and physical health
history according to best practices, completed by a person appropriately credentialed or qualified to
provide the type of assessment pertaining to the service(s) being sought, which includes: a diagnostic
assessment statement, including sufficient information to determine a diagnosis supported by the current
and applicable Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or a placement decision,
using ASAM criteria dimensions, when the assessment indicates the individual is in need of substance use
disorder services.
30
Per the HCA Service Encounter Reporting Instructions, “a new assessment evaluation is not required if an
assessment was completed in the 12 months prior to the current request and medical necessity was established.
The previously completed assessment may be used to authorize care.”

91
SUBSTANCE USE AND RECOVERY SERVICES PLAN
HCA’s Service Encounter Reporting Instructions (SERI), which provides Apple Health Managed Care
Organizations (MCO) and the Behavioral Health Administrative Services Organizations (BH-ASO) in
integrated care regions, and all BH providers in licensed community mental health clinics/licensed
behavioral health agencies assistance for reporting behavioral health service encounters, indicates that
Assessment services are defined as “The activities conducted to evaluate an individual to determine if the
individual has a substance use disorder and determine placement in accordance with the American
Society of Addiction Medicine (ASAM) criteria.”
Medical Necessity: According to WAC 182-500-7010, “medically necessary” or “medical necessity,” with
regard to substance use disorder, is defined by the most recent version of the ASAM Criteria, Treatment
Criteria for Addictive, Substance Related, and Co-Occurring Conditions as published by the American
Society of Addiction Medicine (ASAM). Based on WAC 182-500-0070, “medically necessary” is a term for
describing requested service which is reasonably calculated to prevent, diagnose, correct, cure, alleviate
or prevent worsening of conditions in the client that endanger life, or cause suffering or pain, or result in
an illness or infirmity, or threaten to cause or aggravate a handicap, or cause physical deformity or
malfunction. There is no other equally effective, more conservative or substantially less costly course of
treatment available or suitable for the client requesting the service. For the purposes of this section,
"course of treatment" may include mere observation or, where appropriate, no medical treatment at all.
Background and Supporting Data
Access to timely SUD assessments varies widely across Washington State. In urban areas, people seeking
or needing an assessment may go to drop-in hours multiple times over several weeks before they obtain
an assessment. In rural areas there may be a single provider currently allowed to do assessments and
they may have a multi-week wait list. Alternatively, in some care settings all that is needed to initiate care
is an SUD diagnosis, e.g., a medical clinic with a licensed prescribing provider onsite. The variable access
to care by geography, provider types, and care settings is an example of state and federal rules and
regulations negatively impacting equitable access to care.
The ASAM Criteria is the most widely used and comprehensive set of guidelines for placement, continued
stay, transfer, or discharge of patients with addiction. Other tools, some used in the mental health
system or by Managed Care include the LOCUS, CALOCUS, InterQual, and Milliman. Although ASAM as a
biopsychosocial assessment is not specifically required in a State Plan Amendment for Medicaid, it is
mentioned in Washington State’s 1115 Medicaid Waiver. ASAM is also a requirement in HCA policy (the
SUD Fee-for-Service Billing Guide) and WAC 246-341-0640, “Clinical record content.” This policy is in
place to ensure sufficient information to guide placement decisions when the assessment indicates the
individual is in need of substance use disorder services.
The shorter engagement and measurement processes proposed in this recommendation can therefore
be used to demonstrate medical necessity for any level of behavioral health care / SUD treatment
placement, as long as they include questions that align with the ASAM criteria needed for the health
plan’s utilization review team to apply ASAM to assess medical necessity in order for the service provider
to receive reimbursement for services provided.

92
SUBSTANCE USE AND RECOVERY SERVICES PLAN
However, while the DSM-5 criteria for substance use disorder is composed of 11 yes/no questions , the
ASAM Criteria Assessment Interview Guide is 31 pages long, takes the average clinician about 90 minutes
to complete, and covers six dimensions of assessment (Acute Intoxication and/or Withdrawal Potential,
Biomedical Conditions and Complications, Emotional, Behavioral or Cognitive Conditions and
Complications, Readiness to Change, Relapse, Continued Use or Continued Problem Potential, and
Recovery and Living Environment) intended to identify optimal treatment placement for an individual. It is
typical for individuals who come into contact with providers to have well documented needs, numerous
system encounters and history of assessments and admissions, and ample documentation of necessity
and diagnosis.
The volume of questions, the speed at which they are administered, and the potential personal trauma
from highly sensitive questions (many unrelated to immediate care needs) are all potential reasons for
people to avoid participating in these lengthy assessments, which then becomes a barrier to accessing
treatment services.
Moreover, someone undergoing an SUD assessment may be under the influence of substances and are
not in an appropriate frame of mind to be answering so many personal questions; people need the
opportunity to stabilize / allow their spirit to return to their bodies before engaging in the longer
assessments.
There is usually a small window of readiness when a person with a substance use disorder is ready and
willing to engage in treatment and recovery services, and a lengthy assessment process not only does not
guarantee treatment access, but it can also often lead to frustration, and eventually deter someone from
pursuing treatment and recovery. Neither ASAM nor SAMHSA guidelines should be interpreted or used as
a standard of care or specifically required by Washington State agencies.
The ability to do an assessment should be guided by the scope of practice of a service provider and not be
limited to a single and specific credential in certain settings (e.g., SUDP), as it is currently. For example, a
hospital setting should not need an SUDP to complete an assessment that is reasonably in the scope of
practice of another provider. A solution could include the capturing of necessary information by trained
professionals with supervision and oversight by credentialed practitioners, so that a shortage of SUDPs at
a given facility does not impede someone seeking SUD services from receiving an urgently needed
assessment
Ease of access improves engagement with services: According to the 2019 results of the Washington
State Syringe Exchange Health Survey
31
, among opioid users who had used opioids in the past week
(mainly heroin) and were somewhat or very interested in reducing their opioid use, most of them would
want methadone, buprenorphine, or naltrexone (70%) and withdrawal management services (54%) if
those services were easy to get (see graph from the report below). Low barrier treatment programs,
31
WA State Syringe Exchange Health Survey, 2019 Results | Addictions, Drug & Alcohol Institute (uw.edu)

93
SUBSTANCE USE AND RECOVERY SERVICES PLAN
informed by these clients’ preferences, utilizing buprenorphine at harm reduction programs found high
client uptake and engagement
32
.
Concerns and Considerations
● Role of SUDPs: Providing ASAM Criteria assessments is a significant aspect of the roles of
Substance Use Disorder Professionals (SUDPs). If these assessments are no longer used or needed
prior to initiating SUD care, it could reduce the demand for SUDPs and have a detrimental impact
on their employment opportunities and SUD agency financial viability. SUDPs are vital
contributors in the behavioral health workforce, and we want to ensure their role in providing
evidence-based care going forward. Their value extends beyond the ability to do assessments and
it is important to support their ability to do more valuable work to support people with SUD
including assessment, addiction counseling, case management and care navigation. However,
there is no existing requirement for the service provider to conduct an ASAM-specific
assessment, if the patient’s health plan can use information from the assessing provider to apply
ASAM criteria themselves. For higher acuity needs like withdrawal management, full ASAM
structure for assessments are not always needed, if the member meets criteria in ASAM
dimension 1 (acute intoxication/withdrawal potential) to medically authorize withdrawal
management in those cases.
● Maintaining objectivity: Shorter assessments that do not use ASAM criteria and the specific
decision pathways it provides may increase risk of subjectivity and bias in the assessment
process.
● Demonstrating “Medical necessity” based on level of care needed: There is a “medical necessity”
clause to receive money/be paid for services, depending on the type of care needed.
32
Care Navigation at Harm Reduction Programs: Community-Based “Meds First” Buprenorphine
Program Preliminary Data. | Addictions, Drug & Alcohol Institute (uw.edu)

94
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Regulatory and financial implications: The Treatment subcommittee recognizes that there are
regulatory and financial implications of replacing the ASAM with a shorter version of SUD
Assessment, such as determining whether and how the shorter assessments will be billed; such
details will need to be sorted out within HCA/DBHR.
● Multiple diagnoses and medical necessity: Often, what providers deliver in terms of care and
services are supportive interventions to address symptoms and behaviors. These symptoms and
behaviors are related to any number of diagnoses a client has, and they do meet medical
necessity. Additionally, there are many records and assessments that tell us that. Our current
rules and coding guidelines are precise and restrictive in ways that prevents access. The goal
here is to expand access and allow for interventions to be delivered by qualified professionals. A
consulting SUDP can provide the additional training, consultation, and record oversight.
● Reimbursement parity needed between SUD and MH: We have bifurcated BH treatment into MH
and SUD modalities but when treating symptoms and behaviors we should consider the value of
interventions traditional in the MH system, like CBT, DBT. There is not parity in reimbursement in
SUD system and contracting and credentialing make it challenging to access services in one
system rather than another. An integrated system would consider the interventions for
symptoms and behaviors rather than diagnosis. In other words, know our population, align
with the right services, and support access to additional interventions you are not able to
provide.
Collaboration with Existing Resources:
❖ Community partners: Collaborate with workforce efforts at two and four year higher education
schools. Coordinate with other behavioral health workforce efforts including those underway at
the UW’s Behavioral Health Institute.
Approximate Financial Support and Staffing Needed:
Dollars
FY23
FY24
FY25
Legislative / State Budget Funding
140,000
140,000
140,000
HCA Grant-Based Funding
Total Funds
Staff (FTE)
1
1
1
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

95
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix M – Recommendation 12: Stigma-reducing outreach and education, more importantly
regarding youth and schools
Recommendation – Provide education related to naloxone administration and overdose identification in
Washington State public schools (grade 6
th
– 12
th
) to reduce stigma and save lives. Intended audience for
this recommendation includes students, administrators, teachers, and other educational professionals.
Bill Requirement(s) – ESB 5476 section 1.3 (a)
Consideration of youth, rural areas, and tribes:
Youth: Youth in 5
th
grade and older would receive this stigma-reducing outreach and education
Rural Areas: Schools across the state, including rural areas, would receive this stigma-reducing outreach
and education
Tribes: Support existing stigma-reducing campaigns among tribes
Background and Supporting Data
Youth and Young Adults are overrepresented in substance use related mortality. Surveillance from the
Washington State Department of Health highlighted between 2019 to 2020, there was a 59% increase in
the number of drug overdose deaths among persons aged 24 and under, compared to the overall
population (all ages) an increase of 37.5%. The increase between 2020 to 2021 for the 24 and under was
9.8%.
With the dramatic increase in substance use mortality, it is imperative to improve response to overdose
and education among drug use with youth and young adults. This may be achieved through practical
strategies including, but not limited to naloxone distribution within school settings, overdose education,
evidenced-based drug safety curriculum starting at the 6
th
grade, and partnerships with other community
organizations that advance the health and well-being of young people.
Learning curriculums for young people that are evidenced based include Safety First.
Additionally, strong partnerships must be developed within the educational system ranging from
employers, tribal school boards, local districts, students, and the state to maximum practice and
procedure.
RCW 69.50.412: Prohibited acts: E—Penalties. (wa.gov) prohibits the distribution of a hypodermic
syringes to persons under the age of 18. This RCW prohibits entities and/or individuals from distributing
intramuscular syringes needed for naloxone administration. Intramuscular naloxone is currently
substantially cheaper than nasal formulations – being limited by cost and access of naloxone due to RCWs
may exacerbate any disparities of substance use mortality among persons under the age of 18. This law
will need a technical amendment to remove barriers to life saving medication.
Stocking a “standing order” (as defined in RCW 69.41.095) of “opioid overdose reversal medication” (e.g.,
Naloxone) is required via RCW 28a.210.390 to be stocked in high schools (grades 9-12) already for school
districts with more than 2,000 students. These medications can be administered by a school nurse, a
health care professional, or trained staff person located at a health care clinic on public school property
under contract with the school district, or designed trained school personnel. The opioid overdose

96
SUBSTANCE USE AND RECOVERY SERVICES PLAN
reversal medication may be used on school property, including the school building, playground, or school
bus, as well as during field trips or sanctioned excursions away from school property.
Funding would need to be provided to increase naloxone and overdose education among school aged
young people (6
th
grade – 12
th
grade), which includes funds related to outreach and communication.
Concerns are related to state authority to standardize this work. While the state does play a role, the
decision to implement these activities will belong to the local school districts.
This recommendation shall allow the stocking of naloxone at schools to be used in the event of an
overdose and allow school health staff to provide naloxone to students upon request in a confidential
manner.
Concerns and Considerations –
• If schools begin distributing Naloxone for use outside of schools, principals and superintendents
may come under fire/receive pushback from community. They would likely advise to find
another way to get naloxone to kids outside of schools, such as non-school clubs or athletics.
Another option would be to allow option for parents to opt in/opt out for their child’s
participation in such a distribution program
• Schools are inundated with extra/additional curriculum requests, and they are already behind on
executing the required curriculum from RCW (to create time to administer a new curriculum
longer than 30 minutes, would need to extend the school day). For this reason, finding ways to
weave essential, actionable information into existing curriculum could be more realistic. For
example, the topic of drug use and a short naloxone administration demonstration could be
integrated into existing social-emotional curriculum, as drug use is commonly a form of
emotional self-regulation/self-soothing.
• Alternate ways of promoting educational/informational messages should be explored that do not
require the schools to add to their curriculum (e.g., social media, paid media, etc.)
• Stakeholder opportunities with parents and custodians would be needed for the implementation
of this recommendation.
Collaboration with Existing Resources: Potential collaborating partners and stakeholders include:
School Districts/ School boards
Washington Office of Superintendent of Public Instruction (OSPI)
Washington State Dept of Health Overdose Education/Naloxone Distribution Program
Washington State Health Care Authority Overdose Reversal Medication Program (SB 5195)
Stigma-reducing campaigns for tribes, such as ONE
Local tribal districts
UW ADAI
Approximate Financial Support and Staffing Needed:

97
SUBSTANCE USE AND RECOVERY SERVICES PLAN
There are approximately 500,000 students in Washington in grades 6-12. Stocking enough naloxone in
each school for approximately 10% of students at a time (50,000) – with a clear process for ordering more
as needed -- would cost about $2.75 million dollars.
Funding related to outreach/communication strategies must be allocated in the amount of $5 million.
Funds will be evenly distributed to each local school district.
Additionally, funding for FTE at the department will be allocated in the amount of $200,000 – funds will
cover administrative and data components of naloxone distribution, utilization, and technical assistance.
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period
98
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix N – Recommendation 13: Law Enforcement and Behavioral Health data collection
Recommendation – Build upon, and provide ongoing funding for, a data integration infrastructure that
can receive and analyze standardized data gathered by law enforcement, courts, and prosecutors;
Recovery Navigator Program case management; behavioral health treatment services; and recovery
support services, to meet the mandates of Section 1.3(m).
Bill Requirement(s) – Per Section 1.3(m), this is a recommendation “regarding the collection and
reporting of data that identifies the number of persons law enforcement officers and prosecutors engage
related to drug possession and disparities across geographic areas, race, ethnicity, gender, age, sexual
orientation, and income. The recommendations shall include, but are not limited to, the number and rate
of persons who are diverted from charges to recovery navigator services or other services, who receive
services and what type of services, who are charged with simple possession, and who are taken into
custody.”
Background and Supporting Data
• The focus in this recommendation is on a general data infrastructure for reporting key indicators.
This may have substantial overlap with the data infrastructure required to administer diversion
and the RNP program, including tracking of prior diversions throughout the state as required by
law.
• Data is being collected in various sectors and programs related to substance use and behavioral
health systems (law enforcement encounters, treatment, recovery support services programs,
Recovery Navigator Program, etc.)
• Many of those data systems do not have a consistent identifier across systems, or consistent
standards for data collection and classification, which creates redundancies and makes it difficult
to link the data between sectors. This hinders understanding of the patterns taking place among
different communities and their outcomes following an encounter with law enforcement.
• Consistent data gathering and integration methodologies such as those described in this
recommendation would meet the data mandates of 1.3(m)
• A data integration infrastructure such as the one described in this recommendation has been
implemented in four LEAD pilot sites per RCW 71.24.589 (Whatcom, Snohomish, Mason, and
Thurston counties) and three Arrest and Jail Alternatives grantee sites per RCW 36.238A.450
(Olympia, Port Angeles, Walla Walla).
The data integration infrastructure should be able to gather, share, and report, at a minimum, the
following data elements, most of which are required per 5476 §1.3(m):
Data element Potential Source(s) Mandated per
5476
The number and demographic information of
incidents and unduplicated persons engaged by law
enforcement officers on diversion-eligible charges.
Law Enforcement Records
Management
YES

99
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The number and percentage of persons engaged by
LE on diversion-eligible charges who are arrested,
released, or diverted from charges via referral to
recovery navigator services
, along with the
demographics of both those stopped and those
diverted
(“Diversion utilization percentage” is a measure of
outcomes of all potential diversions)
Law Enforcement Records
Management
Case management records
YES
The number, percentage, and demographics of
diversion-eligible persons engaged by LE who are
diverted from charges via referral to
RNP or other
services
Law Enforcement Records
Management
YES
The number and demographics of diverted people
who
complete enrollment
in RNP
RNP Case Management YES
The number of persons receiving RNP
intensive
case
management
through RNP
RNP Case Management
The number of persons enrolled in RNP who have
received any SUD treatment and/or other support
services
Datasets from SUD
treatment and recovery
support services programs
(many services would not
be captured in claims data)
Provider One
RNP Case Management
YES
If simple
possession
remains
categorized
as criminal
activity:
Of those arrested for simple
possession, the number, rate, and
demographics of persons
charged/prosecuted for simple
possession
Prosecutors’ Offices / AOC
Washington State Courts
Judicial Information System
YES
Of those arrested for simple
possession, the number,
demographics, and rate of persons
booked into jail with charge of
simple possession
Jail records
WASPC/Provider One
Washington State Patrol
(arrest records)
YES
Of those arrested for simple
possession, the number,
demographics, and rate of persons
offered post-arrest diversion
Prosecutors’ Offices / AOC
Washington State Courts
Judicial Information System
Of those arrested for simple
possession, the number,
demographics, and rate of persons
Prosecutors’ Offices / AOC
Washington State Courts
Judicial Information System

100
SUBSTANCE USE AND RECOVERY SERVICES PLAN
receiving case disposition, including,
but not limited to, conviction
In addition to the data above, the following data should be collected and reported using this data
integration infrastructure for inclusion in the Recovery Navigator Quarterly Reports from HCA:
System utilization
• Use of emergency medical services
• Arrest, days in jail
• New charges with incident date after of referral to RNP (divided by felony,
misdemeanor), to be added to Case Management tab in RNP Data Collection tool
• Convictions with incident date after date of referral to RNP (broken into felony /
misdemeanor), to be added to Case Management tab in RNP Data Collection tool
• Access to and engagement with culturally appropriate, non-punitive, community-based
resources
System response
• Capacity and variety of local services aligned with RNP’s commitment to harm reduction
and holistic care
• Number and percent of substance-possession related law enforcement encounters (e.g.,
public order) that result in arrest, booking, and/or convictions for RNP-eligible behaviors,
as well as the demographics of those individuals engaged by law enforcement in these
encounters
• Racial disparity analysis that compares demographics of individuals who are arrested and
booked into jail, compared to the demographics of those who are referred to RNP,
among diversion-eligible individuals
Quality of life
• Self-report quality life/well-being
• Improved mental and physical health
Services and Access Gap Analysis: Indicated by comparing services needed/requested by RNP
participants, referrals made, referred services received by BH-ASO region, and reasons why
services were not received (if applicable). If the data collection burden for case managers is too
great for this level of analysis, request that case managers report areas where service gaps are a
persistent problem.
RNP Participant Satisfaction: Collected via survey every six months following enrollment in RNP,
with procedures in place outlining minimum and maximum contact efforts
Concerns and Considerations

101
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• A substantial investment is needed to secure the necessary software, staff to provide ongoing
technical assistance, and staff to collect, analyze, and report the data.
• We don’t have a list of the entities who are going to be collecting this information.
• The type of data these different organizations have, how they collect data, and specific types of
data needed from each source must be clarified.
• This work needs long-term consistent funding for implementation, collection, and analysis.
• Need to be considering privacy of data; all data collected should be used for specified purposes
and personally identifiable information should not be publicly available, especially to commercial
data brokers.
• Need to confirm whether IRB approval is needed for this type of data collection and reporting.
• All data elements mentioned in this recommendation will need time frames specified (e.g., past
30 days? 90 days? Yearly rates?)
• Care needs to be taken around assigning causation to these data or using these types of
measures as evaluation of efficacy of RNP or other system changes.
• Regarding the recommendation to include a measure of “Improved mental and physical health,”
a specific measurement tool still needs to be identified.
• Regarding the Services and Access Gap Analysis: This is a worthwhile area of inquiry, but it’s
operationally difficult. People may indicate desire for a service (public benefits, let’s say), but the
process of applying, getting denied (which is standard) and reapplying is time consuming and
onerous - usually requires a case manager to help navigate, an SSI specialist, and ongoing effort.
It’s not just a matter of a referral and an outcome.
• For data related to RNP service referrals, “referred” has no operationally consistent definition: Is
it somebody sent an email? Is the provider well-matched and culturally competent? Does the
service provider have capacity, respond to the request, know how to reach the individual (who’s
usually hard to find)? Does the service provider think that completing the referral (getting the
person connected) is their job, the client’s job, or someone else’s job? Does the referral remain
active, meaning somebody keeps working to make it happen? Does the referring agency track
and follow up to ensure the referred agency responds?
• The scope of data collection could be expanded to include other legislated diversion and jail
alternative programs (in addition to RNP)
• Methods to share data must be developed and scaled, including utilization of a common data set,
along with a common data model that automatically matches data fields across entities.
• This proposal doesn’t include other data sources that may be of interest, such as mobile crisis
response teams, the 988 line, and other crisis-level engagement programs.
Collaboration with Existing Resources:
Existing state services/programs
: This recommendation would involve both integration of existing
data streams across agencies, and support for implementing consistent data collection platforms
for recovery navigator programs as needed (where existing LEAD/AJA programs cannot be
leveraged)
Interagency involvement
: This recommendation would require cooperation between all law
enforcement agencies within the state, in addition to HCA, WASPC, local RNPs, local prosecutors,
AOC, and tribal courts.
102
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Community partners
: This recommendation would require collaboration with existing community-
based service providers who are operating as the case management agencies for RNPs, and other
pre-arrest diversion programs.
Related grants or other potential funding sources
: This recommendation would be most effective
if implemented in partnership with existing HCA, WASPC, and other locally- and federally funded
initiatives aligned with the collective impact goals and intentions of the RNP
Approximate Financial Support and Staffing Needed:
Implementation would require additional funding to support the following:
• Staff and technical experts sufficient to develop and lead data strategy, handle data integration,
and manage data interoperability while maintaining privacy and security.
• Staff to provide technical assistance for data collection and management to RNP sites and BH-
ASOs
• Staff and/or outside technical experts to analyze and report.
SURSA committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

103
SUBSTANCE USE AND RECOVERY SERVICES PLAN

104
SUBSTANCE USE AND RECOVERY SERVICES PLAN
105
SUBSTANCE USE AND RECOVERY SERVICES PLAN
106
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix O – Recommendation 14: Safe supply workgroup
Recommendation – Assemble a statewide workgroup to make recommendations on a framework for safe
supply for inclusion in the Washington State Substance Use Recovery Services Plan to provide a
regulated, tested supply of controlled substances to individuals at risk of drug overdoses. The workgroup
should center people who use drugs, with lived and living experience, and who have lost loved ones.
This workgroup should consider values of (1) non-commercialization, and (2) alternative lawful income
source for people who have been trapped in the illicit distribution economy and could be displaced by a
safe supply program, to prevent potential unintended consequences that would disadvantage
communities most impacted.
Bill Requirement(s) – Per 5476, this recommendation considers:
• Points of intersection that persons with substance use disorder have with the health care system
and locations in which persons with untreated substance use disorder congregate (§1.3.a)
• Barriers to accessing the existing behavioral health system and recovery support services for
persons with untreated substance use disorder, and possible innovations that could improve the
quality and accessibility of care for those populations (§1.3.d)
• Evidence-based, research-based, and promising treatment and recovery services appropriate for
target populations, including persons with co-occurring substance use disorders and mental
health conditions (§1.3.e)
Background and Supporting Data
The SURSAC has expressed broad support to establish a system to provide safe supply services in
Washington State. With the understanding that there are several models to explore and many important
implications and logistics to consider within those models, a special workgroup should be formed to
decide on the details for a model that fits the needs and concerns of Washington residents who will be
directly impacted by the implementation of a statewide Safe Supply system, including people who use
drugs.
On September 12
th
, 2022, the SURSAC voted to recommend decriminalization of possession of controlled
substances in Washington State. To realize the greatest public health, safety, and social benefit of this
recommendation, people will need to be able to access their substance(s) of choice in a form that is as
safe as possible to consume (safe supply) and to do so without interference (decriminalization). The
resulting system reduces harm associated with drug use, including overdose and incarceration.
33
Safe supply is defined as “A legal and regulated supply of mind or body altering substances that
traditionally have only been accessible through illicit markets.”
34
Research has shown that:
• Safe supply has been shown to greatly reduce the chance of overdose for those who receive it.
35
33
Addressing the Syndemic of HIV, Hepatitis C, Overdose, and COVID-19 among people who use drugs: The
potential roles for decriminalization and safe supply (2020)
34
Safe Supply — CAPUD
35
Evaluation of an emergency safe supply drugs and managed alcohol program in COVID-19 isolation hotel
shelters for people experiencing homelessness (2022)
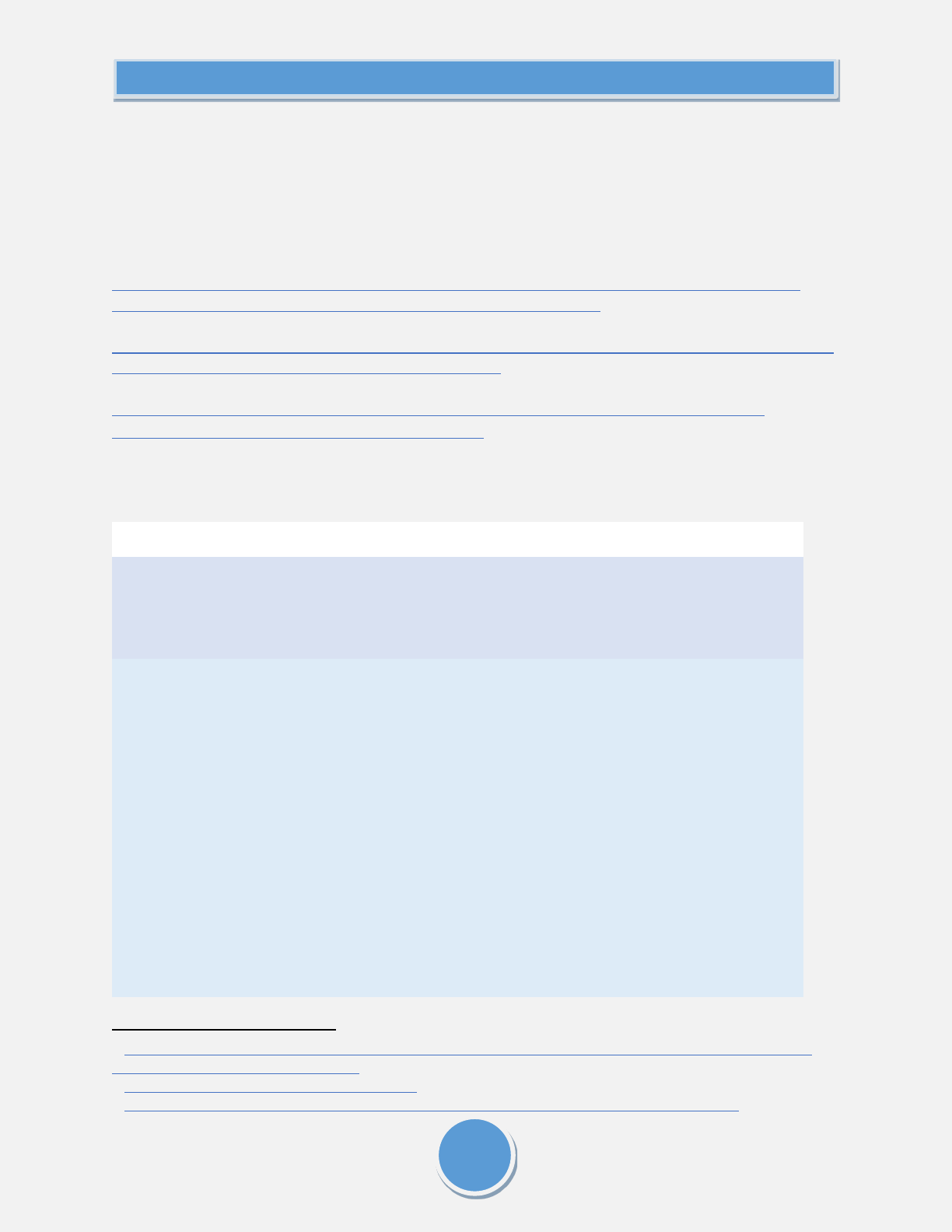
107
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Safe supply reduces riskier use and promotes safer use over time.
36
• Safe supply in certain models reduces theft, petty crime, and syringe litter. It also returns
autonomy and time to people’s day, and increases prosocial engagement with their
communities.
37,38
The following qualitative studies also demonstrate the value of these programs to their communities:
“People need them or else they’re going to take fentanyl and die”: A qualitative study examining the
‘problem’ of prescription opioid diversion during an overdose epidemic (2021)
“It’s helped me a lot, just like to stay alive”: A qualitative analysis of outcomes of a novel hydromorphone
tablet distribution program in Vancouver, Canada (2021)
Implementation of Safe Supply Alternatives During Intersecting COVID-19 and Overdose Health
Emergencies in British Columbia, Canada, 2021 (2022)
Below are four potential models for the workgroup to consider, as presented by Adam Palayew during
the SURSAC Special Meeting on September 9
th
, 2022:
36
Characterizing safer supply prescribing of immediate release hydromorphone for individuals with opioid use
disorder across Ontario, Canada (2022)
37
Safer supply pilot project findings - Canada.ca
38
Vancouver’s Unconventional Approach to Its Fentanyl Crisis - The New York Times (nytimes.com)
Table 1. Characteristics of different safe supply frameworks under consideration.
Scenario
Framework 1:
Prescription
(supervised
consumption)
Framework 2:
Prescription
(unsupervised
consumption)
Framework 3:
Buyer’s Club
Framework 4:
Dispensary (not for
profit/for profit)
Description
Drugs are
prescribed and
administered in a
supervised setting
under the care of
health
professionals
and/or peer
workers.
Drugs are
prescribed and
dispensed by a
health care
provider at a
dedicated
facility, but
PWUD have the
option to
administer it on
their own terms
outside of a
supervised
setting, such as
their own
Buyers Club:
Network of people
in community.
Pool money and
buy from a source
and then use that
to purchase drugs
in bulk, test them,
package them and
provide them back
to the community.
Buyers come
together and
collective
purchasing. (e.g.
Drugs can be made
available without
prescription in
dispensaries and
shops (e.g.,
cannabis). This model
can be run in a for
profit or a non-for
profit manner. There
can also be
restrictions who can
access these
locations including
based on age.

108
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Some safe supply features can be implemented in any of these frameworks
39
:
1. Licenses for purchasing, coupled with education
2. Signing of waivers acknowledging risk
3. Putting labelling on packaging about health messages and where to seek help if desired
4. Education related to use and accompanying harm reduction supplies
Concerns and Considerations
Some questions and concerns that arose following the Safe Supply 101 presentation on September 9
th
(starts at 00:55:30 in the meeting recording) are outlined below, with responses from Adam Palayew
(University of Washington).
Q: (Part 1) You can look at the reduction in death among people who participate in the program.
But how about people out in the community? So that's the first question.
A: There is ongoing work to try and find the answers to those questions. It's very hard to evaluate
because then you need to go and find people who got these diverted medications, which isn't
always easy. There is some qualitative research around it, nothing quantitative, but the
qualitative research is focused on some people getting diverted medications, and it was safer for
them. Some people call it diversion, a reframing of it would be secondary safe supply or
secondary treatment.
However, there is a real concern that people could be getting these medications, and then new
people using them. But I think the alternative is that they [new users] would just be accessing the
street supply instead of these medical grade medications or drugs. The issue becomes that
someone who's accessing the illegal supply is at a much higher chance of overdosing and dying
and not knowing what they're putting in their body versus one of these diverted medications. I
39
A public health based vision for the management and regulation of opioids (2021)
home, in take
home doses.
Dallas Buyers Club;
History of HIV
Meds). Grassroots,
no physical
location. Less
institutional
Delivery
Prescriber
Prescriber
Alternative
Alternative
Population
coverage
PWUD in contact
with health system
PWUD in
contact with
health system
All PWUD All PWUD

109
SUBSTANCE USE AND RECOVERY SERVICES PLAN
think diversion is a real issue. It's hard to quantify. I think there's both benefits and negative
consequences to it.
In some of the ongoing modeling work, there are threshold analyses being built in around
diversion that address what happens if 50% of drug use increases based off these models, what
happens if 100% increase? What happens if there's a 150% increase in people accessing these
drugs? You can change the amount of people that will increase and see at what point where your
model would say that more overdose deaths are happening because we're implementing this,
and so you can get out a number for what percent increase would need to happen for diversion
to be an issue at a population level.
Similar concerns have been raised about methadone and past analyses have looked at mortality
and poisoning data, particularly for children. Such poisoning events are extremely rare, and OTP’s
require patients to store take home medications in a lock box.
Q:
(Part 2) And the second question is the question about scale. I can see this being extremely
helpful for people, but at least my knowledge of the programs in Vancouver, in Zurich, is it's only a
small number of people. And given how big this current epidemic is we're in, I think it's important
to do everything we can, but it's also important to be realistic about how many people were going
to affect.
A: I think scale is an important issue. Safe supply has been tremendously successful for those
who've accessed it. However, as they've tried to scale it up, there's tons of barriers. Some
physicians have not been willing to prescribe it. They say it goes against their Hippocratic Oath.
There are pharmacists who refuse to fill prescriptions. It's hard for people to access it. It's also
only really been implemented for people with a substance use disorder, which is a limited
segment of the population that is at risk of overdose. Thinking boldly about models that are
widely accessible to people in terms of regulation like cannabis and alcohol is how you're going to
have the most scale and impact.
However, that also comes with more extreme options that we have for a safe supply. And I think
the prescriber based safe supplies can be thought of a lot as a continuation of treatment as we've
talked about before, where if you're giving someone heroin three times a day or twice a day,
similar to how they’re dispensing methadone. You need to dispense heroin more because it’s a
shorter half-life, but you basically have just another option for treatment for people to choose
from.
Q: You had mentioned the prescribe and take-home method and then I think you alluded to some
of the difficulties with that, having doctors willing to prescribe and pharmacists. Are there places
where that is successful right now? The reason why I ask is, just looking at my community, I can't
imagine a location where a clinic could go in where there wouldn't be total outrage by the
neighborhood. I'm intrigued by the prescribed and take home and so are there places where that
is being tried?
A: Yes, it has been tried in several places, and it's been very successful. Vancouver is one of them
as well as many places in Canada including Quebec, Ontario, and Nova Scotia. I presented some
of those results. There's also published data from Switzerland where they found that both by

110
SUBSTANCE USE AND RECOVERY SERVICES PLAN
relaxing the take home requirement instead of having people come to the clinic every day, they
both increase the number of people they were able to expand it to, because it allowed more
people to accommodate it in their lives, as well they didn't have any increase in negative
outcomes with the program. It's being done successfully. There are multiple places in Canada and
those references and evidence are in the slides.
On the other hand, you're talking about the political reality of this, and would it be acceptable
and all of that? And I would say you can't know until you try. I completely agree that there will be
a ton of political backlash if one of these are implemented. I think we could all see the headlines
already of what would happen. Someone made a comment in the chat about, dare I ask, who's
paying for this? And I would say that implementing safe supply, I think is going to end up being
cost saving because you're reducing the burden on the medical system by a large amount.
A lot of this evidence now is going to be coming out looking at cost effectiveness or cost savings
with these programs that have been operating for over a year now in other countries, and what
were the economic impact of them.
It's a tough sell. There will be political opposition. But people's lives are at stake. I think this is
something that's been shown to be successful, that has a lot of evidence behind it. And I think we
should be doing and thinking, doing bold action, and thinking boldly about how to keep our
community safest.
Cost analyses would need to look at total societal costs, not just health care system costs to see
the total impact of such a program.
Q: Where do supply testing options fit into any of these models like options for testing street
supply?
A: Testing for the street supply is important because people would still be using the street supply
in some of these models. But drug testing is a reaction to the fractured street supply and how
dangerous it is; we don't go test our alcohol, we don't test our cannabis, we don't test our coffee
for dosage and purity. In an ideal world where safe supply is properly implemented, drug testing
could take a back seat, which again goes to reinvesting resources that are allocated for different
interventions to things that could replace it.
Q: Is there a reduction in crime, in burglaries, and law enforcement issues in those areas where a
safe supply was created? Is one of the metrics the number of individuals who have been
diagnosed, and those who have become addicted to those drugs? Because a safe supply is great
for those who are already in that world, and who are already addicted. But if the safe supply is
promoted, and all it does is create more addicts, then I'm not sure that is quite the direction we
want to go. But I do like the idea for addressing the people who already have that addiction.
A: In terms of the reductions in crime, I would say there hasn't been any spatial analysis where
they look at the neighborhood level and these programs. However, in the data that I was
referring to, they directly asked the participants –did you commit, more crime, less crime, did you
commit any crime as well to get your drugs – and asking how their behavior individually changed,
but there hasn't been any neighborhood level studies that have been done around crime and

111
SUBSTANCE USE AND RECOVERY SERVICES PLAN
burglary and law enforcement, for safe supply yet. There's only the individual level data as of
now. It's always hard to look at the neighborhood level data to then extrapolate to the individual
level. There's so much going on that influences what's happening at that macro scale. [There are
research approaches to investigating neighborhood crime associated with different types of
venues such as bars, OTP’s, and convenience stores
https://www.jsad.com/doi/10.15288/jsad.2016.77.17 ]
And in terms of safe supply for those who don't use, I agree that you need to think about the
alternative. I know it could be a little uneasy that people who don't use drugs could be accessing
these drugs, but if we think about our 20-year-old linebacker who died, in the prime of his life in
college, he used the street supply trying to access Xanax where he didn't know what he was
getting, and that's truly the alternative to a safe supply: our current status quo where people are
accessing illegal supply that is from a very fractured supply, that has a ton of contaminants.
It may be uncomfortable, but are we OK with letting people use drugs die knowing that they're
going to use drugs? We need to give them a safe alternative, like what we've done with alcohol.
Rep Davis made a really good point about the commercialization of alcohol, which I think is a
really important point; we need to think about how you legalize these in terms of restrictions on
advertisement restrictions on making profits, because when these were more widely available in
the early 2000s, there was a lot of deceit in advertisement that was going on, and it was really
dangerous and really damaging to the public health. And so I think we need to be very careful in
how we legalize this and offer a safe supply, thinking about designing these systems to better the
public health, instead of making it into a type of capitalistic feeding frenzy. [Concerns were raised
at the meeting and have been raised publicly that the cannabis market in Washington State has
been very poorly regulated, with profit driving perverse incentives e.g. high potency products and
that we would definitely want to avoid the negative impacts of the market structure currently
seen with cannabis in WA.]
Comment: Let’s remember that's we've had safe supply for 70 years, and that is in the form of
other treatment medications. So safe supply isn't really safe supply, it is medications, right?
Methadone is a full opiate agonist. All we're talking about is other types of full opiate agonist.
Research in Canada has examined the use of hydromorphone (e.g. Dilaudid) and diacetylmorphine
(aka heroin) https://pubmed.ncbi.nlm.nih.gov/27049826/ . We're just trying to fight a fight of a
brand new super synthetic high potency drug with tools that are 70 years old and all that we're
talking about is bringing their tools and other medications into the mix. The reason why we're in
this problem of fentanyl and especially in counterfeit pills, is because we did so much to tamp
down on prescribing practices that we took a fully regulated supply on, and we got rid of it. We
created this inadvertent marketplace for a really contaminated drugs in public health. One of the
questions I get all the time is do we have fentanyl in marijuana and that is such an easy question
to answer here in the state of the Washington. And the answer is no. Almost across the board, No.
And the reason is because we have end to end quality control on that; when we don't have end to
end quality control, we create this marketplace for this toxic drug.
Collaboration with Existing Resources: To implement safe supply services, collaboration will be needed
with:
Doctors and other prescribing medical providers

112
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Pharmacies and pharmacists
Insurance providers
Approximate Financial Support and Staffing Needed: To be determined by workgroup
Dollars
FY23
FY24
FY25
Legislative / State Budget Funding
HCA Grant-Based Funding
Total Funds
Staff (FTE)
0
0
0
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

113
SUBSTANCE USE AND RECOVERY SERVICES PLAN

114
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix P – Recommendation 15: Expanding funding for OTPs to include partnerships with
rural areas
Recommendation – Increase access to opioid treatment program (OTP) services in rural areas
Definitions to know for recommendations
Opioid treatment program
- An opioid treatment program (OTP) is a behavioral health treatment
agency which is licensed by the state and federal government, and in accordance with RCW 71.24.590
and 42 CFR § 8.11. OTPs offers both counseling services and medical services to all clients who attend.
It is the only type of outpatient treatment setting, where an individual can receive all three types of
medication for the treatment of an Opioid Use Disorder: Methadone, Buprenorphine products
(Suboxone, Subutex), and Naltrexone (Vivitrol). A client who attends an OTP receives their MOUS
medication and doses to take home directly from the OTP site, instead of a pharmacy. There are no
prescriptions.
To provide this array of services, OTPs have multidisciplinary treatment teams that include: Prescribing
practitioners (i.e., medical doctors, doctors of osteopathy, advanced registered nurse practitioners,
physician assistants); Nurses (i.e., licensed practical nurses and registered nurses); and Counselors
(SUD professionals)
• Opioid treatment program guide (wa.gov)
OTP Medication Unit
- According to 42 CFR § 8.11(i)(1), a certified OTP may establish a medication unit
or units to administer or dispense medication therapy. The state and federal licensed OTP assumes all
responsibilities for any medication units associated with it. Such a unit is intended to facilitate access to
medication-assisted treatment for patients who would otherwise have to travel great distances. These
medication units under federal law can be (1) located as a free-standing facility; (2) co-located within in
a variety of community settings such as but not limited to hospitals/medical primary care
systems/pharmacies/FQHCs etc.; and (3) located as a mobile medication vehicle.
Detailed recommendations for consideration:
1. Require the Dept. of Health’s Health Services Quality Assurance (HSQA) division create a
regulatory workshop with OTP provider stakeholders in 2023 to:
Create state rules/regulatory process for OTP that want to establish offsite medication units (1)
located as a free-standing facility; (2) co-located within in a variety of community settings such as
but not limited to hospitals/medical primary care systems/pharmacies/FQHCs, as well as
correctional health settings, etc.
• DOH already has set up a regulatory process for OTP to apply for mobile medication units
specifically, but not other types of medication units.
• DOH should set up a process for regulating and establishing all types of OTP medication
units allowable under federal law.
• Ensure DOH includes invited stakeholders from geographic regions areas of WA with
lower population density, Eastern Washington, rural, tribal nations, etc. This way DOH
can ensure decision making is done in a more equitable manner that is inclusive of

115
SUBSTANCE USE AND RECOVERY SERVICES PLAN
important stakeholder partners who may be impacted by changes proposed to help their
communities.
Goal: To increase number of OTP and methadone access in Central and Eastern WA and/or rural
areas
Requires: Regulatory changes, and directive to State Agency- Dept. of Health
2. Change RCW 36.70A.200 and WAC 365-196-550 to ensure that OTP branch sites of all kinds
(including mobile, and fixed, site medication units) are clearly seen as “essential public facilities”
and that they cannot be zoned out or stalled by moratoriums by City and/or County legislative
authorities.
• RCW 71.35.590(b) references that OTP are to be seen as an essential public facility
• However, RCW 36.70A.200 and WAC 365-196-550, which are written to define “essential
public facilities” are written in a way that many City and County legislative Authorities,
and their respective planning commissions have reported as being less than optimal in
clarity, if opioid treatment programs are included.
• Updating RCW 36.70A.200 and WAC 365-196-550 to be explicit that opioid treatment
programs are clearly defined as a “essential public facility” type would help city and
county legislative authorities in their confusion, and hopefully help to assert that our
continuum of care values this provider setting as “essential” brining dignity and equity to
patients, declaring this is the same setting type as other healthcare setting types.
• Washington State Opioid Treatment Authority has had to interact with many City and
County Legislative Authorities and their respective planning commissions on this topic,
and often local municipalities want to create zoning requirements for OTP that are
different and more burdensome than other behavioral health and/or physical health
setting types.
For example, many local municipalities have set up burdensome moratoriums
before decision making and/or stigmatizing public comment periods specifically
for prospective OTP providers, before allowing zoning feedback for opioid
treatment programs that should be treated the same as other healthcare
facilities.
Recently 4 King County Cities would not allow a prospective OTP mobile
medication unit to bring services to their cities, and several of the cities talked
with the OTP about the need to set up moratoriums while they wait to decide if
the OTP mobile medication unit should be zoned as a “food truck” and/or
threatened to not allow them a permit to operate in a mobile capacity within city
limits saying they needed to be zones as a “permanent” structure.
• Clearer state laws and rules on this topic would help local municipalities to make
decisions with their respective planning commissions and help to bring much needed
MOUD/methadone treatment to communities that previously have not had access to
MOUD/methadone.

116
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Goal: To increase number of OTP in Central and Eastern WA and/or rural areas, bring more
alignment with state and federal civil rights laws like ADA and WLAD, and bring more equity and
dignity and respect for patients
Requires: Regulatory Changes, and changes to RCW and WAC
3. Update RCW 71.24.590 to remove several requirements for the siting of opioid treatment
programs that stigmatize the treatment setting type and treat it in ways that other SUD
behavioral health agencies and health care facilities settings are not.
This would include removing the largely symbolic RCW requirement in RCW 71.24.590(2) that
allows a county legislative authority to cap the patient census of an OTP specific setting, at no
less the 350 individuals.
This would include removing all OTP public hearing requirements in this RCW, that describe how
DOH must facilitate a public hearing in the community which an OTP will be cited in, before a
new OTP can open to operate.
Consideration for resources to help create opportunities for public engagement that center
patients and prospective patients at educational opportunities for the general public. Include a
community engagement process that seeks to reduce stigma around those with substance use
and has a primary goal to center and protect patients through education related to sharing
evidence-based treatment outcomes related to OTP.
• Recommend removing all “patient census cap” language in this RCW. Instead, specifically
state that “no city or county legislative authority can create a patient census cap” at an
OTP.
• Possibly tie a reference into any changes to RCW, related to the previous
recommendation that an OTP be noted clearly as a “essential public facility” and assert
clearly that they need to be treated like any other essential public healthcare facility and
be privy to the same reasonable conditional use requirements as other health care
settings.
• Remove all OTP public hearing requirements in this RCW, as DOH is legally required to
license any qualified treatment setting provider and causing OTP to need to go through
public hearings is not a good use of taxpayer dollars, adds time and burden to providers
who seek to become licensed by Washington State to open an OTP and allows for further
stigmatization against this setting type in the communities where they operate.
• No other behavioral health agency setting type, or medical setting type needs to undergo
an RCW mandated public hearing facilitated by WA DOH HSQA staff. Why are OTP being
treated differently than any other SUD Behavioral Health Agency (BHA) provider type? It
is stemming from a history of stigma and “othering” that needs to end.
• The siting of OTP treatment settings should be treated in a manner similar to the siting of
other behavioral health agencies, and health care facilities in Washington State.

117
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Goal: To increase number of OTP in Central and Eastern WA and/or rural areas, bring more
alignment with state and federal civil rights laws like Americans with Disabilities ACT (ADA) and
Washington Law Against Discrimination (WLAD), and bring more equity and dignity and respect
for patients
Requires: Regulatory Changes to RCW 71.35.590
4. Funding for capital construction costs to help start up OTP in Central and Eastern- WA
A model of funding already exists where Dept. of Commerce has been given funds by the WA
Legislature to help with capital construction costs to build recovery housing/transitional housing
stock- Perhaps a similar model should be offered to help cover capital construction costs to build
new OTP.
• The service delivery and treatment services of an OTP are already insurance
reimbursable, so the request for funding would go to helping with capital construction,
startup costs only to help bring an OTP to specific regions of the state that currently lack
OTP/methadone access.
• Recommendation could easily be scaled upward and downward and implemented in a
targeted region(s).
• Please see high level estimated budget costs below.
• More detailed cost estimates could be available from HCA staff upon request in the event
the Legislature seeks to fund this.
• Could also be recommended as a use of opioid settlement funds, GSF etc.
• There should be support for provider evaluation of outcomes
Goal: To increase number of OTP in Central and Eastern WA and/or rural areas, bringing
treatment to new populations who have previously not had access to MOUD/methadone.
Requires: Resources and funding and legislative directives with State Agency- Dept. of Commerce.
5. The Governor’s Office and/or Legislature should provide funding to a State Agency such as WA
Health Care Authority to provide an RFI/RFP to resource established OTP in Washington State to
operate an increased number of OTP medication units to expand their geographic reach
These medication units could be established in a variety of forms. (1) Located as a free-standing
facility; (2) co-located within in a variety of community settings such as but not limited to
hospitals/medical primary care systems/pharmacies/FQHCs etc.; and (3) located as mobile
medication vehicles.
This could be done to extend the geographic reach of OTP and bring medications for opioid use
disorder, counseling, and other recovery support/SUD treatment services to greater geographic
areas and to literally meet novel patient patients where they are at.

118
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• WA Legislature funded 5 OTP mobile medication units in the State of WA.
Implementation is in the works at the present time.
• Recommendation could easily be scaled upward and downward and implemented in a
targeted region(s).
• Please see high level estimated budget costs below.
• More detailed cost estimates could be available from HCA FSD staff upon request in the
event the Legislature seeks to fund this.
• Also, could be recommended as a use of opioid settlement funds, SABG, SOR and GSF
funds.
o There should be support for provider evaluation of outcomes
Goal: To increase number of OTP and methadone access in Central and Eastern WA and/or rural
areas, bring treatment to new populations who previously have not had access to
MOUD/methadone.
Requires: Resources and funding, and legislative directives.
Bill Requirement(s)
This recommendation establishes new community-based care access points (1.3.b), expands regional
capacity for treatment via opioid treatment programs (1.3.c), and removes geographic barriers to
accessing OTPs (1.3.d).
Background and Supporting Data
Washington State is experiencing a fentanyl-driven overdose crisis. Current trends shown on the
Washington State Department of Health (DOH) Opioid Overdose website suggest the total number of
overdoses will be the highest recorded. Fortunately, there are effective medications for the treatment of
OUD.
While two of the three Food and Drug Administration (FDA)-approved medications can be prescribed in a
primary care office, OTP behavioral health agencies are the only outpatient treatment setting where
federal law permits the use of all FDA-approved medications for the treatment of OUD: methadone-,
buprenorphine-, and naltrexone-containing products.
Methadone is described as a “full agonist”, meaning it completely binds to and fully activates opioid
receptors in the body. It is the most potent FDA-approved medication allowed for the treatment of OUD.
It can only be dispensed for the treatment of OUD in an outpatient OTP or “methadone clinic”.
Buprenorphine, which can be prescribed outside of OTPs, also occupies the opioid receptor, but it is not
as potent as methadone. This is an important distinction to highlight. Buprenorphine was developed to
treat OUD, when heroin and prescription opioids were the primary substances being used by people with
OUD. Because fentanyl is a much more potent opioid than heroin or oxycodone, many people using
fentanyl require methadone medication to treat their OUD, increasing the need for services provided in
OTPs.
As of September 1, 2022, there are 32 OTPs in Washington State, each serving between 200 to more than
1,000 patients. There is no federal rule limiting the number of individuals an OTP can serve, but state law

119
SUBSTANCE USE AND RECOVERY SERVICES PLAN
in RCW 71.24.590(2) does allow counties to set patient census limits (i.e., maximum capacity for a
program).
5 of the 32 OTPs are owned and operated by Washington State Tribes (i.e., Lummi, Muckleshoot,
Stillaguamish, Swinomish, Jamestown S’Klallam).
OTPs in Washington State collectively serve more than 14,000 people with a primary OUD diagnosis.
Using information from the HCA Opioid Use Disorder Treatment for Medicaid Population dashboard, 15%
of people with Medicaid being treated for OUD are receiving care in OTPs.
Access to methadone is not equal across the state. Few programs exist in central and eastern
Washington.
Below is a map created for HCA by the Pew Charitable Trust representing areas of Washington State with
significant gaps in the treatment continuum for patients looking or methadone medication access in
opioid treatment programs.
As you can see, most of Central, Eastern and/or rural Washington is 2, 3, or 3+ hours drive time away
from an OTP and thus methadone medication for the treatment of OUD.
Given the increased potency of fentanyl, the need to use methadone as the most potent opioid
replacement therapy is expected to increase. As OTPs are the only agencies allowed by federal law to
treat people experiencing OUD with methadone, this report has become more relevant. The need to
provide standardized, high-quality care in OTPs that meets federal and state requirements has never
been more important.
Concerns and Considerations
There was zero dissension of any kind from any of the SURSAC Treatment subcommittee members, when
these recommendations were offered in the SURSAC Treatment Subcommittees on August 23, 2022, and
September 6, 2022.

120
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Additional Feedback from SURSAC Treatment subcommittee members included:
• If work happens with DOH for OTP rulemaking- To please ensure DOH includes invited
stakeholders from geographic regions areas of WA with lower population density, Eastern
Washington, rural, tribal nations, etc. This way DOH can ensure decision making is done in a more
equitable manner that is inclusive of important stakeholder partners who may be impacted by
changes proposed to help their communities.
• Request that one of the SURSAC subcommittees should take up a future a recommendation to
find a way to include syringe service programs as a facility setting type that would benefit from
protection under RCW as a “essential public facility”
• Request that one of the SURSAC subcommittees should take up in the future a recommendation
MOUD in jails specific setting recommendation to support increased methadone access in jail
settings.
• Request that one of the SURSAC subcommittees should take up in the future a recommendation
to address more thoroughly and holistically whole person health needs (physical, mental health,
SUD) of individuals in any setting of incarceration (Jails and Prison and JRA settings)
Collaboration with Existing Resources: How can this recommendation collaborate with existing services /
programs / resources?
Existing state services/programs:
• Opioid treatment programs are already a behavioral health agency setting type that exists,
are clearly defined in state and federal law, and offer both medical and counseling services to
patients making them fully in alignment with the state’s goals of offering integrated care
settings to Washingtonians.
• Opioid treatment programs are existing and insurance reimbursable integrated behavioral
health services under Medicaid, Medicare, and all other third-party insurance payers.
• There are already 32 opioid treatment programs in Washington State as of 9/20/22.
• Opioid treatment program guide (wa.gov)
Interagency involvement:
• These recommendations involve changes that would require work from the Washington State
legislature, Washington State Dept. of Health, Washington State Health Care Authority,
Washington State Dept. of Commerce, and Washington State DOC to implement. Partners
are dependence on the respective recommendations.
Community partners:
• Licensed behavioral health agencies that are opioid treatment programs
• Other entities that can refer to opioid treatment programs, including primary care providers,
hospitals, emergency departments, FQHCA, rural health clinics, behavioral health agencies,
office based opioid treatment settings, syringe service programs, Hep C/HIV providers,
settings that help drug user health locations, etc.
• There are also currently 5 tribally owned and operated OTPs in Washington State, the most in
the nation, serving both tribal member and non-tribal affiliated patients in their communities.
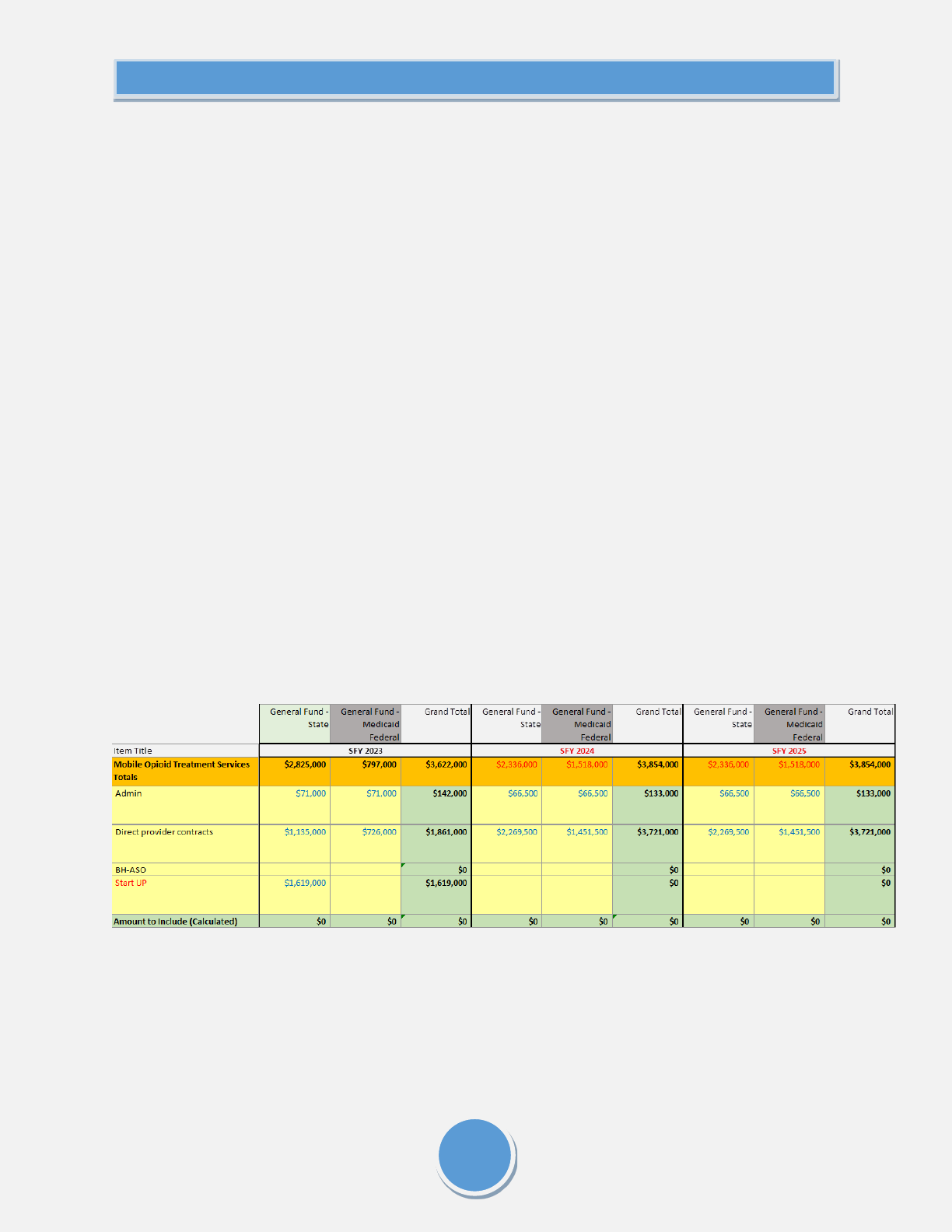
121
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Related grants or other potential funding sources:
• Many of the recommendations are regulatory in nature and do not require funding
• The recommendations where is funding required could be funded through GSF, opioid
settlement funds, and one specific recommendation could also potentially be assisted with
use of SABG funds and SOR funds.
Approximate Financial Support and Staffing Needed:
For the OTP Capital construction Costs with Dept. of Commerce recommendation:
As per opioid treatment program Providers:
o As per initial provider feedback: $600,000 up to $1.2 million per OTP to remodel an
existing structure and turn into an OTP that could be leased to a provider
o As per initial provider feedback: $1.2 million up to $2.4 million to build from scratch an
OTP that would be owned and operated by an OTP provider.
o Dept. of Commerce would need an TBD FTE to help implement
o Dept. of Commerce Financial staff would need to do modeling of whatever final amounts
would be requested; variables will differ based on a large number of TBD factors.
For the increasing OTP medication unit proposal with WA Health Care Authority recommendation:
• WA Legislature provided HCA with funds in 2022 to bring up to 5 OTP mobile medication units in
the State of WA.
• Costs covered capital, start up and staffing costs in an ongoing manner. Implementation is in the
works at the present time.
Below is a summary by year of amounts budgeted for the 5 mobile OTP project. They are rounded to
nearest 1000.
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

122
SUBSTANCE USE AND RECOVERY SERVICES PLAN

123
SUBSTANCE USE AND RECOVERY SERVICES PLAN

124
SUBSTANCE USE AND RECOVERY SERVICES PLAN

125
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix Q – Recommendation 16: Addressing zoning issues regarding behavioral health
services
Recommendation – Addressing outdated language regarding recovery houses licensing and zoning
barriers affecting treatment, harm reduction, and recovery support services.
Bill Requirement(s) –5476 Section 1.3 (a),(c),(d),(j)
Background and Supporting Data:
This recommendation addresses outdated language regarding recovery residence licensing and zoning
barriers affecting treatment, harm reduction, and recovery services, as well as the inconsistency between
state, county, and city/town regulations regarding zoning for these types of facilities.
A blanket statement from the state level would provide considerable changes to these areas in regard to
providing adequate space for treatment, harm reduction, and recovery support services.
Currently, WAC 365-196-550 outlines essential public facilities when it comes to community development
regulations. Siting these essentially public facilities are outlined in RCW 36.70A.200 which states that
county and city planning includes a process for identify and siting the facilities that are named under the
WAC and RCW which includes inpatient facilities including substance ‘abuse’ facilities, mental health
facilities, group homes, and community facilities. It is left to the discretion of the city and county to identify
and site these locations within their areas.
Oftentimes, this provides city and counties to not provide adequate services due to the lack of appropriate
identification and appropriate language of the services that are needed to address the substance use,
mental health, and co-occurring population.
The language should be updated to include in-patient, out-patient, recovery residences, harm reduction
(including SSP), community-based, and treatment related programs, including OTPs and mobile treatment
services. Furthermore, there should be consistency, regardless of demographic, for enforcing cities and
counties to provide the maximum amount of services within their regions.
Recovery Residences should be defined as: Recovery housing can range along a continuum of four non-
linear levels described by the National Association of Recovery Residences (NARR). These levels range from
peer-run establishments like Oxford Housing (level I), to monitored sober living homes (level II), to
supervised housing (level III), and residential treatment housing (level IV). While recovery residences vary
widely in structure, all are centered on peer support and a connection to services that promote long-term
recovery.
Recovery housing benefits individuals in recovery by reinforcing a substance-free lifestyle and providing
direct connections to other peers in recovery, mutual support groups and recovery support services.
Substance-free does not prohibit prescribed medications taken as directed by a licensed prescriber, such as
pharmacotherapies specifically approved by the Food and Drug Administration (FDA) for treatment of opioid
use disorder as well as other medications with FDA-approved indications for the treatment of co-occurring
disorder.
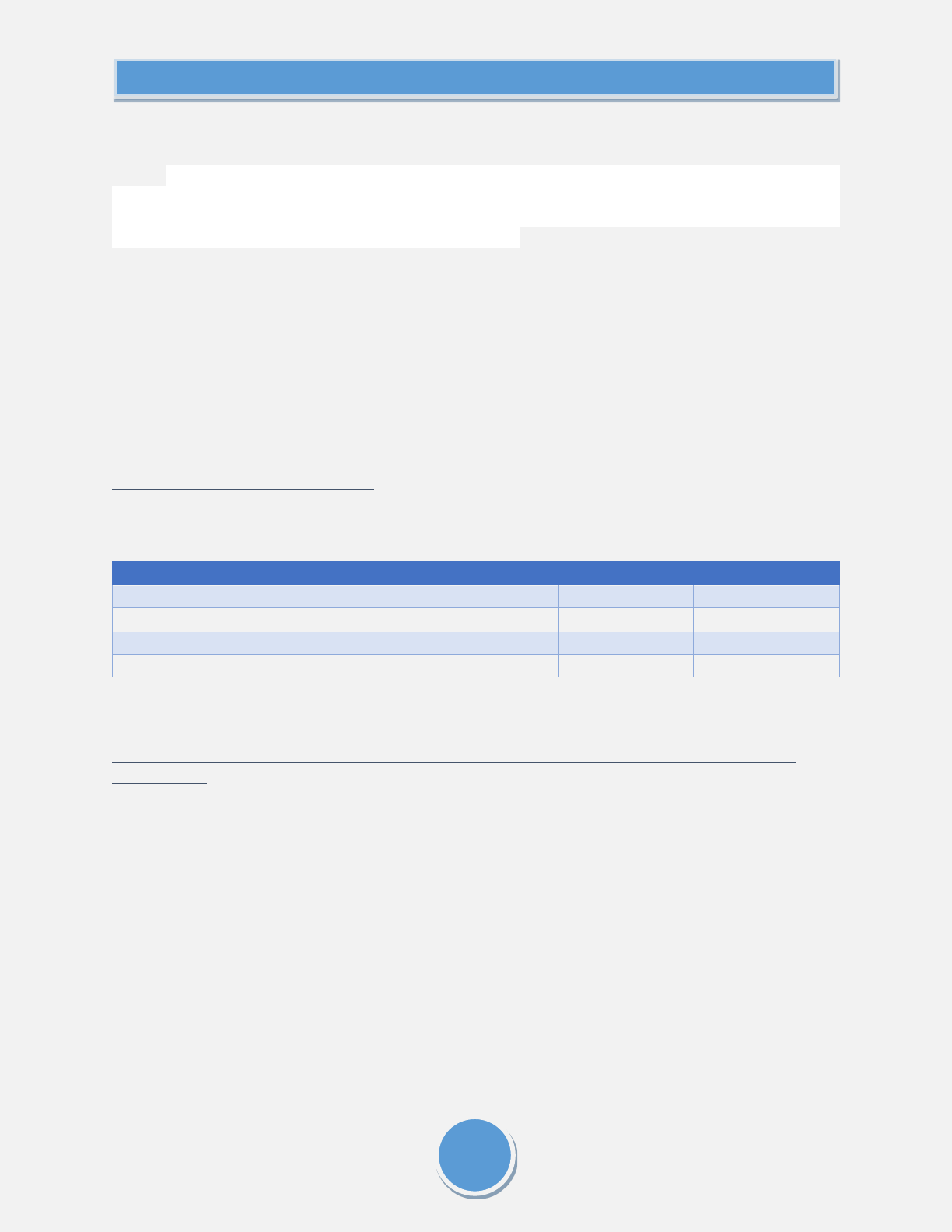
126
SUBSTANCE USE AND RECOVERY SERVICES PLAN
To further this recommendation in efforts to support harm reduction services in Washington, the
subcommittee recommends adopting similar language to California Health and Safety Code 11364 which
states “a public health measure intended to prevent the transmission of HIV, viral hepatitis, and other
bloodborne diseases among persons who use syringes and hypodermic needles, and to prevent subsequent
infection of sexual partners, newborn children, or other persons, this section shall not apply to the possession
solely for personal use of hypodermic needles or syringes.” Allows for providing supplies to reduce harm
associated with SUD, which includes safe smoking supplies.
To help facilitate the changes to zoning regulations, we believe municipal officials would benefit from
orientation to the services we are recommending be sited in their jurisdictions. When given adequate
information and statistical data, officials would be better able to make informed changes for their
communities to address the current substance use crisis. Educational campaigns should be provided to
city and county officials and communities to provide valuable information regarding the services that may
be sited in their areas. Stigma and misunderstanding can cause resistance that could hinder the
expansion of vital services.
Collaboration with Existing Resources:
N/A
Approximate Financial Support and Staffing Needed:
Dollars
FY23
FY24
FY25
Legislative / State Budget Funding
HCA Grant-Based Funding
Total Funds
Staff (FTE)
8
6
6
SURSA Committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

127
SUBSTANCE USE AND RECOVERY SERVICES PLAN

128
SUBSTANCE USE AND RECOVERY SERVICES PLAN

129
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix R – Recommendation 18: Continuum of Housing
Recommendation – The SURSAC urges the state to provide capital budget and operating funding for
options for housing at the various points of intersection along the continuum of care for housing people
who are currently using to those who are in recovery, which may or may not include abstinence, from
immediate shelter to bridge/transitional housing through long-term permanent housing. It is urgent that
the Legislature fund a continuum of housing and housing services for individuals who use drugs and those
who are abstinent. The resources need to include capital and operating investments.
Participation in, and collaboration with, work on these topics already being done is also encouraged,
including but not limited to:
• Permanent Supportive Housing Advisory Committee, established per HB 1724v
• Behavioral Health Housing Action Plan
• Washington State Health Care Authority
• Washington State Department of Health
• Washington State Department of Commerce
• Low Income Housing Institute
• The Washington Alliance for Quality Recovery Residences
• Public Defender Association (PDA) CoLEAD/JustCARE
• Evergreen Treatment Services REACH Program
• Downtown Emergency Service Center
• Plymouth Housing
• Catholic Community Services
Participation and collaboration in this work should include bringing forth known models and systems for
consideration, such as:
• Extending the Housing and Recovery through Peer Services program (HARPS)
• Expanding longer-term rental resources
• Building on the work from the Permanent Supportive Housing (PSH) advisory group, Behavioral
Health Housing Plan, AHAB housing needs assessment, and other ongoing efforts to address
housing needs
• Replicating the JustCARE model of immediate placement in bridge housing and creating
permanent housing placements via coordination with Coordinated Entry teams (now being
employed by King County Regional Homelessness Authority to respond to individuals living on
state transportation rights of way under contract with the Department of Commerce)
• Creation of state or local long term housing voucher programs for up to 100% of housing costs
• Leveraging existing sources of funding for housing
• Crisis stabilization housing for those waiting for a withdrawal management/detox or an inpatient
treatment bed
o Outreach programs that assist individuals in accessing treatment often use motel/hotel
vouchers while someone is waiting for inpatient treatment; however, these funds are not
always available

130
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Housing for those who have an active drug addiction and/or a mental health disorder
• Recovery-supportive housing for those who are in recovery or seeking recovery from substance
use disorder
• Master leasing as a strategy to address the affordable housing crisis
• Government-subsidized housing for persons receiving Medications for Opioid Use Disorder
(MOUD) as part of active treatment (e.g., Kate’s House model) Level 1 and Level 2 recovery
residences.
This is the registry of Level 1 and 2 recovery residences in Washington State.
Counties with no Level 1 or 2 residences listed are: Jefferson, San Juan, Pacific, Lewis,
Wahkiakum, Skamania, Klickitat, Ferry, Stevens, Pend Oreille, Lincoln, Adams, Whitman
(no data available to confirm), Columbia, Garfield, Asotin
• Obtaining additional grant funding to expand current accredited and reputable operators to
develop recovery residential options for the regions indicated above (counties with no level 1 or 2
residences, according to the online registry), and expand residential options into these areas for
underserved and marginalized communities.
• Amending RCW 59.18.030 as part of transitioning individuals from long-term or supportive
housing into permanent housing, such as by adding the underlined language provided in the two
following examples:
(5) "Criminal history" means a report containing or summarizing (a) the prospective tenant's
criminal convictions, not including criminal convictions related to Unlawful Possession of
Controlled Substances under RCW 69.50.4013 and pending cases, the final disposition of which
antedates the report by no more than seven years, and (b) the results of a sex offender registry
and United States department of the treasury's office of foreign assets control search, all based on
at least seven years of address history and alias information provided by the prospective tenant or
available in the consumer credit report
OR
(5) "Criminal history" means a report containing or summarizing (a) the prospective tenant's
criminal convictions, not including all drug-related convictions and pending cases, the final
disposition of which antedates the report by no more than seven years, and (b) the results of a sex
offender registry and United States department of the treasury's office of foreign assets control
search, all based on at least seven years of address history and alias information provided by the
prospective tenant or available in the consumer credit report.
• Reducing financial barriers to securing permanent housing posed by the cost of housing
applications, background checks, and move-in fees
• Models for connecting private property owners and managers with those who need affordable
housing (e.g., Housing Connector)

131
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Expanding Housing First Model across Washington
o Principles for Housing First temporary lodging or permanent housing investments:
Non-congregate: We learned during the pandemic that non-congregate lodging
arrangements are in general calmer, more dignified, and more welcoming for
many people with behavioral health conditions, than congregate shelter settings.
Non-congregate bridge housing arrangements can include self-contained
apartments, SRO-style accommodations, hotel-style accommodations, or tiny
homes.
24/7 availability: Accommodations that require people to exit during the day
foster instability, and force individuals into public areas, increasing vulnerability
to physical harm; bridge housing should allow individuals to come and go, leave
their belongings, arrange their own space, and count on having a place to return
to
Low barrier: Subject to screening for current or past behaviors that would
reasonably be viewed as posing a risk to program staff or other participants,
housing or lodging should be offered and maintained regardless of criminal
history, current drug use, or other behavioral health conditions
Intensive Stabilization Support ("meet people where they're at--but don't leave
them there"): Low barrier doesn't mean accepting that people will just remain
stuck in harmful patterns but will live indoors. That will doubtless be true for
some and living inside is still preferable for them and for the surrounding
community in nearly all cases. But, for most, intensive, trauma-informed on-site
support can help to decrease ongoing trauma and vulnerability, create safety,
allow the identification of barriers and trauma-based reactions, foster goal
setting, increase hygiene, and work on barriers to housing, health, and economic
stabilization, including legal system coordination for those who have active court
obligations. Many individuals who, at entry, would have been assumed to need
long term permanent supportive housing (PSH--an essential but costly kind of
housing for people who need on-site support), can live independently with or
without a housing subsidy in scattered-site units in the private housing market or
in public housing. Intensive case management on-site in bridge housing or
temporary lodging can facilitate optimal permanent housing placements as
individuals move on.
We recommend that the work is centered on people who use substances and/or experience mental
health conditions who have lived/living experience with homelessness and/or housing instability, such as:
• Individuals who encountered barriers in the shelter and homeless housing systems due to active
drug use or being in recovery from substance use disorder

132
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Individuals who used shelter and/or homeless housing systems while actively using drugs or
working on their recovery
• Individuals with expertise designing and operating bridge housing or temporary lodging for
people with high barriers including current drug use
• Individuals with expertise bridging systems and designing systems to meet the needs of
historically under-served populations
• Individuals with knowledge of current State investments in homelessness response
• Individuals with knowledge of Trueblood housing investments
• Individuals with knowledge of Continuums of Care/Coordinated Entry in homeless housing
Bill Requirement(s) – This recommendation meets several considerations for the Substance Use Recovery
Services Plan:
Bill requirement: Section 1(3)(a), (b), (e)
Concerns and Considerations
• In keeping with the broad SAMHSA definition of recovery, it's essential to engage and offer
stabilization for individuals who aren't at a point that they can or will abstain from drug use, but
whose harm to self and others can be reduced by providing secure and dignified non-congregate
lodging, either permanent housing or "bridge housing," that permits intensive support teams to
work with individuals to identify, address and shift barriers to recovery. Creating systems of
engagement and care that presume traditional treatment, abstinence and/or sobriety, will, by
definition, leave out huge numbers of those engaged in harmful drug use, diminish the perceived
efficacy of the state's other investments, and will particularly miss most of those at highest
exposure of law enforcement action and criminal legal system involvement. We must make a
path for those who are currently using and not immediately ready to stop, to not be living in
public, to live in comparative safety, and to have a strong support framework to begin to work on
personal objectives, healing, and recovery (broadly defined). This is the logic behind Housing
First.
• Placement in bridge/transitional housing often causes individuals to lose their homelessness
status and therefore, their eligibility for many next step housing options. It will be important to
explore barriers posed by homelessness definitions and possible solutions.
• Living in housing with individuals who are actively using can jeopardize the safety and well-being
of those who are in early recovery. Therefore, it will be important to establish a full continuum of
housing options to meet the needs of people who are in recovery or seeking recovery as well as
those who are actively using. To protect other residents, many recovery homes have adopted a
zero-tolerance approach to drug use. It will be important to explore ways that recovery homes
can balance protecting the safety and recovery of all residents with providing an opportunity for
individuals who have had a recurrence of use to stabilize and remain housed, including availability
of crisis stabilization housing in the community that could provide interim housing for an

133
SUBSTANCE USE AND RECOVERY SERVICES PLAN
individual who is awaiting a bed at a withdrawal management/detox or inpatient facility or a
return to the recovery home
• Expansion of Homeless Outreach services that represent their communities. We need to first
reach the underserved and marginalized communities. Add additional funds to build peers for
Homeless Outreach that represents BIPOC communities.
Collaboration with Existing Resources:
Currently Offered Housing Programs and Government Funding
• List of homeless shelters in Washington State by city/county
• HARPS and Trueblood Forensics HARPS: Housing and Recovery Through Peer Services (HARPS)
provides supportive housing services and short-term housing bridge subsidies to at risk
individuals (people who are exiting, or at risk of entering inpatient behavioral healthcare
settings).
• Through proviso 96 Expansion of Housing First services, HCA/DBHR/RSS is in the process of
identifying 9 regions that will receive a grant.
SURSA committee feedback
No feedback on this recommendation was provided from SURSAC members during the pre-meeting
review period

134
SUBSTANCE USE AND RECOVERY SERVICES PLAN

135
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix S - Resources to inform a recommendation for the state’s criminal-legal response to
possession of controlled substances
Substance Use
Recovery
Services Advisory
Committee
Resources to inform a
recommendation for the state’s
criminal-legal response to
possession of controlled
substances
Updated 06-27-2022

136
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Committee Charge
5476 Section 1
The authority, in collaboration with the substance use recovery services advisory committee established in
subsection (2) of this section, shall establish a substance use recovery services plan. The purpose of the plan is to
implement measures to assist persons with substance use disorder in accessing outreach, treatment, and recovery
support services that are low barrier, person centered, informed by people with lived experience, and culturally and
linguistically appropriate. The plan must articulate the manner in which continual, rapid, and widespread access to a
comprehensive continuum of care will be provided to all persons with substance use disorder.
(3) The plan must consider:
(l) Recommendations regarding the appropriate criminal legal system response, if any, to possession of controlled
substances
Document Development
At the May 2
nd
SURSAC meeting, committee members were asked about what information would be helpful to have
to formulate a recommendation for the appropriate criminal-legal response to possession of controlled substances,
if any. The 5476 support team at HCA gathered several resources to meet those information requests, which were
emailed to the SURSAC on Wednesday, June 1
st
. At the June 6
th
SURSAC meeting, there was a request to invite
additional contributions. On June 6
th
, Michelle sent an email to all SURSAC meeting attendees titled, “SURSAC:
Opportunity to add Criminal-Legal Response resources”, inviting contributions to this document by June 24
th
, so that
the revised document could be shared June 27
th
, providing the SURSAC two full weeks to review before the July 11
th
meeting.
Summary of Hyperlinked Resources
Cannabis Legalization and Racial Disparities in Washington State
Drug Decriminalization in Oregon, One Year Later: Thousands of Lives not Ruined by Possession Arrests,
$300 million+ in Funding for Services
Depenalization, diversion and decriminalization: A realist review and programme theory of alternatives to
criminalization for simple drug possession
Drug decriminalization policy: Literature review: Models, implementation and outcomes
Drug Decriminalization | Drug Policy Alliance
Racial, Gender, and County Disparities for Simple Drug Possession Convictions in Washington State
Washington State Court Directory
Determination of Eligibility (Therapeutic Courts) – RCW 2.30.030
Drug Courts are not the answer: Toward a Health-Centered Approach to Drug Use (Drug Policy Alliance,
March 2021)
America’s problem-solving courts: The criminal costs of treatment and the case for reform (National
Association of Criminal Defense Lawyers, September 2009)

137
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Addicted to courts: How a growing dependence on drug courts impacts people and communities (Justice
Policy Institute, March 2011)
Drug Court Outcomes (2013)
Drug Court Participants: Recidivism and Key Outcome Measures (DSHS)
Chemical Dependency Treatment for Incarcerated individuals: A Review of the Evidence and Benefit-Cost
Findings
RNP: Recovery Navigator Program (Intercepts 0, 1)
The Arrest and Jail Alternatives program
Seattle’s Law Enforcement Assisted Diversion (LEAD) Program: Within-Subjects Changes on Housing,
Employment, and Income / Benefits Outcomes and Associations with Recidivism
Seattle’s law enforcement assisted diversion (LEAD) program effects on criminal justice and legal system
utilization and costs
Seattle’s Law Enforcement Assisted Diversion (LEAD): Program effects on recidivism outcomes
LEAD Program Evaluation: Describing LEAD case management in participants’ own words (Harm
Reduction Research and Treatment Center, UW, November 2016)
DOC Institutional Costs, Average Daily Population, and Cost Per Incarcerated Individual per Day (FY2019)
Hidden Consequences: The Impact of Incarceration on Dependent Children | National Institute of Justice
Cost-Benefit Analysis of public policies and programs
Peer Reviewed Research About Syringe Service Programs | Washington State Department of Health
County Profiles of Social Determinants of Health
Study after study shows ex-prisoners would be better off without intense supervision (Brookings, July
2018)
JustCARE: The development and impact of a multi-faceted collective impact model (University of
Washington, June 2021)
Summary of Attachments
A Quiet Revolution: Drug Decriminalization Across the Globe (March 2016)
Effects of Criminalization Key Points 2021 Update
National Association of Drug Court Professionals (NADCP) Equity and Inclusion Research Brief:
Exclusionary Criteria and Their Impacts on the Likelihood to Reoffend, Racial Bias, and Outcomes in
Treatment Court
Racial Distribution of Drug Court Participants (CJTA Panel July 31 2020_Racial Distribution)
Drug Offender Sentencing Alternatives (DOSA)

138
SUBSTANCE USE AND RECOVERY SERVICES PLAN
DOC Substance Abuse Recovery Unit (SARU)
Behavioral Health Agencies Directory
Behavioral Health Treatment Availability in Rural Counties
NOTE: Hyperlinks are provided as often as possible for easy access to the resources included in this document.
Resources that could not be hyperlinked are included as email attachments, noted with “ATTACHMENT”
Drug Criminalization and Racial Disparities
Since Oregon is the first state in the nation to decriminalize (small amount) possession of controlled substances, and
the law has only been in effect for one year, it will take time to understand the full racial impact of this policy in OR,
and the potential impact for our own state if this policy were to be adopted in Washington State long-term.
However, we can look at the racial impact of decriminalization – and the legalization of supply – related to cannabis
to help us understand potential impacts.
Cannabis Legalization and Racial Disparities in Washington State
This report from ADAI (March 2019) examines publicly available data on cannabis use and racial disparities in WA in
three areas of interest: criminal justice, youth consumption, and treatment for substance use disorders. The article
notes:
“Before legalization, African American/Blacks were 2.8 times more likely to be arrested for marijuana possession
than Whites, in Washington State (3.8 times nationwide). Most of these arrests (88%) were for cannabis-possession-
only, yet adult marijuana use was similar across racial and ethnic groups.
After legalization, analysis from the Washington State University Crime, Cannabis and Police Research Group
indicated that disparities between African American/Black and white adults varied by the type of crime committed.
The relative disparity in arrests for selling marijuana has more than doubled since legalization while there was a
small decrease in possession-related disparities.
The disparity in court filings for marijuana possession among African American/Black adults has remained
unchanged after legalization. African American/Black adults are nearly three times more likely to be prosecuted for
a low-level marijuana possession offense than white adults after legalization”
Drug Decriminalization in Oregon, One Year Later: Thousands of Lives not Ruined by Possession Arrests,
$300 million+ in Funding for Services
This article from DrugPolicy.org, “Drug Decriminalization in Oregon, One Year Later” notes a prediction from the
Oregon Criminal Justice Commission that Measure 110’s passage would result in a 95% reduction in racial disparities
in drug arrests.”
ATTACHMENT: A Quiet Revolution: Drug Decriminalization Across the Globe (March 2016)
Depenalization, diversion and decriminalization: A realist review and programme theory of alternatives to
criminalization for simple drug possession
Drug decriminalization policy : Literature review: Models, implementation and outcomes
Drug Decriminalization | Drug Policy Alliance
ATTACHMENT – Effects of Criminalization Key Points 2021 Update

139
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This document provides support information for HB 1499, offered by the Office of Infectious Disease (OID within
DCHS) at the Washington State Dept of Health, which notes citations for the following findings:
• Criminalization negatively impacts racial justice and health equity
• Criminalization negatively impacts women and families
• Criminalization negatively impacts efforts to prevent and treat infectious disease among people who use
drugs
• Criminalization contributes to overdose morbidity and mortality
• Criminalization is expensive and burdens the state budget
• Criminalization of paraphernalia for personal use impacts public health and safety efforts
Conviction Rates for Possession of Controlled Substances
Racial, Gender, and County Disparities for Simple Drug Possession Convictions in Washington State
Therapeutic Courts
Washington State Court Directory
Here you can find a list of all the therapeutic courts in Washington, which are generally available at Intercept 3
(Specialty Courts), including:
• Drug Courts
• Juvenile Courts
• Family Treatment
• Mental Health Court
Determination of Eligibility (Therapeutic Courts) – RCW 2.30.030
This statute lays out some statewide therapeutic court eligibility limitations. However, before those limits are
reached, there are a lot of differences between counties in terms of what charges they take and what additional
exclusionary criteria they apply. For example, some counties will not take drug delivery charges. And, nationwide,
according to the National Association of Drug Court Professionals (NADCP), although White individuals are more
likely to be involved in trafficking, Black individuals are more likely to be arrested for drug trafficking, so there cold
certainly be racial disparities that result from various eligibility decisions.
To understand why cases do not qualify, we’d need data from every county prosecutor, and it would involve digging
into every case, which is an undertaking that we do not have capacity for. One other thing to note is that one of the
main reasons people don’t get offered drug court is that their defense attorneys don’t request it – either because
they don’t know about it, don’t believe in it, don’t think it is the best possible deal, or don’t think the case will be
approve for entry by the prosecutor. In some cases, drug court may be disincentivized because attorneys may get
better deals if their client will just plea mainstream. Defense guidance is a major reason why any individual would or
would not end up in drug court, which makes it much harder to quantify than a situation where a prosecutor is
actually denying a case entry.
The Administrative Office of the Courts (AOC) Behavioral Health Court Program is working on an assessment that
will take a deeper dive into Treatment Court eligibility criteria, but the results of those reports and any court-specific
data won’t likely be available until mid-late 2023. Tessa Clemments (the AOC BH Court Program Lead) suggests
looking at each court’s policy and procedure manual to find their stated eligibility criteria.

140
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Drug Courts are not the answer: Toward a Health-Centered Approach to Drug Use (Drug Policy Alliance,
March 2021)
America’s problem-solving courts: The criminal costs of treatment and the case for reform (National
Association of Criminal Defense Lawyers, September 2009)
Addicted to courts: How a growing dependence on drug courts impacts people and communities (Justice
Policy Institute, March 2011)
• The King County Drug Diversion Court Procedure and Policy Manual (Eligibility begins on page 5)
• National Association of Drug Court Professionals (NADCP) Equity and Inclusion Research Brief:
Exclusionary Criteria and Their Impacts on the Likelihood to Reoffend, Racial Bias, and Outcomes
in Treatment Court
• Racial Distribution of Drug Court Participants (CJTA Panel July 31 2020_Racial Distribution)
Drug Court Outcomes (2013)
Describes the criminal and CD treatment participation outcomes of 1,671 adults charged with felonies who were
eligible for treatment, primarily funded through CJTA, and who were admitted to formally established drug courts.
Three-year outcomes are compared to a statistically matched comparison group of 1,671 adults charged with similar
felonies in the same jurisdictions and two-year time period (July 2007 through June 2009), but who were not
admitted to a drug court. Arrests, incarceration rates, and treatment participation over a three-year follow-up
period are examined, as are net benefits associated with reductions in crime.
• Drug Court Participants were less likely to be incarcerated during the follow-up period than individuals in
the comparison group (17 versus 23 percent)
• Controlling for other factors leading to arrest, drug court participants were twice as likely to remain free of
arrest as those in the comparison group (30 vs. 15 percent)
• Nearly universal participation in chemical dependency treatment was obtained by drug court participants
(97 percent compared to 46 percent in the comparison group)
• Drug court participants were over 3 times more likely to enter treatment within 90 days and 4 times more
likely to be in treatment – primarily outpatient – for 90 or more days
• Reductions in crime observed in this analysis translate into a net benefit to taxpayers and society of
approximately $22,000 per participant, or $4.02 in benefits per dollar spent
Drug Court Participants: Recidivism and Key Outcome Measures (DSHS)
These reports do not include reasons for arrest (they are not specific to arrests related to possession of controlled
substance), but they do include demographics, SUD treatment participation, recidivism, employment, and Medicaid
enrollment among Drug Court enrollees. These reports present recidivism measures and other key outcomes and
characteristics of offenders participating in adult drug courts across Washington State. The reports contain yearly
trends for individual courts and for courts statewide. The reports were written in collaboration with the Criminal
Justice Treatment Account Panel and the HCA Division of Behavioral Health and Recovery, and will be updated
annually. To protect client confidentiality, reports for courts with a small number of participants are not included.
• King
• Kitsap
• Pierce

141
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Snohomish
• Spokane
• Thurston
Drug Offender Sentencing Alternatives Outcomes
ATTACHMENT - Drug Offender Sentencing Alternatives (DOSA)
The Fact sheet including demographic and county data for the DOSA program (attached), designed to provide SUD
treatment and community supervision for individuals diagnosed with an SUD who have committed a drug or other
statutory eligible crime. Individuals sentenced to a DOSA are required to participate in SUD treatment in lieu of
prison time, or a reduced prison sentence.
SUD Treatment Programs and Outcomes for Incarcerated Individuals
ATTACHMENT - DOC Substance Abuse Recovery Unit (SARU)
The DOC Substance Abuse Recovery Unit is one of the largest certified treatment agencies in the State of
Washington, with services located in 11 of 12 state prison facilities (as of July 2021) and nine work release locations.
The Washington State Institute for Public Policy found that incarcerated individuals who participate in Substance
Use treatment programs have lower recidivism rates than those who did not participate by 4 to 9 percent.
The SARU statistics document (attached) outlines the SUD treatment recovery programs available to incarcerated
individuals and provides some data by gender but not by race.
Chemical Dependency Treatment for Incarcerated individuals: A Review of the Evidence and Benefit-Cost
Findings
In this The Washington State Institute for Public Policy found that for each dollar spent on drug treatment in
confinement and partial confinement there is a taxpayer benefit ranging between $5.05 to $13.91 (depending on
level of care and sentencing type).
Diversion Programs for Youth and Adults
RNP: Recovery Navigator Program (Intercepts 0, 1)
The intent of the RNP is to provide behavioral health services to individuals who intersect with police because of
simple drug possession, people who have frequent criminal-legal system contact, and others who are referred from
community sources. These programs are to serve people who are at risk of arrest, or already have been involved in
the criminal legal system due to unmet behavioral health needs.
• Fact Sheet
• Uniform Program Standards
• RCW 71.24.115
AJA: Arrest and Jail Alternatives Grant Program

142
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The Arrest and Jail Alternatives program was established per HB 1767, RCW 36.28A.450, and created a partnership
between WASPC and the LEAD National Support Bureau, to develop and implement a grant program aimed at
supporting local initiatives to properly identify criminal justice system-involved persons with substance use disorders
and other behavioral health needs and engage those persons with therapeutic interventions and other
services. Grants for this work have been provided to the following 3 organizations:
• Catholic Community Services (Olympia)
• Olympic Peninsula Community Clinic (Port Angeles)
• Comprehensive Healthcare (Walla Walla)
Click here for the AJA 2021 Annual Report.
LEAD in Seattle/King County
Seattle’s Law Enforcement Assisted Diversion (LEAD) program is the first known pre-booking diversion program for
people arrested on narcotics and prostitution charges in the United States. Launched in October 2011, LEAD is the
product of a multi-year collaboration involving a wide range of organizations, including The Defender Association’s
Racial Disparity Project, the Seattle Police Department, the ACLU of Washington, the King County Prosecuting
Attorney’s Office, the Seattle City Attorney’s office, the King County Sheriff’s Office, Evergreen Treatment Services,
the King County Executive, the Washington State Department of Corrections, and others.
Seattle’s Law Enforcement Assisted Diversion (LEAD) Program: Within-Subjects Changes on Housing,
Employment, and Income / Benefits Outcomes and Associations with Recidivism
Seattle’s law enforcement assisted diversion (LEAD) program effects on criminal justice and legal system
utilization and costs
Seattle’s Law Enforcement Assisted Diversion (LEAD): Program effects on recidivism outcomes
LEAD Program Evaluation: Describing LEAD case management in participants’ own words (Harm
Reduction Research and Treatment Center, UW, November 2016)
HCA LEAD Expansion Pilot Program
Per SSB5380 Sec. 29, the Health Care Authority partnered with the Public Defender’s Association and LEAD
National Support Bureau to expand availability of LEAD programs statewide / outside King County. In 2020, HCA
contracted with four different sites ($4.1 million total) to provide and implement LEAD programs in the following
counties, which receive technical assistance from PDA’s National Support Bureau:
• Whatcom
• Snohomish
• Mason
• Thurston
Cost and Benefits of Incarceration vs. Community-Based Harm Reduction and Treatment Programs
Fiscal Cost of Incarceration
DOC Institutional Costs, Average Daily Population, and Cost Per Incarcerated Individual per Day (FY2019)

143
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Does not include MOUD, SUD-treatment specific, or other healthcare specific expenses, but provides a snapshot of
total cost to incarcerate someone
Social Cost: Impact on Children of Incarcerated Parents
Hidden Consequences: The Impact of Incarceration on Dependent Children | National Institute of Justice
Discusses “cost” of incarceration in terms of the impact on the children of incarcerated parents, which
disproportionately impacts communities of color.
“One consequence of this dramatic increase is that more mothers and fathers with dependent children are in
prison. Since the war on drugs began in the 1980s, for example, the rate of children with incarcerated mothers has
increased 100 percent, and the rate of those with incarcerated fathers has increased more than 75 percent.”
“Data from 2007 (the most recent data available) show that African-American children and Hispanic children were
7.5 times more likely and 2.3 times more likely, respectively, than white children to have an incarcerated parent.”
Cost-Benefit Analysis of public policies and programs
This report from RDA includes several diversion and community-based treatment programs:
• Drug Offender Sentencing Alternative (for persons convicted of drug offenses)
• Case management (“swift, certain, and fair”) for drug-involved persons
• Mental health courts
• Drug Courts
• Inpatient or intensive outpatient drug treatment during incarceration
• Therapeutic communities (in the community) for individuals with co-occurring disorders
• Drug Offender Sentencing Alternatives (for persons convicted of property offenses)
• Outpatient or non-intensive drug treatment during incarceration
• Outpatient or non-intensive drug treatment in the community
• Housing assistance without services
• Housing assistance with services
• Police diversion for low-severity offenses (pre-arrest)
• Police diversion for individuals with mental illness (pre-arrest)
Peer Reviewed Research About Syringe Service Programs | Washington State Department of
Health
“These analyses indicate that it would be highly cost-saving to invest additional funds to expand syringe exchange
services in the US.”
Community Behavioral Health Services
Social Determinants of Health by County

144
SUBSTANCE USE AND RECOVERY SERVICES PLAN
This report includes data by county including:
• Drug Trafficking Zone
• Drugs deaths per 100,000
• Opioid hospitalizations per 100,000
• Opioid deaths per 100,000
• Mental health providers per 100,000
• Specialist providers (e.g., gastroenterology, hepatology, infectious disease, addiction medicine) per
100,000
• HIV cases per 100,000
• HCV cases per 100,000
ATTACHMENT - Behavioral Health Agencies Directory
Attached is the DOH’s Behavioral Health Agency Directory, which includes information about the number of
behavioral health agencies in each county, and what services they provide (Mental Health, SUD, or both). The
patient capacities of the agencies are not listed.
ATTACHMENT - Behavioral Health Treatment Availability in Rural Counties
Also attached is an excel spreadsheet that summarizes the BH agencies in Washington’s rural counties, alongside
recent population and population growth rate data, to provide a starting point for identifying areas that are under-
resourced with behavioral health services provided through these agencies.
Additional Resource Contributions
Study after study shows ex-prisoners would be better off without intense supervision (Brookings, July
2018)
JustCARE: The development and impact of a multi-faceted collective impact model (University of
Washington, June 2021)

145
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix T – RDA evaluation recommendation
Evaluation Recommendations for the Blake-bill Interventions
JUNE 30, 2022
Background
The Healthcare Authority (HCA) Division of Behavioral Health and Recovery (DBHR) requested an
evaluation plan for selected programs targeting the population of individuals who are the focus of Blake
Bill (SB 5476). Blake-bill Interventions are programs intended to provide treatment and support services
to individuals who may have otherwise been subject to criminal prosecution, pre-Blake. The following
programs are the focus of the evaluation recommendations provided by the Department of Social and
Health Services (DSHS) Research and Data Analysis Division (RDA):
• Recovery Navigator Program (RNP): A statewide (~50-site) effort in partnership with Behavioral
Health Administrative Organizations (BH-ASOs), the RNP provides community-based outreach,
intake, assessment, and connection to services for youth and adults with substance use and co-
occurring—SUD and mental health—disorders.
• Medication for Opioid Use Disorder (MOUD) in Jails: In nineteen participating facilities, incarcerated
individuals will be assessed for an opioid use disorder (OUD) and offered medication for OUD where
indicated. MOUD will be provided throughout the period of incarceration and individuals will be
connected to continuing treatment after release or transfer to another facility.
• Peer-Run and Clubhouse Services Expansion: This is an expansion (of 10 sites) of Clubhouse
International and Peer Run organizations, including organizations incorporating evidence-based
models such as Clubhouse International, Recovery Community Organizations, and Recovery Cafes.
• Homeless Outreach Stabilization Transition (HOST) Expansion: This is an expansion of the existing
HOST programs (of 5 sites). HOST is an outreach-based multidisciplinary approach intended to
provide medical, behavioral, peer, and case management services to high-acuity individuals with
substance use and co-occurring disorders who do not access existing services.

146
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Substance Use Disorder Family Navigators: This program (3 sites) supports parents, partners, and
other adult family members of youth and young adults experiencing SUD-related challenges in
navigating systems of care. Services to adult family members are provided by trained and certified
family-support peers and include one-to-one peer coaching, socialization, peer group support,
education groups, employment support, supportive housing, and referrals.
While each of these programs focuses on different services, settings, and individuals, and has different
immediate aims (such as the provision of MOUD in jails or peer support services), the expectation is that
they all will achieve, to differing degrees, the following common outcomes:
• Reduce criminal justice involvement,
• Reduce the use of emergency medical services and hospitalizations,
• Increase the use of behavioral mental health and SUD treatment, and
• Improve indicators of well-being such as access to primary care, employment, and housing.
The RDA-recommended evaluation strategy will focus on efficiently estimating the impact of each Blake
Intervention on the above outcomes to inform decision makers about their overall and relative
effectiveness. RDA is recommending a general analysis of outcomes broadly applicable to all Blake
Interventions; program-specific strategies/outcomes may be further developed with input from the
evaluator, RDA, program staff, and other individuals designated by HCA. These recommendations do not
address routine performance monitoring or other important elements of program evaluation such as
fidelity measurement or qualitative descriptions of the interventions. If such activities are not subsumed
by HCA program managers or those implementing the programs, HCA may consider contracting with an
entity specializing in these tasks.
Recommended Evaluation Design and Research Questions
Quasi-Experimental Design.
To efficiently estimate the effectiveness of the Blake Interventions, we
recommend a strategy that employs similar methods across the programs and focuses on a common set
of relevant outcomes. For a variety of reasons, random controlled trials—the research “gold-standard”
for determining effectiveness—are not an option for evaluating the Blake Interventions. Instead, RDA
recommends a quasi-experimental, longitudinal design, an evaluation approach frequently employed by
RDA which leverages the extensive, person-level, longitudinal data available in the RDA-curated

147
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Integrated Client Databases (ICDB).
40
The ICDB contains more than two decades of service risks, history,
costs, and outcomes. The data systems span multiple state agencies, including DSHS, HCA, Department of
Corrections (DOC), Employment Security Department (ESD), Department of Commerce, the Washington
State Association of Sheriffs and Police Chiefs (WASPC), and the Washington State Patrol (WSP).
41
The
quasi-experimental approach will allow for the consistent and reliable estimation of program impacts
without imposing burdensome data collection requirements on providers and clients.
Study Populations.
The quasi-experimental evaluation will compare the outcomes of service recipients
“enrolled” in each intervention (treatment group) with the experiences of statistically similar individuals
who were not enrolled in the intervention (comparison group) and then draw inferences about the
effectiveness of a specific intervention. The treatment groups will include anyone enrolled in a particular
Blake Intervention.
42
The definition of “enrollment” will vary depending on the intervention. In general,
clients will be considered enrolled when they receive measurable service provided by a given intervention
(e.g. for the MOUD in Jails program, this may be the day a client was inducted on to MOUD; for RNP, this
may be the day they were assigned a navigator). Membership in the treatment group will be based on
intent-to-treat
rather than whether or not an individual “completed” a program.
43
The comparison groups will include statistically matched samples from the relevant populations of
individuals who qualify for each intervention, but were not enrolled during the study period.
44
In addition
to selecting on qualifying criteria for each type of intervention program, members of the comparison
groups will be identified using one or more of a variety of propensity score matching approaches to
ensure equivalency in relevant characteristics between the treatment and comparison groups. Table 1
lists the possible matching criteria to be used to identify comparison groups.
45
TABLE 1
Proposed Matching Criteria
40
Cite example reports.
41
For more information about the ICDB, see https://www.dshs.wa.gov/ffa/rda/research-reports/dshs-integrated-client-
databases.
42
In the case of the SUD Family Navigator program, the service recipient may be a parent, but the enrolled individual
will be the youth with or at-risk of an SUD.
43
An intent-to-treat analysis ignores non-compliance to an assigned protocol and does not require collection of
additional information on days of treatment or “graduation.” Fisher LD, Dixon DO, Herson J, Frankowski RK, Hearron MS,
Peace KE. Intention to treat in clinical trials. In: Peace KE, editor. Statistical issues in drug research and development. New
York: Marcel Dekker; 1990. pp. 331–50.
44
Criteria for selecting the relevant qualified populations will be determined in collaboration with program managers
and providers and in consideration of the data available in the ICDB.
45
Rosenbaum, P. R. and D. B. Rubin. 1983. The central role of the propensity score in observational studies for causal
effects. Biometrika 70(1): 41–55.

148
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Characteristics
Variables
Demographics
Age, race, ethnicity, gender
Household Characteristics
Number of adults, minors, children under 12
Geography
County of residence, urbanicity
Criminal History
Prior arrests, charges, and convictions (by type), periods of
incarceration (DOC), days in jail
Behavioral Health
Mental health and SUD diagnoses
Behavioral Health Service History
Outpatient mental health treatment, inpatient mental health
treatment, withdrawal management, outpatient SUD treatment,
inpatient SUD treatment, medication-assisted treatment
Health (general)
Medical risk score, chronic disease diagnoses, access to primary
care
Emergency Department (ED)
Usage and Hospitalizations
ED outpatient visits, non-ED outpatient visits, inpatient admissions
Housing Status
Homeless or unstably housed, housing services
Social Services and Other
Assistance
Child welfare, SSI/SSDI, SNAP, TANF, HEN
Employment History
Quarters employed, earnings
Analysis.
With the exception of caveats noted below in Limitations and Considerations, the observed
differences in outcomes between matched treatment and control groups will be attributed to the
relevant intervention. A schematic of the research design is presented in Figure 1.
In addition to its use in the construction of treatment and comparison groups, the longitudinal ICDB data
will support the necessary pre-tests of equivalence between the treatment and comparison groups
regarding the outcomes to be measured. A longitudinal design will also support multiple measures of
program outcomes, which will be the basis of the primary research questions. For each specific outcome,
the proposed design will characterize outcomes in the following ways:
•
Within-Group:
a pre-post analysis of the treatment group that examines participant outcomes
before and after the intervention (e.g. for individuals in a treatment group, what are the differences
in arrest rates in the year before the intervention compared to the year after);
•
Between-Group:
post-period comparisons of treatment and comparison group outcomes in the
follow-up period (e.g. during the year after the intervention, what are the differences in arrest rates
between treatment and comparison groups); and

149
SUBSTANCE USE AND RECOVERY SERVICES PLAN
•
Difference-in-Difference:
this approach compares of the rates of change in outcomes, pre-post,
experienced by the treatment and comparison groups (e.g. in the years before and after the
intervention, what are the differences in the rates of change in arrests between the treatment and
control groups).
FIGURE 1
Research Design
Outcome Measures.
The bases for specific outcomes to be examined in the proposed analyses—all which
are available in the ICDB—are described in Table 2.
TABLE 2
Blake Intervention Outcome Measures
Objective
Basis of Outcome Measure
ICDB Source
Reduce Criminal Justice
Involvement
Arrests
WSP
Days in Jail or DOC Facilities
HCA, WASPC, and DOC
Reduce Utilization of Emergency
Physical and Behavioral Health
Services
ED Visits
HCA
Hospitalizations (Physical)
HCA
Community and State
Psychiatric Hospitalizations
DSHS
Withdrawal Management
HCA
Crisis Services
HCA
Increase use of Behavioral
Health Services
SUD Outpatient Treatment
HCA
SUD Inpatient Treatment
HCA
Medication for SUD
HCA
Outpatient Mental Health
Treatment Services/Medication
HCA
Employment and Earnings
ESD
Treatment Groups
Comparison Groups
Outcome Measures
at Baseline
Outcome Measures
at Baseline
Post-period Outcome
Measures
Post-period Outcome
Measures
Blake
Intervention
Within group differences in outcomes
Between group
differences in
outcomes
Pre-Intervention
(Baseline) Measures
• Demographics
• Criminal History and incarcerations
• Substance use disorders
• Mental health diagnoses
• Chronic Medical Conditions
• Employment
• Housing status
• Etc…
Post-Intervention Outcomes
• Re-arrests and jail days
• ED utilization and hospitalizations
• Behavioral health treatment
• Access to primary care
• Housing services
• Employment

150
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Improve Indicators of Well-
being
Housing Services Utilization
Commerce
Utilization of Primary Care
HCA
Connection to Social Services
(TANF, SNAP, HEN, DVR, etc.)
DSHS
The specific construction of each outcome measure (e.g. number of arrests per year, arrest rates, felony
arrests, months of SUD treatment, etc.) will be determined in collaboration with the evaluator, RDA,
program staff, and other individuals designated by HCA. Baseline descriptions of program participants and
propensity score matching will be possible as soon as a sufficient number of clients are enrolled in any
given program.
46
Post-period Definition.
The rigorous outcomes evaluation activities described here will require sufficient
time post-enrollment for relevant outcomes to occur, to be reported to administrative data systems, and
then updated in the ICDB. Typically analyses of this type employ 12- to 18-month pre- and post- periods
to characterize outcomes (e.g. the number of arrests in the 12 months before an intervention and the
number of arrests in the 12 months after the intervention). The time periods to be used in these analyses
will depend on reporting deadlines (nearer-term deadlines will mean that the evaluation will be based on
shorter post periods); implementation schedules (earlier implementation will allow for longer post
periods); and lags in the availability of data for specific outcome measures (e.g. there is a 6-month lag in
employment outcomes; conviction outcomes are omitted form this proposal because of the time
required for adjudication). Relevant time periods will be determined by the evaluator in concert with the
specific definitions of outcome measures described above. It is possible that there will be different time
periods used for each intervention and measure.
Index Month.
A critical concept in developing the evaluation analytics is the index month. The index
month in this context is the month in which we consider an individual to be under the influence of a
particular intervention. This may be the month they are first inducted onto MOUD in a jail or the month
they were assigned a recovery navigator. In collaboration with program staff, the evaluator will determine
the relevant definition of the index month for each Blake Intervention. Once established, all
measurement concepts associated for a given analysis will be based on events or characteristics
manifesting in the relevant months before and after the index month. RDA recommends using an index
month (rather than a specific index date or index year) because most data in the ICDB are organized by
46
The “sufficient” number of participants will depend on the expected effect size of any given intervention.
Interventions expecting large effect sizes require small samples.

151
SUBSTANCE USE AND RECOVERY SERVICES PLAN
monthly intervals. If the evaluator determines that more refined definitions are required, there will be
additional costs associated with having RDA organize the data accordingly.
Data Collection
As previously noted, the recommended evaluation approach will rely almost exclusively on existing data
curated by RDA in the ICDB. In collaboration with the evaluator, RDA will create person-level analytic
datasets with all the necessary (and available) variables. To support the proposed evaluation, it will be
necessary for the service providers to collect and maintain the following information on each client
served:
• First name
• Last name
• Middle initial
• Date of birth
• SSN if available
• A ProviderOne ID is acceptable in place the above identifiers
• Enrollment Date (there may be multiple enrollments in some cases)
HCA program managers should work closely with service providers and RDA to ensure this information is
routinely and systematically collected and maintained in a medium that supports the efficient
transmission of data to HCA or RDA by secure means. Data collection by the individual Blake Interventions
varies by program. Some programs collect information on disparate spread sheets; others, such as the
RNP, utilize sophisticated case management software. Future opportunities for informative sub-group
analyses on the relative effectiveness of different intervention service components may be possible for
programs that collect sufficient additional information on their clients.
Limitations and Other Considerations
Medicaid Enrollees.
The recommended evaluation approach relies exclusively on data compiled by RDA in
the ICDB. The most complete data in the ICDB are for individuals who are enrolled in Medicaid, therefore
most analyses will be restricted to Medicaid clients. We expect the majority of clients participating in the
Blake Interventions will be Medicaid-enrolled.
Institutional Review Board.
Whomever is tasked with performing an evaluation of the Blake Interventions
will be responsible for submitting a research application or exempt determination to the Washington
State Institutional Review Board and coordinate with RDA on the necessary data request.

152
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Client Identifiers.
HCA program managers should prioritize the collection of the client-level data describe
above and ensure that providers are able to collect and share the relevant data in a timely and efficient
fashion. This may require contract amendments that require this data collection and that include
language allowing data sharing of client identifiers with RDA. Interventions that are unable to provide this
information will need to be evaluated by alternative means beyond the scope of this proposal.
Sample Size.
The recommended evaluation approach may not be feasible for interventions that enroll too
few clients linked with the ICDB to generate meaningful results. In such cases, it may only be possible to
provide baseline characteristics of clients served and descriptive pre-post outcomes (without a
comparison group), which are of limited value.
Unobservable Characteristics.
Propensity score matching reduces biases associated with observed
characteristics and experiences between the treatment and comparison groups. It does not, however,
cannot control for unobserved characteristics such as an individual’s motivation to participate in
behavioral health treatment. As such, it is not possible to guarantee unbiased results in the prosed
outcomes analyses.
Applicability.
This recommended evaluation approach is purposely general and applicable to all of the
Blake Interventions. For some programs, however, the client-level analyses described above may not
provide actionable intelligence. For instance, programs that simply expand existing services—e.g. HOST—
may not benefit from an evaluation of outcomes for clients served only by the expansion. In such cases, it
might be more informative to report on the status of the expansion efforts, the number and type of
clients served, and the fidelity to which the expansion holds to the established model.

153
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Appendix U – Current state programs
Current State-Administered Substance Use
Recovery Support Services
Contents
STATE PLANS .......................................................................................................................................................... 156
SOORP: State Opioid and Overdose Response Plan .................................................................................... 156
Roadmap to Recovery Planning Grant ........................................................................................................... 156
Housing Action Plan .......................................................................................................................................... 156
SUBSTANCE USE PREVENTION & YOUTH ENGAGEMENT .............................................................................. 156
Washington Healthy Youth (WHY) Coalition ................................................................................................ 156
School-based Prevention and Intervention Services ................................................................................... 157
Suicide Prevention and Mental Health Promotion ...................................................................................... 157
State [SUD] Prevention Consortium and Plan .............................................................................................. 157
WA SPF Rx: WA Strategic Prevention Framework for Prescription Drugs ............................................... 158
CPWI: Community Prevention and Wellness Initiative................................................................................ 158
Emergency Response Suicide Prevention Grant ........................................................................................... 159
Prescription Drug/Opioid Prevention ............................................................................................................ 159
Prevention Workforce Development .............................................................................................................. 159
OUTREACH, CRISIS RESPONSE, & SERVICE ENGAGEMENT ............................................................................ 160
Washington Recovery Helpline: 1-866-789-1511........................................................................................... 160
988 Behavioral Health Crisis Line & Mobile Crisis Services ........................................................................ 160
IMC Engagement & Outreach behavioral health coverage ........................................................................ 161
PATH: Projects for Assistance in Transition from Homelessness .............................................................. 161
Peer Pathfinder – Homeless Outreach (opioid use target) ......................................................................... 161
HOST: Homeless Outreach Stabilization Transition (HOST) expansion ................................................... 162
Peer Pathfinder ................................................................................................................................................... 161
SSP: Syringe Service Programs (DOH) ............................................................................................................ 163
Overdose Education and Naloxone Distribution (DOH) ............................................................................. 163
5195: Distributing Opioid Overdose Reversal Medications ........................................................................ 164
RNP: Recovery Navigator Program................................................................................................................. 164
LEAD: Law Enforcement Assisted Diversion .................................................................................................. 165

154
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Mental Health Field Response Teams/Co-Responders ............................................................................... 165
Alternative Response Teams ............................................................................................................................ 165
AJA: Arrest and Jail Alternative Program....................................................................................................... 166
COMMUNITY ASSESSMENT & TREATMENT ...................................................................................................... 166
Fee-for-Service Program for American Indian/Alaska Natives .................................................................. 166
Mental Health Assessments for Young Children .......................................................................................... 166
Youth Substance Use Disorder Treatment Services ..................................................................................... 167
Children’s Long-Term Inpatient Program ...................................................................................................... 167
WISe: Wraparound with Intensive Services ................................................................................................... 168
Healthy Transitions Project .............................................................................................................................. 168
Family Initiated Treatment ............................................................................................................................... 168
Fetal Alcohol Syndrome Diagnostic and Prevention Network (FAS DPN) ............................................... 168
Substance Use Disorder Outpatient Treatment and Residential Services ............................................... 169
BH-ASO: Behavioral Health Administrative Service Organizations .......................................................... 169
Behavioral Health Agencies (BHA) .................................................................................................................. 169
Medicaid State Plan ........................................................................................................................................... 169
Adult Withdrawal Management Services ...................................................................................................... 170
SWMS: Secure Withdrawal Management and Stabilization ....................................................................... 170
Evaluation & Treatment (E&T) Facilities ......................................................................................................... 170
Involuntary Treatment / ITA ............................................................................................................................ 170
Long Term Civil Commitment Bed Capacity (90 or 180 days) .................................................................... 171
Trueblood Programs ......................................................................................................................................... 171
Intensive Outpatient and Partial Hospitalization Pilot Program ............................................................... 171
Intensive Residential Teams – Discharge Wraparound Services ............................................................... 171
PACT: Program of Assertive Community Treatment ................................................................................... 172
BHITF: Behavioral Health Intensive Treatment Facilities ............................................................................ 173
Integrated Managed Care (Apple Health/Medicaid) behavioral health coverage ................................. 174
RSAT: Residential Substance Abuse Treatment (RSAT) ............................................................................. 174
OTN: Opioid Treatment Networks .................................................................................................................. 174
Opioid Treatment Programs (OTP) ................................................................................................................. 175
Hub and Spoke Projects for MOUD ................................................................................................................ 175
MOUD Nurse Care Manager Project .............................................................................................................. 176
Grant Support for Certified Community Behavioral Health Clinic Expansion (CCBHC) ........................ 177
Contingency Management (CM) Project ....................................................................................................... 178

155
SUBSTANCE USE AND RECOVERY SERVICES PLAN
BEHAVIORAL HEALTH SERVICES FOR INDIVIDUALS IN THE CRIMINAL LEGAL SYSTEM .......................... 179
Criminal Justice Treatment Account ............................................................................................................... 179
MOUD (Medication for Opioid Use Disorder) in Jails ................................................................................. 179
Same Day MOUD Visits for people transitioning out of jails ..................................................................... 181
RCSP: Reentry Community Services Program ............................................................................................... 181
HOUSING PROGRAMS........................................................................................................................................... 181
Housing Action Plan .......................................................................................................................................... 181
Housing and Recovery through Peer Services (HARPS) ............................................................................. 182
Recovery Residence Program .......................................................................................................................... 182
Trueblood Forensics HARPS: Housing and Recovery through Peer Services .......................................... 182
Foundational Community Supports (FCS): Supported Housing ................................................................ 182
PATH: Projects for Assistance in Transition from Homelessness .............................................................. 183
MORE RECOVERY SUPPORT SERVICES ............................................................................................................... 183
Foundational Community Supports (FCS): Supported Employment ........................................................ 183
Peer Bridger Program ....................................................................................................................................... 184
Mental Health Peer Respite Centers ............................................................................................................... 184
Clubhouse Services ............................................................................................................................................ 185
Substance Use Peer Support Services ............................................................................................................ 185
PPW: Pregnant and Parenting Women Services .......................................................................................... 185
PCAP: Parent-Child Assistance Program ........................................................................................................ 185
Parent Trust: Parenting Education for Families in Recovery ...................................................................... 187
DATA COLLECTION & COORDINATION ............................................................................................................. 188
Washington State Young Adult Health Survey ............................................................................................. 188
BHDS: Behavioral Health Data System ........................................................................................................... 188
PMP: Prescription Monitoring Program - DOH ............................................................................................ 188
Data for SOORP: State Opioid & Overdose Response Plan ........................................................................ 188
ARM: Analytics and Research Measurement Dashboard Suite .................................................................. 188
Recovery Asset Mapping Tool ......................................................................................................................... 189
HCA Data Strategy and Supporting Five Year Plan ..................................................................................... 189
BEHAVIORAL HEALTH WORKFORCE EXPANSION ............................................................................................ 189
Behavioral Health Marketing Campaign ........................................................................................................ 189
Behavioral Health Workforce Pilot Programs (ESSHB 1504) ...................................................................... 189
Proviso 40: Criminal Background Check ........................................................................................................ 189
Proviso 74: Teaching Clinic Enhancement Rates .......................................................................................... 190

156
SUBSTANCE USE AND RECOVERY SERVICES PLAN
COMMUNITY-DRIVEN SYSTEM IMPROVEMENT .............................................................................................. 190
Family Youth System Partner Round Tables ................................................................................................. 190
Office of Recovery Partnerships ...................................................................................................................... 191
Washington State Children’s Behavioral Health Statewide Family Network .......................................... 191
Statewide Youth Leadership Network ............................................................................................................ 192
FEDERAL SUD & MH FUNDING (Block Grants) ................................................................................................. 192
Substance Abuse Prevention and Treatment Block Grant .......................................................................... 192
MHBG: Community Mental Health Services Block Grant ........................................................................... 193
MHBG: COVID Supplemental Funding ........................................................................................................... 193
SAMHSA System of Care Expansion Grant .................................................................................................... 193
STATE PLANS
SOORP: State Opioid and Overdose Response Plan
Kris Shera
The executive sponsors for this plan are responsible for approving and overseeing the implementation
of the plan. They include:
• Charissa Fotinos (HCA)
• Michael Langer (HCA DBHR)
• Caleb Banta-Green (UW ADAI)
• Tao Kwan-Gett (DOH)
FACT SHEET
Full SOORP PDF
Roadmap to Recovery Planning Grant
Kris Shera
Housing Action Plan
Michael Donovan
SUBSTANCE USE PREVENTION and YOUTH ENGAGEMENT
Washington Healthy Youth (WHY) Coalition
Martha Williams
FACT SHEET
The coalition represents more than 15 state agencies and organizations and focuses on:

157
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Promoting changes in industry policy and practices
• Educating policy makers on prevention issues and best practices
• Monitoring impacts of policy on prevention
• Supporting prevention efforts through development and distribution of educational materials
and resources
• Increasing statewide education, collaboration, and partnerships to reduce youth access to
alcohol and marijuana use
School-based Prevention and Intervention Services
Carola Brenes
FACT SHEET
In 1989, the Washington State Legislature passed the Omnibus Alcohol and Controlled Substances Act
authorizing state agencies to conduct a variety of programs addressing the public’s concern about the
level and consequences of alcohol, tobacco, and other drug use. As a result, the Student Assistance
Prevention and Intervention Services Program (SAPISP), with a mix of local, state, and federal funds,
places prevention and intervention specialists in schools to implement comprehensive student
assistance programs addressing problems associated with substance use and violence. SAPISP funds are
distributed to each of the state’s nine Educational Service Districts (ESDs) as part of the Community
Prevention and Wellness Initiative (CPWI). Funding amounts are allocated to ESDs to support 80% of one
full-time position in each of the nearly 100 CPWI communities. The CPWI communities or school districts
provide a 20% match to support the prevention intervention specialist positions.
Suicide Prevention and Mental Health Promotion
Jen Hogge
FACT SHEET
The Health Care Authority (HCA) Division of Behavioral Health and Recovery (DBHR) funds Community
Prevention and Wellness Initiative (CPWI) coalitions as well as local community-based organizations,
private not-for-profits, and educational organizations for mental health promotion or suicide prevention
services. These communities implement a variety of mental health promotion or suicide prevention
programs. Programming includes both school and community based services, including the use of
evidence-based programs such as PAX Good Behavior Game, Second Step, Sources of Strength, Guiding
Good Choices, Primary Project, and QPR Gatekeeper Training that are effective at promoting mental
health and/or preventing suicide. Communities also provide Youth Mental Health First Aid trainings and
mental health and suicide prevention community awareness events. DBHR also facilitates an ongoing
mental health promotion/suicide prevention workgroup as part of the State Prevention Enhancement
Consortium. The workgroup was organized in March 2013 and meets 6-12 times per year to support the
work of the consortium.
State [SUD] Prevention Consortium and Plan
Alicia Hughes, CBO and Grants Supervisor, SUD Prevention and MH Promotion Section

158
SUBSTANCE USE AND RECOVERY SERVICES PLAN
FACT SHEET
The SPE Policy Consortium designs and implements the five-year Washington State Prevention Strategic
Plan. The Consortium is working to strengthen and support an integrated statewide system of
community-driven substance use disorder prevention, mental health promotion, and related behavioral
health issues. Twenty-six state agencies and organizations and tribal partners represented the
Consortium with more than 45 active members. The 2019 State Substance Use Disorder Prevention and
Mental Health Promotion Plan is implemented by five workgroups that meet on a regular basis and in
cooperation with statewide agencies have some focus on prevention and mental health promotion. The
following workgroups oversee the implementation of action plans to accomplish the goals and mission
of the plan:
The Washington Healthy Youth Coalition: Underage drinking and marijuana misuse/abuse prevention
www.starttalkingnow.org/about-us
Opioid Prevention Workgroup: https://www.theathenaforum.org/rx
Young Adults Alcohol and Marijuana Misuse/Abuse Prevention Workgroup:
https://www.theathenaforum.org/marijuana
Commercial Tobacco and Vapor Products Workgroup: https://www.theathenaforum.org/tobacco
Mental Health Promotion and Suicide Prevention Workgroup:
https://www.theathenaforum.org/mentalhealth
In 2011, the Consortium initiated the strategic planning process to develop a Five-Year Strategic Plan for
2012-2017. The Consortium used the Prevention Planning Framework, based on the Strategic
Prevention Framework (SPF), as the overall planning framework for this process. The SPF was originally
developed by the federal Substance Abuse and Mental Health Services Administration (SAMHSA).
SAMSHA’s SPF is a comprehensive planning process designed to help states and communities build the
infrastructure necessary for effective and sustainable prevention. The Consortium updates the Strategic
Plan every five years, with the last major update being the 2017-2022 plan. In November 2019, a needs
and resources assessment was completed and the Plan was updated at this time. The most recent
version can be found at: https://www.theathenaforum.org/substance-use-disorder-prevention-
and-mental-health-promotion-five-year-strategic-plan
WA SPF Rx: WA Strategic Prevention Framework for Prescription Drugs
Alicia Hughes
FACT SHEET
The HCA’s Division of Behavioral Health and Recovery (DBHR) will lead efforts to address the risks
misusing prescription drugs by implementing a collaborative strategic plan that will include prevention
campaign messaging, evidence-based prevention education, prescriber education, and increased
utilization of the Prescription Monitoring Program (PMP).
CPWI: Community Prevention and Wellness Initiative
Kasey Kates

159
SUBSTANCE USE AND RECOVERY SERVICES PLAN
CPWI Fact Sheet
The Community Prevention and Wellness Initiative (CPWI) is a community-focused approach to
preventing substance abuse in Washington State. It focuses Washington’s limited public resources in
nearly 100 high-need communities
Emergency Response Suicide Prevention Grant
Jen Hogge
FACT SHEET
The Health Care Authority (HCA) Division of Behavioral Health and Recovery (DBHR) funds the University
of Washington Medical Center (UWMC) Department of Psychiatry and Behavioral Sciences Behavioral
Health Institute (BHI) to support adults, 25 and older, who have attempted suicide or experienced a
suicidal crisis. The essential activities of the grant include:
Develop and implement a plan for rapid followup for adults after discharge from emergency
departments and inpatient psychiatric facilities.
Establish follow-up and care transition protocols to help ensure patient safety.
Provide, or assure provision of, suicide prevention training to community and clinical service providers
and systems serving adults at risk.
Provide suicide screening and assessment and appropriate referral for clinical treatment services
required identified in the assessment.
Provide enhanced services for domestic violence survivors and their dependents including a safe place
to stay if individuals are unable to remain safely in the home setting
Prescription Drug/Opioid Prevention
Alicia Hughes
FACT SHEET
To address the opioid crisis in Washington State, The Health Care Authority’s Division of Behavioral
Health and Recovery (HCA/DBHR) and partnering agencies support opioid and prescription medication
prevention strategies that align with the Washington State Opioid and Overdose Response Plan.
https://www.hca.wa.gov/assets/program/WashingtonStateOpioidandOverdoseResponsePlan-
final-2021.pdf
Prevention Workforce Development
Sonja Pipek
FACT SHEET
The Health Care Authority’s Division of Behavioral Health and Recovery (DBHR) has contributed to
expanding the reach and impact of prevention services in throughout the state. DBHR provides
opportunities for new and current prevention providers to continue their education, as well as
opportunities for high school and college students to train into prevention via our Fellowship and

160
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Internship programs. DBHR allows prevention professionals to earn their Certified Prevention
Professional (CPP) to continue to elevate the field of prevention in the continuum of behavioral health
services.
OUTREACH, CRISIS RESPONSE, and SERVICE ENGAGEMENT
Washington Recovery Helpline: 1-866-789-1511
Ryan Keith
FACT SHEET
The Washington Recovery Help Line (the Help Line) is a statewide telephone service and website that is
available 24 hours a day, 365 days a year: 1-866-789- 1511 and www.warecoveryhelpline.org. The Help
Line provides information, referrals, online educational resources, and emotional support, along with a
listing of behavioral health job openings and resumes and a quarterly newsletter.
A Medication Assisted Treatment Locator Database is available on the Help Line website, providing
clients, community members, and professionals with information on where FDA-approved Medications
for Opioid Use Disorder (e.g., Methadone, Naltrexone, Buprenorphine) are available in local
communities. As of October 2021, it lists 644 clinics/programs and 2,852 individual prescribers of
MOUD.
The Help Line provides services to:
Behavioral health professionals, primary health care providers, employers, and other referral sources.
Parents, other family members, friends and others seeking information about how to intervene with
someone who needs help.
People seeking assessment/treatment for themselves.
988 Behavioral Health Crisis Line and Mobile Crisis Services
Matt Gower
HB 1477, the Crisis Call Center Hubs and Crisis Services Act, enhances and expands behavioral health
crisis response and suicide prevention services for all people in Washington State. The work is supported
by recommendations from the Crisis Response Improvement Strategy (CRIS) committee. The 988 dialing
code will be available nationally for call, text, or chat beginning July 15, 2022. Increased collaboration
between crisis service providers aims to reduce the use of emergency room and police departments,
while increasing options for those in crisis and improving system coordination around access to care.
988 Crisis Line Implementation
Crisis Response Improvement Strategy (CRIS) committee
Native and Strong Lifeline is a line dedicated to serving American Indian and Alaska Native individuals
calling the 988 crisis line, working in partnership with the Indian Behavioral Health Hub, a resource
support line for tribes, urban Indian organizations, families, and non-tribal providers who support tribal

161
SUBSTANCE USE AND RECOVERY SERVICES PLAN
and urban Indian communities to identify resources and follow up with those accessing the 988 crisis
line
IMC Engagement and Outreach behavioral health coverage
Service Encounter Reporting Instructions (SERI), published April 2022 >> Engagement and
Outreach (page 140)
PATH: Projects for Assistance in Transition from Homelessness
Lisa Bennet Perry
PATH Fact Sheet
Peer Pathfinder
Lisa Bennett-Perry
FACT SHEET
The Peer Pathfinder Projects build on the already established DBHR Projects for Assistance in Transition
from Homelessness (PATH) program to provide substance use disorder (SUD) peer recovery support in
emergency rooms and homeless encampments. The project links individuals to treatment options to
include Medication for Opioid Use Disorder (MOUD). In Washington State, SUD peer counseling is an
approved Medicaid service. Peer counseling is provided by certified peer counselors who have met state
requirements, taken the approved classes, and passed the state test. Peer counselors use their own
recovery stories in helping others develop hope and improve their lives. Peer Pathfinder SUD Peers
assist individuals in navigating and obtaining services to address barriers to independence and recovery.
These services address housing, financial resources, transportation, habilitation and rehabilitation
services, prevocational and vocational services.
Eligibility
Adults (age 18 or over), with one of the following conditions:
Individuals with Opioid Use Disorders (OUD) or
Stimulant Use Disorder (SUD) at risk of overdose or
Individuals who are suspected of Substance Use and who may be experiencing homelessness or who are
at risk of homelessness or
Individuals experiencing a substance use health crisis and are utilizing emergency room settings
Peer Pathfinder – Homeless Outreach (opioid use target)
Lisa Bennett-Perry
FACT SHEET
The Peer Pathfinder Projects build on the already established DBHR Projects for Assistance in Transition
from Homelessness (PATH) program to provide substance use disorder (SUD) peer recovery support in
emergency rooms and homeless encampments.

162
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The project links individuals to treatment options to include Medication for Opioid Use Disorder
(MOUD). In Washington State, SUD peer counseling is an approved Medicaid service. Peer counseling is
provided by certified peer counselors who have met state requirements, taken the approved classes,
and passed the state test. Peer counselors use their own recovery stories in helping others develop hope
and improve their lives.
Peer Pathfinder SUD Peers assist individuals in navigating and obtaining services to address barriers to
independence and recovery. These services address housing, financial resources, transportation,
habilitation and rehabilitation services, prevocational and vocational services.
Eligibility
Adults (age 18 or over), with one of the following conditions:
Individuals with Opioid Use Disorders (OUD) or
Stimulant Use Disorder (SUD) at risk of overdose or
Individuals who are suspected of Substance Use and who may be experiencing homelessness or who are
at risk of homelessness or
Individuals experiencing a substance use health crisis and are utilizing emergency room settings
HOST: Homeless Outreach Stabilization Transition (HOST) expansion
Meta Hogan
HOST Fact Sheet
The Homeless Outreach Stabilization and Transition (HOST) program provides outreach-based treatment
services to individuals with serious behavioral health challenges including substance use disorder (SUD).
Multidisciplinary teams can provide SUD, medical, rehabilitative, and peer services in the field to
individuals who lack consistent access to these vital services.
HOST eligibility means that an individual has a behavioral health challenge, which can include SUD with
or without co-occurring mental illness, that is untreated, under-treated or undiagnosed, and is
experiencing literal or chronic homelessness. HOSTeligible individuals will also be experiencing
behavioral health symptoms that create a barrier to accessing and receiving conventional behavioral
health services and outreach models
LOCATIONS
In SFY22, the HCA’s Division of Behavioral Health and Recovery (DBHR) will contract four Behavioral
Health Administrative Services Organizations covering five regional service areas:
• King County
• Southwest Washington
• North Sound
• Pierce
• Thurston Mason

163
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The BH-ASOs subcontract HOST services to licensed community behavioral health agencies. DBHR also
contracts with the Downtown Emergency Services Center to provide technical assistance to HOST
providers
SSP: Syringe Service Programs (DOH)
Chelsie Porter
SYRINGE SERVICE PROGRAMS – DOH program info page
Syringe Service Programs provide supplies for safer drug use to prevent health issues including
infectious disease, skin and soft tissue infections, and overdose, as well as other services including:
Outreach and engagement for people who use drugs;
Infectious disease testing/treatment
Low barrier medications for opioid use disorder
Overdose education and naloxone distribution
Case management
Vaccinations
Wound care
Reproductive health
Overdose Education and Naloxone Distribution (DOH)
Sean Hemmerle (DOH), Sue Green (HCA)
DOH Program Info web page
FACT SHEET
Program that offers free naloxone kits, overdose response training and technical assistance to
organizations interested in distributing naloxone to people at risk of opioid overdose.
Works with Washington State-based organizations that can distribute naloxone to the people most likely
to experience or respond to an overdose: people who use drugs and their friends and family. Prioritizes
applications from organizations that do not have the ability to bill insurance, such as syringe service
programs, jails, street outreach teams, etc.
The Washington State Health Care Authority’s (HCA) Division of Behavioral Health and Recovery (DBHR)
is partnering with the Washington State Department of Health (DOH) to provide overdose response
training and distributing naloxone through syringe exchange programs, local agencies, physical health
settings, and emergency services.
Activities engage professional, first responders, local and regional stakeholders, and health care
providers to reduce overdose risk and deaths among people who use heroin and prescription opioids.
HCA DBHR contracts with DOH to carry out the program.

164
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Per the Naloxone Distribution Plan, DOH has taken the lead on naloxone distribution and overdose
response training.
This program is one of the strategies developed by the State Opioid Overdose Response Plan under the
authority of Executive Order 16-109 with the purpose of preventing opioid overdose and deaths from
opioid overdose, and building local infrastructure to plan, implement, evaluate, and fund overdose
prevention efforts in the long-term.
The objectives are:
1) equip lay responders and professionals with overdose response training/naloxone through access at
local agencies/entities;
2) educate health care providers, local agencies, syringe exchange programs, and emergency services on
opioid guidelines, patient overdose education, opioid use disorders, and naloxone distribution; and
3) build and harmonize data infrastructures to inform resource allocation, maintain overdose
surveillance, and measure outcomes;
4) make sure there is not overlap of naloxone distribution between this program and the WA-PDO
program; and
5) work closely with HCA DBHR to develop a sustainability plan, to include funding, in preparation for
the WA-PDO grant expiring in August 2026.
5195: Distributing Opioid Overdose Reversal Medications
Laura Meader
(2SSB 5195) Helps to increase access to Naloxone for all individuals at risk of an opioid overdose. The
law requires hospital emergency departments and many certified and licensed behavioral health
settings to distribute prepackaged naloxone to individuals at risk of opioid overdose.
Informational web page
RNP: Recovery Navigator Program
Suzanne Straub
RNP Fact Sheet
The Recovery Navigator Program (RNP)is a statewide effort, in partnership with Behavioral Health
Administrative Organizations (BH-ASOs), to provide community-based outreach, intake, assessment, and
connection to services. These services support individuals with substance use disorder (SUD), including
individuals with co-occurring substance use disorders and mental health conditions. Before receiving
funding, each BH-ASO submitted a regional recovery navigator program plan that demonstrated the
ability to implement statewide program standards.
The RNP framework incorporates harm reduction and trauma-informed care principles to support the
individual throughout their recovery journey. Coordination and communication between regional RNP
staff, law enforcement, prosecutors, medical providers, and community partners is essential to the

165
SUBSTANCE USE AND RECOVERY SERVICES PLAN
success of each individual. RNP staff facilitate and coordinate connections to a broad range of
community resources for youth and adults including treatment and recovery support services (RSS).
Uniform Program Standards
RCW 71.24.115
LEAD: Law Enforcement Assisted Diversion
Michele Gayle
RCW 71.24.589 – Law enforcement assisted diversion – pilot project
As a result of SSB5380, HCA partnered with the PDA’s National Support Bureau to expand
availability of LEAD programs outside of King County. In 2020, HCA contracted with four
different sites to provide, develop, and implement LEAD programs:
Whatcom County
Snohomish County
Mason County
Thurston County
Mental Health Field Response Teams/Co-Responders
Keith Lewis
Trueblood Program (Mental Health Field Response): The Mental Health Field Response Grant Program
(RCW 36.28A.440) provides grants to local police and sheriff’s departments to improve the interactions
between the public and law enforcement. Mental health professionals assist patrol officers in the field
or in an on-call capacity, they also provide training on best practices. These innovative partnerships
reduce the possibility of using force and improve public safety overall. Instead of booking someone into
jail, they may be connected with services or diverted to a more appropriate facility for care. The
program is one of the ways your local law enforcement is working to find solutions for communities.
VIDEO: Washington State Co-Responder Program
FUNDING: Received 2 million GF-S ESSB 5092§215§83 “$2,000,000 of the general fund—federal
appropriation is provided solely for grants to law enforcement and other first responders to include a
mental health professional on the team of personnel responding to emergencies.”
Alternative Response Teams
Liz Wolkin
Funding is provided for the Authority to support efforts by counties and cities to implement local mobile
intervention response teams to provide therapeutic alternatives in the community resulting in reduced
contact with first responders. These services aim to reduce the number of people with behavioral health
(mental and substance use disorders) that use costly interventions such as jail, emergency rooms, and
hospitals, and to reduce the utilization of calls to the Emergency Management System from individuals

166
SUBSTANCE USE AND RECOVERY SERVICES PLAN
who are not getting their medical needs met due to lack of self-care, community support, or connection
to resources.
FUNDING: This includes $2 million in ongoing funds for a grant to the Association of Washington Cities;
$1.6 million in onetime funding for Whatcom County for facility renovation, equipment, and an
alternative transport vehicle; and $587,000 in ongoing operational support for the Whatcom County
alternative response base station. (General Fund-State).
AJA: Arrest and Jail Alternative Program
Michele Gayle
HCA holds a Memorandum of Understanding and provides contractual oversight in collaboration with
the Criminal Justice Training Center (CJTC) and Washington State Association of Sheriffs and Police
Chiefs (WASPC)
Arrest and Jail Alternatives Law Enforcement grant program
RCW 36.28A.450 Grant program – therapeutic interventions for certain criminal justice system
involved persons
COMMUNITY ASSESSMENT and TREATMENT
Fee-for-Service Program for American Indian/Alaska Natives
Yvonne Keller
FACT SHEET
Clients who have active Apple Health benefits but are not enrolled in a managed care plan may qualify
for fee-for-service behavioral health benefits.
This program was created in response to concerns expressed by the Washington State Tribes and the
Urban Indian Health Organizations. Individuals enrolled in Washington Apple Health (Medicaid) who
identify as American Indian and/or Alaska Native (AI/AN) and are exempt from requirement to enroll in
a managed care organization for physical and behavioral health (substance use disorder and mental
health) treatment.
Fee Schedules (list of cost-per-service that providers collect when the provide these services under the
FFS plan)
Fee-for-service SUD services fee schedule (as of July 2022)
Fee-for-service MH services fee schedule (as of July 2022)
Fee-for-service Specialized MH fee schedule (as of July 2022)
Mental Health Assessments for Young Children
Kimberly “Kiki” Fabian; Christine Cole

167
SUBSTANCE USE AND RECOVERY SERVICES PLAN
FACT SHEET
Youth Substance Use Disorder Treatment Services
Amy Dura
FACT SHEET
Eligibility requirements
Services are available for youth with SUD who meet ASAM criteria for a specific level of care. Youth are
assessed to determine diagnosis, medical necessity, and to recommend appropriate level of treatment.
Apple Health (Medicaid) and low-income, youth ages 13-17 who struggle with substance use are eligible
for services; younger youth or transition-age youth may receive services in some levels of care if
assessed as developmentally appropriate.
Priority is given to youth who are pregnant, use drugs intravenously, are referred from a higher level of
care or secure withdrawal management and stabilization (SWMS) referrals, as well as at-risk/runaway
youth.
The Health Care Authority (HCA) contracts with regional behavioral health administrative services
organizations (BH-ASOs), and managed care organizations (MCOs) to ensure service needs are met for
Medicaid-funded youth in their region. Organizations may set sliding fee scales or non-Medicaid funding
to accommodate youth in greatest need so that funding is not a barrier to youth access.
A youth 13 and older may access outpatient or residential services by signing themselves into treatment,
including cases of a Child in Need of Services (CHINS) petition. A youth under the age of 13 would need
consent of a parent or guardian. Parents or guardians may initiate treatment for non-consenting youth
through:
Family Initiated Treatment (FIT)
The Involuntary Treatment Act (ITA)
Children’s Long-Term Inpatient Program
LaRessa Fourre, Mandy Huber
FACT SHEET
The Children’s Long-term Inpatient Program (CLIP) is the only publicly funded, long-term inpatient
program for youth in Washington State where youth ages 5-17 years old may be voluntarily committed
and those from 13-17 years old may be involuntarily committed. Four CLIP inpatient psychiatric facilities
have a total of 94 funded beds. These facilities are:
The state psychiatric hospital for children and youth, Child Study and Treatment Center (CSTC), in
Lakewood. CSTC is under the authority of the Behavioral Health Administration (BHA) within the
Department of Social and Health Services (DSHS).
Contracted community-based facilities include:

168
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Two Rivers Landing, Yakima
• Tamarack Center, Spokane
• P
earl Youth Residence, Tacoma
WISe: Wraparound with Intensive Services
Tina Burrell
FACT SHEET
WISe provides comprehensive behavioral health services and supports to Medicaid-eligible youth
through age 20 years of age, with complex behavioral health needs. It is focused on the children in our
state with the most intensive, cross-system needs. Providing behavioral health services and supports in
home and community settings, crisis planning, and face-to-face crisis interventions are critical and
required components of the program.
Healthy Transitions Project
Amy Dura
FACT SHEET
The Healthy Transitions Project (HTP) is designed to improve emotional and behavioral health
functioning for transition-age youth and young adults, age 16 to 25 (referred to as TAY hereafter), to
increase self efficacy and maximize their potential to lead full and productive lives. The goal is to support
targeted, effective services statewide through infrastructure development.
Family Initiated Treatment
Enos A. Mbajah
FACT SHEET
A parent or guardian may bring their youth, to a participating outpatient behavioral health provider,
evaluation and treatment(EandT) facility, inpatient facility (licensed under RCW 70.41, 70.12, or 72.23),
a secure withdrawal management facility, or approved substance use disorder (SUD) treatment program
and request an evaluation to determine if the youth need mental health (MH) and/or SUD treatment.
The youth’s consent is not required.
The health care authority (HCA) developed 3 FIT training modules for youth, parents/guardians,
providers, and the community at large. Modules 1 and 2 provide background information and address
what is in the law, while module 3 is focused on best practices for treatment engagement.
Fetal Alcohol Syndrome Diagnostic and Prevention Network (FAS DPN)
Sarah Pine
FACT SHEET
The WA FASDPN:
Provides 100 percent of the state’s interdisciplinary FASD diagnostic and treatment referral services to
individuals with fetal alcohol exposure from birth to 22 years old.

169
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Provides FAS screening and surveillance for high-risk populations.
Identifies and refers high-risk women to intervention programs.
Developed evidence based FASD screening, diagnostic, and intervention tools through its translational
research program.
Provides FASD training to community professionals
Substance Use Disorder Outpatient Treatment and Residential Services
Patricia Dean, Gayle Martinsen
FACT SHEET
BH-ASO: Behavioral Health Administrative Service Organizations
FACT SHEET
BH-ASOs provide certain behavioral health services for anyone, regardless of their insurance status or
income level
Map
Contract
Behavioral Health Agencies (BHA)
The Washington State Dept of Health (DOH) licenses and regulates inpatient and outpatient Behavioral
Health Agencies that may be certified to provide mental health, substance use disorder (SUD), problem
gambling disorder services, or any combination of these types of services (OTPs are considered a BHA
and require additional steps for licensing and accreditation)
BHA Directory (updated December 2021)
RCW 71.24.037 Licensed or certified behavioral health agencies and providers – minimum
standards – investigations and enforcement actions – inspections
Medicaid State Plan
The State Plan is the officially recognized statement describing the nature and scope of Washington
State's Medicaid Program. A State Plan is required to qualify for federal funding for providing Medicaid
services. Essentially, the Plan is our state's agreement that it will conform to the requirements of the Act
and the official issuances of United States Department of health and Human Services (DHHS).
Medicaid (Title XIX) State Plan
Medicaid Services (P. 57- 84)
State Plan Amendments (SPAs) by year (2015-2021)

170
SUBSTANCE USE AND RECOVERY SERVICES PLAN
SPA- Medications for Opioid Use Disorder
Adult Withdrawal Management Services
Gayle Martinsen
Fact Sheet
SWMS: Secure Withdrawal Management and Stabilization
Zephyr Forest
SWMS Fact Sheet
Evaluation & Treatment (E&T) Facilities
Allison Wedin, Involuntary Treatment Administrator; Zephyr Forest, SWMS Coordinator
E&T Fact Sheet
An Evaluation and Treatment Facility (E&T) is any facility which can provide directly, or by direct
arrangement with other public or private agencies, emergency evaluation and treatment, outpatient
care, and timely and appropriate inpatient care to persons suffering from a mental disorder, and which
is licensed or certified as such by the Department of Health. The Health Care Authority may certify single
beds as temporary evaluation and treatment beds under certain circumstances.
There are 2 types of E&T Facilities:
1. Freestanding E&Ts are licensed as a Residential Treatment Facilities (RTF) and certified by Department
of Health for E&T services.
2. Hospital based E&Ts are licensed as hospitals (either a community hospital or psychiatric hospital) and
certified by Department of Health as E&Ts.
Involuntary Treatment / ITA
Alison Wedin
FACT SHEET
The Involuntary Treatment Act (ITA) provides the statutory framework for civil investigation, evaluation,
detention, and commitment of individuals experiencing a mental disorder or a substance use disorder
whose symptoms are so acute that the individual may need to be treated on an involuntary basis in an
Evaluation and Treatment facility (E&T) or Secure Withdrawal Management and Stabilization facility
(SWMS). ITA governs the actions of Designated Crisis Responders (DCRs), law enforcement, health care
providers, and the court process in terms of:
Conducting investigations and evaluations to determine if an individual meets criteria for emergent or
non-emergent involuntary detention and treatment;

171
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Writing petitions so that the court may order an involuntary commitment;
Testifying in court proceedings;
Monitoring compliance for individuals who have been released from commitment under a Less
Restrictive Alternative order.
Long Term Civil Commitment Bed Capacity (90 or 180 days)
Margo Miller
FACT SHEET
Trueblood Programs
Kara Panek, Adult Behavioral Health Section Manager
Trueblood Misdemeanor Diversion
Outpatient Competency Restoration
Forensic HARPS
Forensic PATH
Forensic Peers
Intensive Outpatient and Partial Hospitalization Pilot Program
Enos A. Mbajah
FACT SHEET
During fiscal year 2021, the Health Care Authority (HCA) was tasked with implementing the Intensive
outpatient and partial hospitalization (IOP/PHP) pilot program. Additional funding was provided to
extend the pilot program through 2023. The overarching goal of the pilot is to gather information to
determine if these benefits should be added to the state Medicaid plan.
Intensive Residential Teams – Discharge Wraparound Services
Matt Gower
FACT SHEET
Intensive Residential Teams (IRT) are designed to work with people being discharged or diverted from a
long-term civil commitment or state hospital who have struggled to remain in their community settings
such as adult family homes (AFH) or assisted living facilities. These teams provide intensive mental
health care to the individual in their facility to help them transition to a lower level of care.

172
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The need
The need for this new service was identified as part of a systematic review of the state hospital
discharge process. An informal gap analysis was conducted with state agencies and partners. A gap in
services was identified for people in the hospital slated for discharge to DSHS/ALTSA facilities. Some of
these individuals require intensive support so that they can adjust to their new setting and minimize the
risk of returning to an inpatient level of care or even to a state hospital.
The teams
IRT teams provide services 5 days a week over multiple shifts covering at least 12 hours a day. They work
with individuals with a serious mental illness who live in AFHs or assisted living facilities after discharge
or diversion from a state hospital. Services will be delivered in the ALTSA facility and other appropriate
community settings.
Teams consist of:
A half time dedicated prescriber
A Registered Nurses (RN)
Mental Health Professionals (MHP)
Certified peer counselors
The teams provide recovery focused treatment to promote stability, safety, and help the individual
transition to a lower level of care. The teams provide medication management to the clients and
primary mental health services based on the individual’s need. IRT teams will use cognitive behavioral
therapy for psychosis (CBT-p) as part of their approach.
PACT: Program of Assertive Community Treatment
Matt Gower
PACT Expansion FACT SHEET
PACT is an evidence-based practice which when adopted to fidelity, provides a cost effective method of
service delivery to reduce hospital, emergency services, and jail utilization. PACT teams are a
multidisciplinary team that serve people with severe mental illness who frequently need psychiatric care
or other crisis services. PACT teams come in different sizes, but every PACT team provides care 24/7 and
consist of:
• A psychiatric prescriber
• A team leader
• Registered nurses

173
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• Master’s level mental health professionals
• Substance use disorder professional
• Vocational and housing support
• Peer supports
PACT teams bring their support to the client where they live. This includes taking medication to the
client and transporting them to support their recovery and promote independence. The teams will work
the individual to build skills and work to graduate to a lower level of care.
EXPANSION
Prior to expansion there was 15 PACT teams in Washington: 7 full teams and 8 half teams. They serve
about 1250 individuals with severe mental illness across the state. The need for PACT teams was
established through community feedback and by using a gross estimation method called the Cuddeback
method1 which estimates that .6% of the adult population with severe mental illness. The University of
Washington approximated there are possibly 4,400 individuals in Washington who could benefit from
PACT: a possible difference of about 3,350 from 2018a levels. Not all in this method would be
appropriate or want PACT, but it confirmed the need identified in community discussions
To begin bridging this gap, the Legislature made an appropriation in the operating budget ESHB 1109,
Section 215 (4) for the HCA to stand up three full and two half teams in FY 2020 and more teams
planned for FY2021.
This is intended to increase the capacity to serve individuals in their community and keep them out of
the state hospitals, increasing capacity to serve 700 more individuals.
Five new teams (three full and two half) were added in FY 2020. In FY 2021, 2 new full teams were
added. The third and final team was identified and was being vetted. In FY2020, 1 full PACT team closed
and its replacement was being vetted with the last new team and replacement team to provide services
in spring 2022.
BHITF: Behavioral Health Intensive Treatment Facilities
Matthew Gower
FACT SHEET
During a systematic review of the state hospital discharges, a group of people were identified that no
longer benefited from treatment but were unable to discharge due to the need for further treatment
and no appropriate facility able to provide it.
To meet this need, the legislature established a new facility called Behavioral Health Intensive
Treatment Facilities (BHITF). These facilities have beds for up to 16 people to live in and receive active
rehabilitative treatment. A clinical staff will work to provide recovery-based treatment using evidence-
based practices, independent living skills training, social skills, and community integration. These
facilities will be staffed 24/7 with a clinical team to work with the individual all hours of the day if

174
SUBSTANCE USE AND RECOVERY SERVICES PLAN
needed. The facilities are designed to be residences for the individuals that live there. Individuals will
only be discharged from the facility if they complete their treatment plan objectives and can be safely
served within the community in a less-structured setting. The facility will allow for limited egress from
the facility by monitoring individuals leaving the facility and providing staff when they individual
presents as a risk to themselves or others.
The legislature has provided operation and capital funds to operate four facilities in the state. Selection
for the capital funds for 3 facilities was announced in October through the Department of Commerce’s
Behavioral Health Facilities Grant Program spring competitive process. The chosen facilities will be
located in:
• Chewelah
• Renton
• Tacoma
All three facilities are still working through building permit issues to start construction. Capital funds for
2 more facilities was included in the FY22-23 capital budget.
Integrated Managed Care (Apple Health/Medicaid) behavioral health coverage
Service Encounter Reporting Instructions (SERI), published April 2022
• Substance Use Service Modalities (pg. 101)
• Other Substance Use Services (pg. 122)
• Other Behavioral Health Services (pg. 132)
RSAT: Residential Substance Abuse Treatment (RSAT)
Grace Burkhart, Michelle Gayle
In response to the national rise in substance use and substance related violence, the Residential
Substance Abuse Treatment program was created by the Violent Crime Control and Law Enforcement
Act of 1994 (Public Law 103-322). The RSAT Program assists state, local and tribal governments in
development and implementation of substance use disorder treatment programs in state, local, and
tribal correctional and detention facilities. RSAT also has a focus on evidence based, community
reintegration, providing mental, behavioral, and social health services, to reduce substance use,
substance use related violence, and incarceration.
More information on the RSAT Program may be found here: BJA RSAT Overview.
Currently contract with Jefferson County and Island County jails to provide SUD treatment services and
transition to aftercare services.
OTN: Opioid Treatment Networks
Megan Fowler
**Funding expired September 29, 2022

175
SUBSTANCE USE AND RECOVERY SERVICES PLAN
FACT SHEET
The Division of Behavioral Health and Recovery (DBHR) received funding from the Substance Abuse and
Mental Health Services Administration (SAMHSA) in 2018 for the State Opioid Response (SOR) grant to
develop the Opioid Treatment Network model. This was known as SOR I (year 1 and 2). DBHR was
awarded an extension for SOR I to continue through September 29, 2022 specified as SOR II. SOR Opioid
Treatment Networks (OTNs) The Opioid Treatment Networks (OTNs) are second generation Hub and
Spoke treatment sites that serve patients with opioid use disorder (OUD).
LOCATIONS
OTNs are positioned to provide Medication for Opioid use Disorder (MOUD) in non-traditional
treatment settings. There are 15 OTNs sites located in Washington State. They are located at:
• 7 emergency departments;
• 5 jails;
• a syringe exchange;
• a shelter;
• and a fire department.
OTNs have increased access to medications for opioid use disorder across the state. The initiation sites
are the contract holders and receive funding from DBHR – distribution of funding to OTNs was
prioritized based on data of highest need and location of each project to best reach the populations at
most risk for overdose and death. Each OTN is responsible for providing individuals with their initial
induction onto MOUD. Each OTN is staffed with a medical provider, nurse care manager, care navigator
and data collector to reduce barriers for individuals seeking services at their site. SOR II requires
additional services, including providing Viral Hepatitis and HIV screening and referrals. In SOR II, OTN
sites are allowed to use funding to treat stimulant use disorder in addition to OUD. Sites are encouraged
to refer or use Contingency Management to treat stimulant use disorder.
ELIGIBILITY
Individuals participating in the OTNs must meet the Diagnostic and Statistical Manual of Mental
Disorders (DSM 5) diagnostic criteria for OUD (and/or stimulant use disorder) and meet state and
federal eligibility requirements for admission.
Opioid treatment programs (OTP)
Jessica Blose
Provide opioid use treatment services for people enrolled in Apple Health (Medicaid)
OTP Directory (updated Jan 2022)
Hub and Spoke Projects for MOUD
Linda Barker, Lora Weed

176
SUBSTANCE USE AND RECOVERY SERVICES PLAN
FACT SHEET
Connects a network of community providers around a central hub that offers medications for opioid use
disorder (MOUD) compound to all patients seeking services for opioid use disorder
Hub and Spoke Directory
LOCATIONS (11):
Cascade Medical Advantage • Whatcom, Skagit, Snohomish, Island, San Juan Counties
Rainier Internal Medicine, dba Northwest Integrated Health • Pierce, Thurston Counties
Peninsula Community Health • Jefferson, Clallam, Kitsap Counties
Valley Cities Counseling and Consultation • King County
Harborview Medical Center • King County
Lifeline Connections • Clark, Skamania, Grays Harbor, Pacific Counties
Comprehensive Health Care • Yakima and Kittitas Counties
Ideal Options • Snohomish and Skagit Counties
Multicare Rockway Clinic • Spokane County
Olympic Peninsula Health Services • Jefferson and Clallam Counties
Northeast Washington Medical Group Providence • Pend Oreille, Stevens, and Ferry Counties
MOUD Nurse Care Manager Project
Linda Barker
FACT SHEET
The objective of the Nurse Care Manager project is to increase access to medication for opioid use
disorder services. Funding for this project is part of Governor Jay Inslee’s Executive Order 16-09,
addressing the Opioid Use Public Health Crisis.
ELIGIBILITY
For an individual to receive care through this project they must meet the Diagnostic and Statistical
Manual of Mental Disorders (DSM 5) diagnostic criteria for opioid use disorder (OUD) and meet state
and federal eligibility requirements for admission. Pregnant and intravenous drug users are priority
populations for admission.
LOCATIONS

177
SUBSTANCE USE AND RECOVERY SERVICES PLAN
DBHR contracted with nine organizations to hire a Nurse Care Manager to provide care coordination for
individuals with OUD and provide community outreach regarding OUD and medication for opioid use
disorder:
• Olympia Medical Center, Port Angeles
• Cascade Medical Advantage, Bellingham
• Columbia River Mental Health, Vancouver
• Columbia Valley Community Health, Wenatchee
• Community Health of Central Washington, Ellensburg
• Cowlitz Tribal Health, Tukwila
• Multicare Health Systems, Puyallup
• Peninsula Community Health Service, Port Orchard
• Rainier Internal Medicine, Pierce County Jail
Grant Support for Certified Community Behavioral Health Clinic Expansion (CCBHC)
Alex Stoker
FACT SHEET
The CCBHC Expansion grant program must provide access to services including 24/7 crisis intervention
services for individuals with serious mental illness (SMI) or substance use disorders (SUD), including
opioid use disorders; children and adolescents with serious emotional disturbance (SED); and individuals
with cooccurring mental and substance disorders (COD). SAMHSA expects that this program will provide
comprehensive 24/7 access to community-based mental and substance use disorder services; treatment
of co-occurring disorders; and physical healthcare in one single location.
The funding MUST be used in the following areas:
To support direct services in: (1) 24/7 Crisis Services, including 24-hour mobile crisis teams; (2)
screening, assessment, and diagnosis, including risk assessment; (3) patient-centered treatment
planning or similar processes, including risk assessment and crisis planning; (4) comprehensive
outpatient mental health and substance use CCHBC grants November, 2021 2 treatment services that
include the provision of appropriate psychotropic medications; (5) screening for HIV and Viral Hepatitis
(A, B, C).
To establish cooperative relationships with judicial officials/court systems and provided Assisted
Outpatient Treatment when ordered.
Establish an Advisory Work Group comprising individuals with mental and substance use disorders, and
family members, to provide input and guidance to the CCBHC on implementation, services, and policies.
Develop and implement plans for sustainability to ensure delivery of services once federal funds end.
Recipients should not anticipate the continued renewal of federal funding to support this effort.
Recipients will be asked to report on sustainability plans.
The funding MAY be used in the following areas:

178
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Up to $25,000 per year may be used to purchase Technical Assistance. If recipients do not need these
funds for TA, they may use it for other allowable activities under the grant.
Develop and implement tobacco and vaping cessation programs, activities, and/or strategies.
Conduct an analysis of barriers and facilitators to facilitate changes in services and local relationships
necessary to become fully certified.
Vocational and educational counseling aimed at assisting individuals receiving treatment to be able to
better integrate into their communities and live productive satisfying lives.
Partnering with local housing authority to integrate behavioral health supports into community housing.
CCBHC grant awardees (9):
• Peninsula Behavioral Health (Port Angeles, $2M)
• Comprehensive Healthcare (Yakima, $2M)
• Cascade Community Healthcare (Centralia, $2M)
• Community Health Association of Spokane (Spokane, $4M)
• Lake Whatcom Residential Treatment (Bellingham, $1.8M)
• Columbia River Mental Health Services (Vancouver, $4M)
• Okanogan Behavioral Healthcare (Omak, $733k)
• Lifeline Connections (Vancouver, $4M)
• Columbia Wellness (Longview, $2.3M)
Contingency Management (CM) Project
Amy Dura, Lora Weed, Linda Barker
Research evidence has shown that contingency management (CM) is the most effective intervention for
stimulant use disorder. Studies demonstrate that the use of CM is associated with a reduction in number
of days of stimulant use, stimulant cravings, new stimulant use, and HIV risk behaviors. Stimulant use
disorders not only have adverse effects on the physical and mental health of individuals, but they also
cause negative impacts on society. In the absence of a pharmacological treatment that is approved by
the U.S. Food and Drug Administration (FDA), practitioners rely heavily on behavioral and psychosocial
interventions and practices such as CM.
CM has been implemented at sites in two projects:
State Hub and Spokes (5 sites): The State Hub and Spoke project completed their CM trainings in
September 2021 and are currently working with WSU PRISM staff to implement their programs and
engage in fidelity monitoring.
State Opioid Response Projects (20 sites): The SOR projects for the CM training include the SOR Hub
and Spoke (6 sites) and the Opioid Treatment Networks (14 sites). The CM training start date for the SOR
sites is set for early 2022

179
SUBSTANCE USE AND RECOVERY SERVICES PLAN
BEHAVIORAL HEALTH SERVICES FOR INDIVIDUALS IN THE CRIMINAL LEGAL SYSTEM
Criminal Justice Treatment Account
Michele Gayle
Fact Sheet
RCW
The purpose of this funding is to increase the provision of substance use disorder treatment and
recovery support services to justice-involved individuals. These individuals present with pending criminal
charges or active enrollment in a Therapeutic Court program. A report created by the Department of
Social and Health Services (DSHS) Research and Data Analysis (RDA) division surveyed 27 drug courts in
Washington State and saw a 61% decrease in the rate of re-offending for individuals who participated in
Drug Court.3 In addition, a multi-site drug court evaluation conducted by the Justice Policy Institute
indicated that drug courts produce benefits of over $6,000 for every individual they serve and return as
much as $27 for every $1 invested.
Funding through the Criminal Justice Treatment Account (CJTA) falls under two categories:
Therapeutic court participants
Therapeutic Courts provide individuals the opportunity to obtain treatment services under a closely
monitored diversion program in lieu of the traditional trial track of the criminal justice system. The
Washington State Legislature has indicated that therapeutic courts may decrease re-offense, improve
the safety of the community, and improve the life of the participant.
Individuals with pending criminal charges
An individual may also receive CJTA-funded services outside of a therapeutic court environment. The
county, through the input of a local CJTA panel, can implement services under a local arrangement to
treat legally involved individuals that are not enrolled in a therapeutic court program. These
arrangements coordinate treatment services for individuals who have charges filed by a county
prosecutor and meet the eligibility requirements indicated in 71.24.580.
MOUD (Medication for Opioid Use Disorder) in Jails
Rachel Meade
Fact Sheet
RCW
Although currently there are some jails offering MOUD, not all Washington state jails offer a full MOUD
program. According to a recent Washington State University study, only 37% of Washington State jails

180
SUBSTANCE USE AND RECOVERY SERVICES PLAN
surveyed, provide MOUD to every individual identified as having an OUD. Barriers include funding,
staffing, stigma, and logistics.
A full MOUD in jails program will provide incarcerated individuals the opportunity for an OUD
assessment, evidence-based medication for OUD, sustained treatment throughout incarceration and
connection to continue treatment upon release or transfer. Overall benefits may include, reduction in
morbidity and mortality due to overdose, reduced re-offenses, reduced complications during
withdrawal, improved jail staff safety, cost savings, reduced transfers to emergency departments,
custodial costs, and overall improved relationships.
The MOUD in jails program contributes to the Washington State Opioid and Overdose Response Plan
under goal 2 by expanding low-barrier access to MOUD in state jails (2.2.1), providing alternative
funding to address the Medicaid gap for incarcerated individuals (2.2.10), and expanding access to and
utilization of behavioral health services, including opioid use disorder medications in the juvenile and
adult criminal legal systems, and improve effectiveness and coordination of jail re-entry services across
the state (strategy 2.4).
The MOUD in Jails pilot project is currently operating at the following facilities:
Facility
Clark County Sheriff
Cowlitz County Corrections
Enumclaw Jail Program - Valley Cities
Grays Harbor Public Health (Aberdeen, Hoquiam, Grays Harbor)
Issaquah
Kittitas County Jail
Nisqually Indian Tribe
Okanogan County Jail
Olympic Peninsula Community Clinic (Clallam County Jail)
Public Health Seattle King County (Seattle/Kent)
South Correctional Entity dba SCORE
Tacoma-Pierce County Health Department (Pierce)
Walla Walla County Corrections

181
SUBSTANCE USE AND RECOVERY SERVICES PLAN
WASPC (Ferry, Island, Stevens County Jails)
Whatcom County Sheriff's Office (Downtown Jail/Work Center)
Same Day MOUD Visits for people transitioning out of jails
Gayle Martinsen
The Governor’s Opioid Response Bill, SSB 5380, implemented several policies and programs related to
the current opioid epidemic in Washington State. The Opioid Response Bill included policy to expand the
use of Medications for Opioid Use Disorder (MOUD) and included funding for the purposes of ensuring
continuity of care for individuals being released from jail and are on MOUD.
The Health Care Authority, (HCA) Division of Behavioral Health and Recovery (DBHR) received legislative
appropriations for the purposes of ensuring same day transitional services for individuals being released
from city, county, and tribal jails. The funding is to provide a same day appointment for purposes of
continuing Medication for Opioid Use Disorder (MOUD) and transportation from the jail to the
community medical provider. HCA Currently contracts with Kitsap County, Benton County, King County,
and South Correctional Entity for the provision of transportation and an incentive payment to providers
to hold appointments so that individuals releasing from jail have no disruption in access to medication-
assisted treatment for opioid use disorder.
RCSP: Reentry Community Services Program
Alexander Stoker
FACT SHEET
The Reentry Community Services Program (RCSP) was created in 2000 by Senate Bill 5011 with the
intent to provide improved public safety and additional mental health treatment for dangerous mentally
ill, developmentally disabled and chemically dependent mentally ill individuals exiting a Department of
Corrections (DOC) facility. This program was previously known as Offender Reentry Community Safety
Program (ORCSP) until last legislative session.
ELIGIBILITY
DOC screens individuals to determine if they meet criteria. A statewide RCSP Review Committee
(cochaired by DOC and DBHR RCSP administrators) makes the final determination of entry into the RCSP
program and refers the individuals to the appropriate community behavioral health agency.
HOUSING PROGRAMS
DBHR Supportive Housing Team: Kimberly Castle, Wanda Johns, Nicole Mims, Craig Jacobson, Michael
Donovan, Lisa Bennett-Perry, Scott Tankersley, Maureen Bailey
Housing Action Plan
Michael Donovan, Forensic HARPS Program Manager

182
SUBSTANCE USE AND RECOVERY SERVICES PLAN
John Stovall who is heading up the work for WA Low Income Housing Alliance (WLIHA) on this project is
planning to provide HCA with recommendations based on their findings most likely in late September,
early October before completing the project.
HARPS: Housing and Recovery through Peer Services
Wanda Johns
HARPS Fact Sheet
Trueblood Forensics HARPS: Housing and Recovery through Peer Services
As part of the Trueblood settlement, the Health Care Authority (HCA) is setting up four Forensic Housing
and Recovery through Peer Services (HARPS) teams. These teams are staffed with people who have lived
experience with behavioral health challenges. This staffing model helps foster engagement with people
served by the Forensic HARPS team. The goal is to help participants overcome barriers, find housing and
maintain housing.
Summary Sheet
Recovery Residence Program
Kira Schneider
FACT SHEET
Recovery Residences are for people in recovery from substance use disorders. It provides a home-like
environment free from alcohol and illicit drug use with a focus on peer support, assistance with
obtaining addiction services, and other recovery services and support.
Eligibility requirements
Adults who are newly abstinent or in recovery and want a supportive living environment. Adults
participating in or completing treatment and who need supportive affordable housing. Adults who are
homeless or unstably housed and want a recovery focused environment with others in recovery.
Recovery residence levels
According to the National Alliance of Recovery Residences (NARR) and Substance Abuse and Mental
Health Services Administration (SAMHSA) there are four levels of Recovery Residences, ranging from a
democratically, peer run home (much like an Oxford House) to a Residential Treatment Facility for
people with substance use disorders. In Washington, these four levels have been divided between
housing (levels 1 and 2) and treatment (levels 3 and 4). Levels 3 and 4 are licensed and certified by the
Department of Health (DOH) using WACs 246-311- 1108(2) and 246-341-1112.
Registry of Level 1 and Level 2 recovery residences and Oxford houses
Foundational Community Supports (FCS): Supported Housing
Matt Christie, FCS program administrator

183
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Lisa Bennett-Perry, Supported Employment and Supportive Housing Administrator
FACT SHEET
FCS is currently one of 5 initiatives developed under Washington State’s 1115 Medicaid Transformation
waiver. In 2018, FCS began providing targeted supportive housing (SH) and supported employment (SE)
services to Medicaid beneficiaries with behavioral health needs and other risk factors. By focusing on
the social determinants of health, the program aims to promote health equity and selfsufficiency by
helping participants obtain and maintain housing and employment.
These Medicaid-reimbursable services do not replace services that are currently available, and they do
not pay for room and board or wages.
HCA has contracted with Amerigroup as the third party administrator (TPA) to authorize enrollments,
pay claims, and manage the FCS provider network.
Supportive housing services
These innovative services are demonstrating the positive health effects that safe and secure housing can
provide to people in need. To qualify, individuals must be Medicaid-eligible, complete a needs
assessment, and be experiencing one of the following risk factors:
• Chronic homelessness
• Dependence on costly institutional care
• Dependence on restrictive adult residential care/treatment settings
• An in-home care recipient with complex needs
• At high risk for expensive care and negative outcomes
PATH: Projects for Assistance in Transition from Homelessness
Lisa Bennet Perry
PATH Fact Sheet
MORE RECOVERY SUPPORT SERVICES
Foundational Community Supports (FCS): Supported Employment
Matt Christie, FCS program administrator
Lisa Bennett-Perry, Supported Employment and Supportive Housing Administrator
FACT SHEET
FCS is currently one of 5 initiatives developed under Washington State’s 1115 Medicaid Transformation
waiver. In 2018, FCS began providing targeted supportive housing (SH) and supported employment (SE)

184
SUBSTANCE USE AND RECOVERY SERVICES PLAN
services to Medicaid beneficiaries with behavioral health needs and other risk factors. By focusing on
the social determinants of health, the program aims to promote health equity and selfsufficiency by
helping participants obtain and maintain housing and employment.
These Medicaid-reimbursable services do not replace services that are currently available, and they do
not pay for room and board or wages.
HCA has contracted with Amerigroup as the thirdparty administrator (TPA) to authorize enrollments,
pay claims, and manage the FCS provider network.
Supported employment services
Supported employment services help people who have physical, behavioral, or long-term health needs
that make it difficult for them to find and maintain jobs. These ongoing services include individualized
job coaching and training, help with employer relations, and assistance with job placement. To qualify,
individuals must be Medicaid-eligible, complete a needs assessment, and be experiencing one of the
following risk factors:
• Eligible for the Housing and Essential Needs (HEN) or aged, Blind, Disabled (ABD) program.
• Significant mental illness, substance use disorder (SUD), or co-occurring conditions.
• A long-term care recipient with complex needs.
• Behavioral health challenges related to vulnerable youth and young adults
Peer Bridger Program
Annie Dejka
FACT SHEET
Peer Bridger staff deliver peer support services to individuals in state hospitals prior to discharge and
after their return to their communities. The Peer Bridger program serves those participants currently
admitted to Western or Eastern State Hospital and who have had lengthy hospitalizations or a history of
frequent tor multiple hospitalizations. Participation in the program is voluntary. The program is funded
by the Community Mental Health Services Block Grant (MHBG) funds.
Supported by ESHB 2376, Sec 204.1(v)
Mental Health Peer Respite Centers
Funding is provided for five mental health peer respite centers to divert individuals from crisis services
as well as a pilot program to provide mental health drop-in center services pursuant to Second
Substitute House Bill 1394 (Behavioral health facilities). The HCA must conduct a survey of peer mental
health programs and submit reports to the Legislature on the results of the survey and of the pilot
program.

185
SUBSTANCE USE AND RECOVERY SERVICES PLAN
HB 1394 – Concerning community facilities needed to ensure a continuum of care for
behavioral health patients
Clubhouse Services
Laura Robbins
In response to State v. Blake, HCA has started efforts to expand Clubhouse International and Peer Run
organizations. The expansion will include organizations who incorporate evidence-based practice
models such as Clubhouse International, Recovery Community Organizations, and Recovery Café
Clubhouse Directory – Washington State
Recovery Café Network
Substance Use Peer Support Services
SUD Peer Services Fact Sheet
Certified Peer Counseling (CPC) is an approved Medicaid service in Washington State. CPC pairs
individuals in recovery with trained counselors who share their life experience to help them find hope
and make progress toward recovery. Peer support services are included in both the mental health and
the substance use sections of the Medicaid State Plan, which allows appropriately licensed behavioral
health agencies to provide peer support services for both mental health and substance use disorders
and request Medicaid reimbursement.
PPW: Pregnant and Parenting Women Services
Sarah Pine
FACT SHEET
Pregnant and Parenting Women (PPW) services are designed to meet the needs of pregnant and
parenting women who are seeking services. PPW are a priority population for Federal Substance Abuse
Block Grant funding. PPW provides:
• SUD outpatient treatment services
• SUD residential treatment services
• Housing support services
• Therapeutic intervention for children
PCAP: Parent-Child Assistance Program
Sarah Pine
FACT SHEET

186
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The Parent Child Assistance Program (PCAP) is an evidence-informed program that provides intensive
case management and support services to pregnant and parenting women with substance use disorders
and their young children. Previous Safe Babies, Safe Moms (SBSM) sites transitioned to adopt the PCAP
model beginning in July 2017. There are currently 15 PCAP sites around Washington. PCAP services
include:
• Referral, support, and advocacy for substance use disorder treatment and continuing care.
• Assistance in accessing and using local resources such as family planning, safe housing,
healthcare, domestic violence services, parent skills training, child welfare, childcare,
transportation, and legal services.
• Linkages to health care and appropriate therapeutic interventions for children.
• Timely advocacy based on client needs.
ELIGIBILITY
Individuals are eligible if they meet all three of the following criteria:
Individuals who are currently pregnant or postpartum up to 24 months. Priority shall be given to women
who are pregnant and up to 12 months postpartum; referrals shall be accepted up to 24 months
postpartum on a space available basis.
Individuals who self-report at risk substance use (drugs and/or alcohol) during the current or recent
pregnancy.
Individuals who have not successfully accessed community resources for substance abuse treatment and
long-term recovery.
LOCATIONS
PCAP is available at 15 locations, now serving 20 counties:
• Clallam-Jefferson PCAP
• Kitsap PCAP,
• Thurston-Mason-Lewis PCAP,
• Grays Harbor-Pacific PCAP,
• Cowlitz PCAP,
• Clark PCAP,
• Pierce PCAP,
• King PCAP,
• Snohomish PCAP,
• Skagit PCAP,
• Whatcom PCAP,
• Chelan PCAP,
• Yakima PCAP,
• Benton-Franklin PCAP,
• Spokane PCAP

187
SUBSTANCE USE AND RECOVERY SERVICES PLAN
MANAGEMENT
Addictions, Drug and Alcohol Institute (ADAI) at the University of Washington provides quality
assurance, implementation fidelity, training, and evaluation of all PCAP sites around the state. Division
of Behavioral Health and Recovery (DBHR) program manager conducts contract reviews biennially.
Parent Trust: Parenting Education for Families in Recovery
Sarah Pine
FACT SHEET
Parent Trust Families in Recovery provides research based parenting education and family support
services for families in residential and outpatient substance use disorder treatment centers around
Washington. The overall goal is to strengthen bonding and parenting skills in families at high-risk for
child abuse and neglect/Adverse Childhood Experiences (ACEs).
Parents receive training and support to:
Increase parent-child bonding
Increase positive family management skills
Increase the family’s drug-free social support network
Increase child safety
Use our ACE Prevention Curriculum to decrease the number of Adverse Childhood Experiences (ACEs)
parents pass on to their children.
Support and educate parents on stress management and parenting skills during a pandemic.
Support parents and their children with online schooling during the pandemic.
ELIGIBILITY
Individuals that are pregnant or parenting and experiencing a substance use disorder.
High-risk for permanently losing custody of their children.
LOCATIONS
Parent Trust educational programs are currently available (as of Nov 2021) at the following locations:
• Catholic Charities of Central Washington
• Evergreen Recovery Centers
• Therapeutic Health Services
• Triumph Treatment Services
• New Horizons Care Center
• Partners with Families and Children
• Circle of Parents National Network

188
SUBSTANCE USE AND RECOVERY SERVICES PLAN
DATA COLLECTION and COORDINATION
Washington State Young Adult Health Survey
The Washington State Young Adult Health Survey measures marijuana and other substance use,
perceptions of harm, risk factors, and consequences among young adults (18 to 25 years old) living in
Washington State. Motivated by the passage of Initiative 502 in 2012, the survey began in 2014 before
recreational marijuana stores opened their doors.
FACT SHEET: Washington State Young Adult Health Survey
BHDS: Behavioral Health Data System
V5.1 Behavioral Health Supplemental Transaction Data Guide
PMP: Prescription Monitoring Program - DOH
The program was created to improve patient care and to stop prescription drug misuse by collecting
dispensing records for Schedule II, III, IV and V drugs, and by making the information available to
medical providers and pharmacists as a patient care tool. Program rules, WAC 246-470, took effect
August 27, 2011. The program started data collection from all dispensers October 7, 2011.
Informational website
RCW 70.225 Prescription Monitoring Program
Data for SOORP: State Opioid and Overdose Response Plan
Kris Shera
Currently under development, will collect population health data from DOH/PMP related to:
• Patients on high dose chronic opioid therapy > 90 mg MED
• New opioid patients who become chronic users
• Chronic opioid patients with concurrent sedative use
• Days of opioids supplied to new clients
ARM: Analytics and Research Measurement Dashboard Suite
Healthier Washington Dashboard
ARM Dashboard

189
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Recovery Asset Mapping Tool
Funding for the development of this tool is included as a SURSAC recommendation in the SURS Plan. A
demo version of this tool was presented at the February SURSAC meeting.
HCA Data Strategy and Supporting Five Year Plan
HCA 2021-2025 Data Strategy (full)
Data Strategy one-page overview
BEHAVIORAL HEALTH WORKFORCE EXPANSION
Behavioral Health Marketing Campaign
Steve Perry
FACT SHEET
The goal the Behavioral Health Marketing Campaign is to increased awareness of behavioral health
career opportunities by driving audiences to a mobilefriendly landing page with information about
behavioral health career opportunities, education programs, and financial aid resources.
Landing Page: https://www.startyourpath.org/
YouTube 30 sec Ad: Start your path: Explore behavioral health careers (30 sec. video) - YouTube
Behavioral Health Workforce Pilot Programs (ESSHB 1504)
Steve Perry
FACT SHEET
ESSHB 1504 appropriated funds to the Health Care Authority to establish three behavioral health
workforce pilot programs and a training support grants program for community Mental Health
providers, including clinical social workers, licensed mental health counselors, licensed marriage and
family therapists, clinical psychologist, and substance abuse treatment providers. The Health Care
Authority must implement these services in partnership with or through the regional accountable
communities of health or the University of Washington behavioral health institute.
Proviso 40: Criminal Background Check
Steve Perry
FACT SHEET

190
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The goal of the Proviso 40: Criminal Background task force is to reduce barriers in developing and
retaining a robust Behavioral Health workforce while maintain patient safety measures.
Proviso 74: Teaching Clinic Enhancement Rates
Steve Perry
FACT SHEET
Community behavioral health agencies routinely experience turnover rates of between thirty and fifty
percent while average vacancy rates run three to five months to fill clinical positions. The goal of Proviso
74 is to develop a funding mechanism that recognizes and compensates community behavioral health
agencies for performing a significant training function required for behavioral health workers to obtain
their educational degree and clinical licensure. A service that benefits the entire behavioral health
system.
Community mental health and substance use disorder treatment agencies often serve as training sites
for professionals seeking supervision hours to meet licensure requirements, but stakeholders
consistently report that the true costs incurred in this arrangement are not fully reimbursed, and may be
a net drain on these already lean community organizations. Too often, clinicians leave for better paying
jobs with lower acuity patients after completing their facility-sponsored supervision requirements.
The lack of compensation for serving as a training site, combined with high staff turnover adversely
impact the ability of these sites to meet the needs of individuals who need behavioral health services.
Recognizing and compensating sites for this function may help community-based agencies provide more
training opportunities, and may also lead to better retention. Providing compensation for this role
would partially address reductions in standard clinical productivity as a result of time spent supervising
new workers, enabling better absorption of the costs of high turnover.
COMMUNITY-DRIVEN SYSTEM IMPROVEMENT
Office of Behavioral Health Consumer Advocacy
Effective Date: July 25, 2021; Sections 15-17 take effect October 1, 2022
Authorized by ESHB 1086, the Department of Commerce has established the Office of Behavioral
Health Consumer Advocacy to provide behavioral health consumer advocacy services to patients,
residents, and clients of behavioral health providers or facilities.
Family Youth System Partner Round Tables
Kristen Roya, Patty King
FACT SHEET

191
SUBSTANCE USE AND RECOVERY SERVICES PLAN
Family Youth System Partner Round Tables (FYSPRTs) embrace the idea that youth and families can and
should have an active role in how systems serve them. FYSPRTs are a platform for families, youth, and
system partners to come together to collaborate, listen, and incorporate the voice of the community
into decision making at the regional and state level.
FYSPRTs are based on the System of Care core values:
• Family and youth driven
• Community based
• Culturally and linguistically appropriate
Washington has 10 regional FYSPRTs, one statewide FYSPRT, and multiple local FYSPRTs (where
applicable).
Office of Recovery Partnerships
Dakota Steel
FACT SHEET
The mission of the Office of Recovery Partnerships (ORP), formerly known as the Office of Consumer
Partnerships, is to ensure that service recipient’s individual involvement and communication is
embedded in behavioral health systems. The ORP takes an active role in representation of these
individuals in internal agency activities, promoting recovery and bringing this voice to the work of the
Division. The ORP Manager participates in a leadership role and is on the Management Team. The ORP
also has responsibility for cultivating a recovery culture within state agencies.
Washington State Children’s Behavioral Health Statewide Family Network
Patty King, Kristen Royal
FACT SHEET
Through a contract with WSCC, the Washington State Children’s Behavioral Health Statewide Family
Network provides:
• Four workgroups to identify system trends related to children’s outpatient behavioral health
services, inpatient behavioral health services, peer support and family leader opportunities and
cross-system services. These workgroups meet monthly.
• Four committees to continue the network’s infrastructure development which includes
committees focused on equity, diversity and inclusion, social marketing and communication,
advocacy and leadership training and board of directors’ capacity and advisory committee
• A webinar every other month for the purpose of workgroup and committee updates and to
receive feedback on their work. The webinar can be attended by anyone interested.

192
SUBSTANCE USE AND RECOVERY SERVICES PLAN
• A webinar every other month in an open forum discussion format intended to engage family
leaders who do not participate in committees and workgroups but can also include those who
do.
• Annual weekend training to support parents/caregivers across Washington State.
• Annual Children’s Behavioral Health Summit
• Technical assistance to the regional Family, Youth, System Partner Round Tables to enhance
family engagement.
• Networking for parents/caregivers.
• Leadership and other trainings that include national trainers/experts
Statewide Youth Leadership Network
Kristin Royal
FACT SHEET
The purpose of the Statewide Youth Leadership Network (Youth Network) is to facilitate the
development of working relationships, a united voice and process for youth across Washington,
including youth run organizations and groups, to collaborate and partner in Washington State’s system
change initiatives. The Statewide Youth Leadership Network is also an integral piece to sustaining the
System of Care values in Washington State and will work in collaboration with the Washington State
Children’s Behavioral Health Statewide Family Network (Statewide Family Network).
FEDERAL SUD and MH FUNDING (Block Grants)
Substance Abuse Prevention and Treatment Block Grant
Janet Cornell
FACT SHEET
The Substance Abuse Prevention and Treatment Block Grant (SABG) supports states in planning,
implementing, and evaluating activities to prevent and treat substance abuse and/or illicit use of alcohol
and other drugs. The SABG supports critical services that Medicaid or other federal and state funds do
not cover, such as community prevention, recovery support services, education, training, and support
for individuals seeking services and their families.
A portion of the SABG funds are utilized to train peers with substance use disorder (SUD) to become
certified peer counselors and provides technical assistance to community behavioral health agencies
who want to add SUD peer services. Grant funds are acquired through an application process that
details how the state will spend the federal funds. Grants are awarded on an annual basis, and funding
comes through the Substance Abuse and Mental Health Services Administration's (SAMHSA) Center for
Substance Abuse (CSAT) and the Center for Substance Abuse Prevention (CSAP).

193
SUBSTANCE USE AND RECOVERY SERVICES PLAN
MHBG: Community Mental Health Services Block Grant
Janet Cornell
FACT SHEET
The Community Mental Health Block Grant (MHBG) supports states in reducing their reliance on
psychiatric inpatient services and facilitates the development of effective community-based mental
health services and programs. The MHBG supports critical services that Medicaid or state funds do not
cover, such as homeless services, housing assistance, crisis outreach, peer-operated programs including
mental health clubhouse services, help lines, and education, training, and support for individuals seeking
services and their families.
This program has the following specific goals:
• To ensure access to a comprehensive system of care including employment, housing, case
management, rehabilitation, dental services, and health services, as well as mental health
services and supports.
• To promote participation by individuals seeking services and their families in planning and
implementing services and programs, as well as in evaluating state mental health systems.
• To ensure access for underserved populations including people who are homeless, residents of
rural areas, and older adults.
• To promote recovery and community integration.
• To increase accountability through uniform reporting on access, quality, and outcomes of
services.
MHBG: COVID Supplemental Funding
Janet Cornell
FACT SHEET
Supplemental MHBG Covid Enhancement funding was provided to prevent, prepare for, and respond to
SMI and SED needs and gaps due to the on-going COVID-19 pandemic. The COVID-19 pandemic has
significantly impacted people with mental illness. Public health recommendations, such as social
distancing, are necessary to reduce the spread of COVID-19. However, these public health
recommendations can at the same time negatively impact those with SMI/SED. The COVID-19 pandemic
can increase stress, anxiety, feelings of isolation and loneliness, the use of alcohol or illicit substances,
and other symptoms of underlying mental illness.
SAMHSA System of Care Expansion Grant
Alan “Ace” Bulger, Sonya Wohletz
FACT SHEET

194
SUBSTANCE USE AND RECOVERY SERVICES PLAN
The Substance Abuse and Mental Health Administration (SAMHSA) awarded the System of Care (SOC)
expansion grant in September of 2018 for the improvement of behavioral health systems in Washington
that serve youth, families, and caregivers. The four-year grant is designed to work towards improving
long-term behavioral health outcomes and to minimize placements in restrictive settings, such as
hospitals, juvenile rehabilitation, and residential treatment. SOC funds direct services, including day
support services, intensive therapeutic foster care services, respite care, and also increases the
availability of school-based student support specialists.
195
SUBSTANCE USE AND RECOVERY SERVICES PLAN
